Professional Documents
Culture Documents
Case Analysis - Questions
Case Analysis - Questions
Uploaded by
danicaCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Activity 3.5 Feedback Mechanisms Involved in Regulating Processes in The Female Reproductive System (Menstrual Cycle) - 084506Document1 pageActivity 3.5 Feedback Mechanisms Involved in Regulating Processes in The Female Reproductive System (Menstrual Cycle) - 084506Megan WolvesNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Comprehensive Sexuality Education Learning Area: Araling Panlipunan Grades 1-10Document30 pagesComprehensive Sexuality Education Learning Area: Araling Panlipunan Grades 1-10Jamaica Castillo100% (3)
- Islam, The Quran, and The Five Pillars All Without A Flamewar: Crash Course World History #13Document6 pagesIslam, The Quran, and The Five Pillars All Without A Flamewar: Crash Course World History #13danicaNo ratings yet
- Discharge Instructions For Thyroidectomy: Medications Your IncisionDocument2 pagesDischarge Instructions For Thyroidectomy: Medications Your IncisiondanicaNo ratings yet
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term GoalsDocument3 pagesNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term GoalsdanicaNo ratings yet
- Electrical Burn PathophysiologyDocument1 pageElectrical Burn PathophysiologydanicaNo ratings yet
- Data Collection Procedure Qualitative Data Collection ProcedureDocument3 pagesData Collection Procedure Qualitative Data Collection ProceduredanicaNo ratings yet
- DiaryDocument2 pagesDiarydanicaNo ratings yet
- Geographic Location: Cordillera Administrative RegionDocument6 pagesGeographic Location: Cordillera Administrative RegiondanicaNo ratings yet
- Physiology of The Female Reproductive System: Liu Wei Department of Ob & Gy Ren Ji HospitalDocument24 pagesPhysiology of The Female Reproductive System: Liu Wei Department of Ob & Gy Ren Ji HospitalAmanuel MaruNo ratings yet
- Midwife Led Care BelgiumDocument19 pagesMidwife Led Care BelgiumsinarNo ratings yet
- Pituitary Gland (Hypophysis Cerebri) .PPTX Version 12516491886836300388Document26 pagesPituitary Gland (Hypophysis Cerebri) .PPTX Version 12516491886836300388ritika lamaNo ratings yet
- Sex Tips From A WomanDocument2 pagesSex Tips From A WomanjayadevmotamarriNo ratings yet
- 2 Jurnal Pengaruh Pemberian Minuman Jahe EmpritDocument6 pages2 Jurnal Pengaruh Pemberian Minuman Jahe EmpritMeilani JuneldiNo ratings yet
- Lab Reproductive SDocument8 pagesLab Reproductive SJoyce TorcuatorNo ratings yet
- (Code No. 044) : Term - IDocument6 pages(Code No. 044) : Term - IA KumarNo ratings yet
- Efektifitas Terapi Musik Klasik Lullaby Terhadap Kecemasan Pada Ibu Hamil Trimester IiiDocument6 pagesEfektifitas Terapi Musik Klasik Lullaby Terhadap Kecemasan Pada Ibu Hamil Trimester IiiZeviNo ratings yet
- Review: Diagnosis and Management of Premature Ovarian FailureDocument6 pagesReview: Diagnosis and Management of Premature Ovarian FailureKhong Jac MunNo ratings yet
- Jurnal Plasenta PreviaaDocument41 pagesJurnal Plasenta PreviaacimyNo ratings yet
- Yr 8 WK 2 Bio NoteDocument3 pagesYr 8 WK 2 Bio Notesedrick ocheNo ratings yet
- Final NSVD Short PaperDocument90 pagesFinal NSVD Short PaperACOB, Jamil C.No ratings yet
- Emergency Contraception Use Among Undergraduate Students of The University of Professional Studies - July 2016Document89 pagesEmergency Contraception Use Among Undergraduate Students of The University of Professional Studies - July 2016fzguokeNo ratings yet
- Reproductive Health MindmapDocument11 pagesReproductive Health MindmapSuyagya PundirNo ratings yet
- B Vitamins, Polycystic Ovary Syndrome, and FertilityDocument6 pagesB Vitamins, Polycystic Ovary Syndrome, and FertilityPaolo MessinaNo ratings yet
- Garbhini Case PDFDocument5 pagesGarbhini Case PDFBhavya ParmarNo ratings yet
