Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
71 viewsUrinary Track Infection Pathopysiology 1
Urinary Track Infection Pathopysiology 1
Uploaded by
rraven16The urinary tract is normally sterile but can become infected by bacteria ascending from the urethra or hematogenously. E. coli causes over 75% of community-acquired urinary tract infections (UTIs), while other gram-negative bacteria like Klebsiella, Proteus, and Pseudomonas and gram-positive bacteria like Enterococcus and Staphylococcus account for the remainder. UTIs can infect the bladder (cystitis), urethra, ureters, or kidneys and cause symptoms like burning during urination and abdominal pain. People more susceptible to UTIs include women, diabetics, infants, and those with anatomical abnormalities or lowered immunity.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You might also like
- PharmacologyDocument33 pagesPharmacologyFreeNursingNotes90% (68)
- Medical Microbiology and Immunology Flash Cards - Sample ChapterDocument250 pagesMedical Microbiology and Immunology Flash Cards - Sample Chapterleh.mo931580% (5)
- Types of Urinary Tract InfectionDocument4 pagesTypes of Urinary Tract InfectionGencris Medrano Giray RNNo ratings yet
- Infections of The Urinary TractDocument47 pagesInfections of The Urinary Tractsandrarosok88No ratings yet
- Infeksi Saluran KemihDocument65 pagesInfeksi Saluran KemihHaziq AnuarNo ratings yet
- Urinary Tract InfectionsDocument17 pagesUrinary Tract Infectionss.khan9211rediffmail.comNo ratings yet
- Urinary Tract InfectionsDocument71 pagesUrinary Tract Infectionsdayibon499No ratings yet
- Urinary Tract InfectionDocument5 pagesUrinary Tract InfectionDRANo ratings yet
- Cases of Group 3 LC 1Document13 pagesCases of Group 3 LC 1abdul basithNo ratings yet
- Infection Urinary Tract Urine Bladder KidneyDocument18 pagesInfection Urinary Tract Urine Bladder KidneygdquijanoNo ratings yet
- UTIDocument6 pagesUTIAyessa Marie BarbosaNo ratings yet
- Tai Lieu Tieng Anh Cho Sinh Vien Bai Nhiem Khuan Duong Tiet NieuDocument3 pagesTai Lieu Tieng Anh Cho Sinh Vien Bai Nhiem Khuan Duong Tiet NieuLê Mỹ Khánh LyNo ratings yet
- UTI (Urinary Tract Infection)Document9 pagesUTI (Urinary Tract Infection)Carson BirthNo ratings yet
- Urinary Tract Infection - Kuliah Mahasiswa - Ferbruari 2017 - EDITDocument52 pagesUrinary Tract Infection - Kuliah Mahasiswa - Ferbruari 2017 - EDITRahmawati HamudiNo ratings yet
- The Urinary System. The Urinary System Helps Maintain Proper Water and Salt Balance ThroughoutDocument4 pagesThe Urinary System. The Urinary System Helps Maintain Proper Water and Salt Balance ThroughoutArjay EspañolNo ratings yet
- Urinary Tract Infection (UTI)Document9 pagesUrinary Tract Infection (UTI)ogwal andrewictynetNo ratings yet
- Uti Case StudyDocument7 pagesUti Case StudyStephNo ratings yet
- Urinary Tract InfectionDocument6 pagesUrinary Tract InfectionYalc LapidNo ratings yet
- Urinary Tract InfectionDocument7 pagesUrinary Tract InfectionNader Smadi100% (7)
- CASE STUDY #3 Urinary System (Urninary Tract Infection or UTI)Document5 pagesCASE STUDY #3 Urinary System (Urninary Tract Infection or UTI)Lerma PagcaliwanganNo ratings yet
- RLE Urinary Tract InfectionDocument13 pagesRLE Urinary Tract InfectionAliza AlyyNo ratings yet
- Renal DisDocument166 pagesRenal DisCharles MutaiNo ratings yet
- Urinarytract InfectionDocument61 pagesUrinarytract InfectionsanjivdasNo ratings yet
- Urogenital InfectionsDocument24 pagesUrogenital InfectionsGaurav100% (1)
