Professional Documents
Culture Documents
Tripod PDF
Tripod PDF
Uploaded by
banteng wibisonoCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5824)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- PLE 2019 - Microbiology Questions and Answer KeyDocument16 pagesPLE 2019 - Microbiology Questions and Answer Keydickson100% (4)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Motivation Letter Utrecht UniversityDocument2 pagesMotivation Letter Utrecht UniversityAjit Antony50% (2)
- Bacteria Notes SketchyDocument3 pagesBacteria Notes SketchyJayNo ratings yet
- Measles PamphletDocument2 pagesMeasles Pamphletapi-384459604No ratings yet
- GOLD 2021 Teaching Slide Set v102 12nov2020Document58 pagesGOLD 2021 Teaching Slide Set v102 12nov2020banteng wibisonoNo ratings yet
- A13v12n3 PDFDocument8 pagesA13v12n3 PDFbanteng wibisonoNo ratings yet
- TNF-alpha Levels in Serum and Mononuclear Cell Lysate of Nigerian Tuberculosis Patients at DiagnosisDocument5 pagesTNF-alpha Levels in Serum and Mononuclear Cell Lysate of Nigerian Tuberculosis Patients at Diagnosisbanteng wibisonoNo ratings yet
- Human Anatomy and Physiology SyllabusDocument5 pagesHuman Anatomy and Physiology Syllabusbanteng wibisonoNo ratings yet
- Γ And Tnf-Α Levels: Ir - Perpustakaan Universitas AirlanggaDocument1 pageΓ And Tnf-Α Levels: Ir - Perpustakaan Universitas Airlanggabanteng wibisonoNo ratings yet
- Idsa GuidelineDocument50 pagesIdsa GuidelinenilnaNo ratings yet
- Brain Tumors With Review of Literature: Immunohistochemistry or Biomarkers Versus HistomorphologyDocument5 pagesBrain Tumors With Review of Literature: Immunohistochemistry or Biomarkers Versus Histomorphologybanteng wibisonoNo ratings yet
- Fungi MedicalDocument25 pagesFungi Medicalbanteng wibisono100% (1)
- Pathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun MengDocument20 pagesPathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun Mengbanteng wibisonoNo ratings yet
- Dimorphic Fungi: Prabin Shah BSCMLT, MSC (Biochemistry)Document49 pagesDimorphic Fungi: Prabin Shah BSCMLT, MSC (Biochemistry)banteng wibisonoNo ratings yet
- Brain CancerDocument7 pagesBrain Cancerbanteng wibisonoNo ratings yet
- Selective MediaDocument10 pagesSelective Mediaprincess_likemist4No ratings yet
- POSTER PRESENTATION PDF Aja PDFDocument1 pagePOSTER PRESENTATION PDF Aja PDFShilpa MishraNo ratings yet
- Her Verte Tal 2017Document12 pagesHer Verte Tal 2017Abhishek BanerjeeNo ratings yet
- S60 - Morvinandan Diagnostic Centre LLP: Patientreportscsuperpanel - General - Box - SC (Version: 6)Document8 pagesS60 - Morvinandan Diagnostic Centre LLP: Patientreportscsuperpanel - General - Box - SC (Version: 6)Kapil NagpalNo ratings yet
- Giardia & Giardiasis: (Intestinal Flagellate)Document22 pagesGiardia & Giardiasis: (Intestinal Flagellate)Naing Lin SoeNo ratings yet
- ABO Blood GroupingDocument10 pagesABO Blood GroupingJhon WickNo ratings yet
- MCDB 290b SyllabusDocument2 pagesMCDB 290b SyllabusLalalalaPineapplesNo ratings yet
- Hobbs 2016Document18 pagesHobbs 2016Jônatas CavaliniNo ratings yet
- VaccinationDocument24 pagesVaccinationNitesh GandhiNo ratings yet
