Professional Documents
Culture Documents
Psychology PDF
Psychology PDF
Uploaded by
Papato KongOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Psychology PDF
Psychology PDF
Uploaded by
Papato KongCopyright:
Available Formats
Pikes Peak Model for Training
in Professional Geropsychology
Bob G. Knight University of Southern California
Michele J. Karel Department of Veterans Affairs Boston Health Care
System and Harvard Medical School
Gregory A. Hinrichsen Albert Einstein College of Medicine and American
Psychological Association Congressional Fellow
Sara H. Qualls University of Colorado, Colorado Springs
Michael Duffy Texas A & M University
The aging of the population will increase demand for formal training in aging and felt they needed further training
psychological services for older adults, which challenges to work competently with older adults.
the profession of psychology to provide those services. In The past few decades have seen a growth in training
response to that challenge, professional geropsychology programs to prepare psychologists for work with older
has been developing over the past few decades to meet adults, but there has not been a comprehensive model for
current and prepare for anticipated future demand. The
development of a range of training opportunities is impor-
Bob G. Knight, Davis School of Gerontology and Department of
tant to enable psychologists to work effectively with older Psychology, University of Southern California; Michele J. Karel, De-
adults. This article describes the Pikes Peak model for partment of Veterans Affairs Boston Healthcare System and Depart-
training in professional geropsychology. The model is an ment of Psychiatry, Harvard Medical School; Gregory A. Hinrichsen,
aspirational, competencies-based approach to training Department of Psychiatry, Albert Einstein College of Medicine, and
American Psychological Association (APA) Congressional Fellow;
professional geropsychologists that allows for entry points Sara H. Qualls, Department of Psychology and Gerontology Center,
at multiple levels of professional development. University of Colorado, Colorado Springs; Michael Duffy, Counseling
Psychology Program, Department of Educational Psychology, Texas A
Keywords: aging, older adults, doctoral programs, intern- & M University.
ships, postdoctoral training This material is the result of work supported with resources from and
the use of facilities at the Boston VA Medical Center. Financial support
T
was provided by the Retirement Research Foundation; APA (council
he aging of the population at large and the corre- discretionary funds); Section II of APA Division 12, Society of Clinical
sponding aging of clients receiving psychological Geropsychology; APA Division 20, Adult Development and Aging; APA
services have been recognized for some time (e.g., Board of Educational Affairs; APA Committee on Division/APA Rela-
tions; APA Division 40, Clinical Neuropsychology; Association of Psy-
Knight, Kelly, & Gatz, 1992; Qualls, Segal, Norman, Nie- chology Postdoctoral and Internship Centers; APA Division 12, Society of
derehe, & Gallagher-Thompson, 2002). Workforce short- Clinical Psychology; APA Division 42, Psychologists in Independent
ages for geriatric mental health care are predicted to be Practice; and the Council of University Directors of Clinical Psychology.
significant (Center for Health Workforce Studies, 2005; We acknowledge consultation on postlicensure issues by Paula Hartmann-
Stein and Deborah Frazer.
Halpain, Harris, McClure, & Jeste, 1999; Jeste et al., 1999). We acknowledge the leadership of APA Division 20, Adult Devel-
Multiple factors contribute to the quickly growing need for opment and Aging, and Section II of APA Division 12, Society of Clinical
geriatric mental health services: the growing number of Geropsychology, in planning and providing leadership for the Pikes Peak
Conference. In addition to these two groups, the following APA divisions
adults over 65 years old (He, Sengupta, Velkoff, & DeBar- and other groups with an interest in this topic were represented by
ros, 2005); the aging of the baby boom cohort, which has delegates to the conference: APA Division 35, Society for the Psychology
higher rates of mental disorder than the current cohort of of Women; APA Division 40, Clinical Neuropsychology; APA Division
older adults (e.g., Koenig, George, & Schneider, 1994); 42, Psychologists in Independent Practice; APA Division 44, Society for
the Psychological Study of Lesbian, Gay, and Bisexual Issues; APA
rapid growth of the “oldest-old” population (those over 85 Division 45, Society for the Psychological Study of Ethnic Minority
years old), with associated complex mental health needs Issues; Section II of APA Division 12, Society of Clinical Geropsychol-
related to chronic illness, dementia, and long-term care; ogy; APA Division 20, Adult Development and Aging; Association of
and greater receptivity to mental health services among Psychology Postdoctoral and Internship Centers; and the Council of
Counseling Psychology Training Programs. Applications were sought for
cohorts now entering older age (Gatz & Smyer, 2001; Jeste et 19 at-large and 7 student delegate positions. The planning committee
al., 1999; Qualls et al., 2002). Qualls et al. (2002) found that chose these individual delegates to ensure adequate diversity across geo-
69% of respondents to a survey of American Psychological graphical, ethnic, gender, stage-of-career, work setting, and professional
Association (APA) members reported some professional work interest considerations.
Correspondence concerning this article should be addressed to Bob
with older adults, with only 3% devoting most of their pro- G. Knight, Ethel Percy Andrus Gerontology Center, University of South-
fessional time to older clients. The majority reported very little ern California, Los Angeles, CA 90089-0191. E-mail: bknight@usc.edu
April 2009 ● American Psychologist 205
© 2009 American Psychological Association 0003-066X/09/$12.00
Vol. 64, No. 3, 205–214 DOI: 10.1037/a0015059
Conceptual Bases of Professional
Geropsychology as a Focus of
Specialized Training
What are some of the issues that define geropsychology
as a practice area that requires specialized training?
Psychological assessment and intervention with older
adults and consultation to the care systems that serve
them require some distinctive training beyond what may
be offered in general adult clinical or counseling psy-
chology training. Four broad aspects of professional
geropsychology define the field as a distinctive practice
area.
First, professional geropsychology has roots in life
span developmental psychology, particularly development
during adulthood and old age. This tradition emphasizes
the importance of research designs that address develop-
mental change over the adult years (e.g., the sequential
designs embodied in the Seattle Longitudinal Study;
Bob G. Schaie, 2005). These designs can disentangle developmen-
Knight tal change from historical time influences that affect every-
one during the same time period as well as from differences
between successive birth cohorts that influence the ways in
such training. In this article, we report on the development
which generational groups differ (e.g., the World War II
of the Pikes Peak model for training in professional gero-
psychology. The Pikes Peak model is offered as an aspira- generation, the Boomers, Generation X). The clinical ap-
tional model for training programs and for individual plication of life span psychology emphasizes the impor-
psychologists and psychologists in training who may seek tance of understanding normal aging before attempting to
guidance in selecting programs or creating self-study pro- work with older adults with psychological disorders
grams on their own. (Knight, 2004).
