Professional Documents
Culture Documents
Medicina Integrativa
Medicina Integrativa
Uploaded by
Yuli MSCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medicina Integrativa
Medicina Integrativa
Uploaded by
Yuli MSCopyright:
Available Formats
Open Access Review
Article DOI: 10.7759/cureus.3098
Integrative Medicine as a Vital Component
of Patient Care
Richard Gannotta 1 , Shaista Malik 2 , Alvin Y. Chan 3 , Kamran Urgun 3 , Frank Hsu 4 , Sumeet
Vadera 5
1. Chief Executive Officer, University of California, Irvine, Orange, USA 2. Integrative Medicine,
University of California, Irvine, Irvine, USA 3. Neurological Surgery, University of California, Irvine,
Orange, USA 4. Neurological Surgery, University of California Irvine, Orange, USA 5. Neurosurgery,
University of California, Irvine
Corresponding author: Alvin Y. Chan, alvinyhchan@gmail.com
Disclosures can be found in Additional Information at the end of the article
Abstract
The landscape of medicine in the United States has been slowly progressing toward a more
holistic and individualized approach to healing. Part of this progress has been the integration
between western and alternative forms of medicine, a concept that has been described as
“integrative medicine.” This approach to healthcare incorporates a patient’s mind, spirituality,
and sense of community into the healing process. Integrative medicine has been typically well
received and the demand has been steadily increasing in primary US hospitals. Here we cover a
number of topics that include the definition of integrative medicine, its potential benefits,
current examples of successful implementations, and potential barriers to its expansion. The
aim was to give a primary on integrative medicine and its current state for healthcare providers.
Categories: Medical Education, Preventive Medicine, Quality Improvement
Keywords: alternative medicine, alternative and complementary medicine
Introduction And Background
Culturally diverse communities may benefit from an integration between western and
alternative forms of medicine that takes a holistic approach to caring for patients. The concept
has been given the term “integrative medicine,” which goes beyond simply combining different
forms of medicine and allows for an individualistic approach to patient care that incorporates
the mind, spirituality, and sense of community as well as the body. This benefit has been shown
in a variety of settings across different nations. For example, there was a case-controlled study
conducted in South Korea that compared western-only with integrative medicine (i.e., an
individualistic combination of western and traditional Korean medicine) in managing patients
Received 07/02/2018
with acute strokes [1]. The results were that although patients who received integrative
Review began 07/18/2018
Review ended 08/01/2018
medicine incurred slightly higher costs than those who underwent only western medicine but
Published 08/04/2018 that they also had a reduced all-risk mortality at both three and 12 months after discharge,
which may have prevented additional costs from future admissions. Similarly, another
© Copyright 2018
Gannotta et al. This is an open
retrospective study in Texas showed that patients who received integrative medicine were more
access article distributed under the likely to have reduced pain that resulted in an approximately 4% decrease in hospital costs [2].
terms of the Creative Commons These findings have implications for care providers and stakeholders, as research has shown
Attribution License CC-BY 3.0., which that integrative medicine likely improves patient care and outcomes while ultimately reducing
permits unrestricted use, distribution,
hospital costs.
and reproduction in any medium,
provided the original author and
source are credited. Here we review the current evidence for integrative medicine in the United States as well as
How to cite this article
Gannotta R, Malik S, Chan A Y, et al. (August 04, 2018) Integrative Medicine as a Vital Component of
Patient Care. Cureus 10(8): e3098. DOI 10.7759/cureus.3098
discuss potential benefits and barriers to implementation. The aim was to abate the stigma
associated with the field and educate readers about the potential it has for improving patient
care. Most patients who seek out integrative medicine alternatives are self-referred [3];
therefore, educating practitioners on potential integrative options would likely benefit patient
care and increase access.
Review
What is integrative medicine?
Integrative medicine is the treatment of patients through spiritual, emotional, mental, and
environmental in addition to the physical means. The general principle is that all aspects of the
patient are considered in treating illness, which include natural and less invasive alternatives
when possible. The patient and health care provider form a partnership that allows for a
holistic approach that includes beliefs, overall wellness, and community to the healing of the
mind and body. Specific techniques can include acupuncture, nutritional advisement, mind-
body therapies, and holistic massages [4], but may involve any effective natural treatment
outside of conventional methodology. However, the treatments are still rooted in scientific
discovery and inquiry [5]. Indeed, research and scientific investigation of efficacy are prevalent
and an important guide of treatment [3]. The way integrative medicine is provided can vary by
location but it is ubiquitous across different avenues of healthcare. Many integrative medicine
centers are associated with major teaching hospitals or healthcare organizations and are often
available as consultation, comprehensive care, or a primary service [3].
