Professional Documents
Culture Documents
Resurfacing
Resurfacing
Uploaded by
Daniel ZumárragaCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hitachi ZX85US Operator S ManualDocument313 pagesHitachi ZX85US Operator S Manualalesca1978100% (12)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Automatic Voltage Regulators: SpecificationsDocument4 pagesAutomatic Voltage Regulators: SpecificationsArman Haq100% (9)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Petrel Manual: Vshale CalculationDocument20 pagesPetrel Manual: Vshale CalculationEmira Zrelli100% (1)
- Ee4302 Ca1Document51 pagesEe4302 Ca1Norul Ashikin NorzainNo ratings yet
- Integrated Operations in The Oil and Gas Industry Sustainability and Capability Development PDFDocument458 pagesIntegrated Operations in The Oil and Gas Industry Sustainability and Capability Development PDFkglorstadNo ratings yet
- International RoamingDocument25 pagesInternational RoamingAbu Bakir Akhter75% (4)
- Intrusion Detection System Using Multivariate Control Chart Hotelling's T Based On PCADocument7 pagesIntrusion Detection System Using Multivariate Control Chart Hotelling's T Based On PCARumaisa KrubaNo ratings yet
- Noise Reduction in Images Using AutoencodersDocument7 pagesNoise Reduction in Images Using AutoencodersIJRASETPublicationsNo ratings yet
- 9323a251g PTDocument3 pages9323a251g PTClarice Alves de FreitasNo ratings yet
- WaymakerDocument23 pagesWaymakerJORDAN FREENo ratings yet
- Social Networking Software: A SWOT AnalysisDocument10 pagesSocial Networking Software: A SWOT AnalysisShivani SainiNo ratings yet
- A Tutorial On Jasperreports Ireport and JfreechartDocument21 pagesA Tutorial On Jasperreports Ireport and JfreechartDanijela Milicevic MalisicNo ratings yet
- Concrete & Shuttering Working-R1Document20 pagesConcrete & Shuttering Working-R1vivekNo ratings yet
- Exercícios SemanaisDocument11 pagesExercícios SemanaisElias Carvalho100% (2)
- Odell - Nikon1V1 J1 - Guide v1.064 Excerpt PDFDocument33 pagesOdell - Nikon1V1 J1 - Guide v1.064 Excerpt PDFmasreogNo ratings yet
- Liebherr Tower Cranes enDocument42 pagesLiebherr Tower Cranes enRaman Iyer100% (1)
- Ameyo Product BrochureDocument8 pagesAmeyo Product BrochureSudhanshu Gupta100% (1)
- Heavy Duty BrochureDocument16 pagesHeavy Duty BrochureАлексей ГордиенкоNo ratings yet
- (Kinetico) MachBackwashingFilterownersmanualDocument48 pages(Kinetico) MachBackwashingFilterownersmanualGreg ReynekeNo ratings yet
- Crodasinic LS LeafletDocument2 pagesCrodasinic LS LeafleticraoNo ratings yet
- In: 48 VDC - Out: 35 VDC / 2 A: Miro TR 24Vdc FK 5P Opto-Coupler ModuleDocument2 pagesIn: 48 VDC - Out: 35 VDC / 2 A: Miro TR 24Vdc FK 5P Opto-Coupler ModuleDannyNo ratings yet
- Faculty of Engineering and Applied ScienceDocument30 pagesFaculty of Engineering and Applied ScienceJaspreet SinghNo ratings yet
- Nokia VP8 Infringement Claim Chart For '211 PatentDocument37 pagesNokia VP8 Infringement Claim Chart For '211 PatentFlorian MuellerNo ratings yet
- Site Meeting 03Document4 pagesSite Meeting 03Fakrul AdliNo ratings yet
- Index Page and 2nd Page of EEDocument2 pagesIndex Page and 2nd Page of EEAmir KhanNo ratings yet
- Logic Level Triac: TO92 (Plastic)Document4 pagesLogic Level Triac: TO92 (Plastic)abel gaunaNo ratings yet
- Otc 31506 MsDocument10 pagesOtc 31506 MsAdriana UstarizNo ratings yet
- Deltec Voyage PDFDocument3 pagesDeltec Voyage PDFPaul RasmussenNo ratings yet
- Steam TableDocument1 pageSteam TableKrismawan Saptya YudhaNo ratings yet
Resurfacing
Resurfacing
Uploaded by
Daniel ZumárragaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Resurfacing
Resurfacing
Uploaded by
Daniel ZumárragaCopyright:
Available Formats
Produced with a Trial Version of PDF Annotator - www.PDFAnnotator.
com
Hip Resurfacing
Arthroplasty
Michael A. Mont, MD Abstract
Phillip S. Ragland, MD Hip resurfacing arthroplasty is a type of hip replacement that
Gracia Etienne, MD, PhD involves capping the femoral head and preserving bone of the
Thorsten M. Seyler, MD proximal femur. Metal-on-metal surface replacements have been
manufactured since the early 1990s. Recent studies indicate
Thomas P. Schmalzried, MD
excellent clinical results with low failure rates at 1- to 5-year
follow-up. Although these early results are encouraging, resurfacing
devices must be used with caution because less is known about
their long-term safety and efficacy. The best candidates for
resurfacing are patients younger than age 60 years with good bone
stock. The surgical approach is similar to that for standard total hip
replacements, but with slightly more dissection because the
femoral head must be preserved and displaced to visualize the
Dr. Mont is Director, Center for Joint acetabulum. To reduce complications, resurfacing arthroplasty
Preservation and Reconstruction, Rubin
should be performed by surgeons who have received training
Institute for Advanced Orthopaedics,
Sinai Hospital of Baltimore, Baltimore, specifically in this technique.
