Professional Documents
Culture Documents
Digoxin Dosing: o o o o o
Digoxin Dosing: o o o o o
Uploaded by
LindaCopyright:
Available Formats
You might also like
- Vaccination Roulette: Experiences, Risks and AlternativesDocument336 pagesVaccination Roulette: Experiences, Risks and AlternativesMeryl Dorey100% (3)
- Welcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinDocument16 pagesWelcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinUmair MazharNo ratings yet
- Digoxin PharmacokineticDocument17 pagesDigoxin Pharmacokineticphd0780No ratings yet
- Idamycin PIDocument12 pagesIdamycin PIMichael FreudigerNo ratings yet
- Summary Review Orig1s000SumRDocument26 pagesSummary Review Orig1s000SumRAlvaro MuñozNo ratings yet
- Analise CORTISOL Salivar Jung Et Al. (2014)Document10 pagesAnalise CORTISOL Salivar Jung Et Al. (2014)sandro kanzlerNo ratings yet
- Integrategrated Therapeutics I.Document35 pagesIntegrategrated Therapeutics I.SalahadinNo ratings yet
- Bioequivalence and Pharmacokinetic Study of Two Oral Formulations of Ciprofloxacin Tablets in Healthy Male VolunteersDocument8 pagesBioequivalence and Pharmacokinetic Study of Two Oral Formulations of Ciprofloxacin Tablets in Healthy Male VolunteersSamehabdulla AbdullaNo ratings yet
- Hyper Cvad NHLhiDocument6 pagesHyper Cvad NHLhisevag002816No ratings yet
- Therapeutic Drug Monitoring-: Dr. Justin Kurian Lecturer JSS CP MysoreDocument65 pagesTherapeutic Drug Monitoring-: Dr. Justin Kurian Lecturer JSS CP MysoreSharan GupthaNo ratings yet
- Digoxin Overdose: History & ExamDocument38 pagesDigoxin Overdose: History & ExamMicija CucuNo ratings yet
- 1 s2.0 S0149291803800930 MainDocument15 pages1 s2.0 S0149291803800930 Mainpepe_onetNo ratings yet
- Project DiebeticsDocument69 pagesProject DiebeticsJitendra YadavNo ratings yet
- Multiple IV Bolus AdministrationDocument21 pagesMultiple IV Bolus AdministrationIka NurzijahNo ratings yet
- EVMS Critical Care COVID-19 ProtocolDocument29 pagesEVMS Critical Care COVID-19 ProtocolJonathan LadinoNo ratings yet
- Prepared By: Murari Pavan M.Pharm (Pharmaceutics) Gautham College of PharmacyDocument22 pagesPrepared By: Murari Pavan M.Pharm (Pharmaceutics) Gautham College of PharmacyAshutosh LohumiNo ratings yet
- An Up-To-Date Review of Digoxin Toxicity and Its ManagementDocument6 pagesAn Up-To-Date Review of Digoxin Toxicity and Its ManagementNusieba IbrahimNo ratings yet
- Clinical PharmacokineticsDocument31 pagesClinical PharmacokineticsArdiyanti Puspitasari100% (1)
- DigoxinDocument1 pageDigoxinDedeoendutz Lovelly-brother SsiiCeueembemNo ratings yet
- Case Study Question 29Document12 pagesCase Study Question 29api-532124328100% (2)
- Aj 620214Document7 pagesAj 620214Yuppie RajNo ratings yet
- j3 2010Document12 pagesj3 2010Taha FransNo ratings yet
- Final Pharmacokinetics Workshop (Consized) - 1Document17 pagesFinal Pharmacokinetics Workshop (Consized) - 1Adlina TajuddinNo ratings yet
- Bension Mirzakan - IPPE Assignment 1.13Document4 pagesBension Mirzakan - IPPE Assignment 1.13bmirzakanNo ratings yet
- Farmakologi Klinik 2: Dr. Gestina Aliska, SP - FKDocument30 pagesFarmakologi Klinik 2: Dr. Gestina Aliska, SP - FKFadel WidePutraNo ratings yet
- Paper TemplateDocument9 pagesPaper Templateadham ahmedNo ratings yet
- Chapter 47 - Endocrine SystemDocument3 pagesChapter 47 - Endocrine SystemStacey100% (1)
- Vitamin 1Document9 pagesVitamin 1Andre ChiangNo ratings yet
- HypoglikemiaDocument7 pagesHypoglikemiaNurul MardiahNo ratings yet
- Intrathecal Hydrophilic Opioids For Abdominal SurgeryDocument15 pagesIntrathecal Hydrophilic Opioids For Abdominal Surgeryvalerio.messinaNo ratings yet
- Prof Henny Lucida PHD Apt Calculation of DosespptDocument27 pagesProf Henny Lucida PHD Apt Calculation of DosespptWella CitraersyaNo ratings yet
