Professional Documents
Culture Documents
Handout AY 19-20 Human Anatomy and Physiology Week 2 FINAL PDF
Handout AY 19-20 Human Anatomy and Physiology Week 2 FINAL PDF
Uploaded by
jacc_282Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Handout AY 19-20 Human Anatomy and Physiology Week 2 FINAL PDF
Handout AY 19-20 Human Anatomy and Physiology Week 2 FINAL PDF
Uploaded by
jacc_282Copyright:
Available Formats
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
De La Salle Medical & Health Sciences Institute
College Of Rehabilitation Sciences
Department Of Physical Therapy
PART I: THE SKELETAL SYSTEM
Functions of the Skeletal System
The skeletal system of the body is composed of four structures: bones, cartilage, tendons, and ligaments.
The skeletal system has six general functions:
1. Support . The skeleton serves as the structural framework for the body supporting soft tissues and providing attachment points
for the tendons of most skeletal muscles.
2. Protection . They protect the most important internal organs from injury. An example of this is how the skull protects the brain
and the protection that the ribcage provides for the heart and lungs.
3. Assistance in movement. Skeletal muscles can pull on bones and create body movement.
4. Mineral storage. Bone tissue stores several minerals, especially calcium and phosphorus, which contributes to the strength of
bones. Bone tissues stores about 99% of the body’s calcium supply which the bone tissue can release to the blood stream if
the serum calcium levels become lower than normal.
5. Blood cell production. Within certain types of bones, a connective tissue called a red bone marrow produces red blood cells,
white blood cells, and platelets through a process called hemopoiesis.
6. Triglyceride storage. Yellow bone marrow, consists mainly of adipose tissue, store triglycerides. This type of marrow can be
found in certain type of bones.
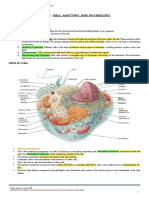
Bone Histology
The composition of the bone matrix is responsible for the characteristic of a bone.
By weight, a mature bone matrix is approximately 35% organic (collagen and proteoglycans) and 65% inorganic material (calcium
phosphate crystals called hydroxyapatite).
The collagen and mineral components of the matrix are responsible for the major functional characteristics of bone. The collagen lends
flexibility and tensile strength to the matrix, while the mineral (hydroxyapatite) provides compression strength and hardness to the bone.
Four types of cells are present in bone tissue: osteoprogenitor cells, osteoblasts, osteocytes, and osteoclasts.
Bone Cells
Cells Description
Osteoprogenitor Cells These are unspecialized bone stem cells that can become osteoblasts or chondroblasts.
Are the only bone cells to undergo cell division.
They are located in the inner perichondrium, periosteum, and endosteum.
Osteoblasts Bone building cells
They synthesize and secrete collagen fibers and other organic components needed to build the
extracellular matrix of bone tissue.
Initiates calcification of the matrix.
Becomes osteocytes once surrounded with extracellular matrix and becomes trapped in their own
secretions.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
1
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Osteocytes Mature bone cells
Are the main cells in bone tissue and maintain its daily metabolism, such as the exchange of nutrients and
wastes with the blood.
Does not undergo cell division.
Osteoclasts Huge cells derived from the fusion of 50 monocytes (a type of white blood cell) and are concentrated in
the endosteum.
They are bone destroying cells which performs resorption or bone breakdown.
Releases H+ which produce an acidic environment necessary for decalcification of bone matrix.
Bone is not completely solid but has many small spaces in between its cells and extracellular matrix components. Depending on
the size and distribution of the spaces, the regions of a bone may be classified as compact or spongy/cancellous.
Compact bone has more bone matrix and less space compared to a cancellous or spongy bone which has less bone matrix and
more space.
In the body, about 80% of the skeleton is considered as compact bone and the remaining 20% is spongy bone.
A. Cancellous or Spongy Bone
These bones are consists of interconnecting rods or plates of bone called trabeculae. Between the trabeculae are spaces filled with
bone marrow and blood vessels.
Most trabecula are thin and consists of concentric lamellae (layers of bone matrix) with osteocytes located in lacunae between the
lamellae. Each osteocyte is associated with the other osteocyte through canaliculi. Usually, no blood vessels penetrate the trabeculae
so osteocytes must obtain nutrients through their canaliculi.
Spongy bone tissue makes up most of the interior bone tissue of short, flat, sesamoid, and irregular shaped bones. In long bones, it
forms the core of the epiphyses beneath the paper-thin layer of compact bone.
Spongy bone is always covered by a layer of compact bone for protection. They are also light which allows the bone to move more
readily when pulled by a skeletal muscle and they support and protect the red bone marrow.
B. Compact Bone
These bones are denser and have fewer spaces than cancellous bone. Because of these characteristics, they are considered stronger
and functions for protection, support, and resistance to the stresses produced by weight and movement.
Anatomy of a compact bone:
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
2
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
o Compact bone is composed of repeating structural units called osteons or haversian systems. Each osteon consists of
concentric lamellae, which are circular plates of mineralized extracellular matrix of increasing diameter, surrounding a small
network of blood vessels and nerves located in the central canal.
o Between rings of lamellae are small spaces called lacunae that contains the osteocytes. Radiating in all directions of the
lacunae are canaliculi, which connect lacunae with one another forming an intricate network of canals.
o Osteocytes receive nutrients and eliminate waste products through the canal system within the compact bone. Blood vessels
from the periosteum or medullary cavity enter the bone through perforating or Volkmann’s canals which run perpendicular
to the long axis of the bone. Blood vessels from the perforating canal join the blood vessels in the central canal, pass into
the canaliculi and move though the cytoplasm of the osteocytes.
o The outer surfaces of compact bones are formed by circumferential lamellae, while in between osteons, are interstitial
lamellae which are remnants of concentric or circumferential lamellae that were partially removed during bone remodeling.
o Circumferential lamellae are connected to the periosteum by the perforating (Shapey’s) fibers.
General Structure of a Bone
Gross Anatomy of a Typical Long Bone
Parts Description
Diaphysis The long, cylindrical, main portion of the bone; the shaft of the bone.
Epiphysis The proximal and distal ends of the bone.
The regions between the diaphysis and the epiphysis. In a growing bone, each metaphysis contains the epiphyseal
Metaphysis
plates.
Epiphyseal plate is a layer of hyaline cartilage that allows the diaphysis of the bone to grow in length. When a bone
Epiphyseal
ceases to grow in length, the cartilage in the epiphyseal plate is replaced by bone which results to a structure called
Plates/Line
the epiphyseal line.
