Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
22 viewsLabor and Birth Process and NURSING MANAGEMENT (Chapter 13 and 14) False Labor Factors That Affect Labor
Labor and Birth Process and NURSING MANAGEMENT (Chapter 13 and 14) False Labor Factors That Affect Labor
Uploaded by
SHARLAIN GAIL V. MELECIOThis document discusses labor and delivery nursing management. It defines true labor versus false labor, and lists factors that affect labor including the five P's: passageway, passenger, powers, position, and psychologic response. The stages of labor are described. Nursing roles include initial maternal assessment, monitoring contraction pattern, and assessing fetal well-being through signs and symptoms. Key aspects of labor such as cervical changes, fetal positioning, and theories of what triggers the onset of labor are summarized.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You might also like
- Physiology of Normal Spontaneous DeliveryDocument2 pagesPhysiology of Normal Spontaneous DeliverySummer Rain100% (2)
- Harare - Essential Guide To Management of Common Obstetric and GynaecologicDocument98 pagesHarare - Essential Guide To Management of Common Obstetric and GynaecologicTapiwa Munikwa100% (5)
- Lecture 7 - Physiology of LaborDocument30 pagesLecture 7 - Physiology of LaborMelissa Aina Mohd Yusof100% (1)
- Nur - 100 Session 2 - SemillaDocument6 pagesNur - 100 Session 2 - SemillaVon R Semilla100% (1)
- Chapter 15 - Labor and Birth: Ob LectureDocument15 pagesChapter 15 - Labor and Birth: Ob LectureMARIA PEARLITA TANNo ratings yet
- Problem With The PassageDocument3 pagesProblem With The PassageLuiciaNo ratings yet
- MD901F Cataloge PDFDocument2 pagesMD901F Cataloge PDFPT Anugerah Mitra MandiriNo ratings yet
- 7-Onset & Physiology of LaborDocument15 pages7-Onset & Physiology of LaborNlsNo ratings yet
- Intrapartum 1: Intrapartum Period Intrapartal CareDocument10 pagesIntrapartum 1: Intrapartum Period Intrapartal CareJane MartinNo ratings yet
- Ncma217 Week 7Document5 pagesNcma217 Week 7Polly ArcheronNo ratings yet
- Overview: Intrapartum Care:: Oxytocin TheoryDocument5 pagesOverview: Intrapartum Care:: Oxytocin TheoryZach BuenavistaNo ratings yet
- MCN MidtermsDocument39 pagesMCN MidtermsJinnijinniNo ratings yet
- NCM 107 - SL - Mat - 1Document100 pagesNCM 107 - SL - Mat - 1marilexdomagsangNo ratings yet
- Intrapartal PeriodDocument6 pagesIntrapartal PeriodKelsey MacaraigNo ratings yet
- LaborDocument32 pagesLaborJustine Vens G. AgustinNo ratings yet
- Ob Lec - Theories of LaborDocument10 pagesOb Lec - Theories of Labortmjrsvz84mNo ratings yet
- 2 August 28Document20 pages2 August 28Emily ChiaravallotiNo ratings yet
- OB1 3.1 Normal Labor and Delivery IDocument6 pagesOB1 3.1 Normal Labor and Delivery IManjulaNo ratings yet
- Intrartum/Intrapartal Period: Phenomena and Process of Labor and Delivery I. Onset of LaborDocument14 pagesIntrartum/Intrapartal Period: Phenomena and Process of Labor and Delivery I. Onset of Laborclaireaongchua1275No ratings yet
- Normal Labor: Ms. Mayuri Patel Sandra Shroff Rofel College of Nursing, VapiDocument48 pagesNormal Labor: Ms. Mayuri Patel Sandra Shroff Rofel College of Nursing, Vapivimmy47100% (1)
- Physiology of Parturition PDFDocument17 pagesPhysiology of Parturition PDFNestley TiongsonNo ratings yet
- Hands Out 3 LaborDocument29 pagesHands Out 3 LaborErin SaavedraNo ratings yet
- Finals Com ElearningDocument35 pagesFinals Com ElearningGladys JhayeNo ratings yet
- (ObstetricsA) Prenatal Care - Dr. San Jose (Lea Pacis)Document12 pages(ObstetricsA) Prenatal Care - Dr. San Jose (Lea Pacis)Karen EstavilloNo ratings yet
- Phy Ist Stag LBRDocument9 pagesPhy Ist Stag LBRAparna KinginiNo ratings yet
- NCM 109 Problems With Power DraftDocument3 pagesNCM 109 Problems With Power DraftJP Porras AliNo ratings yet
- 3F Intranatal NotesDocument5 pages3F Intranatal NotesAlyssa Claire TumulakNo ratings yet
- Normal Labor: Obstetrics and GynecologyDocument3 pagesNormal Labor: Obstetrics and GynecologyLuis PadillaNo ratings yet
- Problem With The PowersDocument9 pagesProblem With The PowersNicole Claire LegaspiNo ratings yet
- ABC Care PentingDocument4 pagesABC Care PentingDina Ayu SavitriNo ratings yet