MD. Dr. Ragland is Clinical Research
Fellow, Center for Joint Preservation and
F
Reconstruction, Rubin Institute for emoral resurfacing is a type of stage osteonecrosis of the femoral
Advanced Orthopaedics, Sinai Hospital hip replacement that conserves head has been continuously em-
of Baltimore. Dr. Etienne is Attending bone in the proximal femur. The ployed through the present day. New
Surgeon, Center for Joint Preservation femoral head is prepared with bone metallurgy allows resurfacing with
and Reconstruction, Rubin Institute for cutting tools that enable the remain- metal-on-metal articulations, and
Advanced Orthopaedics, Sinai Hospital ing femoral head to be capped, sim- there has been a resurgence in the
of Baltimore. Dr. Seyler is Clinical
ilar to the way in which a dentist use of total hip resurfacing to man-
Research Fellow, Center for Joint
caps a tooth. The femoral head ei- age many arthritides. Short-term re-
Preservation and Reconstruction, Rubin
ther articulates with the native ace- sults are excellent with resurfacing
Institute for Advanced Orthopaedics,
tabular cartilage or is mated to an ac- hip arthroplasty, but long-term re-
Sinai Hospital of Baltimore. Dr.
etabular component. sults have yet to be published. To en-
Schmalzried is Associate Director, Joint
Hip resurfacing prostheses pre- sure optimal results, the surgeon
Replacement Institute, Los Angeles, CA.
date the use of stemmed femoral must be aware of the indications and
Reprint requests: Dr. Mont, Rubin components. Various materials were contraindications and should be spe-
Institute of Advanced Orthopaedics, used in the 1930s through the 1950s, cifically trained in resurfacing ar-
Center for Joint Preservation and including ivory, glass, and stainless throplasty.
Reconstruction, Sinai Hospital of steel. Femoral resurfacing coupled
Baltimore, 2401 West Belvedere with cemented polyethylene acetab-
Resurfacing
Avenue, Baltimore, MD 21215. ular resurfacing was popular in the
1970s, but it fell out of use because Advantages
J Am Acad Orthop Surg 2006;14:454-
of high rates of bone resorption Resurfacing of arthritic joint sur-
463
(osteolysis) and loosening within faces with prosthetic components is
Copyright 2006 by the American 5 years of surgery.1-3 The use of a the accepted and widely used stan-
Academy of Orthopaedic Surgeons. femoral resurfacing component dard in total knee replacement. Sim-
alone to treat patients with late- ple resurfacing of the worn joint sur-
454 Journal of the American Academy of Orthopaedic Surgeons
Produced with a Trial Version of PDF Annotator - www.PDFAnnotator.com
Michael A. Mont, MD, et al
faces has less frequently been used as Figure 1
a means of total hip arthroplasty
(THA), however (Figure 1). Resurfac-
ing has several theoretic advantages.
Bone Preservation
One obvious advantage of resur-
facing is that it preserves bone on
the femoral side. It is preferable to
retain the femoral head and avoid us-
ing the intramedullary devices that
are implanted in standard hip re-
placements. However, resurfacing
requires a more difficult surgical ex-
posure to prepare the acetabulum
without excising the femoral head
and neck. For resurfacing to be truly
conservative, the surgeon should not
remove any more bone from the ac-
etabulum than would be required for
a THA, a goal that has only recently
been addressed by companies manu-
facturing thinner acetabular shells.
Stress Transfer
An additional advantage of resur-
facing hip arthroplasty is better
stress transfer to the proximal fe- Preoperative (A) and postoperative (B) anteroposterior radiographs of a metal-on-
mur. This may avoid long-term metal resurfacing hip arthroplasty in a 46-year-old man who was treated for primary
problems caused by stress shielding osteoarthritis.
of the proximal femur, which can oc-
cur with intramedullary fixation of
THA stems. Watanabe et al4 found more closely resembles a normal hip dition, periprosthetic bone loss,
stress shielding below resurfacing and may have better proprioception which was often extensive with
prostheses, but Kishida et al5 noted than conventional THAs.9,10 polyethylene acetabular resurfacing
less loss of bone density of the prox- components, may be markedly re-
imal femur in resurfaced hips than Revision duced with metal-on-metal bearings.
in standard hip replacements. Another theoretic advantage of With early polyethylene acetabular
resurfacing is that revision of the resurfacing components, much bone
Dislocation femoral component, when neces- was removed during insertion. Con-
A large femoral prosthesis (36 to sary, may be easier than revision of temporary components have a met-
54 mm in diameter) is associated an intramedullary THA.6,11 In the al acetabular bearing that requires
with a lower dislocation rate than event of a femoral-side failure (eg, removal of little acetabular bone
conventional total hips with head di- loosening, femoral neck fracture), stock. With femoral side failure, the
ameters between 22 and 32 mm. In the femoral neck can be cut below acetabular component can be left in
three large recent series, no disloca- the prosthesis or fracture line and a place and mated to a standard femo-
tions of the hip were found.6-8 In ad- conventional total hip stem inserted ral component with a large-diameter
dition, resurfacing kinematically into the intramedullary canal. In ad- femoral head12 (Figure 2).
Dr. Mont and Dr. Etienne serve as consultants to or are employees of Wright Medical Technology. Dr. Schmalzried or the department with which
he is affiliated has received research or institutional support from DePuy and Wright Medical Technology. Dr. Schmalzried or the department with
which he is affiliated serves as a consultant to or is an employee of DePuy. None of the following authors or the departments with which they are
affiliated has received anything of value from or owns stock in a commercial company or institution related directly or indirectly to the subject of
this article: Dr. Ragland and Dr. Seyler.
Volume 14, Number 8, August 2006 455
Produced with a Trial Version of PDF Annotator - www.PDFAnnotator.com
Hip Resurfacing Arthroplasty
Figure 2 50 hips resurfaced (22% [11 hips]), remaining osseous defects, which
with one fracture in the next group were seen after bone preparation
of 50 (2%), and no fractures in the that diminished the surface area
next 200 cases. In a recent study of available for fixation.
