Professional Documents
Culture Documents
The Implementation and Outcome of Clinical Pathway: A Systematic Review
The Implementation and Outcome of Clinical Pathway: A Systematic Review
Uploaded by
Angieda SoepartoCopyright:
Available Formats
You might also like
- Classroom Observation Form 2019Document5 pagesClassroom Observation Form 2019Luzviminda Britanico100% (2)
- Full Download Essential Research Methods For Social Work 4th Edition Rubin Test BankDocument35 pagesFull Download Essential Research Methods For Social Work 4th Edition Rubin Test Bankphaethon.meak0ka6o100% (44)
- Test Bank For Medical Surgical Nursing 7th Edition by LewisDocument12 pagesTest Bank For Medical Surgical Nursing 7th Edition by LewisAmos KerrNo ratings yet
- Hulley9781608318049 FMDocument14 pagesHulley9781608318049 FMrarepsyche67% (3)
- Hunsley & Mash (2007)Document25 pagesHunsley & Mash (2007)Raluca AdinaNo ratings yet
- Evidence Based Practice A Concept AnalysisDocument7 pagesEvidence Based Practice A Concept Analysissana naazNo ratings yet
- PatientSafetyProgramManual12 12 2005Document81 pagesPatientSafetyProgramManual12 12 2005Tito Yustiawan100% (2)
- 3563-Article Text-16806-1-10-20181205Document8 pages3563-Article Text-16806-1-10-20181205rizaNo ratings yet
- Mzi040 PDFDocument6 pagesMzi040 PDFselamat parminNo ratings yet
- Mzi040 PDFDocument6 pagesMzi040 PDFselamat parminNo ratings yet
- Effective Orientation Programs For New Graduate Nurses: A Systematic ReviewDocument7 pagesEffective Orientation Programs For New Graduate Nurses: A Systematic ReviewdebbyNo ratings yet
- Patient Experience Quest-Addo 2021Document19 pagesPatient Experience Quest-Addo 2021Claudia MoksidyNo ratings yet
- Clinical Quality Improvement and Quality Improvement ResearchDocument11 pagesClinical Quality Improvement and Quality Improvement ResearchCruz HernandezNo ratings yet
- Kim, 2022 - MADocument26 pagesKim, 2022 - MAAnindya Laksmi LarasatiNo ratings yet
- Relationship of Nursing Knowledge, Skills, Attitudes and Work Environments With Completeness in The Decree of Clinical Pathway by Nurses in Ernaldi Bahar Hospital South Sumatera Province 2018Document4 pagesRelationship of Nursing Knowledge, Skills, Attitudes and Work Environments With Completeness in The Decree of Clinical Pathway by Nurses in Ernaldi Bahar Hospital South Sumatera Province 2018International Journal of Innovative Science and Research TechnologyNo ratings yet
- A Critical Analysis of The Implementation of Service User Involvement in Primary Care Research and Health Service Development Using NormDocument15 pagesA Critical Analysis of The Implementation of Service User Involvement in Primary Care Research and Health Service Development Using NormKrystalChooNo ratings yet
- ACGME Outcome ProjectDocument8 pagesACGME Outcome ProjectsrisetyaNo ratings yet
- Process Mining For Clinical Processes A Comparative AnalysisDocument18 pagesProcess Mining For Clinical Processes A Comparative AnalysisbenNo ratings yet
- Annotated BibDocument4 pagesAnnotated BibAmelia ArnisNo ratings yet
- Ibu Masy - The FS A Health Economic PerspectiveDocument4 pagesIbu Masy - The FS A Health Economic PerspectiveRinaNo ratings yet
- Struggling For A Feasible Tool - The Process of Implementing A Clinical Pathway in Intensive Care: A Grounded Theory StudyDocument15 pagesStruggling For A Feasible Tool - The Process of Implementing A Clinical Pathway in Intensive Care: A Grounded Theory StudyHarumiNo ratings yet
- Repub 133733 O-ADocument12 pagesRepub 133733 O-AZeka ValladolidNo ratings yet
- E O - M A C N P A C N P: Ffect of An Utcomes Anaged Pproach To Are of Euroscience Atients by Cute ARE Urse RactitionersDocument12 pagesE O - M A C N P A C N P: Ffect of An Utcomes Anaged Pproach To Are of Euroscience Atients by Cute ARE Urse RactitionersFathchur RohmanNo ratings yet
- IPE Interprofessional EducationDocument10 pagesIPE Interprofessional EducationdewaNo ratings yet
- Develop and Implement Clinical Pathway PDFDocument10 pagesDevelop and Implement Clinical Pathway PDFAhmad Safi'i Bin SamirinNo ratings yet
- Criteria For Assessing The Quality of Clinical Practice Guidelines in Paediatrics and Neonatology: A Mixed-Method StudyDocument12 pagesCriteria For Assessing The Quality of Clinical Practice Guidelines in Paediatrics and Neonatology: A Mixed-Method StudyGreg RsNo ratings yet
- Capability Beliefs On, and Use of Evidence-Based Practice Among Four Health Professional and Student Groups in Geriatric Care: A Cross Sectional StudyDocument16 pagesCapability Beliefs On, and Use of Evidence-Based Practice Among Four Health Professional and Student Groups in Geriatric Care: A Cross Sectional StudynofitaNo ratings yet
- The Patient Experiences Questionnaire: Development, Validity and ReliabilityDocument12 pagesThe Patient Experiences Questionnaire: Development, Validity and Reliabilityrisa setiaNo ratings yet
- Dialnet AntecedentsOfRecommendationAndRepurchaseIntentionO 8308130Document27 pagesDialnet AntecedentsOfRecommendationAndRepurchaseIntentionO 8308130fahmi ilyasNo ratings yet
- An Overview of Reviews On Interprofessional Collaboration in Primary Care: Barriers and FacilitatorsDocument15 pagesAn Overview of Reviews On Interprofessional Collaboration in Primary Care: Barriers and FacilitatorsGendi CynthiaNo ratings yet
- PCE Framework May 2017 - 2Document12 pagesPCE Framework May 2017 - 2Erezina Odomero OyegwaNo ratings yet
- Using Staffing Ratios For Workforce Planning: Evidence On Nine Allied Health ProfessionsDocument8 pagesUsing Staffing Ratios For Workforce Planning: Evidence On Nine Allied Health ProfessionstikamdxNo ratings yet
- Analysis of Nursing Services On Satisfaction Health Insurance Provider Agency PatientsDocument5 pagesAnalysis of Nursing Services On Satisfaction Health Insurance Provider Agency PatientsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Research in Social and Administrative Pharmacy 16 (2020) 25-32Document8 pagesResearch in Social and Administrative Pharmacy 16 (2020) 25-32School StuffNo ratings yet
- Santana Et Al How To Practice Person Centred CareDocument12 pagesSantana Et Al How To Practice Person Centred CareShita DewiNo ratings yet
- 1 s2.0 S1098301519352179 MainDocument14 pages1 s2.0 S1098301519352179 MainLidya ButarNo ratings yet
- Ebd 2023Document6 pagesEbd 2023dinaNo ratings yet
- Nursing Staffs Self-Perceived Outcome From A Rehabilitation 24/7 Educational Programme - A Mixed-Methods Study in Stroke CareDocument13 pagesNursing Staffs Self-Perceived Outcome From A Rehabilitation 24/7 Educational Programme - A Mixed-Methods Study in Stroke Care2020614266No ratings yet
- Effects of Clinical Pathways: Do They Work?: P Van Herck, K Vanhaecht and W SermeusDocument11 pagesEffects of Clinical Pathways: Do They Work?: P Van Herck, K Vanhaecht and W SermeussuriNo ratings yet
- Economic Evaluation Strategies in Telehealth: Obtaining A More Holistic Valuation of Telehealth InterventionsDocument5 pagesEconomic Evaluation Strategies in Telehealth: Obtaining A More Holistic Valuation of Telehealth InterventionsAlejandro CardonaNo ratings yet