- Antenatal Care in TanzaniaDocument32 pagesAntenatal Care in TanzaniaMichael NyaongoNo ratings yet
- Pink Intimate Brochure PromoitaliaDocument2 pagesPink Intimate Brochure PromoitaliaSkin365 Pty LtdNo ratings yet
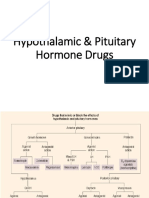
- Hypothalamic & Pituitary Hormone DrugsDocument29 pagesHypothalamic & Pituitary Hormone DrugsDylan MansillaNo ratings yet
- Q2 G5 DLL Oct.31-Nov.4-2022Document33 pagesQ2 G5 DLL Oct.31-Nov.4-2022Mylene DiazNo ratings yet
- PopulationControl in BitchesDocument16 pagesPopulationControl in BitchesDaksh SabharwalNo ratings yet
- 3.3 Fertility TestingDocument57 pages3.3 Fertility Testing21 - Tuazon, AlliahNo ratings yet
- Ordinance No. 2020-09-1Document6 pagesOrdinance No. 2020-09-1Marinel Sese100% (1)
- Ebook Current Diagnosis Treatment Obstetrics Gynecology 12Th Edition Lauren Nathan Online PDF All ChapterDocument69 pagesEbook Current Diagnosis Treatment Obstetrics Gynecology 12Th Edition Lauren Nathan Online PDF All Chaptermichael.gibbs966100% (8)
- How To Do An AbortionDocument5 pagesHow To Do An AbortionShien Brojas OropesaNo ratings yet
- Normal & Abnormal Uterine ActionDocument39 pagesNormal & Abnormal Uterine ActionAy Alex100% (2)
- New TIP Course 6 DepEd TeacherDocument100 pagesNew TIP Course 6 DepEd TeacherHelen HidlaoNo ratings yet
- Angela Davis-Modern Motherhood - Women and Family in England, 1945-2000-Manchester University Press (2012)Document251 pagesAngela Davis-Modern Motherhood - Women and Family in England, 1945-2000-Manchester University Press (2012)MarinaNo ratings yet
Case Analysis - Questions
Case Analysis - Questions
Uploaded by
danicaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Analysis - Questions
Case Analysis - Questions
Uploaded by
danicaCopyright:
Available Formats
Danica Taguiam DRE, VIA, & Ultz Preparation 09-30-2020
A5
I. QUESTIONS:
1. Thirty days post Dilatation and Curretage, Is it recommended for patient Maitha to
have VIA? Why and why not? What are the indications of VIA?
I believe No, because maitha has undergone D & C just 30 days after the procedure her cervix is still
healing and recovering. And it was also observe that after the procedure maitha has experience active
vaginal bleeding which is a possible sign of infection prior to post D & C, which means that it needs
more time to heal and recover. Stated by familydoctor.org (2019), there are some risks to a D and C.
You could get an infection in your uterus/cervix. To help prevent this, avoid putting anything in your
vagina following the procedure. This includes tampons, douches, and some forms of birth control
(familydoctor.org, 2019), in which we can add to this the avoidance of doing VIA after a post D & C.
Since VIA involve the application of acetic acid in the cervix. However, Maitha can still opt to undergo
VIA but not as early as 30 days post D & C, since she is 39 yrs old and is eligible to do VIA test.
Indication includes the ff: 1.All women within the eligible age (30-49years old) attending the cervical
cancer screening clinic for the first time should have VIA, provided the screening protocol
recommends the test. 2. VIA can be done during menstruation if the woman is not bleeding heavily
(Abad et.al. 2020).
2. Before the doctor conducted D and C, What kind of ultrasound did she have? Why?
Give 3 nursing responsibilities you will perform to patient Maitha in preparing the
ultrasound.
Transvaginal Ultrasound, because it helps to determine vaginal bleeding also to see if there is any
abnormality in the uterus (womb), cervix (the neck of the womb), endometrium (lining of the womb),
fallopian tubes, ovaries, bladder or the pelvic cavity prior to D & C. This helps the physician to avoid
missing any structural findings (eg, polyps or fibroids) that may be inside the uterus, cervix, and
endometrium to take a sample of the most visibly abnormal areas prior to D & C.