- Cutaneous Abscess Furuncles and CarbuclesDocument25 pagesCutaneous Abscess Furuncles and Carbuclesazmmatgowher_1219266No ratings yet
- Manual of Infection Control Procedu PDFDocument365 pagesManual of Infection Control Procedu PDFanon_789115535100% (1)
- Biofilm in OtorhinolaryngologyDocument10 pagesBiofilm in OtorhinolaryngologyMohammed SahibNo ratings yet
- Culture Media CombinedDocument131 pagesCulture Media CombinedEmit Rosary PenetranteNo ratings yet
- Pediatric Community-Acquired Pneumonia Clinical Guideline PDFDocument1 pagePediatric Community-Acquired Pneumonia Clinical Guideline PDFJohn Vincent Dy OcampoNo ratings yet
- A. Chlorophyll ADocument16 pagesA. Chlorophyll AKishor SarodeNo ratings yet
- CertificateDocument1 pageCertificatenazmulNo ratings yet
- Materi 16. Peranan Manajemen RS - PGADocument25 pagesMateri 16. Peranan Manajemen RS - PGAAri Wibowo KastaNo ratings yet
- 2019 Book PolymyxinAntibioticsFromLaboraDocument364 pages2019 Book PolymyxinAntibioticsFromLaboraDaniel JiménezNo ratings yet
- 2parasitology AssignmentDocument4 pages2parasitology AssignmentVictor PaulNo ratings yet
- Resume Tutorial A Skenario 1 Blok 14Document74 pagesResume Tutorial A Skenario 1 Blok 14Istaz MaulanaNo ratings yet
- Natural History of DiseaseDocument31 pagesNatural History of Diseasegabo dasNo ratings yet
- Parasitology Short Quiz 1.2Document2 pagesParasitology Short Quiz 1.2JAIRISH YZABELLE SALVADORNo ratings yet
- 571 - Immunization QuizDocument8 pages571 - Immunization QuizMichelle Dinser100% (3)
- Fix PPT Penyakit Kambing DombaDocument52 pagesFix PPT Penyakit Kambing DombaGaluh EnggarNo ratings yet
- Mycology Specimen CollectionDocument6 pagesMycology Specimen CollectionMaam ShaNo ratings yet
- Aerobic Gram-Negative BacilliDocument7 pagesAerobic Gram-Negative BacilliNhoz DoHoNo ratings yet
Tripod PDF
Tripod PDF
Uploaded by
banteng wibisonoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tripod PDF
Tripod PDF
Uploaded by
banteng wibisonoCopyright:
Available Formats
Conclusion. MT remains a serious form of tuberculosis which may compromise in each case.
in each case. Because both isolates were identified in AR State TB laboratory, a complex
the life-threatening. It was mainly seen in young nonvaccinated children but currently, contamination has been considered with no definite resolution at this time.
except among HIV-infected persons, it is more common among older persons who Conclusion. MDR-TB, due to both primary and secondary drug resistance, remains
experience more an endogenous reactivation. These findings emphasize the high effi- a threat in AR. Cooperation and communication between all levels of healthcare are cru-
cacy of BCG vaccination in developing countries to prevent MT. cial to avoid delayed diagnosis of MDR-TB. Timely DST via technologies like GeneXpert
Disclosures. All authors: No reported disclosures. and MDDR service at CDC is critical. Consultation from Centers of Excellence is vital in
the treatment of MDR-TB complicated by diabetes and HIV. Whole-genome sequencing
could provide clarity in the cluster with discordant DST patterns.
769. An Outbreak of Multidrug-Resistant Tuberculosis, Minnesota 2016–2017 Disclosures. All authors: No reported disclosures.