3,497 cases of hip resurfacing in Aus-
tralia, 50 fractures occurred (inci- Metal Degradation
dence, 1.46%).14 Metal degradation may cause pa-
The causes of fracture appear to tient blood and urine metal levels to
be both patient- and technique- exceed levels associated with other
related. Patient-related factors in- bearing surfaces. The role of metal
clude obesity, decreased bone mass, ions in relation to delayed type and
and inflammatory arthritis. Intraop- humeral hypersensitivity reactions
erative characteristics that may lead in patients with metal-on-metal im-
to fracture include femoral neck plants remains unknown.
cysts and exposed bone found during
preparation. Surgical errors include
Metal-on-Polyethylene
notching of the femoral neck, tilting
Resurfacing
of the prosthesis into excess varus
(<130° neck-shaft angle), and im- Metal-on-polyethylene resurfacing
proper prosthetic seating. In the was introduced in the 1970s as a
Australian national study,14 the rel- bone-preserving alternative to con-
ative risk of fracture was twofold ventional THA. Although short-
higher in women than in men (P < term indications for most of these
Postoperative anteroposterior 0.01), and there was an increased devices were promising, mid- and
radiograph of a Big Femoral Head risk of fracture with varus place- long-term follow-up yielded unac-
prosthesis (Wright Medical Technology, ment of the femoral component and ceptably high failure rates.1-3 Failures
Arlington, TN). Note the large femoral with intraoperative notching of the were attributed to patient selection,
head on a standard stem, which is femoral neck. Technical problems surgical technique, and implant
mated with a resurfacing acetabular were noted in 85% of the cases with quality and design. The primary
component. subsequent fracture. cause of failure, however, was
Conversion to standard THA af- polyethylene-induced osteolysis re-
Disadvantages ter fracture has not been difficult. sulting from the mating of large met-
Hip resurfacing has several disad- The two options are completely re- al femoral head components with
vantages. The lack of modularity of vising both components or leaving thin-diameter polyethylene acetabu-
these devices reduces the ability to the acetabular component in place lar cups (Figure 3). Volumetric poly-
adjust leg length. Resurfacing is not with a standard stem, using a large ethylene wear was often 10 times
appropriate in hips with loss of fem- femoral head to articulate with the higher than for standard hip replace-
oral head and neck bone stock or in cup. ments with head sizes ≤32 mm.17 Be-
hips with femoral cysts. In these pa- cause of these discouraging results,
tients, resurfacing may cause femo- Aseptic Loosening resurfacing arthroplasty fell out of
ral neck fracture. Aseptic loosening has been found favor in the early 1980s and only re-
in some series. Amstutz et al6 re- cently has regained some acceptance
Femoral Neck Fracture ported seven cases of femoral pros- for managing osteonecrosis and oth-
Femoral neck fracture is a unique thesis loosening in their series of 400 er arthritides.
complication of resurfacing, with hips. Most occurred in the first 100
an incidence ranging from 0% to cases and were attributed to intraop-
Metal-on-Metal
4%.6-8,13-16 Fracture usually is found erative errors. Demographic factors
Resurfacing for Arthritis
early in series, with declining rates that influenced loosening in this se-
as the surgeon overcomes the learn- ries included an average femoral Metal-on-metal total hip prostheses
ing curve. For example, of 400 total stem shaft angle of 128.3°, which dif- with a conventional femoral stem
hip resurfacing arthroplasties, Am- fered from that of the rest of the pa- were used in the 1960s but were
stutz et al6 reported three fractures, tients (average, 136°). In addition, in abandoned in the 1970s because of
all of which occurred in the first five of the seven hips with loosen- the reported higher success rate of
group of 100. Mont et al7 reported a ing, the authors found large areas of polyethylene bearings. The short-
high fracture rate in the first group of cystic degeneration of the head and term failure rate was high secondary
456 Journal of the American Academy of Orthopaedic Surgeons
Michael A. Mont, MD, et al
to aseptic component loosening, more wear than same-diameter Figure 3
which was caused by multiple fac- heads with smaller clearances.20
tors, including poor initial fixation, The advantages of metal-on-
technical errors in device implanta- metal bearings must be balanced
tion, and problems with implant de- against the possible adverse effects
sign and manufacturing. Design and of particulate metal debris. Several
manufacturing flaws produced high studies18,21-23 have shown increased
frictional torque that led to seizing levels of metallic ions in body fluids
and loosening. In the 1960s and and adjacent tissues after joint ar-
1970s, metal-on-metal articulations throplasties with metal-on-metal
had wide ranges in manufacturing bearings. Clarke et al18 noted in-
tolerance. With innovations in met- creased metal ions in two resurfac-
allurgy, however, metal-metal bear- ing designs, compared with a stan-
ings with tolerances <25 µm now dard metal-on-metal implant with a
can be manufactured. 28-mm head. Additionally, metal
Many surgeons believe that mod- ions may cause allergic hypersensi-
ern metal-on-metal devices can re- tivity.24 Despite occasional anecdot-
duce the incidence of long-term fail- al reports of possible tumor induc-
Anteroposterior radiograph
ure caused by aseptic loosening and tion by metal implants, whether
demonstrating a failed hip resurfacing
osteolysis. It is hoped that wear par- with metal-on-metal or metal-on- combined with a thin polyethylene liner.
ticle generation and the associated polyethylene bearings, no evidence The primary cause of failure is
osteolysis and implant loosening has been published to directly link polyethylene wear and osteolysis.
will be reduced; new metal-on-metal metal-on-metal bearing surfaces
bearing surfaces have low reported with adverse biologic effects. Al-
particulate wear rates.18 Recent ad- though elevated metal ions are may not necessarily be important for
vances in design have led to the in- found in patients and there is a the- excellent results. In a study of resur-
troduction of polar bearing implants, oretic possibility that metal ions facing in patients with osteonecro-
which have reduced surface asperity. may lead to metal hypersensitivity, sis, excellent results were reported
Designers have achieved superior the significance of these factors has for 26 of 27 hips at 2-year follow-
fluid film lubrication for the bearing yet to be determined. Several studies up.28 Longer follow-up is needed on
surfaces. The lubrication depends in report information regarding partic- these hips. Thus, it remains to be de-
part on the precision with which the ulate debris from metal-on-metal termined whether femoral head via-
implant bearing surfaces are manu- bearing couples.18,21,23 bility has an impact on resurfacing
factured. Surface asperities must In the early period of resurfacing survival.
