Professional Documents
Culture Documents
Clinmed 2020-0351 Full
Clinmed 2020-0351 Full
Uploaded by
Isro AlhaqiCopyright:
Available Formats
You might also like
- Exercise 13 Worksheet: FaisanDocument4 pagesExercise 13 Worksheet: FaisanFrancesca FaisanNo ratings yet
- Environmental ToxicologyDocument4 pagesEnvironmental ToxicologyDaniela Mariana RosioruNo ratings yet
- Sexual Reproduction of Land Plants Worksheet For Online CoursesDocument14 pagesSexual Reproduction of Land Plants Worksheet For Online CoursesPAWISHYADA LIKITCAJORNCHAINo ratings yet
- Sars-Cov-2 Antibody Testing-Questions To Be Asked: Methods of Allergy and ImmunologyDocument9 pagesSars-Cov-2 Antibody Testing-Questions To Be Asked: Methods of Allergy and ImmunologyGabriel GuerreiroNo ratings yet
- JCP 29785Document10 pagesJCP 29785Wa Ode Yulianti Asrar JayaNo ratings yet
- Jurnal InternasionalDocument10 pagesJurnal InternasionalWa Ode Yulianti Asrar JayaNo ratings yet
- Cureus 0012 00000010501Document6 pagesCureus 0012 00000010501Anna JuniedNo ratings yet
- (Drug Development Research) Phadke, Mrudula - Saunik, Sujata - COVID-19 Treatment by Repurposing Drugs Until The Vaccine Is in Sight (2020)Document3 pages(Drug Development Research) Phadke, Mrudula - Saunik, Sujata - COVID-19 Treatment by Repurposing Drugs Until The Vaccine Is in Sight (2020)Francisco UrdanetANo ratings yet
- Bioorganic Chemistry: MD Jawaid Akhtar TDocument9 pagesBioorganic Chemistry: MD Jawaid Akhtar TRetno Tri RahayuNo ratings yet
- Medical Hypotheses: SciencedirectDocument4 pagesMedical Hypotheses: SciencedirectDaniel ChávezNo ratings yet
- Document A SaisirDocument46 pagesDocument A SaisirFabrice SeoneNo ratings yet
- Vol 28 2 2020 10Document14 pagesVol 28 2 2020 10Nanang SupriyantoNo ratings yet
- Viruses: Amantadine Inhibits Sars-Cov-2 in VitroDocument10 pagesViruses: Amantadine Inhibits Sars-Cov-2 in VitroTiberiu ScanteieNo ratings yet
- Clinical Epidemiology and Global HealthDocument9 pagesClinical Epidemiology and Global HealthHendri YantoNo ratings yet
- Perspectives On Monoclonal Antibody Therapy As Potential Therapeutic Intervention For Coronavirus Disease-19 (COVID-19)Document9 pagesPerspectives On Monoclonal Antibody Therapy As Potential Therapeutic Intervention For Coronavirus Disease-19 (COVID-19)Juan Gonzalez RoblesNo ratings yet
- The Latest Research On COVID-19 Treatments and Medications in The PipelineDocument18 pagesThe Latest Research On COVID-19 Treatments and Medications in The PipelineUNITY LEARNNo ratings yet
- Antiviral Nucleosides-Flu Viruses-Quinolines-COVID-19: Corresponding AuthorDocument12 pagesAntiviral Nucleosides-Flu Viruses-Quinolines-COVID-19: Corresponding AuthorDrkrishnasarma pathyNo ratings yet
- Ecprm 09 00577Document21 pagesEcprm 09 00577HETA JOSHINo ratings yet
- Covid UpdateDocument25 pagesCovid UpdateAndreea PostolacheNo ratings yet
- High Incidence of Barotrauma in Patients With Severe Coronavirus Disease 2019Document9 pagesHigh Incidence of Barotrauma in Patients With Severe Coronavirus Disease 2019AMBUJ KUMAR SONINo ratings yet
- Medicinal Chemistry Strategies Towards The Development - 2022 - Acta PharmaceutiDocument19 pagesMedicinal Chemistry Strategies Towards The Development - 2022 - Acta PharmaceutiMohammed Shuaib AhmedNo ratings yet
- Advances and Challenges in The Prevention and Treatment of COVID-19Document8 pagesAdvances and Challenges in The Prevention and Treatment of COVID-19RoyNo ratings yet
- Immunosuppressive Drugs and COVID-19: A ReviewDocument20 pagesImmunosuppressive Drugs and COVID-19: A ReviewCristie SumbillaNo ratings yet
- A Short Review On Antibody Therapy For COVID-19Document4 pagesA Short Review On Antibody Therapy For COVID-19Master Littérature et CinémaNo ratings yet
- Covid 19Document14 pagesCovid 19arehmanshafiq727No ratings yet
- Int J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaDocument12 pagesInt J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaRebeca EscutiaNo ratings yet
- Potential Therapeutic Effects of Dipyridamole in The S - 2020 - Acta PharmaceutiDocument11 pagesPotential Therapeutic Effects of Dipyridamole in The S - 2020 - Acta PharmaceutiMohammed Shuaib AhmedNo ratings yet
- COVID-19 and Treatment With NSAIDs and Corticosteroids PDFDocument3 pagesCOVID-19 and Treatment With NSAIDs and Corticosteroids PDFDiego RamosNo ratings yet
- Covid UpdateDocument5 pagesCovid UpdateAndreea PostolacheNo ratings yet
- Convalescent PlasmaDocument42 pagesConvalescent PlasmaOlaniyi John OlajideNo ratings yet
- Provenzani-Polidori2020 Article Covid-19AndDrugTherapyWhatWeLeDocument4 pagesProvenzani-Polidori2020 Article Covid-19AndDrugTherapyWhatWeLeRanaJRspectorzNo ratings yet
- Remdesivir in Treating Coronavirus-A Review: IP International Journal of Periodontology and ImplantologyDocument4 pagesRemdesivir in Treating Coronavirus-A Review: IP International Journal of Periodontology and ImplantologySkAliHassanNo ratings yet
- TCMDocument10 pagesTCM1122GNo ratings yet
- Antivirus CovidDocument12 pagesAntivirus CovidAni RahayuNo ratings yet
- Cells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Document29 pagesCells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Yoni LinggaNo ratings yet
- New Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For COVID19 PDFDocument32 pagesNew Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For COVID19 PDFHendry HuangNo ratings yet
- Comprehensive Treatment COVID 19Document49 pagesComprehensive Treatment COVID 19ekoNo ratings yet
- High-Dose Intravenous Immunoglobulin As A Therapeutic Option For Deteriorating Patients With Coronavirus Disease 2019Document6 pagesHigh-Dose Intravenous Immunoglobulin As A Therapeutic Option For Deteriorating Patients With Coronavirus Disease 2019my accountNo ratings yet
- Covide 19Document12 pagesCovide 19Hamza MehalliNo ratings yet
- Biomedicine & Pharmacotherapy: Rory J. Malek, Colin A. Bill, Charlotte M. VinesDocument21 pagesBiomedicine & Pharmacotherapy: Rory J. Malek, Colin A. Bill, Charlotte M. Vineszahraa ahmedNo ratings yet