Malini Desilva, MD, MPH1; Nora Moore, MPH2; Dzung Thai, MPH1; Mary
Beth Grimm, MPH2; Nadya Sabuwala, RN, MPH1; Milayna Brueshaber,MPH
771. Drug Resistance Tuberculosis (DR-TB), Comorbidities and Risk Factors
NREMT-B1; Sarah Gordon, MPH1; Laura Andersen, DVM MS2; Victoria Hall,
Identified in a Prospective Multicenter Cohort Study in Indonesia
MPH1,3; Sean Buuck, MPH1; Cynthia Hickman, MPH1; Katie Stinebaugh, PhD, MPH1;
Erlina Burhan, Doctor1; Banteng Wibisono, Doctor2; Retna Indah, Doctor3; Gede
Benjamin Silk, MPH4; Kayla Raz, PhD, MPH4; Sarah Talarico, MD4; Jonathan Wortham,
Ketut Sajinadiyasa, Doctor4; Bambang Riyanto, Doctor5; Tutik Kusmiati, Doctor6 and
MPH5; Elisabeth Kingdon, PhD, RN, MPH, APHN-BC1; Gina Pistulka, MS2;
Nugroho Susanto, Doctor3 1Persahabatan Hospital, Jakarta Timur, Indonesia, 2Dr.
Krissie Guerard, PhD1; Lauren Cowan, PhD4; James E. Posey, MT (ASCP)4; Paula
Kariadi Hospital, Semarang, Indonesia, 3INA-RESPOND, National Institute of Health
M. Snippes Vagnone, MD, MPH6; Joel McCullough, MD2; Dean Tsukayama, MD
Resources and Development, Ministry of Health Indonesia, Jakarta Pusat, Indonesia,
MPH7; Rajal K. Mody, MPH8 and Kristen Ehresmann, MPH1; 1Infectious Disease 4
Sanglah Hospital, Denpasar, Indonesia, 5Dr. Sardjito Hospital, Yogyakarta, Indonesia,
Epidemiology, Prevention and Control Division, Minnesota Department of Health, Saint 6
Dr. Soetomo Hospital, Surabaya, Indonesia
Paul, Minnesota, 2Saint Paul – Ramsey County Public Health, Saint Paul, Minnesota,
3
Epidemic Intelligence Service Program, Centers for Disease Control and Prevention, Session: 70. Tuberculosis and Other Mycobacterial Infections
Atlanta, Georgia, 4Centers for Disease Control and Prevention, Atlanta, Georgia, Thursday, October 4, 2018: 12:30 PM
5
Respiratory Diseases Branch, Centers for Disease Control and Prevention, Atlanta,
Georgia, 6Minnesota Department of Health, St. Paul, Minnesota, 7Hennepin County Background. The numbers of patients with drug resistance TB (DR-TB) increased
Medical Center, Minneapolis, Minnesota, 8Division of State and Local Readiness, Office annually by over 20% globally in the last decade. However, data on the prevalence of DR-TB
of Public Health Preparedness and Response, CDC, Atlanta, Georgia in Indonesia are limited. The objective of this study to estimate the proportion of DR-TB in
new and previously treated TB cases, and to identify comorbidities and risk factors.
Session: 70. Tuberculosis and Other Mycobacterial Infections Methods. This study has been conducted at seven hospitals throughout Indonesia
Thursday, October 4, 2018: 12:30 PM since March 2017. Clinically TB patients ≥18-year-old were enrolled and followed until
6 months after treatment completed. Demography and clinical data were recorded;
Background. Multidrug-resistant tuberculosis (MDR TB) is more difficult to
sputum, blood, urine, and PBMC were collected at several time points. AFB smear,
treat and outcomes are worse than for drug-susceptible TB disease. MDR TB cases in
sputum culture, Xpert MTB/RIF, and drug sensitivity tests were performed. Drug
Minnesota increased from zero in 2015 to nine in 2016. Case investigations suggested
resistance TB is determined by Xpert MTB/RIF.
an outbreak. We describe the public health response, challenges of contact investiga-
Results. Of 151 enrolled patients, 103 (68%) were confirmed M. tuberculosis by
tions (CIs), and ongoing management of contacts.
