Professional Documents
Culture Documents
Pharma Midterms Review Uwu
Pharma Midterms Review Uwu
Uploaded by
AJ Bay0 ratings0% found this document useful (0 votes)
59 views11 pagesThe document summarizes drugs that act on the autonomic nervous system. It describes two main divisions - the sympathetic and parasympathetic nervous systems. The sympathetic system uses norepinephrine as a neurotransmitter and is involved in fight or flight responses. The parasympathetic uses acetylcholine and is involved in rest and digest functions. It categorizes drugs that act as agonists or antagonists on adrenergic and cholinergic receptors in these systems and provides examples of drugs that directly or indirectly act on the sympathetic and parasympathetic nervous systems.
Original Description:
Original Title
pharma midterms review uwu
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document summarizes drugs that act on the autonomic nervous system. It describes two main divisions - the sympathetic and parasympathetic nervous systems. The sympathetic system uses norepinephrine as a neurotransmitter and is involved in fight or flight responses. The parasympathetic uses acetylcholine and is involved in rest and digest functions. It categorizes drugs that act as agonists or antagonists on adrenergic and cholinergic receptors in these systems and provides examples of drugs that directly or indirectly act on the sympathetic and parasympathetic nervous systems.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
59 views11 pagesPharma Midterms Review Uwu
Pharma Midterms Review Uwu
Uploaded by
AJ BayThe document summarizes drugs that act on the autonomic nervous system. It describes two main divisions - the sympathetic and parasympathetic nervous systems. The sympathetic system uses norepinephrine as a neurotransmitter and is involved in fight or flight responses. The parasympathetic uses acetylcholine and is involved in rest and digest functions. It categorizes drugs that act as agonists or antagonists on adrenergic and cholinergic receptors in these systems and provides examples of drugs that directly or indirectly act on the sympathetic and parasympathetic nervous systems.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 11
- It is located in the postganglionic
Pharmacology Review. sympathetic nerve endings
- Inhibits the release of norepinephrine
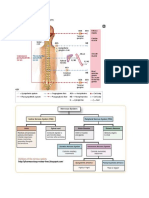
AUTONOMOUS NERVOUS SYSTEM (ANS) DRUGS - Vasodilation; decreases central
sympathetic outflow
Autonomous Nervous System c) Beta 1
It is a division of PNS that acts on smooth muscles - Found in the heart and some in the
and glands. kidney
Also known as visceral system. - Increases heart rate
It controls and regulates the heart, respiratory system, d) Beta 2
GI, bladder, eyes and glands. - Located in the smooth muscles of lungs,
It is involuntary system, which solely means that it GI tract, liver and uterine muscles.
has “little or no control”. - Bronchodilation
It has two sets of neurons: e) D1
1. Afferent (Sensory) Neurons – sends signals - Vasodilation in splanchnic (abdomen)
towards the CNS and renal vessels
2. Efferent (Motor) Neurons – receives the
information and then makes the response NOTE. Other are dopaminergic such as located in the renal,
mesenteric, coronary and cerebral arteries. ONLY
It has two branches (efferent [motor] neurons):
DOPAMINE CAN ACTIVATE THESE.
1. Sympathetic Nervous System
(Sympathomimetic)
Inactivation of Neurotransmitters
- Also known as adrenergic system
1. Reuptake of the neurotransmitter back into the neuron
- NEUROTRANSMITTER:
2. Enzymatic transformation/degradation
Norepinephrine (It is released from the
3. Diffusion away from the receptor
terminal nerve ending and stimulates the
cell receptors to produce a response).
9 The receptors being “stimulated” These 2 enzymes inactivate norepinephrine.
are the adrenergic receptor organ 1. Monoamine Oxidase
cells 2. Catechol-O-Methyltransferase
Beta 1
Beta 2 Classification of Sympathomimetics
Alpha 1 1. Direct-Acting Sympathomimetics
Alpha 2 - Stimulate adrenergic receptors
2. Parasympathetic Nervous System - Ex. Norepinephrine, Epinephrine
(Parasympathomimetic) -
- Also known as cholinergic system. 2. Indirect-Acting Sympathomimetics
- NEUROTRANSMITTER: Acetylcholine - Stimulate the release of norepinephrine from the
(It stimulates the receptor cells (muscarine terminal nerve endings.
and nicotine) to produce a response but - Ex. Amphetamine
ACETYLCHOLINESTERASE may -
inactivate AchE before it reaches the 3. Mixed-Acting Sympathomimetics
receptors). - Stimulate the adrenergic receptors and the releases
of norepinephrine from the terminal nerve
NOTE. The sympathetic and parasympathetic nervous system endings.
may act as stimulants or depressants. - Ex. Ephedrine, Pseudoephedrine
Adrenergic Agonists CATHECOLAMINES
They mimic the neurotransmitter norepinephrine and Chemical structures that can produce a
the epinephrine of the SNS. sympathomimetic response.
Adrenergic Receptors Ex. Epinephrine, Norepinephrine, Dopamine
o ALPHA-ADRENERGIC – located in the blood
vessels, eyes, bladder and prostate.
Side Effects of Sympathomimetics
a) Alpha 1
- It is located into the vascular tissues Hypertension Dizziness
- Vasoconstriction, increases BP Tachycardia Urinary difficulty
Palpitation N/V
b) Alpha 2 Dysrhythmia
Tremors
Direct-Acting Adrenergic Agonists Many are non-selective.
Epinephrine
Stimulates alpha 1, beta 1 and 2 Direct-Acting Cholinergic Agonists
Not given orally - Activates a tissue response
Administered by SQ, IVa (vastus lateralis), IV,
topical, inhalation, IC. Betanechol
Metabolized in the liver Used for urinary distension
It is used to treat anaphylaxis, cardiac arrest, asthma,
COPD and hemostasis Policarpine
It is a potent inotropic (myocardial contraction To prevent symptoms of xeropthalmia.
strengthening)
Nicotine
Albuterol For smoking cessation
Stimulates beta-2 (beta-2 selective)
It is used for relaxation of bronchial smooth muscle Indirect-Acting Cholinergic Agonists
and bronchodilation - Inhibit the action of the cholinesterase.
