Professional Documents
Culture Documents
Archives of Neurology Volume 53 Issue 7 1996 (Doi 10.1001 - Archneur.1996.00550070129021) Levy, Morgan L. - Alzheimer Diseas
Archives of Neurology Volume 53 Issue 7 1996 (Doi 10.1001 - Archneur.1996.00550070129021) Levy, Morgan L. - Alzheimer Diseas
Uploaded by
Sonia BaruaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Archives of Neurology Volume 53 Issue 7 1996 (Doi 10.1001 - Archneur.1996.00550070129021) Levy, Morgan L. - Alzheimer Diseas
Archives of Neurology Volume 53 Issue 7 1996 (Doi 10.1001 - Archneur.1996.00550070129021) Levy, Morgan L. - Alzheimer Diseas
Uploaded by
Sonia BaruaCopyright:
Available Formats
Alzheimer Disease and Frontotemporal Dementias
Behavioral Distinctions
Morgan L. Levy, MD; Bruce L. Miller, MD; Jeffrey L. Cummings, MD; Lynn A. Fairbanks, PhD; Anne Craig, MD
Background: Frontotemporal dementia (FTD) is a syn- Results: Patients with FTD had significantly greater to-
degeneration of the temporal
drome produced by lobar tal Neuropsychiatric Inventory scores than patients with
and/or frontal lobes. AD and exhibited more apathy, disinhibition, euphoria,
and aberrant motor behavior. The Neuropsychiatric In-
Objectives: To quantify the behavioral disturbances ventory accurately assigned 77% of patients with FTD
of FTD and compare them with behavioral changes and 77% of patients with AD to the correct diagnostic
observed in Alzheimer disease (AD). group using disinhibition, apathy, and depression. Pa-
tients with FTD had higher levels of disinhibition and
Design: Cross-sectional comparison of 2 groups de- apathy with relatively lower levels of depression com-
fined by research diagnostic criteria and single photon emis- pared with patients with AD.
sion computed tomography. Behaviors were assessed us-
ing a standardized rating scale\p=m-\Neuropsychiatric Conclusions: The Neuropsychiatric Inventory pro-
Inventory. Groups were matched for dementia severity. vides a behavioral profile that differentiates patients
with FTD from patients with AD. Patients with FTD are
Setting: Patients were seen at 2 university-based outpatient more behaviorally disturbed but are often less
dementia clinics and a Veterans Affairs medical center. depressed than patients with AD relative to their level
of apathy.
Participants: Twenty-two patients with FTD and 30
patients with AD. Arch Neurol. 1996;53:687-690
Arnold
Pick1 in 1892, de¬ phy or magnetic resonance imaging to
scribed the first case of identify the localized atrophy of FTD and
dementia associated with the failure of clinical diagnostic criteria for
lobar atrophy. Pick disease AD to distinguish the 2 disorders. Func¬
became synonymous with tional neuroimaging has been more suc¬
frontotemporal dementia (FTD) until the re¬ cessful in distinguishing FTD and AD; pa¬
cent recognition that several degenerative tients with FTD have predominantly
disorders can produce selective frontotem¬ anterior alterations, while those with AD
poral atrophy. Pick disease with classic Pick- have more marked posterior changes.4"10
type histopathologic features, Pick disease Differentiating FTD and AD has become
without Pick cells, amyotrophic lateral scle¬ more imperative as therapies specifically
From the Departments of rosis dementia, dementia lacking distinctive
Psychiatry and Biobehavioral for AD emerge and FTD-specific treat¬
Sciences (Drs Levy, histological features, and frontal lobe degen¬ ments are sought. our study, we de¬
In
Cummings, and Fairbanks) eration ofnon-Alzheimer type are all names fined the 2 populations using research
and Neurology used recently to describe degenerative dis¬ criteria and single photon emission com¬
(Dr Cummings), University of orders with selective frontal and temporal at¬ puted tomography (SPECT) and then
California at Los Angeles rophy. This group ofdisorders may be more sought behavioral differences between
School of Medicine, West Los common than previously thought, compris¬ them using the Neuropsychiatrie Inven¬
Angeles Veterans Affairs ing 10% to 15% of some autopsy series of tory (NPI) scale.11
Medical Center Psychiatry
Service (Drs Levy, Cummings, degenerative dementias.2
and Craig), and Department of Many cases found at autopsy to have
FTD were misdiagnosed as Alzheimer dis¬
Neurology, Harbor-University ease (AD) during life.3 The reasons for this See Subjects and Methods
of California at Los Angeles on next
Medical Center (Dr Miller), high rate of diagnostic inaccuracy in¬ page
Los Angeles, Calif. clude the failure of computed tomogra-
Downloaded From: http://archneur.jamanetwork.com/ by a Monash University Library User on 06/16/2015
years (SD, 8.1 years) compared with patients with AD
whose mean age was 73.5 years (SD, 8.4 years) (P<.001).