Xpert MTB/RIF, and 47 (46%) were confirmed rifampicin resistance. The distribution
Methods. CDC performed whole-genome sequencing (WGS) to evaluate related-
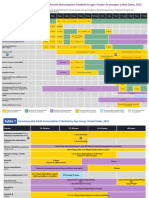
of DR-TB in each study site is shown in Figure 1. Among those with comorbidities
ness of MDR TB isolates. We conducted CIs for infectious cases. We created outbreak
(38%), comorbidity with diabetes (based on HbA1c level and diabetes history), HIV,
specific guidelines for screening and management of contacts, and partnered with var-
and cancer was 9%, 26%, and 7%. Demography, nutrition status, contact and treat-
ious agencies to increase MDR TB awareness.
ment history, and comorbidities are shown in Table 1. DR-TB primary infection con-
Results. WGS results were consistent with an MDR TB outbreak that included 10
tributes to 23% of DR-TB cases. Biomarkers that may predict treatment failure and
cases (70% pulmonary) as of April 2018. Limited provider awareness about TB contrib-
TB-genotyping are underway.
uted to delayed diagnoses. CIs identified 588 contacts; 8.7% (n = 51) of contacts had previ-
Conclusion. The proportion of DR-TB in both new and previously treated
ously documented positive TB infection test results, and 14% (n = 74) were newly positive
patients in our cohort was significantly higher than the estimated number from the
for TB infection (median age: 72 years). Eight cases were epidemiologically linked to one
WHO and Ministry of Health. TB is a serious threat for public health and mitigation
Hmong adult day center. Sixty-two contacts started a fluoroquinolone for latent MDR TB
plan must be implemented at all levels.
infection. Contacts who declined treatment began a 2-year clinical monitoring program.
Conclusion. In this outbreak, delayed diagnoses resulted in long infectious peri-
ods and hundreds of contacts. WGS results were consistent with recent transmission. Table 1: Demography, Nutrition Status, Contact History, TB Treatment History
We discovered adult day centers are an overlooked congregate setting. CIs were compli- and Comorbid Status
cated by limited public health funding and high underlying TB infection prevalence in
the affected community. Increased community and provider awareness and intensified
520 560 570 580 590 All
screening of contacts resulted in additional case finding and prevention interventions.
Disclosures. All authors: No reported disclosures. Demography
Age (Median, IQR) 38 (20) 41 (21) 42 (25) 37 (45) 22 (3) 40 (25)
Male (n, %) 9 (75) 16 (47) 26 (67) 9 (82) 4 (57) 64 (62)
770. Multi-Drug-Resistant Tuberculosis Cases in Arkansas in 2017: A Tale of Two BMI
Threats <18.5 7 (58) 17 (50) 20 (51) 5 (45) 5 (71) 54 (52)
Emily Weldon, BS; Naveen Patil, MD MHSA MA; Jan Voyles, BS; Sandra Chai, 18.5 to <25 5 (42) 13 (38) 13 (33) 5 (45) 2 (29) 38 (37)
MD; Marsha Majors, BSN, RN and Leonard Mukasa, MBChB PhD1; 1Arkansas ≥25 0 4 (12) 6 (15) 1 (10) 0 11 (11)
Department of Health, Little Rock, Arkansas Contact history with 2 (17) 1 (3) 8 (21) 2 (18) 2 (29) 15 (15)
TB patients
Session: 70. Tuberculosis and Other Mycobacterial Infections TB treatment history
Thursday, October 4, 2018: 12:30 PM New 10 (83) 12 (35) 13 (33) 10 (91) 5 (71) 50 (49)
Previously treated 2 (17) 22 (65) 26 (67) 1 (9) 2 (29) 53 (51)
Background. Multi-drug-resistant tuberculosis (MDR-TB) is a threat to TB elim- Comorbid
ination strategies worldwide. From 1998 to 2016, six cases of MDR-TB were reported HIV 2 (18) 0 0 2 (18) 0 4 (4)
in Arkansas. In 2017 alone, three cases were detected. We sought to describe the char- DM 1 (9) 14 (41) 13 (33) 0 1 (14) 29 (28)
acteristics of these cases to inform our MDR-TB prevention strategy in AR.