Better than isoproterenol 1. Reversible – bind the ChE for several minutes
High doses may affect beta-1 receptor 2. Irreversible – bind the enzyme permanently
Half-life: 2.7 – 6 hours
Endrophonium Chloride (Tensilon)
Side effects:
o Tremors Indirect-acting
5-20 minutes increases muscle strength
o Restlessness
If ptosis, then it may indicated MG.
o Nervousness
It is used to distinguish myasthenia crisis or
o Hypertension (MAOI)
cholinergic crisis.
o Myasthenia Crisis – if given to patient, muscle
Dopamine
weakness will be alleviated
Stimulates alpha 1, beta 1 and D1
o Cholinergic Crisis – if given to patient, muscle
Used during cardiogenic shock and heart failure
weakness will be severe
Alpha-Adrenergic Blockers/Alpha Blockers
Side Effects:
o Miosis
Beta-Adrenergic Blockers/Beta Blockers o Salivation
Propanolol (Inderal) o N/V
NON-SELECTIVE o Diarrhea
First beta-blocker to treat angina, cardiac o Bradycardia
dysrhythmia and HTN.
Many side effects due to it being non-selective. Neostigmine (Pro-Stigmin)
It is used to treat angina prophylaxis, HTN, Indirect acting
arrythmias, migraine, performance anxiety and It is used to manage/treat myasthenia gravis.
hyperthyroidism It is used in treatment for myotonia gravis and non-
May reduce renin levels reversal, non-depolarizing neuromuscular blockade
Found In breastmilk Side Effects:
o Miosis
Carvedilol and Labetalol o Salivation
It is used for pheochromocytoma o N/V
Combined both alpha and beta blockade. o Diarrhea
o Bradycardia
Atenolol Muscarinic effects are blocked by atropine.
BETA-1 SELECTIVE Half-life: 0.5 – 1 hour
Used to treat angina, HTN and heart failure Given every 2-4 hours
Cholinergic Drugs NOTE. The antidote for myasthenia gravis medication
There are two (2) types of cholinergic receptors toxicity is atropine sulfate. Muscarinic receptor antagonist is
1. Muscarinic – stimulate smooth muscles; slow the a competitive antagonist for Ach.
HR
2. Nicotinic (Neuromuscular) – stimulates/ affects the Atropine
skeletal muscles Muscarinic
Blocks all muscarinic receptors HALF-LIFE: 9-13 hours
Antidote for betanechol. Amphetamines and dextroamphetamine are
Increases heart rate when bradycardia is present. prescribed for narcolepsy and ADHD when
Well absorbed orally and parentally amphetamine-like drugs are ineffective.
Toxicity: (DUMBBELSS)
o Increase temperature Amphetamine-Like Drugs
o Delusion, confusion Methylphenidate and Dexmethylphenidate
o Temp. blindness; blurred vision These are amphetamine-like drugs
o Flush of the face Given to increase a child’s attention span and
o Dryness cognitive performance and to decrease
impulsiveness, hyperactivity, and restlessness.
It is classified as a Controlled Substance Schedule
CNS and PNS DRUGS (CSS) ll drug.
The CNS drugs has limited use of it which are the Administer to children for atleast 30-45 minutes
following: before breakfast and lunch.
o Treatment for ADHD for children. Should be taken 6 hours before sleeping.
o Narcolepsy Transdermal patches may be worn for 9 hours.
o Reversal respiratory distress It inhibits metabolism of barbiturates, which leads
to increased blood vessels.
The major groups are the following:
1. Amphetamine and Caffeine Educate pt. to avoid foods that contain caffeine.
- Stimulates the cerebral cortex of the brain Report for tachycardia and palpitations.
- Abused and is only used for short-term (up Monitor for children onset of Tourette Syndrome.
to 12 weeks)
2. Analeptics and Caffeine Modafinil
- Acts on the brainstem and medulla to Increases wakefulness of the pt.
stimulate respiration
3. Anorexiants Anorexiants
- Suppress appetite by stimulating satiety Suppress appetite
center in the hypothalamic and limbic areas For wt. loss
of the brain. Children younger than 12 years should not be given
anorexiants, and self-medication with anorexiants
Illnesses in Relation to CNS and PNS Drugs should be discouraged.
ADHD Long-term use of these drugs frequently results in
Characteristics behaviors of the various types of such severe side effects such as nervousness,
ADHD include inattentiveness, inability to restlessness, irritability, insomnia, heart
concentrate, restlessness (fidgety), hyperactivity palpitations, and hypertension.
(excessive and purposeless activity), inability to
complete tasks, and impulsivity.
Abnormal electroencephalograph (EEG) findings Analeptics
Learning disability It has 2 subgroups:
1. Xanthines (Methylxanthines)
Narcolepsy 2. Theophylline
Falling asleep during normal waking activities - It is used to relax bronchioles
SLEEP PARALYSIS – muscle paralysis during - Used to increase respiration for NB.
sleep; accompanied by narcolepsy Caffeine
With the help of caffeine, it stimulates the CNS,
Amphetamines while larger doses of analeptics may lead to
Stimulate the release of dopamine and stimulation of respiration.
norepinephrine. Side effects are similar to anorexiants.
It normally causes euphoria and increase alertness. Other side effects:
It may also cause: o Diuresis (increased urination)
o Insomnia o GI irritation (e.g. nausea, diarrhea)
o Restlessness o Tinnitus [RARE]
o Tremors Half-life: 5 hours
o Irritability
o Weight loss CNS Depressants
Continuous use may cause cardiovascular problems Causes varying degrees of depression
These include: [SGAOAAA] 9 It may cause anterograde
o Sedative-Hypnotic amnesia/memory impairment.
o General anesthetics - Small doses only!
o Analgesics
o Opioid and non-opioid analgesics NOTE. Antidote for overdose is FLUMAZENIL.
o Anticonvulsants
o Antipsychotics 3. Nonbenzodiazepines
- Ex. Zolpidem
o Antidepressants
9 A nonbenzodiazepines that differs
in chemical structure from
Sedative Hypnotics
benzodiazepines.
It is ordered for treatment of sleep disorders 9 It is used for short-term treatment
It diminishes physical and mental responses at lower (<10 days) of insomnia.
dosages of certain CNS depressants but does not - Advise patients to take nonbenzodiazepines
affect consciousness. before bedtime.