Articular cartilage Thin layer of hyaline cartilage covering a bone where it forms a joint (articulation) with another joint.
Double-layered connective tissue membrane covering the outer surface of the bone except where articular cartilage
Periosteum is present; ligaments and tendons attach to the bone through the periosteum; blood vessels and nerves from the
periosteum supply the bone; this is where the bone grows in diameter.
Endosteum The connective tissue membrane lining the inner cavities of bones.
A hollow, cylindrical space within the diaphysis that contains fatty yellow bone marrow and numerous blood vessels in
Medullary Cavity
adults. This cavity minimizes the weight of the bone by reducing dense bone material.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
3
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Bone Formation and Growth
The process by which none forms is called ossification or osteogenesis.
Bone formation occurs in four principal situations: (1) initial formation of bones in an embryo or fetus, (2) growth of bones during
infancy, childhood, and adolescence, (3) the remodeling of bones, and (4) the repair of fractures.
By the 8th week of fetal development, bone tissue begins to develop. Bone formation during fetal development follows one of the two
patterns: intramembranous ossification and endochondral ossification.
A. Intramembranous Ossification
o In this method of ossification, bone forms directly within the mesenchyme, which is arranged in sheetlike layers that resemble
membranes.
o The flat bones of the skull, most of the facial bones are formed in this way.
o The Process:
1. Intramembranous ossification begins when some of the embryonic mesenchymal cells differentiate into osteochondral
progenitor cells, then into osteoblasts. The osteoblasts then start forming bone matrix (ossification center) and making
many tiny trabeculae of woven bone.
2. Additional osteoblasts gather on the surface of the trabeculae and produce more bone creating larger and longer
spongy bone.
3. Cells surrounding the developing bone specialize to form the periosteum. Osteoblasts from the periosteum lay down
bone matrix to form an outer layer of compact bone.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
4
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
B. Endochondral Ossification
o In this method of ossification, bone gradually replaces a cartilage model.
o Most long bones of the body are formed in this way.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
5
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Bone remodeling is the ongoing replacement of old bone tissue by new bone tissue. This involves bone resorption, the removal of
minerals and collagen fibers from bone by the osteoclasts, and bone deposition, the addition of minerals and collagen fibers to bone
by osteoblasts.
One of the benefits of bone remodeling is the improve strength of the bone which will make it more resistant to breakage or fracture.
A. Bone Resorption
Osteoclasts move along the surface of the bone and digs depressions or grooves as they break down the bone matrix.
The ruffled border of the osteoclasts clings tightly to the bone and secretes acid (H+) that dissolves the bone minerals and lysosomal
enzymes that digest the organic matrix.
The digested matrix end product are then endocytosed, transported, and released to the interstitial fluid then the blood.
When resorption of a given bone area is completed, the osteoclast undergo apoptosis (cell death).
B. Control of Remodeling
Remodeling goes on continuously in the skeletal system, and are primarily regulated by two control loops that serve different
purpose:
o Maintenance of calcium homeostasis: a hormonal negative feedback loop involving parathyroid hormone (PTH)
maintains calcium homeostasis in the blood.
o Keeping bone strong: Mechanical and gravitational forces acting on the bone drive remodeling where it is required to
strengthen the bone.
Hormonal Controls
99% of the body’s calcium is stored in bones from which they can make withdrawals (resorption) or deposits as needed to
maintain serum calcium levels in the normal range.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
6
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Hormonal control primarily involves the parathyroid hormone (PTH), which is produced by the parathyroid glands. When
blood calcium level decline, PTH is released in the bloodstream. The increase in PTH levels stimulate the osteoclasts to
resorb bone, releasing calcium into the blood. As blood calcium level rise, the stimulus for the release of PTH ends.
It is important to take note that the control by PTH acts to preserve blood calcium level, not the bone’s strength or well-
being.
Response to Mechanical Stress
Wolff’s Law states that a bone grows or remodels in response to the demands or stress placed to it.
In response to mechanical stressors, osteoblasts are simulated and help build thicker, stronger bones, particularly on areas
where mechanical stress are greatest.
Other Factors Affecting Bone Remodeling
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
7
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Gross Anatomy of the Skeletal System
Classification of Bones Based on Shape
Classification Description
Long Bones These bones have greater length than width, consists of a shaft and a variable number of extremities or
epiphyses, and are slightly curved for strength.
Long bones consist mostly of compact bone tissue in their diaphysis and spongy bone tissue in their
epiphyses.
Example: femur, radius and ulna, phalanges, humerus
Short Bones Are somewhat cube-shaped and are nearly equal in length and width.
Consist of spongy bone tissue except at the surface, which has a thin layer of compact bone tissue.
Example: carpal bones and tarsal bones
Flat Bones Are generally thin and composed of two nearly parallel plates of compact bone tissue enclosing a layer of
spongy bone tissue.
Example: cranial bones, sternum, ribs, scapula
Irregular Bones Have complex shapes and cannot be grouped into the other categories.
They vary in the amount of spongy and compact bone present.
Example: vertebrae, sphenoid bone, hip bones
Sesamoid Bones Sesame seed shaped bones
They develop in certain tendons where there is considerable friction, tension, and physical stress.
Example: patella
The adult human skeleton consists of 206 named bones, most of them are paired, with one member of each pair on the right and
left sides of the body.
Bones of the adult skeleton are grouped into two principal divisions: the appendicular skeleton and the axial skeleton.
The axial skeleton consists of bones that lie around the longitudinal axis of the human body. This include the skull, the auditory
ossicles, ribs, and sternum.
On the other hand, the appendicular skeleton consists of bones from the appendages or extremities plus the bones forming the
girdles that connects the limbs to the axial skeleton.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
8
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
The external surface of a bone is rarely smooth and featureless. Bones have distinct markings and features that provide a wealth
of information about how that bone and its attached muscles and ligaments work together.