- Urinary Tract Infection: CC Ricky G. JalecoDocument56 pagesUrinary Tract Infection: CC Ricky G. JalecoRicky JalecoNo ratings yet
- An Individual Case Study ON Urinary Tract Infection (UTI) : Southern Isabela General HospitalDocument20 pagesAn Individual Case Study ON Urinary Tract Infection (UTI) : Southern Isabela General HospitalhanapotakoNo ratings yet
- Urinary Tract InfectionDocument10 pagesUrinary Tract Infectionjaah diazNo ratings yet
- UTI Pediatric NotesDocument2 pagesUTI Pediatric NotesSanya BNo ratings yet
- Microbial Diseases of The Urinary System: Yemane Weldu (MSC., Assistant Professor)Document65 pagesMicrobial Diseases of The Urinary System: Yemane Weldu (MSC., Assistant Professor)Lidiya TeshomeNo ratings yet
- Urinary Tract InfectionsDocument39 pagesUrinary Tract InfectionsYordanos GetnetNo ratings yet
- Symptoms: For Bladder InfectionsDocument5 pagesSymptoms: For Bladder InfectionsGene Ryuzaki SeseNo ratings yet
- Urinary Tract InfectionDocument30 pagesUrinary Tract InfectionLeo Mar MakilanNo ratings yet
- ####Bahan Kuliah ISK Blok 23 (Nov 2015)Document32 pages####Bahan Kuliah ISK Blok 23 (Nov 2015)ajengdmrNo ratings yet
- Prevalence of Uti in Benin PDFDocument54 pagesPrevalence of Uti in Benin PDFcamiladovalle95No ratings yet
- Urinary Tract Infection (Maramag Eunice Laman Jenny Pearl)Document16 pagesUrinary Tract Infection (Maramag Eunice Laman Jenny Pearl)Carlojay IniegoNo ratings yet
- Infections of The Urinary Genirouty TractDocument4 pagesInfections of The Urinary Genirouty Tractfifa nasrul ummahNo ratings yet
- Uti ReadingsDocument6 pagesUti ReadingskarenbelnasNo ratings yet
- DR Lana Sundac - LGRS Urinary Tract InfectionsDocument4 pagesDR Lana Sundac - LGRS Urinary Tract Infectionsoxford_commaNo ratings yet
- Renal Notes Step 2ckDocument34 pagesRenal Notes Step 2cksamreen100% (1)
- Handout 2Document1 pageHandout 2api-320812761No ratings yet
- Background: Urinary Tract InfectionDocument9 pagesBackground: Urinary Tract InfectionOnieBoy CurayagNo ratings yet
- Urinary Tract InfectionDocument24 pagesUrinary Tract InfectionraddagNo ratings yet
- Theoretical Background Urinary Tract InfectionDocument7 pagesTheoretical Background Urinary Tract Infectiondenebrench23No ratings yet
- Urinary Tract Infection (Uti) Definition:: TypesDocument2 pagesUrinary Tract Infection (Uti) Definition:: TypesAneela ManzoorNo ratings yet
- Urinary Tract InfectionDocument3 pagesUrinary Tract InfectionHo Yong WaiNo ratings yet
- Urinary Tract Infection (UTI)Document39 pagesUrinary Tract Infection (UTI)Sabita TripathiNo ratings yet
- IskDocument35 pagesIskfadliNo ratings yet
- Urinary Tract InfectionDocument50 pagesUrinary Tract Infectionpokhara gharipatan100% (1)
- What Is A Urinary Tract InfectionDocument2 pagesWhat Is A Urinary Tract InfectionYmelda ComediamNo ratings yet
- Urinary Tract Disorders/Infectio NDocument44 pagesUrinary Tract Disorders/Infectio NrintyosoNo ratings yet
- Ec2 UrinaryDocument4 pagesEc2 UrinaryDiana Marie ReyesNo ratings yet
- Urinary Tract Infections: by John MbawaDocument33 pagesUrinary Tract Infections: by John MbawaAlvin OmondiNo ratings yet
- 1 Infeksi Saluran Kemih New-1Document61 pages1 Infeksi Saluran Kemih New-1Dezttie IdEss NdessNo ratings yet
- Bab 1 Pendahuluan A. Latar BelakangDocument2 pagesBab 1 Pendahuluan A. Latar BelakangZainul HumamNo ratings yet
- Predisposing FactorsDocument14 pagesPredisposing FactorsThomas GealonNo ratings yet
- Uti PathoDocument15 pagesUti PathoEden Astred ObilloNo ratings yet
- Case Study 102Document6 pagesCase Study 102Cheska Lopez100% (1)