- n3633 MM Module 1 Unit 1Document71 pagesn3633 MM Module 1 Unit 1jonscastro450No ratings yet
- Intrapartum Complications: Kristen AzusanoDocument3 pagesIntrapartum Complications: Kristen AzusanokirbsNo ratings yet
- MCHN FinalsDocument26 pagesMCHN FinalsMahdiyah AgasNo ratings yet
- Onset of LaborDocument4 pagesOnset of LaborK louiseNo ratings yet
- Maternal Reviewer MidtermmDocument5 pagesMaternal Reviewer Midtermmriveraapriljan22No ratings yet
- What Is LaborDocument8 pagesWhat Is LaborEdsylaine BumatayNo ratings yet
- Faal Partus: Naifah Luthfiyah Putri 15-009Document58 pagesFaal Partus: Naifah Luthfiyah Putri 15-009NaifahLuthfiyahPutriNo ratings yet
- Maternal & Child Health Nursing Flashcards QuizletDocument1 pageMaternal & Child Health Nursing Flashcards QuizletJosh PagnamitanNo ratings yet
- Intrapartum-Unit ExamDocument2 pagesIntrapartum-Unit ExamChris AnnNo ratings yet
- OB2 - Problems With The PowerDocument10 pagesOB2 - Problems With The PowerYanaNo ratings yet
- Labor and DeliveryDocument7 pagesLabor and DeliveryMikaella CondeNo ratings yet
- ANNOTATIONDocument2 pagesANNOTATIONVaniegrace Angel BalagonNo ratings yet
- Client Initials: Medical Diagnosis: Cephalopelvic Disproportion Eu DEFINITION: The RelationshipDocument2 pagesClient Initials: Medical Diagnosis: Cephalopelvic Disproportion Eu DEFINITION: The RelationshipLyssa Monique67% (3)
- 1 Labor and Delivery ProcessDocument13 pages1 Labor and Delivery ProcessBardiaga JmayNo ratings yet
- COMPONENTS OF LABOR - 5PsDocument5 pagesCOMPONENTS OF LABOR - 5PslumpiaNo ratings yet
- LESSON-PLAN-ON-PHYSIOLogical Changes During PregnancyDocument22 pagesLESSON-PLAN-ON-PHYSIOLogical Changes During PregnancyV.srivaniNo ratings yet
- Puerperium (Trans)Document7 pagesPuerperium (Trans)Charlie65129No ratings yet
- MALPRESENTATIONDocument13 pagesMALPRESENTATIONLady Jane CaguladaNo ratings yet
- Normal Labor and DeliveryDocument142 pagesNormal Labor and DeliveryRosalie RoselloNo ratings yet
- Abnormal Labor and Infertility 2016 PDFDocument12 pagesAbnormal Labor and Infertility 2016 PDFLarissa TacalanNo ratings yet
- Abnormal Labor + InfertilityDocument12 pagesAbnormal Labor + InfertilityKristine VanzuelaNo ratings yet
- Normal LaborDocument42 pagesNormal Laborhacker ammerNo ratings yet
- Definition: Related Diagnostic TestsDocument8 pagesDefinition: Related Diagnostic TestsQuinn Xylon VillanuevaNo ratings yet
- 10.theories of LaborDocument18 pages10.theories of LaborJulia Ramos100% (1)
- Holistic Pregnancy Manual: Maternal Health Manuals, #1From EverandHolistic Pregnancy Manual: Maternal Health Manuals, #1No ratings yet
- It Takes Two... And a Uterus: The Ultimate Guide to Understanding and Enhancing Your FertilityFrom EverandIt Takes Two... And a Uterus: The Ultimate Guide to Understanding and Enhancing Your FertilityNo ratings yet
- Teen Girl Guide to Puberty: Understanding Hormonal Changes, Body care and Personal HygieneFrom EverandTeen Girl Guide to Puberty: Understanding Hormonal Changes, Body care and Personal HygieneNo ratings yet
- How to Boost Your Fertility and Get Pregnant FastFrom EverandHow to Boost Your Fertility and Get Pregnant FastRating: 5 out of 5 stars5/5 (1)
- Government College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-IDocument6 pagesGovernment College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-Ipriyanka100% (1)
- OB Drug Study - OxytocinDocument3 pagesOB Drug Study - OxytocinJustin AncogNo ratings yet
- Fetal Distress: Philip J. SteerDocument7 pagesFetal Distress: Philip J. Steeryenni anggrainiNo ratings yet
- Partograph NextDocument50 pagesPartograph NextPrag GK Subedi0% (1)
- Fetal Assessment DRDocument1 pageFetal Assessment DRMicah Lou CalambaNo ratings yet
- Conduct of Normal Labor and DeliveryDocument141 pagesConduct of Normal Labor and DeliveryRea Dominique CabanillaNo ratings yet
- Carla Hernandez 100Document4 pagesCarla Hernandez 100JhunnieEy ReyesNo ratings yet
- Post-Term Labor - NCPDocument7 pagesPost-Term Labor - NCPCameron De GuzmanNo ratings yet
- Introduction of Labour MonitoringDocument29 pagesIntroduction of Labour MonitoringMishti MokarramaNo ratings yet
- Apfs 2012 MidDocument79 pagesApfs 2012 Middaniel meresaNo ratings yet
- OB I For 2nd YearDocument122 pagesOB I For 2nd YeardiribaNo ratings yet