Benefits of integrative medicine
The demand for integrative medicine in primary US hospitals has been increasing. To meet this
demand, a number of hospitals have been trialing integrative medicine programs and
investigating the result on patient care. A number of studies and reviews have detailed that
these types of programs have been well received with positive outcomes [6-10]. When an
integrative medicine clinic was implemented in a large California community hospital, 160
patients were recruited to investigate the effects of the clinic on their overall health [11]. The
researchers concluded that clients reported substantial improvements in their symptoms and
that an integrative health clinic could co-exist with a traditional major western medical center.
The main limitation was that the trial was not controlled and thus they could not make any
definitive statements about the outcomes.
Another benefit is symptom improvement during the course of disease, which is especially true
within the realm of cancer when conventional treatments are often limited [4, 10, 12-14]. For
example, a large portion of patients with breast cancer seeks alternative treatment in addition
to conventional western medicine for symptomatic treatment [15]. Similarly, in an
observational study of 238 unspecified cancer patients, who were referred to an inpatient
integrative medicine consultation service, the patients were less likely to be distressed by the
disease and more involved in their own care afterward [16]. The authors argue that the
integrative medicine service helped the patients address their concerns, which helped with
coping. Another case-controlled study of almost 500 patients with breast or gynecological
cancer showed those undergoing integrative medicine were more likely to have an
improvement in appetite, fatigue, cognitive and emotional functioning, pain, anxiety, sleep,
and overall global health [17]. The benefits of integrative medicine are unsurprising. The
concept is that bio-medicine does not necessarily address the complexity of healing or
palliative treatment necessary to fully abate cancer symptoms, which can include emotional
and spiritual distress beyond the physical pain. Also, cancer is not the only disease where
integrative medicine has been successful but it has been an important topic of research.
Providing integrative medicine treatment plans may also increase patient satisfaction. The
2018 Gannotta et al. Cureus 10(8): e3098. DOI 10.7759/cureus.3098 2 of 5
University of Michigan introduced an integrative medicine clinic in 2003 and investigated the
effect by surveying 85 patients about their experience [18]. The program included shared
decision making and an emphasis on understanding patient life stories to better put their
illnesses into context during treatment. The results of the survey suggested that patients were
satisfied with their experience at the clinic and that customizing integrative medicine regimens
allowed to improvements in mental and emotional well-being in addition to symptomatic and
disease improvement. Despite the limitations of the study, which included the voluntary nature
of the surveys, the authors argued that the results were promising and should foster additional
discussion about the potential benefits of integrative medicine clinics. It is intuitive that
patients who feel more control over their treatment and believe they have more options are
likely to be more satisfied.
There are potential drawbacks to integrative medicine. One is that treating multiple systems
and modalities of the patient often requires multiple teams that may disagree on conflicting
treatment avenues. This can be avoided likely if there is one main team who consults other
specialists for different patient needs. In general, the positives outweigh the negatives and
integrative medicine should be considered when appropriate.
Barriers to implementation
There are a number of barriers to implementing integrative medicine in modern western
hospitals. First, there are increased hospital costs of adding programs and centers. At our
institution, the University of California, Irvine, Medical Center, the Susan Samueli Center for
Integrative Medicine was started due to a generous donation from Henry and Susan Samueli.
We understand that donations are not always possible for starting these programs. However,
there is evidence that integrative medicine programs may actually ultimately decrease hospitals
costs in the long-term perspective due to decreased treatment requirements and fewer follow-
up [7]. The patient population that is most likely to benefit immediately is the chronically ill
and those suffering from depression [7]. Therefore, implementing integrative medicine
programs slowly and then expanding as resources become more readily available is likely the
most realistic course.