Bone Surface Markings and Anatomical Features
Term Description Example
Body Main part of the bone Body of thoracic vertebra
Head Enlarged, often rounded end Humeral head
Neck Constriction between head and body Anatomical neck of humerus
Margin, border Edge of a surface Interosseous border of tibia
Angle Bend in a bone Inferior angle of scapula
Ramus Branch of the body beyond the angle Ramus of mandible
Condyle Smooth, rounded articular surface Femoral condyles
Facet Small, flattened articular surface Superior facet of vertebrae
Ridges
Linea, Line Low ridge Intertrochanteric line of femur
Crest, crista Prominent ridge Intertrochanteric crest of femur
Spine Very high ridge Spine of scapula
Projections
Process Prominent projection Spinous process of vertebra
Tubercle Small, rounded bump Pubic tubercle
Tuberosity, tuber Knob, larger than tubercle Greater tuberosity of humerus
Trochanter Tuberosity on the proximal femur Greater trochanter of femur
Epicondyle Upon a condyle Lateral epicondyle of humerus
Lingula Flat, tongue like shaped process Lingual of mandible
Hamulus Hooked-shaped process Pterygoid Hamulus of sphenoid bone
Cornu Horn-shaped process Greater cornu of hyoid bone
Openings
Foramen Hole Foramen magnum
Canal, meatus Tunnel External auditory meatus
Fissure Cleft Inferior orbital fissure
Sinus, labyrinth Cavity Frontal sinus
Depressions
Fossa General term for a depression Infraspinous fossa of scapula
Notch Depression in the margin of a bone Scapular notch
Fovea Little pit Fovea of the head of radius
Groove, sulcus Deep, narrow depression Bicipital groove of humerus
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
9
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
PART 2: JOINTS AND MOVEMENT
Joint Structure and Function
A joint or articulation is the site where two or more bones come together. Movement of the body as a whole occurs primarily through
rotation of bones about an individual joints.
Joints are classified structurally, based on their anatomical characteristics, and functionally, based on the type of movement it permits.
Structural Classification of Joints
Fibrous Joint Cartilaginous Joint Synovial Joint
Description Articulating surfaces of the bones Bones are connected by means of a Articular surfaces of the bones are
are connected by fibrous tissue hyaline cartilage or fibrocartilage covered by a thin layer of hyaline
cartilage separated by a joint cavity
lined by a synovial membrane.
Connective tissue Fibrous connective tissue and Hyaline cartilage and fibrocartilage Fibrous capsule with ligaments
present fibroelsatic tissue predominates
Joint cavity Not present Not present Present and contains synovial fluid
Movement Little to no movement Little or no movement Freely moveable
available
Sub-classification Sutures Synchondroses (hyaline plane, saddle, pivot, condyloid,
Syndesmoses cartilage) ellipsoid, ball and socket
Gomphoses Symphyses (fibrocartilage)
Examples Lambdoid suture, dentoalveolar joint Pubic symphysis, epiphyseal plates Glenohumeral joint,
acetabulofemoral joint
A. Fibrous Joints
Sutures
These are seams found only between the bones of the skull.
This is a fibrous joint composed of a thin layer of dense irregular connective tissue.
They are immovable or slightly movable.
Example: lambdoid suture and coronal suture of the skull
Syndesmosis
This is a fibrous joint in which there is a greater distance between the articulating surfaces and denser irregular connective
tissue than in a suture.
The bone are farther apart than in a suture and are joined by ligaments.
Some movements may occur because ligaments are flexible.
Example: distal tibiofibular joint, interosseous membrane
Gomphoses
Are specialized joints consisting of pegs that fit into sockets and are held in place by fine bundles of regular collagenous
connective tissue.
No movement is available
Example: dentoalveloar joint
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
10
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
B. Fibrous Joints
Synchondrosis
Are cartilaginous joints which are connected by hyaline cartilage and is immovable or slightly movable.
Example: 1st sternocostal joint
Symphysis
Are cartilaginous joints in which the ends of the articulating bones are covered with a broad, flat disc of fibrocartilage.
All symphysis occurs in the midline of the body.
They are slightly movable joints.
Example: intervertebral joints, pubic symphysis
C. Synovial Joints
These joints contain synovial fluid and allow considerable movements between articulating bones.
They are anatomically more complex than fibrous and cartilaginous joints.
Most joints of the appendicular skeleton are synovial joints.
Examples: glenohumeral joint, tibiofemoral joint
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
11
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Parts of a Typical Synovial Joint
Part Description
Articular Thin layer of hyaline cartilage that line up the articular surfaces of bones.
cartilage Has a wear-resistant, low frictional, lubricated surface which is slightly compressible and elastic and is thus ideally
constructed for easy movement over a similar surface.
Able to absorb large forces of compression and shear generated by gravity and muscular power.
Thicker in larger joints (5-7 mm) and thinner in smaller joints (1-2mm)
Articular Also known as joint capsule
capsule Encloses the synovial cavity and unites articulating bones.
Composed of two layers: an outer fibrous membrane and an inner synovial membrane.
1. Fibrous membrane: outer layer that is continuous with the fibrous layer of the periosteum.
2. Synovial membrane: lines the joint cavity except over the articular cartilage and discs. It also produces
synovial fluid which is a thin lubricating film that covers the surfaces of joints.
Synovial A viscous, clear or yellow fluid consists of hyaluronic acid.
fluid It functions in reducing friction by lubricating the joint, absorbing shock, and supplying oxygen and nutrients and
removing carbon dioxide and metabolic wastes in the articular cartilage.
Accessory Structures
Ligaments Bundles of dense regular connective tissue that holds two bones together and are highly adapted for resisting strains.
Can be classified into two: extracapsular and intracapsular
1. Extracapsular ligaments: ligaments that lie outside the articular capsule.
2. Intracapsular ligaments: ligaments the occur within the articular capsule but are excluded from the
synovial cavity by folds of the synovial membrane.
Articular Crescent-shaped pads of fibrocartilage that lie between the articular surfaces of the bones and are attached to the
discs fibrous capsule.
They help adjust the connection between articulating bones, which improves stability and reduces wear on the
articular cartilage.
Meniscus: a type of articular disc with a hole in the center.
Labrum Prominent in the ball-and-socket joint of the shoulder and hip.
The fibrocartilaginous lip that extends from the edge of the joint socket.
It helps deepen the joint socket and increase the area of contact between the socket and the ball-like surface of the
bone.
Bursa Strategically located saclike structures that function to alleviate friction in some joints.
They are extensions of the synovial membrane and contains synovial fluid that provides cushion between structures.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
12
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Classification of Synovial Joints
Type Description Type Description
Plane/ Consists of two flat bone surfaces of about equal size between Saddle Consists of two saddle-shaped articulating surfaces oriented at
Gliding which a slight gliding motion can occur. right angles to each other so that their complementary surfaces
articulate.
Hinge A convex cylinder in one bone is applied to a corresponding Pivot Consists of a relatively cylindrical bony process that rotates
concavity in the other bone. within a ring composed partly of bone and partly ligament.
Ball- Consists of a ball (head) at the end of one bone and a socket in Ellipsoi A modified ball-and-socket joint. The articular surfaces are
and- an adjacent bone into which a portion of the ball fits. d/ ellipsoid in shape, rather than spherical.