- Jurnal Pendukung PDFDocument12 pagesJurnal Pendukung PDFMita AmaliaNo ratings yet
- A Systematic Review of The Effects of Residency Training On Patients OutcomesDocument11 pagesA Systematic Review of The Effects of Residency Training On Patients OutcomesMaik MouraNo ratings yet
- Training Code (GE.008) - CQMRDocument11 pagesTraining Code (GE.008) - CQMRBung HerryNo ratings yet
- Health Expectations - 2022 - Adams The Ultimate Question Evaluating The Use of Net Promoter Score in HealthcareDocument12 pagesHealth Expectations - 2022 - Adams The Ultimate Question Evaluating The Use of Net Promoter Score in HealthcareEliana PedrazaNo ratings yet
- 1-S2.0-S1939865422000315-MainDocument8 pages1-S2.0-S1939865422000315-MainnersrosdianaNo ratings yet
- Modified Delphi Consensus On Developing Home Care Service Quality Indicator For Stroke Survivor in Yogyakarta IndonesiaDocument7 pagesModified Delphi Consensus On Developing Home Care Service Quality Indicator For Stroke Survivor in Yogyakarta IndonesiaJufran, R (2018)No ratings yet
- CE of Diagnostic Tests Good Practice Recommendations 1709007663Document14 pagesCE of Diagnostic Tests Good Practice Recommendations 1709007663Sandro PaimNo ratings yet
- Full Download Test Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo Wood PDF Full ChapterDocument36 pagesFull Download Test Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo Wood PDF Full Chapterpapismlepal.b8x1100% (21)
- Evidence-Based Practice Project ProposalDocument7 pagesEvidence-Based Practice Project Proposalwamburamuturi001No ratings yet
- Clinical Practice Guidelines in Breast Cancer: N. Kumar Tyagi and S. Dhesy-ThindDocument10 pagesClinical Practice Guidelines in Breast Cancer: N. Kumar Tyagi and S. Dhesy-ThindsanNo ratings yet
- Research ArticleDocument11 pagesResearch ArticleJorge Durán MartínezNo ratings yet
- Test Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo WoodDocument8 pagesTest Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo WoodSusan Palacios100% (42)
- Health Coaching in Pharmacy Practice: A Systematic ReviewDocument14 pagesHealth Coaching in Pharmacy Practice: A Systematic ReviewrujaklutisNo ratings yet
- Dimensions of Patient Experience in Addiction and Mental HealthDocument11 pagesDimensions of Patient Experience in Addiction and Mental HealthVĩ Vũ NgọcNo ratings yet
- Indicators 2Document8 pagesIndicators 2giovanna.jangarelliNo ratings yet
- PDSA Improvement Plan - Kingston General Hospital: Name Institution Course Professor DateDocument5 pagesPDSA Improvement Plan - Kingston General Hospital: Name Institution Course Professor DateNilanjana ChakrabortyNo ratings yet
- Level of Pharmacist Knowledge On Writing Integrated Patient Progress Notes in One of The Government Hospital in The City of Bukittinggi, West Sumatra, IndonesiaDocument4 pagesLevel of Pharmacist Knowledge On Writing Integrated Patient Progress Notes in One of The Government Hospital in The City of Bukittinggi, West Sumatra, IndonesiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Bird Et Al. 2014. Fit For PurposeDocument17 pagesBird Et Al. 2014. Fit For PurposeGursheen KaurNo ratings yet
- Interprofessional Communication (IPC) ForDocument17 pagesInterprofessional Communication (IPC) FornersrosdianaNo ratings yet
- Factors Affecting The Choice of Public, Private, or Charity Health Care ProvidersDocument8 pagesFactors Affecting The Choice of Public, Private, or Charity Health Care ProvidersYonathan ArdhanaNo ratings yet
- Darren L. Mungcal BSN 123 Group 92 Evidence Based NursingDocument6 pagesDarren L. Mungcal BSN 123 Group 92 Evidence Based NursingRowena MungcalNo ratings yet
- Critical Pathways and Health Care ReformDocument11 pagesCritical Pathways and Health Care Reformrosie101998No ratings yet
- Integrated Care PathwayDocument3 pagesIntegrated Care PathwayFitri EmiNo ratings yet
- 556-Appropriateness of Clinical Decision Support - Final White Paper-Wei WuDocument15 pages556-Appropriateness of Clinical Decision Support - Final White Paper-Wei Wuapi-398506399No ratings yet
- Preparation For Practice of Newly Qualified Dental Practitioners in AustrailaDocument72 pagesPreparation For Practice of Newly Qualified Dental Practitioners in Austrailadk42tbcfk9No ratings yet
- Quality and Safety in Nursing: A Competency Approach to Improving OutcomesFrom EverandQuality and Safety in Nursing: A Competency Approach to Improving OutcomesGwen SherwoodNo ratings yet
- Ijms 21 08776Document22 pagesIjms 21 08776Angieda SoepartoNo ratings yet
- Fecal Calprotectin in Combination With Standard Blood Tests in The Diagnosis of Inflammatory Bowel Disease in ChildrenDocument8 pagesFecal Calprotectin in Combination With Standard Blood Tests in The Diagnosis of Inflammatory Bowel Disease in ChildrenAngieda SoepartoNo ratings yet
- Reaching Malaria Elimination On 2030-Materi Dr. Inke Nadia Diniyanti Lubis, M.Ked (Ped), Sp.A, PH.DDocument32 pagesReaching Malaria Elimination On 2030-Materi Dr. Inke Nadia Diniyanti Lubis, M.Ked (Ped), Sp.A, PH.DAngieda SoepartoNo ratings yet
- Seminar PERSI DR. WahyuniDocument52 pagesSeminar PERSI DR. WahyuniAngieda SoepartoNo ratings yet
- Action Research As A Practice-Based Practice-Kemmis-2013Document13 pagesAction Research As A Practice-Based Practice-Kemmis-2013Angieda SoepartoNo ratings yet
- An Action Research Approach To The Development of A Clinical Pathway For Women Requiring Caesarean Section-Moody-2015Document13 pagesAn Action Research Approach To The Development of A Clinical Pathway For Women Requiring Caesarean Section-Moody-2015Angieda SoepartoNo ratings yet
- A Closer Look at Using Stringer Action Research Model in Improving Student Learning-Nasrollahi-2015Document7 pagesA Closer Look at Using Stringer Action Research Model in Improving Student Learning-Nasrollahi-2015Angieda SoepartoNo ratings yet
- Alt Richter 2002Document8 pagesAlt Richter 2002Angieda SoepartoNo ratings yet
- Editorial: Insider Action ResearchDocument6 pagesEditorial: Insider Action ResearchAngieda SoepartoNo ratings yet
- Jurnal AnakDocument2 pagesJurnal AnakAngieda SoepartoNo ratings yet
- " Ekosistem Digital ": Untuk Kedaulatan Medis Indonesia, Peta Jalan, Tantangan Dan KesempatanDocument30 pages" Ekosistem Digital ": Untuk Kedaulatan Medis Indonesia, Peta Jalan, Tantangan Dan KesempatanAngieda SoepartoNo ratings yet
- Chemical Risk Assessment-Framework PDFDocument77 pagesChemical Risk Assessment-Framework PDFBoni MagtibayNo ratings yet
- Borntrager & Lyon 2015Document13 pagesBorntrager & Lyon 2015chocolatec00kieNo ratings yet
- Product Advertisements in Orthodontic Journals AJODO April 2021Document7 pagesProduct Advertisements in Orthodontic Journals AJODO April 2021saja IssaNo ratings yet
- Joc70081 1010 1022Document13 pagesJoc70081 1010 1022Diego UrrunagaNo ratings yet
- N A M A: Prof. Dr. Dr. Rozaimah Zain-Hamid, MS, SPFK PekerjaanDocument54 pagesN A M A: Prof. Dr. Dr. Rozaimah Zain-Hamid, MS, SPFK PekerjaanRitta Kumari PermaluNo ratings yet
- Human Resources For Health: What Difference Does ("Good") HRM Make?Document7 pagesHuman Resources For Health: What Difference Does ("Good") HRM Make?Shah NewazNo ratings yet