The Pikes Peak model takes the position that spe- Second, professional geropsychology requires knowl-
cific training in geropsychology is not needed by all edge of and skills relevant to late-life psychopathologies,
psychologists who see older adult clients. Most practi- including those with higher prevalence in later life, espe-
tioners will see some older adults who are similar to the cially the dementias, and those with different presentations,
younger adults in their practice and will do competent etiologies, or treatment implications in older adults, includ-
work with them. As issues become more complex and ing the distinction between early- and late-life onset of
more specialized in their nature (e.g., potential presence disorders (Gatz, Kasl-Godley, & Karel, 1996; Zarit & Zarit,
of dementia, complications from comorbid medical 2007). Psychopathology shared with younger adults may
problems, assessment of decision-making capacity, nurs- present differently in later life (e.g., Alexopoulos et al.,
ing home consultation), the need for geropsychology 2002; Sheikh, 2005; Sorocco & Ferrell, 2006), and risk
competence increases. factors may differ for early- versus late-onset conditions.
The Pikes Peak competencies and related training Depression, anxiety, alcohol abuse, psychotic symptoms,
recommendations are geared toward the level of a newly and personality disorders may all have distinct features in
licensed psychologist who plans to focus on work with older adults.
older clients. Such a psychologist is likely not yet an expert A third major aspect of professional practice in gero-
but has basic competence to serve older adults and knows
psychology is the common presence of chronic medical
when expert consultation is needed. Such a geropsycholo-
conditions in older adults. This fact makes understanding
gist knows enough about the field and related competencies
to work within the limits of his or her competence. the interactions of physical and psychological symptoms of
In this article, we first provide a conceptual context for critical importance and also makes knowledge of the psy-
the delineation of a professional geropsychology training chological effects of medications for physical disorders (as
model at this time. We then describe the methods and well as psychotropic medications) essential to professional
outcomes of the Pikes Peak conference on training in practice with older adults. This tradition draws attention to
professional geropsychology. The outcomes include the the need for geropsychologists to understand the health
definition of attitude, knowledge, and skill competencies psychology of late-life medical disorders (e.g., Aldwin,
for geropsychology practice (see Appendix) and the core Park, & Spiro, 2007; Frazer, 1995; Haley, 1996) and the
features of training recommended for psychologists to de- impact of both medical and psychological conditions on
velop these competencies. functional disability in older adults.
206 April 2009 ● American Psychologist
Pikes Peak Model for
Geropsychology Training
Methodology for the Development of the
Pikes Peak Model
Three national training conferences on the preparation of
psychologists to work with older adults have been held. Older
Boulder I, which took place in Boulder, Colorado, in 1981,
focused on the knowledge base in geropsychology and began
the discussion of how this knowledge base could be taught to
new geropsychologists (Santos & VandenBos, 1982). Older
Boulder II, which met in Washington, DC, in 1992, continued
this discussion, but with a greater focus on skills training and
more attention to the various levels of clinical training
(Knight, Teri, Wohlford, & Santos, 1995). The third confer-
ence, called the Pikes Peak conference, met in Colorado
Springs, Colorado, in 2006 and focused on the development
of a model for training professional geropsychologists.
Michele J. The list of geropsychology attitude, knowledge, and
Karel skill competencies was developed through an iterative pro-
Photo by Jerilyn G. cess during the Pikes Peak conference meeting and refined
Willig
in ongoing discussions after the meeting on the conference
electronic mailing list. Conference participants met in
groups organized by competency domains and levels of
training. Because each participant was a member of each
A fourth source of specificity in work with older type of group, cross-fertilization of ideas occurred across
adults is the range of age-specific environmental contexts these thematic groups. Summaries of all groups’ decisions
in which older adult clients are embedded, including fam- were distributed each day to all participants. The meeting
ily, residential, health care, and community systems that closed with a final plenary session in which all conferees
serve older adults. Geropsychologists must have a working had the opportunity to respond to an initial draft of the
knowledge of these various systems and interface with attitude, knowledge, and skill competencies list and of key
them as appropriate. How and when to include family principles related to training programs at all levels. After
members in geropsychological care is a critical issue with the meeting, the planning committee further refined the list
ethical and clinical implications (Qualls, 2000). An exam- of competencies, and it was circulated to the attendees via
ple of a specific environmental context where psychologists electronic mailing list for feedback. The list in the Appen-
increasingly provide services is that of long-term care dix and the main recommendations of this article represent
settings, such as nursing homes and assisted living facilities the outcome of this conference process. Note that the
(e.g., Hyer & Intrieri, 2006; Lichtenberg et al., 1998; Mo- conference delegates did not produce a formal consensus
linari, 2000; Rosowsky, Casciani, & Arnold, 2008). In statement but rather a “sense of the meeting” regarding key
addition to being able to attend to the complex needs of recommendations; we, as the authors of this article, take
frail older adults in long-term care, the psychologist work- final responsibility for the geropsychology competencies
ing in the long-term care setting must be capable of training list and training recommendations presented here.
all levels of staff from nurses’ aides to administrators,
organizational consultation, and skilled work within inter- Competencies for Training in Professional
disciplinary teams. Geropsychology
This brief overview outlines key conceptual founda- The Pikes Peak model’s focus on competencies in gero-
tions of professional geropsychology and illustrates why psychology is consistent with the movement toward com-
practice in the field may require some specialized training. petency-based education, training, and credentialing within
It also illustrates important ways in which geropsychology professional psychology (Kaslow, 2004; Kaslow et al.,
as a practice area shares competencies with other practice 2004; Rodolfa et al., 2005). Thus, the Pikes Peak model
areas like neuropsychology and health psychology. To was influenced by outcomes of the 2002 Competencies
date, geropsychology (like most of child clinical psychol- Conference: Future Directions in Education and Creden-
ogy) has existed as a concentration within clinical psychol- tialing in Professional Psychology. In particular, the cube
ogy and counseling psychology. Recently, there have been model conceptual framework that considers the develop-
signs of training programs at internship and postdoctoral ment of both foundational and functional competencies
levels with strong concentrations in health psychology and across a psychologist’s training career helped to inform the
neuropsychology developing foci in professional geropsy- conference work on geropsychology competencies
chology. (Rodolfa et al., 2005).
April 2009 ● American Psychologist 207
portance for psychologists of being aware of individual
diversity in all of its manifestations, including how gender,
ethnicity, language, religion, socioeconomic status, sexual
orientation, gender identity, disability status, and urban or
rural residence interact with attitudes and beliefs about
aging. The roots of geropsychology in life span develop-
mental psychology suggested that a focus on the interac-
tions between age and cohort and other aspects of individ-
ual diversity are critical for understanding the social
context of an individual’s experiences in late life.
Knowledge. The Pikes Peak model highlights
four domains of knowledge.
1. The conceptual basis of professional geropsychol-
ogy in life span developmental psychology leads to
an emphasis on general knowledge about adult de-
velopment, aging, and the older adult population
(e.g., normal adult biological, psychological, emo-
tional, and social development).
2. The interaction of life span development with in-
creased neurological and health problems in later
Gregory A. life leads to a focus on cognitive changes, func-
Hinrichsen
tional changes, and specific presentations of psy-
chopathology in later adulthood as foundations of
clinical practice with older adults.