Socket condyl
oid
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
13
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Functional Classification of Joints
Type Description Example
Synarthosis/ Synarthodial Joints An immovable joint. Sutures of the skull
Their primary purpose is to offer stability.
Amphiarthrosis/ Amphiarthrodial Joints A slightly movable joint Pubic symphysis
Provides both stability and mobility.
Diarthrosis/ Diarthrodial Joints A freely movable joint Synovial joins such as the
Primary purpose is to provide mobility. glenohumeral joint
When classifying joints, the specific joint classification, both structural and functional joint classifications, should be present.
Example:
o Proximal Radioulnar Joint Synovial, diarthrodial, pivot joint
o Pubic symphysis Cartilaginous, amphiarthrodial, symphysis joint
Joint Movements
Movement of joints can be described in terms of its osteokinematics and arthrokinematics. Osteokinematics describes the motion
of bones relative to the three cardinal planes, while arthrokinematics describe the motion that occurs between articular surfaces.
This describes the movement that occurs between the shafts of two adjacent bones as the two body segments move with regard
to each other.
Osteokinematics motions are described as taking place in one plane of the body and around their corresponding axes.
A. Axis of Rotation and Degrees of Freedom
Axis of Rotation. The axis of rotation of a joint may be considered the pivot point about which joint motion occurs. Consequently,
the axis of rotation is always perpendicular to the plane of motion.
Degrees of Freedom. This refers to the number of planes of motion allowed at a joint. A joint can have a maximum of three degrees
of freedom. For example, the humeroulnar joint of the elbow has one degree of freedom (a uniaxial joint), this means that the elbow
can move freely only 1 plane of motion.
o Uniaxial joints: joints that only have one degree of freedom and moves in only one axis.
o Biaxial joints: joints that have two degrees of freedom and moves in two axes.
o Triaxial joints: joints that have three degrees of freedom and moves in all three axes.
Summary of Joints and its Motions
Degrees of Number of Planes of
Type of Joint Axes Movement
Freedom Axes Motion
Hinge Joint 1 1, Uniaxial X Sagittal Flexion-extension
Pivot Joint 1 1, Uniaxial Y Transverse Rotation
Saddle Joint X Sagittal Abduction-adduction*
2 2, Biaxial
(i.e., 1 st CMC) Z Frontal Flexion-extension*
Ellipsoid/ X Sagittal Flexion-extension
2 2, Biaxial
Condyloid Joint Z Frontal Abduction-adduction
X Sagittal Flexion-extension
Ball-and-socket
3 3, Triaxial Z Frontal Abduction-adduction
Joint
Y Transverse Rotation
*The plane of the 1st carpometacarpal joint of the thumb is rotated 90 degrees anteriorly. This is the reason why thumb flexion and extension happens
in the frontal plane and thumb abduction-adduction in the sagittal plane.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
14
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
B. Kinematic Chains
Kinematic chains refers to a combination of several joints uniting successive body segments.
There are two types of kinematic chains: open kinematic chain (OKC) and closed kinematic chain (CKC)
o Open Kinematic Chain. This describes a situation in which the distal segment of a kinematic chain is not fixed to an
immovable surface. The distal segment is therefore free to move. An example would be reaching overhead. This is an
OKC movement of the joints of the upper extremities.
o Closed Kinematic Chain. This describes a situation in which the distal segment of the kinematic chain is fixed to an
immovable surface. In this case, the proximal segment is free to move. An example is performing push-ups or sitting
down to a chair.
This is concerned with how the two articulating joint surfaces actually move on each other.
A. Joint Morphology
The shapes of the articular surfaces of joints range from flat to curved. However, most joint surfaces are at least slightly curved,
with one surface being relatively convex and one relatively concave. This convex-concave relationship improves the congruency,
increases surface area, and helps guide motions.
B. Fundamental Movements Between Joint Surfaces
Three fundamental movements exist between curved joint surfaces: roll, slide, spin.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
15
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
C. Convex-Concave Rule
RULE #1: When the bone with a convex surface is rolling, it typically involves a concurrent slide in a direction opposite to the motion
of the shaft of the bone. The combination of roll and the opposite direction slide maintains the articular stability of the joint surfaces
and avoids the bone from “rolling out” of the joint.
SLIDE
Example 1. DIP Joint going into flexion in closed
kinematic Chain
The bone (middle phalanx) with the convex surface is moving
towards flexion. To maintain the stability of the joint, the bone
surface also has to slide towards extension (opposite direction
of the roll).
RULE #2: When the bone with a concave surface moves about a stationary convex joint surface, the roll and slide occurs in the
same direction. The combination of roll and slide in the same direction maintains firm contact between articular surfaces and
prevents a dislocation from happening.
Example 2. DIP Joint going into flexion in open
kinematic Chain
The bone (distal phalanx) with the concave surface is moving
towards flexion. The joint surface also moves in the same
direction as the shaft of the bone rolling.
Factors Affecting Joint Contact and Range of Motion
The articular surfaces of synovial joints contact one another and determine the type and possible range of motion. Range of motion (ROM)
refers to the range, measured in degrees of a circle, through which the bones of a joint can be moved.
1. Shape of the articulating bones. This factor determines how closely the joint can fit together. An interlocking fit allows rotational
movement.
2. Strength and tension of the joint ligaments. Ligaments can be taut depending on the position of the joint. Tense or taut ligaments
not only restrict joint ROM but also direct the movement of the articulating bones.
3. Arrangement and tension of the muscles. Muscle tension reinforces the restraint placed on a joint by its ligaments, and thus
restrict movement. An example would be the restriction in joint ROM brought about by a tight muscle passing through a joint.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
16
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
4. Contact of soft parts. The point at which one body surface contacts another may limit ROM. For example, if you bend you knee,
the bulk of the gastrocnemius muscle imposed with adipose tissue can hinder the full ROM of the knee joint towards flexion.
5. Hormones. A hormone called relaxin, released by the placenta and ovaries during pregnancy, increase flexibility of the fibrocartilage
of the pubic symphysis and the ligaments of the sacrum and hip bone to permit the expansion of the pelvis during the late term of
pregnancy.
6. Disuse. If a joint has been immobilized for a prolonged period of time, this may result in limited ROM due to the decrease in synovial
fluid, diminished flexibility of ligaments, and muscular atrophy (muscle wasting).
PART 3: THE MUSCULAR SYSTEM
The Muscle Tissue
The following are some of the functions of the muscular system:
1. Body movement. Contraction of muscles is responsible for the overall movement of the body such as walking, running, etc.