- Choi2014 231128 194257Document13 pagesChoi2014 231128 194257TaraaNo ratings yet
- 1 s2.0 S2589936824000173 MainDocument10 pages1 s2.0 S2589936824000173 MainluciaNo ratings yet
- Therapeutic Drug MonitoringDocument10 pagesTherapeutic Drug MonitoringAnnie SethiNo ratings yet
- PK CHARTS ContdDocument38 pagesPK CHARTS Contdshreya245sureshNo ratings yet
- (2019) Pharmaceutics IVIVC MircioiuDocument15 pages(2019) Pharmaceutics IVIVC MircioiuValentina AnutaNo ratings yet
- Clonidine WeanDocument10 pagesClonidine WeanJorge HinojosaNo ratings yet
- Non-Linear PharmacokineticsDocument6 pagesNon-Linear PharmacokineticsaristapasisingiNo ratings yet
- Diphenhydramine Hydrochloride (Benadryl) 50mg/1mlDocument6 pagesDiphenhydramine Hydrochloride (Benadryl) 50mg/1ml'SheenMarkReal'No ratings yet
- Dexmedetomidine: Pediatric Drug InformationDocument15 pagesDexmedetomidine: Pediatric Drug InformationАлексей НиколаевNo ratings yet
- Daptomycin Guidance Note - Revision 20200430Document6 pagesDaptomycin Guidance Note - Revision 20200430Marcelo UGNo ratings yet
- Digoxin PharmacokineticsDocument15 pagesDigoxin PharmacokineticsLama SaudNo ratings yet
- TDM Basic PrinciplesDocument10 pagesTDM Basic PrinciplesabinchandrakumarNo ratings yet
- Diabetes MellitusDocument37 pagesDiabetes MellitusAhmad Makhlouf100% (1)
- PK Design Doses PDFDocument7 pagesPK Design Doses PDFJuan CarNo ratings yet
- Dosage Calculations (Adult and Pediatrics)Document7 pagesDosage Calculations (Adult and Pediatrics)kirsleone_16293757No ratings yet
- Khowaja2018 Article GlycemicControlInHospitalizedP PDFDocument9 pagesKhowaja2018 Article GlycemicControlInHospitalizedP PDFMade Dedy KusnawanNo ratings yet
- 2 51 1624856559 Ijmpsdec20213Document10 pages2 51 1624856559 Ijmpsdec20213TJPRC PublicationsNo ratings yet
- Concept of Therapeutic Drug Monitoring TDMDocument33 pagesConcept of Therapeutic Drug Monitoring TDMWalaa YousefNo ratings yet
- Vitamin C, Hydrocortisone and Thiamine in Patients With Septic Shock (VITAMINS) Trial: Study Protocol and Statistical Analysis PlanDocument7 pagesVitamin C, Hydrocortisone and Thiamine in Patients With Septic Shock (VITAMINS) Trial: Study Protocol and Statistical Analysis Planjesus peñaNo ratings yet
- Dapagli Ozin Treatment For Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument18 pagesDapagli Ozin Treatment For Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsVictoria Maya ChyntiaNo ratings yet
- Udy 2010Document3 pagesUdy 2010aNo ratings yet
- Therapeutic Drug MonitoringDocument50 pagesTherapeutic Drug MonitoringKapusetti Vanaja0% (1)
- Abstract Early IdentificationDocument4 pagesAbstract Early IdentificationrhezagiovNo ratings yet
- Nephroprotective Effects of Dapagliflozin in Patients With Type 2 DiabetesDocument8 pagesNephroprotective Effects of Dapagliflozin in Patients With Type 2 DiabetesLorenaNo ratings yet
- Msic Consensus Statement: Corticosteroids For Covid-19: 27 January 2021Document4 pagesMsic Consensus Statement: Corticosteroids For Covid-19: 27 January 2021Syed Shahrul Naz SyedNo ratings yet
- Pharmacokinetics of Oral Vitamin C: I, II III IVDocument25 pagesPharmacokinetics of Oral Vitamin C: I, II III IVmarkuswolf11No ratings yet
- Fasting and TumorsDocument9 pagesFasting and Tumorsislamrnr123No ratings yet
- Batu Saluran KemihDocument22 pagesBatu Saluran KemihAgung pribadiNo ratings yet
- Renal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysFrom EverandRenal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysNo ratings yet
- Residues of Antibiotics and Sulfonamides in Honeys From Basque Country (NE Spain)Document10 pagesResidues of Antibiotics and Sulfonamides in Honeys From Basque Country (NE Spain)ivnadvNo ratings yet