SUBJECTS AND METHODS The MMSE scores were not significantly different be¬
tween the 2 groups (mean FTD MMSE score, 14.9 [SD,
All patients were referred for dementia assessment 9.9] and mean AD MMSE score, 17.5 [SD, 7.0], not sig¬
to 1 of 2 university specialty clinics or to a memory nificant). The total NPI scores were significantly differ¬
disorders clinic at a Veterans Affairs medical center. ent. Patients with FTD hadamean score of 23.2 (SD, 17.0)
Patients were screened for chronic mental illness, head compared with patients with AD who had a mean score
trauma, vascular dementia, extrapyramidal disor¬ of 15.7 (SD, 11.6) (P<.05).
ders, vitamin deficiency, hypothyroidism, syphilis, Comparing mean NPI subscale scores, patients with
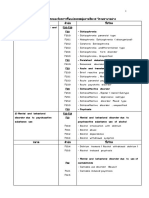
and other medical conditions. Thirty patients re¬ FTD had significantly more disinhibition (t, 2.71; P=.01),
ceived a clinical diagnosis of AD based on criteria es¬
tablished by the National Institute of Neurological
euphoria (t, 2.55; P<.05), apathy (t, 2.89; P-C01), and
aberrant motor behavior (t, 2.04; P<.05) than patients
and Communicative Disorders and Stroke-
with AD (Figure 1 ). There were no statistically signifi¬
Alzheimer's Disease and Related Disorders Associa¬
cant differences between 6 of the 10 mean subscale scores
tion. 12 There were 19 women and 11 men with a mean
age of 73.5 years (range, 54-85 years). Their mean including delusions, hallucinations, agitation, depres¬
Mini-Mental State Examination (MMSE)13 score was sion, anxiety, and irritability.
17.5 (SD, 7.0; range, 0-27). Seventeen patients re¬ Contrasting the percentage of patients with spe¬
ceived a clinical diagnosis of FTD based on criteria cificbehaviors, we found differences between FTD and
developed by the Lund and Manchester Groups.H This AD (Figure 2). Disinhibition and euphoria were much
group included 6 women and 11 men with a mean more common in patients with FTD (68% and 36%)
age of 65 years (range, 52-81 years). Their mean than in patients with AD (23% and 7%) (P<.01 for
MMSE score was 14.9 (SD, 9.2; range, 0-28). Every
both). Apathy was common in both groups but was
patient underwent magnetic resonance imaging and more common in patients with FTD (95%) than in
technetium Tc 99m hexamethyl propylenamine ox-
ime SPECT as part of their diagnostic assessment. All patients with AD (80%), although this difference did
not reach statistical significance. Likewise, aberrant
patients included in the FTD group had predomi¬
motor behavior and anxiety occurred in both groups
nantly anterior cerebral hypoperfusion and all pa¬
tients with AD had predominantly posterior cere¬ but were more common in patients with FTD (73% and
bral hypoperfusion. Patients were included in the 59%) than in patients with AD (47% and 43%); these
study only if they met clinical diagnostic criteria and differences also failed to reach statistical significance.
had compatible SPECT findings for a diagnosis of Delusions and hallucinations occurred in a larger per¬
AD FTD.
or
Behavioral data collected
centage of patients with AD (33% and 7%) than in
were during care¬
patients with FTD (23% and 0%), but the differences
giver interviewsusing the NPI. This instrument
assesses 10 behaviors occurring in dementing
were not statistically significant. Depression, irritability,
illnesses, including delusions, hallucinations, agita¬ and agitation occurred in similar proportions in both
tion, depression, anxiety, euphoria, apathy, disinhi¬ groups.
bition, irritability, and aberrant motor behavior (in¬ A stepwise discriminate function analysis was
cluding pacing, rummaging, and compulsions). A performed to identify the subset of NPI behaviors that
frequency rating (1-4) multiplied by a severity rat¬ best discriminated patients with FTD from patients
ing (1-3) produces a subscale score for each behav¬ with AD. Disinhibition was the first variable to enter
ior and the summation of subscale scores produces the discriminate analysis (F to enter, 9.49; Wilks ,
the total NPI score. All interviews were performed
within 3 months of the diagnostic assessment and in
0.84; canonical coefficient, 0.27), followed by apathy
most cases they were done on the same day. The NPI
(F to enter, 6.11; Wilks 1 , 0.75; canonical coefficient,
has been shown to be valid when compared with a 0.22). Euphoria and aberrant motor activity, which
were significantly different between groups when
variety of other diagnostic approaches and to have assessed independently, were positively correlated
high interrater and test-retest reliability.11
We compared the mean total NPI scores and sub- with the first 2 variables and did not add significantly
scale scores between the FTD and AD groups for each to the discrimination. A new variable, depression,
behavior using t tests. In addition, a stepwise dis¬ which did not appear in the independent analyses,
criminative function analysis with an F to enter of added significantly to the prediction of diagnostic
4.0 was performed to determine the degree to which group once disinhibition and apathy had been taken
patients could be assigned to the correct diagnostic into account (F to enter, 5.92; Wilks , 0.67; canoni¬
group using the NPI subscale scores. Informed con¬ cal coefficient, —0.38). Patients who had high-scale
sent for all procedures was obtained from both pa¬
scores for disinhibition and apathy and relatively low
tients and caregivers.
scores for depression were members of the FTD group.
