Professional Documents
Culture Documents
Onset Depression Health Related Risc Dztp2
Onset Depression Health Related Risc Dztp2
Uploaded by
Levente DobaiOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Onset Depression Health Related Risc Dztp2
Onset Depression Health Related Risc Dztp2
Uploaded by
Levente DobaiCopyright:
Available Formats
See
discussions, stats, and author profiles for this publication at: http://www.researchgate.net/publication/14319481
Depression and Risk for Onset of Type II
Diabetes: A prospective population-based study
ARTICLE in DIABETES CARE · NOVEMBER 1996
Impact Factor: 8.42 · DOI: 10.2337/diacare.19.10.1097 · Source: PubMed
CITATIONS READS
394 77
5 AUTHORS, INCLUDING:
Joseph Gallo Daniel Ford
Johns Hopkins Bloomberg School of Public … Johns Hopkins University
141 PUBLICATIONS 6,760 CITATIONS 198 PUBLICATIONS 12,052 CITATIONS
SEE PROFILE SEE PROFILE
Available from: Joseph Gallo
Retrieved on: 24 September 2015
N A L A R T I C L E
Depression and Risk for Onset of
Type II Diabetes
A prospective population-based study
WILLIAM W. EATON, PHD LAURIE PRATT, BA not suggest strong differences between
HAROUTUNE ARMENIAN, MD, DRPH DANIEL E. FORD, MD, MPH subtypes in the cross-sectional relation-
JOSEPH GALLO, MD, MPH ship of diabetes to depression.
The relationship of age to diabetes and
depression is important since the age of
onset is related to the subtype of diabetes.
Depression has its peak period of onset in
OBJECTIVE — To determine whether depression is associated with an increased risk for
the early adult years (12). A review of 17
onset of diabetes.
studies of children and adolescents with
RESEARCH DESIGN A N D M E T H O D S — In 1981, a total of 3,481 household-resid- type I diabetes concluded that the findings
ing adults participated in the Epidemiologic Catchment Area (ECA) Program survey at the concerning the association of psychiatric
East Baltimore site. A follow-up of that cohort after 13 years completed 1,897 interviews, disorders to diabetes were equivocal (13).
amounting to >72% of survivors. In 1981, depression was assessed with the National Insitutes However, one study found a higher rate of
of Mental Health (NIMH) Diagnostic Interview Schedule and diabetes, by self-report. This "introversive" disorders (i.e., anxiety and
prospective analysis focused on subjects at risk for onset of diabetes by removing from the depression) among insulin-dependent dia-
analysis individuals with diabetes in 1981. betic subjects (14). Most studies adjusted
for age but none reported whether there
RESULTS — There were 89 new cases of diabetes among 1,715 individuals at risk, yielding was a statistical interaction between age,
a 13-year cumulative incidence of diabetes of 5.2%. In logistic models, major depressive dis-
order, but not milder forms of depression or other forms of psychiatric disorder, predicted the
diabetes subtype, and the association
onset of diabetes (estimated relative risk, 2.23; 95% CI 0.90-5.55). Controlling for age, race, between diabetes and depression. Thus,
sex, socioeconomic status, education, use of health services, other psychiatric disorders, and there is nothing in the literature to suggest
body weight did not weaken the relationship. differences between age groups in the rela-
tionship of diabetes to depression.
CONCLUSIONS — Major depressive disorder signals increased risk for onset of type II dia- The cross-sectional relationship of
betes. Limitations of the findings arise from the difficulty in determining temporal order with depression to diabetes could arise in sev-
two chronic conditions, even when the temporal order of measurement is clear. In addition, eral ways. There may be a common neu-
even though control variables were introduced for the use of health services, it is possible that roendocrine basis that underlies or pre-
the treatment for depression led to an earlier diagnosis of diabetes in this sample. cedes both disorders (14,15). It may be
that this common basis is stimulated by
an episode of depression or the onset of
T
here has been speculation for a long samples containing both type I and type II diabetes so that the direction of causation
time that psychopathology and diabetic subjects, the association with could be either from diabetes to depres-
specifically depression are related to depression did not differ by type of dia- sion, from depression to diabetes, or both.
the onset and course of diabetes (1-5). betes (8,9). Wing et al. (10) reported that It could be that a depressive episode pro-
Most studies of diabetes and depression depressive symptomatology was more duces a bodily change, such as in the
have focused on adults, and results would common among type II diabetic subjects immune system (16), that raises the risk
be expected to be dominated by type II than control subjects. A study of adults for diabetes. The cross-sectional relation-
diabetes, since it is more prevalent among with type I diabetes who were awaiting ship could arise because diabetes, similar
adults. Seven out of eight controlled stud- pancreas transplant also found a higher to other severe medical conditions (17,18),
ies reviewed by Gavard et al (4) that were than expected rate of depression in the causes a psychological reaction to the stress
limited to type II diabetic subjects showed diabetic subjects than in the control sub- of illness or to the threat of loss of life or
a positive relationship between diabetes jects (11). In summary, the research litera- function as a consequence of diabetes
and depression, as did two later studies of ture has not focused on the subtypes of or its complications (5,6,19). Finally,
type II diabetic subjects (6,7). In studies of diabetes, but the evidence presented does depression may be related to a variety of
confounding factors, such as obesity,
exercise, and use of medications, that
From the Johns Hopkins University, Baltimore, Maryland. could increase the risk for diabetes and
Address correspondence and reprint requests to William W. Eaton, PhD, School of Public Hygiene and lead to poor control after the onset of dia-
Public Health, Department of Mental Hygiene, Johns Hopkins University, 624 N. Broadway, Baltimore, MD betes (8,20-22). Our research examines,
21205-1999.
Received for publication 9 August 1995 and accepted in revised form 16 May 1996.
for the first time, the relationship of clini-
DIS, Diagnostic Interview Schedule; ECA, Epidemiologic Catchment Area; NIMH, National Insitutes of cal depression to diabetes in a prospec-
Mental Health; OR, odds ratio. tive fashion.