3. Both the normative changes with adult development
The APA Guidelines for Psychological Practice With
and aging and the distinctive features of psychopa-
Older Adults (APA, 2004) provided the substantive starting
thology in later life lead to a need for specialized
point for the Pikes Peak model. The guidelines are orga-
knowledge regarding assessment methods and in-
nized around six categories: (a) attitudes; (b) general
struments suitable for assessing older adults.
knowledge about adult development, aging, and older
4. Knowledge about developmental, cohort, contex-
adults; (c) clinical issues; (d) assessment; (e) intervention,
tual, and systemic issues, as well as of efficacy and
consultation, and other service provision; and (f) continu-
effectiveness research, must inform psychological
ing education regarding practice with older adults. The
interventions with older adults.
guidelines give practitioners working with older adults a
framework for thinking about the relevant attitudes, knowl- Skills. The first skill domain specified in the Pikes
edge, and skills but do not speak specifically to the training Peak model is called professional geropsychology func-
pathways to acquire such skills. The Pikes Peak competen- tioning, which describes the foundational competencies for
cies build on the guidelines to provide additional detail, professional geropsychology practice. According to
particularly regarding skills, framed as an outline of aspi- Rodolfa et al. (2005), foundational competencies are “the
rational goals for training. The Pikes Peak competencies building blocks of what psychologists do” (p. 350), and the
list is not intended to be a revision of the guidelines but a competencies include reflective practice–self-assessment,
tool to be used specifically to enable programs and persons scientific knowledge–methods, relationships, ethical–legal
seeking training in geropsychology to plan and evaluate a standards–policy, individual– cultural diversity, and inter-
course of training in the field. disciplinary systems. A core foundational competency of
The Pikes Peak model thus includes a summary of the the Pikes Peak model is respect for older adults and aware-
attitude, knowledge, and skill competencies needed to become ness of one’s own ageist biases. Key methods used to
a competent geropsychologist. The Pikes Peak geropsychol- combat ageist bias include acquiring an understanding of
ogy competencies (see Appendix) are intended to be aspira- normative aging and experiential learning contacts with
tional in nature and helpful for training programs and individ- older adults who are exemplars of normative and successful
ual psychologists alike. They are geared toward the aging. Other foundational geropsychology competencies
psychologist who plans to practice extensively with older include, but are not limited to, (a) understanding and ap-
adults, across a wide range of clinical needs and care settings. plying aging-specific aspects of informed consent, confi-
Attitudes. Core attitudes for geropsychology dentiality, capacity and competency, end-of-life decision
practice were specified in the APA Guidelines for Psycho- making, and elder abuse and neglect; (b) applying under-
logical Practice With Older Adults (APA, 2004). They standing of cultural and individual diversity among older
include practicing within one’s scope of competence and adults to assessment, intervention, and consultation; (c)
recognizing how one’s personal attitudes and beliefs about working with multi- and interdisciplinary teams and other
aging and older adults may affect one’s work with them. professionals; and (d) practicing appropriate documenta-
Further, the Pikes Peak model emphasizes the central im- tion and billing for geropsychological services in compli-
208 April 2009 ● American Psychologist
Other competencies for psychologists include research–
evaluation, supervision–teaching, and management–adminis-
tration (Rodolfa et al., 2005). These latter competency do-
mains, which are critical for the ongoing development and
advancement of professional geropsychology, are considered
advanced or leadership competencies for geropsychology and,
as such, are not elaborated here as fundamental competencies
for geropsychology practice.
Finally, again drawing on the recognition of the mul-
tiple specialized contexts in which older adults are served,
the Pikes Peak model recognizes that psychologists who
work with older adults should be competent to provide
services across a range of possible clinical, community, or
residential settings and be aware of special issues that arise
in providing care in varied settings. The basic recommen-
dation is that geropsychologists should be able to deliver
services in at least two (and likely more) of the following
settings: outpatient mental health services; outpatient pri-
mary care or medical settings; inpatient medical service;
inpatient psychiatric service; long-term care settings in-
Sara H.
Qualls cluding nursing homes, assisted living facilities, home care
services, and day programs; rehabilitation settings; hos-
pice; community-based programs; forensic settings; home;
and research settings.
ance with federal and state laws and regulations (e.g., These competencies represent the aspirational goals
Medicare and Medicaid). for training in professional geropsychology. We next dis-
The Pikes Peak assessment skills domain addresses cuss the ways in which these competencies can be taught to
the special issues associated with the evaluation of older persons wanting to become geropsychologists who are at
adults, who often have multiple comorbidities that chal- different levels of training.
lenge differential diagnosis, and also addresses develop-
mental and disease-related changes in functional capacities Development of Competencies Across Levels
and the multiple social contexts in which older adults can of Training
be found. Geropsychologists are able to tailor assessments Core principles and features. A core prin-
to accommodate older adults’ specific characteristics and ciple of the Pikes Peak model is a commitment both to high
contexts and use reliable and valid screening instruments to standards of competence for psychological services to older
assess and diagnose common late-life clinical problems. adults and to inclusiveness in order to build the needed
They evaluate decision-making and functional capacities geropsychology workforce. To achieve the goal of training
and risk issues, then communicate assessment results to
as many psychologists as possible to develop geropsychol-
various stakeholders with practical and clearly understand-
ogy competencies, training systems in geropsychology
able recommendations.
must be open for practitioners to enter at various points in
Geropsychology intervention competencies include
using evidence-based treatments for older adults when training and career development, including postlicensure.
available; adapting individual, group, and family interven- Given the limitations of any one training program, it is
tions to accommodate distinctive biopsychosocial function- probable that geropsychology training will involve multi-
ing of the older adult; using common late-life interventions ple programs at different levels of training (e.g., graduate,
such as those addressing life review, grieving, caregiving, internship, postdoctoral, and/or a range of postlicensure
and end-of-life care; and using interventions to enhance the training options). For example, some psychologists might
health of diverse older persons. gain initial exposure to geropsychology in graduate school
Because professional geropsychologists recognize and pursue further internship training, whereas others will
that older adults can be found in multiple specialized con- initially receive geropsychology training on internship. A
texts, consultation competencies are central to geropsy- few will seek specialized postdoctoral training. Others will
chology practice. Geropsychologists are able, for example, design independent training programs postlicensure. To some
to consult with families, other professionals, and a range of extent, developing a personal plan for geropsychology train-
agencies and care systems; to participate in interprofes- ing entails self-assessment of competencies by a trainee, with
sional geriatric care teams; to provide training to a variety input from teachers, supervisors, and consultants.
of professional and nonprofessional audiences; and to de- The following six aspects of training in professional
sign and participate in different models of aging services geropsychology are identified as key elements of a training
delivery. program for a professional geropsychologist.
April 2009 ● American Psychologist 209
Development of Competencies Within Levels
of Training
The Pikes Peak model provides recommendations for gero-
psychology training at graduate, internship, postdoctoral
fellowship, and postlicensure levels. Although the specific
goals and methods of geropsychology training differ some-
what across these developmental levels, level-specific rec-
ommendations all draw on the elements outlined above.