- Urinary Tract InfectionsDocument9 pagesUrinary Tract InfectionsGeethika GummadiNo ratings yet
- UTI LectureDocument62 pagesUTI LectureHaidar ShiddiqNo ratings yet
- Cystitis, A Simple Guide To The Condition Treatment And Urinary DiseasesFrom EverandCystitis, A Simple Guide To The Condition Treatment And Urinary DiseasesNo ratings yet
- A Simple Guide to Sexually Transmitted DiseasesFrom EverandA Simple Guide to Sexually Transmitted DiseasesRating: 5 out of 5 stars5/5 (9)
- Urinary Tract Infection in Children - Classification, Diagnosis and TreatmentFrom EverandUrinary Tract Infection in Children - Classification, Diagnosis and TreatmentNo ratings yet
- Schematic Diagram: Predisposing Factors: DiabeticsDocument1 pageSchematic Diagram: Predisposing Factors: Diabeticsrraven16No ratings yet
- IMCI GuidelinesDocument173 pagesIMCI Guidelineskabamba0% (1)
- First Edition Surgical Safety ChecklistDocument1 pageFirst Edition Surgical Safety Checklistrraven16No ratings yet
- Surgical Safety ChecklistDocument1 pageSurgical Safety Checklistmillechilli1No ratings yet
- First Edition Surgical Safety ChecklistDocument1 pageFirst Edition Surgical Safety Checklistrraven16No ratings yet
- Vibrio CholeraeDocument20 pagesVibrio CholeraeBernadette BeltranNo ratings yet
- Case Study of MicrobiologyDocument4 pagesCase Study of MicrobiologyQaisrani Y9No ratings yet
- Biological Control 178 (2023) 105145 M. Yousefvand Et AlDocument5 pagesBiological Control 178 (2023) 105145 M. Yousefvand Et AlGenaina CristofoliNo ratings yet
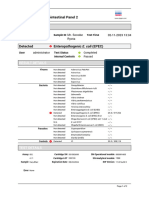
- Mr. SONOBE RYOTA - 2311020007AJDocument2 pagesMr. SONOBE RYOTA - 2311020007AJmolekular diagnosNo ratings yet
- 28 - 04 RPS Pulmonologi TB SO, TB RO, TB Laten-1Document46 pages28 - 04 RPS Pulmonologi TB SO, TB RO, TB Laten-1ANISA SALAMAHNo ratings yet
- 2014 ProsidingSNIJADocument17 pages2014 ProsidingSNIJASayu Putu Yuni ParyatiNo ratings yet
- MicrobiologyDocument81 pagesMicrobiologyAmanuel MaruNo ratings yet
- Classification of Clinically Significant Bacteria by GenusDocument2 pagesClassification of Clinically Significant Bacteria by GenusSEAN BUINo ratings yet
- MCQsDocument2 pagesMCQsAhmad RajoubNo ratings yet
- Am Positive & Gram Negative Cocci InfectionsDocument33 pagesAm Positive & Gram Negative Cocci InfectionsRebeka Costantina Weriditi0% (1)
- Soal Pretest AnaerobDocument4 pagesSoal Pretest AnaerobmuthiajayantiNo ratings yet
- Domain Bacteria 1Document3 pagesDomain Bacteria 1Ezra JungNo ratings yet
- FOUNDATION OF CONTROL QUESTIONS OF EXAM 2020-2021 General MedicineDocument7 pagesFOUNDATION OF CONTROL QUESTIONS OF EXAM 2020-2021 General MedicineSoz P. KawaniNo ratings yet
- 29725Document10 pages29725zzzzNo ratings yet
- Types of HemolysisDocument17 pagesTypes of HemolysisThe tooth fairyNo ratings yet
- Brochura UrgoTul AGDocument4 pagesBrochura UrgoTul AGDaniguedesNo ratings yet
- CV Titik Nuryastuti UGM, Januari 2021Document6 pagesCV Titik Nuryastuti UGM, Januari 2021Hanny Siti NuraeniNo ratings yet
- Spec FarmaDocument8 pagesSpec FarmaМилан ЂурђевићNo ratings yet
- List of Medically Important BacteriaDocument11 pagesList of Medically Important BacteriaMary ChristelleNo ratings yet
- Yuca Fermentada de BrasilDocument7 pagesYuca Fermentada de BrasilLuis Enrique Ortega SalinasNo ratings yet
- Lab Report 9Document14 pagesLab Report 9Jhon Patrick DelmonteNo ratings yet
- Istoric: Din Antichitate Pina in Sec. 19Document303 pagesIstoric: Din Antichitate Pina in Sec. 19Lyly LylyNo ratings yet