DIABETES CARE, VOLUME 19, NUMBER 10, OCTOBER 1996 1097
Depression and type II diabetes
RESEARCH DESIGN AND Table 1—Comparison of 1981 cohort with 1993-1994 sample
METHODS— The Epidemiologic
Catchment Area (ECA) Program was a
1981 cohort 1981 survivors 1993-1994 interviewed
national effort to assess the prevalence and
incidence of specific psychopathological Men
disorders by interviewing >20,000 per- Sample size 1,322 951 700
sons in five cities who were over 18 years 18-29 years 27.2 36.1 35.0
of age (23,24). The target population for 30-44 years 23.4 30.6 29.0
the Baltimore site of the ECA in 1981 was 45-64 years 22.9 21.9 24.0
household residents of East Baltimore, an 65+ years 26.6 11.5 12.1
area of 175,000 adult inhabitants. In 100.1 100.1 100.0
1981, 3,481 individuals were selected Women
based on probability sampling methods Sample size 2,159 1,683 1,197
and interviewed in their households, with 18-29 years 26.2 33.2 29.5
a completion rate of 82%. Details of the 30-44 years 22.3 27.6 28.3
ECA method are available elsewhere (25). 45-64 years 25.0 24.8 26.7
The instrument used in the ECA pro- 65+ years 26.5 14.5 15.5
gram was the NIMH Diagnostic Interview 100.0 100.1 100.0
Schedule (DIS) (26). The DIS is a highly Total sample 3,481 2,634 1,897
structured survey interview that is Data are n or %.
designed to produce diagnoses of specific
mental disorders according to criteria
established by the American Psychiatric
Association (27). In the DIS, close-ended are assessed via the DIS. But the literature and interviewing. These individuals
(mostly yes or no) questions are asked by on diabetes and depression does not indi- included males and females and a range of
interviewers who have had ~ 1 week of cate whether the precise criteria for estab- ages >18 (Table 1). Credible information
training but no clinical experience. To be lishing the presence or absence of a psy- on death (in most cases, a positive match
rated as a "plausible psychiatric symptom" chiatric disorder yields the strongest rela- from the National Death Index) was avail-
that contributes to diagnosis, the report of tionship to risk for diabetes onset; thus, a able on 847 respondents who died during
the symptom must meet criteria of impair- depression syndrome below the threshold the follow-up period. The address of 437
ment (i.e., seeking help from a profes- of diagnosis—or simply dysphoria itself— individuals of the 3,481 could not be
sional, taking medication more than once, could possibly be related to onset of dia- established, and 300 refused to participate.
or having one's life or activities disrupted betes under any of the possible theoretical Mortality was a significant factor in the
"a lot"). The respondents must state that models discussed above. Therefore, indi- 13-year follow-up, as shown in Table 1.
the symptom was not always caused by cators of depressive syndrome and dys- The bulk of tracing and interviewing was
drugs, alcohol, medical illness, or injury. A phoria as used in prior ECA research stud- completed in 1993 and 1994, with a hand-
computer algorithm combines the ies (29) are entertained as predictors of ful of respondents being located and inter-
responses into diagnostic categories. The diabetes onset. The DIS includes anxiety viewed in 1995 and 1996. By the end of
symptoms and diagnoses have a temporal and other disorders that have been the field work in 1996, over 72% of the 2,652
dimension, including the report that a subject of prior research on diabetes. The survivors had been located and inter-
symptom or diagnosis has ever occurred wide range of psychopathologies assessed viewed. Respondents with completed
over the lifetime of the respondent. This in 1981 by the DIS allows the examination interviews did not differ appreciably in
"lifetime prevalence" report of the diagno- of many other possible predictors in an terms of age and sex with those survivors
sis of a major depressive disorder is the exploratory mode of analysis. who were not interviewed. In another
subject of analysis here. Studies of the reli- The 1981 ECA surveys in Baltimore analysis (30), it was shown that certain
ability and validity of the DIS show that it included questions on diabetes that were aspects of psychopathology, such as sub-
has good reliability and acceptable validity drawn from the Health Interview Survey stance abuse and antisocial behavior, are
(26). The DIS has been used in some dia- that was conducted by the National Center related to attrition among survivors, but
betes research (8), including an analysis of for Health Statistics. The questions were: 1) that depression is not related to attrition.
diabetes in another ECA site in Los Ange- Have you ever had high sugar or diabetes? For 1993-1996, 1,897 respondents com-
les (28). 2) Do you have diabetes now? and 3) Are pleted interviews.
Depression denotes sad mood (dys- you being treated by a health professional The follow-up survey contained more
phoria); it also denotes a psychiatric syn- for diabetes? Positive answers to one or detailed questions on diabetes, since it was
drome or disorder involving sad mood more of these questions were used to anticipated that there would be ~100 per-
and the accompanying somatic symptoms define a subset of individuals who already sons who had become diabetic during the
that surpass a threshold of clinical impor- had diabetes and, therefore, were not at follow-up period. The pertinent section of
tance. The operational criteria for the psy- risk for onset of diabetes. Subjects not at the questionnaire included the same ques-
chiatric disorder, major depressive disor- risk were excluded from the analyses. tions as asked in 1981 and 1982, with
der, are laid out in the Diagnostic and Statis- In 1993 and 1994, the Baltimore additional questions on the age of onset,
tical Manual of Mental Disorders (27) and cohort of 3,481 was the target for tracing gestational diabetes, treatment, complica-
1098 DIABETES CARE, VOLUME 19, NUMBER 10, OCTOBER 1996
Eaton and Associates
Table 2—Cumulative incidence of diabetes between 1981 and 1993-1994 by age and sex, substantially higher in middle-aged and
Baltimore ECA follow-up elderly persons than in young adults
(Table 2).