These recommendations will be detailed in other publica-
tions and are aimed at helping training programs that wish
to add or develop geropsychology concentrations. Al-
though excellent models for geropsychology training exist
at graduate, internship, and postdoctoral levels, postlicen-
sure training models need continued elaboration. One out-
come of the Pikes Peak conference was the establishment
of the Council of Professional Geropsychology Training
Programs, which serves as a forum for existing and new
geropsychology programs at all levels of training to share
resources, ideas, and mutual support.
Summary
Michael Duffy
In summary, the Pikes Peak model is intended to describe
the competencies that psychologists aspire to attain for
competent practice when engaging in specialized work
1. Normal aging is taught so that students have a basis with older adults. The Pikes Peak model is not intended to
for understanding abnormal aging experiences. imply that all psychologists who work with older clients
2. Bona fide professional geropsychologists using ob- need to achieve all of the geropsychology competencies,
servational methods are employed as supervisors in because many older adults will be well-served by generalist
geropsychology training programs so that students psychologists working within the scope of their practice.
can develop appropriate skills in working with The greater the presence of older adults in a psychologist’s
older adults. practice or the greater the specialized needs of specific
3. Training in geropsychology includes facilitated ex- older adults, the more relevant these specialized competen-
periences to gain self-awareness about one’s re- cies are for psychological services for older clients.
sponses to aging that vary by health status (e.g., Several themes thread throughout the model. We ex-
frail as well as healthy aging), cultural and individ- pect that the existing pattern of multiple entry points to
ual identities (e.g., wealthy or poor, rural or urban, training for specialized practice with older adults will con-
ethnic identity, gender identity, sexual orientation, tinue. Training in the professional geropsychology compe-
religious identity, disability status), and also di- tencies will involve both didactic and observed experiential
verse historical cohort experiences. education at all levels of training. The further along train-
4. Experiential professional training with older adults ees are in their careers, the greater the reliance on self-
is provided across a variety of settings. Trainees assessment and self-direction in the training process. The
need experience in diverse settings (e.g., nursing model strongly emphasizes recognizing and countering
homes, assisted living, primary care medical prac- one’s own explicit or implicit ageism. Interdisciplinary
tice, hospitals, clients’ homes). collaboration and the influence of a range of social envi-
5. Interprofessional team training is an essential part ronments on older adults are also emphasized.
of professional geropsychology training. Trainees Global population aging, the greater proportion (as com-
must learn about the knowledge base, scope of pared with earlier generations) of older adults with psycho-
practice, and distinct professional work styles of logical disorders that will likely be evident when the Baby
other disciplines. Boom generation reaches old age, and the increasing presence
6. The distinct ethical and legal issues and practice of older clients in psychologists’ practices all support the
standards that are part of practice with older adults proposition that professional geropsychology is a specialized
are included in professional geropsychology train- area of psychological practice whose time has come. The
ing programs. Examples include late-life decision- Pikes Peak training model is intended to facilitate increased
making and functional capacities, advance care growth of resources and opportunities for high-quality training
planning and surrogate decision making, commu- in geropsychology and, we hope, will inspire professional
nication with caregiving families in a manner that psychologists to expand their practices to include the under-
respects the confidentiality of the older client, and served, professionally challenging, and personally rewarding
end-of-life care. population of older persons in need of psychological services.
210 April 2009 ● American Psychologist
REFERENCES directions in education and credentialing in professional psychology.
Journal of Clinical Psychology, 60, 699 –712.
Aldwin, C. M., Park, C. L., & Spiro, A. (Eds.). (2007). Handbook of Knight, B. G. (2004). Psychotherapy with older adults (3rd ed.). Thou-
health psychology and aging. New York: Guilford Press. sand Oaks, CA: Sage.
Alexopoulos, G. S., Borson, S., Cuthbert, B. N., Devanand, D. P., Mul- Knight, B. G., Kelly, M., & Gatz, M. (1992). Psychotherapy and the older
sant, B. H., Olin, J. T., & Oslin, D. W. (2002). Assessment of late life adult. In D. K. Freedheim (Ed.), The history of psychotherapy: A
depression. Society of Biological Psychiatry, 52, 164 –174. century of change (pp. 528 –551). Washington, DC: American Psycho-
American Psychological Association. (2004). Guidelines for psychologi- logical Association.
cal practice with older adults. American Psychologist, 59, 236 –260. Knight, B. G., Teri, L., Wohlford, P., & Santos, J. (Eds.). (1995). Mental
Center for Health Workforce Studies. (2005). The impact of the aging health services for older adults: Implications for training and practice
population on the health workforce in the United States. Rensselaer, in geropsychology. Washington, DC: American Psychological Associ-
NY: University at Albany, School of Public Health. ation.
Frazer, D. (1995). The medical issues in geropsychology training and Koenig, H. G., George, L. K., & Schneider, R. (1994). Mental health care
practice. In B. G. Knight, L. Teri, P. Wohlford, & J. Santos (Eds.), for older adults in the year 2020: A dangerous and avoided topic. The
Mental health services for older adults: Implications for training and Gerontologist, 34, 674 – 679.
practice in geropsychology (pp. 63–72). Washington, DC: American Lichtenberg, P. A., Smith, M., Frazer, D., Molinari, V., Rosowsky, E.,
Psychological Association. Crose, R., et al. (1998). Standards for psychological services in long-
Gatz, M., Kasl-Godley, J. E., & Karel, M. J. (1996). Aging and mental term care facilities. The Gerontologist, 38, 122–127.
disorders. In J. E. Birren & K. W. Schaie (Eds.), Handbook of the Molinari, V. (Ed.). (2000). Professional psychology in long term care.
psychology of aging (4th ed., pp. 365–382). San Diego, CA: Academic New York: Hatherleigh Press.
Press.
Qualls, S. H. (2000). Therapy with aging families: Rationale, opportuni-
Gatz, M., & Smyer, M. A. (2001). Mental health and aging at the outset
ties, and challenges. Aging and Mental Health, 4, 191–199.
of the twenty-first century. In J. E. Birren & K. W. Schaie (Eds.),
Qualls, S. H., Segal, D. L., Norman, S., Niederehe, G., & Gallagher-
Handbook of the psychology of aging (5th ed., pp. 523–544). San
Thompson, D. (2002). Psychologists in practice with older adults:
Diego, CA: Academic Press.
Current patterns, sources of training, and need for continuing education.
Haley, W. E. (1996). The medical context of psychotherapy with the
Professional Psychology: Research and Practice, 33, 435– 442.
elderly. In S. H. Zarit & B. G. Knight (Eds.), A guide to psychotherapy
and aging: Effective clinical interventions in a life-stage context (pp. Rodolfa, E., Bent, R., Eisman, E., Nelson, P., Rehm, L., & Ritchie, P.