- Medicinal and Aromatic Plants: Trade, Production, and Management of Botanical ResourcesDocument21 pagesMedicinal and Aromatic Plants: Trade, Production, and Management of Botanical ResourcesKenan CengicNo ratings yet
- Bacterial Histidine Kinases As Novel Antibacterial Drug TargetsDocument12 pagesBacterial Histidine Kinases As Novel Antibacterial Drug TargetsSritapa Basu MallickNo ratings yet
- Purdue Pharma-Mass. AGDocument312 pagesPurdue Pharma-Mass. AGWews WebStaff100% (1)
- Empirical Prescribing Chart GlasgowDocument1 pageEmpirical Prescribing Chart GlasgowHariharan Narendran75% (4)
- Tugas Praktek Spesialite Iv - Vii (Kel 1)Document6 pagesTugas Praktek Spesialite Iv - Vii (Kel 1)agustinus randa100% (1)
- Anaphylactic Shock Treatment KitDocument2 pagesAnaphylactic Shock Treatment KitSurya DilaNo ratings yet
- Clean Room HVAC Design For Pharmaceutical Facilities: Presented By: Under Guidance ofDocument40 pagesClean Room HVAC Design For Pharmaceutical Facilities: Presented By: Under Guidance ofRobin Erazo BenitezNo ratings yet
- Report 5-FU 35 Days ENG 150115Document14 pagesReport 5-FU 35 Days ENG 150115Grace ValenciaNo ratings yet
- Catalog BenylinDocument4 pagesCatalog Benylinapi-312329159No ratings yet
- Can I Apply?: P.O. Box 5727, Louisville, Kentucky 40255-0727 Phone: 1-800-830-9159 Fax: 1-800-497-0928Document4 pagesCan I Apply?: P.O. Box 5727, Louisville, Kentucky 40255-0727 Phone: 1-800-830-9159 Fax: 1-800-497-0928VelozaNo ratings yet
- Stress Ulcer Ditinjau Dari Aspek Patofisiologi Dan TreatmentDocument16 pagesStress Ulcer Ditinjau Dari Aspek Patofisiologi Dan TreatmentJufri NstNo ratings yet
- GuideDocument124 pagesGuideBenjamin TantiansuNo ratings yet
- USP Stim Article On Calculation-PF-2005Document12 pagesUSP Stim Article On Calculation-PF-2005Mubarak PatelNo ratings yet
- Handout - PBM BTM - l1 To l4Document113 pagesHandout - PBM BTM - l1 To l4Bob BinNo ratings yet
- Royal Pharmac Euticals: GmailDocument2 pagesRoyal Pharmac Euticals: GmailArisha NusratNo ratings yet
- Timolol 2Document19 pagesTimolol 2Atthapu ThirupathaiahNo ratings yet
- NovoRapid (Insulin Aspart) PDFDocument113 pagesNovoRapid (Insulin Aspart) PDFAchmad SuryadiNo ratings yet
- Formulation and Evaluation of Fast Dissolving Tablets of Aceclofenac by Using Ispaghula Husk Powder As Natural Super DisintegrantDocument9 pagesFormulation and Evaluation of Fast Dissolving Tablets of Aceclofenac by Using Ispaghula Husk Powder As Natural Super DisintegrantBaru Chandrasekhar RaoNo ratings yet
- FDC Guidelines - Revised1Document38 pagesFDC Guidelines - Revised1gpg19751215No ratings yet
- Fentanyl Analouge SynthDocument11 pagesFentanyl Analouge SynthamesffNo ratings yet
- Hospital and Clinical PharmacyDocument18 pagesHospital and Clinical PharmacySayeeda MohammedNo ratings yet
- Q.P. Code: 544172Document5 pagesQ.P. Code: 544172mybdsexamsourceNo ratings yet
- IVIVCDocument33 pagesIVIVCPrashant GargNo ratings yet
- St. John's Wort: Clinical OverviewDocument14 pagesSt. John's Wort: Clinical OverviewTrismegisteNo ratings yet
- 24 Emergency DrugsDocument7 pages24 Emergency DrugsApple BelicanNo ratings yet
- Aonla Cultivation Is Profitable SereddyDocument3 pagesAonla Cultivation Is Profitable SereddyDr.Eswara Reddy SiddareddyNo ratings yet
- PDDPharmacyprojectDocument22 pagesPDDPharmacyprojectGeeta G. Kulkarni100% (1)
- MGT490 Group Assignemnt 01Document22 pagesMGT490 Group Assignemnt 01Dark RushNo ratings yet
Digoxin Dosing: o o o o o
Digoxin Dosing: o o o o o
Uploaded by
LindaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Digoxin Dosing: o o o o o
Digoxin Dosing: o o o o o
Uploaded by
LindaCopyright:
Available Formats
Digoxin dosing
I. Introduction
Digoxin is one of the most commonly used drugs in medicine. Despite this widespread use and a history of over
200 years of clinical use and research, much controversy continues concerning its efficacy and safety.