have lower dimensions than the arthroplasty, osteonecrosis of the
thickness of the fluid film to achieve femoral head was proposed as a Recent Prostheses
fluid film lubrication. This, in turn, cause of failure.25,26 Campbell et al25 Metal-on-metal surface replace-
should minimize both frictional histologically examined 25 resur- ments have been used since the ear-
torque on the implants and the gen- faced femoral heads removed at revi- ly 1990s. Most devices feature
eration of wear particles. Some stud- sion and found only viable bone, cobalt-chrome components for ce-
ies have shown much lower num- with minimal evidence of femoral mentless fixation on the acetabular
bers of wear particles generated by head necrosis at 15 to 144 months side and cemented fixation on the
metal-on-metal bearings than by after surgery. Only 12% of the spec- femoral side (Figure 4).
metal-on-polyethylene bearings;17,19 imens had any osteonecrosis; these
however, this may not be true with patients had prior fractures and sur- Second-Generation
modern prostheses. Small clearance geries that may have damaged the Metal-on-Metal
between the femoral head and ace- head vasculature. The areas found Resurfacing
tabular component in metal-on- were small and did not cause the re- Unfortunately, there are few pub-
metal devices can be achieved with surfacing failure. Bell et al27 reported lished studies of resurfacing THA
large-diameter heads. This in turn similar findings, with only 1 case of done with modern designs (Table 1).
may enable greater fluid film lubri- osteonecrosis in 18 cases of failure of Daniel et al8 studied 446 hip resur-
cation and, subsequently, less wear the Wagner device (Sulzer Limited, facings in 384 patients using the Mc-
and less metal ion production. In a Winterthur, Switzerland) at mean of Minn Resurfacing Hip Arthroplasty
recent study, diametrical clearance 2 years postoperatively. (Corin Medical, Cirencester, United
of 300 µm produced considerably The viability of the femoral head Kingdom) and the Birmingham Hip
Volume 14, Number 8, August 2006 457
Hip Resurfacing Arthroplasty
Figure 4
Metal-on-metal resurfacing devices.
A, Birmingham Hip Resurfacing device
(Midland Medical Technologies,
Birmingham, United Kingdom).
B, Conserve Plus implant (Wright
Medical Technology, Arlington, TN).
Resurfacing (BHR) prosthesis (Mid- failure from metallosis and osteoly- 0.04 to 0.08, depending on the zone
land Medical Technologies, Birming- sis. analyzed). The authors concluded
ham, United Kingdom) implanted Three recent studies have exam- that the BHR component preserves
between March 1994 and April 2001, ined implant stability and proximal proximal femoral bone stock by
but excluding 1996. The McMinn femoral bone density after BHR im- transferring load to the proximal fe-
device was implanted in 43 hips plantation. Glyn-Jones et al36 recent- mur in a more physiologic manner
from 1994 to 1995, and the BHR was ly described a roentgenostereophoto- than do long-stem devices, thus pre-
used in 403 hips between July 1997 grammetric analysis (RSA) of the venting stress shielding.
and April 2001. Both devices consist- BHR component in 22 hips. RSA Watanabe et al4 conducted a finite
ed of a cemented femoral compo- was used to evaluate the hips at element analysis study of the BHR
nent and a hydroxyapatite-coated ac- 3-month intervals up to 24 months. implant and found stress shielding
etabular component. All patients At last follow-up (24 months), the in the anterosuperior region of the
were younger than age 55 years, and total migration of the head was 0.2 femoral neck beneath the prosthesis
mean follow-up was 3.3 years (range, mm, which was not statistically sig- as well as stress concentration
1.1 to 8.2 years). The authors report- nificant. The authors concluded that around the short stem in the inferi-
ed only one revision in a group of pa- the BHR femoral component is a sta- or cross-section of the femoral neck.
tients with high-level occupations ble device. The authors speculated that this
and recreational activities (1/446 Kishida et al5 analyzed proximal may lead to fracture and long-term
[0.02%]). Importantly, the authors femoral bone mineral density in 26 loosening. Yoo et al32 recently re-
excluded 186 patients operated on in hips, half of which had a BHR com- ported on 40 hips with osteonecrosis
1996 who had a different device that ponent (group A) and half, a proxi- managed with a BHR implant. At
was found to be defective. That de- mally coated cementless standard mean follow-up of 4 years, there
vice had two post-cast heat treat- THA (group B). Loss of bone miner- were no complications, osteolysis,
ments, which led to microstructural al density was less in group A (≤1% or component loosening.