221–240). Washington, DC: American Psychological Association. (2005). A cube model for competency development: Implications for
Halpain, M. C., Harris, M. J., McClure, F. S., & Jeste, D. V. (1999). psychology educators and regulators. Professional Psychology: Re-
Training in geriatric mental health: Needs and strategies. Psychiatric search and Practice, 36, 347–354.
Services, 50, 1205–1208. Rosowsky, E., Casciani, J. M., & Arnold, M. (2008). Geropsychology and
He, W., Sengupta, M., Velkoff, V. A., & DeBarros, K. A. (2005, Decem- long term care: A practitioner’s guide. New York: Springer.
ber). 65⫹ in the United States (U.S. Census Bureau Current Population Santos, J. F., & VandenBos, G. R. (Eds.). (1982). Psychology and the
Report, Special Study P23–209). Washington, DC: U.S. Government older adult: Challenges for training in the 1980s. Washington, DC:
Printing Office. American Psychological Association.
Hyer, L., & Intrieri, R. C. (2006). Geropsychological interventions in Schaie, K. W. (2005). Developmental influences on adult intelligence: The
long-term care. New York: Springer. Seattle Longitudinal Study. New York: Oxford University Press.
Jeste, D. V., Alexopoulos, G. S., Bartels, S. J., Cummings, J. L., Gallo, Sheikh, J. I. (2005). Investigations of anxiety in older adults: Recent
J. J., Gottlieb, G. L., et al. (1999). Consensus statement on the upcom- advances and future directions. Journal of Geriatric Psychiatry and
ing crisis in geriatric mental health: Research agenda for the next 2 Neurology, 18, 59 – 60.
decades. Archives of General Psychiatry, 56, 848 – 853. Sorocco, K. H., & Ferrell, S. W. (2006). Alcohol use among older adults.
Kaslow, N. J. (2004). Competencies in professional psychology. Ameri- The Journal of General Psychology, 133, 453– 467.
can Psychologist, 59, 774 –781. Zarit, S. H., & Zarit, J. M. (2007). Mental disorders in older adults:
Kaslow, N. J., Borden, K. A., Collins, F. L., Jr., Forrest, L., Illfelder-Kay, Fundamentals of assessment and treatment (2nd ed.). New York:
J., Nelson, P. D., et al. (2004). Competencies conference: Future Guilford Press.
(Appendix follows)
April 2009 ● American Psychologist 211
Appendix
The Pikes Peak Model Competencies: Attitude, Knowledge, and Skill
Competencies for Practice in Professional Geropsychology
I. Attitudes B. Knowledge: Foundations of Clinical Practice With
Older Adults
1. Psychologists are encouraged to work with older
adults within their scope of competence and to seek con- 1. The neuroscience of aging, its applications to
sultation or make appropriate referrals when indicated. changes in cognition, and its implications for clinical in-
2. Psychologists are encouraged to recognize how their terventions with older adults
attitudes and beliefs about aging and about older individuals 2. Knowledge of the salience of functional changes in
may be relevant to their assessment and treatment of older later adulthood, including resulting problems in daily living
adults and to seek consultation or further education about 3. Awareness of the concept of person– environment
these issues when indicated. interaction and the implications of this concept for adapta-
3. Psychologists are encouraged to expand their tion in late life
awareness of how individual diversity in all of its manifes- 4. Psychopathology in middle and later adulthood,
tations (including gender, age, cohort, ethnicity, language, including differences in the prevalence, etiology, presenta-
religion, socioeconomic status, sexual orientation, gender tion, associated features, comorbidity, and course of mental
identity, disability status, and urban or rural residence) disorders in older adults, as well as the health-related
interacts with attitudes and beliefs about aging, to use this consequences of treated and untreated psychological dis-
awareness to inform their assessment and treatment of
orders in late life
older adults, and to seek consultation or further education
5. Knowledge of common acute, chronic, and terminal
when indicated.
medical illnesses in late life
4. Psychologists are encouraged to increase their
knowledge, understanding, and skills with respect to work-
ing with older adults through continuing education, train- C. Knowledge: Foundations of Assessment of Older
ing, supervision, and consultation. Adults
1. Theory and research informing psychological as-
II. Knowledge Base sessment of older adults, including the broad array of
A. Knowledge: General Knowledge About Adult Develop- assessment domains, methods, and instruments that are
ment, Aging, and the Older Adult Population psychometrically suitable for assessing older adults
2. Issues in the limits of using assessment instruments
1. Theoretical models and research methodologies for created for younger persons with older adults without ad-
understanding the processes of aging, including the life- equate standardization
span developmental perspective, conceptions of positive or 3. Knowledge of contextual issues in the assessment
successful aging, and methodological issues in conducting of older adults, including the system or environment in
or evaluating research on aging
which the elder functions, and the impact on assessment
2. Demographics of aging, including where to obtain
process and outcomes
current knowledge on changes in population dynamics
3. Normal or “usual” aging, including the following:
D. Knowledge: Foundations of Intervention, Consulta-
● Biological and health-related aspects of aging and tion, and Other Service Provision
mind– body interactions 1. Theory, research, and practice of various methods
● Psychology of aging, including normative continu- of intervention with older adults, including current research
ity and change in the domains of sensory processes, evidence about their efficacy and effectiveness as applied
cognition, personality, and emotions to diverse groups within the older adult population
● Social dynamics of the aging process including is- 2. Health, illness, and pharmacology as related to
sues such as work and retirement, friendships, roles,
assessment and treatment of late-life mental health prob-
and family relationships
lems, including awareness of medical or medication factors
4. Awareness of diversity in the aging process, par- that may affect treatment outcomes (e.g., illness, medica-
ticularly how sociocultural factors such as gender, age, tion side effects, polypharmacy)
cohort, ethnicity, language, religion, socioeconomic status, 3. Issues pertaining to the provision of services in the
sexual orientation, gender identity, disability status, and specific settings in which older adults typically live or seek
urban–rural residence may influence the experience and treatment
expression of health and of psychological problems in later 4. Knowledge of aging services in the local commu-