- Safety and Adverse Reaction of Therapeutic Antibodies Against Sars-Cov-2Document26 pagesSafety and Adverse Reaction of Therapeutic Antibodies Against Sars-Cov-2preeti yadavNo ratings yet
- Remdesivir For Severe Acute Respiratory Syndrome Coronavirus 2 Causing Covid 19 An Evaluation of The Evidence Yu Chen Cao All ChapterDocument53 pagesRemdesivir For Severe Acute Respiratory Syndrome Coronavirus 2 Causing Covid 19 An Evaluation of The Evidence Yu Chen Cao All Chapterdora.morales550100% (16)
- Autoimmunity Reviews: SciencedirectDocument9 pagesAutoimmunity Reviews: SciencedirectRia GandaNo ratings yet
- Jurnal Penelitian Meta AnalisisDocument10 pagesJurnal Penelitian Meta Analisisraihanul khairiNo ratings yet
- 1 s2.0 S2213398420301767 MainDocument9 pages1 s2.0 S2213398420301767 MainNunungTriwahyuniNo ratings yet
- Ebook Remdesivir For Severe Acute Respiratory Syndrome Coronavirus 2 Causing Covid 19 An Evaluation of The Evidence PDF Full Chapter PDFDocument63 pagesEbook Remdesivir For Severe Acute Respiratory Syndrome Coronavirus 2 Causing Covid 19 An Evaluation of The Evidence PDF Full Chapter PDFcarol.thompson605100% (26)
- SARS-CoV-2 X ERDocument6 pagesSARS-CoV-2 X ERJulia MouraNo ratings yet
- Clinical Observation and Management of COVID-19 PatientsDocument5 pagesClinical Observation and Management of COVID-19 PatientsJasper VanhaerenNo ratings yet
- 1 s2.0 S1156523321000585 MainDocument4 pages1 s2.0 S1156523321000585 MainAna PerfeitoNo ratings yet
- New Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For Covid 19 Christian A Devaux Full ChapterDocument29 pagesNew Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For Covid 19 Christian A Devaux Full Chapternorman.pregler293100% (12)
- 1 s2.0 S2590059523001930 MainDocument10 pages1 s2.0 S2590059523001930 MainHarithaNo ratings yet
- Inflammation, Immunity and Potential Target Therapy of SARS-COV-2 ADocument23 pagesInflammation, Immunity and Potential Target Therapy of SARS-COV-2 AShukr Wesman BlbasNo ratings yet
- Passive Immunotherapeutics COVID 19Document11 pagesPassive Immunotherapeutics COVID 19Daniel PratamaNo ratings yet
- Insight Into 2019 Novel Coronavirus An Updated Intrim Review and Lessons From Sars Cov and Mers Cov Mingxuan Xie Download 2024 Full ChapterDocument45 pagesInsight Into 2019 Novel Coronavirus An Updated Intrim Review and Lessons From Sars Cov and Mers Cov Mingxuan Xie Download 2024 Full Chaptertom.beckett574100% (11)
- PRL CovidDocument8 pagesPRL Covidzainy zehraNo ratings yet
- Ebook New Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For Covid 19 PDF Full Chapter PDFDocument28 pagesEbook New Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For Covid 19 PDF Full Chapter PDFglenn.mcdonald396100% (24)
- Medical HypothesesDocument5 pagesMedical Hypothesesnow youloseNo ratings yet
- Preprints ChloroquineDocument24 pagesPreprints ChloroquineJorgelina BernetNo ratings yet
- COVID 19 An Emerging Coronavirus Infection Advances and Prospects in Designing and Developing Vaccines Immunotherapeutics and TherapeuticsDocument8 pagesCOVID 19 An Emerging Coronavirus Infection Advances and Prospects in Designing and Developing Vaccines Immunotherapeutics and TherapeuticsCertaf MaghnjaNo ratings yet
- Can Phytotherapy With Polyphenols Serve As A Powerful Approach For The Prevention and Therapy Tool of Novel Coronavirus Disease 2019? 2020Document20 pagesCan Phytotherapy With Polyphenols Serve As A Powerful Approach For The Prevention and Therapy Tool of Novel Coronavirus Disease 2019? 2020Kelly DickinsonNo ratings yet
- Treatment Options For Covid 19 The Reality and Challenges Shio Shin Jean Download 2024 Full ChapterDocument47 pagesTreatment Options For Covid 19 The Reality and Challenges Shio Shin Jean Download 2024 Full Chaptermari.artrip178100% (10)
- 11 PDF FSLCE Biology QPDocument21 pages11 PDF FSLCE Biology QPishikamani07No ratings yet
- Mice Rats in Biomedical Research FBRDocument2 pagesMice Rats in Biomedical Research FBRChikondi TemboNo ratings yet
- Cancer ImmunotherapyDocument15 pagesCancer Immunotherapyqud86100% (1)
- Journal RefstylesDocument27 pagesJournal RefstylesChun-Yi YangNo ratings yet
- Genetics Practice ProbsDocument4 pagesGenetics Practice Probsajaysharma19686191No ratings yet
- Class 7 Science Chapter 1 Revision NotesDocument2 pagesClass 7 Science Chapter 1 Revision NotesRao Saijal YadavNo ratings yet
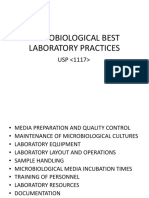
- KM5-2560 MicrobiologicalBestPracticeDocument64 pagesKM5-2560 MicrobiologicalBestPracticeAbid IqbalNo ratings yet
- h24 Dstrainingguide Usen Rev03Document5 pagesh24 Dstrainingguide Usen Rev03Elisan BrasilNo ratings yet
- Chapter 31 - HematopoiesisDocument20 pagesChapter 31 - HematopoiesisMauricio AndrésNo ratings yet
- DLL Science Quarter 2 Week 1-9Document24 pagesDLL Science Quarter 2 Week 1-9Argie PiaNo ratings yet
- Blood & Immunology McqsDocument6 pagesBlood & Immunology McqsAbdullah TheNo ratings yet
- Bioteknologi Farmasi PendahuluanDocument65 pagesBioteknologi Farmasi PendahuluanNadhifa MukarommNo ratings yet
- Patentability of Biotech Subject MatterDocument136 pagesPatentability of Biotech Subject MatterGareth WealeNo ratings yet
- Chapter 4Document6 pagesChapter 4Kate Wen GuanNo ratings yet
- Revised Syllabus - Degree Module Approved by 24th AC Meeting Held On 6th May 2017 PDFDocument153 pagesRevised Syllabus - Degree Module Approved by 24th AC Meeting Held On 6th May 2017 PDFUjual BasnetNo ratings yet
- Course Structure Course: Bio101 Essentials of Biology, Lab (4 CR) PrerequisiteDocument2 pagesCourse Structure Course: Bio101 Essentials of Biology, Lab (4 CR) PrerequisiteAaron ChongNo ratings yet
- GeneticDocument3 pagesGeneticbebaNo ratings yet
- Pages From 1-Molecular Cell Biology Lodish 5Th EdDocument4 pagesPages From 1-Molecular Cell Biology Lodish 5Th Edapi-3733156100% (1)
- CH 15 WorkbookDocument10 pagesCH 15 Workbookapi-237586441100% (1)
- Anavar (Oxandrolone)Document26 pagesAnavar (Oxandrolone)illicitdrugsNo ratings yet
- PIGMENTS Mbbs - Dr. SuchitaDocument53 pagesPIGMENTS Mbbs - Dr. SuchitaRushi VaghelaNo ratings yet