- Venepuncture Before Internship ResearchDocument14 pagesVenepuncture Before Internship Researchkamedi99No ratings yet
- Module 02 Evidence Based Practice Sy 2021Document7 pagesModule 02 Evidence Based Practice Sy 2021Ariane Pearl GabrielesNo ratings yet
- Guidelines ASPENDocument138 pagesGuidelines ASPENJaqueline Odair100% (1)
- Raw 1Document91 pagesRaw 1Gopaul UshaNo ratings yet
- Plantar Fasciitis GuidelinesDocument19 pagesPlantar Fasciitis Guidelinesband12No ratings yet
- Contemp Project Model-Gov8Document19 pagesContemp Project Model-Gov8Ahmed Mohamed Walid100% (1)
- Assignment Guidelines-HSC 6 016 1819 2Document2 pagesAssignment Guidelines-HSC 6 016 1819 2rjt903No ratings yet
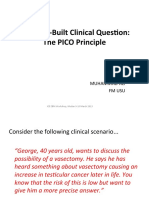
- Well-Built Clinical Question (PICO)Document32 pagesWell-Built Clinical Question (PICO)noniNo ratings yet
- Test Bank For Introductory Medical Surgical Nursing 10th Edition Barbara TimbyDocument8 pagesTest Bank For Introductory Medical Surgical Nursing 10th Edition Barbara Timbycoopeeglottishe6y1No ratings yet
- Using Evidence For Public Health Decision Making: Preventing Excessive Alcohol Consumption and Related HarmsDocument48 pagesUsing Evidence For Public Health Decision Making: Preventing Excessive Alcohol Consumption and Related Harmsyamira27No ratings yet
- Ebp LectureDocument31 pagesEbp LectureTHEA KERSTI ECOTNo ratings yet
- 4.73 (FCM) EBM - Critical Appraisal On Therapy and PreventionDocument6 pages4.73 (FCM) EBM - Critical Appraisal On Therapy and PreventionEver Mary Joy EscaleraNo ratings yet
- Wood 2020Document16 pagesWood 2020facu22marmisolleNo ratings yet
- Systematic Reviews of Interventions Following Physical Abuse: Helping Practitioners and Expert Witnesses Improve The Outcomes of Child Abuse, UK, 2009Document6 pagesSystematic Reviews of Interventions Following Physical Abuse: Helping Practitioners and Expert Witnesses Improve The Outcomes of Child Abuse, UK, 2009Beverly TranNo ratings yet
- Colin Palfrey - Paul Thomas - Ceri Phillips - Evaluation For The Real World - The Impact of Evidence in Policy Making-Policy Press (2012)Document258 pagesColin Palfrey - Paul Thomas - Ceri Phillips - Evaluation For The Real World - The Impact of Evidence in Policy Making-Policy Press (2012)Inayat KhanNo ratings yet
- Exploring The Science of Complementary and Alternative MedicineDocument68 pagesExploring The Science of Complementary and Alternative MedicineAurutchat VichaiditNo ratings yet
- EBP Deliverable Module 2Document6 pagesEBP Deliverable Module 2Marian SmithNo ratings yet
- Analisa Jurnal Kelompok 9 (The History of Evidence-Based Practice in Nursing Education and Practice)Document9 pagesAnalisa Jurnal Kelompok 9 (The History of Evidence-Based Practice in Nursing Education and Practice)Viola AlvionitaNo ratings yet
The Implementation and Outcome of Clinical Pathway: A Systematic Review
The Implementation and Outcome of Clinical Pathway: A Systematic Review
Uploaded by
Angieda SoepartoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Implementation and Outcome of Clinical Pathway: A Systematic Review
The Implementation and Outcome of Clinical Pathway: A Systematic Review
Uploaded by
Angieda SoepartoCopyright:
Available Formats
THE IMPLEMENTATION AND OUTCOME OF
CLINICAL PATHWAY: A SYSTEMATIC REVIEW
Rizka Chairani Riza, Atik Nurwahyuni
Faculty of Public Health, University of Indonesia
ABSTRACT
Background: Clinical pathways provide detailed guidance for each stage in the
management of a patient, such as treatments and interventions, with a specific
condition over a given time period. Clinical pathway implementation has the potential
to standardize treatment and improve outcomes. The purpose of this study was to
explore the implementation and outcome of clinical pathway.
Subjects and Method: This was a systematic review which carried out by searching
articles from 2000 to 2018 in PubMed, BMC, Science Direct and Indonesian Health
Economics Journal databases. The keywords for this review included clinical pathway,
care maps, care pathway, integrated clinical pathway, implementation, and evaluation.
The data were analyzed by PRISMA method.
Results: Clinical pathway affected patients, medical staffs, and hospital management.
The impact of clinical pathway on patients included: (1) reduced length of stay; and (2)
reduced total cost of hospitalization. Clinical pathway increased communication, know-
ledge, teamwork among hospital staffs, and quality of health care service for patients.
Conclusion: Good implementation of clinical pathway affects patients, medical staffs,
and hospital management. Clinical pathway can improve quality of health services in
the hospital.
Keywords: clinical pathway, implementation, evaluation, health service, hospital
Correspondence:
Rizka Chairani Riza. Faculty of Public Health, University of Indonesia. Depok, West
Java. Email: rizkachairani12@gmail.com. Mobile: 081380684872.
BACKGROUND of services, efficiency, and accessibili-
Hospitals have an obligation to pro- ty of health services were some of the
vide safe, quality and effective servi- priorities in health service manage-
ces while prioritizing the interests of ment (Asmirajanti et al., 2018). One
patients in accordance with the stan- of the efforts made by hospitals and
dards of service from the hospital. other health care providers to impro-
The primary goal of health care pro- ve service quality and cost efficiency
viders was to produce profitable out- was to use Clinical Pathway.
comes not only for patients but also Clinical pathway (CP) also
health care providers and the commu- known as critical pathway, care maps
nity. Achieving the desired outcome or integrated clinical pathway, was a
depend on the quality of hospital ser- multidisciplinary treatment plan and
vices. based on clinical practice that was
Efforts to continuously improve used in groups of patients with certain
service quality and efficiency in the diagnoses designed to minimize ser-
health care system at the hospital vice delays, optimize resource utiliza-
were always carried out. The quality tion and maximize service quality
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 677
https://doi.org/10.26911/theicph.2019.05.33
(Ismail et al., 2012). CP was a tool in standard that would provide the basis
health services that formulated the for medical audits at the hospital.
work of a multidisciplinary team Although there were many bene-
where each medical person joined in fits from the use of CP, there were still
the team can analyze their respective many hospitals or other health care
roles and responsibilities. CP map the providers who cannot run CP properly
course of the disease and the pattern and correctly. The main purpose of
of care that would be received by the this study was to find out what factors
patient and aimed to make the right influence and the impact of applying
doctor do the right treatment, care clinical pathways on medical person-
was given at the right time so that nel, hospitals and patients.