2. Maintenance of posture . Skeletal muscles constantly maintain tone which allows us to maintain an erect position.
3. Respiration . Skeletal muscles of the thorax are responsible for respiration (diaphragm and external intercostals).
4. Production of body heat . When they contract, skeletal muscles give off heat as a product. This released heat is critical for
maintenance of body temperature.
5. Constriction of organs. Contraction of smooth muscles within walls of hollow organs and vessels causes constriction of those
structures which can propel substances such as food in the GI or regulation of blood flow in blood vessels.
6. Contraction of the heart. Contraction of cardiac muscles causes heart to beat, propelling blood to all parts of the body.
Excitability. The capacity of a muscle to receive and respond to a stimulus by changing its membrane potential.
Contractility. The ability to shorten forcibly when adequately stimulated. When muscles contract it causes movement of the structures
to which it is attached (skeletal muscle), or it may increase pressure inside hollow organs or vessels (smooth muscles).
Extensibility. The ability to extend or stretch. Muscle cells shorten when contracting, but they can be stretched, even beyond their
resting length, when relaxed.
Elasticity. The ability of a muscle to recoil and resume its resting length after stretching.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
17
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Skeletal Muscle Anatomy and Histology
A. Connective Tissue Coverings
Connective tissue surrounds and protects muscular tissue.
Fascia is a dense sheet of irregular connective tissue that lines the body wall and limbs. They surround and hold muscles with similar
function together. They allow free movement of muscles; carries blood vessels, nerves, and lymphatic vessels; and fill spaces between
muscles.
Three layers of connective tissue extend from the fascia to protect and strengthen the skeletal muscle:
a. Epimysium: the outer layer, encircling the muscle.
b. Perimysium: surrounds groups of muscle fibers, separating them into bundles called fascicles. These fascicles are visible to
the naked eye.
c. Endomysium: penetrates the interior of each fascicle and separates individual muscle fibers from one another.
The epimysium, perimysium, and endomysium all continue with the connective tissue that attaches skeletal muscle to create a tendon.
B. Nerves and Blood Vessels
Skeletal muscles have rich supply of blood vessels and nerves.
Motor neurons are specialized nerve cells originating from the brain that are responsible for stimulating skeletal muscles.
At the fascicles, the axons of the motor neurons branch repeatedly, each branch projecting toward the center of individual muscle
fiber. The contact point between the axons and the muscle fibers is called a neuromuscular junction or synapse.
Each motor neuron innervates more than one muscle fiber but more than one motor neuron innervates most of the skeletal muscles
in the body.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
18
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
C. Skeletal Muscle Fiber
Cells found in skeletal muscles are highly specialized. Each cell is called a muscle fiber. They are long, cylindrical cells, each with
several nuclei located near the plasma membrane.
Structure of the Muscle Fiber
Part Description
Sarcolemma Plasma membrane of muscle fiber.
Many nuclei of each muscle fiber lie just inside the sarcolemma
Sarcoplasm The cytoplasm of muscle fibers.
Contains red-colored protein called myoglobin.
Myofibrils The contractile organelles of the muscle fiber.
Threadlike structure which extends from one end of a muscle fiber to another.
Contains two kinds of long, thin, protein filaments called myofilaments.
Myofilaments Protein filaments which are the major components of myofibrils.
Can be classified into two: actin myofilament (thin myofilaments) and the myosin myofilament (thick
myofilament)
Transverse Tube-like invaginations through which the sarcolemma extends to the interior part of a muscle fiber.
Tubules (T-
Tubules)
Sarcoplasmic Suspended in the sarcoplasm near the T tubules.
reticulum A fluid-filled system of membranous sacs that encircles each myofibril.
This is similar to the smooth endoplasmic reticulum of nonmuscular cells.
D. The Sarcomere
The sarcomere is the basic structural and functional unit of skeletal muscle.
This is the smallest portion of skeletal muscle capable of contracting.
A sarcomere extends from one Z disk to another.
Structure of a Sarcomere
Part Description
Z-Disk A filamentous network of protein forming a disk-like structure for the attachment of actin
I-Band Light band
Includes a z-disk and extends from each side of the z-disk to the ends of the myosin filaments
Consists of only actin
A-Band Extends the length of the myosin filaments within a sarcomere
Actin and myosin filaments overlap for some distance at both ends of the A-band producing a darker
appearance.
H-Zone Center of each band where actin and myosin do not overlap
Contains only myosin
M-Line Dark line in the middle of the H-zone.
Helps hold the myosin filaments in place similar to the way z-disks hold actin filaments in place.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
19
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
E. The Myofilaments
Types of Myofilaments
Myofilament Description
Actin A thin myofilament
Resembles two strands of pearls twisted together.
Each strand of pearl is a fibrous action (F actin), while each pearl is a globular actin (G actin).
Each G actin has an active site to which the myosin binds during muscle contraction.
Troponin molecules are attached at specific intervals along the actin myofilament and have calcium binding sites.
Troponin is also attached to tropomyosin molecules located along the groove between the twisted strands of the F
actin. When calcium is not bound to troponin, tropomyosin covers the active sites on the G actin. But when calcium
binds to troponin, tropomyosin moves, exposing the active sites.
Myosin Thick myofilaments
Resembles bundles of mini golf clubs. Each golf club is a myosin molecule consisting of a head, a hinged region,
and a rod.
The head of a myosin molecule has a deep cleft where myosin can bind to the active site of G actin to form a
cross bridge.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
20
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
The point of contact of motor neuron axon branches with the muscle fiber is called the neuromuscular junction (NMJ).
This is the site where the motor neuron stimulates the muscle fiber to begin the sequence known an action potential and eventually
a contraction.
The NMJ consist of a group of enlarged axon terminals that rest in an invagination of the sarcolemma.
Each axon terminal is the presynaptic terminal, the space between the axon the muscle fiber is the synaptic cleft, and the
sarcoplasm in the area of the junction is the postsynaptic membrane or motor end-plate.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
21
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Physiology of Muscle Contraction
For muscles to contract, nerves must give off electrical signals to the muscle fibers. Muscle fibers, like other cells of the body, are
electrically excitable. Electrically excitable cells are polarized, meaning the inside of the plasma membrane is negatively charged
compare to the outside which creates a voltage difference.
The charge difference across the plasma membrane of an unstimulated cell is called the resting membrane potential (RMP).
A. Resting Membrane Potential
Action potentials cannot be produced without a single resting membrane potential.
The resting membrane potential is the result of three factors: (1) The concentration of K+ inside the plasma membrane is higher
than the outside, (2) the concentration of Na+ outside the plasma membrane is higher than the inside, and (3) the plasma
membrane is more permeable to K+ ions than Na+.