- Labor and DeliveryDocument14 pagesLabor and Deliverydexter100% (15)
- Shoulder DystociaDocument20 pagesShoulder DystociaDanielle Francis Hirang0% (1)
- Osce - Non Stress Test Remarks YES NODocument3 pagesOsce - Non Stress Test Remarks YES NOKALAI AKSHAYANo ratings yet
- Nursing Care of The Family During Labor and BirthDocument16 pagesNursing Care of The Family During Labor and BirthGladys YaresNo ratings yet
- ფიზიოლოგიური მშობიარობის მართვაDocument30 pagesფიზიოლოგიური მშობიარობის მართვაAchi BeridzeNo ratings yet
- Government College of Nursing Jodhpur (Raj.)Document5 pagesGovernment College of Nursing Jodhpur (Raj.)priyanka100% (1)
- Mengukur DJJDocument6 pagesMengukur DJJYuni PurwatiNo ratings yet
- Radha Antenatal Fetal Well Being1Document32 pagesRadha Antenatal Fetal Well Being1Shaells JoshiNo ratings yet
- Nlex - MCNDocument19 pagesNlex - MCNAileen AlphaNo ratings yet
- Obg Unit - 4Document55 pagesObg Unit - 4Preeti ChouhanNo ratings yet
- Chapter 9 (Margot-Desevo)Document11 pagesChapter 9 (Margot-Desevo)Jesse ParkNo ratings yet
- Obs-UM - Paper - 1Document16 pagesObs-UM - Paper - 1Muhammad Abbas AliNo ratings yet
- Antepartum Fetal Surveillance ACOG Bulletin 2014-1Document11 pagesAntepartum Fetal Surveillance ACOG Bulletin 2014-1William Rodriguez CoronadoNo ratings yet
- Sonicaid Team CTG - Operators Manual PDFDocument113 pagesSonicaid Team CTG - Operators Manual PDFDaniel Galindo100% (1)
- MCHN Finals 1st-QuizDocument20 pagesMCHN Finals 1st-QuizhknNo ratings yet
- Contraction Stress Test: The Underline Physiological and Technological Basis For The CST Are As FollowsDocument3 pagesContraction Stress Test: The Underline Physiological and Technological Basis For The CST Are As FollowsSagar HanamasagarNo ratings yet
Labor and Birth Process and NURSING MANAGEMENT (Chapter 13 and 14) False Labor Factors That Affect Labor
Labor and Birth Process and NURSING MANAGEMENT (Chapter 13 and 14) False Labor Factors That Affect Labor
Uploaded by
SHARLAIN GAIL V. MELECIO0 ratings0% found this document useful (0 votes)
22 views7 pagesThis document discusses labor and delivery nursing management. It defines true labor versus false labor, and lists factors that affect labor including the five P's: passageway, passenger, powers, position, and psychologic response. The stages of labor are described. Nursing roles include initial maternal assessment, monitoring contraction pattern, and assessing fetal well-being through signs and symptoms. Key aspects of labor such as cervical changes, fetal positioning, and theories of what triggers the onset of labor are summarized.
Original Description:
Original Title
ii
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses labor and delivery nursing management. It defines true labor versus false labor, and lists factors that affect labor including the five P's: passageway, passenger, powers, position, and psychologic response. The stages of labor are described. Nursing roles include initial maternal assessment, monitoring contraction pattern, and assessing fetal well-being through signs and symptoms. Key aspects of labor such as cervical changes, fetal positioning, and theories of what triggers the onset of labor are summarized.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
22 views7 pagesLabor and Birth Process and NURSING MANAGEMENT (Chapter 13 and 14) False Labor Factors That Affect Labor
Labor and Birth Process and NURSING MANAGEMENT (Chapter 13 and 14) False Labor Factors That Affect Labor
Uploaded by
SHARLAIN GAIL V. MELECIOThis document discusses labor and delivery nursing management. It defines true labor versus false labor, and lists factors that affect labor including the five P's: passageway, passenger, powers, position, and psychologic response. The stages of labor are described. Nursing roles include initial maternal assessment, monitoring contraction pattern, and assessing fetal well-being through signs and symptoms. Key aspects of labor such as cervical changes, fetal positioning, and theories of what triggers the onset of labor are summarized.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 7
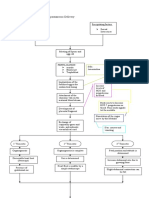
LABOR AND BIRTH PROCESS AND move. same.