Second, integrative medicine programs may not be well received or practiced by clinicians,
which could be due to ideological differences or poor education on the topic. An 18-question
survey conducted on pediatric resident physicians at Baylor University in Texas showed that
although over 80% of their patients had asked about integrative medicine options, almost 90%
of the respondents felt their knowledge of integrative medicine needed expansion [19]. The
authors concluded that lack of knowledge was the primary barrier to implementation in the
resident physicians’ practices. There are a variety of ways to circumvent this barrier. The
simplest way would be for physicians and other caretakers to undergo training in terms of their
patients’ integrative medicine options [20]. For example, the University of Arizona Center for
Integrative Medicine provides an online course for resident physicians to expand their
knowledge on the subject [21]. Indeed, online courses for physicians have been shown to be
effective education for teaching integrative medicine [22]. More formal education is also
available and could be sought as well [23]. A similar alternative would be to implement
integrative medicine as a core part of medical school curriculums [24]. Other methods include
the development of a consulting integrative team or referral to an integrative medicine clinic.
There are likely a number of barriers that must be overcome for integrative medicine to be
integrated into traditional western hospital. There may also be a hostility toward alternative
medicines as well as cultural differences [15]. However, implementation of integrative medicine
should be considered when possible due to its potential benefit for patients. Moreover, patients
may also exhibit higher satisfaction with integrative treatment plans [18], which could lead to
benefits for the providers and hospital stakeholders as well. Indeed, there is evidence that
2018 Gannotta et al. Cureus 10(8): e3098. DOI 10.7759/cureus.3098 3 of 5
healthcare professionals are more likely than the general public to use integrative medicine
techniques, which could be due to easier access or paradoxically more knowledge about its
efficacy [25].
Conclusions
The increasing popularity of integrative medicine is rooted in the effort to improve patient care
and reduce suffering. The basis of its ideal is that true healing requires nurturing of the mind
and soul in addition to the body, which goes above the idea of simply combining alternative
with conventional medicine. A variety of therapies outside of conventional bio-medicine can
often help patients deal with difficult illness. Integrative medicine services can take the form of
a consultation, stand-alone clinic, or primary service. The benefits are likely reduced patient
distress and pain in addition to lowering associated hospital costs. However, there are a number
of barriers to implementation where the services are not already available, which include costs
and low caregiver knowledge on integrative medicine options available. If these barriers can be
overcome, patient care is likely to improve and that is the ultimate goal.
Additional Information
Disclosures
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors
declare the following: Payment/services info: All authors have declared that no financial
support was received from any organization for the submitted work. Financial relationships:
All authors have declared that they have no financial relationships at present or within the
previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or
activities that could appear to have influenced the submitted work.
References
1. Park M, Hunter J, Kwon S: Evaluating integrative medicine acute stroke inpatient care in
South Korea. Health Policy. 2018, 122:373-379. 10.1016/j.healthpol.2018.02.004
2. Dusek JA, Griffin KH, Finch MD, Rivard RL, Watson D: Cost savings from reducing pain
through the delivery of integrative medicine program to hospitalized patients. J Altern
Complement Med. 2018, 24:557-563. 10.1089/acm.2017.0203
3. Horrigan B, Lewis S, Abrams DI, Pechura C: Integrative medicine in America—How integrative
medicine is being practiced in clinical centers across the United States. Glob Adv Health Med.
2012, 1:18-52. 10.7453/gahmj.2012.1.3.006
4. Deng GE, Rausch SM, Jones LW, et al.: Complementary therapies and integrative medicine in
lung cancer: diagnosis and management of lung cancer. Chest. 2013, 143:420-436.
10.1378/chest.12-2364
5. Bell IR, Caspi O, Schwartz GE, et al.: Integrative medicine and systemic outcomes research:
issues in the emergence of a new model for primary health care. Arch Intern Med. 2002,
162:133-140. 10.1001/archinte.162.2.133
6. Maizes V, Rakel D, Niemiec C: Integrative medicine and patient-centered care . Explore. 2009,
5:277-289. 10.1016/j.explore.2009.06.008
7. Guarneri E, Horrigan BJ, Pechura CM: The efficacy and cost effectiveness of integrative
medicine: a review of the medical and corporate literature. Explore. 2010, 6:308-312.
10.1016/j.explore.2010.06.012
8. Ashford JW, Mahoney L, Burkett T: A role for complementary and integrative medicine in
Alzheimer's Disease prevention. J Alzheimers Dis. 2015, 48:13-14. 10.3233/JAD-150505
9. Dossett ML, Cohen EM, Cohen J: Integrative medicine for gastrointestinal disease . Prim Care.
2017, 44:265-280. 10.1016/j.pop.2017.02.002
10. Armstrong K, Lanni T Jr, Anderson MM, Patricolo GE: Integrative medicine and the oncology
patient: options and benefits. Support Care Cancer. 2018, 26:2267-2273. 10.1007/s00520-017-
4007-y
2018 Gannotta et al. Cureus 10(8): e3098. DOI 10.7759/cureus.3098 4 of 5
11. Scherwitz L, Stewart W, McHenry P, Wood C, Robertson L, Cantwell M: An integrative
medicine clinic in a community hospital. Am J Public Health. 2003, 93:549-552.