The resting membrane potential of large nerve fibers when not transmitting nerve signals is about -70 mV.
Maintenance of Resting Membrane Potential
1. K+-Na + Leak Ion Channels
o Excitable cells have many K+ leak ion channels, at rest K+ moves out of the cell faster than Na+ moves into the cell.
This is because these channels are far more permeable to potassium that to sodium, normally 100 times as
permeable.
o Because K+ is positively charged, its movement from inside to outside of the plasma membrane causes the inside of
the plasma membrane to be more negatively charged compared to the outside.
o Potassium ions diffuse down across the concentration gradient only until the charge difference across the plasma
membrane is great enough to prevent any additional diffusion of K+ out of the cell.
2. Sodium-Potassium Pump
o The sodium-potassium pump maintains the uneven distribution of Na+ and K+ across the plasma membrane.
o Since there is a normal tendency for Na+ ions to diffuse inside the cell, Na+ influx will make the cell positive or less
negative. To maintain the RMP, Na-K pump will move 3 Na+ ions out and 2 K+ ions in, this leaves a net deficit of
positive ions inside the cell, maintaining the RMP.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
22
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
B. Action Potential
This is the rapid change in the membrane potential that spreads rapidly along the nerve fiber membrane.
This begins with a sudden change from the normal negative RMP to a positive potential then ends with an almost equally
rapid change back to the negative membrane potential.
Nerve signals to the muscles are transmitted by action potentials that moves along the nerve fiber until it comes to the fiber’s
end.
The successive stages of action potentials are as follows:
a. Resting stage. This is the resting membrane potential before the action potential begins. The membrane is said to be
“polarized” during this stage. The RMP of the nerve at this stage is said to be -70 mV.
b. Depolarization stage. At this stage, the membrane potential suddenly becomes permeable to sodium ions, allowing large
amount of positively charged ions to diffuse to the interior of the axon. This immediately neutralize the RMP which is
-70mV, with the potential rising in a positive direction (depolarization). Remember that a threshold must be reached in
order for an action potential to occur (all-or-none principle), a sudden rise in the RMP of 15-30 mV is necessary to generate
an action potential. If this is not reached, no action potential will occur. However, when the threshold is reached, voltage
gated Na+ channels open, causing influx of Na+ until +35 mV is reached.
c. Repolarization stage. When the membrane potential is +35mV, there will be complete opening of the voltage gated K +
channels. This cause the K+ ions to move out of the cell making the cell negative. At the same time, the voltage gated Na +
channels close such that Na+ can no longer enter the cell.
d. Hyperpolarization stage. Because the voltage gated K+ channels remain open, this causes further K+ efflux which brings
the membrane potential to a more negative charge, even if the RMP of a nerve fiber has already been reached. As the
K+ channels close, the membrane potential returns to the resting level of -70mV.
Refractory Period
o This is time period after an action potential begins during which an excitable cell cannot generate another action potential.
This is further divided into the absolute refractory period or the relative refractory period.
During the absolute refractory period, even a strong stimulus cannot initiate a second action potential because
all the Na+ gates are open (during the repolarization stage) and when it close (during the start of the repolarization
stage), the Na+ channels will not reopen until the membrane potential returns to or near the RMP level. The
existence of the absolute refractory period guarantees that once an action potential begun, both depolarization
and repolarization phases will be completed or nearly completed before another action potential can begin.
The relative refractory period is the period of time during which a second action potential can be initiated, but
only by a larger-than-normal stimulus. It coincides with the period when the voltage-gated K+ channels are still
open after inactivated Na+ channels have returned to its resting state.
Propagation of an Action Potential
o An action potential occurs in a very small area of the plasma membrane and does not affect the entire plasma membrane.
However, the action potentials can propagate across the plasma membrane because an action potential produced at one
location can stimulate the production of an action potential in an adjacent location. Which in turn, stimulates the
production of another, and so on.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
23
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Once the action potential reaches the presynaptic terminal, it will now transfer its signals to the muscle tissue for muscle
contraction.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
24
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
–
This is a mechanism by which and action potential in the sarcolemma causes contraction of a muscle fiber.
Movement of the cross bridges causes muscle contraction.
1. The heads of the cross bridges bind with ATP, which is the source of energy for contraction. The ATPase activity of the
myosin head immediately cleaves the ATP but leaves the cleavage products, ADP plus phosphate ion, bound to the head.
2. When the troponin-tropomyosin complex binds with calcium, active sites on the G actin are exposed and binds with the
myosin heads.
3. The bond between the head of the cross-bridge and the active site of the actin filament causes conformational change in the
head, prompting the head to tilt toward the arm of the cross-bridge. This provides the power stroke.
4. Once the head of the cross-bridge tilts, this allows the release of the ADP and phosphate ion that were previously attached to
the head. At the site of the release of the ADP, a new ATP binds. This binding of new ATP causes detachment of the head
from the actin.
5. After the head has detached from the actin, the new molecule of ATP is cleaved to begin the next cycle, leading to a new
power stroke.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
25
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Muscle relaxation occurs when acetylcholine is no longer released at the neuromuscular junction.
The cessation of action potential along the sarcolemma stops calcium release from the sarcoplasmic reticulum and calcium is
actively transported back into the sarcoplasmic reticulum.
As the calcium concentration decreases in the sarcoplasm, the calcium diffuses away from the troponin molecule.
The troponin-tropomyosin complex then reestablishes its position, which blocks the active sites on actin. This will prevent cross-
bridges to reform, and the muscle relaxes.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
26
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Muscle Twitch: a single, brief contraction and relaxation cycle in a muscle fiber. This does not last long enough or generate
enough tension to perform any work.
Motor unit: consists of a single motor neuron and all the muscle fiber it innervates. Motor units vary in terms of their sensitivity to
stimuli for contraction; some motor units respond readily to weak stimuli, whereas others respond only to strong stimuli.
A. Stimulus Strength and Motor Response
The strength of muscle contraction varies from weak to strong. The force of contraction is increased in two ways: (1)
summation and (2) recruitment.
o Summation. It means adding together of individual twitch contractions to increase the intensity of overall muscle
contraction. Can be classified into multiple motor unit summation (number of motor unit stimulated increases) or multiple
wave summation (summation produced when many action potentials are produced).
o Recruitment. It involves increasing the number of muscle fibers contracting.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
27
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Treppe. This phenomenon occurs when a muscle begins to contract after a long period of rest. At the start of the contraction,
its initial strength may be as little as one half of its strength 10 to 50 muscle twitches later. Increased tension may result from
the accumulation of small amounts of calcium in the sarcoplasm for the first few contractions or from an increasing rate of
enzyme activity.
