Professional Documents
Culture Documents
Australian Dental Journal
Australian Dental Journal
Uploaded by
garexathOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Australian Dental Journal
Australian Dental Journal
Uploaded by
garexathCopyright:
Available Formats
Australian Dental Journal
The official journal of the Australian Dental Association
Australian Dental Journal 2013; 58: 117–119
CASE REPORT
doi: 10.1111/adj.12025
Acute fetal distress following tooth extraction and abscess
drainage in a pregnant patient with maxillofacial infection
ß elebi,* MS K€
NC uk,† M Tasß,† E Soylu,* OA Et€
ut€ oz,* A Alkan*
*Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Erciyes University, Kayseri, Turkey.
†Department of Obstetrics and Gynecology, Faculty of Medicine, Erciyes University, Kayseri, Turkey.
ABSTRACT
Oral infections have been implicated in adverse pregnancy outcomes such as pre-eclampsia, premature delivery and
growth retardation. A 28-year-old and 9 months pregnant otherwise healthy woman with a complaint of facial swelling
and dental pain was referred to the Department of Oral and Maxillofacial Surgery. Oral examination revealed periman-
dibular and masticator space infection related to the left mandibular third molar tooth. Eight hours after surgical inter-
vention, fetal distress developed. The patient was immediately taken into surgery and a male baby delivered by
Caesarean section. The baby was then admitted to the intensive care unit. On the twelfth day of his admission, the baby
was discharged in good health. Severe maxillofacial infection in pregnancy is a medically complicated situation which
should be treated by an oral and maxillofacial surgeon in consultation with an obstetric and gynaecology service.
Keywords: Tooth extraction, maxillofacial infection, pregnancy.
(Accepted for publication 12 August 2012.)
INTRODUCTION PATIENT AND METHOD
Tooth extraction is a relatively safe procedure during A 28-year-old and 9 months pregnant otherwise
pregnancy. A pregnant patient with a maxillofacial healthy woman with the complaint of facial swelling
infection requires special attention due to major and dental pain was referred to the Department of
changes in physiology and metabolism including car- Oral and Maxillofacial Surgery at Erciyes University,
diovascular, respiratory and gastrointestinal systems, Kayseri, Turkey. The patient said her pregnancy had
as well as changes in the oral cavity and increased been proceeding without difficulty. Clinical examina-
susceptibility to oral infection.1 tion revealed a large soft tissue swelling under the
Recently, oral infections have been implicated in mandible, extending superiorly to the zygomatic arc
adverse pregnancy outcomes such as pre-eclampsia, and inferiorly to the angles of the mandible in the
premature delivery and miscarriage.2 Gram-negative form of combined perimandibular and masticator
anaerobes, which play an important role in maxillo- space infections, with no fever nor abnormal vital
facial infections, may serve as a source for endotox- signs. Oral examination was complicated with trismus
ins and lipopolysaccharides, which then increase with a maximal mouth opening of 15 mm; however,
local inflammatory mediators, leading to such com- a mandibular third molar tooth with a deep carious
plications.3 In theory, extraction of an infected tooth lesion could be observed on the left. The patient had
may act as a portal of entry for both bacterial agents already been given ampicillin sulbactam (1 g) three
and cytokines, and set the stage for systemic inflam- times a day for 5 to 7 days by her general dentist.
matory response, culminating in fetal distress which After consulting with the Department of Obstetrics
implies that the viability of the fetus is compro- and Gynecology for a surgical intervention under local
mised. anaesthesia, we decided to proceed with the extraction
Fetal distress, developed after the treatment of of the tooth with extraoral drainage of the abscess
a severe maxillofacial infection in a 28-year-old and under local anaesthesia and antibiotic coverage.
9 months pregnant otherwise healthy woman is Although minimal discharge was obtained from the
described. incision, a Penrose drain was left in place for two days.
© 2013 Australian Dental Association 117
ß elebi et al.
NC
decreased variability denoting fetal distress (Fig. 2 and
3). The patient was immediately taken into surgery and
a male baby delivered by caesarean section. The baby
was admitted to the intensive care unit and discharged
in good health 12 days later.