good treatment results can be achi-
eved. SUBJECTS AND METHOD
CP was a collection of medical 1. Study Design
opinions that contained the stages of This study was used Systematic re-
care for patients. CP was made up of view by using the PRISMA method.
the latest evidence based which obtai- Online databases used were Pubmed,
ned from systematic reviews and in- ScienceDirect, BMC (BioMed Central),
put from multidisciplinary teams, to and Indonesian Health Economics
describe the optimal treatment stages Journal with keywords "clinical path-
intended for patients who have cer- way" OR "critical pathway" OR "care
tain specific conditions or were un- maps" AND "development" OR "im-
dergoing certain treatment procedu- plementation" OR "evaluation" AND
res. "Multidisciplinary", "developmen and
The use of CP has several main implementation of clinical pathways",
advantages, namely, improving the AND "development, implementation
quality of evidence-based service ser- of clinical pathway", "evaluation", and
vices, the services provided were mul- "clinical pathway" carried out the ad-
tidisciplinary, increasing the level of dition of sentences in the keywords
care of medical personnel to patients, "implementation of clinical pathway".
as an effective communication tool Articles used from 2000 to 2018
between medical personnel and medi- which obtained 1217 articles with the
cal personnel-patients, as a basis for application of inclusion criteria, 11
planning medical services according articles were selected with full text
to patient needs, outcome oriented, and assessed for their feasibility.
used as a consistent documentation
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 678
https://doi.org/10.26911/theicph.2019.05.33
Database Pubmed, BMC, ScienceDirect
Using, JEKI using keyword or their
synonyms
N = 1217
Limitation Duplication
years N = 918
Title Exclusion
Identificatio N = 844
n
Title Inclusion
N = 74
Abstract
Exclusion N = 37
Screening
Abstract Inclusion
N = 37
Full text articels
excluded with
reason N= 26
Full text inclusion
Full text N= 11
Include and Abstract only = 0 Inclusion criteria:
Exclude
Year 2000 to
2018
paper which
Studies included in main of
qualitative synthesis discussion
N= 11 clinical pathway
Figure 1. PRISMA method flowchart
2. Inclusive and Exclusive crite- that did not show the factors that in-
ria fluence the application and impact of
The entry journal and assessed for the use of CP.
feasibility in this study was a journal 3. PICO
that showed the factors that influence The problem (P) focused on this re-
the application and impact of the search was to conclude the factors
application of CP to medical person- that can influence the development
nel, hospitals and patients. This in- and application of CP, the advantages
cluded barriers that can be encoun- and disadvantages of applying CP to
tered in implementing and impacting both medical personnel, hospitals and
the implementation of CP. Journal patients. The purpose (O) of this stu-
which was not included was a journal dy was to know clearly the factors that
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 679
https://doi.org/10.26911/theicph.2019.05.33
influence the application of CP so that was conducted in three stages: (1)
the implementation can be carried out searching for and collecting literature,
well and to determine the impact of (2) analyzing and evaluating the
the use of CP on medical personnel, literature found, and (3) categorizing
hospitals and patients. This research and summarizing the literature.
Table 1. Selected publication articles through PRISMA method
RESULTS ration of CP; (3) Establish a multidis-
1. The Development and Imp- ciplinary team; (4) Conducting main-
lementation of Clinical Path- tenance flow mapping; (5) Evaluating
way and collecting data; (6) CP Develop-
The implementation of CP made hos- ment; (7) Dissemination and appli-
pitals have standard planning in car- cation of CP; (8) Conduct ongoing
ing for patients so that services beca- evaluations of CP that have been
me more effective, service quality was implemented (Davis, 2005; Lavelle,
maintained and service costs were Schast and Keren, 2015). Good docu-
under control. Therefore, the applica- mentation played an important role,
tion of CP was one of the important and must be made by each medical
points for the hospital. 8 steps taken staff in a scientific discipline (Scottish
in the preparation of CP, namely: (1) Goverment executive health
Making a selection of a diagnosis or department, 2003).
procedure; (2) Identification of stake-
holders who play a role in the prepa-
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 680
https://doi.org/10.26911/theicph.2019.05.33
2. That affect the development be the obstacles in the application of
and implementation of clini- CP (Evans-Lacko et al., 2010; Ismail
cal pathways et al., 2012; Said, Abd El-Sadik and
Evans-Lacko et al (2010) explained Mahmoud, 2017; Asmirajanti et al.,
the factors that influence the deve- 2018)
lopment and application of CP which A study conducted in China,
were divided into 3 stages, namely at found two major obstacles in the pro-
the stage of making CP, implement- cess of implementing CP, the first
ing CP and evaluating CP. According obstacle came from hospital manage-
to Francke et al (2008), there were 5 ment who were passive in conducting
factors that would influence the im- CP socialization programs. The seco-
plementation of CP, namely (1) the nd obstacle came from the doctor, the
characteristics of CP; (2) selection of implementation of CP would reduce
strategies to be used in implementing the bonus income, where 70% of the
CP; (3) characteristics of professional doctor's bonus income in China every
medical personnel. Lack of awareness, month was based on the number of
understanding, and the disapproval prescribed drugs and medical test
of medical professionals on the con- given (Evans-Lacko et al., 2010; He
tents of CP would lead to thee disrup- and Yang, 2015).
tion of the CP application; (4) charac- 4. The impact of applying clini-
teristics of patients and (5) character- cal pathways to medical per-
istics of the environment (hospital). sonnel, hospitals and patients
3. Factors that inhibit the imple-
mentation of the clinical a. Knowledge of medical personnel
pathway Regarding the impact of the applica-
Inhibiting factors can occur at the tion of CP on medical personnel.
level of hospital staff (medical staff), Said, Abd El-Sadik and Mahmoud
the level of health service organizati- (2017), conducted a study of CP
ons (hospital management and hospi- typhoid fever in pediatric patients.
tal resources) or at the level of exter- Studies conducted emphasized on the
nal factors (government policies and level of nurses' knowledge of CP, the
patient characteristics). Obstacles can content of CP, the application of CP
also arise because of the differences and evaluation of CP typhoid fever.
in thinking between members of the The results of the study statistically
multidisciplinary team, unrecorded showed a significant difference after
variations, lack of support from hos- the implementation of CP, namely (1)
pital staff in implementing CP, and an increase in nurses' knowledge
lack of direction and support from about CP; (2) increasing knowledge
senior medical personnel. Lack of of nurses about typhoid fever; (3)
knowledge, awareness and familiarity increasing nurses' knowledge about
of medical personnel (doctors or nur- multidisciplinary teams and (4) after
ses) related to CP, the contents of CP, the implemantation of CP disease
the process of disease travel and education by medical personnel to
disease treatment procedures would
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 681
https://doi.org/10.26911/theicph.2019.05.33
patients and families, the success be significantly shortened. In the CP
increased. hemorrhagic fever study, after one
Increased knowledge of medical year of application CP reduced LoS
personnel was also found in a study from 5.32 days to 3.95 days while in
conducted by Deneckere et al, it was CP Appendicitis there was a reduct-
found that the application of CP in- ion of LoS by 37% (Cheah, 2000;
creased the competence and know- Nimah and Nurwahyuni, 2017; Rejeki
ledge of medical staff (Deneckere et and Nurwahyuni, 2017).
al., 2012, 2013). Asmirajanti et al (2018) condu-
cted a study on CP pelvic fractures,
b. Length of stay (LoS) total knee arthroplasty, neck and
In 2015, He and Yang conducted a CP head surgery, pneumonia in infants
study in China, the results showed and esophagectomy by comparing the
that in the first year after the im- mean LoS and cost effectiveness in
plementation of CP LoS patients and groups that applied CP and groups
total treatment costs showed a signi- that did not apply CP, there was a
ficant decrease, but in the second decrease in LoS in the group which
year after the implementation of CP, applied CP. The same thing was fou-
the length of stay was not showing nd in the study conducted by Denec-
significant changes while the total kere et al. The use of CP would incre-
cost of care increased compared to ase the return of patients, in the
the first year (He and Yang, 2015). group which used CP, 80% of pati-
Rotter et al (2008) conducted a ents were returned and groups which
systematic and meta-analysis reviews did not use use CP, 45% of patients
of the application of CP. 12 of the 17 were returned (Deneckere et al.,
journals reviewed, LoS was found to 2012).