NURSING MANAGEMENT (chapter 13
and 14)
False Labor Factors That Affect Labor
Irregular contractions The Five P’s:
No regular pattern Passageway (birth canal)
Discomfort in lower abdomen and Passenger (fetus and placenta)
groin Powers (contractions)
Show is not present Position of the mother
Does not cause cervical change Psychologic response
Activity does not increases Labor Definition
contractions Coordinated sequence of
Sedation will stop or decrease involuntary uterine contractions
contractions Contractions 3 minutes apart or less
lasting 60 seconds or longer
True Labor Resulting in effacement and
Regular contractions dilatation of the cervix and delivery of
Contractions Progresses to a pattern the fetus and placenta.
Discomfort begins in back and
radiates to the abdomen Possible Causes of Labor Maternal
Activity increases contraction Uterine muscle stretching
frequency Pressure on the cervix
Sedation does not diminish Oxytocin
contraction pattern Placental aging
Causes cervical changes Estrogen/Progesterone ratio change
Show usually present Fetal cortisol concentration
Prostaglandins
FACTOR TRUE LABOR FALSE LABOR
THEORIES:
Contractions Produce Do not OXYTOCIN STIMULATION: term
progressive produce uterus sensitive to oxytocin leading to
dilation and progressive pressure exerted on cervix by fetus.
effacement of and PROGESTERONE WITHDRAWAL:
the cervix. effacement. decreases progesterone by fetus &
Occur Irregular and and increases prostaglandins in
regularly and do not chorioamnion resulting to increase
increase in increase in uterine contractions.
frequency, frequency, ESTROGENSTIMULATIONL:
duration, and duration, and decreases progesterone allows
intensity. intensity. estrogen to increase contractile
response of uterus.
Show Is present Not present, FETAL CORTISOL: changes
may have biochemistry of fetal membrane and
brownish decreases progesterone & increases
discharge prostaglandin in placenta.
that may be DISTENTION: uterine muscles
from vaginal stretch causing increase of
exam if prostaglandin.
within the AMNIOTIC MEMBRANES (sac) makes
last 48 hrs. arachidonic acid to prostaglandin -^
uterine contractility.
Cervix Becomes Usually
effaced and uneffaced
Signs Preceding Labor
dilates and closed.
Lightening
progressively.
Increase vaginal discharge
Fetal No significant May intensify Cervix softening
movement change, even for a short Rupture of membranes
though fetus period or may Energy burst
continues to remain the Braxton-Hicks contractions
Weight loss
Bloody show Passageway
Presenting Part Pelvic structure and shape
Cephalic Soft tissues
Shoulder Cervix
Breech Pelvic floor
o Frank- hips are flexed and Vagina
legs extended Passenger
o Full or complete- hips and Size of the fetal head
knees are flexed and the feet are Presenting part
not below the level of the feral Fetal lie
buttocks. Fetal attitude
o Footling or incomplete- one Fetal position
or both feet are presenting as
the lowest part of the fetus. Fetal Skull
Fetal Lie Largest and least compressible
Fetal lie is the relationship of the structure
spine of the fetus to the spine of the Sutures: allow for overlapping and
mother changes in shape (molding); help
Longitudinal identify position of fetal head
Transverse Fontanels: intersections of sutures;
Fetal Attitude help in identifying position of fetal
Fetal attitude is flexion or extension head and in molding
of the joints and the relationship of
fetal parts to one another
Fetal Position
relationship of the presenting part
of the fetus to a designated point of
the maternal pelvic structure
RIGHT OCCIPUT POSTERIOR (ROP)
o Baby's back favors mothers
right and the back of baby's head
is towards mothers posterior. In
ROP, baby is head down and the
back is to the right side. This
position can be deceptively
reassuring. ROP is the most Four Stages of Labor
common of the four posterior First Stage starts with Onset of labor
positions. to complete dilation
Powers o Latent phase Dilatation 0 to 3
Contractions primary force cm
Frequency Effacement 0 to 40%
Duration o Active phase Dilatation 4 to 7
Intensity cm
Pushing secondary force Effacement 40 to 80%
o Transition Dilatation 8–10 cm o Sense of mastery, self-
Effacement 100% confidence
Second stage complete dilation to o Trust in staff caring for her
birth o Positive reaction to the
Third stage birth to placental pregnancy
separation and expulsion o Personal control over
Fourth stage four hours following breathing
delivery of the place o Preparation for the childbirth
experience
Factors That Affect Labor
5 Additional P’s
o Philosophy
o Partner
o Patience
o Pain management
Cardinal movements of Labor
Engagement
Descent
Flexion
Internal rotation
Initial Maternal Assessment Extension
Presenting complaint External rotation (restitution)
EDC Expulsion (birth)
Gravida/Para
o GRAVIDA- number of Nurses Role
pregnancies During labor and delivery fetal
o PARA- number of births after assessment includes determining fetal
20 weeks well-being and interpreting signs and
Contraction Pattern symptoms of possible compromise