The final equation using these 3 variables accurately
assigned 77% of the patients with FTD and 77% of the
patients with AD to the correct diagnostic groups.
RESULTS Jackknifed classification was 73% accurate for patients
with FTD and 67% accurate for patients with AD.
Patients with FTD were significantly younger than pa¬ On average, the patients with FTD were younger
tients with AD. Patients with FTD had a mean age of 65 than the patients with AD. To assess whether the con-
Downloaded From: http://archneur.jamanetwork.com/ by a Monash University Library User on 06/16/2015
Figure 1. Mean composite subscale scores (frequency severity) for Figure 2. The percentage of patients with frontotemporal dementia (FTD)
behavioral symptoms in patients with frontotemporal dementia (FTD) and and Alzheimer disease (AD) with non-0 scores for each subscale. Asterisks
in patients with Alzheimer disease (AD) measured by the Neuropsychiatrie indicate 2, P<.01 (see Figure 1 for expansion of abbreviations).
Inventory (NPI). Apa indicates apathy; AbM, aberrant motor behavior; Dis,
disinhibition; Eup, euphoria; Hal, hallucinations; Del, delusions; Dep,
depression; Irr, irritability; Anx, anxiety; Agi, agitation; and error bars, SD.
ing that these findings are robust even in a retrospective
study.
Disinhibited behaviors suchas acting impulsively
founding of age with diagnosis biased the above results, or making socially inappropriate remarks have been
Pearson correlations of patients' ages with subscale reported to help differentiate patients with FTD from
scores were computed within the AD group for each of patients with AD.9 Starkstein et al7 demonstrated ante¬
the variables that differentiated the patients with FTD rior hypoperfusion with SPECT in patients who were
from the patients with AD. The magnitude of the corre¬ defined as "mildly demented with disinhibition," and
lations ranged from —0.10 to 0.17 and none was statis¬ Miller et al18 reported 5 cases of FTD with behavioral
tically significant. This indicates that the difference in disinhibition and noted a specific association with right
neurobehavioral symptoms found between the 2 groups frontal lobe hypoperfusion. This study confirms the
is unlikely to be because of the younger age of the relationship of anterior hypoperfusion with disinhibi-
patients with FTD. tion.
Finally, 2 general types of behaviors have been as¬ Aberrant motorbehavior was significantly more
sociated with frontal lobe dysfunction: disinhibition and common patients with FTD than in patients with
in
apathy. The data were analyzed to see if 2 distinct types AD. The character of the motor activity was not specifi¬
of FTD were identifiable. Of 15 patients with disinhibi- cally studied in this investigation, but previous reports
tion, the mean apathy score was 3.1 (SD, 3.6) compared indicate that the behaviors exhibited by the 2 diagnostic
with 7 patients without disinhibition whose mean apa¬ groups differ. Patients with FTD manifest stereotyped
thy score was 8.6 (SD, 2.8) (P<.05). Thus, patients with behaviors ranging from overt compulsions to elemen¬
marked disinhibition were less apathetic than those with¬ tary repetitions such as repeatedly eating the same
out, supporting the suggestion of 2 subgroups of pa¬ food.19 Patients with AD are more likely to pace, move
tients. furniture, unpack closets, and rummage through draw¬
ers. The nature of the aberrant motor behavior
may
COMMENT help distinguish the 2 groups and warrants further
study.
Standardized assessment of behavioral symptoms pro¬ Apathy is commonly reported in patients with AD,20
vides a means of characterizing neuropsychiatrie but it is more prominent in patients with FTD and oc¬
syndromes associated with different neurologic condi¬ curs at earlier stages of the disease. Apathy is commonly
tions. Numerous articles3'7·914"17 describe behavioral mistaken for depression and a number of patients re¬
differences between FTD and other dementias includ¬ ceived treatment for depression in the years just prior to
ing AD, but instruments for quantitative assessment and being diagnosed with FTD, when apathy had become ap¬
differentiation have been lacking. The NPI is a new be¬ parent. Our results show that patients with FTD have sig¬
havioral rating scale that measures symptoms common nificantly more apathy, but relatively less depression for
in a variety of dementing syndromes including FTD and their level of apathy.
has been shown to be both valid and reliable.11 Using the Euphoria, in the form of elevated mood or inap¬
NPI, highly significant differences between AD and FTD propriate jocularity, was reported by Gustafson21 in
were identified. about one third of his patients with FTD, and he noted
Disinhibition, apathy, aberrant motor behavior, eu¬ that when euphoria occurs in conjunction with restless¬
phoria, and total NPI scores were significantly more ness, these symptoms could closely mimic hypomania
elevated in the FTD group, consistent with previous or mania. We found that 8 of 22 patients with FTD had
descriptions of behavioral differences between FTD and euphoria compared with only 2 of 30 patients with AD.