DISCUSSION
The mandibular third molar tooth is one of the most
common source of odontogenic infections. These
infections can spread into perimandibular spaces
namely submandibular, sublingual and submental
spaces, as well as masticator spaces, whose
components may be considered separately as sub-
masseteric, pterygomandibular and temporal spaces.4
The infection may disseminate through the blood-
stream to distant body sites causing cerebral abscess,
cavernous sinus thrombosis, and to the systemic circu-
lation causing bacterial endocarditis.5
Fig. 1 Submandibular and masticator space infection arising from left lower
third molar. Arrows show the enlargement of masticatory muscles. Certain conditions, such as immunosupression, may
place patients at risk of impaired resistance to infec-
A postoperative computed tomography confirmed that tion. Although pregnant patients are usually not
infection was limited to masticator spaces and not lead- immunocompromised, the maternal immune system
ing to airway obstruction (Fig. 1). Because the patient does become suppressed in response to the fetus.6 As
refused to be admitted, she was advised to continue her such, there is a decrease in cell-mediated immunity
medication and return for follow-up the next day. and natural killer cell activity.1 Therefore, bacterial
Eight hours after the intervention, the patient returned agents can easily enter the bloodstream and conse-
to the emergency department complaining of high fever quently intrauterine infection may develop.7
and decreased perception of fetal movement. At initial Diffusion of bacteria or their by-products from the
evaluation, blood pressure was 100/90 mm Hg, heart oral cavity to the bloodstream has been directly or
rate 90 and fever 38.7 °C. The patient was then sent to indirectly correlated with adverse pregnancy out-
the Department of Obstetrics and Gynecology. Ultraso- comes8 such as preterm birth, low birth weight, fetal
nographic examination revealed a 35-week-old single- growth restriction, pre-eclampsia and perinatal mor-
ton fetus with normal growth. Amniotic fluid volume tality. The increase of pro-inflammatory cytokines has
and placental image were normal. Cardiotocography been considered to be responsible for placental modifi-
showed severe persistent late decelerations with cations that lead to such complications.7
Fig. 2 Preoperative fetal heart rate tracing showing normal baseline heart rate, variability and acceleration (arrows). Note the absence of deceleration. This
is a completely normal and reassuring fetal heart rate pattern.
118 © 2013 Australian Dental Association
Fetal distress following tooth extraction in a pregnant patient
occurrence of acute fetal distress in an otherwise
uneventful pregnancy, after the treatment of a maxil-
lofacial infection, may indicate a different implica-
tion of interaction between systemic inflammatory
response, oral cytokines and pregnancy. Further
research is required to evaluate the relationship
between maxillofacial infections and adverse preg-
nancy outcomes.
ACKNOWLEDGEMENT
This report was presented as a poster at the 6th
AC _ International Oral and Maxillofacial Surgery
ß BID
Society Congress held in Antalya, Turkey (30 May –
Fig. 3 Fetal heart rate tracing showing late deceleration. 3 June 2012).
Although adverse pregnancy outcomes associated REFERENCES
with oral infections are widely examined in the 1. Giglio JA, Lanni SM, Laskin DM, Giglio NW. Oral health care
periodontal literature, there are only a few reports for the pregnant patient. J Can Dent Assoc 2009;75:43–48.
relating to maxillofacial infections. In one case of 2. Xiong X, Buekens P, Fraser WD, Beck J, Offenbacher S. Peri-
odontal disease and adverse pregnancy outcomes: a systematic
Ludwig’s angina, delivery was indicated given the review. BJOG 2006;113:135–143.
non-reassuring fetal tracing, which was speculated to 3. Offenbacher S, Jared HL, O’Reilly PG, et al. Potential patho-
be associated with fetal hypoxia or acidosis.9 In our genic mechanisms of periodontitis associated pregnancy compli-
case, a maxillofacial infection, arising from the left cations. Ann Periodontol 1998;3:233–250.
mandibular third molar, involved both the masticator 4. Ryan P, McMahon G. Severe dental infections in the emergency
department. Eur J Emerg Med 2012;19:208–213.
and the perimandibular spaces and resulted in severe
5. Flynn TR. The swollen face. Severe odontogenic infections.
trismus. The patient was advised to be admitted; Emerg Med Clin North Am 2000;18:481–519.
however, she refused and was therefore instructed to 6. Gordon MC. Maternal physiology in pregnancy. In: Gabbe SG,
continue her medication and to return for a follow- Niebyl JR, Simpson J, eds. Obstetrics: normal and problem
up the next day. Although the patient was healthy pregnancies. 4th edn. New York: Churchill Livingstone, 2002:
63–91.
and the severity of infection suppressed by antibiot-
ics, fetal distress with severe persisted late decelera- 7. Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection
and preterm delivery. N Engl J Med 2000;342:1500–1507.
tions and decreased variability in cardiotocography
8. Han YW, Redline RW, Li M, Yin L, Hill GB, McCormick TS.
developed eight hours after the surgical intervention. Fusobacterium nucleatum induces premature and term stillbirths
This outcome may be attributed to a systemic in pregnant mice: implication of oral bacteria in preterm birth.
inflammatory response to bacterial agents and cyto- Infect Immun 2004;72:2272–2279.
kines which spread into the bloodstream after the 9. Moorhead K, Guiahi M. Pregnancy complicated by Ludwig’s
angina requiring delivery. Infect Dis Obstet Gynecol 2010;
surgical intervention. 2010:158264.