Membrane status Nurse needs to be knowledgeable of
Presence of fetal movement the different FHR categories and the
Complications appropriate interventions that may be
Five digit system required
o G- total number of Monitoring Techniques
pregnancies Electronic fetal monitoring
o T- full term pregnancies (37- External monitoring
40 weeks) o FHR—ultrasound transducer
o P- preterm deliveries (20-36) o UCs—Toco transducer
o A- abortions and Internal monitoring (invasive)
miscarriages (before 20 weeks) o Spiral electrode (FSE)
o L-- living children o Intrauterine pressure
Maternal Position catheter (IUPC)
Affects woman’s anatomic and FHR Categories
physiologic adaptations to labor Category I normal
Frequent changes in position Category II indeterminate
o Relieve fatigue Category III predictive of abnormal
o Increase comfort fetus acid base status
o Improve circulation
o Facilitates decent and Determining FHR Patterns
rotation Fetal assessment
o Baseline FHR
Psychological Response o Variability
Factors Influencing a Positive Birth o Accelerations
Experience o Periodic changes
o Clear information on (decelerations)
procedures o Early (head compression)
o Support, not being alone
o Late (placental insufficiency) Fetal heart rate changes due to
o Variable (cord compression) contractions
Baseline Fetal Heart Rate Fetal circulation & respiratory
Baseline Rate is the average FHR changes preparing for birth
that occurs during a 10-minute Fetal heart rate baseline and
segment excluding periodic or variability
episodic rate changes Fetal heart rate response to
Normal 110-160 contractions
Bradycardia <110 o Prolonged Deceleration
Tachycardia >160 Abrupt decrease in FHR of at
Fetal Heart Rate Variability least 15 bpm lasting longer
Irregular Fluctuations in FHR than 2 minutes, but less
baseline measured as amplitude of than 10 minutes.
the peak to trough in bpm FHR usually drops to less
Absent fluctuation undetectable than 90 bpm
Minimal <5 bpm Fetal Heart Rate
Moderate (normal) 6-25 bpm V Variable
Marked >25bpm E Early
A Acceleration
Fetal Assessment L Late
FHR provides information about the C Cord
fetal oxygen status. H Head Compression
Locations for auscultating O Oxygenated fetus
Doppler Nursing Procedure 12.1 pg. P Placental problems
355
Continuous FHR via ultrasound Fetal Assessment Methods
transducer Umbilical Cord Blood Analysis
Fetal movement Fetal Scalp Stimulation
Pain Management
Contraction Assessment Nonpharmacologic
Frequency o Simple, safe, and inexpensive
Duration o Provide sense of control over
Strength/Intensity childbirth
Resting tone o Natural child birth requires
practice for best results
Pelvic Exam o Try variety of methods and
Effacement seek alternatives, including
Dilation pharmacologic methods if
Presenting part needed
Station o Imagery and visualization
Status of membranes o Position Changes Table 14.2
pg.437
General Systems Assessment o Music
Vital signs o Touch and massage
General physical assessment o Breathing techniques
Leopold’s maneuvers Procedure o Effleurage and counter
14.1 pg. 424 pressure
Review prenatal record for lab o Water therapy
results and history (hydrotherapy)
Physiologic Adaptation to Labor Pharmacologic
Maternal Adaptation o Systemic Analgesia
Cardiovascular changes Use of one or more
Respiratory changes drugs administered orally,
Musculoskeletal changes IM, or IV. These meds are
Gastrointestinal changes distributed via the
Fetal adaptation to labor circulatory system.
Pain relief can occur until the contraction has
within a few min. and last ended
up to several hrs. Caused by
Side effect can be uteroplacental insufficiency
respiratory depression in Fetus is in distress
the mother as well as the o Variable Decelerations
newborn after birth Abrupt decrease in
Opioids FHR below the baseline.
Ataractics/Antiemetic The decrease is at least 15
s bpm, lasting between 15
Benzodiazepines sec and under 2 minutes.
They can vary with
contractions.
Fetal Heart Rate Patterns Shaped like a “V” or a
Changes in fetal heart rate “W”
Periodic occur with Contractions Associated with cord
Episodic (non-periodic) not compression
associated with contractions Gown, gloves, and protective
Accelerations equipment for personnel
Decelerations Cleansing of the perineum
Accelerations Deliver the newborn
Positive sign of fetal wellbeing
Abrupt increase in FHR above the Second Stage of Labor
base line lasting <30 sec from onset to Assessment of contractions and FHR
peak Fetal descent
Term 15 bpm above baseline & Psychological considerations
duration >15 sec. but <2min Maternal positioning
Prior to 32 weeks 10 by 10 Coaching maternal breathing and
Prolonged 2 min. to <10min pushing efforts
Decelerations Perineal
Early decelerations o Lacerations (Depth)
Late decelerations * 1st degree
Variable decelerations * 2nd degree
Prolonged decelerations * 3rd degree
o Early Decelerations * 4th degree
Gradual decrease in Episiotomy
FHR, The nadir of the early o Midline
deceleration occurs with o mediolateral
the peak of a contraction.