life and how this knowledge may inform the assessment nity (e.g., day care, transportation, residential) and how to
and treatment of older adults refer clients to these services
212 April 2009 ● American Psychologist
5. Prevention and health promotion services and their other clinically relevant problems, formulation of treatment
relevance for middle-aged and older adults at risk for plans, and, specifically, differential diagnosis (common
mental disorders problems and issues include but are not limited to depres-
6. Awareness of the broad array of potential clients sion, anxiety, grief, delirium, dementia, medication effects,
(e.g., family members, other caregivers, health care profes- and physical disorders and their effects on functioning)
sionals, and organizations) for psychological consultation 2. Use psychometrically sound screening instruments
and intervention and appropriate intervention strategies in for cognition, psychopathology, and personality to inform
these contexts treatment planning
7. Models and methods of interdisciplinary collabora- 3. Refer for neuropsychological, neurological, psychi-
tion, including an understanding of the varied components, atric, medical, or other evaluations as indicated
roles, and contexts of interdisciplinary treatment of late-life 4. Use cognitive assessments and/or neuropsycholog-
mental disorders ical reports to clarify clinical issues and inform treatment
8. Knowledge of ethical and legal standards related to planningA2
psychological intervention with older adults and care sys- 5. Evaluate decision-making and functional capacities
tems, with particular attention to aging-specific issues of (e.g., for managing finances, independent living, driving,
informed consent, confidentiality, substitute or end-of-life making health care decisions)
decision making and potential conflicts of interest, capacity 6. Assess risk (e.g., suicidality, self-neglect, elder
and competency, and elder abuse and neglect abuse)
7. Adapt instruments and tailor assessments to accom-
III. Skill CompetenciesA1 modate older adults’ specific characteristics and contexts
A. Skills: Professional Geropsychology Functioning 8. Communicate assessment results to various stake-
(Foundational Competencies) holders with relevant, practical, and clearly understandable
recommendations, with appropriate consideration for con-
1. Understand and apply ethical and legal standards, fidentiality issues
with particular attention to aging-specific issues, such as
informed consent, confidentiality, capacity and compe- C. Skills: Intervention
tency, end-of-life decision making, and elder abuse and
neglect 1. Apply individual, group, and family interventions
2. Understand cultural and individual diversity as rel- to older adults using appropriate modifications to accom-
evant to assessment, intervention, and consultation and modate distinctive biopsychosocial functioning of older
apply to practice with diverse older adults adults and distinct therapeutic relationship characteristics
3. Address complex biopsychosocial issues among 2. Use available evidence-based treatments for older
many older adults by collaborating with other disciplines in adults
multi- and interdisciplinary teams 3. Develop psychotherapeutic interventions based on
4. Practice self-reflection, self-assessment (e.g., self- empirical literature, theory, and clinical judgment when
awareness of ageist assumptions and biases, recognition of insufficient efficacy research is available on older adults
boundaries of competence and when and how to refer 4. Be proficient in using commonly applied late-life
elsewhere) interventions such as those focusing on life review, grief,
5. Relate effectively and empathically with older adult end-of-life care, and caregiving
clients, families, and other stakeholders in a range of pro- 5. Use interventions to enhance the health of diverse
fessional roles and settings (e.g., senior center, hospital, older persons (e.g., chronic health problems, healthy aging,
long-term care) cognitive fitness)
6. Apply scientific knowledge to geropsychology 6. Demonstrate ability to intervene in settings where
practice and policy advocacy older adults and their family members are often seen (e.g.,
7. Practice appropriate documentation, billing, and
reimbursement procedures for geropsychological services
A1
in compliance with state and federal laws and regulations In preparing this document, the conference delegates acknowl-
edged that skills in supervision–teaching, research– evaluation, and manage-
(especially regarding Medicare and Medicaid services), ment–administration are also critical for geropsychology practice in many
including assessment and documentation of medical neces- settings, as well as for the further development of professional geropsy-
sity chology as a field. Although many geropsychologists will also have
8. Advocate for clients’ needs and provide case man- competencies in those skill domains, they are not considered to be core
competencies for geropsychology practice. Rather, skills in supervision–
agement for needed services teaching, research– evaluation, and management–administration are
viewed as leadership skills to be encouraged through training, mentoring,
B. Skills: Assessment and career development.
A2
Some geropsychologists have also been trained as neuropsycholo-
1. Conduct clinical assessment leading to Diagnostic gists and would thus be able to conduct neuropsychological evaluations
and Statistical Manual of Mental Disorders diagnoses and within their scope of competence.
(Appendix continues)
April 2009 ● American Psychologist 213
health services, housing, community programs) with a 7. Collaborate and coordinate with other agencies and
range of strategies including those targeted at the individ- professionals that serve older adults
ual, family, environment, and system 8. Recognize and negotiate multiple roles in older
adult consultation settings
D. Skills: Consultation–Training
E. Skills: Delivery of Services in Different Settings
1. Consult to families, professionals, programs, health
care facilities, legal systems, and other agencies and orga- Delivery of services in two or more different settings,
nizations that serve older adults including the following:
2. Provide training on geropsychological issues (e.g., 1. Outpatient mental health services
in-services, workshops, community education) to different 2. Outpatient primary care or medical settings
disciplines 3. Inpatient medical service
3. Participate in interprofessional teams that serve 4. Inpatient psychiatric service
older adults 5. Long-term care settings including nursing homes,
4. Communicate psychological conceptualizations to assisted living facilities, home care, day programs
medical and other professionals in a concise and useful 6. Rehabilitation settings