B. Stimulus Frequency and Whole Muscle Contraction
As the frequency of action potentials in a skeletal muscle increases, the frequency of contraction also increases until a period
of sustained contraction, or tetanus, is achieved.
Tetanization. This happens when the frequency reaches a critical level, the successive contractions eventually become so
rapid that they fuse together and the whole muscle contraction appears to be completely smooth and continuous. At a slightly
higher frequency, the strength of contraction reaches its maximum, and thus any additional increase infrequency beyond that
point has not further effect in increasing contractile force.
C.Length-Tension Relationship
This indicates how the forcefulness of muscle contraction depends on the length of the sarcomeres within a muscle before the
contraction begins.
As the sarcomeres are stretched to a longer length, the zone of overlap shortens, and fewer myosin heads can make contact
with the thin filaments. Therefore, the tension the fiber can produce decreases. On the other hand, the same goes if a sarcomere
length becomes increasingly short. The thick filaments crumple, resulting to fewer myosin heads making contact with the
filaments.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
28
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
D. Types of Muscle Contraction
Muscle contraction are classified based on the type of contraction that predominates.
a. Isometric contractions. In this type of contraction, the length of the muscle does not change but the amount of tension
increases during contraction.
b. Isotonic contractions. In this type of contraction, the amount of tension produced by the muscle is contant during
contraction but the length of the muscle changes. This can be classified into two:
1. Concentric contraction: are isotonic contractions in which tension in the muscle is great enough to overcome
the opposing resistance, and the muscle shortens. Concentric activity produces acceleration of body segments.
2. Eccentric contraction: are isotonic contractions in which tension in the muscle, but the opposing resistance is
great enough to cause the muscle to increase in length. Eccentric motion decelerates the body segments and
provides shock absorption as when landing from a jump or walking.
Gross Anatomy of the Muscular System
Skeletal muscles produce movements by pulling on bones. They extend from bone to bone across the linking joint. Most muscles
are attached to bone by tendons at their origins and insertions.
Origin. The attachment of the muscle that is usually the most stationary, proximal end of the muscle. Muscles can have more than
one origin (e.g., triceps brachii). In the case of multiple origins, each origin is called a head.
Insertion. This is usually the distal end of the muscle attached to the bone being pulled toward the other bone of the joint. A rule of
thumb is that the insertion is always pulled towards the origin.
Belly. This is the part of the muscle that is between the origin and the insertion.
Tendons. These are dense connective tissue that connect muscles to bones. Tendons can be long and ropelike, short, or broad
and sheet-like (aponeurosis).
The muscle shape and size can influence the degree to which it can contract and the amount of force it can generate.
As a muscle fiber contracts, it shortens to about 70% of its resting length. The longer the fibers, the greater the range of motion it
can produce.
On the other hand, the power of a muscle depends on its total cross sectional area. The more fiber per unit of cross sectional area
a muscle has, the more power it can produce.
Muscle fiber arrangement can vary from pennate, fusiform, circular, triangular, or parallel.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
29
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
Movements often are the result of several skeletal muscles acting as a group. The following terms are often used to describe the
actions of a muscle:
Terms used for Describing Muscle Action
Term Description Example
Agonist or Prime The muscle or muscle group that is most directly related to the When the elbow bends, the biceps brachii
Mover initiation and execution of a particular movement. is the prime mover of the movement.
Antagonist The muscle or muscle group that is considered to have the opposite When bending the elbow, the triceps
action of a particular agonist. brachii is considered as the antagonist of
the movement of the biceps brachii.
Synergist Muscles or group of muscles are considered synergists when they When flexing the shoulder, the deltoids,
cooperate during the execution of a particular movement. biceps brachii, and the pectoralis major all
help to perform the movement. They are
considered as synergists.
Fixator These are muscles that hold one bone in place relative to the body When moving the humerus, the scapular
while a more distal bone is moved. It often stabilizes the origin of the muscles acts as fixators to hold the
prime mover, so that the action occurs at its insertion point. scapula in place.
Force couple A type of muscle synergy wherein two or more muscles The hip flexors and the lower back
simultaneously produces forces in different linear directions, with the extensors create a force-couple to
resulting torque act in the same rotatory direction. produce anterior pelvic tilt.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
30
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
The names of skeletal muscles contain combinations of the root words of their distinctive features.
In producing movement, bones act as levers, and joints function as the fulcrums of these levers.
A lever is a rigid structure that can move around a fixed point called a fulcrum. A lever acts on two different points by two different
forces: the effort which causes movement, and the load or resistance, which opposes the movement.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
31
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
The relative distance between the fulcrum and load and the point at which the effort is applied determine whether a given level
operates at a mechanical advantage or disadvantage.
o Mechanical advantage: arrangement of forces requires a smaller force to produce movement.
o Mechanical disadvantage: arrangement of forces requires a larger force to produce movement.
Levers can be categorized into three classes according to the position of forces.
A. First Class Levers
Axis or fulcrum of rotation is located between the effort and the load.
This type of lever is comparable to scissors of see-saws.
This type of lever gain either force or distance, depending on the relative lengths of the force arm and the resistance arm.
Example in the body: lever formed by the head resting on the vertebral column. When the head is raised, the contraction of the
posterior neck muscles provide the effort, the atlanto-occipital joint as the fulcrum, and the weight of the anterior skull is the load.
B. Second Class Levers
The point of resistance application lies between the force and the fulcrum so the lever arm is shorter than the lever arm of the force.
They provide a force advantage so large weights can be supported or moved by a smaller force.
An example of a second class lever is a wheel barrow. In the body this is observable when a person stand in tiptoes.
C.Third Class Levers
The point of force application lies between the resistance and fulcrum.
The most common type of lever in the human body.
This lever is designed to produce speed of the distal segment and move as small weight a long distance.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
32
A&P: Neuromusculoskeletal System
College of Rehabilitation Sciences
Del La Salle Medical & Health Sciences Institute
In the human body, this type of levers produces small amount of shortening of a muscle causes a large arc of motion at the
joint.
References
Hall, J. E., & Guyton, A. C. (2016). Guyton and Hall textbook of medical physiology (13th ed.). Philadelphia (PA): Elsevier.
Houglum, P.A. & Bertoti, D.B. (2012). Brunnstrom’s clinical kinesiology (6th edition). Philadelphia: FA Davis Company
Marieb, E.N. & Hoehn, K. (2019). Human anatomy and physiology (11th ed.). San Francisco: Pearson Benjamin Cummings
Neumann, D. (2017). Kinesiology of the musculoskeletal system foundations for physical rehabilitation (3 rd edition). Mosby, USA
Seeley, R. R., VanPutte, C. L., Regan, J., Russo, A., Stephens, T., & Tate, P. (2017). Seeley's anatomy and physiology (11th ed.). New York, NY: McGraw-
Hill.