Mostly used during daytime. - Alprazolam takes effect within 15 to 30
Hypnotics maybe short or intermediate acting: minutes
o Short Acting – achieving sleep
o Intermediate Acting – sustaining sleep. Anesthetics
The ideal hypnotic promotes natural sleep without A. Balance Anesthesia
disrupting normal patterns of sleep and produces no - Combination of drugs used in GA.
hangover or undesirable effect. - May include the following:
A hypnotic given the night before
NOTE. Ramelteon the only major sedative-hypnotic Premedication with an opioid analgesic or
approved for long-term use. benzodiazepine (e.g. midazolam) plus an
anticholinergic (e.g. atropine) given about
The following are categories of sedative-hypnotics: 1 hour before surgery to decrease
1. Barbiturates (-barbital) secretions.
Long-Acting Group A short-acting nonbarbiturate such as
- For seizures and epilepsy propofol
- Ex. Phenobarbital Mephobarbital An inhaled gas, often a combination of an
Intermediate-Acting Group inhalation anesthetic, nitrous oxide, and
- For maintaining long periods of sleep. oxygen.
- Ex. Butabarbital A muscle relaxant given as needed
Slow-Acting Group
- For procedure sedation B. General Anesthesia
- Ex. Secobarbital - Used for surgical procedures.
- Stage 4. Medullary Paralysis might cause loss
Pentobarbital or respiration
Increases hepatic enzyme action, causing an
increased metabolism and decreased effects of drugs C. Inhalation Anesthesia (-lanes)
such as oral anticoagulants, glucocorticoids, tricyclic - Used during surgery
antidepressants, and quinidine. - Example.
Pentobarbital may cause hepatoxicity if taken with o Halothane, isoflurane, and enflurane,
large dose of acetaminophen. recovery of consciousness usually occurs
Together with secobarbital they are used for t(x) of in approximately 1 hour.
insomnia. o Desflurane and sevoflurane is within
minutes.
2. Benzodiazepines (-am)
- Induce sleeping D. Intravenous Anesthetics
- Benzodiazepines (except temazepam) can - Used for the induction stage of anesthesia.
suppress stage 4 of NREM sleep, which - Ex. Propofol and Midazolam
may result in vivid dreams or nightmares - It may cause adverse reactions such as:
and can delay REM sleep. o Respiratory and cardiovascular
- Ex. Triazolam depression
9 A short-acting hypnotic with a half-
life of 2 to 5 hours. It does not E. Topical Anesthesia
produce any active metabolites.
F. Local Anesthesia
- Block pain at the site where the drug is Most commonly ordered as sustained-release (SR)
administered by preventing conduction of capsule
nerve impulses For IV:
o 50mg/min – adults
G. Spinal Anesthesia o 25 mg/min – older adults
- Requires that a local anesthetic be injected into It displaces anticoagulants and aspirin
the subarachnoid space. Barbiturates, rifampin, and chronic ingestion of
o Spinal Block - penetration of the ethanol increase hydantoin metabolism
anesthetic into the subarachnoid space o Drugs like sulfonamides and cimetidine can
o Epidural Block – epidural space increase the action of hydantoins by inhibiting
o Caudal Block – sacral hiatus liver metabolism.
Antacids, calcium preparations, sucralfate, and
NOTE. Blood pressure should be monitored during antineoplastic drugs also decrease the absorption of
administration of these types of anesthesia because a decrease hydantoins
in blood pressure resulting from the drug and procedure might Ex. Phenytoin
occur.
Barbiturates
Antiseizure Drugs Prescribed to treat tonic-clonic, partial, and
Used for epileptic seizures myoclonic seizures and status epilepticus, a rapid
Stabilize never cell membranes and suppress the succession of epileptic seizures
abnormal electric impulses in the cerebral cortex Reduce seizures by enhancing the activity of GABA.
Prevent seizures but do not eliminate the cause or THERAPEUTIC RANGE: 20-40 mcg/ml
provide a cure.
Stop medication of after 3-5 years there is no Benzodiazepines
occurrence of seizure. CLONAZEPAM - effective in controlling absence
Types of anticovulsants: and myoclonic seizures, but tolerance may occur 6
o Hydantoins (Phenytoin) months after drug therapy starts.
o Long-acting Barbiturates CLORAZEPATE DIPOTASSIUM - treating
o Benzodiazepines partial seizures.
o Succinimides DIAZEPAM - treat status epilepticus
o Carbamazepine Ex. Clonazepam, clorazepate dipotassium,
o Valproate lorazepam, and diazepam
Physiology of anticonvulsants:
1. Suppressing sodium influx Succinimides
o Phenytoin, fosphenytoin, Used to treat absent seizures
carbamazepine, oxcarbazepine, Decrease calcium influx
valproic acid, topiramate, Ex. Ethosuximide
zonisamide, and lamotrigine. 9 THERAPEUTIC RANGE: 40- 100
2. Suppressing calcium influx mcg/ml.
o Valproic acid and ethosuximide.
3. Increase the action of gamma-aminobutyric Carbamazepine
acid (GABA) It is used to control tonic-clonic and partial seizures.
o Barbiturates, benzodiazepines, and THERAPEUTIC RANGE: 4-12 mcg/ml.
tiagabine.
Valproate
Hydantoins For mixed-type of seizures.
Suppressing sodium influx
Stabilize cell membranes Drugs for Parkinson’s Disease
Reduce receptive neural firing PARKINSON’S D(X): It is a chronic, progressive,
Limit seizures and neurologic disorder that affects the
Newborns, persons with liver disease, and older extrapyramidal motor tract, which controls posture,
adults require a lower dose because of a decrease in balance, and locomotion.
metabolism that results in more available drug Pseudoparkinsonism – adverse reaction from:
THERAPEUTIC RANGE: 10-20 mcg/ml o Chloropromazine
ONSET OF ACTION: 30 minutes – 2 hours o Haloperidol
PEAK CONCENTRATION: 1.5 – 6 hours o Lithium
o Methyldopa
o Metoclopramide Pt. who does not respond to AchE inhibitors may
o Reserpine use prednisone instead, if lower dose, add
azathioprine.