manner 7. Hospice
5. Implement strategies for systems analysis and 8. Community-based programs
change in organizations and facilities that serve older adults 9. Forensic settings
6. Design and participate in different models of aging 10. Home-delivered psychological services
services delivery (e.g., integrated care) 11. Research settings
214 April 2009 ● American Psychologist
You might also like
- 2018 Geriatric Psychiatry PDFDocument738 pages2018 Geriatric Psychiatry PDFNungki100% (10)
- Home For The Elderly CitizensDocument4 pagesHome For The Elderly CitizensJaymar PadolinaNo ratings yet
- Ambulating ClientDocument4 pagesAmbulating ClientRegineCuasSulibNo ratings yet
- Guidelines APA PDFDocument25 pagesGuidelines APA PDFPau NndNo ratings yet
- Older AdultsDocument63 pagesOlder AdultsLuis RamosNo ratings yet
- Cognitive-Behavioral Interventions With Older AdulDocument38 pagesCognitive-Behavioral Interventions With Older AdulMARIELA LIZETH VALENTE CORTEZNo ratings yet
- Military Culture Strometal Et. Al. 2012Document10 pagesMilitary Culture Strometal Et. Al. 2012Lauren RyanNo ratings yet
- A 0029328Document12 pagesA 0029328Cristina MPNo ratings yet
- Ethical-Practice-in-Geropsychology-Intro-SampleDocument8 pagesEthical-Practice-in-Geropsychology-Intro-SampleYago CarvalhoNo ratings yet
- RecommendedDocument9 pagesRecommendedMaya Putri Haryanti100% (1)
- 9p - Intellectual Disability and Mental Health - Is Psychology PreparedDocument9 pages9p - Intellectual Disability and Mental Health - Is Psychology Preparedtiagompeixoto.psiNo ratings yet
- 2014 - APA Guidelines Older AdultsDocument32 pages2014 - APA Guidelines Older AdultsQueralt BNo ratings yet
- Art. Psicología Infantil Clínica - Una Especialidad para Niños, Adolescentes y Sus Familias 1Document8 pagesArt. Psicología Infantil Clínica - Una Especialidad para Niños, Adolescentes y Sus Familias 1Henry RiveraNo ratings yet
- Child and Adolescent Psychological Assessment CurrDocument9 pagesChild and Adolescent Psychological Assessment CurrArif Erdem KöroğluNo ratings yet
- Guidelines Assessment Intervention DisabilitiesDocument61 pagesGuidelines Assessment Intervention DisabilitiesBladimir Iles ChavesNo ratings yet
- A Model For Home-Based Psychology From The Veterans Health AdministrationDocument7 pagesA Model For Home-Based Psychology From The Veterans Health AdministrationStephanie SouzaNo ratings yet
- Assessment and Treatment of Gender Dysphoria and Gender Variant Patients: A Primer For PsychiatristsDocument1 pageAssessment and Treatment of Gender Dysphoria and Gender Variant Patients: A Primer For Psychiatristssergi pascualNo ratings yet
- Test Bank For Introduction To Clinical Psychology 8 e 8th Edition Geoffrey P Kramer Douglas A Bernstein Vicky PharesDocument11 pagesTest Bank For Introduction To Clinical Psychology 8 e 8th Edition Geoffrey P Kramer Douglas A Bernstein Vicky PharesMarlyn Islam100% (40)
- Park KubzanskyDocument11 pagesPark KubzanskyJONNABEL ROQUEZNo ratings yet
- (11 V) From The Laboratory To The Therapy RoomDocument16 pages(11 V) From The Laboratory To The Therapy RoomricardorickiNo ratings yet
- Only Human: Mental Health Difficulties Among Clinical, Counseling, and School Psychology Faculty and TraineesDocument49 pagesOnly Human: Mental Health Difficulties Among Clinical, Counseling, and School Psychology Faculty and TraineescrisolarisNo ratings yet
- Geropsychology Content in Clinical TrainDocument10 pagesGeropsychology Content in Clinical TrainTheo Buana ParandaNo ratings yet
- UC San Diego Previously Published WorksDocument12 pagesUC San Diego Previously Published WorkszahoNo ratings yet
- Behaviour Research and Therapy: Alan E. KazdinDocument12 pagesBehaviour Research and Therapy: Alan E. KazdinDroguNo ratings yet
- The Abstracts of The 36th Annual Conference of The Australian Psychological SocietyDocument50 pagesThe Abstracts of The 36th Annual Conference of The Australian Psychological Societymoch.al.irsyad19No ratings yet
- Content ServerDocument9 pagesContent ServerNariman Abed Alganey AkariNo ratings yet
- Guidelines Dementia Age Related Cognitive ChangeDocument32 pagesGuidelines Dementia Age Related Cognitive ChangeFernanda Keren de PaulaNo ratings yet
- Feeny 2006 CBT For Bipolar Pilot 19719Document8 pagesFeeny 2006 CBT For Bipolar Pilot 19719shobaNo ratings yet
- Measures of Psychological Stress and Physical Health in Family Caregivers of Stroke Survivors A Literature ReviewDocument11 pagesMeasures of Psychological Stress and Physical Health in Family Caregivers of Stroke Survivors A Literature ReviewaNo ratings yet
- IndianJPsychiatry60524-4490945 122829Document25 pagesIndianJPsychiatry60524-4490945 122829EnaraNo ratings yet
- 2012 Positive Psy OverviewDocument17 pages2012 Positive Psy OverviewDivia RainaNo ratings yet
- Pottik 2007Document8 pagesPottik 2007Stijn VanheuleNo ratings yet
- CD QuestDocument20 pagesCD QuestDindini FanaiNo ratings yet
- Texto Sobre Foco No Terapeuta (4980)Document17 pagesTexto Sobre Foco No Terapeuta (4980)Fabiana H. ShimabukuroNo ratings yet
- Horan 2001Document49 pagesHoran 2001moch.al.irsyad19No ratings yet
- Bringing Psychotherapy To Primary Care: Innovations and ChallengesDocument24 pagesBringing Psychotherapy To Primary Care: Innovations and ChallengespqpnbnrmNo ratings yet
- Health Promotion With Older Adults Experiencing Mental Health Challenges: A Literature Review of Strength-Based ApproachesDocument28 pagesHealth Promotion With Older Adults Experiencing Mental Health Challenges: A Literature Review of Strength-Based ApproachesDewi AgustianiNo ratings yet
- Artigo SM 3Document10 pagesArtigo SM 3selfemanNo ratings yet
- Mental Health Diagnostic Considerations in Racial Ethnic Minority YouthDocument15 pagesMental Health Diagnostic Considerations in Racial Ethnic Minority YouthJohn BitsasNo ratings yet
- Mental Health and Palliative Care Literature ReviewDocument4 pagesMental Health and Palliative Care Literature ReviewafdtbwkhbNo ratings yet
- Hirvikoski, Et Al.j. (2015) - Cognitive Behavior Therapy-Based Psychoeducational Groups For Adults With ADHD and Their Significant OthersDocument11 pagesHirvikoski, Et Al.j. (2015) - Cognitive Behavior Therapy-Based Psychoeducational Groups For Adults With ADHD and Their Significant OthersjuanNo ratings yet
- Inpatient Geriatric Psychiatry: Optimum Care, Emerging Limitations, and Realistic GoalsFrom EverandInpatient Geriatric Psychiatry: Optimum Care, Emerging Limitations, and Realistic GoalsHoward H. FennNo ratings yet
- 2011 Adhd Npsy-AssessmentDocument15 pages2011 Adhd Npsy-AssessmentRoberta Finamore de AraujoNo ratings yet
- Hardaker Halcomb GriffithsBolzan Arblaster 2007Document11 pagesHardaker Halcomb GriffithsBolzan Arblaster 2007AdriánNo ratings yet