Estimation of annual incidence rates
Men Women Total
allows further comparison with other sim-
Age in 1981 (years) ilar surveys. In Table 3, the annual inci-
18-29 2.1 (5/239) 3.7 (12/327) 3.0 (566) dence is estimated approximately by
30-44 4.2 (8/189) 3.8(11/304) 4.0 (503) adjusting the age categories and dividing
45-64 6.0 (9/149) 9.4 (26/276) 8.2 (425) age- and sex-specific estimates by 13,
65+ 6.9 (5/72) 8.1 (12/149 7.7(221) allowing a rough comparison with rates
Total 4.2 (27/649) 5.8(62/1,066) 5.2(89/1,715) presented in work of the National Dia-
Data are % (frequency). Individuals not at risk, 103; missing, 79; total, 1,897. betes Data Group (33). The annual age-
specific incidence rates per 1,000 individ-
uals in the population are quite close in
tions, and the use of health care services. lence of DIS-Diagnostic and Statistical the two studies, but the ECA data (weakly)
New cases of diabetes were identified by Manual (DSM-III) major depressive disor- suggest an increased rate for females, a
positive answers to the questions on dia- der in the 148 diabetic respondents inter- trend not seen in the national data.
betes, combined with a negative answer to viewed during the 1993-1996 period was There were 76 Baltimore ECA follow-
the question on gestational diabetes. Eight 6.1%, compared with 5.3% in the 1,600 up respondents who, in 1981, met the cri-
individuals reported an age of onset nondiabetic respondents. This cross-sec- teria for the diagnosis of major depressive
younger than their age in 1981; they were tional association was not as strong as it disorder and had complete data on dia-
eliminated from the group of new cases in has been found to be in some prior stud- betes in the follow-up. Among these there
order to make the definition of incident ies, reviewed above, wherein the preva- were 6 new cases of diabetes (7.9%), com-
cases as conservative as possible. Of the lence of depression was ^50% higher in pared with 80 new cases of diabetes (5.0%)
1,897 interviews, 98 were conducted with diabetic subjects than in nondiabetic sub- among the 1,604 respondents who did not
informants, and there were 6 incident jects. However, age adjustment is required meet criteria for major depressive disorder
cases of diabetes reported by these infor- to compare rates because depression is in 1981. The relative risk for this two-by-
mants that were included in the analysis. more common in young adults and dia- two cross-classification is 1.58, with 95%
In this sample, which had a minimum age betes, in older adults. When the age range confidence interval of 0.71-3.51.
of 18 in 1981, there were two respondents is restricted to those >54 years, the Major depressive disorder has a mod-
who reported ages of onset below the age results appeared similar to previous stud- erate-sized relationship to the risk of
of 30 (22 and 28 years, respectively). ies. For example, among the 92 individu- becoming diabetic (Table 4). The table
A series of multiple logistic regressions als with diabetes who were >54 years of includes three hierarchical models that
was estimated to assess the effects of age in 1993-1996, the prevalence of show the independent effects of major
depression on diabetes while controlling major depressive disorder was 3.3%, potential confounding and mediating
for factors that might confound the rela- compared with 2.2% in the 598 nondia- variables. In Table 4, odds ratios (ORs)
tionship. First, a best fitting model for betic respondents. with values close to 1.0 show no or weak
sociodemographic variables related to dia- There were 89 new cases of diabetes association; ORs >1.0 show a direct rela-
betes or to depression was estimated, test- among 1,715 individuals at risk. The tionship; ORs <1.0 reveal a protective
ing variables one by one and then exhaust- cumulative incidence, or proportion of the relationship. Reference categories for sex,
ing all combinations of variables (i.e., not at-risk group having a first onset (31), was age, and race are shown with ORs of 1.0;
using opportunistic selection procedures). 5.2% (Table 2). This ECA incidence com- the reference category for depressive dis-
The variables examined (age, sex, race, pares roughly with a 16-year cumulative order consists of those in the sample who
and socioeconomic status) were those incidence of 7.9% in the NHANES I fol- do not meet the criteria for diagnosis. The
related to diabetes or depression in either low-up study (32). Incidence was slightly left-most model in Table 4 shows the rela-
our data or prior research. Then, an initial higher in women than in men, and was tionship of age, sex, and race to the onset
depression model focused on major
depressive disorder; additional models, Table 3—Annual incidence of diabetes per 1,000"
estimated separately, used a variety of
measures of depression to assess whether Baltimore 1981 and 1993-1994 U.S. 1979-1981t
the degree of depression affected the rela-
Age (years)^ Men Women Total Men Women Total
tionship. Consistent with interpretations
of some earlier work in other samples 18-24 0.3 0.5 0.4
(29), the findings were strongest for major 25-44 2.4 2.5 2.4 1.6 2.4 2.0
depressive disorder; the models for that 45-54 3.8 6.9 5.8 6.2 2.7 4.4
variable are presented below. 55-64 3.9 7.3 6.0 6.2 5.6 5.9
65-74 6.1 6.8 6.5 4.1 5.0 4.6
RESULTS— Before considering the 75+ 2.7 5.6 5.0 4.2 6.0 5.4
prospective results the cross-sectional * Annual incidence obtained by dividing cumulative incidence from 1981 through 1993/1994 by 13.
associations were examined. The preva- TAdapted from Table 2 in Everhart et al. (33). TAge at midpoint of follow-up.
DIABETES CARE, VOLUME 19, NUMBER 10, OCTOBER 1996 1099
Depression and type II diabetes
Table 4—Predictors of diabetes onset, Baltimore ECA follow-up, logistic regression model interview in 1981 (data not shown), but
adjusted odds ratios neither of these variables had significant
parameters in the model, and none of the
adjustments had any appreciable effect on
Predictors Model 1 Model 2 Model 3
the parameter for depression.