Anticholinergics 9 WBC count and liver enzymes should be
Reduce the rigidity and some of the tremors closely monitored to avoid leukopenia and
characteristic of Parkinson’s disease but have a hepatoxicity.
minimal effect on bradykinesia.
Decrease salivation Skeletal Muscle Relaxant
Ex. Trihexyphenidyl and Benztropine Relieve muscular spasms and pain associated with
traumatic injuries and spasticity form chronic
Dopaminergics (-dopa) debilitating disorders (e.g. MS, stroke, cerebral palsy,
LEVODOPA – first dopaminergic drug head and spinal cord injuries).
9 Effective in diminishing symptoms of o SPASTICITY - increased muscle tone from
Parkinson’s disease and increasing mobility. hyperexcitable neurons. It is caused by
Combined with CARBIDOPA increase stimulation from the cerebral
9 Inhibit the enzyme dopa decarboxylase neurons or lack of inhibition in the spinal
Urge patients who take high doses of selegiline to cord or at the skeletal muscles
avoid foods high in tyramine such as aged cheese, red Spasticity
wine, cream, yogurt, chocolate, bananas, and raisins Drugs used to treat spasticity are:
to prevent crisis o Baclofen
Urge patients taking amantadine to report any signs o Dantrolene
of skin lesions, seizures, or depression o Tizanidine
Advise patients taking bromocriptine to report o Diazepam
symptoms of lightheadedness o Benzodiazepine
Monoamine Oxidase B Inhibitor (-gilines) Muscle Spasm
MAO-B causes catabolism of dopamine A great expection for cyclobenzaprine.
SELEGILINE Drugs used to treat muscle spasm are carisoprodol,
9 Inhibits MAO-B and thus prolongs the action chlorzoxazone, cyclobenzaprine, metaxalone,
of levodopa. methocarbamol, and orphenadrine citrate.
9 Large doses of selegiline may inhibit MAO-
A, an enzyme that promotes metabolism of NOTE. The side effects from centrally acting muscle
tyramine in the GI tract. If they are not relaxants include drowsiness, dizziness, lightheadedness,
metabolized by MAO- A, ingestion of foods headaches, and occasional GI sensitivity (e.g. nausea,
high in tyramine- such as aged cheese, red vomiting, abdominal distress).
wine, and bananas- can cause a hypertensive
crisis. Psychiatric Agent
RASAGILINE These include:
9 MAO-B inhibitor used for the treatment of o Antipsychotics
Parkinson’s disease - Also known as neuroleptics
- Drug that modifies psychotic behavior and
Cathecol-O-Methyltransferase Inhibitors (-capone) exerts an antipsychotic effect
Increase the amount of levodopa concentration in the o Anxiolytics
brain. - To treat anxiety and sometimes insomnia
Drugs for Alzheimer’s Diseases Antipsychotics
Acetylcholinesterase Inhibitors It has two main categories namely:
RIVASTIGMINE 1. Typical Antipsychotics
9 Has effective penetration into the CNS, thus - These are divided into 2:
cholinergic transmission is increased I. Phenothiazines
Ex. Donepezil, memantine, galantamine, and Blocks norepinephrine
rivastigmine Ex. Thioxanthines
II. Nonphenothiazines
Drugs for Myasthenia Gravis Ex. Butyrophenones
Acetylcholinesterase Inhibitors (block dopamine)
Ex. Neostigmine and pyridostigmine Other examples.
PYRIDOSTIGMINE -given every 4-6 hours and 9 Dibenzoxazepines,
has an intermediate action 9 Dihydroindolones
9 Thioxanthenes Often given at night.
CLOMIPRAMINE – cause NMS.
2. Atypical Antipsychotics Most common AR: cardiotoxicity
- Ex. Clozapine
- Effective in treating schizophrenia and Selective Serotonin Reuptake Inhibitors
other psychotic disorders in patients Block the reuptake of serotonin into the nerve
who do not respond to or are terminal of the CNS, thereby enhancing its
intolerant of atypical antipsychotic transmission of the serotonergic synapse
AR: EPS and NMS Commonly used to treat depression than are TCAs
Most common side effect is drowsiness. Ex. Fluoxetine, Fluvoxamine, Sertraline, Paroxetine,
Citalopram and Escitalopram
Interaction with grapefruit juice that can lead to
possible toxicity
NONPHENOTHIAZINES
Frequently prescribed nonphenothiazines is Fluoxetine
haloperidol. S/E:
Administration precautions should be taken to o Dry mouth, blurred vision, insomnia, headache,
prevent soreness and inflammation at the injection nervousness, anorexia, nausea, diarrhea, and
site. suicidal ideation.
Medication is a viscous liquid, a large-gauge needle
(e.g. 21 gauge) should be used with the Z-track Monoamine Oxidase Inhibitors
method for administration in a deep muscle. Inactivates norepinephrine, dopamine, epinephrine,
Use to control psychosis and to decrease agitation in and serotonin.
adults and children MAO-A and MAO-B are found in the liver and the
brain.
Anxiolytics o MAO-A: Inactivates dopamine in the brain
It is used to treat anxiety and insomnia o MAO-B: Inactivates norepinephrine and
BENZODIAZEPINE. serotonin.
Benzodiazepine are considered more effective than Ex. Tranylcypromine Sulfate, Isocarboxazid,
barbiturates because they enhance the action of Selegiline HCl, Phenelzine Sulfate.
gamma aminobutyric acid (GABA), an inhibitory
neurotransmitter within the CNS. Mood Stabilizers
It is used to treat bipolar affective disorder
Antidepressant Drugs
Ex. Lithium (Antimania), Carbamazepine, Valproic
1. Tricyclic antidepressants (TCAs)
acid or Divalproex, and Lamotrigine.
2. Selective serotonin reuptake inhibitors (SSRIs)
Patient may not achieve the desired effect for 5 to 6
3. Serotonin-norepinephrine reuptake inhibitors
days
(SNRIs)
4. Atypical antidepressants that affect the
NOTE. The antipsychotic drugs olanzapine, ziprasidone, and
neurotransmitters
aripiprazole are approved to treat acute mania and mixed
5. Monoamine oxidase inhibitors
episodes of bipolar disorder.
Tricyclic Antidepressants
RESPIRATORY DRUGS
Used to treat major depression because they are
effective and are less expensive.