- Cashel, M.L. (2002) - Child and Adolescent Psychological Assessment. Current Clinical Practices and The Impact of Managed CareDocument8 pagesCashel, M.L. (2002) - Child and Adolescent Psychological Assessment. Current Clinical Practices and The Impact of Managed CareRicardo NarváezNo ratings yet
- Harker Washington 0250E 19146Document109 pagesHarker Washington 0250E 19146CHEE KOK SENGNo ratings yet
- JamaDocument11 pagesJamaDipin MutrejaNo ratings yet
- HHS Public Access: Mental Health Diagnostic Considerations in Racial/Ethnic Minority YouthDocument25 pagesHHS Public Access: Mental Health Diagnostic Considerations in Racial/Ethnic Minority YouthTry Wahyudi Jeremi LoLyNo ratings yet
- E144 Vol. 52 No. 6 December 2016 Selected AbstractsDocument2 pagesE144 Vol. 52 No. 6 December 2016 Selected AbstractsJos CanalesNo ratings yet
- Benefits of An Experimental Program of Equestrian Therapy For Children With ADHD PDFDocument10 pagesBenefits of An Experimental Program of Equestrian Therapy For Children With ADHD PDFJuli DeviaNo ratings yet
- 01 Taylor-Rodgers Evaluation of An Online 2014Document7 pages01 Taylor-Rodgers Evaluation of An Online 2014sushmita bhartiaNo ratings yet
- A2 Uedp2 223Document6 pagesA2 Uedp2 223arundhatisah01No ratings yet
- Intellectual DevelopmentalDocument29 pagesIntellectual DevelopmentalAnne de AndradeNo ratings yet
- Fields of PsychologyDocument14 pagesFields of Psychologyhumna naeemNo ratings yet
- Pauta Discapacidad N&ADocument29 pagesPauta Discapacidad N&APedro Y. LuyoNo ratings yet
- Chapter 4Document44 pagesChapter 4AnonimoNo ratings yet
- Prevalence and Correlates of DepressionDocument9 pagesPrevalence and Correlates of Depressioncristel.talladaNo ratings yet
- Pacha Nager o Psych Training 2010Document11 pagesPacha Nager o Psych Training 2010Theo Buana ParandaNo ratings yet
- Aging, Mental Health and Demographic Challenges For PsychotherapistsDocument8 pagesAging, Mental Health and Demographic Challenges For PsychotherapistsChristian RiveraNo ratings yet
- Videoconferencing Psychotherapy: A Systematic Review: Psychological Services May 2012Document22 pagesVideoconferencing Psychotherapy: A Systematic Review: Psychological Services May 2012juan acuñaNo ratings yet
- Sareeceguerrero-324-Litreviewfinal-Bosa 1Document7 pagesSareeceguerrero-324-Litreviewfinal-Bosa 1api-520930030No ratings yet
- Statistical Bulletin: Health Expectancies at Birth and at Age 65 in The United Kingdom, 2007-2009Document17 pagesStatistical Bulletin: Health Expectancies at Birth and at Age 65 in The United Kingdom, 2007-2009Papato KongNo ratings yet
- p95 09 1 PDFDocument196 pagesp95 09 1 PDFPapato KongNo ratings yet
- Measuring National Well-Being at What Age Is Personal Well-Being The HighestDocument6 pagesMeasuring National Well-Being at What Age Is Personal Well-Being The HighestPapato KongNo ratings yet
- M01 S09 Gender Stereotypes PDFDocument9 pagesM01 S09 Gender Stereotypes PDFPapato KongNo ratings yet
- Social Communication Assessment After Traumatic Brain Injury A Narrative Review of Innovations in Pragmatic and Discourse Assessment MethodsDocument15 pagesSocial Communication Assessment After Traumatic Brain Injury A Narrative Review of Innovations in Pragmatic and Discourse Assessment MethodsPapato KongNo ratings yet
- T ADLQMunoz NeiraSlachevskyetal2012 - PDFDocument12 pagesT ADLQMunoz NeiraSlachevskyetal2012 - PDFPapato KongNo ratings yet
- Computational Neuroscience: Rajesh P. N. Rao Adrienne Fairhall University of Washington, Seattle, USADocument7 pagesComputational Neuroscience: Rajesh P. N. Rao Adrienne Fairhall University of Washington, Seattle, USAPapato KongNo ratings yet
- House Democratic Caucus Task Force On Aging and Families LTR To Biden Harris Transition - Geriatrician To COVID Advisory BoardDocument2 pagesHouse Democratic Caucus Task Force On Aging and Families LTR To Biden Harris Transition - Geriatrician To COVID Advisory BoardPeter SullivanNo ratings yet
- Late Life and Neurocognitive DisordersDocument24 pagesLate Life and Neurocognitive DisordersJonnaNo ratings yet
- Health Sciences 2711B 2011 - Health Issues in AgingDocument8 pagesHealth Sciences 2711B 2011 - Health Issues in AgingJillKellyNo ratings yet
- Posterior Cortical AtrophyDocument9 pagesPosterior Cortical AtrophyAnonymous zxTFUoqzklNo ratings yet
- Ebp PresentationDocument12 pagesEbp Presentationapi-267985804No ratings yet
- Drug Study HaldolDocument2 pagesDrug Study HaldolGracia EvangelistaNo ratings yet
- UTI Treatment Guidelines PDFDocument5 pagesUTI Treatment Guidelines PDFMuhammad IhsanuddinNo ratings yet
- TMH ResumeDocument2 pagesTMH Resumeapi-257873078No ratings yet
- Nursing InterventionsDocument1 pageNursing InterventionsTancred UyNo ratings yet
- RLE NCMB 314-M2-CU 9 Respiratory ChangesDocument6 pagesRLE NCMB 314-M2-CU 9 Respiratory ChangesJordz PlaciNo ratings yet
- Biomechanics and Clinical Implications of Complete Edentulous StateDocument4 pagesBiomechanics and Clinical Implications of Complete Edentulous StateDorobantuMihaiGabiNo ratings yet
- Assessment Constipation PDFDocument6 pagesAssessment Constipation PDFDennis CobbNo ratings yet
- Mood Affect....Document3 pagesMood Affect....Michael ReidNo ratings yet
- NFDN 2003Document2 pagesNFDN 2003api-319220519No ratings yet
- Tpo Ward BMDocument3 pagesTpo Ward BMAhl A PurujiNo ratings yet
- Daftar Pustaka 13 Permasalahan Terkait Obat Antihipertensi Pada Pasien Usia Lanjut Di Poli Geriatri RSUD DR - Soetomo PDFDocument6 pagesDaftar Pustaka 13 Permasalahan Terkait Obat Antihipertensi Pada Pasien Usia Lanjut Di Poli Geriatri RSUD DR - Soetomo PDFDave AbrahamNo ratings yet
- What Is CaregivingDocument3 pagesWhat Is CaregivingjasmineNo ratings yet
- PermethrinDocument3 pagesPermethrinaficoNo ratings yet
- Escala Internacional de Demencia HIVDocument8 pagesEscala Internacional de Demencia HIVctobonaNo ratings yet
- Assessment of Older People 2: Assessing The Physical DomainDocument5 pagesAssessment of Older People 2: Assessing The Physical DomainJastine SabornidoNo ratings yet
- Vascular Dementia, With Lacunar StrokeDocument28 pagesVascular Dementia, With Lacunar StrokeTimotius Wira YudhaNo ratings yet
- NeuropsychiatricDocument18 pagesNeuropsychiatricSamuel JohnsonNo ratings yet
- J Neurol Neurosurg Psychiatry 1998 Royall 588 94Document8 pagesJ Neurol Neurosurg Psychiatry 1998 Royall 588 9454321000No ratings yet
- Gastritis Erosif PatofisiologiDocument3 pagesGastritis Erosif PatofisiologiLargactil CpzNo ratings yet
- Nursing Manangment of Older PersonDocument5 pagesNursing Manangment of Older PersonRaiden VizcondeNo ratings yet
- Save The Date: 94th Anniversary DinnerDocument4 pagesSave The Date: 94th Anniversary DinnerthehebrewhomeNo ratings yet
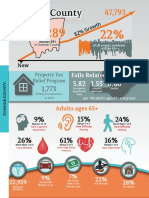
- Sumner County Senior StatisticsDocument1 pageSumner County Senior StatisticsJen ToddNo ratings yet
- VirtualSx Event (Invite-Only)Document2 pagesVirtualSx Event (Invite-Only)SexRecoveryNo ratings yet