10.2105/ajph.93.4.549
12. Deng GE, Frenkel M, Cohen L, et al.: Evidence-based clinical practice guidelines for
integrative oncology: complementary therapies and botanicals. J Soc Integr Oncol. 2009, 7:85-
120.
13. Cassileth BR, Deng G: Complementary and alternative therapies for cancer . Oncologist. 2004,
9:80-89. 10.1634/theoncologist.9-1-80
14. Knutson L, Johnson PJ, Sidebottom A, Fyfe-Johnson A: Development of a hospital-based
integrative healthcare program. J Nurs Adm. 2013, 43:101-107.
10.1097/NNA.0b013e31827f2229
15. Witt CM, Cardoso MJ: Complementary and integrative medicine for breast cancer patients -
evidence based practical recommendations. Breast. 2016, 28:37-44.
10.1016/j.breast.2016.04.012
16. Frenkel M, Cohen L, Peterson N, Palmer JL, Swint K, Bruera E: Integrative medicine
consultation service in a comprehensive cancer center: findings and outcomes. Integr Cancer
Ther. 2010, 9:276-283. 10.1177/1534735410378663
17. Shalom-Sharabi I, Samuels N, Lavie O, Lev E, Keinan-Boker L, Schiff E, Ben-Arye E: Effect of a
patient-tailored integrative medicine program on gastro-intestinal concerns and quality of
life in patients with breast and gynecologic cancer. J Cancer Res Clin Oncol. 2017, 143:1243-
1254. 10.1007/s00432-017-2368-8
18. Myklebust M, Pradhan EK, Gorenflo D: An integrative medicine patient care model and
evaluation of its outcomes: the University of Michigan experience. J Altern Complement Med.
2008, 14:821-826. 10.1089/acm.2008.0154
19. Ziodeen KA, Misra SM: Complementary and integrative medicine attitudes and perceived
knowledge in a large pediatric residency program. Complement Ther Med. 2018, 37:133-135.
10.1016/j.ctim.2018.02.004
20. Chaudry SS, McGuire MJ, Lam C, Hatef E, Wright SM, Alexander MH: Teaching integrative
medicine to residents: a focus on populations rather than individual patients. Am J Prev Med.
2015, 49:285-289. 10.1016/j.amepre.2015.08.001
21. McClafferty H, Dodds S, Brooks AJ, et al.: Pediatric integrative medicine in residency (PIMR):
description of a new online educational curriculum. Children. 2015, 2:98-107.
10.3390/children2010098
22. Lebensohn P, Kligler B, Brooks AJ, Teets R, Birch M, Cook P, Maizes V: Integrative medicine in
residency: feasibility and effectiveness of an online program. Fam Med. 2017, 49:514-521.
23. Maizes V, Schneider C, Bell I, Weil A: Integrative medical education: development and
implementation of a comprehensive curriculum at the University of Arizona. Acad Med. 2002,
77:851-860.
24. Kligler B, Maizes V, Schachter S, et al.: Core competencies in integrative medicine for medical
school curricula: a proposal. Acad Med. 2004, 79:521-531.
25. Johnson PJ, Ward A, Knutson L, Sendelbach S: Personal use of complementary and alternative
medicine (CAM) by U.S. health care workers. Health Serv Res. 2012, 47:211-227.