AD. Barber et al13 described similar differences based on Thus, the presence of euphoria is unusual in AD and is
a retrospective questionnaire given to close relatives of common in FTD. This diagnosis should be seriously
autopsy-proven patients with FTD and AD, demonstrat- considered in patients with euphoric dementia and in
Downloaded From: http://archneur.jamanetwork.com/ by a Monash University Library User on 06/16/2015
patients presenting with late-onset mood disorders with REFERENCES
manic features.
The NPI provided an accurate means of differenti¬
1. Pick A. On the relation between aphasia and senile atrophy of the brain (1892).
ating FTD from AD in this sample. Seventy-seven per¬ In: Rottenberg DA, Hochberg FH, eds; Schoene WC, trans. Neurological Clas-
cent of patients were accurately classified using the NPI sics in Modern Translation. New York, NY: Hafner Press; 1977:35-40.
when compared with current "gold standard" research 2. Brun A. Frontal lobe degeneration of non-Alzheimer type, I: neuropathology.
clinical and SPECT criteria. This is well above the accu¬ Arch Gerontol Geriatr. 1987;6:193-208.
racy rates of clinical diagnosis of FTD reported from 3. Mendez MF, Selwood A, Mastri AR, Frey WH. Pick's disease versus Alzhei-
mer's disease: a comparison of clinical characteristics. Neurology. 1993;43:
brain banks where only 14% of patients (3 of 21) were 289-292.
recognized.3 Thus, the NPI may provide a useful means 4. Read SL, Miller BL, Mena I, Kim R, Itabashi H, Darby A. SPECT in dementia:
of identifying these patients for involvement in FTD- clinical and pathological correlation. J Am Geriatr Soc. 1995;43:243-247.
specific research or as a means of eliminating them 5. Frisoni GB, Pizzolato G, Geroldi C, Rossato A, Bianchetti A, Trabucchi M. Dementia
of the frontal type: neuropsychological and [99Tc]-HM-PAO SPECT features.
from AD research projects and trials of an ti-AD drugs.
J Geriatr Psychiatry Neurol. 1995;8:42-48.
We have obtained postmortem histopathologic confir¬
6. Herholz K. FDG PET and differential diagnosis of dementia. Alzheimer Dis As-
mation of the diagnosis of 3 of the 22 patients with FTD soc Disord. 1995;9:6-16.
and all of them had lobar atrophy with Pick bodies and 7. Starkstein SE, Migliorelli R, Teson A, et al. Specificity of changes in cerebral
without AD-type pathological changes. blood flow in patients with frontal lobe dementia. J Neurol Neurosurg Psy-
The FTDs are a heterogeneous group of disorders chiatry. 1994;57:790-796.
with varying degrees of anatomical and physiological
8. Risberg J, Passant U, Warkentin S, Gustafson L. Regional cerebral blood flow
in frontal lobe dementia of non-Alzheimer type. Dementia. 1993;4:186-187.
dysfunction in the right or left frontal or temporal 9. Miller BL, Cummings JL, Villanueva-Meyer J, et al. Frontal lobe degeneration:
regions. Even within the frontal lobes there is heteroge¬ clinical, neuropsychological, and SPECT characteristics. Neurology. 1991;41:
1374-1382.
neity of regional involvement and some patients show 10. Neary D, Snowden JS, Shields RA, et al. Single photon emission tomography
intense changes in the cingulum, while others demon¬
using 99mTc-HM-PAO in the investigation of dementia. J Neurol Neurosurg Psy-
strate more severe orbitobasal or dorsolateral alter¬
chiatry. 1987;50:1101-1109.
ations. Additionally, there is significant variability in 11. Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gorn-
the neurochemical deficits associated with FTD with bein J. The Neuropsychiatric Inventory: comprehensive assessment of psy-
individual differences in the severity of serotonin defi¬ chopathology in dementia. Neurology. 1994;44:2308-2314.
12. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clini-
ciency. This anatomical and biochemical heterogeneity cal diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA work group
may account for the variability in behavioral profile under the auspices of Department of Health and Human Services Task Force
exhibited by patients with FTD. on Alzheimer's Disease. Neurology. 1984;34:939-944.
These results must be considered preliminary be¬ 13. Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: a practical method
cause of the relatively small sample size. In addition, some for grading the cognitive state of patients for the clinician. J Psychiatr Res.