Lower Respiratory Disorders
Block the uptake of the neurotransmitters,
Common Colds
norepinephrine and serotonin in the brain
Acute Rhinitis
Ex. Imipramine [t(x) for enuresis].
Allergic Rhinitis
POLYDRUG THERAPY - The practice of giving
several antidepressants or antipsychotics together,
Antihistamines
should be avoided if possible because of potential
Blocks the release of histamine (the chemical
side effects.
mediator for inflammation which causes increase of
It elevates mood, increases interest in daily living and
secretions and bronchoconstriction.
activity, and decreases insomnia.
For acute rhinitis (ig?)
For agitated persons:
o Amitriptyline – can cause EPS
H1 Blocker/Antagonist
o Doxepin
It competes with histamine receptors
o Trimipramine
Relieve respiratory symptoms and allergic conditions - Lack of the alpha-1 antitrypsin protein that
It has 5 classifications: inhibits proteolytic enzymes that destroy
1. Ethanolamines alveoli.
2. Piperazine o Asthma
3. Alkylamines - Inflammatory disorder of the airway walls
4. Phenothiazines associated with a varying amount of airway
5. 1st and 2nd Generation H1 Blockers obstruction.
o 1st Generation - BRONCHIAL ASTHMA. Bronchospasm.
- It causes drowsiness A decrease in forced expiratory volume in 1 second
- It causes sedation and anticholinergic as measured by pulmonary function test.
effects
- Ex. Diphenhydramine Restrictive Lung Disease
o 2nd Generation It is a decrease in total lung capacity as a result of
- Opposite of 1st generation for it fluid accumulation or loss of elasticity of the lung.
doesn’t cause sedation (little) or any It is usually caused by the following:
anticholinergic effects. o Pulmonary edema
- Ex. Cetirizine, Fexofenadine, o Pulmonary fibrosis
Loratadine, Azelastine o Pneumonitis
o Lung tumor
Nasal Decongestant o Thoracic deformities (scoliosis)
Stimulate the alpha-adrenergic receptors which o Myasthenia gravis
leads to vascular constrictions of nasal mucosa.
Medications
Systemic Decongestant Bronchodilators – assist in opening narrow airways
Ex. Pseudoephedrine, Phenyleprine, Ephenperine o Sympathomimetics (adrenergics)
o Parasympatholytics (anticholinergic drugs,
Intranasal Glucocorticoids
ipratropium bromide)
T(x) for allergic rhinitis o Methylxanthines (caffeine, theophylline)
Ex. Beclomethason, Budesonide, Dexamethasone,
Glucocorticoids (steroids) – used to decrease
Flunisolide
inflammation
Leukotriene modifiers – reduce inflammation of the
Antitussives
lung tissue
Suppresses cough reflex of the medulla oblongata
Cromolyn (anti-inflammatory agent) – suppressing
the release of histamine and other mediators from the
LOWER RESPIRATORY DRUGS (book_pharma.exe)
mast cells
Lower Respiratory Disorders Expectorants – loosening mucus from the airways
1. Chronic Obstructive Pulmonary Disease Antibiotics – prevent serious complications from
2. Restrictive Pulmonary/Lung Disease bacterial infections.
IRREVERSIBL
Chronic Obstructive Pulmonary Disease E Bronchodilators
REVERSIBLE
It is caused by airway obstruction with increased Sympathomimetics (Alpha- and Beta-Adrenergic Agonists)
airway resistance of airflow to lung tissues. Increases cAMP (Cyclic Adenosine Monophosphate),
It is usually caused by the following: causing dilation of the bronchioles
o Chronic Bronchitis NON-SELECTIVE SYMPATHOMIMETICS
- A progressive lung disease caused by (Epinephrine) – given subcutaneously to promote
smoking or chronic lung infections. bronchodilation and elevate BP. Administered during
- Productive coughing (excess mucous emergency situation to restore circulation and
secretions result in airway obstruction) increase airway patency.
o Bronchiectasis Beta-2 Adrenergics are given by means of
- Dilation of the bronchi and bronchioles inhalation/oral for people exp. Bronchospasm
- Abnormal frequent infection and (associated with chronic asthma/COPD)
inflammation.
- Breakdown of the epithelium of the Albuterol
bronchial mucosa. A beta-2 adrenergic drug for asthma.
o Emphysema High dose and overuse of this may lead response to
beta-1 receptor
It’s effective for the control of asthma by causing Used for the maintenance t(x) of bronchospasms
bronchodilation with a long duration of action associated with COPD.
Inhalation only with HandiHaler device (dry-powder
Metaproterenol capsule inhaler)
It has some beta-1 effects but it is primarily used as a Side Effects and Adverse Rxn.:
beta-2 agent o Dry mouth
Administered orally or by inhalation o Constipation
o Vomiting
NOTE. o Dyspepsia (pain in upper chest)
Onset of Action o Abdominal pain
INHALATION – 1 minute o Depression
NEBULIZATION – 5-30 minutes o Insomnia
ORAL – 15-30 minutes o Headache
o Joint pain
If pt. is using inhalers and effectivity is not evident, o Peripheral edema
advice the pt. to attach a space device in the inhaler to o Chest pain (during administration)
improve drug delivery to the lung with less disposition
in the mouth. Ipratropium Bromide
It is used to treat asthmatic conditions by dilating the
bronchioles.
Side Effects and Adverse Rxn.
Administered by MDI.
Epinephrine
o Tremors Other Examples of Anticholinergics
o Dizziness Ipratropium bromide
o Hypertension Aclidinium
o Tachycardia Tiotropium
o Heart palpitations Umeclidinium
o Cardiac dysrhythmias
o Angina NOTE. Ipratropium Bromide + Albuterol Sulfate = T(x) for
Beta-2 Adrenergic Drugs (Albuterol) COPD.
o Tremors
o Headaches Methylxanthine Derivatives
o Nervousness Stimulate the CNS and respiration, dilate coronary
o Increased Pulse Rate and pulmonary vessels and cause diuresis.
o Palpation (high doses) It includes the following:
o Increase blood glucose o Aminophylline
o Theophylline
Other Examples of Sympathomimetics o Caffeine
Alpha- and Beta-Adrenergics
o Ephedrine Sulfate Theophylline
o Epinephrine It relaxes the smooth muscles of the bronchi,
Beta-2 Adrenergics bronchioles and pulmonary blood vessels by
o Albuterol inhibiting the enzyme phosphodiesterase, resulting in
o Formoterol an increase in cAMP, which promotes
o Levalbuterol bronchodilation.
o Metaproterenol sulfate THERAPEUTIC RANGE: 5-15 mcg/mL
o Salmeterol TOXICITY: 20 mcg/mL
o Terbutaline sulfate It is well-absorbed by oral administration; absorbed
o Arformoterol tartrate from oral liquids and uncoated plain tablets.
o Indacaterol Food and antacids may decrease the rate but not the
extent of absorption; large volume fluids and high-
o Olodaterol
protein meals may increase the rate of absorption.