- The Fetal Period: by DR - Abdallah GreeballahDocument55 pagesThe Fetal Period: by DR - Abdallah GreeballahrawanNo ratings yet
- Synopsis, FormatDocument14 pagesSynopsis, FormatHira Hameed100% (1)
- S2 - Ch06 - Biotransformation of XenobioticsDocument92 pagesS2 - Ch06 - Biotransformation of XenobioticsWachi PampasNo ratings yet
- Worksheets: Digestive SystemDocument9 pagesWorksheets: Digestive SystemAbigailBarrionGutierrezNo ratings yet
- Resilience Definitions Theory and ChallengesDocument14 pagesResilience Definitions Theory and ChallengesRaji Rafiu BoyeNo ratings yet
- Muscle HistologyDocument50 pagesMuscle HistologyKhalid H MuseNo ratings yet
Clinmed 2020-0351 Full
Clinmed 2020-0351 Full
Uploaded by
Isro AlhaqiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinmed 2020-0351 Full
Clinmed 2020-0351 Full
Uploaded by
Isro AlhaqiCopyright:
Available Formats
Clinical Medicine Publish Ahead of Print, published on August 30, 2020 as doi:10.7861/clinmed.
2020-0351
COVID-19 RAPID REPORT Clinical Medicine 2020 Vol 20, No 6 November 2020
Inhaled and systemic heparin as a repurposed direct
antiviral drug for prevention and treatment of COVID-19
Authors: Carina Conzelmann,A* Janis A Müller,B* Lukas Perkhofer,C Konstantin MJ Sparrer,D
Alexander N Zelikin,E# Jan Münch,F# and Alexander KlegerG#
Here, we advocate a highly favourable opportunity for the rate. It is caused by severe acute respiratory syndrome coronavirus 2
ABSTRACT
treatment of COVID-19 disease by repurposing a long-serving (SARS-CoV-2), which is transmitted between humans by respiratory
medical agent with an excellent history of clinical use, namely droplets, aerosols or rarely via contaminated surfaces.1,2 SARS-
heparin. Heparin is best known as an anticoagulant, but it CoV-2 is a betacoronavirus which was described in Wuhan, China in
also exhibits direct antiviral activity against many enveloped December 2019 for the first time.2 It is genetically 79.5% identical
viruses and has anti-inflammatory activity. The high incidence to SARS-CoV which caused the SARS outbreak in 2002 and similar
of thromboembolic events in COVID-19 patients suggests to the MERS-CoV (Middle East respiratory syndrome-related
that coagulopathy plays an important role in the SARS-CoV-2 coronavirus) discovered in 2012.3
pathogenesis. This already makes heparin a unique, potentially The virus primarily infects the respiratory tract, causing no or
curative agent that can be used immediately to help resolve mild symptoms in the majority of cases, while a smaller proportion
the ongoing crisis associated with SARS-CoV-2 infection and develops severe disease with pneumonia and, upon spread to other
COVID-19 disease. We demonstrate here in vitro that heparin body compartments, multi-organ failure. Currently, patients with
does indeed inhibit SARS-CoV-2 infection. The three concurrent COVID-19 are mostly treated with supportive care. Accordingly,
modes of activity of heparin (antiviral, anticoagulant and anti- literature survey reveals that the highest success registered
inflammatory) against SARS-CoV-2/COVID-19 form a unique to date lies not in the realm of antiviral drugs to address the
therapeutic combination. Thus, repurposing of heparin to fight infectivity of SARS-CoV-2, but is instead due to this symptomatic
SARS-CoV-2 and COVID-19 appears to be a powerful, readily and supportive treatment of COVID-19 itself.3 Widely available
available measure to address the current pandemic. vaccination strategies are not expected before the year 2021.6 As
the development of novel drugs usually takes years, the fastest
KEYWORDS: COVID-19, heparin, SARS-CoV-2, Inhalation, route to establish a new treatment option is to repurpose an
pulmonary coagulation existing drug.4,5 Indeed, a number of drug preparations developed
in another context are currently being evaluated in clinical trials
DOI: 10.7861/clinmed.2020-0351 for COVID-19. Of these, the direct antiviral agent remdesivir has
recently received an emergency use authorisation from the US
Food and Drug Administration (FDA) and the European Medicines
Agency (EMA).7 However, according to the most recent data,
Introduction remdesivir only shortens hospitalisation and weakens disease
COVID-19 is an emerging infectious disease with a high case fatality course without reducing overall mortality.3 The first repurposed
drug was dexamethasone, which reduced 28-day mortality among
patients receiving invasive mechanical ventilation, as recently
communicated by the RECOVERY consortium and published as
Authors: APhD student, Institute of Molecular Virology, Ulm University a preprint manuscript.8 Conversely, several promising repurposed
Medical Centre, Ulm, Germany; Bpostdoctoral fellow, Institute of formulations have failed.9,10 Active viral replication and shedding
Molecular Virology, Ulm University Medical Centre, Ulm, Germany; seems to take place in the upper respiratory tract during the early
C
attending physician in gastroenterology, Department of Internal phase of COVID-19,5 followed by either immune-mediated viral
Medicine, Ulm University Hospital, Ulm, Germany; Djunior principal clearance or transmission to the lower respiratory tract.11 In its later
investigator, Institute of Molecular Virology, Ulm University Medical stages, COVID-19 presents with progressive respiratory failure,
Centre, Ulm, Germany; Eassociate professor, Department of Chemistry possibly caused by viral replication in the lungs and cytokine-
and iNano Interdisciplinary Nanoscience Centre, Aarhus University, induced hyperinflammation.4 Hence, one strategy to prevent
Aarhus, Denmark; Fprofessor of molecular virology, Institute of clinical deterioration and respiratory failure might be to impede
Molecular Virology, Ulm University Medical Centre, Ulm, Germany; locoregional viral replication in the early disease phase, eg by
G
professor of molecular oncology, Department of Internal Medicine, inhaled drug formulations.12–14
Ulm University Hospital, Ulm, Germany; *equal contributions; #equal
contribution and joint supervision
1 © Royal College of Physicians 2020. All rights reserved.