1975;12:189-198.
patients with AD may have significant frontal involve¬ 14. Brun A, Englund B, Gustafson L, et al. Consensus statement: clinical and neu-
ment and the ability of the NPI to distinguish FTD from ropathological criteria for frontotemporal dementia: the Lund and Manchester
these patients remains to be investigated. We conclude Groups. J Neurol Neurosurg Psychiatry. 1994;57:416-418.
that the NPI reliably differentiates degenerative syn¬ 15. Barber R, Snowden JS, Craufurd D. Frontotemporal dementia and Alzheimer's
disease: retrospective differentiation using information from informants. J Neu-
dromes with anterior or posterior cerebral involvement rol Neurosurg Psychiatry. 1995;59:61-70.
and helps distinguish the behavioral syndromes of FTD 16. Gustafson L. Clinical picture of frontal lobe degeneration of non-Alzheimer type.
and AD. Dementia. 1993;4:143-148.
17. Neary D, Snowden JS, Northen B, Goulding P. Dementia of frontal lobe type.
J Neurol Neurosurg Psychiatry. 1988;51:353-361.
Accepted for publication March 18, 1996. 18. Miller BL, Chang L, Mena I, Boone K, Lesser IM. Progressive right frontotem-
This study was supported by grant AG10123 from
poral degeneration: clinical, neuropsychological and SPECT characteristics.
the Department of Veterans Affairs, a National Institute Dementia. 1993;4:204-213.
on Aging Alzheimer's Disease Center, Bethesda, Md, and 19. Ames D, Cummings JL, Wirshing WC, Quinn B, Mahler M. Repetitive and com-
the Irving and Helga Cooper Geriatric Research Award of pulsive behavior in frontal lobe degenerations. J Neuropsychiatry Clin Neuro-
the UCLA Center on Aging, Los Angeles, Calif. sci. 1994;6:100-113.
20. Mega MS, Cummings JL, Fiorello T, Gorbein J. The spectrum of behavioral
Reprints: Jeffrey L. Cummings, MD, UCLA Neuro¬ changes in Alzheimer's disease. Neurology. 1996;46:130-135.
psychiatrie Institute, 760 Westwood Plaza, Room 37-431, 21. Gustafson L. Frontal lobe degeneration of non-Alzheimer type, II: clinical pic-
Los Angeles, CA 90024. ture and differential diagnosis. Arch Gerontol Geriatr. 1987;6:209-223.
Downloaded From: http://archneur.jamanetwork.com/ by a Monash University Library User on 06/16/2015
You might also like
- F20 Schizophrenia Case StudyDocument45 pagesF20 Schizophrenia Case StudyRichard Joseph DomingoNo ratings yet
- Neurocognitive Differential Diagnosis of Dementing Diseases - Alzheimer's Dementia, Vascular Dementia, Frontotemporal Dementia, and Major Depressive DisorderDocument23 pagesNeurocognitive Differential Diagnosis of Dementing Diseases - Alzheimer's Dementia, Vascular Dementia, Frontotemporal Dementia, and Major Depressive DisorderryrihelmiNo ratings yet
- Hemisync ConcentrationDocument1 pageHemisync ConcentrationbsorinbNo ratings yet
- Annotated BibliographyDocument7 pagesAnnotated Bibliographyapi-340360607No ratings yet
- Behaviour in Frontotemporal Dementia, Alzheimer's Disease and Vascular DementiaDocument13 pagesBehaviour in Frontotemporal Dementia, Alzheimer's Disease and Vascular DementiaFrancisco Ribeiro RachinasNo ratings yet
- Papageorgiou2009 PDFDocument10 pagesPapageorgiou2009 PDFGraziella AguiarNo ratings yet
- Advantage of Modified MRI Protocol For HDocument148 pagesAdvantage of Modified MRI Protocol For HasasakopNo ratings yet
- Clinicopathological Correlations in BehaviouralDocument17 pagesClinicopathological Correlations in BehaviouralAlexandra CastellanosNo ratings yet
- Jamapsychiatry Devanand 2022 Oi 210088 1648226520.73569Document9 pagesJamapsychiatry Devanand 2022 Oi 210088 1648226520.73569Juan Carlos Perez ParadaNo ratings yet
- Evaluation of The NINCDS-ADRDA CriteriaDocument6 pagesEvaluation of The NINCDS-ADRDA Criteriadogstar23No ratings yet
- 184 FullDocument5 pages184 FullJenny LeeNo ratings yet