Table 2 Comparison of the average length of stay and cost effectiveness
for patients who applied CP
Source: Asmirajanti et al. (2018)
c. Multidisciplinary team and nurs- tation of care performed by multiple
ing care professions, reducing the occurrence
The application of CP gave positive of medication prescribing errors by
results to nursing care to patients in up to 30%, significantly increasing
the form of increasing medical care documentation the return of patients
provided by medical personnel and by 19%, follow-up of patients increas-
hospital facilities, more organized ed, communication between medical
nursing levels, influencing documen- personnel and patients was more
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 682
https://doi.org/10.26911/theicph.2019.05.33
established and CP improved clinical was slightly different from the study
contact with medical personnel to conducted by He and Yang (2015), in
patients (Deneckere et al., 2012, the first year of CP implementation, it
2013; Asmirajanti et al., 2018). was found that the cost of treatment
The implementation of CP decreased in heart disease patients
would introduce evidence-based care, and acute appendicitis but it increas-
improve communication between ed in the second year so that the total
professions, increase commitment to cost increased by around 18.4% (He
teamwork, support training for medi- and Yang, 2015).
cal personnel and maximize the use In a study conducted by Nimah
of resources while prioritizing service and Nurwahyuni (2017) in acute CP
quality efficiently (Deneckere et al., appendicitis, there were differences
2012, 2013; Ismail et al., 2012; between the bills of patients which
Asmirajanti et al., 2018). according to CP and not according to
CP. The difference in average bills
d. Readmission and Complications occurred with average bills: general
From the review conducted in several monitoring, investigation, room bills,
articles, the application of CP helped drug bills and medical management.
hospitals to provide effective and effi- After implementing CP, the patient
cient care so that fewer complications bills were lower than before, the mag-
occurred, minimize treatment delays, nitude of the difference in the outco-
errors in care and duplication of in- me variable was caused by the compli-
terventions (Asmirajanti et al., 2018). ance of medical personnel to CP.
But in the research conducted by Rot-
ter et al and Cheah, there were no DISCUSSION
significant differences in the occur- Clinical pathway (CP) was a way to
rence of readmission and complica- manage, monitor and record services
tions between before and after the to patients, also known by other na-
application of CP, CP also had no mes such as: care maps, critical path-
effect on short-term results, mortality ways, integrated clinical pathway or
and morbidity (Cheah, 2000; Rotter critical care pathway was a treatment
et al., 2008). plan that described in detail about
every important stage of health servi-
e. The cost of treatment ces, for patients with certain clinical
The application of CP will increase problems. CP must contain a clear
the awareness of doctors about cost statement of the purpose of the ser-
control by avoiding drug administra- vices provided and the important ele-
tion and examinations that were not ments of evidence-based care, best
needed so that the cost of hospi- practices and expectations of patients,
talization would be significantly low- as a communication facilitation tool,
er, reduced LoS would certainly have the sequence of care paths that would
an impact on decreasing maintenance be carried out by multidisciplinary
costs (Rotter et al., 2008; Ismail et al., teams and those received by patients,
2012; Asmirajanti et al., 2018). This documentation, monitoring results
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 683
https://doi.org/10.26911/theicph.2019.05.33
and evaluation of the results of care of CP as a cost control quality control
and identification of resources (Pane- tool was highly dependent on the re-
lla, Marchisio and Stanislao, 2003). lated human resources, because HR
The application of CP can have would carry out both quantity and
a number of impacts on medical staff, quality. Strong commitment from all
hospitals and patients. Impacts found staff can also obtain from the suffi-
include; CP can reduce patient LoS, cient of socialization and evaluation.
increase knowledge, competence of Linking service data (based on CP) to
medical personnel related to CP and hospital expenditures and income can
disease, knowledge of medical per- be used as a way to further increase
sonnel about multidisciplinary teams the commitment of all hospital staff,
and medical care to be provided. The so that the staff can find out the
use of CP in treating patients also impact of successful CP implemen-
caused more organized nursing care, tation not only related to patient ser-
increasing collaboration between me- vice quality, but also hospital opera-
dical professions so as to minimize tional finance (Cheah, 2000; Nimah
the possibility of duplication of inter- and Nurwahyuni, 2017).
ventions and prescribing errors by At the stage of socializing the
doctors. implementation of CP, communica-
The use of CP can reduce the tion between all parties involved was
possibility of burnout in medical per- an important factor in the successful
sonnel. In this study, it was found implementation of CP. All staff relat-
that the application of CP would in- ed to the implementation of CP must
crease the workload of nurses' medi- understand the important role of
cal personnel. This was happened be- each and the importance of the suc-
cause in the application of CP, there cess of CP for hospitals. Multidis-
were several forms that must be filled ciplinary teams, case managers, doc-
(Deneckere et al., 2012; Nimah and tors and other health personnel have
Nurwahyuni, 2017). an important role in the successful
The application of CP is an implementation of CP if they under-
effective way as an educational tool stand their duties and obligations.
for medical personnel, patients and The form of support from the
families that would have a good im- management and the leadership of
pact on the quality of care for the the hospital for the successful imple-
patients. The standard of care pro- mentation of CP can be done by giv-
vided and the reduced length of stay ing direction and examples to all rele-
for patients would affect the income vant staff. The responsibility for the
of the hospital but at the same time successful implementation of CP was
the costs that must be paid by the a shared responsibility, starting from
patient would decrease. the hospital leadership to the staff
Some obstacles that occurred who implemented the CP.
were due to the lack of understanding, The occurrence of variations in
readiness and support from related the application of CP can also hampe-
HR. The successful implementation red the application of CP. CP was a
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 684
https://doi.org/10.26911/theicph.2019.05.33
device that was flexible/not rigid. Wales: National Leadership
Therefore, evaluation of CP must al- and innovation agency for
ways be done in order to adjust to the healthcare. Available at: www.-
development of new science and agaaoi.cymru.nhs.uk
patient characteristics. The clinical (Accessed: 22 November 2018).
Deneckere, S. et al. (2012) ‘Care
pathway that successfully implement-
pathways lead to better
ed would bring benefits to both pati- teamwork: Results of a syste-
ents and hospitals. Eliminating unne- matic review’, Social Science &
cessary actions, decreasing length of Medicine, 75(2), pp. 264–268.
stay, increasing knowledge and reduc- doi: 10.1016/j.socscimed.2012-
ing treatment costs can be achieved .02.060.
when the treatment was standardized. Deneckere, S. et al. (2013) ‘Better
The quality of service to patients was Interprofessional Teamwork,
the main goal of hospitals so standar- Higher Level of Organized Care,
dization must focus on improving the and Lower Risk of Burnout in
Acute Health Care Teams
quality which focusing on cost control
Using Care Pathways’, Medical
thereafter. The leadership and com- Care, 51(1), pp. 99–107. doi:
mitment of all stakeholders held a 10.1097/MLR.0b013e31827633
crucial point in implementing CP so 12.
that the best clinical care and mana- Evans-Lacko, S. et al. (2010)
gement system can be achieved. ‘Facilitators and barriers to
implementing clinical care
REFERENCE pathways’, BMC Health Ser-
Asmirajanti, M. et al. (2018) vices Research, 10(1), p. 182.