10.1111/j.1475-6773.2011.01304.x
2018 Gannotta et al. Cureus 10(8): e3098. DOI 10.7759/cureus.3098 5 of 5
You might also like
- Textbook of Clinical Nutrition and Functional Medicine, vol. 1: Essential Knowledge for Safe Action and Effective TreatmentFrom EverandTextbook of Clinical Nutrition and Functional Medicine, vol. 1: Essential Knowledge for Safe Action and Effective TreatmentNo ratings yet
- HLTINF006 Student Assessment Task 2Document9 pagesHLTINF006 Student Assessment Task 2Rebeca RaducuNo ratings yet
- Person-Centred Care and Naturopathy: Patient Beliefs and ValuesDocument15 pagesPerson-Centred Care and Naturopathy: Patient Beliefs and Valuesromantictroupe314No ratings yet
- Build A Homeopathic First Aid KitDocument2 pagesBuild A Homeopathic First Aid Kitmiera_2014No ratings yet
- Ab 5 Im Overview LudwigDocument2 pagesAb 5 Im Overview Ludwigapi-610178988No ratings yet
- Integrative Medicine and Patient Centered Care PDFDocument35 pagesIntegrative Medicine and Patient Centered Care PDFCristobal Carrasco100% (1)
- Complementary and Alternative Medicine (CAM) For Coronary Diseases, Related Issues, and Future of CAMDocument4 pagesComplementary and Alternative Medicine (CAM) For Coronary Diseases, Related Issues, and Future of CAMAsim AnwarNo ratings yet
- 11.perception of Risk and CommunicationDocument14 pages11.perception of Risk and Communicationbunga mawarNo ratings yet
- Paper Trend and Issues Complementary CareDocument11 pagesPaper Trend and Issues Complementary CareWeda SastrawanNo ratings yet
- 1.) Define The FollowingDocument2 pages1.) Define The FollowingIC BNo ratings yet
- The Value of Self Medication Summary of Existing Evidence PDFDocument12 pagesThe Value of Self Medication Summary of Existing Evidence PDFRoberto GarceteNo ratings yet
- Improving Health Outcomes Through Patient Education and Partnerships With PatientsDocument3 pagesImproving Health Outcomes Through Patient Education and Partnerships With Patientsmanishms1No ratings yet
- Attitudes Toward Integration of Complementary and Alternative Medicine in Primary Care - Perspectives of Patients, Physicians and Complementary PractitionersDocument8 pagesAttitudes Toward Integration of Complementary and Alternative Medicine in Primary Care - Perspectives of Patients, Physicians and Complementary PractitionersAlvin HalconNo ratings yet
- Medication Adherence PDFDocument11 pagesMedication Adherence PDFAnonymous nuVdtDGTEtNo ratings yet
- Briggs, 2015, Complementary and Integrative MedicineDocument10 pagesBriggs, 2015, Complementary and Integrative MedicinearuesjasNo ratings yet
- Effective Factors in Providing Holistic CareDocument11 pagesEffective Factors in Providing Holistic CareSilvaniAdelaUtami SiagianNo ratings yet
- Alternative Medicine - EditedDocument9 pagesAlternative Medicine - EditedWriting PersonNo ratings yet
- Assignment 2Document8 pagesAssignment 2akincade999No ratings yet
- 3Document335 pages3Shubneesh kumarNo ratings yet
- Integrating CAM Practices Into The Conventional Health Systems (Integrative Medicine)Document12 pagesIntegrating CAM Practices Into The Conventional Health Systems (Integrative Medicine)Joud D.No ratings yet
- Terapi Komplementer Dalam Keperawatan: January 2008Document6 pagesTerapi Komplementer Dalam Keperawatan: January 2008oktaviana riskyNo ratings yet
- Alternative ModalitiesDocument28 pagesAlternative ModalitiesJay PaulNo ratings yet
- Complementary and Alternative MedicineDocument7 pagesComplementary and Alternative MedicinenaveenkhanalNo ratings yet
- Patient Centred Clinical MethodDocument4 pagesPatient Centred Clinical MethodSanita BNo ratings yet
- WHO PaperDocument5 pagesWHO PaperIhsan JayaNo ratings yet
- British Pain ClinicDocument11 pagesBritish Pain ClinicdanaNo ratings yet
