Professional Documents
Culture Documents
BCMJ 49 Vol3 Articles Posttraumatic Stress
BCMJ 49 Vol3 Articles Posttraumatic Stress
Uploaded by
Francisca AldunateOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BCMJ 49 Vol3 Articles Posttraumatic Stress
BCMJ 49 Vol3 Articles Posttraumatic Stress
Uploaded by
Francisca AldunateCopyright:
Available Formats
Myles Blank, MD, FRCPC
Posttraumatic stress
disorder in infants,
toddlers, and preschoolers
Play therapy, psychoeducation, and family support are key when
trauma affects children in the preverbal and early verbal years.
osttraumatic stress disorder in prevalence statistics. The DSM-IV-
(PTSD) in infants and young TR indicates that 1% of people in the
P
ABSTRACT: Posttraumatic stress
children is a relatively new general population have been diag-
disorder in children, like pain con-
concept. Awareness of this phenome- nosed with a full syndrome and 14%
trol and other issues of children’s
non has grown out of knowledge of with a partial syndrome. Others have
perceptions of their environment, is
PTSD in adults and older children, in found a higher prevalence. In contrast
a relatively new concept. Although
combination with case reports high- to the DSM-IV numbers, Hidalgo and
studies are rare, we do have an
lighting unique aspects of trauma in Davidson found prevalence of 8% to
understanding of special diagnostic
small children. There is relatively lit- 9%2 in the general population and
criteria that should be considered,
tle research on this subject, but the Breslau found a similar 1:12 ratio in
along with the role played by attach-
field is growing. At this time, we the adult population. 3 Thus, it is prob-
ment, temperament, memory, cogni-
know that: ably more appropriate to look at the
tion, and affect regulation. Repeated
• PTSD does occur in the preverbal percentage of individuals exposed to
trauma may affect children pro-
and early verbal years. trauma who develop PTSD rather than
foundly during sensitive periods of
• PTSD has some unique presenting the percentage of the general popu-
brain development through putative
features related to the developmental lation. Here the estimates indicate
biological stress mediators. This
level and other contextual features of that 15% to 24% of exposed individu-
response to trauma may also par-
the child’s life. als develop PTSD. Most authors also
tially explain the high incidence of
• The Diagnostic and Statistical Man- feel that the type of exposure is sig-
psychiatric comorbidity in these
ual of Mental Disorders (DSM-IV- nificant, with some severe exposures,
children. Developmentally appropri-
TR)1 criteria are often not sensitive such as watching the sexual assault of
ate assessment and therapy require
enough to diagnose PTSD in infants a parent, resulting in an incidence rate
awareness of the nonverbal (behav-
and young children. of almost 100%, while others, such as
ioral) presenting features in the very
• Therapy is possible using play, be - a minor dog bite, may result in much
young and sensitivity to the caregiv-
havioral techniques, psychoeduca- lower rates of PTSD. 4
er’s stress and attachment issues.
tion, and family support.
Interview and therapeutic techniques
• PTSD can occur in different forms
used in tertiary care and other set-
based on the nature of the trauma
tings include play, storytelling, psy-
itself.
choeducation, grief work, and fami- Dr Blank is a clinical associate professor in
ly support. In addition to being aware the Department of Psychiatry at the Uni-
of diagnostic criteria and treatment versity of British Columbia as well as a staff
There are no studies regarding the
strategies, physicians should know Epidemiology psychiatrist in the Infant Psychiatry Clinic at
prevalence of PTSD specifically in
about medicolegal pitfalls and pos- BC Children’s and Women’s Hospital. He
very young children. Even in the area
sible therapist reactions when car- also consults to Vancouver Community
of older youth, there is some variation
ing for young children with posttrau- Mental Health Services and has a private
matic stress disorder. clinical practice.
VOL. 49 NO. 3, APRIL 2007 BC MEDICAL JOURNAL 133
Posttraumatic stress disorder in infants, toddlers, and preschoolers
PTSD was first described as “shell
Historical overview Table 1. Symptoms of posttraumatic stress disorder in children 0 to 36 months.