‘Clinical care pathway streng- doi: 10.1186/1472-6963-10-182.
hens interprofessional collabo- Francke, A. L. et al. (2008) ‘Factors
ration and quality of health influencing the implemen-
service: a literature review’, tation of clinical guidelines for
Enfermería Clínica, 28, pp. health care professionals: A
240–244. doi: 10.1016/S1130- systematic meta-review’, BMC
8621(18)30076-7. Medical Informatics and De-
Cheah, J. (2000) ‘Clinical Pathways cision Making, 8(1), p. 38. doi:
– An Evaluation of its Impact 10.1186/1472-6947-8-38.
on the Quality of Care in an He, J. A. and Yang, W. (2015)
Acute Care General Hospital in ‘Clinical pathways in China –
Singapore’, Singapore Med J an evaluation’, International
MMed (Public Health). Wales, Journal of Health Care Quality
41(7), pp. 335–346. Available Assurance, 28(4), pp. 394–411.
at: doi: 10.1108/IJHCQA-09-20-
https://pdfs.semanticscholar.o 14-0096.
rg/694a/bd761328a10a0793b4 Ismail, A. et al. (2012) ‘Clinical
b8cadb2b1c9042949f.pdf Pathways: Development and
(Accessed: 28 May 2018). Implementation at a Tertiary
Davis, N. (2005) Integrated Care Hospital in Malaysia’, Interna-
Pathways a guide to good tional Journal of Public Health
practice. Edited by N. Davis. Research, 2(2), pp. 153–160.
Available at: http://journal-
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 685
https://doi.org/10.26911/theicph.2019.05.33
article.ukm.my/5590/1/vol%2 RS X Jakarta’, Jurnal Ekonomi
5202%2520no%25202%25202 Kesehatan Indonesia, 2(2). doi:
012_20.pdf (Accessed: 10 10.7454/eki.v2i2.2146.
December 2018). Rotter, T. et al. (2008) ‘A systematic
Lavelle, J., Schast, A. and Keren, R. review and meta-analysis of the
(2015) ‘Standardizing Care effects of clinical pathways on
Processes and Improving Qua- length of stay, hospital costs
lity Using Pathways and and patient outcomes’, BMC
Continuous Quality Improve- Health Services Research, 8(1),
ment’, Curr Treat Options Peds, p. 265. doi: 10.1186/1472-
1, pp. 347–358. doi: 6963-8-265.
10.1007/s40746-015-0026-4. Said, K. M., Abd El-Sadik, B. R. and
Nimah, K. and Nurwahyuni, A. Mahmoud, F. S. (2017) ‘In-
(2017) ‘Evaluasi Implementasi tegrated Clinical Pathway
Clinical Pathway Apendisitis Regarding Care of Children
Akut Terhadap Tagihan Pasien with Typhoid Fever’, IOSR
Di Rumah Sakit X’. Journal of Nursing and Health
Panella, M., Marchisio, S. and Science, 6(2), pp. 1–12. doi:
Stanislao, A. F. Di (2003) 10.9790/1959-0602040112.
‘Reducing clinical variations Scottish Goverment executive health
with clinical pathways: do department (2003) Effective
pathways work?’, International Interventions Unit Developing
Journal for Quality in Health and Implementing Integrated
Care, 15(156), pp. 509–521. Care Pathways (Guide 2:
doi: 10.1093/intqhc/mzg057. Developing Integrated Care
Rejeki, V. M. M. and Nurwahyuni, A. Pathways). Scotland. Available
(2017) ‘Cost of Treatment at: www.drugmisuse.isdscotl-
Demam Berdarah Dengue and.org/eiu/intcare/intcare.ht
(DBD) di Rawat Inap Ber- m (Accessed: 22 November
dasarkan Clinical Pathway di 2018).
The 5th International Conference on Public Health
Best Western Premier Hotel, Solo, Indonesia, February 13-14, 2019 | 686
https://doi.org/10.26911/theicph.2019.05.33
You might also like
- Classroom Observation Form 2019Document5 pagesClassroom Observation Form 2019Luzviminda Britanico100% (2)
- Full Download Essential Research Methods For Social Work 4th Edition Rubin Test BankDocument35 pagesFull Download Essential Research Methods For Social Work 4th Edition Rubin Test Bankphaethon.meak0ka6o100% (44)
- Test Bank For Medical Surgical Nursing 7th Edition by LewisDocument12 pagesTest Bank For Medical Surgical Nursing 7th Edition by LewisAmos KerrNo ratings yet
- Hulley9781608318049 FMDocument14 pagesHulley9781608318049 FMrarepsyche67% (3)
- Hunsley & Mash (2007)Document25 pagesHunsley & Mash (2007)Raluca AdinaNo ratings yet
- Evidence Based Practice A Concept AnalysisDocument7 pagesEvidence Based Practice A Concept Analysissana naazNo ratings yet
- PatientSafetyProgramManual12 12 2005Document81 pagesPatientSafetyProgramManual12 12 2005Tito Yustiawan100% (2)
- 3563-Article Text-16806-1-10-20181205Document8 pages3563-Article Text-16806-1-10-20181205rizaNo ratings yet
- Mzi040 PDFDocument6 pagesMzi040 PDFselamat parminNo ratings yet
- Mzi040 PDFDocument6 pagesMzi040 PDFselamat parminNo ratings yet
- Effective Orientation Programs For New Graduate Nurses: A Systematic ReviewDocument7 pagesEffective Orientation Programs For New Graduate Nurses: A Systematic ReviewdebbyNo ratings yet
- Patient Experience Quest-Addo 2021Document19 pagesPatient Experience Quest-Addo 2021Claudia MoksidyNo ratings yet
- Clinical Quality Improvement and Quality Improvement ResearchDocument11 pagesClinical Quality Improvement and Quality Improvement ResearchCruz HernandezNo ratings yet
- Kim, 2022 - MADocument26 pagesKim, 2022 - MAAnindya Laksmi LarasatiNo ratings yet
- Relationship of Nursing Knowledge, Skills, Attitudes and Work Environments With Completeness in The Decree of Clinical Pathway by Nurses in Ernaldi Bahar Hospital South Sumatera Province 2018Document4 pagesRelationship of Nursing Knowledge, Skills, Attitudes and Work Environments With Completeness in The Decree of Clinical Pathway by Nurses in Ernaldi Bahar Hospital South Sumatera Province 2018International Journal of Innovative Science and Research TechnologyNo ratings yet
- A Critical Analysis of The Implementation of Service User Involvement in Primary Care Research and Health Service Development Using NormDocument15 pagesA Critical Analysis of The Implementation of Service User Involvement in Primary Care Research and Health Service Development Using NormKrystalChooNo ratings yet
- ACGME Outcome ProjectDocument8 pagesACGME Outcome ProjectsrisetyaNo ratings yet
- Process Mining For Clinical Processes A Comparative AnalysisDocument18 pagesProcess Mining For Clinical Processes A Comparative AnalysisbenNo ratings yet
- Annotated BibDocument4 pagesAnnotated BibAmelia ArnisNo ratings yet
- Ibu Masy - The FS A Health Economic PerspectiveDocument4 pagesIbu Masy - The FS A Health Economic PerspectiveRinaNo ratings yet
- Struggling For A Feasible Tool - The Process of Implementing A Clinical Pathway in Intensive Care: A Grounded Theory StudyDocument15 pagesStruggling For A Feasible Tool - The Process of Implementing A Clinical Pathway in Intensive Care: A Grounded Theory StudyHarumiNo ratings yet
- Repub 133733 O-ADocument12 pagesRepub 133733 O-AZeka ValladolidNo ratings yet