Two of the most prominent features of the clinical use of digoxin are its narrow therapeutic index and an
endpoint of therapy which is difficult to define and measure. Digitalis toxicity is one of the most frequently
encountered drug-related causes of hospitalization. Conversely, the effect of serum digoxin concentrations
below 0.8 ng/ml is clinically unimportant in most patients.
The great variability in serum digoxin concentrations in patients given the same dose has led to the
development of nomograms and equations designed to estimate the optimal digoxin dosage. These methods
include factors such as age, weight, sex, renal function, disease state, and concurrent drug therapy to calculate
the dose and corresponding serum concentration. An accurate method could decrease the potential for drug
toxicity, which can be life-threatening, and decrease the time period required to optimize therapy, which is
otherwise done by trial and error.
Lalonde and Pao compared the accuracy of eighteen different digoxin dosing methods. The method of Dobbs
and Koup as modified by Koda-Kimble, appeared to produce the best balance of minimum bias and greatest
precision. Using a target concentration of 1.2 ng/ml, the Koda-Kimble method achieves a concentration
between 0.9 and 1.5 ng/ml in 80% of cases. However, some patients will have measured serum digoxin
concentrations well outside this range.
An adequate loading dose is necessary for rapid attainment of therapeutic serum levels. Choosing to initiate
therapy with out a loading dose means that, because of digoxin's long half-life, therapeutic serum levels may
not be achieved for weeks.
II. Monitoring parameters
1. The following patient parameters should be monitored during digoxin therapy:
o Digoxin serum level
Obtain level within 24 hours of digitalization, weekly until stable, and at steady state.
o BUN and serum creatinine
Measure every two days, or every day in unstable renal function.
o Weigh patient daily.
o Measure and monitor urine output daily
o Monitor apical pulse daily.
2. Therapeutic serum concentrations
The usual digoxin therapeutic range is 0.8 to 2 ng/ml.
III. Precautions
1. Proper timing of serum sampling is critical.
Serum samples should be drawn just prior to the daily dose and no sooner than six hours after administration of
the drug.
2. Factors affecting digoxin pharmacokinetics
a. Factors which predispose to digoxin toxicity:
Hypokalemia, hypomagnesemia, coronary artery disease, cor pulmonale, uncorrected hypothyroidism,
renal dysfunction, and interacting drugs which decrease digoxin clearance (quinidine, spironolactone,
and verapamil).
b. Factors which predispose to suboptimal clinical response:
Hyperkalemia, uncorrected hyperthyroidism, interacting drugs which delay or prevent oral absorption
(antacids, cholestyramine, metoclopramide).
IV. Program procedure
Before calculating an initial dose or adjusting the maintenance dose the program must know the target digoxin
serum level, whether the patient is in acute congestive failure and whether any interacting drugs are being
concurrently administered.
1. Initial dosing
The program first calculates an ideal loading dose, enter a practical dose and the desired dosage form of
the loading dose. Enter 0 if no loading dose is desired. The program calculates an ideal maintenance
dose, the user enters a practical maintenance dose and interval. The program then displays an estimated
steady-state serum level.
2. Dosage adjustment based on serum levels
First enter the measured serum digoxin concentration, the dosage form, digoxin dose and interval. The
program then requires the date and time the current dosage regimen was initiated, this is used to
determine whether the patient’s digoxin level is at a steady-state. The program then calculates an
incremental loading dose or temporary interruption, depending upon whether the serum level is below
or above the target level. The user enters a practical loading dose or temporary interruption. The
program calculates an ideal maintenance dose and the user enters a practical maintenance dose and
interval. The program then displays an estimated steady-state serum level.