shock” in war veterans, a diagnosis
that frequently resulted in a dishonor-
0–6 6–12 12–18 18–24 24–36
able discharge from the army. In terms
months months months months months
of children, early groundwork was laid
by Anna Freud, 5 who looked at trau-
Hypervigilance, exaggerated
startle response, irritability,
matized war orphans; Rene Spitz, who
X X X X X
physiologic deregulation
described “hospitalism” in children
and/or withdrawal
who were severely neglected in insti-
tutions; 6 and David Levy, who pub-
Increased anxiety in strange
situations, angry reactions,
lished a landmark study in 1945 on
X X X X
sleep disorders, active avoid-
psychic traumas connected with child-
ance of specific situations
hood surgeries. 7 More recently, Lenore
Clinginess to caretaker,
Terr has produced a strong body of
over/under use of words X X X
work, including a study of 26 young-
related to the trauma
sters who were kidnapped and buried in
Nightmares, enlarged verbal
California. 8 She also looked at what
preoccupations with symbols X X
happened to memories of early trauma
of trauma
in 20 youngsters who had suffered psy-
chic traumas before age 5. This latter
Symptoms seen in older
children, as described in X
study was noteworthy in that these
DSM-IVR-TR*
children had forensic evidence sup-
porting the specific trauma histories. 9
Adapted from: Handbook of Infant Mental Health10
* A PTSD diagnosis requires all of the following: A. Trauma event. B. One or more re-experiencing
In 1993, the first book chapter about
symptoms, e.g., nightmares. C. Three or more avoidance symptoms, e.g., avoiding places, activities,
posttraumatic reactions in children
and people that arouse recollections of trauma. D. Two or more symptoms of persistent arousal e.g.,
from birth to age 3 was published. 10
hypervigilance or exaggerated startle response. E. Duration greater than 1 month. F. Clinically signif-
icant distress or impairment.
specific one. These studies conclude a primary caregiver. While this makes
that there is in fact validation for the sense from an attachment perspective,
In 1994, the Zero to Three organiza- recommended modifications of DSM- it is also crucial to consider the devel-
Diagnostic criteria
tion listed “traumatic stress disorder” IV criteria to deal with infants, tod- opmental capacity of a given child in
in their manual classifying mental dlers, and preschoolers. The Infant assessing the effects of trauma and/or
health and developmental disorders Psychiatry Clinic at BC Children’s the presence of PTSD.
of infancy and early childhood DC: Hospital routinely uses criteria from PTSD per se can occur in infants 9
0–3.11 Subsequently, a study compared DC: 0–3R,14 the second edition of the months of age or older. Prior to this,
the DSM-IV criteria with the DC: 0–3 Zero to Three manual. This allows infants can have conditioned respons-
criteria in infants, 12 and this study was more highly symptomatic young chil- es to fear, which certainly can be sig-
later expanded to look at trauma in dren to receive a diagnosis and, in turn, nificant, but do not seem to represent
preschoolers. 13 What was discovered in appropriate treatment. PTSD as we understand it. Actual man-
both of these studies is that the ifestations of PTSD vary during dif-
DSM-IV criteria diagnose very few ferent periods of infant development,
cases, even in the most extremely dis- as seen in Table 1 . When considering
Etiology and individual
turbed infant survivors of trauma. The It is as important to consider the indi- the role of developmental capacities in
differences
explanation offered is that a verbal vidual characteristics of the child who PTSD, the following factors must be
report of symptoms is required for is experiencing the trauma as it is to taken into account.
nearly one half of DSM-IV criteria, look at the features of the trauma itself.
which is beyond the developmental Recent studies have shown, somewhat Temperament. While there are no
capacity of most of these children. It surprisingly, that the most potent vari- specific studies on this, children with
has also been noted that the “B” set of able affecting the degree of trauma and more difficult temperaments can be
diagnostic criteria is the only trauma- its resolution is the perceived threat to expected to have more severe or com-
134 BC MEDICAL JOURNAL VOL. 49 NO. 3, APRIL 2007
Posttraumatic stress disorder in infants, toddlers, and preschoolers
plex reactions to trauma. explain why only some individuals matic “states” become “traits.” Perry
exposed to traumatic stress will devel- has described how infants and older
comprehension. These will inevitably op PTSD. The caregivers in the type individuals respond to a threat along
Cognitive functioning and level of
affect the child’s reaction. D attachment situation are character- two pathways. One is the well-known
ized in the literature as “frightened and “fight or flight” response, which Perry
These two features go together in the frightening” and, particularly in the calls the arousal continuum, whereby
Memory and verbal expression.