- Sid PH PortfolioDocument14 pagesSid PH PortfolioKrishna SinghNo ratings yet
- Complementaryandalternativemedicine OverviewDocument8 pagesComplementaryandalternativemedicine OverviewNomiNo ratings yet
- Different Perceptions of Narrative Medicine Between Western and Chinese Medicine StudentsDocument8 pagesDifferent Perceptions of Narrative Medicine Between Western and Chinese Medicine Studentstino valenNo ratings yet
- Frenkel Homeopathy and Cancer 2015Document7 pagesFrenkel Homeopathy and Cancer 2015Para EmhNo ratings yet
- Ajap 2 5 1Document5 pagesAjap 2 5 1Mai Nguyễn Thị NgọcNo ratings yet
- International Journal of Nursing Studies: Hannah Snyder, Jon Engstro MDocument28 pagesInternational Journal of Nursing Studies: Hannah Snyder, Jon Engstro MSitti Rosdiana YahyaNo ratings yet
- Complementary and Alternative Medicin1Document8 pagesComplementary and Alternative Medicin1Sammy ChegeNo ratings yet
- A Career Guide To Becoming A Naturopathic Doctor-1 PDFDocument31 pagesA Career Guide To Becoming A Naturopathic Doctor-1 PDFJuan Capone100% (1)
- HGFDocument2 pagesHGFJaylord VerazonNo ratings yet
- Enhancing Patient Care: A Comprehensive Approach For Healthcare ProfessionalsDocument5 pagesEnhancing Patient Care: A Comprehensive Approach For Healthcare ProfessionalsJyoti GaudNo ratings yet
- PH 109 PrelimDocument52 pagesPH 109 PrelimbaytadokiNo ratings yet
- Public Health Campaigns and Medicine Use Awareness: A Systematic Literature ReviewDocument22 pagesPublic Health Campaigns and Medicine Use Awareness: A Systematic Literature ReviewALEN AUGUSTINENo ratings yet
- Hunter2012 The Integrative Medicine Team-Is Biomedical Dominance InevitableDocument6 pagesHunter2012 The Integrative Medicine Team-Is Biomedical Dominance InevitableSiu KiuNo ratings yet
- Interprofessional EducationDocument3 pagesInterprofessional Educationapi-301357653No ratings yet
- Decision MakingDocument17 pagesDecision MakingPuskesmas CikajangNo ratings yet
- NURS-FPX6026 - WhitneyPierre - Assessment 3-1docxDocument6 pagesNURS-FPX6026 - WhitneyPierre - Assessment 3-1docxCaroline AdhiamboNo ratings yet
- 225 Lesson 1&2 - MergedDocument24 pages225 Lesson 1&2 - MergedNing BalderasNo ratings yet
- Complementary Alternative Medicinepada: NERS JURNAL KEPERAWATAN, Volume 12, No.1, Maret 2016, (Hal 14-22)Document9 pagesComplementary Alternative Medicinepada: NERS JURNAL KEPERAWATAN, Volume 12, No.1, Maret 2016, (Hal 14-22)nonika sianturiNo ratings yet
- Coding Complementary and Alternative Medicine: by Cindy Parman, CPC, CPC-H, RCCDocument4 pagesCoding Complementary and Alternative Medicine: by Cindy Parman, CPC, CPC-H, RCCSet GrinNo ratings yet
- Alternative Vs Conventional MedicineDocument2 pagesAlternative Vs Conventional MedicineJennifer TrujilloNo ratings yet
- Take Home Uas Keperawatan Anak IiDocument43 pagesTake Home Uas Keperawatan Anak IiDianNo ratings yet
- 6-Hnd-713 - Motivating Behavioural Change To Promote Public HealthDocument8 pages6-Hnd-713 - Motivating Behavioural Change To Promote Public HealthSaira JabeenNo ratings yet
- Medical Pluralism Theoretical Perspectives and Real Situation in Relationships With Public Health ViewpointDocument4 pagesMedical Pluralism Theoretical Perspectives and Real Situation in Relationships With Public Health ViewpointJames LoganNo ratings yet
- Unit 1-3Document13 pagesUnit 1-3Sky Primo WalkerNo ratings yet
- 03 BodyDocument81 pages03 BodyAnonymouscatNo ratings yet
- JaffeDocument2 pagesJafferbtakemotoNo ratings yet
- 1.pdf JsessionidDocument39 pages1.pdf JsessionidAlvin Josh CalingayanNo ratings yet
- Wu 2022Document9 pagesWu 2022Anindya Laksmi LarasatiNo ratings yet
- CusickhDocument4 pagesCusickhapi-639782898No ratings yet
- Tugas " Farmasi Komunitas Dan Klinis "Document20 pagesTugas " Farmasi Komunitas Dan Klinis "Icha FebrianiNo ratings yet