In conclusion, a severe maxillofacial infection in
pregnancy is a medically complicated situation as Address for correspondence:
there are effectively two patients at risk of serious Dr Nukhet C ß elebi
complications. Therefore, general dental practitioners Department of Oral and Maxillofacial Surgery
must understand the severity of infections in the Faculty of Dentistry
maxillofacial region in this particular patient popula- Erciyes University
tion, and consider referring such patients to an oral Kayseri
and maxillofacial surgeon working in association Turkey
with an obstetric and gynaecology service. Also, the Email: NCelebi@erciyes.edu.tr
© 2013 Australian Dental Association 119
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5825)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Optimizing Thyroid Medications Ebook-3Document133 pagesOptimizing Thyroid Medications Ebook-3martuca100% (1)
- Case Study HypothyroidismDocument6 pagesCase Study HypothyroidismGabriela Valdivia100% (2)
- Urn Uvci 01 Ro Yd731x8e2voz1dl92xngp046lrm59w#tDocument2 pagesUrn Uvci 01 Ro Yd731x8e2voz1dl92xngp046lrm59w#tGeorge HonciugNo ratings yet
- UntitledDocument4 pagesUntitledCharisse Alexia DinopolNo ratings yet
- Hafnia AlveiDocument5 pagesHafnia AlveiluisNo ratings yet
- Brugada SyndromeDocument5 pagesBrugada SyndromevitriaNo ratings yet
- Public Health Nursing Population Centered Health Care in The Community Stanhope 8th Edition Test BankDocument3 pagesPublic Health Nursing Population Centered Health Care in The Community Stanhope 8th Edition Test BankMichael SingletonNo ratings yet
- Autism and EpilepsyDocument5 pagesAutism and Epilepsyclarajimena25No ratings yet
- Sindrom Uko Ene Osobe (Moersch-Woltman) : Lije Vjesn 2010 132:110-114Document5 pagesSindrom Uko Ene Osobe (Moersch-Woltman) : Lije Vjesn 2010 132:110-114bimtolaNo ratings yet
- Ski Injury Trauma Gallery Original PicturesDocument12 pagesSki Injury Trauma Gallery Original PicturesSurgicalgownNo ratings yet
- Arthroscopy: If You Have Persistent Joint Pain, Your Doctor May Suggest ArthrosDocument4 pagesArthroscopy: If You Have Persistent Joint Pain, Your Doctor May Suggest ArthrosCaty RamosNo ratings yet
- Spinal Cord Injury Without Radiological AbnormalitDocument3 pagesSpinal Cord Injury Without Radiological Abnormalitcollestein christdianNo ratings yet
- Lennox Gastaut SyndromeDocument12 pagesLennox Gastaut SyndromedulcejuvennyNo ratings yet
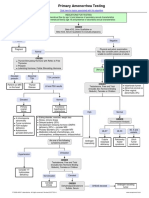
- Primary Amenorrhea Testing AlgorithmDocument1 pagePrimary Amenorrhea Testing AlgorithmfarmasiNo ratings yet
- PasienDocument12 pagesPasienDharma Abdi Riel ManullangNo ratings yet
- Omacor: Municipal Planning and Development OfficeDocument9 pagesOmacor: Municipal Planning and Development OfficeArthur MericoNo ratings yet
- AchillodyniaDocument1 pageAchillodyniaBos NaibahoNo ratings yet
- HEALTH ASSESSMENT Module 1Document52 pagesHEALTH ASSESSMENT Module 1Sharifa Badaria AtalNo ratings yet
- Canine Parvo VirusDocument60 pagesCanine Parvo VirusPutrina SiregarNo ratings yet
- Dissociative DisordersDocument24 pagesDissociative DisordersSimón Ortiz LondoñoNo ratings yet
- UCLA Mobile Eye Clinic 2019 Needs AssessmentDocument1 pageUCLA Mobile Eye Clinic 2019 Needs AssessmentUMEC Young Professionals InitiativeNo ratings yet
- Ophthalmology Clinical Cases pixOpOpDocument61 pagesOphthalmology Clinical Cases pixOpOpUsman ImtiazNo ratings yet
- Authorization To Walk HomeDocument50 pagesAuthorization To Walk HomeAidan FranciscoNo ratings yet
- Journal Pre-Proof: Advances in Chronic Kidney DiseaseDocument19 pagesJournal Pre-Proof: Advances in Chronic Kidney DiseaseAbdul RokhmanNo ratings yet
- 1 Introduction To Medical JurisprudenceDocument2 pages1 Introduction To Medical JurisprudenceMowanNo ratings yet
- TachycardiaDocument12 pagesTachycardiaPuskesmas Pinang JayaNo ratings yet
- Nursing Care PlanDocument9 pagesNursing Care PlanRenea Joy ArruejoNo ratings yet
- Psychiatric Exam Part 1Document7 pagesPsychiatric Exam Part 1Charmaine Danica MadridNo ratings yet
- Ground Floor Plan (Main Building Facility: Project Title John Paul Silloren PiteroDocument1 pageGround Floor Plan (Main Building Facility: Project Title John Paul Silloren PiteroBryan Silloren PiteroNo ratings yet
- S.subashini Hospital Waste ManagementDocument70 pagesS.subashini Hospital Waste ManagementVenkatram PrabhuNo ratings yet