Tortora, G.J. & Derrickson, B. (2017). Principles of anatomy and physiology (15th edition). USA: John Wiley & Sons, Inc.
© Ram Janzen C. Fauni, PTRP
Unauthorized use and/or duplication of this material without express and written permission from the owner and/or author is strictly prohibited.
33
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Chapter 9 Muscles and Muscle TissueDocument23 pagesChapter 9 Muscles and Muscle TissueYi Pan Chen100% (11)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Lood Vessel Structure An Function: Objectives MaterialsDocument9 pagesLood Vessel Structure An Function: Objectives MaterialsArthur HamadaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 25 Phlebotomy ProcedureDocument10 pages25 Phlebotomy ProcedureMichael TaylorNo ratings yet
- ART ACT No.1Document1 pageART ACT No.1Alfred BajarNo ratings yet
- Anatomy of The Upper Extremities: The Shoulder ComplexDocument8 pagesAnatomy of The Upper Extremities: The Shoulder ComplexAlfred BajarNo ratings yet
- Human Anatomy Worksheet1Document1 pageHuman Anatomy Worksheet1Alfred BajarNo ratings yet
- Human Anatomy Worksheet1Document1 pageHuman Anatomy Worksheet1Alfred BajarNo ratings yet
- BAJAR, Pheodor Alfred D. 10/09/2020 PT 1-3 Sir Jed AbatayoDocument2 pagesBAJAR, Pheodor Alfred D. 10/09/2020 PT 1-3 Sir Jed AbatayoAlfred Bajar0% (1)
- Membrane Potential Summary - FinalDocument6 pagesMembrane Potential Summary - FinalAlfred BajarNo ratings yet
- 002 Cell Membrane PhysiologyDocument12 pages002 Cell Membrane PhysiologyAlfred BajarNo ratings yet
- 001 HomeostasisDocument3 pages001 HomeostasisAlfred BajarNo ratings yet
- 004 Handout Musculoskelital - Upper Extremities PDFDocument13 pages004 Handout Musculoskelital - Upper Extremities PDFAlfred BajarNo ratings yet
- 002 Handout Basic Concepts Part 2Document8 pages002 Handout Basic Concepts Part 2Alfred BajarNo ratings yet
- CBC ReportDocument1 pageCBC Reportdivyanshuglmp937No ratings yet
- Transportation - Life Processes Class 10 Notes: Transportation in Human Beings: The Circulatory System Is Responsible ForDocument4 pagesTransportation - Life Processes Class 10 Notes: Transportation in Human Beings: The Circulatory System Is Responsible ForGeetanjali jadhavNo ratings yet
- BLOODDocument5 pagesBLOODSora TensaiNo ratings yet
- Haemophilia AssignmentDocument2 pagesHaemophilia AssignmentKhadija JaraNo ratings yet
- Forensics BloodDocument40 pagesForensics BloodJared IrwinNo ratings yet
- Bleeding and Coagulation Time:: 1-Procedure of Duke MethodDocument2 pagesBleeding and Coagulation Time:: 1-Procedure of Duke MethodAnonymous 59sx7W4No ratings yet
- Hemolytic Disease of NewbornDocument15 pagesHemolytic Disease of Newborncyphochilus100% (1)
- World Health Organization Collaborating Center For Nursing DevelopmentDocument3 pagesWorld Health Organization Collaborating Center For Nursing DevelopmentNicole Angeli ManuelNo ratings yet
- Rehman Medical Institute: Test Result Unit Reference ValuesDocument1 pageRehman Medical Institute: Test Result Unit Reference ValuesfahadbasahirNo ratings yet
- Hema FC Part 2 1Document10 pagesHema FC Part 2 1Lynther Myle ArizoNo ratings yet
- RETICULOCYTESDocument4 pagesRETICULOCYTESVarun ShahNo ratings yet
- Unit 3 Muscle Physiology - BPT PDFDocument55 pagesUnit 3 Muscle Physiology - BPT PDFRadhikaNo ratings yet
- Von-Willebran D: Group 6: Rodillo Garrido Jr. Princess Cendaña Karmella Santos Ellis M. MilagrosoDocument12 pagesVon-Willebran D: Group 6: Rodillo Garrido Jr. Princess Cendaña Karmella Santos Ellis M. Milagrosoellis milagrosoNo ratings yet
- Labex8 Epithelial TissuesDocument6 pagesLabex8 Epithelial TissuesJulian SobremisanaNo ratings yet
- Complete Blood Count Result Biological Reference Interval 16.30Document5 pagesComplete Blood Count Result Biological Reference Interval 16.30Kabir ShelkeNo ratings yet
- (HEMA) Practice QuestionsDocument4 pages(HEMA) Practice QuestionsElyssa VergaraNo ratings yet
- Circulatory System Stations-1Document30 pagesCirculatory System Stations-1kartik.goel3010No ratings yet
- Activity 3 Epithelial TissueDocument11 pagesActivity 3 Epithelial TissueAesthetics MinNo ratings yet
- Hema 2Document31 pagesHema 2Mark SyNo ratings yet
- Complete Blood Count: Result Test Reference RangeDocument1 pageComplete Blood Count: Result Test Reference RangeRajaNo ratings yet
- Counting of RBC's and WBC's Using Image Processing TechniqueDocument6 pagesCounting of RBC's and WBC's Using Image Processing TechniqueEditor IJRITCCNo ratings yet
- Introduction To Hematology: What Is Blood ?Document5 pagesIntroduction To Hematology: What Is Blood ?Missy Vergara FloriaNo ratings yet
- Konsep Dasar Hematology, Imunology and Onkology PDFDocument62 pagesKonsep Dasar Hematology, Imunology and Onkology PDFBintang Yahasri Gita BuanaNo ratings yet
- Cold Chain Presentation Erick 2Document26 pagesCold Chain Presentation Erick 2Airep OiralihNo ratings yet
- Haematological Profile and Erythrocyte Indices in Different Breeds of PoultryDocument4 pagesHaematological Profile and Erythrocyte Indices in Different Breeds of PoultrySukma WijayaNo ratings yet
- Blood BankingDocument2 pagesBlood BankingJENNIFER CAMANo ratings yet
- Complications of Blood TransfusionsDocument4 pagesComplications of Blood TransfusionsZain Hadi100% (1)