It can also be administered by IV.
Side Effects and Adverse Rxn.:
o Anorexia
Anticholinergics
Tiotropium o N/V
o Gastric pain increased by gastric acid secretion
o Intestinal bleeding o IV: Dexamethasone
o Nervousness More effective than beta-2 agonist (reduction of
o Dizziness bronchial hyperresponsiveness)
o Headache It includes the following:
o Irritability o Prednisone
o Cardiac dysrhythmias o Prednisolone
o Tachycardia o Methylprednisolone
o Palpitations o Dexamethasone
o Marked hypotension It can irritate the gastric mucosa and should be taken
o Hyperreflexia with food to avoid ulceration.
o Seizures One inhalation in the morning and night.
o Hyperglycemia Side Effects
o Decreased clotting time o Headache
o Leukocytosis o Euphoria
o Confusion
Leukotriene Receptor Antagonists and Synthesis Inhibitors o Sweating
LEUKOTRIENE – a chemical mediator that can o Hyperglycemia
cause inflammatory changes in the lung. o Insomnia
CYSTEINYL LEUKOTRIENE – promote an o N/V
increase in eosinophil migration, mucous production o Weakness
and aiway wall edema that results in o Menstrual irregularities
bronchoconstriction. Adverse Rxn.:
Effective in reducing the inflammatory symptoms of o Depression
asthma triggered by allergic and environmental o Peptic ulcer
stimuli. o Loss of bone density
NOT RECOMMENDED FOR ASTHMATIC o Development of osteoporosis
ATTACKS o Psychosis
It includes the following drugs:
o Zafirlukast NOTE. Fluticasone propionate + Salmeterol = Controlling
o Zileuton asthma symptoms.
o Montelukast
Cromolyn
Leukotriene Receptor Antagonist T(x) for bronchial asthma
Zafirlukast Inhibits release of histamine and other chemical
First drug in the class of leukotriene modifiers. mediators for inflammation
Reduce the inflammatory process and decreasing Common side effects:
bronchoconstriction. o Postnasal drip
Administered orally. o Irritation of the nose and throat
o Cough
Montelukast
Effectivity will decrease if taken with water
Administered to children (2 years of age)
Can be used with xanthine and beta-adrenergics
SERIOUS SIDE EFFECTS: Rebound
Leukotriene Synthesis Inhibitors
bronchospasm
Zileuton
Decrease the inflammatory process and decreasing
Mucolytics
bronchoconstriction.
Detergents to liquify and loosen mucous secretions so
they can be expectorated.
Glucocorticoids
Ex. Acetylcysteine
It is used to treat respiratory disorders (asthma).
9 Nebulization, bronchopulmonary disorders
Have an anti-inflammatory action and are indicated if
SHOULD NOT BE MIXED WITH OTHER DRUGS
asthma is unresponsive to bronchodilator therapy or
if the pt. has an asthmatic attack while on maximum Bronchodilator should be given 5 minutes before
doses of theophylline. giving mucolytics
Synergistic effect with beta-2 agonist Maybe diluted in softdrinks.
Can be given with the following methods:
Antimicrobial
o MDI Inhaler: Beclomethasone
Ex. Trimethoprim-sulfamethoxazole
o Tablet: Dexamethasone, Prednisone
9 Effective for t(x) of mild to moderate acute
exacerbations of chronic bronchitis (AECBs)
from infectious causes.
You might also like
- Care of Mother, Child and Adolescent (Well-Client)Document2 pagesCare of Mother, Child and Adolescent (Well-Client)AJ Bay100% (4)
- Care of Mother, Child and Adolescent (Well-Client) : Service CapabilityDocument4 pagesCare of Mother, Child and Adolescent (Well-Client) : Service CapabilityAJ Bay100% (3)
- Apportionment Methods - EDITEDDocument45 pagesApportionment Methods - EDITEDAJ BayNo ratings yet
- Sympathetic Receptors and Their Responses: Nervous SystemDocument3 pagesSympathetic Receptors and Their Responses: Nervous Systemjulinka beyla yansonNo ratings yet
- NCM 106 Week 7 ReviewerDocument16 pagesNCM 106 Week 7 ReviewerCrecia Bullecer2No ratings yet
- Pharma Mod 11Document12 pagesPharma Mod 11ANGELA SHANE AGUSTINNo ratings yet
- Pharma - AnsDocument9 pagesPharma - AnsAlyssa Claire TumulakNo ratings yet
- If These Are Stimulated It Produces An Array of Effects in The BodyDocument4 pagesIf These Are Stimulated It Produces An Array of Effects in The BodyAnne Giselle PatocNo ratings yet
- DBMS Notes - Module 02 Section 02 Sympathetic Nervous SystemDocument11 pagesDBMS Notes - Module 02 Section 02 Sympathetic Nervous SystemSaeidreza SardariNo ratings yet
- Sympathomimetics and SympatholyticsDocument3 pagesSympathomimetics and Sympatholyticsbunso padillaNo ratings yet
- FINALSDocument19 pagesFINALSOdyNo ratings yet
- Norepinephrine - Released From Postganglionic: Autonomic Nervous System MedicationsDocument7 pagesNorepinephrine - Released From Postganglionic: Autonomic Nervous System MedicationsJohn denver FloresNo ratings yet
- L9 Sympathomimetics Lytics REVISED 2017 PDFDocument49 pagesL9 Sympathomimetics Lytics REVISED 2017 PDFVea AngelesNo ratings yet
- CNS 06 AnsDocument8 pagesCNS 06 AnsJeff ParkNo ratings yet