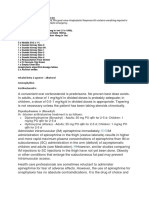
V. Digoxin dosing flow chart
VI. Pharmacokinetic formulas
The digoxin model is not hard-coded into the program. The parameters are found in the drug model database
and are fully user-editable. You can tailor each drug model to fit your patient population, or you can create your
own models.
Initial dosing
1. Estimate Volume of Distribution (Jusko Equation)
Vd = 226 + [(298 x CrCl) / (29.1 + CrCl)] x (BSA / 1.73)
where CrCl = normalized creatinine clearance (ml/min)
BSA = Body surface area (square meters)
2. Calculate Loading Dose
LD = Vd x Cp/F
where Vd = Volume of distribution (liters)
Cp = target serum level (mcg/l)
F = bioavailability factor
IV push = 1
capsules= 0.95
elixir = 0.8
tablets = 0.75
3. Estimate Clearance (Koda-Kimble)
Cl = [(A x CrCl) + B] x C
where A = 0.88, for patient with Acute CHF, otherwise=1
B = 23, for patient with Acute CHF, otherwise=40
C = correction factor for interacting drugs
Quinidine = 0.65
Spironolactone = 0.75
Verapamil = 0.7
4. Calculate Maintenance Dose
MD = (Cl x Cp x tau) / F
where Cl = Clearance (liters/hour)
Cp = target serum level (mcg/l)
tau = dosing interval (hours)
F = bioavailability factor
5. Estimate steady-state trough level
Cpss = (MD x F) / (Cl x tau)
where MD = Maintenance dose (mcg)
F = bioavailability factor
Cl = Clearance (liters/hour)
tau = dosing interval (hours)
B. Adjust maintenance dose
1. Estimate Volume of Distribution (Jusko Equation - see above)
2. Calculate digoxin clearance
Cl = [(MD x F) / Cp] / tau
where MD = Maintenance dose (mcg)
F = Bioavailability factor
Cp = Steady-state serum digoxin concentration (mcg/l)
tau = Dosing interval (hours)
3. Calculate Maintenance Dose
MD = (Cl x Cp x tau) / F
where Cl = Digoxin clearance (l/hr)
Cp = target serum level (mcg/l)
tau = dosing interval (hours)
F = bioavailability factor
4. Estimate steady-state trough level
Cpss = (MD x F) / (Kel x Vd x tau)
where MD = Maintenance dose (mcg)
F = bioavailability factor
Kel = Elimination rate (1/hours)
Vd = Volume of distribution (liters)
tau = dosing interval (hours)
VII. Bibliography
1. Jusko WJ, et al. Pharmacokinetic design of digoxin dosage regimens in relation to renal function. J Clin
Pharmacol 1974;14:525-35.
2. Koup JR, et al. Digoxin pharmacokinetics: role of renal failure in dosage regimen design. Clin Pharmacol Ther
1975;18:9-21.
3. Walsh FM, Sode J. Significance of non-steady-state serum digoxin concentrations. Am J Clin Pathol 1975;63:446-
50.
4. Dobbs SM, Mawer GE. Prediction of digoxin dose requirements. Clin Pharmacok 1977;2:281-91.
5. Koda-Kimble MA: Congestive heart failure, in Applied Therapeutics for Clinical Pharmacists, 2nd ed, edited by
MA Koda-Kimble et al, Applied Therapeutics, Inc, San Francisco 1978; pp 161-86.
6. Thomas RW, Maddox RR. The interaction of spironolactone and digoxin: a review and evaluation. Ther Drug
Monit 1981;3:117-20.
7. Klein HO, et al. The influence of verapamil on serum digoxin concentration. Circul 1982;65:998-1003.
8. Hyneck ML, et al. Comparison of methods for estimating digoxin dosing regimens. AJHP 1981;38:69-73.
9. Bigger JT. The quinidine-digoxin interaction. Mod Con Card Dis 1982;51:73-78.
10. Lalonde RL, Pao D. Correlation coefficient versus prediction error in assessing the accuracy of digoxin dosing
methods. Clin Pharm 1984;3:178-83.
11. Reuning RH, Garaets DR. "Digoxin", in Evans W, Schentag J, Jusko J (eds): Applied Pharmacokinetics. Applied
Therapeutics, Inc, San Francisco 1986; pp 908-43.