Male (reference) 1.00 1.00 1.00 Other types of psychopathology were
Female 1.29 1.20 1.08 investigated in the same manner as
White (reference) 1.00 1.00 1.00 depression. These included depression
Black 1.49* 1.50* 1.27 defined at different levels of severity. Rela-
tive risk, estimated via the OR, for the var-
18-29 years (reference) 1.00 1.00 1.00 ious measures of depression from mildest
30-44 years 1.34 1.33 1.23 to most severe included: dysphoria
45-64 years 3.05* 3.09* 3.15* (defined as feeling sad or depressed nearly
^ 6 5 years 2.98* 3.00* 4.24* all the time for 2 weeks or more; OR =
Major depressive disorder (1981) — 2.05 2.23* 1.02, 95% CI 0.61-1.68); depression syn-
BMI 1.09* drome (defined as dysphoria clustered
with symptoms in at least three symptom
•P < 0.1; fP< 0.01.
groups in criterion B of the DSM-III defin-
ition; OR = 1.02, 95% CI 0.50-2.07);
of diabetes, with a significantly higher OR the high end of the range.) In a logistic major depressive disorder without exclu-
for older age-groups, as suggested in model by itself, BMI was associated with sions (defined as dysphoria clustered
Tables 2 and 3. This basic sociodemo- an 8% increase in the risk for onset of dia- with symptoms in at least four of the cri-
graphic model was also estimated with betes (OR= 1.08,95% CI 1.06-1.12). The terion B symptom groups and not disal-
measures of socioeconomic status, includ- effect of BMI is not changed greatly by lowed either for reason of recent grief or
ing the Nam-Powers index (34), and entry into the model with depression; as organic mental disorder; OR = 1.83, 95%
grade of schooling achieved forced into shown in the right-most column of Table CI 0.74-4.53); and major depressive dis-
the model, both together and singly. 4, each unit of BMI raised the odds of order (defined as major depressive disor-
These variables of socioeconomic status becoming diabetic by 9% over the follow- der not attributable to grief or other psy-
never had anything larger than a trivial up. However, the estimated odds of chopathology and that led to seeking
effect and were not included in further becoming diabetic associated with major treatment or the disruption of normal life
analyses. Sex was retained throughout the depressive disorder grew slightly stronger or activities; OR = 2.23 [as in Table 4],
analyses, even though its effect was not when BMI was included in the model 95% CI 0.90-5.55). ORs for other types
significant, because of its known relation- (Table 3; OR = 2.23, 95% CI 0.90-5.55). of psychopathology, estimated in logistic
ship to depression. Race was retained The level of significance with a conserva- models analogous to model 3 with adjust-
because of its relationship to treatment for tive two-tailed approach is P = 0.084, indi- ments for age, sex, race, and BMI, were:
diabetes (35). cating that the strength of relationship DIS/DSM-III panic disorder, 1.07 (95%
The second model, in the middle col- would occur less than 9 times out of 100 CI 0.14-8.33); DIS/DSM-III phobia,
umn of Table 4, shows that major depres- purely by chance. 0.84 (95% CI 0.48-1.48); DIS/DSM-III
sive disorder was associated with an Another possible explanation for the alcohol abuse or dependence, 0.66
increased risk of becoming diabetic by a relationship between depression and the (95% CI 0.28-1.57); and DIS/DSM-III
factor of about two (OR = 2.05). This onset of diabetes is ascertainment bias. For obsessive-compulsive disorder, 1.23 (95%
moderately strong OR is different from the example, it may be that depressive indi- CI 0.37-4.18). Models were also esti-
reference value of 1.0 at a marginal level of viduals are more likely to obtain health mated that included major depressive dis-
significance (P = 0.113). care, either in order to receive treatment order and many other types of psy-
Even though the design is prospective, for depression or because they are more chopathology simultaneously and a vari-
many confounding variables may explain likely to seek treatment in general for ordi- able indicating the number of different
the relationship between depression and nary or trivial somatic symptoms. Diabetic psychiatric disorders for which the
the onset of diabetes. The most important individuals may be more likely to be respondent met diagnostic criteria. These
possibility is the body weight. Being over- noticed by a physician and to be reported other models are not shown because the
weight is associated with onset of diabetes by the respondent in the follow-up inter- parameters were trivial in size, were not
(33), and depressed individuals some- view. To attempt to adjust for this possibil- statistically significant, and did not affect
times suffer from problems with appetite ity, the third model was estimated with the estimates for major depressive disor-
and weight (both too much appetite and measures of the use of health services in der. Thus, no other area of psychopathol-
weight gain and too little appetite and 1981, such as whether the respondent ogy had findings as strong as for major
weight loss). Therefore, BMI was esti- reported having a usual source of health depressive disorder.
mated from height and weight as reported care and the number of medical visits
by the respondent in the follow-up. The made in the 6 months prior to the 1981 C O N C L U S I O N — I n 1684, Thomas
BMI ranged from 15.2 to 85.8 kg/m2, with interview. Subjects with depression were Willis wrote about diabetes: "Sadness, or
a mean of 27.3 kg/m2. (A single individual more likely to have seen a medical care long sorrow . . . and other depressions
who reported weighing 514 lb generated provider in the 6 months prior to the and disorders of the animal spirits, are
1100 DIABETES CARE, VOLUME 19, NUMBER 10, OCTOBER 1996
Eaton and Associates
used to generate or foment this morbid types of diabetes. The prospective findings and women with type I and type II dia-
disposition" (cited in ref. 15). The data reported here pertain to type II diabetes. betes mellitus. Manuscript, 1996
presented above address, for the first These results suggest the direction of 10. Wing R, Marcus M, Blair E, Epstein L, Bur-