changes in the metal, deterioration in any radiographic zone) than in Beaule et al16 studied 94 hips (83
of wear characteristics, and early group B (≤17% for certain zones; P = patients) resurfaced with the Con-
458 Journal of the American Academy of Orthopaedic Surgeons
Michael A. Mont, MD, et al
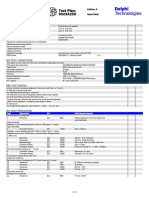
Table 1
Results of Studies Using Metal-on-Metal Total Hip Resurfacing
Follow-up Clinical Success
Study Prosthesis No. of Hips (mos) Rate (%)
McMinn et al29 Cementless, uncoated design 70 50.2 (range, 87
44-54)
Cementless, hydroxyapatite-coated design 6 40.2 (range, 100
38-42)
Cemented design 43 33.2 (range, 91
23-38)
Cemented femoral design and cementless, 116 8.3 (range, 100
hydroxyapatite-coated acetabular design 1-19)
Schmalzried et al30 Wagner prosthesis (Sulzer, Winterthur, 4 16 (range, 100
Switzerland) 10-25)
McMinn prosthesis (Corin Medical, 17 16 (range, 100 (progressive
Cirencester, United Kingdom) 10-25) cement bone
interface
radiolucencies
in 71%)
Wagner and Wagner prosthesis 35 20 (range, 86
Wagner31 6-54)
Amstutz et al19 McMinn prosthesis and Wagner prosthesis 50 (12-48) 74
Daniel et al8 McMinn prosthesis 43 40 (range, 81
13-98)
Birmingham Hip Resurfacing (BHR) 403 40 (range, 100
system (Smith and Nephew, Memphis, 13-98)
TN)
Yoo et al32 Birmingham Hip Resurfacing (BHR) 40 36.8 100
system
Beaule et al16 Conserve Plus (Wright Medical 94 36 (range, 97
Technology, Arlington, TN) 24-60)
Amstutz et al6 Conserve Plus 400 42 (range, 94
26-74)
Etienne et al28 Conserve Plus 30 24 (range, 97
12-48)
Treacy et al15 Birmingham Hip Resurfacing (BHR) 144 72 98
system
Beaule et al13 Conserve Plus 56 58.8 (range, 95
28-100)
Mont et al33 Conserve Plus 84 41 (range, 98
26-61)
Beaule et al34 McMinn prosthesis 42 104 (range, 79
86-120)
Schmalzried et al35 Conserve Plus 81 24 98
serve Plus metal-on-metal total re- ure, the authors calculated a surface (355 patients) implanted with the
surfacing device (Wright Medical, Ar- arthroplasty risk index (4.7 for 13 Conserve Plus device. Patient mean
lington, TN). They included only problem hips, 2.6 for remaining hips) age was 48 years (range, 15 to 77
patients who had a minimum 2-year to predict the risk of failure. Factors years). The overall rate of survival at
follow-up or who had undergone re- leading to increased risk included 4 years was 94.4%. Patients with a
vision. Mean age was 34 years (range, prior surgery, femoral cyst >1 cm, and high surface arthroplasty risk index
15 to 40 years). Based on their anal- valgus positioning of the stem. (>3) demonstrated a survival rate of
ysis of 3 hips that required revision Amstutz et al6 reported 2- to 89%, compared with 97% for those
and 10 hips that had impending fail- 6-year follow-up of the first 400 hips with a low risk index (≤3). Twelve
Volume 14, Number 8, August 2006 459
Hip Resurfacing Arthroplasty
Figure 5 achieved, but horizontal offset is es-
sentially unchanged by resurfacing.
In contrast, when necessary, both pa-
rameters can be increased reliably in
standard THAs. The authors con-
cluded that arthritic hips that are at
least 1 cm shorter than the con-
tralateral limb or that have low hor-
izontal femoral offset may be better
managed with a standard THA.
Etienne et al28 implanted 30
metal-on-metal Conserve Plus resur-
facing components in patients with
late-stage osteonecrosis. At a mean
follow-up of 2 years (range, 1 to 4
years), they reported only one fail-
ure, which was caused by a femoral
neck fracture.
Indications and
Contraindications
Advocates of hip resurfacing be-
lieve that the indications are similar
to those for any standard THA, with
Hip abduction moments. Resurfaced hips have close to normal (shaded) abduction certain provisos. Table 2 provides a
moments, which are greater than in patients with standard total hip replacement list of absolute and relative contrain-
(THR). Patients with osteoarthritis (OA) have the lowest abduction moments.
dications as well as instances in
LR = loading response, MOM = metal-on-metal
which to use these devices with cau-
tion. Patients who are considering
hips were revised to a standard THA significant difference in hip abductor resurfacing should be counseled that,
(3%). Of those 12 hips, 7 were re- and extensor moments between pa- compared with standard THA, less is
vised because of loosening, 3 be- tients with resurfacing and patients known about the long-term safety
cause of femoral neck fracture, and 1 with healthy hips. The hip abductor and efficacy of resurfacing devices
each because of recurrent sublux- moment in osteoarthritic and stan- and the outcome of revision surgery.
ation and infection. Most complica- dard THA groups was significantly Contraindications for resurfacing
tions occurred in the first 100 hips reduced (P < 0.05) compared with the include deficiency of femoral head or
operated on, indicating the learning normal group (Figure 5). Patients neck bone stock, and a small or
curve involved in proper resurfacing with resurfacing hip arthroplasty bone-deficient acetabulum. The hip
implantation. Revision was straight- demonstrated superior hip kinemat- with loss of femoral head bone stock
forward. Important risk factors for ics compared with standard hip re- after a fracture or other causes, such
femoral component failure included placements. However, the series was as rapidly progressive osteoarthri-
large femoral head cysts, patient neither prospective nor randomized, tis (“disappearing bone disease”),
height, and female sex. and although patients were retro- cannot be resurfaced. When large
Mont et al9 compared gait charac- spectively matched, the study may femoral neck or head cysts are en-
teristics of resurfacing patients with have been subject to selection bias. countered, resurfacing may be inap-
healthy hips, patients with osteoar- Silva et al10 studied the biome- propriate (Figure 6). The best candi-
thritic hips, and patients with stan- chanical results of resurfacing, com- dates for metal-on-metal resurfacing
dard THAs. Patients with resurfac- paring the joint reactive force of 50 are patients younger than age
ing walked faster (average, 126 m/s), resurfaced hips with that of 40 hips 60 years with good bone stock.