You might also like
- Vaccination Roulette: Experiences, Risks and AlternativesDocument336 pagesVaccination Roulette: Experiences, Risks and AlternativesMeryl Dorey100% (3)
- Welcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinDocument16 pagesWelcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinUmair MazharNo ratings yet
- Digoxin PharmacokineticDocument17 pagesDigoxin Pharmacokineticphd0780No ratings yet
- Idamycin PIDocument12 pagesIdamycin PIMichael FreudigerNo ratings yet
- Summary Review Orig1s000SumRDocument26 pagesSummary Review Orig1s000SumRAlvaro MuñozNo ratings yet
- Analise CORTISOL Salivar Jung Et Al. (2014)Document10 pagesAnalise CORTISOL Salivar Jung Et Al. (2014)sandro kanzlerNo ratings yet
- Integrategrated Therapeutics I.Document35 pagesIntegrategrated Therapeutics I.SalahadinNo ratings yet
- Bioequivalence and Pharmacokinetic Study of Two Oral Formulations of Ciprofloxacin Tablets in Healthy Male VolunteersDocument8 pagesBioequivalence and Pharmacokinetic Study of Two Oral Formulations of Ciprofloxacin Tablets in Healthy Male VolunteersSamehabdulla AbdullaNo ratings yet
- Hyper Cvad NHLhiDocument6 pagesHyper Cvad NHLhisevag002816No ratings yet
- Therapeutic Drug Monitoring-: Dr. Justin Kurian Lecturer JSS CP MysoreDocument65 pagesTherapeutic Drug Monitoring-: Dr. Justin Kurian Lecturer JSS CP MysoreSharan GupthaNo ratings yet
- Digoxin Overdose: History & ExamDocument38 pagesDigoxin Overdose: History & ExamMicija CucuNo ratings yet
- 1 s2.0 S0149291803800930 MainDocument15 pages1 s2.0 S0149291803800930 Mainpepe_onetNo ratings yet
- Project DiebeticsDocument69 pagesProject DiebeticsJitendra YadavNo ratings yet
- Multiple IV Bolus AdministrationDocument21 pagesMultiple IV Bolus AdministrationIka NurzijahNo ratings yet
- EVMS Critical Care COVID-19 ProtocolDocument29 pagesEVMS Critical Care COVID-19 ProtocolJonathan LadinoNo ratings yet
- Prepared By: Murari Pavan M.Pharm (Pharmaceutics) Gautham College of PharmacyDocument22 pagesPrepared By: Murari Pavan M.Pharm (Pharmaceutics) Gautham College of PharmacyAshutosh LohumiNo ratings yet
- An Up-To-Date Review of Digoxin Toxicity and Its ManagementDocument6 pagesAn Up-To-Date Review of Digoxin Toxicity and Its ManagementNusieba IbrahimNo ratings yet
- Clinical PharmacokineticsDocument31 pagesClinical PharmacokineticsArdiyanti Puspitasari100% (1)
- DigoxinDocument1 pageDigoxinDedeoendutz Lovelly-brother SsiiCeueembemNo ratings yet
- Case Study Question 29Document12 pagesCase Study Question 29api-532124328100% (2)
- Aj 620214Document7 pagesAj 620214Yuppie RajNo ratings yet
- j3 2010Document12 pagesj3 2010Taha FransNo ratings yet
- Final Pharmacokinetics Workshop (Consized) - 1Document17 pagesFinal Pharmacokinetics Workshop (Consized) - 1Adlina TajuddinNo ratings yet
- Bension Mirzakan - IPPE Assignment 1.13Document4 pagesBension Mirzakan - IPPE Assignment 1.13bmirzakanNo ratings yet
- Farmakologi Klinik 2: Dr. Gestina Aliska, SP - FKDocument30 pagesFarmakologi Klinik 2: Dr. Gestina Aliska, SP - FKFadel WidePutraNo ratings yet
- Paper TemplateDocument9 pagesPaper Templateadham ahmedNo ratings yet
- Chapter 47 - Endocrine SystemDocument3 pagesChapter 47 - Endocrine SystemStacey100% (1)
- Vitamin 1Document9 pagesVitamin 1Andre ChiangNo ratings yet
- HypoglikemiaDocument7 pagesHypoglikemiaNurul MardiahNo ratings yet
- Intrathecal Hydrophilic Opioids For Abdominal SurgeryDocument15 pagesIntrathecal Hydrophilic Opioids For Abdominal Surgeryvalerio.messinaNo ratings yet
- Prof Henny Lucida PHD Apt Calculation of DosespptDocument27 pagesProf Henny Lucida PHD Apt Calculation of DosespptWella CitraersyaNo ratings yet