- Biofilms in EntDocument4 pagesBiofilms in EntDrsiya MedfriendNo ratings yet
- Microbial Control Part 2Document26 pagesMicrobial Control Part 2Christiel John MagtibayNo ratings yet
- Ornithine Hippurate Nitrate VP/MR Casein/ Tyrosine Niacin Tween 80 HOH Pyrazinamidas eDocument2 pagesOrnithine Hippurate Nitrate VP/MR Casein/ Tyrosine Niacin Tween 80 HOH Pyrazinamidas eKristine PangahinNo ratings yet
- Essentials of Genetics 9th Edition Klug Test Bank 1Document36 pagesEssentials of Genetics 9th Edition Klug Test Bank 1stevenknappkorcfzgiwa100% (32)
- Glycerol PreservationDocument7 pagesGlycerol Preservationashra sindhikkaaNo ratings yet
- Jurnal A Kel 1Document7 pagesJurnal A Kel 1Pratiwi IshakNo ratings yet
Urinary Track Infection Pathopysiology 1
Urinary Track Infection Pathopysiology 1
Uploaded by
rraven160 ratings0% found this document useful (0 votes)
71 views3 pagesThe urinary tract is normally sterile but can become infected by bacteria ascending from the urethra or hematogenously. E. coli causes over 75% of community-acquired urinary tract infections (UTIs), while other gram-negative bacteria like Klebsiella, Proteus, and Pseudomonas and gram-positive bacteria like Enterococcus and Staphylococcus account for the remainder. UTIs can infect the bladder (cystitis), urethra, ureters, or kidneys and cause symptoms like burning during urination and abdominal pain. People more susceptible to UTIs include women, diabetics, infants, and those with anatomical abnormalities or lowered immunity.
Original Description:
Hope you it helped you
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe urinary tract is normally sterile but can become infected by bacteria ascending from the urethra or hematogenously. E. coli causes over 75% of community-acquired urinary tract infections (UTIs), while other gram-negative bacteria like Klebsiella, Proteus, and Pseudomonas and gram-positive bacteria like Enterococcus and Staphylococcus account for the remainder. UTIs can infect the bladder (cystitis), urethra, ureters, or kidneys and cause symptoms like burning during urination and abdominal pain. People more susceptible to UTIs include women, diabetics, infants, and those with anatomical abnormalities or lowered immunity.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
71 views3 pagesUrinary Track Infection Pathopysiology 1
Urinary Track Infection Pathopysiology 1
Uploaded by
rraven16The urinary tract is normally sterile but can become infected by bacteria ascending from the urethra or hematogenously. E. coli causes over 75% of community-acquired urinary tract infections (UTIs), while other gram-negative bacteria like Klebsiella, Proteus, and Pseudomonas and gram-positive bacteria like Enterococcus and Staphylococcus account for the remainder. UTIs can infect the bladder (cystitis), urethra, ureters, or kidneys and cause symptoms like burning during urination and abdominal pain. People more susceptible to UTIs include women, diabetics, infants, and those with anatomical abnormalities or lowered immunity.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 3
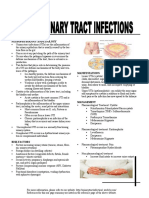
Pathophysiology:
The urinary tract, from the kidneys to the urethral meatus,
is normally sterile and resistant to bacterial colonization
despite frequent contamination of the distal urethra with colonic
bacteria. Mechanisms that maintain the tract's sterility include
urine acidity, emptying of the bladder at micturition,
ureterovesical and urethral sphincters, and various immunologic
and mucosal barriers.