time, Willis' idea with the same precision influence from depression to diabetes, but ton L: Depressive symptomatology in
of temporal orientation as his conception. they should not be extrapolated to type I obese adults with type II diabetes. Diabetes
Care 13:170-171, 1990
This prospective study lends support to diabetes. The research literature is now
11. Popkin M, Callies A, Lentz R, Colon E,
the hypothesis that antecedent depression reaching the stage in which distinctions
Sutherland D: Prevalence of major depres-
raises risk for future onset of diabetes. between types of diabetes and age ranges sion, simple phobia, and other psychiatric
This study contrasted major depressive of samples are increasingly important in disorders in patients with long-standing
disorder with milder depression and with furthering understanding of the direction type I diabetes mellitus. Arch Gen Psychia-
other aspects of psychopathology for of causality and possible causal mecha- try 45:64-68,1988
which no such prospective relationship nisms in the association of diabetes and 12. Eaton WW, Kramer M, Anthony JC, Dry-
was shown. The data suggest that reactive depression. For example, the cross-sec- man A, Shapiro S, Locke BZ: The inci-
depression is unlikely as a total explana- tional relationship of depression to dia- dence of specific DIS/DSM III mental dis-
tion for the cross-sectional association of betes in adolescence, if it exists (13,14), orders: data from the NIMH Epidemio-
diabetes and depression. could possibly occur because the onset of logic Catchment Area Program. Acta
Psychiatr Scand 79:163-178, 1989
An important limitation of this work is diabetes in childhood or adolescence con-
13. Blanz B, Rensch-Reimann B, Eritz-Sig-
the problem of undetected diabetes. A tributes to the risk for onset of mild reac- mund D, Schmidt M: IDDM is a risk factor
recent estimate is that as many as 50% of tive depression, as distinct from the rela- for adolescent psychiatric disorders. Dia-
diabetic subjects who would be diagnosed tionship demonstrated in this analysis betes Care 16:1579-1587, 1993
by hemoglobin assay or glucose challenge where severe forms of depression were 14. Barglow P, Hatcher R, Edidin D, Sloan-
do not report having the illness (35). The associated with an elevated risk for the Rossiter D: Stress and metabolic control in
implications for this prospective design are onset of diabetes later in life. These possi- diabetes: psychosomatic evidence and
that some of those designated "at risk" for bilities can be explored in future longitu- evaluation of methods. Psychosom Med
diabetes onset may have already had dinal research. 46:127-144, 1984
15. Geringer E: Affective disorders and dia-
onset. Factors that predict whether an
betes mellitus. In Neuropsychological and
individual has undiagnosed diabetes (i.e., Behavioral Aspects of Diabetes. Holmes C,
age, race, and sex, as in ref. 36) were Acknowledgments— This paper was sup- Ed. New York, Springer-Verlag, 1990.
adjusted for in this analysis or had no ported by National Institutes of Mental Health 16. Herbert TB, Cohen S: Depression and
effect on the depression or diabetes OR. grant MH 47447. The paper has benefited from immunity: a meta-analytic review. Psycho/
But it is possible that undetected onset the comments of anonymous reviewers. Bull 113:472-486,1993
could have elevated the prevalence of 17. Rodin G, Voshart K: Depression in the
depression before the baseline interview in medically ill: an overview. AmJ Psychiatry
1981, thus contributing to the apparent References 143:696-705, 1986
incidence of diabetes among depressive 1. Hauser S, Pollets D: Psychological aspects 18. Moidin S, Scheftner W, Ric J, Nelson E,
of diabetes mellitus: a critical review. Dia- Knesvich M, Akiskal H: Association
subjects versus nondepressive subjects.
betes Care 2:227-232, 1979 between major depressive disorder and
This possibility suggests that certain 2. Dunn S, TurtleJ: The myth of diabetic per- physical illness. Psychol Med 2:755-761,
symptoms shared by diabetic subjects and sonality. Diabetic Care 4:640-646, 1981 1993
depressive subjects, such as fatigue, 3. Lustman PJ, Amado H, Wetzel RD: 19. Lloyd CE, Matthews KA, Wing RR, Orchard
should be more common among new Depression in diabetics: a critical TJ: Psychosocial factors and complications
cases of diabetes, even before the apparent appraisal. Compr Psychiatry 24:65-74, of IDDM: The Pittsburgh Epidemiology of
onset of diabetes in 1981. The data, how- 1983 Diabetes Complications Study, VII. Dia-
ever, do not show this pattern. For exam- 4. Gavard J, Lustman PJ, Clouse R: Preva- betes Care 15:166-172, 1992
ple, among 86 new cases of diabetes with lence of depression in adults with diabetes. 20. Mazze R, Lucido D, Shamoon H: Psycho-
data on self-reported fatigue (i.e., DIS Diabetes Care 16:1167-1178, 1993 logical and social correlates of glycemic
5. Jacobson A: Depression and diabetes. Dia- control. Diabetes Care 7:360-366, 1984
question 79), 14.0% reported fatigue;
betes Care 16:1621-1624, 1993 21. Wilson W, Aiy D, Biglan A, Glasgow E,
among the 1,595 at-risk subjects who did 6. Leedom L, Meehan W, Procci W, Zeidler A: Toobert D, Campbell D: Psychosocial pre-
not become diabetic and had good data on Symptoms of depression in patients with dictors of self-care behaviors (compliance)
fatigue, 13.6% reported fatigue. Unrecog- type II diabetes mellitus. Psychosomatics and glycemic control in non-insulin-
nized diabetes could not reasonably affect 32:280-286,1991 dependent diabetes mellitus. Diabetes Care
depression through a reaction to the dia- 7. Palinkas L, Barrett-Connor E, Wingard D: 9:614-622, 1986
betes, which suggests that, if undiagnosed Type 2 diabetes and depressive symptoms 22. Eaton W, Mengel M, Mengel L, I .arson D,
diabetes explains the longitudinal associa- in older adults: a population-based study. Campbell R, Montague R: Psychosocial
tion between diabetes and depression, the DiabetMed 8:439-532, 1991 and psychopathologic influences on man-
effect is mediated by factors that are not 8. Lustman P, Griffith L, Clouse R, Cryer P: agement and control of insulin-dependent
Psychiatric illness in diabetes mellitus: diabetes, bit] Psychiatry Med 22:105-117,
psychological.