- Choi2014 231128 194257Document13 pagesChoi2014 231128 194257TaraaNo ratings yet
- 1 s2.0 S2589936824000173 MainDocument10 pages1 s2.0 S2589936824000173 MainluciaNo ratings yet
- Therapeutic Drug MonitoringDocument10 pagesTherapeutic Drug MonitoringAnnie SethiNo ratings yet
- PK CHARTS ContdDocument38 pagesPK CHARTS Contdshreya245sureshNo ratings yet
- (2019) Pharmaceutics IVIVC MircioiuDocument15 pages(2019) Pharmaceutics IVIVC MircioiuValentina AnutaNo ratings yet
- Clonidine WeanDocument10 pagesClonidine WeanJorge HinojosaNo ratings yet
- Non-Linear PharmacokineticsDocument6 pagesNon-Linear PharmacokineticsaristapasisingiNo ratings yet
- Diphenhydramine Hydrochloride (Benadryl) 50mg/1mlDocument6 pagesDiphenhydramine Hydrochloride (Benadryl) 50mg/1ml'SheenMarkReal'No ratings yet
- Dexmedetomidine: Pediatric Drug InformationDocument15 pagesDexmedetomidine: Pediatric Drug InformationАлексей НиколаевNo ratings yet
- Daptomycin Guidance Note - Revision 20200430Document6 pagesDaptomycin Guidance Note - Revision 20200430Marcelo UGNo ratings yet
- Digoxin PharmacokineticsDocument15 pagesDigoxin PharmacokineticsLama SaudNo ratings yet
- TDM Basic PrinciplesDocument10 pagesTDM Basic PrinciplesabinchandrakumarNo ratings yet
- Diabetes MellitusDocument37 pagesDiabetes MellitusAhmad Makhlouf100% (1)
- PK Design Doses PDFDocument7 pagesPK Design Doses PDFJuan CarNo ratings yet
- Dosage Calculations (Adult and Pediatrics)Document7 pagesDosage Calculations (Adult and Pediatrics)kirsleone_16293757No ratings yet
- Khowaja2018 Article GlycemicControlInHospitalizedP PDFDocument9 pagesKhowaja2018 Article GlycemicControlInHospitalizedP PDFMade Dedy KusnawanNo ratings yet
- 2 51 1624856559 Ijmpsdec20213Document10 pages2 51 1624856559 Ijmpsdec20213TJPRC PublicationsNo ratings yet
- Concept of Therapeutic Drug Monitoring TDMDocument33 pagesConcept of Therapeutic Drug Monitoring TDMWalaa YousefNo ratings yet
- Vitamin C, Hydrocortisone and Thiamine in Patients With Septic Shock (VITAMINS) Trial: Study Protocol and Statistical Analysis PlanDocument7 pagesVitamin C, Hydrocortisone and Thiamine in Patients With Septic Shock (VITAMINS) Trial: Study Protocol and Statistical Analysis Planjesus peñaNo ratings yet
- Dapagli Ozin Treatment For Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument18 pagesDapagli Ozin Treatment For Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsVictoria Maya ChyntiaNo ratings yet
- Udy 2010Document3 pagesUdy 2010aNo ratings yet
- Therapeutic Drug MonitoringDocument50 pagesTherapeutic Drug MonitoringKapusetti Vanaja0% (1)
- Abstract Early IdentificationDocument4 pagesAbstract Early IdentificationrhezagiovNo ratings yet
- Nephroprotective Effects of Dapagliflozin in Patients With Type 2 DiabetesDocument8 pagesNephroprotective Effects of Dapagliflozin in Patients With Type 2 DiabetesLorenaNo ratings yet
- Msic Consensus Statement: Corticosteroids For Covid-19: 27 January 2021Document4 pagesMsic Consensus Statement: Corticosteroids For Covid-19: 27 January 2021Syed Shahrul Naz SyedNo ratings yet
- Pharmacokinetics of Oral Vitamin C: I, II III IVDocument25 pagesPharmacokinetics of Oral Vitamin C: I, II III IVmarkuswolf11No ratings yet
- Fasting and TumorsDocument9 pagesFasting and Tumorsislamrnr123No ratings yet
- Batu Saluran KemihDocument22 pagesBatu Saluran KemihAgung pribadiNo ratings yet
- Renal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysFrom EverandRenal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysNo ratings yet