- E O - M A C N P A C N P: Ffect of An Utcomes Anaged Pproach To Are of Euroscience Atients by Cute ARE Urse RactitionersDocument12 pagesE O - M A C N P A C N P: Ffect of An Utcomes Anaged Pproach To Are of Euroscience Atients by Cute ARE Urse RactitionersFathchur RohmanNo ratings yet
- IPE Interprofessional EducationDocument10 pagesIPE Interprofessional EducationdewaNo ratings yet
- Develop and Implement Clinical Pathway PDFDocument10 pagesDevelop and Implement Clinical Pathway PDFAhmad Safi'i Bin SamirinNo ratings yet
- Criteria For Assessing The Quality of Clinical Practice Guidelines in Paediatrics and Neonatology: A Mixed-Method StudyDocument12 pagesCriteria For Assessing The Quality of Clinical Practice Guidelines in Paediatrics and Neonatology: A Mixed-Method StudyGreg RsNo ratings yet
- Capability Beliefs On, and Use of Evidence-Based Practice Among Four Health Professional and Student Groups in Geriatric Care: A Cross Sectional StudyDocument16 pagesCapability Beliefs On, and Use of Evidence-Based Practice Among Four Health Professional and Student Groups in Geriatric Care: A Cross Sectional StudynofitaNo ratings yet
- The Patient Experiences Questionnaire: Development, Validity and ReliabilityDocument12 pagesThe Patient Experiences Questionnaire: Development, Validity and Reliabilityrisa setiaNo ratings yet
- Dialnet AntecedentsOfRecommendationAndRepurchaseIntentionO 8308130Document27 pagesDialnet AntecedentsOfRecommendationAndRepurchaseIntentionO 8308130fahmi ilyasNo ratings yet
- An Overview of Reviews On Interprofessional Collaboration in Primary Care: Barriers and FacilitatorsDocument15 pagesAn Overview of Reviews On Interprofessional Collaboration in Primary Care: Barriers and FacilitatorsGendi CynthiaNo ratings yet
- PCE Framework May 2017 - 2Document12 pagesPCE Framework May 2017 - 2Erezina Odomero OyegwaNo ratings yet
- Using Staffing Ratios For Workforce Planning: Evidence On Nine Allied Health ProfessionsDocument8 pagesUsing Staffing Ratios For Workforce Planning: Evidence On Nine Allied Health ProfessionstikamdxNo ratings yet
- Analysis of Nursing Services On Satisfaction Health Insurance Provider Agency PatientsDocument5 pagesAnalysis of Nursing Services On Satisfaction Health Insurance Provider Agency PatientsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Research in Social and Administrative Pharmacy 16 (2020) 25-32Document8 pagesResearch in Social and Administrative Pharmacy 16 (2020) 25-32School StuffNo ratings yet
- Santana Et Al How To Practice Person Centred CareDocument12 pagesSantana Et Al How To Practice Person Centred CareShita DewiNo ratings yet
- 1 s2.0 S1098301519352179 MainDocument14 pages1 s2.0 S1098301519352179 MainLidya ButarNo ratings yet
- Ebd 2023Document6 pagesEbd 2023dinaNo ratings yet
- Nursing Staffs Self-Perceived Outcome From A Rehabilitation 24/7 Educational Programme - A Mixed-Methods Study in Stroke CareDocument13 pagesNursing Staffs Self-Perceived Outcome From A Rehabilitation 24/7 Educational Programme - A Mixed-Methods Study in Stroke Care2020614266No ratings yet
- Effects of Clinical Pathways: Do They Work?: P Van Herck, K Vanhaecht and W SermeusDocument11 pagesEffects of Clinical Pathways: Do They Work?: P Van Herck, K Vanhaecht and W SermeussuriNo ratings yet
- Economic Evaluation Strategies in Telehealth: Obtaining A More Holistic Valuation of Telehealth InterventionsDocument5 pagesEconomic Evaluation Strategies in Telehealth: Obtaining A More Holistic Valuation of Telehealth InterventionsAlejandro CardonaNo ratings yet
- Jurnal Pendukung PDFDocument12 pagesJurnal Pendukung PDFMita AmaliaNo ratings yet
- A Systematic Review of The Effects of Residency Training On Patients OutcomesDocument11 pagesA Systematic Review of The Effects of Residency Training On Patients OutcomesMaik MouraNo ratings yet
- Training Code (GE.008) - CQMRDocument11 pagesTraining Code (GE.008) - CQMRBung HerryNo ratings yet
- Health Expectations - 2022 - Adams The Ultimate Question Evaluating The Use of Net Promoter Score in HealthcareDocument12 pagesHealth Expectations - 2022 - Adams The Ultimate Question Evaluating The Use of Net Promoter Score in HealthcareEliana PedrazaNo ratings yet
- 1-S2.0-S1939865422000315-MainDocument8 pages1-S2.0-S1939865422000315-MainnersrosdianaNo ratings yet
- Modified Delphi Consensus On Developing Home Care Service Quality Indicator For Stroke Survivor in Yogyakarta IndonesiaDocument7 pagesModified Delphi Consensus On Developing Home Care Service Quality Indicator For Stroke Survivor in Yogyakarta IndonesiaJufran, R (2018)No ratings yet
- CE of Diagnostic Tests Good Practice Recommendations 1709007663Document14 pagesCE of Diagnostic Tests Good Practice Recommendations 1709007663Sandro PaimNo ratings yet
- Full Download Test Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo Wood PDF Full ChapterDocument36 pagesFull Download Test Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo Wood PDF Full Chapterpapismlepal.b8x1100% (21)
- Evidence-Based Practice Project ProposalDocument7 pagesEvidence-Based Practice Project Proposalwamburamuturi001No ratings yet
- Clinical Practice Guidelines in Breast Cancer: N. Kumar Tyagi and S. Dhesy-ThindDocument10 pagesClinical Practice Guidelines in Breast Cancer: N. Kumar Tyagi and S. Dhesy-ThindsanNo ratings yet
- Research ArticleDocument11 pagesResearch ArticleJorge Durán MartínezNo ratings yet
- Test Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo WoodDocument8 pagesTest Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo WoodSusan Palacios100% (42)
- Health Coaching in Pharmacy Practice: A Systematic ReviewDocument14 pagesHealth Coaching in Pharmacy Practice: A Systematic ReviewrujaklutisNo ratings yet
- Dimensions of Patient Experience in Addiction and Mental HealthDocument11 pagesDimensions of Patient Experience in Addiction and Mental HealthVĩ Vũ NgọcNo ratings yet
- Indicators 2Document8 pagesIndicators 2giovanna.jangarelliNo ratings yet
- PDSA Improvement Plan - Kingston General Hospital: Name Institution Course Professor DateDocument5 pagesPDSA Improvement Plan - Kingston General Hospital: Name Institution Course Professor DateNilanjana ChakrabortyNo ratings yet
- Level of Pharmacist Knowledge On Writing Integrated Patient Progress Notes in One of The Government Hospital in The City of Bukittinggi, West Sumatra, IndonesiaDocument4 pagesLevel of Pharmacist Knowledge On Writing Integrated Patient Progress Notes in One of The Government Hospital in The City of Bukittinggi, West Sumatra, IndonesiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Bird Et Al. 2014. Fit For PurposeDocument17 pagesBird Et Al. 2014. Fit For PurposeGursheen KaurNo ratings yet
- Interprofessional Communication (IPC) ForDocument17 pagesInterprofessional Communication (IPC) FornersrosdianaNo ratings yet