relationship to symptoms and glucose 1992
The literature on diabetes and depres- control. J Nerv Ment Dis 174:736-742, 23. Eaton W, Regier D, Locke B, Taubc C: The
sion reveals cross-sectional associations 1986 Epidemiologic Catchment Area Program
across the span of ages from adolescence 9. Samson J, de Groot M, Jacobson A: of the NIMH. Public Health Rep
through adult life and including both sub- Comorbid psychiatric diagnoses in men 96:319-325, 1981
DIABETES CARE, VOLUME 19, NUMBER 10, OCTOBER 1996 1101
Depression and type II diabetes
24. Regier D, Myers J, Kramer M, Robins L, tive, substance use and anxiety disorders sample: The NHANES I Epidemiologic
Blazer D, Hough R, Eaton WW Locke BZ: in persons with arthritis, diabetes, heart follow- up study. Am J Epidemiol
The NIMH Epidemiologic Catchment Area disease, high blood pressure, or chronic 138:826-839,1993
Program: historical context, major objec- lung conditions. Gen Hosp Psychiatry 33. Everhart J, Knowler W, Bennett P: Inci-
tives, and study design. Arch Gen Psychiatry 11:320-327,1989 dence and risk factors for noninsulin-
41:934-941,1984 29. Anthony J, Petronis K: Suspected risk fac- dependent diabetes. Diabetes in America:
25. Eaton W Kessler L, Eds.: Epidemiologic tors for depression among adults 18-44 Diabetes Data Compiled 1984. Bethesda,
Field Methods in Psychiatry: The NIMH Epi- years old. Epidemiology 2:123-132,1991 MD, National Institutes of Health, 1985,
demiologic Catchment Area Program. 30. Badawi M, Eaton WW, Myllyluoma J, p. IV1-IV35 (Pub. 85-1468)
Orlando, Academic Press, 1985 Gallo J: Psychopathology and Attrition in the34. Nam CB, Powers MG: Variations in socioe-
26. Robins L, Helzer J, CroughanJ, Ratcliff K: Baltimore ECA Follow-up. Manuscript, conomic structure by race, residence, and
National Institute of Mental Health Diag- 1995 life cycle. Am Sociol Rev 30:97-103,1965
nostic Interview Schedule: its history, 31. Kleinbaum DG, Kupper LL, Morgenstern 35. Harris M: Undiagnosed NIDDM: clinical
characteristics, and validity. Arch Gen Psy- H: Epidemiologic Research: Principles and and public health issues. Diabetes Care
chiatry 38:381-389,1981 Quantitative Methods. Belmont, CA, Life- 16:642-652,1993
27. American Psychiatric Association: Diag- time Learning Publications, 1982 36. Herman W, Smith P, Thompson T, Engel-
nostic and Statistical Manual oj Mental Dis- 32. Lipton R, Liao Y, Cao G, Cooper R, gau M, Aubert R: A new and simple ques-
orders. Washington, DC, American Psychi- McGee D: Determinants of incident tionnaire to identify people at increased
atric Association, 1980 non-insulin-dependent diabetes mellitus risk for undiagnosed diabetes. Diabetes
28. Wells KB, Golding JM, Bumam MA: Affec- among blacks and whites in a national Care 18:382-387, 1995
1102 DIABETES CARE, VOLUME 19, NUMBER 10, OCTOBER 1996
You might also like
- CBC 21st NC IIDocument14 pagesCBC 21st NC IIMichael IbarraNo ratings yet
- Onset Depression Health Related Risc Dztp2Document7 pagesOnset Depression Health Related Risc Dztp2Levente DobaiNo ratings yet
- The Thrifty Psychiatric PhenotypeDocument3 pagesThe Thrifty Psychiatric Phenotypeeduardobar2000No ratings yet
- Diabetes and Mental HealthDocument3 pagesDiabetes and Mental HealthVENNA FADILLAHNo ratings yet
- DiabetesSchizophreniaInterview CITROME BehavHealthCare2006Document8 pagesDiabetesSchizophreniaInterview CITROME BehavHealthCare2006Leslie CitromeNo ratings yet
- Depresi Pada DMDocument5 pagesDepresi Pada DMnigoNo ratings yet
- NIDDK International Conference Report On Diabetes and Depression: Current Understanding and Future DirectionsDocument11 pagesNIDDK International Conference Report On Diabetes and Depression: Current Understanding and Future Directionsyeremias setyawanNo ratings yet
- The Association Between Diabetes Mellitus and DepressionDocument6 pagesThe Association Between Diabetes Mellitus and DepressionMeidy RamschieNo ratings yet
- Artikel Bahasa Inggris Depresi 2Document6 pagesArtikel Bahasa Inggris Depresi 2Serli SafitriNo ratings yet
- Diabetes y Patologias OralesDocument11 pagesDiabetes y Patologias OralesMedusa GorgonNo ratings yet
- Depression in Type 2 Diabetes MellitusDocument11 pagesDepression in Type 2 Diabetes MellitusSerli SafitriNo ratings yet
- On The Association Between Diabetes and Mental Disorders in A Community SampleDocument6 pagesOn The Association Between Diabetes and Mental Disorders in A Community SampleribkaNo ratings yet
- Campayo 2010Document5 pagesCampayo 2010Matthew DemicoliNo ratings yet
- PTJ 1254Document11 pagesPTJ 1254angsokasatuNo ratings yet
- Diabetes DepressionDocument6 pagesDiabetes DepressionHaleelu Abdul JaleelNo ratings yet
- Hypoglycemia, Diabetes, and Cardiovascular Events: C V. D, G B. B, V FDocument6 pagesHypoglycemia, Diabetes, and Cardiovascular Events: C V. D, G B. B, V FHervi LaksariNo ratings yet
- Depression and Increased Mortality in Diabetes: Unexpected Causes of DeathDocument8 pagesDepression and Increased Mortality in Diabetes: Unexpected Causes of DeathAna LemesNo ratings yet
- Review of Related Literature and StudiesDocument16 pagesReview of Related Literature and Studiesannamargie07No ratings yet