- Residues of Antibiotics and Sulfonamides in Honeys From Basque Country (NE Spain)Document10 pagesResidues of Antibiotics and Sulfonamides in Honeys From Basque Country (NE Spain)ivnadvNo ratings yet
- Medicinal and Aromatic Plants: Trade, Production, and Management of Botanical ResourcesDocument21 pagesMedicinal and Aromatic Plants: Trade, Production, and Management of Botanical ResourcesKenan CengicNo ratings yet
- Bacterial Histidine Kinases As Novel Antibacterial Drug TargetsDocument12 pagesBacterial Histidine Kinases As Novel Antibacterial Drug TargetsSritapa Basu MallickNo ratings yet
- Purdue Pharma-Mass. AGDocument312 pagesPurdue Pharma-Mass. AGWews WebStaff100% (1)
- Empirical Prescribing Chart GlasgowDocument1 pageEmpirical Prescribing Chart GlasgowHariharan Narendran75% (4)
- Tugas Praktek Spesialite Iv - Vii (Kel 1)Document6 pagesTugas Praktek Spesialite Iv - Vii (Kel 1)agustinus randa100% (1)
- Anaphylactic Shock Treatment KitDocument2 pagesAnaphylactic Shock Treatment KitSurya DilaNo ratings yet
- Clean Room HVAC Design For Pharmaceutical Facilities: Presented By: Under Guidance ofDocument40 pagesClean Room HVAC Design For Pharmaceutical Facilities: Presented By: Under Guidance ofRobin Erazo BenitezNo ratings yet
- Report 5-FU 35 Days ENG 150115Document14 pagesReport 5-FU 35 Days ENG 150115Grace ValenciaNo ratings yet
- Catalog BenylinDocument4 pagesCatalog Benylinapi-312329159No ratings yet
- Can I Apply?: P.O. Box 5727, Louisville, Kentucky 40255-0727 Phone: 1-800-830-9159 Fax: 1-800-497-0928Document4 pagesCan I Apply?: P.O. Box 5727, Louisville, Kentucky 40255-0727 Phone: 1-800-830-9159 Fax: 1-800-497-0928VelozaNo ratings yet
- Stress Ulcer Ditinjau Dari Aspek Patofisiologi Dan TreatmentDocument16 pagesStress Ulcer Ditinjau Dari Aspek Patofisiologi Dan TreatmentJufri NstNo ratings yet
- GuideDocument124 pagesGuideBenjamin TantiansuNo ratings yet
- USP Stim Article On Calculation-PF-2005Document12 pagesUSP Stim Article On Calculation-PF-2005Mubarak PatelNo ratings yet
- Handout - PBM BTM - l1 To l4Document113 pagesHandout - PBM BTM - l1 To l4Bob BinNo ratings yet
- Royal Pharmac Euticals: GmailDocument2 pagesRoyal Pharmac Euticals: GmailArisha NusratNo ratings yet
- Timolol 2Document19 pagesTimolol 2Atthapu ThirupathaiahNo ratings yet
- NovoRapid (Insulin Aspart) PDFDocument113 pagesNovoRapid (Insulin Aspart) PDFAchmad SuryadiNo ratings yet
- Formulation and Evaluation of Fast Dissolving Tablets of Aceclofenac by Using Ispaghula Husk Powder As Natural Super DisintegrantDocument9 pagesFormulation and Evaluation of Fast Dissolving Tablets of Aceclofenac by Using Ispaghula Husk Powder As Natural Super DisintegrantBaru Chandrasekhar RaoNo ratings yet
- FDC Guidelines - Revised1Document38 pagesFDC Guidelines - Revised1gpg19751215No ratings yet
- Fentanyl Analouge SynthDocument11 pagesFentanyl Analouge SynthamesffNo ratings yet
- Hospital and Clinical PharmacyDocument18 pagesHospital and Clinical PharmacySayeeda MohammedNo ratings yet
- Q.P. Code: 544172Document5 pagesQ.P. Code: 544172mybdsexamsourceNo ratings yet
- IVIVCDocument33 pagesIVIVCPrashant GargNo ratings yet
- St. John's Wort: Clinical OverviewDocument14 pagesSt. John's Wort: Clinical OverviewTrismegisteNo ratings yet
- 24 Emergency DrugsDocument7 pages24 Emergency DrugsApple BelicanNo ratings yet
- Aonla Cultivation Is Profitable SereddyDocument3 pagesAonla Cultivation Is Profitable SereddyDr.Eswara Reddy SiddareddyNo ratings yet
- PDDPharmacyprojectDocument22 pagesPDDPharmacyprojectGeeta G. Kulkarni100% (1)
- MGT490 Group Assignemnt 01Document22 pagesMGT490 Group Assignemnt 01Dark RushNo ratings yet