- PHARMACOLOGY M13 TransesDocument8 pagesPHARMACOLOGY M13 TransesdestroyerNo ratings yet
- Second Seminar Discussion On ANS PharmacologyDocument21 pagesSecond Seminar Discussion On ANS PharmacologyDavid lufafaNo ratings yet
- Pharmacol Ogy PHL 313: Chapter 5-6-7 Drugs Affecting The Autonomic Nervous System (ANS)Document14 pagesPharmacol Ogy PHL 313: Chapter 5-6-7 Drugs Affecting The Autonomic Nervous System (ANS)Abdullah Al-TuraifiNo ratings yet
- Lecture 2 PDFDocument15 pagesLecture 2 PDFAya MuhannadNo ratings yet
- NCM 106 Drugs Acting On ANS - Synchronous Session Ver 2Document7 pagesNCM 106 Drugs Acting On ANS - Synchronous Session Ver 2Crecia Bullecer2No ratings yet
- CH 2. AnsDocument96 pagesCH 2. Anstariku fekaduNo ratings yet
- Introduction To ANS and Parasympathomimic DrugsDocument39 pagesIntroduction To ANS and Parasympathomimic DrugsOmima WassalNo ratings yet
- Resume Sa: Anatomi Dan Fisiologi ManusiaDocument30 pagesResume Sa: Anatomi Dan Fisiologi Manusiatata ciripahNo ratings yet
- 06b Pharmacology Learning Material Drugs Affecting The Autonomic Nervous SystemDocument23 pages06b Pharmacology Learning Material Drugs Affecting The Autonomic Nervous SystemJewel Ramos GalinatoNo ratings yet
- NCM 106 Week 5 and 6 ReviewerDocument15 pagesNCM 106 Week 5 and 6 ReviewerCrecia Bullecer2No ratings yet
- Pharma LE EndoANSCardioRenalDocument69 pagesPharma LE EndoANSCardioRenalnibbles nibblesNo ratings yet
- Pharmacology Module For FinalsDocument11 pagesPharmacology Module For FinalsCarlo GaradoNo ratings yet
- IntroductIon To AutonomousDocument29 pagesIntroductIon To AutonomousMerve kdkkNo ratings yet
- Neurotransmitters: A. Paracrine Regulators (Tissue Hormones)Document11 pagesNeurotransmitters: A. Paracrine Regulators (Tissue Hormones)Prasana100% (1)
- Sheet 10Document9 pagesSheet 10zademansi2004.medNo ratings yet
- UNIT II Autonomic Nervous System MPCPDocument21 pagesUNIT II Autonomic Nervous System MPCPgauravkumarsaras838No ratings yet
- Autonomic Nervous SystemDocument130 pagesAutonomic Nervous Systempmm21d229No ratings yet
- Adrenergic and SympatholyticDocument12 pagesAdrenergic and SympatholyticJoyce VillanuevaNo ratings yet
- SynapseDocument6 pagesSynapseGracielle Angelyka PeraltaNo ratings yet
- Neuroanatomy: Autonomic Nervous System Dr. Antonio T. Parong JRDocument10 pagesNeuroanatomy: Autonomic Nervous System Dr. Antonio T. Parong JRZllison Mae Teodoro MangabatNo ratings yet
- Sulio, Rhay Anderzon D.Document7 pagesSulio, Rhay Anderzon D.Glaiza Mae BerongoyNo ratings yet
- Autonomic and Systemic Pharmacology DR DahalDocument119 pagesAutonomic and Systemic Pharmacology DR Dahalअविनाश भाल्टरNo ratings yet
- Pharma PPT TodocDocument40 pagesPharma PPT TodocPrincess Jovelyn GutierrezNo ratings yet
- Autonomic Nervous System: Rodina Rivera-Gorospe, M.DDocument44 pagesAutonomic Nervous System: Rodina Rivera-Gorospe, M.DPogo LocoNo ratings yet
- 03 CNS AnsDocument153 pages03 CNS AnsMaria Arlyn Lacuña SagosoNo ratings yet
- Chemical Transmission in The SynapseDocument24 pagesChemical Transmission in The SynapselibreizanNo ratings yet
- ANS PharmaDocument75 pagesANS Pharmarab yo100% (1)
- Ans HandoutsDocument6 pagesAns HandoutsNoriko MatsumotoNo ratings yet
- 2.1 Physiological and Pharmacological Aspects of The Central Nervous SystemDocument3 pages2.1 Physiological and Pharmacological Aspects of The Central Nervous SystemMyriam LajeunesseNo ratings yet
- Nervous System and MedicationDocument30 pagesNervous System and MedicationNicole SantayoNo ratings yet
- Autonomic Drugs 2020 Part 1 IntroDocument29 pagesAutonomic Drugs 2020 Part 1 Introعون عليNo ratings yet
- Manan 1000 Q - ADocument294 pagesManan 1000 Q - ADrSamia El Wakil0% (1)
- Adrenergic System: Dr. Mozna TalpurDocument18 pagesAdrenergic System: Dr. Mozna TalpurShahid HameedNo ratings yet
- (PSEN) - PSEN 1 and PSEN 2.: Alzheimer's DiseaseDocument4 pages(PSEN) - PSEN 1 and PSEN 2.: Alzheimer's DiseaseZeedan MohammedNo ratings yet
- NeurotransmittersDocument21 pagesNeurotransmittersYannie GomezNo ratings yet
- Introduction To Autonomic PharmacologyDocument44 pagesIntroduction To Autonomic PharmacologyZemburukaNo ratings yet
- L16 - Adrenergics IDocument7 pagesL16 - Adrenergics Iyasaira707No ratings yet
- Medical-Surgical Nursing The Neurologic Concepts: Jimmellee Ellen P. Olilang, RNDocument225 pagesMedical-Surgical Nursing The Neurologic Concepts: Jimmellee Ellen P. Olilang, RNKatrina Sarah Mae MabasaNo ratings yet
- Pharmacological Organization of The CNSDocument8 pagesPharmacological Organization of The CNSLeo PerezNo ratings yet
- NCM 106 (PHARMA) - Lec 19 To 28Document18 pagesNCM 106 (PHARMA) - Lec 19 To 28Aine Jermaine GatchalianNo ratings yet
- Wa0000.Document26 pagesWa0000.halayehiahNo ratings yet
- Drugs Affecting CNSDocument30 pagesDrugs Affecting CNSGwen De CastroNo ratings yet