- Atkinson 2014Document14 pagesAtkinson 2014nagitagtgtNo ratings yet
- JAMA Intern Med 2021 Apr 1 181 (4) 520-521Document2 pagesJAMA Intern Med 2021 Apr 1 181 (4) 520-521Samuel SalazarNo ratings yet
- PCC 11258Document5 pagesPCC 11258Alina PopaNo ratings yet
- Literature Review UpdatedDocument7 pagesLiterature Review Updatedapi-392259592No ratings yet
- Polsky 2005Document7 pagesPolsky 2005Tatiana FlorianNo ratings yet
- Xu 2018Document7 pagesXu 2018ZUNENo ratings yet
- 1 s2.0 S0953620522002151 MainDocument6 pages1 s2.0 S0953620522002151 MainErika WulandariNo ratings yet
- Differentiation of Diabetes by Pathophysiology, Natural History, and Prognosis PDFDocument15 pagesDifferentiation of Diabetes by Pathophysiology, Natural History, and Prognosis PDFHadi PrasetyoNo ratings yet
- Review: Orit Pinhas-Hamiel, Philip ZeitlerDocument9 pagesReview: Orit Pinhas-Hamiel, Philip ZeitlerNadhifaNo ratings yet
- Cardiovascular Disease in People With DiabetesDocument11 pagesCardiovascular Disease in People With DiabetesSajal S.KumarNo ratings yet
- Format PengkajianDocument8 pagesFormat PengkajianHandiniNo ratings yet
- Diabetic Medicine - 2017 - Perrin - The Prevalence of Diabetes Specific Emotional Distress in People With Type 2 DiabetesDocument13 pagesDiabetic Medicine - 2017 - Perrin - The Prevalence of Diabetes Specific Emotional Distress in People With Type 2 Diabetesnirmala amirNo ratings yet
- Diabetik Dan KelainannyaDocument11 pagesDiabetik Dan Kelainannyalatifah zahrohNo ratings yet
- Comorbid Depression in Medical DiseasesDocument22 pagesComorbid Depression in Medical DiseasesArmando Marín FloresNo ratings yet
- Pelumi 2Document11 pagesPelumi 2oluwasegunnathaniel0No ratings yet
- Type 1 Diabetes ReviewDocument14 pagesType 1 Diabetes Reviewmonday125No ratings yet
- Effects of Diet and Exercise in Preventing NIDDM in People With Impaired Glucose ToleranceDocument8 pagesEffects of Diet and Exercise in Preventing NIDDM in People With Impaired Glucose ToleranceAzielNo ratings yet
- ADA Consenssus DM Eldery 2012Document15 pagesADA Consenssus DM Eldery 2012Jason CarterNo ratings yet
- Seminar: Epidemiology, Comorbidity, and DiagnosisDocument11 pagesSeminar: Epidemiology, Comorbidity, and DiagnosisMartin GiraudoNo ratings yet
- Does Depression Cause Obesity?: A Meta-Analysis of Longitudinal Studies of Depression and Weight ControlDocument8 pagesDoes Depression Cause Obesity?: A Meta-Analysis of Longitudinal Studies of Depression and Weight ControlSergio Machado NeurocientistaNo ratings yet
- Knowledge Gap in DiabetesDocument3 pagesKnowledge Gap in Diabetesamit545No ratings yet
- Fulltext01 PDFDocument92 pagesFulltext01 PDFغاز الشمالNo ratings yet
- Neurobiology of Disease: ReviewDocument10 pagesNeurobiology of Disease: ReviewmarselyagNo ratings yet
- Management of Dyslipidemia in Adults With DiabetesDocument19 pagesManagement of Dyslipidemia in Adults With DiabetesWahyuningsih HamidNo ratings yet
- International Journal of Health Sciences and Research: Stress and Diabetes MellitusDocument8 pagesInternational Journal of Health Sciences and Research: Stress and Diabetes Mellitusamalia dikaNo ratings yet
- Depression and Diabetes Revised 2021Document30 pagesDepression and Diabetes Revised 2021SenaNo ratings yet
- International Journal of Health Sciences and Research: Stress and Diabetes MellitusDocument8 pagesInternational Journal of Health Sciences and Research: Stress and Diabetes MellitusmariahelenaneiNo ratings yet
- Type 2 Diabetes Mellitus in Children and Adolescents: A Relatively New Clinical Problem Within Pediatric PracticeDocument5 pagesType 2 Diabetes Mellitus in Children and Adolescents: A Relatively New Clinical Problem Within Pediatric PracticeAnnisa FujiantiNo ratings yet
- Distress ExperienceDocument9 pagesDistress ExperienceTengku EltrikanawatiNo ratings yet
- Jurnal DiabetesDocument50 pagesJurnal DiabetesYusmiyati YusmiyatiNo ratings yet
- The Risk Factors of Diabetes Mellitus in Adolescent Senior High School in Malang CityDocument10 pagesThe Risk Factors of Diabetes Mellitus in Adolescent Senior High School in Malang CityJurnal Ners UNAIRNo ratings yet
- Geriatria Articulo EspecialDocument15 pagesGeriatria Articulo EspecialBonchita BellaNo ratings yet
- Nouwen 2019Document11 pagesNouwen 2019Adrian SilaghiNo ratings yet
- Diabetes 5Document16 pagesDiabetes 5patricia osei-owusuNo ratings yet
- Obesity and Depression in Adolescence and Beyond: Reciprocal RisksDocument7 pagesObesity and Depression in Adolescence and Beyond: Reciprocal RisksrezkyagustineNo ratings yet
- Diab2 2Document5 pagesDiab2 2mono1144No ratings yet
- The Two-Way Relationship Between Diabetes and Periodontal DiseaseDocument12 pagesThe Two-Way Relationship Between Diabetes and Periodontal DiseaseDevi AlfianiNo ratings yet
- Stress and Diabetes A Review of The LinksDocument7 pagesStress and Diabetes A Review of The LinksHaruNo ratings yet
- Diabetes Stigma and Its Association With Diabetes Outcomes: A Cross-Sectional Study of Adults With Type 1 DiabetesDocument7 pagesDiabetes Stigma and Its Association With Diabetes Outcomes: A Cross-Sectional Study of Adults With Type 1 Diabetesbsndbh65wcNo ratings yet