Methods. The surveillance database identified three MDR-TB cases in 2017.
A detailed review was done to define the demographics, clinical presentation, and
laboratory reports relating to drug susceptibility testing (DST), including molecular
detection of drug resistance (MDDR). A search was done in the Genotyping database
for genotype patterns of the patient isolates.
Results. All three cases were born outside the United States and developed active
disease after arrival in AR. Case 1, age 52, was born in the Marshall Islands, arrived
in 2016, and had a history of Type 2 diabetes. He developed MDR-TB in February
2017. Case 2, age 42, was born in Mexico, arrived over 20 years ago, and was HIV
positive. He developed TB in July 2016 with a pan-sensitive organism and completed
an intermittent treatment regimen. A second TB episode with matching genotype but
different drug sensitivities occurred in April 2017, less than 4 months after treatment
completion, and was considered treatment failure. Case 3, age 56, was born in the
Philippines, arrived in 1990, and was reportedly treated for latent TB infection in 1993
with 6 months of isoniazid. She visited the Philippines April–May 2017 and developed
MDR-TB in October 2017. Her isolate was in cluster with a case in Oklahoma who
came from Mexico in 2006 and was admitted in an AR hospital with a pan-sensitive
organism. There are no epidemiological links between the two cases; only one isolate Disclosures.All authors: No reported disclosures.
S276 • OFID 2018:5 (Suppl 1) • Poster Abstracts
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5824)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- PLE 2019 - Microbiology Questions and Answer KeyDocument16 pagesPLE 2019 - Microbiology Questions and Answer Keydickson100% (4)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Motivation Letter Utrecht UniversityDocument2 pagesMotivation Letter Utrecht UniversityAjit Antony50% (2)
- Bacteria Notes SketchyDocument3 pagesBacteria Notes SketchyJayNo ratings yet
- Measles PamphletDocument2 pagesMeasles Pamphletapi-384459604No ratings yet
- GOLD 2021 Teaching Slide Set v102 12nov2020Document58 pagesGOLD 2021 Teaching Slide Set v102 12nov2020banteng wibisonoNo ratings yet
- A13v12n3 PDFDocument8 pagesA13v12n3 PDFbanteng wibisonoNo ratings yet
- TNF-alpha Levels in Serum and Mononuclear Cell Lysate of Nigerian Tuberculosis Patients at DiagnosisDocument5 pagesTNF-alpha Levels in Serum and Mononuclear Cell Lysate of Nigerian Tuberculosis Patients at Diagnosisbanteng wibisonoNo ratings yet
- Human Anatomy and Physiology SyllabusDocument5 pagesHuman Anatomy and Physiology Syllabusbanteng wibisonoNo ratings yet
- Γ And Tnf-Α Levels: Ir - Perpustakaan Universitas AirlanggaDocument1 pageΓ And Tnf-Α Levels: Ir - Perpustakaan Universitas Airlanggabanteng wibisonoNo ratings yet
- Idsa GuidelineDocument50 pagesIdsa GuidelinenilnaNo ratings yet
- Brain Tumors With Review of Literature: Immunohistochemistry or Biomarkers Versus HistomorphologyDocument5 pagesBrain Tumors With Review of Literature: Immunohistochemistry or Biomarkers Versus Histomorphologybanteng wibisonoNo ratings yet
- Fungi MedicalDocument25 pagesFungi Medicalbanteng wibisono100% (1)
- Pathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun MengDocument20 pagesPathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun Mengbanteng wibisonoNo ratings yet
- Dimorphic Fungi: Prabin Shah BSCMLT, MSC (Biochemistry)Document49 pagesDimorphic Fungi: Prabin Shah BSCMLT, MSC (Biochemistry)banteng wibisonoNo ratings yet
- Brain CancerDocument7 pagesBrain Cancerbanteng wibisonoNo ratings yet
- Selective MediaDocument10 pagesSelective Mediaprincess_likemist4No ratings yet
- POSTER PRESENTATION PDF Aja PDFDocument1 pagePOSTER PRESENTATION PDF Aja PDFShilpa MishraNo ratings yet
- Her Verte Tal 2017Document12 pagesHer Verte Tal 2017Abhishek BanerjeeNo ratings yet
- S60 - Morvinandan Diagnostic Centre LLP: Patientreportscsuperpanel - General - Box - SC (Version: 6)Document8 pagesS60 - Morvinandan Diagnostic Centre LLP: Patientreportscsuperpanel - General - Box - SC (Version: 6)Kapil NagpalNo ratings yet
- Giardia & Giardiasis: (Intestinal Flagellate)Document22 pagesGiardia & Giardiasis: (Intestinal Flagellate)Naing Lin SoeNo ratings yet
- ABO Blood GroupingDocument10 pagesABO Blood GroupingJhon WickNo ratings yet
- MCDB 290b SyllabusDocument2 pagesMCDB 290b SyllabusLalalalaPineapplesNo ratings yet
- Hobbs 2016Document18 pagesHobbs 2016Jônatas CavaliniNo ratings yet
- VaccinationDocument24 pagesVaccinationNitesh GandhiNo ratings yet
- Cutaneous Abscess Furuncles and CarbuclesDocument25 pagesCutaneous Abscess Furuncles and Carbuclesazmmatgowher_1219266No ratings yet
- Manual of Infection Control Procedu PDFDocument365 pagesManual of Infection Control Procedu PDFanon_789115535100% (1)
- Biofilm in OtorhinolaryngologyDocument10 pagesBiofilm in OtorhinolaryngologyMohammed SahibNo ratings yet
- Culture Media CombinedDocument131 pagesCulture Media CombinedEmit Rosary PenetranteNo ratings yet
- Pediatric Community-Acquired Pneumonia Clinical Guideline PDFDocument1 pagePediatric Community-Acquired Pneumonia Clinical Guideline PDFJohn Vincent Dy OcampoNo ratings yet
- A. Chlorophyll ADocument16 pagesA. Chlorophyll AKishor SarodeNo ratings yet
- CertificateDocument1 pageCertificatenazmulNo ratings yet
- Materi 16. Peranan Manajemen RS - PGADocument25 pagesMateri 16. Peranan Manajemen RS - PGAAri Wibowo KastaNo ratings yet
- 2019 Book PolymyxinAntibioticsFromLaboraDocument364 pages2019 Book PolymyxinAntibioticsFromLaboraDaniel JiménezNo ratings yet
- 2parasitology AssignmentDocument4 pages2parasitology AssignmentVictor PaulNo ratings yet
- Resume Tutorial A Skenario 1 Blok 14Document74 pagesResume Tutorial A Skenario 1 Blok 14Istaz MaulanaNo ratings yet
- Natural History of DiseaseDocument31 pagesNatural History of Diseasegabo dasNo ratings yet
- Parasitology Short Quiz 1.2Document2 pagesParasitology Short Quiz 1.2JAIRISH YZABELLE SALVADORNo ratings yet
- 571 - Immunization QuizDocument8 pages571 - Immunization QuizMichelle Dinser100% (3)
- Fix PPT Penyakit Kambing DombaDocument52 pagesFix PPT Penyakit Kambing DombaGaluh EnggarNo ratings yet
- Mycology Specimen CollectionDocument6 pagesMycology Specimen CollectionMaam ShaNo ratings yet
- Aerobic Gram-Negative BacilliDocument7 pagesAerobic Gram-Negative BacilliNhoz DoHoNo ratings yet