Copyright 2020 by Royal College of Physicians.
Inhaled and systemic heparin for COVID-19
a Heparin (µg/ml) b c
60 150
Uninfected 250
Number of plaques per well
CPE (normalised %)
40 100
0 500
20 50
125 1,000 0 0
0
125
250
500
1,000
0
125
250
500
1,000
Uninfected
Uninfected
Heparin (µg/ml) Heparin (µg/ml)
Fig 1. Heparin inhibits SARS-CoV-2 plaque formation. a) 800,000 Vero E6 cells were seeded in a 12-well plate the day before infection to result in a 100%
confluent cell monolayer. The next day, medium was removed, cells were washed once with PBS and medium containing heparin (Sigma-Aldrich) was added.
Cells were then inoculated with SARS-CoV-2 isolate BetaCoV/Netherlands/01/NL/2020 (#010V-03903; European virus archive – global) in 500 µl and incubated
for 2 h at 37°C with shaking every 15 to 30 min. Next, cells were overlaid with 1.5 ml of 0.8% Avicel RC-581 (FMC Corporation) in medium containing heparin
and incubated for 3 days. Cells were fixed, stained with crystal violet and imaged. b) Virus-induced plaques shown in Fig 1a were counted. c) Cytopathic effect
(CPE) was quantified using a custom ImageJ macro as the percentage of non-stained area within one well. Raw images were converted to greyscale, regions
of interest (= one well) defined, automatic thresholding (Minimum algorithm) applied and total/white pixel areas calculated. Values represent means of two
technical replicates ± sd.
Thromboembolic events during COVID-19 administration via inhalation has also been proven to be safe in
patients.24 Specifically, inhaled dosages of up to 150,000 IU/d
Besides obvious respiratory symptoms, the broad tropism of SARS- heparin marked a threshold dose to cause systemic effects detected
CoV-2 appears responsible for a variety of atypical manifestations by activated partial thromboplastin time (aPTT) prolongation while
of COVID-19.15 Accordingly, a series of manuscripts reported causing no relevant side effects in patients with distinct chronic
the importance of anticoagulation to prevent and/or treat lung disease.13,20 Accordingly, in 2006 an orphan designation to
thromboembolic complications in COVID-19 patients.16–19 Along improve mucosal clearance in cystic fibrosis patients with inhaled
these lines, a recent autopsy study, among others, confirmed heparin has been provided by the EMA. Further to being the most
thromboembolic events as a major cause of death in critically prominent approved anticoagulant, heparin is also known to have
ill COVID-19 patients, all pointing toward an obviously relevant antiviral activity against diverse viruses, including SARS-CoV-2 (Fig
prothrombotic condition caused by SARS-CoV-2.17,19 Thus, 1).25–27 Thus, the overall effect of heparin to treat SARS-CoV-2/
systemic anticoagulation becomes one of the major columns in COVID-19 is unique, and, unlike directly acting antivirals, covers
lowering death rates in critically ill COVID-19 patients. A recent both the pathogen and the ensuing disease. Specifically, it has three
study conducted a propensity score matching to illuminate modes of action: direct antiviral,25,26,28 anti-inflammatory,29 and
the thromboembolic event rate in non-COVID-19 ARDS (acute anticoagulant,22 as outlined below.
respiratory distress syndrome) and COVID-19 ARDS patients.
Although both groups comprised similar numbers of patients
receiving either prophylactic or therapeutic dosing of heparin, Heparin exerts direct antiviral activity
thromboembolic events occurred significantly more frequently in Heparin is a broadly active antiviral agent that inhibits different
COVID-19 ARDS than in non-COVID-19 ARDS patients (18% vs 6%, enveloped viruses including coronaviruses.25–27 Applying heparin
respectively).16 Accordingly, anticoagulation even appears to reduce per inhalationem could imply that concentrations of heparin
mortality in severe COVID-19 patients fulfilling sepsis-induced would be highest in tissues that are most affected by SARS-CoV-2,
coagulopathy (SIC) criteria or having markedly elevated D-dimers.20 namely the upper and lower respiratory tract. Of note, inhaled
Therefore, the latter criteria identify a high-risk population heparin has a proven broad distribution in the respiratory tract
particularly likely to benefit from systemic anticoagulation.20 Thus, including the alveolar space.7,30-32 Specifically, the antiviral activity
even more aggressive anticoagulation therapy like the salvage use of heparin is based on affinity of viral glycoproteins to negatively
of tissue plasminogen activator (tPA) may improve recovery of charged glycosaminoglycans such as sulfated heparan, which are
COVID-19 ARDS patients;21 however, such measures require further ubiquitously expressed on the surface of mammalian cells. It has
prospective evaluation. recently been demonstrated in a published and a preprint article
that soluble heparin interacts with the SARS-CoV-2 spike protein28,33
Potential advantage of inhaled heparin and inhibits SARS-CoV-2 spike pseudovirus entry.34 In line with
these findings, another preprint article showed that porcine heparin
There are various therapeutic options to achieve systemic prevents wildtype SARS-CoV-2 infection of Vero E6 cells.26
anticoagulation. Among these, unfractionated but also fractionated Thus, we here set out to determine the antiviral activity of heparin
heparins have a long clinical history of being well tolerated, with against SARS-CoV-2. We conducted a viral plaque reduction assay
limited and manageable side effects.22 Thus, heparin is currently in Vero E6 cells inoculated with a Dutch SARS-CoV-2 isolate in the
included in the WHO recommendation for COVID-19 treatment absence or presence of various concentrations of heparin. Heparin
via subcutaneous systemic administration.23 In addition, heparin not only resulted in a decrease in the number of plaques (Fig 1a,b)
© Royal College of Physicians 2020. All rights reserved. 2
COVID-19 rapid reports
but in particular also resulted in a decrease in the size of the plaques already available,43 and stronger efforts are now needed to fully
(Fig 1a). In order to quantify the plaque sizes, we calculated the realise this potential. Thus, clinical trials designed in a prospective
total virus-induced cytopathic effect per well using a custom ImageJ randomised controlled manner are urgently warranted to rapidly
macro as the percentage of non-stained area within one well (Fig accelerate this unique strategy toward clinical application.