A late deceleration is Third Stage of Labor
defined as a waveform Delivery of the placenta
with a gradual decrease Assess for perineal trauma
and return to baseline with Repair of episiotomy/Perineal
time from onset of the lacerations
deceleration to the lowest Newborn care
point of the deceleration Emotional support /Foster bonding
(nadir) >30 seconds
Head Placental separation and expulsion
compression/vagal Firmly contracting fundus
response Change in uterus
No treatment Sudden gush of dark blood from
required/benign pattern introitus
o Late Decelerations Apparent lengthening of umbilical
Gradual decrease in cord
FHR of the deceleration Vaginal fullness
occurring after the peak of
the contraction. The FHR Newborn care
does not return to baseline Time of birth noted
Drying, stimulation, suctioning of Preparation for Delivery
the newborn Prepare instrument table
Respiratory effort, heart rate, color, Adequate lighting
tone noted Oxygen and suction equipment
One- and five-minute Apgar scores Radiant warmer, blankets,
Cord blood obtained identification for newborn
Identification Pitocin
Positioning of mother for birth
Regional Analgesia/Anesthesia
Pudendal never block
Epidural (Vaginal Del or C/S) Fourth Stage of Labor
Spinal (C/S)
General (C/S) Maternal Assessment
Uterus
Lochia
Perineum
Bladder
Epidural Analgesia Vital signs
Combination of local anesthetic Pain
(lidocaine) & an opioid (morphine or Newborn-family attachment
fentanyl) Breastfeeding initiated
Injected into the epidural space
Medication can be balanced to
provide pain relive and the ability to
ambulate
General Anesthesia
Reserved for emergency cesarean
births when there is not enough time
to do a spinal or epidural for
anesthesia
Combination of IV injection and
inhalation agents
Epidurals/Spinals/General Anesthesia
Anesthesia interview
Consent form
Labs (platelets less than 100,000 can
place an epidural/spinal)
Nursing Responsibilities During 1st Stage of
Labor
Vital signs
Hydration and nutrition
Elimination
Assessment of contractions and FHR
Labor Support
Comfort measures/Pain
management
Education
Heart Rate Absent < 100 bpm > 100 bpm
Respiratory Apneic Slow, irregular, shallow Regular 30-60
effort breaths/min
Strong, good cry
Muscle Tone Limp, Flaccid Some flexion, limited Tight flexion, good
resistance to extension resistance to extension
with quick response to
flexed position
Reflex No Response Sneeze, cough, or
irritability Grimace or frown when vigorous cry
irritated
Skin color Cyanotic or Appropriate body color; blue Completely pink
Pale extremities
You might also like
- Physiology of Normal Spontaneous DeliveryDocument2 pagesPhysiology of Normal Spontaneous DeliverySummer Rain100% (2)
- Harare - Essential Guide To Management of Common Obstetric and GynaecologicDocument98 pagesHarare - Essential Guide To Management of Common Obstetric and GynaecologicTapiwa Munikwa100% (5)
- Lecture 7 - Physiology of LaborDocument30 pagesLecture 7 - Physiology of LaborMelissa Aina Mohd Yusof100% (1)
- Nur - 100 Session 2 - SemillaDocument6 pagesNur - 100 Session 2 - SemillaVon R Semilla100% (1)
- Chapter 15 - Labor and Birth: Ob LectureDocument15 pagesChapter 15 - Labor and Birth: Ob LectureMARIA PEARLITA TANNo ratings yet
- Problem With The PassageDocument3 pagesProblem With The PassageLuiciaNo ratings yet
- MD901F Cataloge PDFDocument2 pagesMD901F Cataloge PDFPT Anugerah Mitra MandiriNo ratings yet
- 7-Onset & Physiology of LaborDocument15 pages7-Onset & Physiology of LaborNlsNo ratings yet
- Intrapartum 1: Intrapartum Period Intrapartal CareDocument10 pagesIntrapartum 1: Intrapartum Period Intrapartal CareJane MartinNo ratings yet
- Ncma217 Week 7Document5 pagesNcma217 Week 7Polly ArcheronNo ratings yet
- Overview: Intrapartum Care:: Oxytocin TheoryDocument5 pagesOverview: Intrapartum Care:: Oxytocin TheoryZach BuenavistaNo ratings yet
- MCN MidtermsDocument39 pagesMCN MidtermsJinnijinniNo ratings yet