- Arevision Criterios PDFDocument7 pagesArevision Criterios PDFMilenaNo ratings yet
- Chare-14 Criterios DX FTDDocument7 pagesChare-14 Criterios DX FTDMARIA MONTSERRAT SOMOZA MONCADANo ratings yet
- Cummings, 2024 - Progress in Pharmacologic Management of Neuropsychiatric Syndromes in Neurodegenerative DisordersDocument9 pagesCummings, 2024 - Progress in Pharmacologic Management of Neuropsychiatric Syndromes in Neurodegenerative DisordersalinesancNo ratings yet
- Mendez Et Al 2020 Bipolar Disorder Among Patients Diagnosed With Frontotemporal DementiaDocument9 pagesMendez Et Al 2020 Bipolar Disorder Among Patients Diagnosed With Frontotemporal DementiagyzuvlxsusyxdjcjtlNo ratings yet
- Clinica Encefalitis Nmda InglesDocument7 pagesClinica Encefalitis Nmda InglesOskr MezaNo ratings yet
- Cold Spring Harb Perspect Biol-2018-Erkkinen-A033118Document46 pagesCold Spring Harb Perspect Biol-2018-Erkkinen-A033118Brenda GutiérrezNo ratings yet
- Neuroimaging in DementiaDocument11 pagesNeuroimaging in DementiaAndika ResaNo ratings yet
- Neuropsychiatry in Clinical Practice: The Challenge of Diagnosing Behavioral Variant Frontotemporal DementiaDocument53 pagesNeuropsychiatry in Clinical Practice: The Challenge of Diagnosing Behavioral Variant Frontotemporal DementiaMark A. FosterNo ratings yet
- Criteria For The Diagnosis of Alzheirmer DiseaseDocument13 pagesCriteria For The Diagnosis of Alzheirmer DiseaseRegistro psiNo ratings yet
- FDG-PET Improves Accuracy in Distinguishing Frontotemporal Dementia and Alzheimer's DiseaseDocument20 pagesFDG-PET Improves Accuracy in Distinguishing Frontotemporal Dementia and Alzheimer's DiseaseMoch Syafrudin RidwanNo ratings yet
- James R BurrellDocument13 pagesJames R BurrellCarolina MoralesNo ratings yet
- FABDocument4 pagesFABNadine SmithNo ratings yet
- Alladi2011 PDFDocument7 pagesAlladi2011 PDFRajvi AmlaniNo ratings yet
- Marino S Et Al, Longitudinal Analysis of Brain Atrophy in Alzheimer's Disease and Frontotemporal Dementia, 2019Document9 pagesMarino S Et Al, Longitudinal Analysis of Brain Atrophy in Alzheimer's Disease and Frontotemporal Dementia, 2019henryfv2010No ratings yet
- Cohort Study On Somatoform Disorders in Parkinson Disease and Dementia With Lewy BodiesDocument9 pagesCohort Study On Somatoform Disorders in Parkinson Disease and Dementia With Lewy BodiesHelena AlessiNo ratings yet
- FTD Vs TABDocument7 pagesFTD Vs TABDomi ValenciaNo ratings yet
- Art Therapy and Neuroscience Blend: Working With Patients Who Have DementiaDocument8 pagesArt Therapy and Neuroscience Blend: Working With Patients Who Have DementiaLiliana Duarte PedrozaNo ratings yet
- Enfermedad de AlzheimerDocument10 pagesEnfermedad de AlzheimerJessicaNo ratings yet
- Adultos EpilepticosDocument11 pagesAdultos EpilepticosCata Marimon SierraNo ratings yet
- DID and The BrainDocument8 pagesDID and The BrainkatiaNo ratings yet
- Radiologically Isolated SyndromeDocument8 pagesRadiologically Isolated Syndromesara laadamiNo ratings yet
- Nonmotor Symptoms of Parkinson's DiseaseDocument18 pagesNonmotor Symptoms of Parkinson's Diseaseelenac67No ratings yet
- Deterioro Cognitivo Canino y Enfermedad de AlzheimerDocument8 pagesDeterioro Cognitivo Canino y Enfermedad de AlzheimerzikiuNo ratings yet
- 2023 Neuroimg Dementia MoreDocument16 pages2023 Neuroimg Dementia MoreNeuro IztacalaNo ratings yet
- Le BoucDocument13 pagesLe BoucLucía Camila PizarnikNo ratings yet
- Konduksi DSP NcsDocument7 pagesKonduksi DSP NcsMutiara Kristiani PutriNo ratings yet
- Demencia Mixta DNDocument8 pagesDemencia Mixta DNCARDIO 2019No ratings yet
- 10.1016@B978 0 444 64012 3.00003 4Document13 pages10.1016@B978 0 444 64012 3.00003 4loloasbNo ratings yet
- Narayanaswami 2014Document13 pagesNarayanaswami 2014tuliocsgNo ratings yet
- Demencia SemanticaDocument5 pagesDemencia SemanticaJesus DecepcionadoNo ratings yet