sense that the right brain is dominant case of the “frightening” caregiver, the a progression of biochemical reactions
for approximately the first 18 months child is in a dilemma. The person who result in increased cortisol (as well as
of life15 and the memory that a child is supposed to be providing safety and other more poorly understood phe-
lays down during this time is of a non- security is also the perpetrator, pre- nomena). The other pathway Perry
verbal or “implicit” type. Feelings senting the vulnerable child with a ter- describes is the dissociative contin-
associated with memories are encoded rible approach-avoid situation. Cur- uum, whereby there are gaps in the
in somatic and sensory areas, which rently, the literature strongly supports stream of consciousness. Endogenous
are unconscious, but not necessarily a much higher incidence of type D opiates and activation of the parasym-
“repressed” in the traditional sense of attachment patterns with children of pathetic nervous system lead to the
the term. The implication is that just parents who have a history of unre- “freeze or surrender” response, with
because children cannot or do not talk solved trauma and loss. 17 Type D decreased movement and decreased
about their feelings does not mean that attachment can work at the very earli- attention. With repeated activation, the
feelings are not there. Another way of est level of “implicit-unconscious arousal pathways can make a child
looking at this is that some of the mechanisms” to limit a child’s ability with anxiety or trauma appear to have
memories may be in pictures that are to communicate and read emotional attention deficit hyperactivity disorder
triggered by sensory reminders to the states of self and others. It can also (ADHD), while older children with the
limbic system and lower centres of the contribute to difficulties maintaining more dissociative aspects may appear
brain. Clinicians and researchers have interactions with a social environ- to have not only attention problems
theorized that brain development, par- ment, difficulty using higher levels but also learning disabilities, memory
ticularly of limbic structures, accounts of defences at a later age, lower problems, and behavior problems. 18
for the fact that age 3 (28 to 36 months) empathic capacity, and more difficulty Children with PTSD can certainly
appears to be an approximate cut-off in recovering from stressful states. manifest a combination of arousal and
separating the children who will have Critical periods of brain development dissociation, and any given child may
absent or spotty verbal memories of (especially the first 2 years of life) rep- demonstrate different types of reac-
their traumas from those who will resent a time when attachment func- tions to a given trauma. Physical pain,
have a full verbal recollection. Some tioning and caregiver interactions can along with the nature of the trauma,
others have noted that verbal recollec- establish either resilience or vulner- may also modify these manifestations
tions appear to require a degree of con- ability toward trauma. 15 Affect dys - of PTSD.
scious awareness, while behavioral regulation is now seen to be a funda- It should be noted that dissociation
memories and enactments do not. 9 mental mechanism of all psychiatric and dissociative disorders per se are
dis orders. 15 Type D early “relational closely related to psychic trauma and
Bowlby16 and Schore15 along with other trauma” could predispose a child to can be looked at as both a neurobio-
Attachment and affect regulation.
investigators have noted the vul - more chronic expressions of PTSD. logical reaction and a psychological
nerability of children with less secure defence.
at tachments. S chore has focused
particular attention on the type D
The biology of
(disorganized/disoriented) attachment Trauma is an external factor that clear-
early trauma Clinical presentation of
pattern, where the infant displays dis- ly appears to change brain chemistry Trauma can present in a relatively obvi-
trauma and PTSD
oriented, apprehensive, contradictory, and probably structure. While these ous fashion, with observable behavioral
or chaotic behaviors upon reunion neurobiological changes15 are beyond changes that are recognized by the child’s
with the caregiver. He points to this the scope of this article, other aspects caregivers. It is not uncommon, how-
type D attachment pattern as one cause of biological change should be men- ever, to have a partially hidden or con-
for PTSD (see “The biology of early tioned. For example, Perry and col- fusing presentation, particularly where
trauma,” below). This may help to leagues 18 have considered how trau- a child has been repeatedly abused or the
VOL. 49 NO. 3, APRIL 2007 BC MEDICAL JOURNAL 135
Posttraumatic stress disorder in infants, toddlers, and preschoolers
entire history of the trauma is not • Complete play assessment of the
known. Terr has called PTSD the Once PTSD has been diagnosed, it will child, allowing the child to make use
preschoolers
“rheumatic fever” of child psychiatry,”19 depend on the practitioner’s level of of play objects and observing for spe-
and this refers to the fact that if not rec- comfort whether referral for further cific themes particularly related to
ognized and treated early on, the disorder specific assessment is required. If nec- the trauma. While this has been used
can have multiple manifestations later essary, referral can be made to a private extensively and written about in the
in life. These manifestations can include psychologist, psychiatrist, or other literature, it has been difficult to val-
a tendency toward affective, dissocia- infant mental health specialist, or to idate procedurally. Nonetheless, it is
tive, or personality disorders, substance the Infant Psychiatry Department at very helpful to see what a nonintru-
abuse, and conduct problems, to name a BC Children’s and Women’s Hospital sive play assessment can achieve.
few. Terr has described type I, type II, and specialized programs, such as the Generally, it is recommended that the
and crossover-type traumas in a land- Alan Cashmore Centre in Vancouver. caregiver(s) be present during the
mark paper. 19 While this information is Outside major urban areas, where refer- assessment.
not included in the DSM-IV, it is high- ral can take longer, it is important to • Consider medicolegal consequences.