comparable with the walking speed managed with standard cementless Amstutz et al19 described three
in normal subjects. Patients with os- THA. The authors reported that the especially good indications for un-
teoarthritic hips and standard THAs biomechanical results of hip resur- dertaking resurfacing rather than
walked at significantly slower speeds facing were dependent on the preop- standard THA surgery: (1) patients
(96 and 99 m/s, respectively; P < erative anatomy of the proximal fe- with proximal femoral deformity,
0.001 for both groups). There was no mur. Limb lengthening can be which makes standard stemmed
460 Journal of the American Academy of Orthopaedic Surgeons
Michael A. Mont, MD, et al
prostheses difficult to place (Figure Table 2
7); (2) patients with a high risk of
sepsis because of prior infection or Contraindications to Metal-on-Metal Hip Resurfacing
immunosuppression; and (3) pa- Absolute contraindications
tients with a neuromuscular disor- Loss of femoral head (severe bone loss)
Large femoral neck cysts found at surgery
der. (A large-diameter ball reduces
Small or bone-deficient acetabulum
dislocation risk in patients with a Relative contraindications
neuromuscular disorder). Based on Poor bone stock (assessed via DEXA scans)
our experience, two other excellent Chronologic age >65 years
Body mass index >35
indications for resurfacing are (1) re-
Use with caution
tained hardware that would be diffi- Patient with rheumatoid arthritis
cult to remove for a standard stem Tall and thin patient
placement (Figure 8), and (2) patients Female patient
with conditions with a high risk for Patient with femoral head cyst >1 cm as demonstrated in preoperative
radiograph
failure using standard THAs (eg, Patient with osteonecrosis of the femoral head
sickle cell disease; alcoholism,
which has a high dislocation rate). DEXA = dual-energy x-ray absorptiometry
Surgical Techniques
Figure 6
Resurfacing can be performed with
standard approaches used in conven-
tional THA. No studies have com-
pared the two major approaches: an-
terior and posterior. We have used
both approaches. Anterior approach-
es have been used in an attempt to
preserve blood supply to the femoral
head, but most surgeons use posteri-
or approaches that retain the cap-
sule, with no adverse effects on the
blood supply. More dissection is usu-
ally involved in resurfacing THA be-
cause the femoral head has to be pre-
served and displaced to visualize the
acetabulum. Reaming of the acetab-
ulum is performed routinely, but
sufficient bone must be taken to al- Intraoperative photograph of a cyst, which precluded hip resurfacing. The patient
low placement of an appropriately received a conventional total hip replacement.
sized femoral component without
notching the femoral neck. When with various positioning devices almost always cemented in place.
too-small an acetabular component around the femoral neck to mimic Recently, techniques have been de-
is placed, it necessitates a smaller the native femoral head. The femoral veloped with new instrumentation
femoral component, which may pre- neck is of paramount importance; that enable the use of smaller inci-
clude using a component that com- the surgeon must avoid notching any sions.37 Resurfacing arthroplasty
pletely surrounds the femoral neck. part of it, especially the lateral cor- should be performed only by the sur-
Fortunately, most modern designs tex, to avoid a stress riser, which geon who has received training spe-
are made with thin components that could lead to femoral neck fracture. cifically in this technique.
do not require excessive reaming Most components have a small, thin,
away of acetabular bone. straight stem that enters the femoral
Future Directions
All modern acetabular compo- neck or extends slightly beyond into
nents are made for cementless press- the intertrochanteric area. The fem- In the future, use of ceramic-on-
fit insertion. On the femoral side, oral head is prepared with two ream- ceramic resurfacing may be possible.
components usually range in size ers to mimic the inner geometry of Such interfaces are presently pre-
from 36 to 54 mm; they are placed the femoral components, which are cluded because of the thickness of
Volume 14, Number 8, August 2006 461
Hip Resurfacing Arthroplasty
Figure 7 Figure 8
Postoperative anteroposterior (A) and lateral (B) radiographs of a patient with
posttraumatic extra-articular proximal femoral deformity secondary to trauma, who
was treated with resurfacing hip arthroplasty.
ceramic necessary, which would not tions, such as women, patients old-
be bone-sparing on the acetabular er than 60 years of age, patients with Postoperative anteroposterior
side. With newer materials, ceramic- poor bone stock, and patients with radiograph of a patient in whom an
intramedullary rod was placed to
on-polyethylene articulations may inflammatory arthritis. The risk of
correct a bowing deformity of the
be a possibility. Such devices previ- dislocation is much lower than for femur. The patient underwent hip
ously failed because of polyethylene standard THAs. The true incidence resurfacing rather than a conventional
wear. With the advent of newer, of osteonecrosis of the femoral head total hip replacement to avoid removal
highly cross-linked polyethylenes, under the component is low. Con- of the femoral intramedullary rod.
which have superior wear character- verting failed resurfacing to standard
istics, there may be a return to this THA is relatively straightforward.
material as a bearing surface. The resurfacing procedure has a
learning curve, with a higher rate of assistance with the preparation of
failure in the initial patients. Long- this manuscript.
Summary
term follow-up of metal-on-metal
Many of the technical problems that resurfacing implants is necessary to References
affected early resurfacing implants determine the appropriate use of
have been identified and resolved these devices. Surgical techniques Evidence-based Medicine: There are
with improved engineering and for implantation likely will evolve no level I or II randomized prospec-
manufacturing techniques. Recent as use becomes more widespread. tive studies. Reported are level III
studies have demonstrated excellent and IV case-control series.
short-term results with metal-on- Citation numbers printed in bold
Acknowledgments
metal resurfacing in patients young- type indicate references published
er than 60 years of age. Cementless The authors acknowledge Harlan within the past 5 years.
acetabular components are mated to Amstutz, the pioneer and an ever-
cemented femoral components be- present driving force for resurfacing 1. Amstutz HC, Graff-Radford A, Gruen
cause of the unsatisfactory results of hip arthroplasty for each of us per- TA, Clarke IC: THARIES surface re-
placements: A review of the first 100
cemented acetabular fixation. Al- sonally and for the entire field. We
cases. Clin Orthop Relat Res 1978;
though the loosening and fracture also thank Pat Fisher (Wright Medi- 134:87-101.
risk is relatively low, there are cer- cal Technology), for providing fig- 2. Howie DW, Campbell D, McGee M,
tain at-risk demographic popula- ures, and Colleen Kazmarek, for her Cornish BL: Wagner resurfacing hip
462 Journal of the American Academy of Orthopaedic Surgeons
Michael A. Mont, MD, et al
arthroplasty: The results of one hun- ing versus metal-on-metal hybrid re- heads after failed resurfacing arthro-
dred consecutive arthroplasties after surfacing. J Arthroplasty 2004;19(8 plasty of the hip. J Bone Joint Surg Br
eight to ten years. J Bone Joint Surg suppl 3):54-58. 2005;87:320-323.