Explain the reasons for performing the procedure to the patient and inform patients that the
examination may be uncomfortable.
Instruct patient to empty bladder prior to transvaginal ultrasound.
Assist patient to the examining table, help her to undress and drape her for privacy.
3. Give 3 independent nursing interventions addressing the vaginal bleeding.
Assess vital signs, especially the blood pressure and monitor for signs of shock.
Place the patient on bed rest with legs elevated to helps venous return and slows bleeding.
Collect and save all perineal pads used during bleeding and weigh them to determine the
amount of blood loss.
4. What is the purpose of oxygen therapy?
Since the patient is experiencing active vaginal bleeding there is decreased in blood circulation that
carries oxygen causing the patient to experience difficulty of breathing, changes in the color of the
skin, tachycardia, hypotension etc. By administering oxygen it increases the amount of oxygen carried
by available hemoglobin in the blood to compensate to the bleeding.
5. Give 6 nursing responsibilities you will perform before (2), during (2) and after (2)
patient Maitha's Blood Transfusion
Before
Verify the BT order, double-check the order for transfusion and correlate this with the clinical
diagnosis and care plan of the patient.
Acquire blood specimens quickly, to obtain baseline complete blood count, and to type and
crossmatch the blood in anticipation of blood transfusions.
During
Obtain vital signs prior to the start of the BT and several times during the BT (At the first 5 minutes
after starting the transfusion;15 minutes after transfusion started; on the 30 th minute; and every hour
until the transfusion is done).
Observe/Assess patient on an on-going basis for any untoward signs and symptoms such as flushed
skin, chills, elevated temperature, itchiness, urticaria, and dyspnea. If any of these symptoms occur,
stop the transfusion, open the IV line with Plain NSS and regulate accordingly, and report to the
doctor immediately.
After
Once transfusion is done, the line should be flushed with normal saline solution. If there are no more
succeeding transfusions, the line is discontinued, and the BT set is disposed properly.
Continue to monitor vital signs 1 hour after the transfusion is over and instruct to report delayed
reaction to the transfusion such as nausea, swelling, jaundice, or an itchy rash.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Activity 3.5 Feedback Mechanisms Involved in Regulating Processes in The Female Reproductive System (Menstrual Cycle) - 084506Document1 pageActivity 3.5 Feedback Mechanisms Involved in Regulating Processes in The Female Reproductive System (Menstrual Cycle) - 084506Megan WolvesNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Comprehensive Sexuality Education Learning Area: Araling Panlipunan Grades 1-10Document30 pagesComprehensive Sexuality Education Learning Area: Araling Panlipunan Grades 1-10Jamaica Castillo100% (3)
- Islam, The Quran, and The Five Pillars All Without A Flamewar: Crash Course World History #13Document6 pagesIslam, The Quran, and The Five Pillars All Without A Flamewar: Crash Course World History #13danicaNo ratings yet
- Discharge Instructions For Thyroidectomy: Medications Your IncisionDocument2 pagesDischarge Instructions For Thyroidectomy: Medications Your IncisiondanicaNo ratings yet
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term GoalsDocument3 pagesNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term GoalsdanicaNo ratings yet
- Electrical Burn PathophysiologyDocument1 pageElectrical Burn PathophysiologydanicaNo ratings yet
- Data Collection Procedure Qualitative Data Collection ProcedureDocument3 pagesData Collection Procedure Qualitative Data Collection ProceduredanicaNo ratings yet