1c). This evaluation shows that in the presence of 500–1,000 µg/
ml heparin, viral replication is almost completely inhibited, and Acknowledgments
at 125–250 µg/ml suppressed by more than 60%. Thus, heparin
prevents SARS-CoV-2 infection and subsequent replication with a CC is part of the International Graduate School in Molecular
half maximal inhibitory concentration (IC50) below 125 µg/ml. Medicine, Ulm. This work was supported by grants from the MWK
Baden-Württemberg to JM and AK, and the Horizon 2020 project
Fight-nCoV to JM and ANZ.
Anti-inflammatory and anticoagulant effects of
heparin in the lung
References
Apart from these direct antiviral properties, heparin is known to have
anti-inflammatory activity via, among other mechanisms, its ability 1 Wadman M, Couzin-Frankel J, Kaiser J, Matacic C. A rampage through
the body. Science 2020; 368:356–60.
to neutralise a variety of cationic immune mediators including IL-6
2 Meselson M. Droplets and aerosols in the transmission of SARS-
and IL-8 and to inhibit chemotaxis.35,36 In mammals, heparin is found CoV-2. N Engl J Med 2020; 382:2063.
in mast cells, suggesting its physiological usefulness in mucosal and 3 Beigel JH, Tomashek KM, Dodd LE et al. Remdesivir for the treatment
connective tissue. Inhaled heparin has been used in patients with of Covid-19 - Preliminary Report. N Engl J Med 2020, in press (DOI:
cystic fibrosis for its proposed mucolytic activity and a reduction of 10.1056/NEJMoa2007764).
serum levels of IL-6 and IL-8 were observed.29,37 A third proposed 4 Pushpakom S, Iorio F, Eyers PA et al. Drug repurposing: progress,
mechanism of action of inhaled heparin in COVID-19 patients is its challenges and recommendations. Nat Rev Drug Discovery
2019;18:41–58.
anticoagulative property unfolding locally in the lung.38 ARDS, one
5 Li G, De Clercq E. Therapeutic options for the 2019 novel coronavirus
of the severe and potentially lethal complications of SARS-CoV-2, is (2019-nCoV). Nat Rev Drug Discov 2020;19:149–50.
marked, among other features, by a deposition of fibrin in the alveolar 6 Graham BS. Rapid COVID-19 vaccine development. Science
space and microcirculation, leading to hyaline membranes and 2020;368:945–6.
ultimately to thrombosis, a process called pulmonary coagulopathy 7 Dixon B, Santamaria JD, Campbell DJ. A phase 1 trial of nebulised
(PC). The anticoagulative and fibrinolytic properties of heparin could heparin in acute lung injury. Crit Care 2008;12:R64.
prevent this through per inhalationem application by preventing 8 Horby P, Lim WS, Emberson J et al. Effect of dexamethasone in
hospitalized patients with COVID-19: preliminary report. medRxiv
alveolar collapse, lung oedema and impaired gas exchange.7 Thus, 2020: 2020.2006.2022.20137273.
PC might be more relevant during COVID-19-associated ARDS than 9 Geleris J, Sun Y, Platt J et al. Observational study of
during classical ARDS, as a significantly perturbed gas exchange, eg hydroxychloroquine in hospitalized patients with Covid-19. N Engl J
from fibrin deposition, may lead to perturbed surfactant function Med 2020;382:2411–8.
and thus alveolar collapse. Unusually high D-dimers in critically ill 10 Cao B, Wang Y, Wen D et al. A trial of lopinavir–ritonavir in adults
COVID-19 patients might therefore serve as an early indicator of hospitalized with severe Covid-19. N Engl J Med 2020;382:1787–99.
11 Wölfel R, Corman VM, Guggemos W et al. Virological assessment of
PC subsequently leading to alveolar damage.39 Of note, systemically
hospitalized patients with COVID-2019. Nature 2020;581:465–9.
elevated D-dimers are currently considered to be strong predictors 12 Dixon B, Schultz MJ, Smith R et al. Nebulized heparin is associated
of severe COVID-19 disease.39 In this light, the anti-inflammatory with fewer days of mechanical ventilation in critically ill patients: a
and thrombolytic activity of heparin in injured lungs40 could serve as randomized controlled trial. Crit Care 2010;14:R180.
effective measures against COVID-19. 13 Smoot P. Nebulized heparin for the treatment of COVID-19 induced
Finally, inhalation is strongly suggested herein as a route of lung injury. https://clinicaltrials.gov/ct2/show/NCT04397510.
administration, as the lungs are most affected in COVID-19, 14 Gilead Sciences Inc. Working to supply remdesivir for COVID-19.
www.gilead.com/purpose/advancing-global-health/covid-19/
and this strategy has proven to be highly effective for a range of
working-to-supply-remdesivir-for-covid-19.
other drugs.41 A randomised, placebo-controlled study currently 15 Puelles VG, Lutgehetmann M, Lindenmeyer MT et al. Multiorgan and
aims to determine if nebulised heparin may reduce the severity renal tropism of SARS-CoV-2. N Engl J Med 2020;383:590–2.
of lung injury caused by COVID-19.13 Similarly, the COVID-19 16 Helms J, Tacquard C, Severac F et al. High risk of thrombosis in
HOPE (nebulised Heparin-N-acetylcysteine in COVID-19 Patients patients with severe SARS-CoV-2 infection: a multicenter prospective
by Evaluation of pulmonary function) trial tests the combination cohort study. Intensive Care Med 2020, in press (DOI: 10.1007/
treatment of nebulized heparin with N-acetylcysteine (NAC), which s00134-020-06062-x).
may have the potential to improve pulmonary function and reduce 17 Bompard F, Monnier H, Saab I et al. Pulmonary embolism in patients
or eliminate mechanical ventilation in patients with a coronavirus with Covid-19 pneumonia. Eur Respir J 2020;56:2001365.
18 Stoneham SM, Milne KM, Nuttal E et al. Thrombotic risk in COVID-19:
infection.42 Of note, substantial increase of PC has also been
a case series and case-control study. Clin Med 2020;20:e76–e81.
reported for influenza pneumonia-associated ARDS.20 19 Wichmann D, Sperhake JP, Lutgehetmann M et al. Autopsy findings
and venous thromboembolism in patients with COVID-19: a
Conclusion prospective cohort study. Ann Intern Med 2020, in press (DOI:
10.7326/M20-2003).
The three concurrent modes of activity of heparin against 20 Yang Y, Tang H. Aberrant coagulation causes a hyper-inflammatory
SARS-CoV-2/COVID-19 form a unique therapeutic combination. response in severe influenza pneumonia. Cell Mol Immunol
Repurposing of heparin to fight SARS-CoV-2 and COVID-19 appears 2016;13:432–42.