- NCM 107 - SL - Mat - 1Document100 pagesNCM 107 - SL - Mat - 1marilexdomagsangNo ratings yet
- Intrapartal PeriodDocument6 pagesIntrapartal PeriodKelsey MacaraigNo ratings yet
- LaborDocument32 pagesLaborJustine Vens G. AgustinNo ratings yet
- Ob Lec - Theories of LaborDocument10 pagesOb Lec - Theories of Labortmjrsvz84mNo ratings yet
- 2 August 28Document20 pages2 August 28Emily ChiaravallotiNo ratings yet
- OB1 3.1 Normal Labor and Delivery IDocument6 pagesOB1 3.1 Normal Labor and Delivery IManjulaNo ratings yet
- Intrartum/Intrapartal Period: Phenomena and Process of Labor and Delivery I. Onset of LaborDocument14 pagesIntrartum/Intrapartal Period: Phenomena and Process of Labor and Delivery I. Onset of Laborclaireaongchua1275No ratings yet
- Normal Labor: Ms. Mayuri Patel Sandra Shroff Rofel College of Nursing, VapiDocument48 pagesNormal Labor: Ms. Mayuri Patel Sandra Shroff Rofel College of Nursing, Vapivimmy47100% (1)
- Physiology of Parturition PDFDocument17 pagesPhysiology of Parturition PDFNestley TiongsonNo ratings yet
- Hands Out 3 LaborDocument29 pagesHands Out 3 LaborErin SaavedraNo ratings yet
- Finals Com ElearningDocument35 pagesFinals Com ElearningGladys JhayeNo ratings yet
- (ObstetricsA) Prenatal Care - Dr. San Jose (Lea Pacis)Document12 pages(ObstetricsA) Prenatal Care - Dr. San Jose (Lea Pacis)Karen EstavilloNo ratings yet
- Phy Ist Stag LBRDocument9 pagesPhy Ist Stag LBRAparna KinginiNo ratings yet
- NCM 109 Problems With Power DraftDocument3 pagesNCM 109 Problems With Power DraftJP Porras AliNo ratings yet
- 3F Intranatal NotesDocument5 pages3F Intranatal NotesAlyssa Claire TumulakNo ratings yet
- Normal Labor: Obstetrics and GynecologyDocument3 pagesNormal Labor: Obstetrics and GynecologyLuis PadillaNo ratings yet
- Problem With The PowersDocument9 pagesProblem With The PowersNicole Claire LegaspiNo ratings yet
- ABC Care PentingDocument4 pagesABC Care PentingDina Ayu SavitriNo ratings yet
- n3633 MM Module 1 Unit 1Document71 pagesn3633 MM Module 1 Unit 1jonscastro450No ratings yet
- Intrapartum Complications: Kristen AzusanoDocument3 pagesIntrapartum Complications: Kristen AzusanokirbsNo ratings yet
- MCHN FinalsDocument26 pagesMCHN FinalsMahdiyah AgasNo ratings yet
- Onset of LaborDocument4 pagesOnset of LaborK louiseNo ratings yet
- Maternal Reviewer MidtermmDocument5 pagesMaternal Reviewer Midtermmriveraapriljan22No ratings yet
- What Is LaborDocument8 pagesWhat Is LaborEdsylaine BumatayNo ratings yet
- Faal Partus: Naifah Luthfiyah Putri 15-009Document58 pagesFaal Partus: Naifah Luthfiyah Putri 15-009NaifahLuthfiyahPutriNo ratings yet
- Maternal & Child Health Nursing Flashcards QuizletDocument1 pageMaternal & Child Health Nursing Flashcards QuizletJosh PagnamitanNo ratings yet
- Intrapartum-Unit ExamDocument2 pagesIntrapartum-Unit ExamChris AnnNo ratings yet
- OB2 - Problems With The PowerDocument10 pagesOB2 - Problems With The PowerYanaNo ratings yet
- Labor and DeliveryDocument7 pagesLabor and DeliveryMikaella CondeNo ratings yet
- ANNOTATIONDocument2 pagesANNOTATIONVaniegrace Angel BalagonNo ratings yet
- Client Initials: Medical Diagnosis: Cephalopelvic Disproportion Eu DEFINITION: The RelationshipDocument2 pagesClient Initials: Medical Diagnosis: Cephalopelvic Disproportion Eu DEFINITION: The RelationshipLyssa Monique67% (3)
- 1 Labor and Delivery ProcessDocument13 pages1 Labor and Delivery ProcessBardiaga JmayNo ratings yet
- COMPONENTS OF LABOR - 5PsDocument5 pagesCOMPONENTS OF LABOR - 5PslumpiaNo ratings yet
- LESSON-PLAN-ON-PHYSIOLogical Changes During PregnancyDocument22 pagesLESSON-PLAN-ON-PHYSIOLogical Changes During PregnancyV.srivaniNo ratings yet
- Puerperium (Trans)Document7 pagesPuerperium (Trans)Charlie65129No ratings yet
- MALPRESENTATIONDocument13 pagesMALPRESENTATIONLady Jane CaguladaNo ratings yet
- Normal Labor and DeliveryDocument142 pagesNormal Labor and DeliveryRosalie RoselloNo ratings yet
- Abnormal Labor and Infertility 2016 PDFDocument12 pagesAbnormal Labor and Infertility 2016 PDFLarissa TacalanNo ratings yet