About 95% of UTIs occur when bacteria ascend the urethra to the
bladder and, in the case of acute uncomplicated pyelonephritis,
ascend the ureter to the kidney. The remainder of UTIs are
hematogenous. Systemic infection can result from UTI,
particularly in the elderly. About 6.5% of cases of hospital-
acquired bacteremia are attributable to UTI.
A urinary tract infection is an infection of any of the organs in
the urinary tract, which consist of the bladder, the ureter, the
urethra, and the kidneys.
A urinary tract infection (UTI) may occur in the: Bladder -
Cystitis is an infection of the bladder. This is the most common
form of UTI; it can be aggravated if the bladder does not empty
completely when you urinate. Urethra - Urethritis is
infection/inflammation of the urethra. This can be due to other
things besides the organisms usually involved in UTI’s; in
particular, many sexually transmitted diseases (STD’s) appear
initially as urethritis. Ureter – Ureteritis is infection of a
ureter. This can occur if the bacteria entered the urinary tract
from above, or if the ureter-to-bladder valves don’t work
properly and allow urine to “reflux” from the bladder into the
ureters. Kidney – Pyelonephritis is an infection of the kidney
itself. This can happen with infection from above, or if reflux
into the ureters is so bad that infected urine refluxes all the
way to the kidney.
Commensal colonic gram-negative aerobic bacteria cause most
bacterial UTIs. In relatively normal tracts, strains of E. coli
with specific attachment factors for transitional epithelium of
the bladder and ureters are the most frequent causes. The
remaining gram-negative urinary pathogens are other
enterobacteria, especially Klebsiella , Proteus mirabilis, and
Pseudomonas aeruginosa. Enterococci (group D streptococci) and
coagulase-negative staphylococci (eg, Staphylococcus
saprophyticus) are the most frequently implicated gram-positive
organisms.
E. coli causes > 75% of community-acquired UTIs in all age
groups; S. saprophyticus accounts for about 10%. In hospitalized
patients, E. coli accounts for about 50% of cases. The gram-
negative species Klebsiella , Proteus, Enterobacter, and Serratia
account for about 40%, and the gram-positive bacterial cocci
Enterococcus faecalis and S. saprophyticus and Staphylococcus
aureus account for the remainder.
People more susceptible to UTI’s:
Diabetics because of changes in the immune system
Infants who are born with abnormalities of the urinary tract
A woman has shorter length of the urethra.
Women whose partners use a condom with spermicidal foam
A person who has already had a UTI
Pregnant women
Post-menopausal women
Women with lowered immunity
Women with obstructions in the urinary tract
Signs and Symptoms of UTI
Burning sensation at the start of urination
Burning sensation in the middle of urination
Fever
Lower abdominal pain
Funny smell, color, or appearance (cloudy, dark, blood
tinged) of urine
Pain in back, flanks, or abdomen
Nausea
Vomiting
Other Signs and Symptoms of UTI
Uncomfortable pressure above pubic bone
Fullness in rectum (in men only)
Small amount of urine, despite urge to urinate
Irritability (in children only
You might also like
- PharmacologyDocument33 pagesPharmacologyFreeNursingNotes90% (68)
- Medical Microbiology and Immunology Flash Cards - Sample ChapterDocument250 pagesMedical Microbiology and Immunology Flash Cards - Sample Chapterleh.mo931580% (5)