- NEUROTRANSMITTERSDocument6 pagesNEUROTRANSMITTERShashmatamin9No ratings yet
- Neurological Disorder: NeuronDocument8 pagesNeurological Disorder: NeuronMaica Lectana100% (2)
- Assignment On Adrenergic ReceptorDocument13 pagesAssignment On Adrenergic ReceptoryannaingNo ratings yet
- Maternal AND Child Nursing: PreschoolerDocument2 pagesMaternal AND Child Nursing: PreschoolerAJ BayNo ratings yet
- Care of Mother, Child and Adolescent (Well-Client) AdolescenceDocument3 pagesCare of Mother, Child and Adolescent (Well-Client) AdolescenceAJ BayNo ratings yet
- Lecture Discussion With QUIZDocument11 pagesLecture Discussion With QUIZAJ BayNo ratings yet
- Growth and Development: Toddler: Play Behavior Traits Physical Other Development Developmental Stage TheoriesDocument6 pagesGrowth and Development: Toddler: Play Behavior Traits Physical Other Development Developmental Stage TheoriesAJ BayNo ratings yet
- Nr-Nur 113 (Health Education)Document3 pagesNr-Nur 113 (Health Education)AJ BayNo ratings yet
- Case StudyDocument3 pagesCase StudyAJ BayNo ratings yet
- Assignment 1: Renal Treatment: InstructionsDocument16 pagesAssignment 1: Renal Treatment: InstructionsAJ BayNo ratings yet
- Meal PlanDocument3 pagesMeal PlanAJ Bay100% (1)
- Subclinical Celiac Disease and Crystal-Induced Kidney Disease Following Kidney TransplantDocument6 pagesSubclinical Celiac Disease and Crystal-Induced Kidney Disease Following Kidney TransplantsigmundmaharajanNo ratings yet
- Introduction To ObjectDocument42 pagesIntroduction To ObjectHanan KemalNo ratings yet
- Physiology in Sports - PE, Class 12Document21 pagesPhysiology in Sports - PE, Class 12Jasnoor Singh RainooNo ratings yet
- College of Engineering Pune: Marathwada Mitra Mandal'sDocument3 pagesCollege of Engineering Pune: Marathwada Mitra Mandal'sTejas TaleleNo ratings yet
- Pain Management - 03-07 VersionDocument51 pagesPain Management - 03-07 VersionanreilegardeNo ratings yet
- Transpiration Diagram-Based QuestionsDocument9 pagesTranspiration Diagram-Based Questionsthe lillyNo ratings yet
- Guillain Barre SyndromeDocument16 pagesGuillain Barre SyndromeAgnes NesiaNo ratings yet
- Myocardial InfractionDocument16 pagesMyocardial InfractionYAMINIPRIYANNo ratings yet
- La Faringe. SNM Del Nervio Glosofaríngeo. Plexo FaríngeoDocument24 pagesLa Faringe. SNM Del Nervio Glosofaríngeo. Plexo FaríngeocristinaNo ratings yet
- Right Inguinal Hernia RepairDocument1 pageRight Inguinal Hernia Repairsgod34No ratings yet
- Pharmaceutical Aids and NecessitiesDocument6 pagesPharmaceutical Aids and NecessitiestriciapascualMD100% (1)
- Introductory Zoology: The Science of ZoologyDocument11 pagesIntroductory Zoology: The Science of ZoologyJayson BuenosairesNo ratings yet
- Article 1548935521Document5 pagesArticle 1548935521shishir badveNo ratings yet
- Referat NystagmusDocument44 pagesReferat NystagmusNadira Danata100% (1)
- Against All Odds Preventing Pressure Ulcers in High-Risk Cardiac Surgery PatientsDocument8 pagesAgainst All Odds Preventing Pressure Ulcers in High-Risk Cardiac Surgery PatientsjokoNo ratings yet
- HUBS1105 Bones and Joints of The Skull and FaceDocument5 pagesHUBS1105 Bones and Joints of The Skull and FaceChloe HeuchanNo ratings yet
- Complications of Blood TransfusionDocument10 pagesComplications of Blood Transfusionpinkcherub4No ratings yet
- Introduction To Welfare AssessmentDocument27 pagesIntroduction To Welfare AssessmentYoga RivaldiNo ratings yet
- Cognitive Perception Pattern of Nursing CareDocument9 pagesCognitive Perception Pattern of Nursing CareGloria Khan100% (4)
- Biology DefinitionDocument9 pagesBiology DefinitionMRhines GadgetBasketNo ratings yet
- Diare: Arlinda Silva Prameswari 201810401011044Document28 pagesDiare: Arlinda Silva Prameswari 201810401011044Lilian Rahma AnandaNo ratings yet
- Drilling QuestionDocument56 pagesDrilling QuestionMohamad HattaNo ratings yet
- Introduction To Anatomy and PhysiologyDocument43 pagesIntroduction To Anatomy and Physiologyaarti HingeNo ratings yet
- Fowl Course 214Document10 pagesFowl Course 214Mohamed MaherNo ratings yet
- Hemostasis:: (Stoppage of Blood Flow After Damage)Document5 pagesHemostasis:: (Stoppage of Blood Flow After Damage)raanja2No ratings yet
- Resources - Fat Embolism Syndrome (FES)Document19 pagesResources - Fat Embolism Syndrome (FES)Hareen Reddy100% (1)
- Final OutputDocument16 pagesFinal OutputAnonymous USxVK0No ratings yet
- Oral Pathology - Physical & Chemical Injuries of Oral CavityDocument44 pagesOral Pathology - Physical & Chemical Injuries of Oral CavityRachit Srivastava83% (18)
- Foods That Cause Acne: SUNDAY, APRIL 8, 2012Document3 pagesFoods That Cause Acne: SUNDAY, APRIL 8, 2012FitriAndriyaniNo ratings yet
- Clinical-Chemistry-MB-Reviewer 2Document14 pagesClinical-Chemistry-MB-Reviewer 2Aubrey Jane TagolinoNo ratings yet