- 18 Gouri Et AlDocument6 pages18 Gouri Et AleditorijmrhsNo ratings yet
- Gpcc-Broschyr Eng 160321 WebDocument12 pagesGpcc-Broschyr Eng 160321 WebFaiz AzharNo ratings yet
- Culture and Complementary Therapies PDFDocument8 pagesCulture and Complementary Therapies PDFradamirNo ratings yet
- Terapi Komplementer Dalam Keperawatan: January 2008Document7 pagesTerapi Komplementer Dalam Keperawatan: January 2008TaufikNo ratings yet
- JEduHealthPromot516-2877995 075939Document6 pagesJEduHealthPromot516-2877995 075939Fitri RachmadaniNo ratings yet
- Fast Facts: Medication Adherence: A practical approach to optimizing medication useFrom EverandFast Facts: Medication Adherence: A practical approach to optimizing medication useNo ratings yet
- NCP CvaDocument4 pagesNCP CvamannyV1990100% (1)
- ACCP Farmakoterapi 2013Document296 pagesACCP Farmakoterapi 2013Decy RahmawatiNo ratings yet
- Animal HusbandryDocument4 pagesAnimal HusbandryDanish KamaalNo ratings yet
- Sample Essay 2 - COVID-19 PreventionDocument2 pagesSample Essay 2 - COVID-19 Preventionsirthana697547No ratings yet
- Doh ProgramsDocument7 pagesDoh ProgramsFatima Grace EchemNo ratings yet
- Adolescent SmokingDocument9 pagesAdolescent SmokingSarah Ong SiuNo ratings yet
- Jun07 NleDocument82 pagesJun07 NledrakyboyNo ratings yet
- Normal Parturition and Management of Dystocia in Dogs and CatsDocument7 pagesNormal Parturition and Management of Dystocia in Dogs and Catsmcs.vet8473No ratings yet
- Ezolvin Syrup Patient Information LeafletDocument1 pageEzolvin Syrup Patient Information Leafletpharmacia1.comNo ratings yet
- Bioidentical Hormone Replacement Therapy - A GuideDocument12 pagesBioidentical Hormone Replacement Therapy - A GuidethewoodliffsNo ratings yet
- HWDCDocument2 pagesHWDCJeshiNo ratings yet
- Anembryonic Pregnancy/ Gestation (O02.0)Document137 pagesAnembryonic Pregnancy/ Gestation (O02.0)Marvin Mark AbamongaNo ratings yet
- Listening Test - 2: Extract 1: Question 1-12 Part ADocument6 pagesListening Test - 2: Extract 1: Question 1-12 Part AsruthyNo ratings yet
- The Child With CancerDocument6 pagesThe Child With CancerWai SitNo ratings yet
- TareDocument25 pagesTaremelkamu AssefaNo ratings yet
- Social and Preventive MedicineDocument15 pagesSocial and Preventive MedicineRuthwik Regatti100% (1)
- Antenatal CareDocument11 pagesAntenatal CareManasi ChaskarNo ratings yet
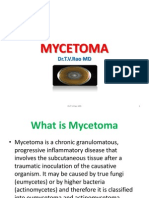
- MycetomaDocument26 pagesMycetomaTummalapalli Venkateswara RaoNo ratings yet
- Biohorizons Symposium Series Italy 2012Document2 pagesBiohorizons Symposium Series Italy 2012hottgayy0% (1)
- NSTP 011 Module 7 - 12Document31 pagesNSTP 011 Module 7 - 12Michael Jack SalvadorNo ratings yet
- Non Viral HepatitisDocument8 pagesNon Viral HepatitisKeith Wesley YbutNo ratings yet
- Pediatric Dentisry: Crowns in Pediatric DentistryDocument25 pagesPediatric Dentisry: Crowns in Pediatric DentistrymahmoodNo ratings yet
- Periodic Assignment 1 Fall 21 201 B-1Document1 pagePeriodic Assignment 1 Fall 21 201 B-1Patrick MillerNo ratings yet
- Hasil Pemeriksaan Laboratorium: Laboratory Test ResultDocument1 pageHasil Pemeriksaan Laboratorium: Laboratory Test ResultAmoy Ida Royani NababanNo ratings yet
- Scabies:: A Review of Diagnosis and Management Based On Mite BiologyDocument14 pagesScabies:: A Review of Diagnosis and Management Based On Mite BiologyElva Wanty ArifinNo ratings yet
- Ethics Committee Resignation Letter 20161018Document3 pagesEthics Committee Resignation Letter 20161018CVRecordNo ratings yet
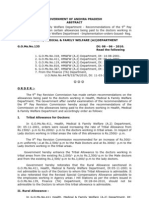
- Ap PRC Allowances GODocument4 pagesAp PRC Allowances GOMadhu Mohan75% (8)
- TMC Annual Report 2011Document16 pagesTMC Annual Report 2011Ole Kristian LosvikNo ratings yet