- Types of Urinary Tract InfectionDocument4 pagesTypes of Urinary Tract InfectionGencris Medrano Giray RNNo ratings yet
- Infections of The Urinary TractDocument47 pagesInfections of The Urinary Tractsandrarosok88No ratings yet
- Infeksi Saluran KemihDocument65 pagesInfeksi Saluran KemihHaziq AnuarNo ratings yet
- Urinary Tract InfectionsDocument17 pagesUrinary Tract Infectionss.khan9211rediffmail.comNo ratings yet
- Urinary Tract InfectionsDocument71 pagesUrinary Tract Infectionsdayibon499No ratings yet
- Urinary Tract InfectionDocument5 pagesUrinary Tract InfectionDRANo ratings yet
- Cases of Group 3 LC 1Document13 pagesCases of Group 3 LC 1abdul basithNo ratings yet
- Infection Urinary Tract Urine Bladder KidneyDocument18 pagesInfection Urinary Tract Urine Bladder KidneygdquijanoNo ratings yet
- UTIDocument6 pagesUTIAyessa Marie BarbosaNo ratings yet
- Tai Lieu Tieng Anh Cho Sinh Vien Bai Nhiem Khuan Duong Tiet NieuDocument3 pagesTai Lieu Tieng Anh Cho Sinh Vien Bai Nhiem Khuan Duong Tiet NieuLê Mỹ Khánh LyNo ratings yet
- UTI (Urinary Tract Infection)Document9 pagesUTI (Urinary Tract Infection)Carson BirthNo ratings yet
- Urinary Tract Infection - Kuliah Mahasiswa - Ferbruari 2017 - EDITDocument52 pagesUrinary Tract Infection - Kuliah Mahasiswa - Ferbruari 2017 - EDITRahmawati HamudiNo ratings yet
- The Urinary System. The Urinary System Helps Maintain Proper Water and Salt Balance ThroughoutDocument4 pagesThe Urinary System. The Urinary System Helps Maintain Proper Water and Salt Balance ThroughoutArjay EspañolNo ratings yet
- Urinary Tract Infection (UTI)Document9 pagesUrinary Tract Infection (UTI)ogwal andrewictynetNo ratings yet
- Uti Case StudyDocument7 pagesUti Case StudyStephNo ratings yet
- Urinary Tract InfectionDocument6 pagesUrinary Tract InfectionYalc LapidNo ratings yet
- Urinary Tract InfectionDocument7 pagesUrinary Tract InfectionNader Smadi100% (7)
- CASE STUDY #3 Urinary System (Urninary Tract Infection or UTI)Document5 pagesCASE STUDY #3 Urinary System (Urninary Tract Infection or UTI)Lerma PagcaliwanganNo ratings yet
- RLE Urinary Tract InfectionDocument13 pagesRLE Urinary Tract InfectionAliza AlyyNo ratings yet
- Renal DisDocument166 pagesRenal DisCharles MutaiNo ratings yet
- Urinarytract InfectionDocument61 pagesUrinarytract InfectionsanjivdasNo ratings yet
- Urogenital InfectionsDocument24 pagesUrogenital InfectionsGaurav100% (1)
- Urinary Tract Infection: CC Ricky G. JalecoDocument56 pagesUrinary Tract Infection: CC Ricky G. JalecoRicky JalecoNo ratings yet
- An Individual Case Study ON Urinary Tract Infection (UTI) : Southern Isabela General HospitalDocument20 pagesAn Individual Case Study ON Urinary Tract Infection (UTI) : Southern Isabela General HospitalhanapotakoNo ratings yet
- Urinary Tract InfectionDocument10 pagesUrinary Tract Infectionjaah diazNo ratings yet
- UTI Pediatric NotesDocument2 pagesUTI Pediatric NotesSanya BNo ratings yet
- Microbial Diseases of The Urinary System: Yemane Weldu (MSC., Assistant Professor)Document65 pagesMicrobial Diseases of The Urinary System: Yemane Weldu (MSC., Assistant Professor)Lidiya TeshomeNo ratings yet
- Urinary Tract InfectionsDocument39 pagesUrinary Tract InfectionsYordanos GetnetNo ratings yet
- Symptoms: For Bladder InfectionsDocument5 pagesSymptoms: For Bladder InfectionsGene Ryuzaki SeseNo ratings yet