- Factors Affecting The Choice of Public, Private, or Charity Health Care ProvidersDocument8 pagesFactors Affecting The Choice of Public, Private, or Charity Health Care ProvidersYonathan ArdhanaNo ratings yet
- Darren L. Mungcal BSN 123 Group 92 Evidence Based NursingDocument6 pagesDarren L. Mungcal BSN 123 Group 92 Evidence Based NursingRowena MungcalNo ratings yet
- Critical Pathways and Health Care ReformDocument11 pagesCritical Pathways and Health Care Reformrosie101998No ratings yet
- Integrated Care PathwayDocument3 pagesIntegrated Care PathwayFitri EmiNo ratings yet
- 556-Appropriateness of Clinical Decision Support - Final White Paper-Wei WuDocument15 pages556-Appropriateness of Clinical Decision Support - Final White Paper-Wei Wuapi-398506399No ratings yet
- Preparation For Practice of Newly Qualified Dental Practitioners in AustrailaDocument72 pagesPreparation For Practice of Newly Qualified Dental Practitioners in Austrailadk42tbcfk9No ratings yet
- Quality and Safety in Nursing: A Competency Approach to Improving OutcomesFrom EverandQuality and Safety in Nursing: A Competency Approach to Improving OutcomesGwen SherwoodNo ratings yet
- Ijms 21 08776Document22 pagesIjms 21 08776Angieda SoepartoNo ratings yet
- Fecal Calprotectin in Combination With Standard Blood Tests in The Diagnosis of Inflammatory Bowel Disease in ChildrenDocument8 pagesFecal Calprotectin in Combination With Standard Blood Tests in The Diagnosis of Inflammatory Bowel Disease in ChildrenAngieda SoepartoNo ratings yet
- Reaching Malaria Elimination On 2030-Materi Dr. Inke Nadia Diniyanti Lubis, M.Ked (Ped), Sp.A, PH.DDocument32 pagesReaching Malaria Elimination On 2030-Materi Dr. Inke Nadia Diniyanti Lubis, M.Ked (Ped), Sp.A, PH.DAngieda SoepartoNo ratings yet
- Seminar PERSI DR. WahyuniDocument52 pagesSeminar PERSI DR. WahyuniAngieda SoepartoNo ratings yet
- Action Research As A Practice-Based Practice-Kemmis-2013Document13 pagesAction Research As A Practice-Based Practice-Kemmis-2013Angieda SoepartoNo ratings yet
- An Action Research Approach To The Development of A Clinical Pathway For Women Requiring Caesarean Section-Moody-2015Document13 pagesAn Action Research Approach To The Development of A Clinical Pathway For Women Requiring Caesarean Section-Moody-2015Angieda SoepartoNo ratings yet
- A Closer Look at Using Stringer Action Research Model in Improving Student Learning-Nasrollahi-2015Document7 pagesA Closer Look at Using Stringer Action Research Model in Improving Student Learning-Nasrollahi-2015Angieda SoepartoNo ratings yet
- Alt Richter 2002Document8 pagesAlt Richter 2002Angieda SoepartoNo ratings yet
- Editorial: Insider Action ResearchDocument6 pagesEditorial: Insider Action ResearchAngieda SoepartoNo ratings yet
- Jurnal AnakDocument2 pagesJurnal AnakAngieda SoepartoNo ratings yet
- " Ekosistem Digital ": Untuk Kedaulatan Medis Indonesia, Peta Jalan, Tantangan Dan KesempatanDocument30 pages" Ekosistem Digital ": Untuk Kedaulatan Medis Indonesia, Peta Jalan, Tantangan Dan KesempatanAngieda SoepartoNo ratings yet
- Chemical Risk Assessment-Framework PDFDocument77 pagesChemical Risk Assessment-Framework PDFBoni MagtibayNo ratings yet
- Borntrager & Lyon 2015Document13 pagesBorntrager & Lyon 2015chocolatec00kieNo ratings yet
- Product Advertisements in Orthodontic Journals AJODO April 2021Document7 pagesProduct Advertisements in Orthodontic Journals AJODO April 2021saja IssaNo ratings yet
- Joc70081 1010 1022Document13 pagesJoc70081 1010 1022Diego UrrunagaNo ratings yet
- N A M A: Prof. Dr. Dr. Rozaimah Zain-Hamid, MS, SPFK PekerjaanDocument54 pagesN A M A: Prof. Dr. Dr. Rozaimah Zain-Hamid, MS, SPFK PekerjaanRitta Kumari PermaluNo ratings yet
- Human Resources For Health: What Difference Does ("Good") HRM Make?Document7 pagesHuman Resources For Health: What Difference Does ("Good") HRM Make?Shah NewazNo ratings yet
- Venepuncture Before Internship ResearchDocument14 pagesVenepuncture Before Internship Researchkamedi99No ratings yet
- Module 02 Evidence Based Practice Sy 2021Document7 pagesModule 02 Evidence Based Practice Sy 2021Ariane Pearl GabrielesNo ratings yet
- Guidelines ASPENDocument138 pagesGuidelines ASPENJaqueline Odair100% (1)
- Raw 1Document91 pagesRaw 1Gopaul UshaNo ratings yet
- Plantar Fasciitis GuidelinesDocument19 pagesPlantar Fasciitis Guidelinesband12No ratings yet
- Contemp Project Model-Gov8Document19 pagesContemp Project Model-Gov8Ahmed Mohamed Walid100% (1)
- Assignment Guidelines-HSC 6 016 1819 2Document2 pagesAssignment Guidelines-HSC 6 016 1819 2rjt903No ratings yet
- Well-Built Clinical Question (PICO)Document32 pagesWell-Built Clinical Question (PICO)noniNo ratings yet
- Test Bank For Introductory Medical Surgical Nursing 10th Edition Barbara TimbyDocument8 pagesTest Bank For Introductory Medical Surgical Nursing 10th Edition Barbara Timbycoopeeglottishe6y1No ratings yet
- Using Evidence For Public Health Decision Making: Preventing Excessive Alcohol Consumption and Related HarmsDocument48 pagesUsing Evidence For Public Health Decision Making: Preventing Excessive Alcohol Consumption and Related Harmsyamira27No ratings yet
- Ebp LectureDocument31 pagesEbp LectureTHEA KERSTI ECOTNo ratings yet
- 4.73 (FCM) EBM - Critical Appraisal On Therapy and PreventionDocument6 pages4.73 (FCM) EBM - Critical Appraisal On Therapy and PreventionEver Mary Joy EscaleraNo ratings yet
- Wood 2020Document16 pagesWood 2020facu22marmisolleNo ratings yet
- Systematic Reviews of Interventions Following Physical Abuse: Helping Practitioners and Expert Witnesses Improve The Outcomes of Child Abuse, UK, 2009Document6 pagesSystematic Reviews of Interventions Following Physical Abuse: Helping Practitioners and Expert Witnesses Improve The Outcomes of Child Abuse, UK, 2009Beverly TranNo ratings yet
- Colin Palfrey - Paul Thomas - Ceri Phillips - Evaluation For The Real World - The Impact of Evidence in Policy Making-Policy Press (2012)Document258 pagesColin Palfrey - Paul Thomas - Ceri Phillips - Evaluation For The Real World - The Impact of Evidence in Policy Making-Policy Press (2012)Inayat KhanNo ratings yet
- Exploring The Science of Complementary and Alternative MedicineDocument68 pagesExploring The Science of Complementary and Alternative MedicineAurutchat VichaiditNo ratings yet
- EBP Deliverable Module 2Document6 pagesEBP Deliverable Module 2Marian SmithNo ratings yet
- Analisa Jurnal Kelompok 9 (The History of Evidence-Based Practice in Nursing Education and Practice)Document9 pagesAnalisa Jurnal Kelompok 9 (The History of Evidence-Based Practice in Nursing Education and Practice)Viola AlvionitaNo ratings yet