21 Choudhury R, Barrett CD, Moore HB et al. Salvage use of tissue
to be a powerful, readily available measure to address the current
plasminogen activator (tPA) in the setting of acute respiratory
pandemic. The first clinical evidence to validate this hypothesis is distress syndrome (ARDS) due to COVID-19 in the USA: a Markov
3 © Royal College of Physicians 2020. All rights reserved.
Inhaled and systemic heparin for COVID-19
decision analysis. World J Emerg Surg 2020;15:29. 35 Lever R, Page CP. Non-anticoagulant effects of heparin: an overview.
22 Oduah EI, Linhardt RJ, Sharfstein ST. Heparin: past, present, and Handb Exp Pharmacol 2012:281–305.
future. Pharmaceuticals (Basel) 2016;9:38. 36 Miller MD, Krangel MS. Biology and biochemistry of the chemokines:
23 Laterre PF, Wittebole X, Dhainaut JF. Anticoagulant therapy in acute a family of chemotactic and inflammatory cytokines. Crit Rev
lung injury. Crit Care Med 2003;31:S329–36. Immunol 1992;12:17–46.
24 Yip LY, Lim YF, Chan HN. Safety and potential anticoagulant effects 37 Ledson M, Gallagher M, Hart CA, Walshaw M. Nebulized heparin
of nebulised heparin in burns patients with inhalational injury at in Burkholderia cepacia colonized adult cystic fibrosis patients. Eur
Singapore General Hospital Burns Centre. Burns 2011;37: 1154–60. Respir J 2001;17:36–8.
25 Lang J, Yang N, Deng J et al. Inhibition of SARS pseudovirus cell entry 38 Juschten J, Tuinman PR, Juffermans NP et al. Nebulized
by lactoferrin binding to heparan sulfate proteoglycans. PLOS ONE anticoagulants in lung injury in critically ill patients-an updated
2011;6:e23710. systematic review of preclinical and clinical studies. Ann Transl Med
26 Mycroft-West C, Su D, Elli S et al. The 2019 coronavirus (SARS-CoV-2) 2017;5:444.
surface protein (Spike) S1 receptor binding domain undergoes 39 Zhou F, Yu T, Du R et al. Clinical course and risk factors for mortality
conformational change upon heparin binding. bioRxiv 2020: of adult inpatients with COVID-19 in Wuhan, China: a retrospective
2020.2002.2029.971093. cohort study. Lancet 2020;395:1054–62.
27 Vicenzi E, Canducci F, Pinna D et al. Coronaviridae and SARS- 40 Miller AC, Elamin EM, Suffredini AF. Inhaled anticoagulation
associated coronavirus strain HSR1. Emerg Infect Dis 2004;10:413–8. regimens for the treatment of smoke inhalation-associated acute
28 Mycroft-West CJ, Su D, Pagani I et al. Heparin inhibits cellular lung injury: a systematic review. Crit Care Med 2014;42:413–9.
invasion by SARS-CoV-2: structural dependence of the interaction of 41 Newman SP. Delivering drugs to the lungs: The history of repurposing
the surface protein (spike) S1 receptor binding domain with heparin. in the treatment of respiratory diseases. Adv Drug Deliv Rev
bioRxiv 2020: 2020.2004.2028.066761. 2018;133:5–18.
29 Young E. The anti-inflammatory effects of heparin and related 42 Quay S. The COVID-19 HOPE clinical trial. https://drquay.com/covid-
compounds. Thrombosis Research 2008;122:743–52. 19-doctor/.
30 Bendstrup KE, Jensen JI. Inhaled heparin is effective in exacerbations 43 Shi C, Wang C, Wang H et al. The potential of low molecular
of asthma. Respir Med 2000;94:174–5. weight heparin to mitigate cytokine storm in severe COVID-19
31 Markart P, Nass R, Ruppert C et al. Safety and tolerability of inhaled patients: a retrospective clinical study. medRxiv 2020;
heparin in idiopathic pulmonary fibrosis. J Aerosol Med Pulm Drug 2020.2003.2028.20046144.
Deliv 2010;23:161–72.
32 Monagle K, Ryan A, Hepponstall M et al. Inhalational use of
antithrombotics in humans: Review of the literature. Thromb Res
2015;136:1059–66.
33 Kim SY, Jin W, Sood A et al. Characterization of heparin and severe
acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) spike
glycoprotein binding interactions. Antiviral Res 2020;181:104873.
Address for correspondence: Professor Alexander Kleger,
34 Tandon R, Sharp JS, Zhang F et al. Effective inhibition of SARS- Department of Internal Medicine 1, Ulm University Medical
CoV-2 entry by heparin and enoxaparin derivatives. bioRxiv 2020; Center, Ulm, Germany
2020.06.08.140236. Email: alexander.kleger@uni-ulm.de
© Royal College of Physicians 2020. All rights reserved. 4
You might also like
- Exercise 13 Worksheet: FaisanDocument4 pagesExercise 13 Worksheet: FaisanFrancesca FaisanNo ratings yet
- Environmental ToxicologyDocument4 pagesEnvironmental ToxicologyDaniela Mariana RosioruNo ratings yet
- Sexual Reproduction of Land Plants Worksheet For Online CoursesDocument14 pagesSexual Reproduction of Land Plants Worksheet For Online CoursesPAWISHYADA LIKITCAJORNCHAINo ratings yet
- Sars-Cov-2 Antibody Testing-Questions To Be Asked: Methods of Allergy and ImmunologyDocument9 pagesSars-Cov-2 Antibody Testing-Questions To Be Asked: Methods of Allergy and ImmunologyGabriel GuerreiroNo ratings yet
- JCP 29785Document10 pagesJCP 29785Wa Ode Yulianti Asrar JayaNo ratings yet
- Jurnal InternasionalDocument10 pagesJurnal InternasionalWa Ode Yulianti Asrar JayaNo ratings yet
- Cureus 0012 00000010501Document6 pagesCureus 0012 00000010501Anna JuniedNo ratings yet
- (Drug Development Research) Phadke, Mrudula - Saunik, Sujata - COVID-19 Treatment by Repurposing Drugs Until The Vaccine Is in Sight (2020)Document3 pages(Drug Development Research) Phadke, Mrudula - Saunik, Sujata - COVID-19 Treatment by Repurposing Drugs Until The Vaccine Is in Sight (2020)Francisco UrdanetANo ratings yet
- Bioorganic Chemistry: MD Jawaid Akhtar TDocument9 pagesBioorganic Chemistry: MD Jawaid Akhtar TRetno Tri RahayuNo ratings yet
- Medical Hypotheses: SciencedirectDocument4 pagesMedical Hypotheses: SciencedirectDaniel ChávezNo ratings yet