- Urinary Tract InfectionDocument30 pagesUrinary Tract InfectionLeo Mar MakilanNo ratings yet
- ####Bahan Kuliah ISK Blok 23 (Nov 2015)Document32 pages####Bahan Kuliah ISK Blok 23 (Nov 2015)ajengdmrNo ratings yet
- Prevalence of Uti in Benin PDFDocument54 pagesPrevalence of Uti in Benin PDFcamiladovalle95No ratings yet
- Urinary Tract Infection (Maramag Eunice Laman Jenny Pearl)Document16 pagesUrinary Tract Infection (Maramag Eunice Laman Jenny Pearl)Carlojay IniegoNo ratings yet
- Infections of The Urinary Genirouty TractDocument4 pagesInfections of The Urinary Genirouty Tractfifa nasrul ummahNo ratings yet
- Uti ReadingsDocument6 pagesUti ReadingskarenbelnasNo ratings yet
- DR Lana Sundac - LGRS Urinary Tract InfectionsDocument4 pagesDR Lana Sundac - LGRS Urinary Tract Infectionsoxford_commaNo ratings yet
- Renal Notes Step 2ckDocument34 pagesRenal Notes Step 2cksamreen100% (1)
- Handout 2Document1 pageHandout 2api-320812761No ratings yet
- Background: Urinary Tract InfectionDocument9 pagesBackground: Urinary Tract InfectionOnieBoy CurayagNo ratings yet
- Urinary Tract InfectionDocument24 pagesUrinary Tract InfectionraddagNo ratings yet
- Theoretical Background Urinary Tract InfectionDocument7 pagesTheoretical Background Urinary Tract Infectiondenebrench23No ratings yet
- Urinary Tract Infection (Uti) Definition:: TypesDocument2 pagesUrinary Tract Infection (Uti) Definition:: TypesAneela ManzoorNo ratings yet
- Urinary Tract InfectionDocument3 pagesUrinary Tract InfectionHo Yong WaiNo ratings yet
- Urinary Tract Infection (UTI)Document39 pagesUrinary Tract Infection (UTI)Sabita TripathiNo ratings yet
- IskDocument35 pagesIskfadliNo ratings yet
- Urinary Tract InfectionDocument50 pagesUrinary Tract Infectionpokhara gharipatan100% (1)
- What Is A Urinary Tract InfectionDocument2 pagesWhat Is A Urinary Tract InfectionYmelda ComediamNo ratings yet
- Urinary Tract Disorders/Infectio NDocument44 pagesUrinary Tract Disorders/Infectio NrintyosoNo ratings yet
- Ec2 UrinaryDocument4 pagesEc2 UrinaryDiana Marie ReyesNo ratings yet
- Urinary Tract Infections: by John MbawaDocument33 pagesUrinary Tract Infections: by John MbawaAlvin OmondiNo ratings yet
- 1 Infeksi Saluran Kemih New-1Document61 pages1 Infeksi Saluran Kemih New-1Dezttie IdEss NdessNo ratings yet
- Bab 1 Pendahuluan A. Latar BelakangDocument2 pagesBab 1 Pendahuluan A. Latar BelakangZainul HumamNo ratings yet
- Predisposing FactorsDocument14 pagesPredisposing FactorsThomas GealonNo ratings yet
- Uti PathoDocument15 pagesUti PathoEden Astred ObilloNo ratings yet
- Case Study 102Document6 pagesCase Study 102Cheska Lopez100% (1)
- Urinary Tract InfectionsDocument9 pagesUrinary Tract InfectionsGeethika GummadiNo ratings yet
- UTI LectureDocument62 pagesUTI LectureHaidar ShiddiqNo ratings yet
- Cystitis, A Simple Guide To The Condition Treatment And Urinary DiseasesFrom EverandCystitis, A Simple Guide To The Condition Treatment And Urinary DiseasesNo ratings yet
- A Simple Guide to Sexually Transmitted DiseasesFrom EverandA Simple Guide to Sexually Transmitted DiseasesRating: 5 out of 5 stars5/5 (9)
- Urinary Tract Infection in Children - Classification, Diagnosis and TreatmentFrom EverandUrinary Tract Infection in Children - Classification, Diagnosis and TreatmentNo ratings yet
- Schematic Diagram: Predisposing Factors: DiabeticsDocument1 pageSchematic Diagram: Predisposing Factors: Diabeticsrraven16No ratings yet