- DiaryDocument2 pagesDiarydanicaNo ratings yet
- Geographic Location: Cordillera Administrative RegionDocument6 pagesGeographic Location: Cordillera Administrative RegiondanicaNo ratings yet
- Physiology of The Female Reproductive System: Liu Wei Department of Ob & Gy Ren Ji HospitalDocument24 pagesPhysiology of The Female Reproductive System: Liu Wei Department of Ob & Gy Ren Ji HospitalAmanuel MaruNo ratings yet
- Midwife Led Care BelgiumDocument19 pagesMidwife Led Care BelgiumsinarNo ratings yet
- Pituitary Gland (Hypophysis Cerebri) .PPTX Version 12516491886836300388Document26 pagesPituitary Gland (Hypophysis Cerebri) .PPTX Version 12516491886836300388ritika lamaNo ratings yet
- Sex Tips From A WomanDocument2 pagesSex Tips From A WomanjayadevmotamarriNo ratings yet
- 2 Jurnal Pengaruh Pemberian Minuman Jahe EmpritDocument6 pages2 Jurnal Pengaruh Pemberian Minuman Jahe EmpritMeilani JuneldiNo ratings yet
- Lab Reproductive SDocument8 pagesLab Reproductive SJoyce TorcuatorNo ratings yet
- (Code No. 044) : Term - IDocument6 pages(Code No. 044) : Term - IA KumarNo ratings yet
- Efektifitas Terapi Musik Klasik Lullaby Terhadap Kecemasan Pada Ibu Hamil Trimester IiiDocument6 pagesEfektifitas Terapi Musik Klasik Lullaby Terhadap Kecemasan Pada Ibu Hamil Trimester IiiZeviNo ratings yet
- Review: Diagnosis and Management of Premature Ovarian FailureDocument6 pagesReview: Diagnosis and Management of Premature Ovarian FailureKhong Jac MunNo ratings yet
- Jurnal Plasenta PreviaaDocument41 pagesJurnal Plasenta PreviaacimyNo ratings yet
- Yr 8 WK 2 Bio NoteDocument3 pagesYr 8 WK 2 Bio Notesedrick ocheNo ratings yet
- Final NSVD Short PaperDocument90 pagesFinal NSVD Short PaperACOB, Jamil C.No ratings yet
- Emergency Contraception Use Among Undergraduate Students of The University of Professional Studies - July 2016Document89 pagesEmergency Contraception Use Among Undergraduate Students of The University of Professional Studies - July 2016fzguokeNo ratings yet
- Reproductive Health MindmapDocument11 pagesReproductive Health MindmapSuyagya PundirNo ratings yet
- B Vitamins, Polycystic Ovary Syndrome, and FertilityDocument6 pagesB Vitamins, Polycystic Ovary Syndrome, and FertilityPaolo MessinaNo ratings yet
- Garbhini Case PDFDocument5 pagesGarbhini Case PDFBhavya ParmarNo ratings yet
- Antenatal Care in TanzaniaDocument32 pagesAntenatal Care in TanzaniaMichael NyaongoNo ratings yet
- Pink Intimate Brochure PromoitaliaDocument2 pagesPink Intimate Brochure PromoitaliaSkin365 Pty LtdNo ratings yet
- Hypothalamic & Pituitary Hormone DrugsDocument29 pagesHypothalamic & Pituitary Hormone DrugsDylan MansillaNo ratings yet
- Q2 G5 DLL Oct.31-Nov.4-2022Document33 pagesQ2 G5 DLL Oct.31-Nov.4-2022Mylene DiazNo ratings yet
- PopulationControl in BitchesDocument16 pagesPopulationControl in BitchesDaksh SabharwalNo ratings yet
- 3.3 Fertility TestingDocument57 pages3.3 Fertility Testing21 - Tuazon, AlliahNo ratings yet
- Ordinance No. 2020-09-1Document6 pagesOrdinance No. 2020-09-1Marinel Sese100% (1)
- Ebook Current Diagnosis Treatment Obstetrics Gynecology 12Th Edition Lauren Nathan Online PDF All ChapterDocument69 pagesEbook Current Diagnosis Treatment Obstetrics Gynecology 12Th Edition Lauren Nathan Online PDF All Chaptermichael.gibbs966100% (8)
- How To Do An AbortionDocument5 pagesHow To Do An AbortionShien Brojas OropesaNo ratings yet
- Normal & Abnormal Uterine ActionDocument39 pagesNormal & Abnormal Uterine ActionAy Alex100% (2)
- New TIP Course 6 DepEd TeacherDocument100 pagesNew TIP Course 6 DepEd TeacherHelen HidlaoNo ratings yet
- Angela Davis-Modern Motherhood - Women and Family in England, 1945-2000-Manchester University Press (2012)Document251 pagesAngela Davis-Modern Motherhood - Women and Family in England, 1945-2000-Manchester University Press (2012)MarinaNo ratings yet