- The Costs of Depression - Kessler2012Document14 pagesThe Costs of Depression - Kessler2012chen eliseNo ratings yet
- A Study of Depression in Diabetes Mellitus: Analysis From Rural Hospital, India 1Document6 pagesA Study of Depression in Diabetes Mellitus: Analysis From Rural Hospital, India 1International Medical PublisherNo ratings yet
- Rethinking Diabetes: Entanglements with Trauma, Poverty, and HIVFrom EverandRethinking Diabetes: Entanglements with Trauma, Poverty, and HIVNo ratings yet
- Ampalaya: Nature's Remedy for Type 1 & Type 2 DiabetesFrom EverandAmpalaya: Nature's Remedy for Type 1 & Type 2 DiabetesRating: 5 out of 5 stars5/5 (1)
- Germany, France, The United Kingdom, China, Iran, Turkey, Belgium, The Russian Federation, Canada andDocument4 pagesGermany, France, The United Kingdom, China, Iran, Turkey, Belgium, The Russian Federation, Canada andLevente DobaiNo ratings yet
- Feelings and Emotions Flash Cards: How To Shrink The Print SizeDocument15 pagesFeelings and Emotions Flash Cards: How To Shrink The Print SizeLevente DobaiNo ratings yet
- Onset Depression Health Related Risc Dztp2Document7 pagesOnset Depression Health Related Risc Dztp2Levente DobaiNo ratings yet
- Empirically Supported Treatment: Recommendations For A New ModelDocument22 pagesEmpirically Supported Treatment: Recommendations For A New ModelLevente DobaiNo ratings yet
- Acne PPT Azithral PulseDocument21 pagesAcne PPT Azithral PulsesaurabhNo ratings yet
- Project Certificates Hospital Revised2019Document3 pagesProject Certificates Hospital Revised2019S V ENTERPRISESNo ratings yet
- Upper Gastrointestin Al Bleeding: Case Presentation BSN 3-1Document80 pagesUpper Gastrointestin Al Bleeding: Case Presentation BSN 3-1Lanrose Parocha100% (1)
- Principles of SWDocument2 pagesPrinciples of SWJane D VargasNo ratings yet
- Pneumonia: General Medical Officer (GMO) Manual: Clinical SectionDocument3 pagesPneumonia: General Medical Officer (GMO) Manual: Clinical SectionEni RahmawatiNo ratings yet
- Shampoo On BedDocument2 pagesShampoo On BedSean Rene Duay100% (1)
- 02 Revman Exercise Caffeine Articles JournalsDocument8 pages02 Revman Exercise Caffeine Articles JournalsKenneth TorresNo ratings yet
- Supporting Children and Families Fact SheetDocument8 pagesSupporting Children and Families Fact SheetMark FreieNo ratings yet
- UNEP Env Sustainability and SDGsDocument1 pageUNEP Env Sustainability and SDGsA'del JummaNo ratings yet
- 22-04-2021 HMB EnglishDocument22 pages22-04-2021 HMB EnglishdarshNo ratings yet
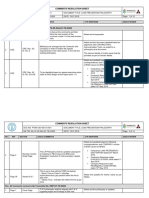
- PE-ZR-DAS-NT-TR-02209: Comments Resolution SheetDocument81 pagesPE-ZR-DAS-NT-TR-02209: Comments Resolution SheetSheik BenasudeenNo ratings yet
- Module II On PFA: Calming Down and Managing One's Emotions and Thoughts (DAY 2)Document2 pagesModule II On PFA: Calming Down and Managing One's Emotions and Thoughts (DAY 2)Jenny RoseNo ratings yet
- TACFIT - Kettlebell Spetsnaz 101Document10 pagesTACFIT - Kettlebell Spetsnaz 101Fabrizio Mosca100% (1)
- JR 1 Course Schedule CompleteDocument19 pagesJR 1 Course Schedule CompleteBrooke GoldenNo ratings yet
- Science Investigatory Project - FinalDocument10 pagesScience Investigatory Project - FinalErich Benedict ClerigoNo ratings yet
- Introduction To Dairy Farming PPT 1114fcdDocument24 pagesIntroduction To Dairy Farming PPT 1114fcdShubham JaiswalNo ratings yet
- 352-Article Text-2821-1-10-20230803Document16 pages352-Article Text-2821-1-10-20230803Winda Hernida 02No ratings yet
- Type of IncisionsDocument2 pagesType of Incisionsdemoniac1420100% (4)
- Contests Npcnewsonline Com Contests 2018 NPC - North - American - Championships Krechelle - HymasDocument6 pagesContests Npcnewsonline Com Contests 2018 NPC - North - American - Championships Krechelle - Hymaskinghall2891No ratings yet
- Chapter Three: Physical Examination of UrineDocument34 pagesChapter Three: Physical Examination of UrineRebuma BeleteNo ratings yet
- Translation As Techné - Female Sexuality and The Science of Social Progress in Colonial IndiaDocument27 pagesTranslation As Techné - Female Sexuality and The Science of Social Progress in Colonial IndiabtNo ratings yet
- Tien Cheu 2021Document11 pagesTien Cheu 2021Ismael Cervantes ChavezNo ratings yet
- Soal Lokasi KIK - 2Document2 pagesSoal Lokasi KIK - 2novida nainggolanNo ratings yet
- (Ký, ghi rõ họ tên) (Ký, ghi rõ họ tên)Document15 pages(Ký, ghi rõ họ tên) (Ký, ghi rõ họ tên)Nguyen Phuong ThanhNo ratings yet
- Gestural Apraxia: SciencedirectDocument10 pagesGestural Apraxia: SciencedirectDiane MxNo ratings yet
- Rubber Dam - 07 - HandoutDocument12 pagesRubber Dam - 07 - HandoutOmar Al-AboodNo ratings yet
- EF-SSEMR-M-3003 - Weekly Safety Minutes of Meeting (WS-MOM)Document1 pageEF-SSEMR-M-3003 - Weekly Safety Minutes of Meeting (WS-MOM)Younis KhanNo ratings yet
- Physical Education and Health: (Weeks 5-8)Document19 pagesPhysical Education and Health: (Weeks 5-8)Charmie DagonNo ratings yet
- Rapid HFDocument9 pagesRapid HFDoc Tor StrangeNo ratings yet