- Abnormal Labor + InfertilityDocument12 pagesAbnormal Labor + InfertilityKristine VanzuelaNo ratings yet
- Normal LaborDocument42 pagesNormal Laborhacker ammerNo ratings yet
- Definition: Related Diagnostic TestsDocument8 pagesDefinition: Related Diagnostic TestsQuinn Xylon VillanuevaNo ratings yet
- 10.theories of LaborDocument18 pages10.theories of LaborJulia Ramos100% (1)
- Holistic Pregnancy Manual: Maternal Health Manuals, #1From EverandHolistic Pregnancy Manual: Maternal Health Manuals, #1No ratings yet
- It Takes Two... And a Uterus: The Ultimate Guide to Understanding and Enhancing Your FertilityFrom EverandIt Takes Two... And a Uterus: The Ultimate Guide to Understanding and Enhancing Your FertilityNo ratings yet
- Teen Girl Guide to Puberty: Understanding Hormonal Changes, Body care and Personal HygieneFrom EverandTeen Girl Guide to Puberty: Understanding Hormonal Changes, Body care and Personal HygieneNo ratings yet
- How to Boost Your Fertility and Get Pregnant FastFrom EverandHow to Boost Your Fertility and Get Pregnant FastRating: 5 out of 5 stars5/5 (1)
- Government College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-IDocument6 pagesGovernment College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-Ipriyanka100% (1)
- OB Drug Study - OxytocinDocument3 pagesOB Drug Study - OxytocinJustin AncogNo ratings yet
- Fetal Distress: Philip J. SteerDocument7 pagesFetal Distress: Philip J. Steeryenni anggrainiNo ratings yet
- Partograph NextDocument50 pagesPartograph NextPrag GK Subedi0% (1)
- Fetal Assessment DRDocument1 pageFetal Assessment DRMicah Lou CalambaNo ratings yet
- Conduct of Normal Labor and DeliveryDocument141 pagesConduct of Normal Labor and DeliveryRea Dominique CabanillaNo ratings yet
- Carla Hernandez 100Document4 pagesCarla Hernandez 100JhunnieEy ReyesNo ratings yet
- Post-Term Labor - NCPDocument7 pagesPost-Term Labor - NCPCameron De GuzmanNo ratings yet
- Introduction of Labour MonitoringDocument29 pagesIntroduction of Labour MonitoringMishti MokarramaNo ratings yet
- Apfs 2012 MidDocument79 pagesApfs 2012 Middaniel meresaNo ratings yet
- OB I For 2nd YearDocument122 pagesOB I For 2nd YeardiribaNo ratings yet
- Labor and DeliveryDocument14 pagesLabor and Deliverydexter100% (15)
- Shoulder DystociaDocument20 pagesShoulder DystociaDanielle Francis Hirang0% (1)
- Osce - Non Stress Test Remarks YES NODocument3 pagesOsce - Non Stress Test Remarks YES NOKALAI AKSHAYANo ratings yet
- Nursing Care of The Family During Labor and BirthDocument16 pagesNursing Care of The Family During Labor and BirthGladys YaresNo ratings yet
- ფიზიოლოგიური მშობიარობის მართვაDocument30 pagesფიზიოლოგიური მშობიარობის მართვაAchi BeridzeNo ratings yet
- Government College of Nursing Jodhpur (Raj.)Document5 pagesGovernment College of Nursing Jodhpur (Raj.)priyanka100% (1)
- Mengukur DJJDocument6 pagesMengukur DJJYuni PurwatiNo ratings yet
- Radha Antenatal Fetal Well Being1Document32 pagesRadha Antenatal Fetal Well Being1Shaells JoshiNo ratings yet
- Nlex - MCNDocument19 pagesNlex - MCNAileen AlphaNo ratings yet
- Obg Unit - 4Document55 pagesObg Unit - 4Preeti ChouhanNo ratings yet
- Chapter 9 (Margot-Desevo)Document11 pagesChapter 9 (Margot-Desevo)Jesse ParkNo ratings yet
- Obs-UM - Paper - 1Document16 pagesObs-UM - Paper - 1Muhammad Abbas AliNo ratings yet
- Antepartum Fetal Surveillance ACOG Bulletin 2014-1Document11 pagesAntepartum Fetal Surveillance ACOG Bulletin 2014-1William Rodriguez CoronadoNo ratings yet
- Sonicaid Team CTG - Operators Manual PDFDocument113 pagesSonicaid Team CTG - Operators Manual PDFDaniel Galindo100% (1)
- MCHN Finals 1st-QuizDocument20 pagesMCHN Finals 1st-QuizhknNo ratings yet
- Contraction Stress Test: The Underline Physiological and Technological Basis For The CST Are As FollowsDocument3 pagesContraction Stress Test: The Underline Physiological and Technological Basis For The CST Are As FollowsSagar HanamasagarNo ratings yet