- IMCI GuidelinesDocument173 pagesIMCI Guidelineskabamba0% (1)
- First Edition Surgical Safety ChecklistDocument1 pageFirst Edition Surgical Safety Checklistrraven16No ratings yet
- Surgical Safety ChecklistDocument1 pageSurgical Safety Checklistmillechilli1No ratings yet
- First Edition Surgical Safety ChecklistDocument1 pageFirst Edition Surgical Safety Checklistrraven16No ratings yet
- Vibrio CholeraeDocument20 pagesVibrio CholeraeBernadette BeltranNo ratings yet
- Case Study of MicrobiologyDocument4 pagesCase Study of MicrobiologyQaisrani Y9No ratings yet
- Biological Control 178 (2023) 105145 M. Yousefvand Et AlDocument5 pagesBiological Control 178 (2023) 105145 M. Yousefvand Et AlGenaina CristofoliNo ratings yet
- Mr. SONOBE RYOTA - 2311020007AJDocument2 pagesMr. SONOBE RYOTA - 2311020007AJmolekular diagnosNo ratings yet
- 28 - 04 RPS Pulmonologi TB SO, TB RO, TB Laten-1Document46 pages28 - 04 RPS Pulmonologi TB SO, TB RO, TB Laten-1ANISA SALAMAHNo ratings yet
- 2014 ProsidingSNIJADocument17 pages2014 ProsidingSNIJASayu Putu Yuni ParyatiNo ratings yet
- MicrobiologyDocument81 pagesMicrobiologyAmanuel MaruNo ratings yet
- Classification of Clinically Significant Bacteria by GenusDocument2 pagesClassification of Clinically Significant Bacteria by GenusSEAN BUINo ratings yet
- MCQsDocument2 pagesMCQsAhmad RajoubNo ratings yet
- Am Positive & Gram Negative Cocci InfectionsDocument33 pagesAm Positive & Gram Negative Cocci InfectionsRebeka Costantina Weriditi0% (1)
- Soal Pretest AnaerobDocument4 pagesSoal Pretest AnaerobmuthiajayantiNo ratings yet
- Domain Bacteria 1Document3 pagesDomain Bacteria 1Ezra JungNo ratings yet
- FOUNDATION OF CONTROL QUESTIONS OF EXAM 2020-2021 General MedicineDocument7 pagesFOUNDATION OF CONTROL QUESTIONS OF EXAM 2020-2021 General MedicineSoz P. KawaniNo ratings yet
- 29725Document10 pages29725zzzzNo ratings yet
- Types of HemolysisDocument17 pagesTypes of HemolysisThe tooth fairyNo ratings yet
- Brochura UrgoTul AGDocument4 pagesBrochura UrgoTul AGDaniguedesNo ratings yet
- CV Titik Nuryastuti UGM, Januari 2021Document6 pagesCV Titik Nuryastuti UGM, Januari 2021Hanny Siti NuraeniNo ratings yet
- Spec FarmaDocument8 pagesSpec FarmaМилан ЂурђевићNo ratings yet
- List of Medically Important BacteriaDocument11 pagesList of Medically Important BacteriaMary ChristelleNo ratings yet
- Yuca Fermentada de BrasilDocument7 pagesYuca Fermentada de BrasilLuis Enrique Ortega SalinasNo ratings yet
- Lab Report 9Document14 pagesLab Report 9Jhon Patrick DelmonteNo ratings yet
- Istoric: Din Antichitate Pina in Sec. 19Document303 pagesIstoric: Din Antichitate Pina in Sec. 19Lyly LylyNo ratings yet
- Biofilms in EntDocument4 pagesBiofilms in EntDrsiya MedfriendNo ratings yet
- Microbial Control Part 2Document26 pagesMicrobial Control Part 2Christiel John MagtibayNo ratings yet
- Ornithine Hippurate Nitrate VP/MR Casein/ Tyrosine Niacin Tween 80 HOH Pyrazinamidas eDocument2 pagesOrnithine Hippurate Nitrate VP/MR Casein/ Tyrosine Niacin Tween 80 HOH Pyrazinamidas eKristine PangahinNo ratings yet
- Essentials of Genetics 9th Edition Klug Test Bank 1Document36 pagesEssentials of Genetics 9th Edition Klug Test Bank 1stevenknappkorcfzgiwa100% (32)
- Glycerol PreservationDocument7 pagesGlycerol Preservationashra sindhikkaaNo ratings yet
- Jurnal A Kel 1Document7 pagesJurnal A Kel 1Pratiwi IshakNo ratings yet