- Document A SaisirDocument46 pagesDocument A SaisirFabrice SeoneNo ratings yet
- Vol 28 2 2020 10Document14 pagesVol 28 2 2020 10Nanang SupriyantoNo ratings yet
- Viruses: Amantadine Inhibits Sars-Cov-2 in VitroDocument10 pagesViruses: Amantadine Inhibits Sars-Cov-2 in VitroTiberiu ScanteieNo ratings yet
- Clinical Epidemiology and Global HealthDocument9 pagesClinical Epidemiology and Global HealthHendri YantoNo ratings yet
- Perspectives On Monoclonal Antibody Therapy As Potential Therapeutic Intervention For Coronavirus Disease-19 (COVID-19)Document9 pagesPerspectives On Monoclonal Antibody Therapy As Potential Therapeutic Intervention For Coronavirus Disease-19 (COVID-19)Juan Gonzalez RoblesNo ratings yet
- The Latest Research On COVID-19 Treatments and Medications in The PipelineDocument18 pagesThe Latest Research On COVID-19 Treatments and Medications in The PipelineUNITY LEARNNo ratings yet
- Antiviral Nucleosides-Flu Viruses-Quinolines-COVID-19: Corresponding AuthorDocument12 pagesAntiviral Nucleosides-Flu Viruses-Quinolines-COVID-19: Corresponding AuthorDrkrishnasarma pathyNo ratings yet
- Ecprm 09 00577Document21 pagesEcprm 09 00577HETA JOSHINo ratings yet
- Covid UpdateDocument25 pagesCovid UpdateAndreea PostolacheNo ratings yet
- High Incidence of Barotrauma in Patients With Severe Coronavirus Disease 2019Document9 pagesHigh Incidence of Barotrauma in Patients With Severe Coronavirus Disease 2019AMBUJ KUMAR SONINo ratings yet
- Medicinal Chemistry Strategies Towards The Development - 2022 - Acta PharmaceutiDocument19 pagesMedicinal Chemistry Strategies Towards The Development - 2022 - Acta PharmaceutiMohammed Shuaib AhmedNo ratings yet
- Advances and Challenges in The Prevention and Treatment of COVID-19Document8 pagesAdvances and Challenges in The Prevention and Treatment of COVID-19RoyNo ratings yet
- Immunosuppressive Drugs and COVID-19: A ReviewDocument20 pagesImmunosuppressive Drugs and COVID-19: A ReviewCristie SumbillaNo ratings yet
- A Short Review On Antibody Therapy For COVID-19Document4 pagesA Short Review On Antibody Therapy For COVID-19Master Littérature et CinémaNo ratings yet
- Covid 19Document14 pagesCovid 19arehmanshafiq727No ratings yet
- Int J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaDocument12 pagesInt J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaRebeca EscutiaNo ratings yet
- Potential Therapeutic Effects of Dipyridamole in The S - 2020 - Acta PharmaceutiDocument11 pagesPotential Therapeutic Effects of Dipyridamole in The S - 2020 - Acta PharmaceutiMohammed Shuaib AhmedNo ratings yet
- COVID-19 and Treatment With NSAIDs and Corticosteroids PDFDocument3 pagesCOVID-19 and Treatment With NSAIDs and Corticosteroids PDFDiego RamosNo ratings yet
- Covid UpdateDocument5 pagesCovid UpdateAndreea PostolacheNo ratings yet
- Convalescent PlasmaDocument42 pagesConvalescent PlasmaOlaniyi John OlajideNo ratings yet
- Provenzani-Polidori2020 Article Covid-19AndDrugTherapyWhatWeLeDocument4 pagesProvenzani-Polidori2020 Article Covid-19AndDrugTherapyWhatWeLeRanaJRspectorzNo ratings yet
- Remdesivir in Treating Coronavirus-A Review: IP International Journal of Periodontology and ImplantologyDocument4 pagesRemdesivir in Treating Coronavirus-A Review: IP International Journal of Periodontology and ImplantologySkAliHassanNo ratings yet
- TCMDocument10 pagesTCM1122GNo ratings yet
- Antivirus CovidDocument12 pagesAntivirus CovidAni RahayuNo ratings yet
- Cells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Document29 pagesCells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Yoni LinggaNo ratings yet
- New Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For COVID19 PDFDocument32 pagesNew Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For COVID19 PDFHendry HuangNo ratings yet
- Comprehensive Treatment COVID 19Document49 pagesComprehensive Treatment COVID 19ekoNo ratings yet
- High-Dose Intravenous Immunoglobulin As A Therapeutic Option For Deteriorating Patients With Coronavirus Disease 2019Document6 pagesHigh-Dose Intravenous Immunoglobulin As A Therapeutic Option For Deteriorating Patients With Coronavirus Disease 2019my accountNo ratings yet
- Covide 19Document12 pagesCovide 19Hamza MehalliNo ratings yet
- Biomedicine & Pharmacotherapy: Rory J. Malek, Colin A. Bill, Charlotte M. VinesDocument21 pagesBiomedicine & Pharmacotherapy: Rory J. Malek, Colin A. Bill, Charlotte M. Vineszahraa ahmedNo ratings yet
- Safety and Adverse Reaction of Therapeutic Antibodies Against Sars-Cov-2Document26 pagesSafety and Adverse Reaction of Therapeutic Antibodies Against Sars-Cov-2preeti yadavNo ratings yet
- Remdesivir For Severe Acute Respiratory Syndrome Coronavirus 2 Causing Covid 19 An Evaluation of The Evidence Yu Chen Cao All ChapterDocument53 pagesRemdesivir For Severe Acute Respiratory Syndrome Coronavirus 2 Causing Covid 19 An Evaluation of The Evidence Yu Chen Cao All Chapterdora.morales550100% (16)
- Autoimmunity Reviews: SciencedirectDocument9 pagesAutoimmunity Reviews: SciencedirectRia GandaNo ratings yet
- Jurnal Penelitian Meta AnalisisDocument10 pagesJurnal Penelitian Meta Analisisraihanul khairiNo ratings yet
- 1 s2.0 S2213398420301767 MainDocument9 pages1 s2.0 S2213398420301767 MainNunungTriwahyuniNo ratings yet
- Ebook Remdesivir For Severe Acute Respiratory Syndrome Coronavirus 2 Causing Covid 19 An Evaluation of The Evidence PDF Full Chapter PDFDocument63 pagesEbook Remdesivir For Severe Acute Respiratory Syndrome Coronavirus 2 Causing Covid 19 An Evaluation of The Evidence PDF Full Chapter PDFcarol.thompson605100% (26)