- Anhedonia and Reward Circuit Connectivity Distinguish Nonresponders From Responders To Dorsomedial Prefrontal Repetitive Transcranial Magnetic Stimulation in Major DepressionDocument10 pagesAnhedonia and Reward Circuit Connectivity Distinguish Nonresponders From Responders To Dorsomedial Prefrontal Repetitive Transcranial Magnetic Stimulation in Major DepressionKhory Aurora BertyNo ratings yet
- Hallucinations in Dementia Psychosis in Neurodegenerative Disease Differential Patterns of Hallucination and Delusion SymptomsDocument14 pagesHallucinations in Dementia Psychosis in Neurodegenerative Disease Differential Patterns of Hallucination and Delusion SymptomsSultan TarlacıNo ratings yet
- Arnaldi 2017Document10 pagesArnaldi 2017Jaime AguilarNo ratings yet
- 878 Saturday, 17 June 2017: Scientific AbstractsDocument1 page878 Saturday, 17 June 2017: Scientific AbstractsDavid Gimenez RomeroNo ratings yet
- Artigo AlzheimerDocument21 pagesArtigo Alzheimerbeatriz assunesNo ratings yet
- Prevalence Obsessive Compulsive Disorder PatientsDocument6 pagesPrevalence Obsessive Compulsive Disorder PatientsKrasimir KostadinovNo ratings yet
- Tab VS DFTDocument15 pagesTab VS DFTAntu NandaNo ratings yet
- 7.tardive Dyskinesia Prevalence in The Period of Second-Generation Antipsychotic UseDocument15 pages7.tardive Dyskinesia Prevalence in The Period of Second-Generation Antipsychotic UseDebit SophasingNo ratings yet
- Sobrelapamiento ELA y DFT 2020Document10 pagesSobrelapamiento ELA y DFT 2020siralkNo ratings yet
- Behavioural-Variant Frontotemporal Dementia: An Update: Dementia E Neuropsychologia March 2013Document10 pagesBehavioural-Variant Frontotemporal Dementia: An Update: Dementia E Neuropsychologia March 2013claudiaNo ratings yet
- PNES ClinicalApproachesDocument19 pagesPNES ClinicalApproachesClaudia100% (1)
- Michiel Sen 2017Document1 pageMichiel Sen 2017Muhammad IlhaamNo ratings yet
- Posterior Cortical Atrophy: A Brief Review: Howard S. Kirshner, MD, and Patrick J. M. Lavin, MB, BCH, Bao, MrcpiDocument4 pagesPosterior Cortical Atrophy: A Brief Review: Howard S. Kirshner, MD, and Patrick J. M. Lavin, MB, BCH, Bao, MrcpiEugenia FiginiNo ratings yet
- Alzheimer Dementia JAMADocument4 pagesAlzheimer Dementia JAMAAna RendónNo ratings yet
- Alzheimer MCIDocument13 pagesAlzheimer MCIAsef AntonioNo ratings yet
- Alzheimer and Vascular Dementia - DDDocument4 pagesAlzheimer and Vascular Dementia - DDMARIA MONTSERRAT SOMOZA MONCADANo ratings yet
- Diabetes Articulo NuevoDocument9 pagesDiabetes Articulo NuevoAn GelNo ratings yet
- Ranasinghe 2016Document12 pagesRanasinghe 2016Luciana CassimiroNo ratings yet
- EpilepsyDocument6 pagesEpilepsyHelena DVNo ratings yet
- Anderson 11 HDDocument10 pagesAnderson 11 HDMARIA MONTSERRAT SOMOZA MONCADANo ratings yet
- Diagnostic Criteria For The Behavioral Variant FTDDocument5 pagesDiagnostic Criteria For The Behavioral Variant FTDMusleh AlgarniNo ratings yet
- Fast Facts: Psychosis in Parkinson's Disease: Finding the right therapeutic balanceFrom EverandFast Facts: Psychosis in Parkinson's Disease: Finding the right therapeutic balanceNo ratings yet
- Retracted: Inhibition of Spinal 5-Ht3R Reverted Diabetes-Induced Mechanical Hypersensitivity in A Gaba R-Mediated Neurotransmission-Dependent MannerDocument1 pageRetracted: Inhibition of Spinal 5-Ht3R Reverted Diabetes-Induced Mechanical Hypersensitivity in A Gaba R-Mediated Neurotransmission-Dependent MannerSonia BaruaNo ratings yet
- PHAR 7633 Chapter 15 Multiple Oral Dose Administration: CP EquationDocument4 pagesPHAR 7633 Chapter 15 Multiple Oral Dose Administration: CP EquationSonia BaruaNo ratings yet
- Biopharmaceutics 4rth USTC-2Document60 pagesBiopharmaceutics 4rth USTC-2Sonia BaruaNo ratings yet