Am 1990;72:708-714. 14. Shimmin AJ, Back D: Femoral neck 27. Bell RS, Schatzker J, Fornasier VL,
3. Amstutz HC, Grigoris P, Dorey FJ: fractures following Birmingham hip Goodman SB: A study of implant fail-
Evolution and future of surface re- resurfacing: A national review of 50 ure in the Wagner resurfacing arthro-
placement of the hip. J Orthop Sci cases. J Bone Joint Surg Br 2005;87: plasty. J Bone Joint Surg Am 1985;67:
1998;3:169-186. 463-464. 1165-1175.
4. Watanabe Y, Shiba N, Matsuo S, et al: 15. Treacy RB, McBryde CW, Pynsent PB: 28. Etienne G, Mont MA, Ragland PS:
Biomechanical study of the resurfac- Birmingham hip resurfacing arthro- The diagnosis and treatment of non-
ing hip arthroplasty: Finite element plasty: A minimum follow-up of five traumatic osteonecrosis of the femo-
analysis of the femoral component. years. J Bone Joint Surg Br 2005;87: ral head. Instr Course Lect 2004;53:
J Arthroplasty 2000;15:505-511. 167-170. 67-85.
5. Kishida Y, Sugano N, Nishii T, Miki 16. Beaule PE, Dorey FJ, LeDuff M, Gruen 29. McMinn D, Treacy R, Lin K, Pynsent
H, Yamaguchi K, Yoshikawa H: Pres- T, Amstutz HC: Risk factors affecting P: Metal on metal surface replace-
ervation of the bone mineral density outcome of metal-on-metal surface ment of the hip: Experience of the Mc-
of the femur after surface replacement arthroplasty of the hip. Clin Orthop Minn prosthesis. Clin Orthop Relat
of the hip. J Bone Joint Surg Br 2004; Relat Res 2004;418:87-93. Res 1996;(329 suppl):S89-98.
86:185-189. 17. Kabo JM, Gebhard JS, Loren G, Am- 30. Schmalzried TP, Fowble VA, Ure KJ,
6. Amstutz HC, Beaule PE, Dorey FJ, stutz HC: In vivo wear of polyethyl- Amstutz HC: Metal on metal surface
Le Duff MJ, Campbell PA, Gruen T: ene acetabular components. J Bone replacement of the hip: Techniques,
Metal-on-metal hybrid surface ar- Joint Surg Br 1993;75:254-258. fixation, and early results. Clin
throplasty: Two to six-year follow-up 18. Clarke MT, Lee PT, Arora A, Villar Orthop Relat Res 1996;(329 suppl):
study. J Bone Joint Surg Am 2004;86: RN: Levels of metal ions after small- S106-S114.
28-39. and large-diameter metal-on-metal 31. Wagner M, Wagner H: Preliminary re-
7. Mont MA, Ragland PS, Bezwada HP, hip arthroplasty. J Bone Joint Surg Br sults of uncemented metal on metal
Thomas CM, Etienne G: Abstract: 2003;85:913-917. stemmed and resurfacing hip replace-
The results of metal-on-metal resur- 19. Amstutz HC, Grigoris P, Dorey FJ: ment arthroplasty. Clin Orthop
facing hip arthroplasty: Learning Evolution and future of surface re- Relat Res 1996;(329 suppl):S78-S88.
curve stratification of results. 72nd placement of the hip. J Orthop Sci 32. Yoo MC, Cho YJ, Kim KI, Chun YS,
Annual Meeting Proceedings. Rose- 1998;3:169-186. Ha JH, Park JY: Resurfacing arthro-
mont, IL: American Academy of Or- 20. Dowson D, Hardaker C, Flett M, Isaac plasty in patients with osteonecrosis
thopaedic Surgeons, 2005, p 368. GH: A hip joint simulator study of of the femoral head. J Bone Joint Surg
8. Daniel J, Pynsent PB, McMinn DJ: the performance of metal-on-metal Br 2004;86:151.
Metal-on-metal resurfacing of the hip joints: II. Design. J Arthroplasty 33. Mont MA, Seyler TM, Delanois RE:
in patients under the age of 55 years 2004;19(8 suppl 3):124-130. Use of metal-on-metal total hip resur-
with osteoarthritis. J Bone Joint Surg 21. Jacobs JJ, Skipor AK, Doorn PF, et al: facing for osteonecrosis of the femoral
Br 2004;86:177-184. Cobalt and chromium concentrations head: An analysis of 42 hips compared
9. Mont MA, Seyler TM, Ragland PS, in patients with metal-on-metal total to osteoarthritis. J Bone Joint Surg
Starr R, Erhart J, Bhave A: Gait analy- hip replacements. Clin Orthop Relat Am, in press.
sis of patients with resurfacing hip ar- Res 1996;(329 suppl):S256-263. 34. Beaule PE, Le Duff M, Campbell P,
throplasty compared to hip osteoar- 22. Hallab NJ, Anderson S, Caicedo M, Dorey FJ, Park SH, Amstutz HC:
thritis and standard total hip Skipor A, Campbell P, Jacobs JJ: Metal-on-metal surface arthroplasty
arthroplasty. J Arthroplasty, in press. Immune responses correlate with with a cemented femoral component:
10. Silva M, Lee KH, Heisel C, Dela Rosa serum-metal in metal-on-metal A 7- to 10-year follow-up study.
MA, Schmalzried TP: The biome- hip arthroplasty. J Arthroplasty 2004; J Arthroplasty 2004;19(8 suppl 3):17-
chanical results of total hip resurfac- 19(8 suppl 3):88-93. 22.
ing arthroplasty. J Bone Joint Surg 23. MacDonald SJ, Brodner W, Jacobs JJ: A 35. Schmalzried TP, Silva M, de la Rosa
Am 2004;86:40-46. consensus paper on metal ions in MA, Choi E-S, Fowble VA: Opti-
11. Ragland PS, Mont MA: Total hip re- metal-on-metal hip arthroplasties. mizing patient selection and out-
placement revision after limited fem- J Arthroplasty 2004;19(8 suppl 3):12- comes with total hip resurfacing.
oral resurfacing: comparison to a 16. Clin Orthop Relat Res 2005;441:200-
matching group. Presented at the 24. Willert HG, Buchhorn G, Fayyazi A, 204.