- SARS-CoV-2 X ERDocument6 pagesSARS-CoV-2 X ERJulia MouraNo ratings yet
- Clinical Observation and Management of COVID-19 PatientsDocument5 pagesClinical Observation and Management of COVID-19 PatientsJasper VanhaerenNo ratings yet
- 1 s2.0 S1156523321000585 MainDocument4 pages1 s2.0 S1156523321000585 MainAna PerfeitoNo ratings yet
- New Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For Covid 19 Christian A Devaux Full ChapterDocument29 pagesNew Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For Covid 19 Christian A Devaux Full Chapternorman.pregler293100% (12)
- 1 s2.0 S2590059523001930 MainDocument10 pages1 s2.0 S2590059523001930 MainHarithaNo ratings yet
- Inflammation, Immunity and Potential Target Therapy of SARS-COV-2 ADocument23 pagesInflammation, Immunity and Potential Target Therapy of SARS-COV-2 AShukr Wesman BlbasNo ratings yet
- Passive Immunotherapeutics COVID 19Document11 pagesPassive Immunotherapeutics COVID 19Daniel PratamaNo ratings yet
- Insight Into 2019 Novel Coronavirus An Updated Intrim Review and Lessons From Sars Cov and Mers Cov Mingxuan Xie Download 2024 Full ChapterDocument45 pagesInsight Into 2019 Novel Coronavirus An Updated Intrim Review and Lessons From Sars Cov and Mers Cov Mingxuan Xie Download 2024 Full Chaptertom.beckett574100% (11)
- PRL CovidDocument8 pagesPRL Covidzainy zehraNo ratings yet
- Ebook New Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For Covid 19 PDF Full Chapter PDFDocument28 pagesEbook New Insights On The Antiviral Effects of Chloroquine Against Coronavirus What To Expect For Covid 19 PDF Full Chapter PDFglenn.mcdonald396100% (24)
- Medical HypothesesDocument5 pagesMedical Hypothesesnow youloseNo ratings yet
- Preprints ChloroquineDocument24 pagesPreprints ChloroquineJorgelina BernetNo ratings yet
- COVID 19 An Emerging Coronavirus Infection Advances and Prospects in Designing and Developing Vaccines Immunotherapeutics and TherapeuticsDocument8 pagesCOVID 19 An Emerging Coronavirus Infection Advances and Prospects in Designing and Developing Vaccines Immunotherapeutics and TherapeuticsCertaf MaghnjaNo ratings yet
- Can Phytotherapy With Polyphenols Serve As A Powerful Approach For The Prevention and Therapy Tool of Novel Coronavirus Disease 2019? 2020Document20 pagesCan Phytotherapy With Polyphenols Serve As A Powerful Approach For The Prevention and Therapy Tool of Novel Coronavirus Disease 2019? 2020Kelly DickinsonNo ratings yet
- Treatment Options For Covid 19 The Reality and Challenges Shio Shin Jean Download 2024 Full ChapterDocument47 pagesTreatment Options For Covid 19 The Reality and Challenges Shio Shin Jean Download 2024 Full Chaptermari.artrip178100% (10)
- 11 PDF FSLCE Biology QPDocument21 pages11 PDF FSLCE Biology QPishikamani07No ratings yet
- Mice Rats in Biomedical Research FBRDocument2 pagesMice Rats in Biomedical Research FBRChikondi TemboNo ratings yet
- Cancer ImmunotherapyDocument15 pagesCancer Immunotherapyqud86100% (1)
- Journal RefstylesDocument27 pagesJournal RefstylesChun-Yi YangNo ratings yet
- Genetics Practice ProbsDocument4 pagesGenetics Practice Probsajaysharma19686191No ratings yet
- Class 7 Science Chapter 1 Revision NotesDocument2 pagesClass 7 Science Chapter 1 Revision NotesRao Saijal YadavNo ratings yet
- KM5-2560 MicrobiologicalBestPracticeDocument64 pagesKM5-2560 MicrobiologicalBestPracticeAbid IqbalNo ratings yet
- h24 Dstrainingguide Usen Rev03Document5 pagesh24 Dstrainingguide Usen Rev03Elisan BrasilNo ratings yet
- Chapter 31 - HematopoiesisDocument20 pagesChapter 31 - HematopoiesisMauricio AndrésNo ratings yet
- DLL Science Quarter 2 Week 1-9Document24 pagesDLL Science Quarter 2 Week 1-9Argie PiaNo ratings yet
- Blood & Immunology McqsDocument6 pagesBlood & Immunology McqsAbdullah TheNo ratings yet
- Bioteknologi Farmasi PendahuluanDocument65 pagesBioteknologi Farmasi PendahuluanNadhifa MukarommNo ratings yet
- Patentability of Biotech Subject MatterDocument136 pagesPatentability of Biotech Subject MatterGareth WealeNo ratings yet
- Chapter 4Document6 pagesChapter 4Kate Wen GuanNo ratings yet
- Revised Syllabus - Degree Module Approved by 24th AC Meeting Held On 6th May 2017 PDFDocument153 pagesRevised Syllabus - Degree Module Approved by 24th AC Meeting Held On 6th May 2017 PDFUjual BasnetNo ratings yet
- Course Structure Course: Bio101 Essentials of Biology, Lab (4 CR) PrerequisiteDocument2 pagesCourse Structure Course: Bio101 Essentials of Biology, Lab (4 CR) PrerequisiteAaron ChongNo ratings yet
- GeneticDocument3 pagesGeneticbebaNo ratings yet
- Pages From 1-Molecular Cell Biology Lodish 5Th EdDocument4 pagesPages From 1-Molecular Cell Biology Lodish 5Th Edapi-3733156100% (1)
- CH 15 WorkbookDocument10 pagesCH 15 Workbookapi-237586441100% (1)
- Anavar (Oxandrolone)Document26 pagesAnavar (Oxandrolone)illicitdrugsNo ratings yet
- PIGMENTS Mbbs - Dr. SuchitaDocument53 pagesPIGMENTS Mbbs - Dr. SuchitaRushi VaghelaNo ratings yet
- The Fetal Period: by DR - Abdallah GreeballahDocument55 pagesThe Fetal Period: by DR - Abdallah GreeballahrawanNo ratings yet
- Synopsis, FormatDocument14 pagesSynopsis, FormatHira Hameed100% (1)
- S2 - Ch06 - Biotransformation of XenobioticsDocument92 pagesS2 - Ch06 - Biotransformation of XenobioticsWachi PampasNo ratings yet
- Worksheets: Digestive SystemDocument9 pagesWorksheets: Digestive SystemAbigailBarrionGutierrezNo ratings yet
- Resilience Definitions Theory and ChallengesDocument14 pagesResilience Definitions Theory and ChallengesRaji Rafiu BoyeNo ratings yet
- Muscle HistologyDocument50 pagesMuscle HistologyKhalid H MuseNo ratings yet