- Sonia, You Have 1 Job Change and 16 New Updates Waiting For You On LinkedinDocument1 pageSonia, You Have 1 Job Change and 16 New Updates Waiting For You On LinkedinSonia BaruaNo ratings yet
- Presented By: Imran Ahammad ChowdhuryDocument8 pagesPresented By: Imran Ahammad ChowdhurySonia BaruaNo ratings yet
- Pharmacokinetics Accumulation: M. RossumDocument4 pagesPharmacokinetics Accumulation: M. RossumSonia BaruaNo ratings yet
- Hepatology Volume Issue 2020 (Doi 10.1002 - Hep.31423) Kim, Yun Seok Nam, Hyeon Joo Han, Chang Yeob Joo, Min Sung J - LXRÃŽÂ ActivaDocument33 pagesHepatology Volume Issue 2020 (Doi 10.1002 - Hep.31423) Kim, Yun Seok Nam, Hyeon Joo Han, Chang Yeob Joo, Min Sung J - LXRÃŽÂ ActivaSonia BaruaNo ratings yet
- Single-Dose and Multiple-Dose Pharmacokinetics of Zaltoprofen After Oral Administration in Healthy Chinese VolunteersDocument7 pagesSingle-Dose and Multiple-Dose Pharmacokinetics of Zaltoprofen After Oral Administration in Healthy Chinese VolunteersSonia BaruaNo ratings yet
- Hindi Ocd BookletDocument20 pagesHindi Ocd BookletAnonymous zNHxbrsETT100% (2)
- SpeechDocument2 pagesSpeechAsriantiNo ratings yet
- Pengaruh Massage Kaki Terhadap Penurunan Insomnia Pada Lansia Di Banjar Temesi Desa Temesi Kabupaten GianyarDocument9 pagesPengaruh Massage Kaki Terhadap Penurunan Insomnia Pada Lansia Di Banjar Temesi Desa Temesi Kabupaten GianyaryanuarNo ratings yet
- Body Integrity Identity DisorderDocument6 pagesBody Integrity Identity DisorderCarla MesquitaNo ratings yet
- 0404CP Pearls3 PDFDocument1 page0404CP Pearls3 PDFPriya PuriNo ratings yet
- Autism and Case Studies Research-1Document2 pagesAutism and Case Studies Research-1NAA NYC Metro ChapterNo ratings yet
- Dysthymia More Than "Minor" DepressionDocument5 pagesDysthymia More Than "Minor" DepressionNathaly BerríoNo ratings yet
- Task 3 - Special EducationDocument3 pagesTask 3 - Special EducationShainna BaloteNo ratings yet
- ResearchDocument4 pagesResearchDave Delos ReyesNo ratings yet
- Recent Advances in The Management of ASDDocument53 pagesRecent Advances in The Management of ASDPriyash JainNo ratings yet
- Measure of Parental StyleDocument2 pagesMeasure of Parental StyleGianina TudosăNo ratings yet
- DR Halit Ibrahimi - Social Withdrawal and Bizarre Behavior in An 18 Years Old ManDocument11 pagesDR Halit Ibrahimi - Social Withdrawal and Bizarre Behavior in An 18 Years Old ManbardhoshNo ratings yet
- Personality DisordersDocument128 pagesPersonality DisordersKirsten100% (10)
- Mental ExamDocument7 pagesMental ExamEricka Mae GarciaNo ratings yet
- Research Essay Final Draft 1Document10 pagesResearch Essay Final Draft 1api-548724051No ratings yet
- AutPlay Autism Checklist RevisedDocument2 pagesAutPlay Autism Checklist RevisedTina LalNo ratings yet
- Advances in Integrative Medicine: Stuart Richard ThomasDocument4 pagesAdvances in Integrative Medicine: Stuart Richard ThomasVictor Raul JuramaNo ratings yet
- Causes of KleptomaniaDocument7 pagesCauses of Kleptomaniatrew_wertNo ratings yet
- On Being Sane in Insane Places SummaryDocument5 pagesOn Being Sane in Insane Places SummarySharon KimNo ratings yet
- DSMDocument14 pagesDSMSanthoshi TallaNo ratings yet
- Torret SyndromeDocument14 pagesTorret SyndromeAhmad HaqulNo ratings yet
- Assignment 1 2 The Soloist CollinsDocument7 pagesAssignment 1 2 The Soloist Collinsapi-326194051No ratings yet
- Bipolar Disorder Outline 2016Document20 pagesBipolar Disorder Outline 2016Catlyn ChatpmanNo ratings yet
- Child Adhd TreatmentDocument34 pagesChild Adhd TreatmentRoberto Alexis Molina Campuzano100% (1)
- Icd 10Document4 pagesIcd 10ÜnŶäÜnClubEverydayNo ratings yet
- Howtohelpsomeonewithaneatingdisorderwebquest MegankleinDocument3 pagesHowtohelpsomeonewithaneatingdisorderwebquest Megankleinapi-299839434No ratings yet
- Chapter 14Document26 pagesChapter 14slg233No ratings yet