72nd Annual Meeting of the Ameri- Lohmann C: Histopathological 36. Glyn-Jones S, Gill HS, McLardy-
can Academy of Orthopaedic Sur- changes around metal/metal joints in- Smith P, Murray DW: Roentgen ste-
geons, Washington, DC, February 23- dicate delayed type hypersensitivity: reophotogrammetric analysis of the
27, 2005. Preliminary results in 14 cases. Birmingham hip resurfacing arthro-
12. Seyler TM, Etienne G, Plate JF, Fisher Osteologie 2000;9:2. plasty: A two-year study. J Bone Joint
P, Mont MA: Use of large femoral 25. Campbell P, Mirra J, Amstutz HC: Surg Br 2004;86:172-176.
heads without liners in total hip ar- Viability of femoral heads treated 37. Mont MA, Ragland PS, Marker D: Re-
throplasty. Surg Technol Int, in press. with resurfacing arthroplasty. surfacing hip arthroplasty: Compari-
13. Beaule PE, Amstutz HC, Le Duff M, J Arthroplasty 2000;15:120-122. son of a minimally invasive versus
Dorey F: Surface arthroplasty for os- 26. Little CP, Ruiz AL, Harding IJ, et al: standard approach. Clin Orthop
teonecrosis of the hip: Hemiresurfac- Osteonecrosis in retrieved femoral Relat Res 2005;441:125-131.
Volume 14, Number 8, August 2006 463
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hitachi ZX85US Operator S ManualDocument313 pagesHitachi ZX85US Operator S Manualalesca1978100% (12)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Automatic Voltage Regulators: SpecificationsDocument4 pagesAutomatic Voltage Regulators: SpecificationsArman Haq100% (9)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Petrel Manual: Vshale CalculationDocument20 pagesPetrel Manual: Vshale CalculationEmira Zrelli100% (1)
- Ee4302 Ca1Document51 pagesEe4302 Ca1Norul Ashikin NorzainNo ratings yet
- Integrated Operations in The Oil and Gas Industry Sustainability and Capability Development PDFDocument458 pagesIntegrated Operations in The Oil and Gas Industry Sustainability and Capability Development PDFkglorstadNo ratings yet
- International RoamingDocument25 pagesInternational RoamingAbu Bakir Akhter75% (4)
- Intrusion Detection System Using Multivariate Control Chart Hotelling's T Based On PCADocument7 pagesIntrusion Detection System Using Multivariate Control Chart Hotelling's T Based On PCARumaisa KrubaNo ratings yet
- Noise Reduction in Images Using AutoencodersDocument7 pagesNoise Reduction in Images Using AutoencodersIJRASETPublicationsNo ratings yet
- 9323a251g PTDocument3 pages9323a251g PTClarice Alves de FreitasNo ratings yet
- WaymakerDocument23 pagesWaymakerJORDAN FREENo ratings yet
- Social Networking Software: A SWOT AnalysisDocument10 pagesSocial Networking Software: A SWOT AnalysisShivani SainiNo ratings yet
- A Tutorial On Jasperreports Ireport and JfreechartDocument21 pagesA Tutorial On Jasperreports Ireport and JfreechartDanijela Milicevic MalisicNo ratings yet
- Concrete & Shuttering Working-R1Document20 pagesConcrete & Shuttering Working-R1vivekNo ratings yet
- Exercícios SemanaisDocument11 pagesExercícios SemanaisElias Carvalho100% (2)
- Odell - Nikon1V1 J1 - Guide v1.064 Excerpt PDFDocument33 pagesOdell - Nikon1V1 J1 - Guide v1.064 Excerpt PDFmasreogNo ratings yet
- Liebherr Tower Cranes enDocument42 pagesLiebherr Tower Cranes enRaman Iyer100% (1)
- Ameyo Product BrochureDocument8 pagesAmeyo Product BrochureSudhanshu Gupta100% (1)
- Heavy Duty BrochureDocument16 pagesHeavy Duty BrochureАлексей ГордиенкоNo ratings yet
- (Kinetico) MachBackwashingFilterownersmanualDocument48 pages(Kinetico) MachBackwashingFilterownersmanualGreg ReynekeNo ratings yet
- Crodasinic LS LeafletDocument2 pagesCrodasinic LS LeafleticraoNo ratings yet
- In: 48 VDC - Out: 35 VDC / 2 A: Miro TR 24Vdc FK 5P Opto-Coupler ModuleDocument2 pagesIn: 48 VDC - Out: 35 VDC / 2 A: Miro TR 24Vdc FK 5P Opto-Coupler ModuleDannyNo ratings yet
- Faculty of Engineering and Applied ScienceDocument30 pagesFaculty of Engineering and Applied ScienceJaspreet SinghNo ratings yet
- Nokia VP8 Infringement Claim Chart For '211 PatentDocument37 pagesNokia VP8 Infringement Claim Chart For '211 PatentFlorian MuellerNo ratings yet
- Site Meeting 03Document4 pagesSite Meeting 03Fakrul AdliNo ratings yet
- Index Page and 2nd Page of EEDocument2 pagesIndex Page and 2nd Page of EEAmir KhanNo ratings yet
- Logic Level Triac: TO92 (Plastic)Document4 pagesLogic Level Triac: TO92 (Plastic)abel gaunaNo ratings yet
- Otc 31506 MsDocument10 pagesOtc 31506 MsAdriana UstarizNo ratings yet
- Deltec Voyage PDFDocument3 pagesDeltec Voyage PDFPaul RasmussenNo ratings yet
- Steam TableDocument1 pageSteam TableKrismawan Saptya YudhaNo ratings yet