ly useful when looking at survivors. assess the child as thoroughly as pos- The practitioner must maintain a
Type I represents a single-blow trauma, sible and to focus on safety and avoid- neutral, supportive stance that de-
such as a motor vehicle accident or a dog ance of retraumatization, whether acci- monstrates a willingness to listen
bite from which there is recovery. Type dental or otherwise, within the child’s and to observe whatever commun-
II refers to multiple and repeated trau- environment. In all cases, psychoedu- ications the child may offer. If
mas, such as covert sexual abuse by a cation should be provided, since it can the identity of a suspected abuser
relative. Terr notes that in type I trauma, be very effective when presented by a has never been revealed, questions
the memories are likely to be more fully trusted health professional, such as a mentioning the name or role of the
elaborated, with a tendency to ruminate family physician. suspected individual are clearly
over the details of the trauma, whereas Any assessment should include contraindicated. This also applies
type II can have spotty memories or the following steps: when you suspect witnessed trauma
some amnesia with aspects of denial, • Obtain a detailed history of the trau- (whereby the child was not the pri-
psychic numbing, dissociation, and ma with the nonoffending parent or mary target of the action).
even changes in pain tolerance. She caregiver present. This should in- Frequently, other conditions occur
refers to crossover-type traumas as clude associated events and any inter- along with trauma in this age group.
those involving a single incident with ventions undertaken to date. Some It is helpful, when possible, to delin-
long-lasting effects, such as an acci- interventions can be as traumatic as eate whether the symptoms are related
dent that results in permanent facial the initial event (e.g., hospital care to the trauma or whether they are pre-
scarring. involving surgery). existing diagnoses that may influence
The fact that there can be multiple • Obtain a simple verbal description how the trauma presents itself. Some
presentations over time, different from the child, depending on the diagnoses to consider are shown in
combinations of symptoms, and un - child’s age, emotional readiness, and Table 2 .
known or unreported trauma makes willingness.
diagnosing PTSD challenging. In addi- • Obtain a chronological history of all There are no specific studies regarding
Treatment of PTSD
tion, countertransference may signifi- new symptoms by asking clear ques-
cantly interfere with the therapist’s/ tions about whether these symp-
physician’s interpretation of symp- toms, even in milder forms, predat-
Table 2. Differential diagnoses to
toms. If the personal experience and ed the trauma.
consider during assessment of PTSD.
attitudes of the clinician are not care- • Determine the effect the trauma has
fully examined in difficult cases (e.g., had on attachment behaviors for the
Attention deficit hyperactivity disorders
with the help of a colleague), the clin- child and caregiver(s).
Phobias
ician may be more likely to overdiag- • Note the reaction of caregivers and
Attachment disorder
nose or, conversely, minimize a given consider individual treatment if
situation. needed, as parental and family func-
Complicated grief/bereavement
tioning are key predictors of out-
Depression
come. 20
Medical illness
Assessment of PTSD in
infants, toddlers, and
136 BC MEDICAL JOURNAL VOL. 49 NO. 3, APRIL 2007
Posttraumatic stress disorder in infants, toddlers, and preschoolers
treatment in this age group, but the ma, the therapist may need to shift become more complex. Psychoeduca-
following tenets are paramount: the focus to trust, bonding, and self- tion and intermittent sessions with
• Establish safety in the child’s life esteem-building through pleasant ac- caregivers can help children understand
and in the playroom. tivities. However, the child will still the generalization of fears. For exam-
• Help to decrease the intensity of need to re-experience parts of the trau- ple, a child who was bitten by one ani-
overwhelming affects. This involves ma in tolerable doses within an em- mal may suddenly be afraid of many
maintaining or beginning appropri- pathic setting. This key therapeutic animals.
ate soothing activities and routines principle has always been part of play
and assisting the caregiver to provide therapy, and is consistent with cogni-
these at the appropriate times. tive-behavioral therapy (CBT) strate- There are a few uncontrolled trials of
Medication
• Help the young child establish a gies as well, although classic CBT is medication use in children with PTSD.
coherent narrative of the trauma not widely applicable to treatment of In a study of clonidine, the agent was
using the child’s own terms, includ- the very young child. Even for very found to decrease hyperarousal symp-
ing art and play tools. This com- young children, some behavioral de- toms for several children. 21 Medication
monly involves play therapy and the sensitization can be appropriate. For for PTSD is at most an adjunct for
use of metaphor. Children who do example, the child might be gradually patients of any age, and in this age
not have or cannot access their feel- and gently exposed to a feared object, group in particular it is not a major
ings verbally can often react appro- such as a car seat after an accident or a feature of treatment. If medications are
priately to an injured animal in play room where a traumatic event occurred. used, specific symptoms need to be
through the use of figurines or pup- Caregivers should be informed that targeted. Following from this, of
pets. children may have more nightmares or course, the symptoms of comorbid
• Promote integration and mastery of re-enactment behaviors while the ther- conditions may need to be treated with
trauma. This can often be achieved apist is exploring the trauma and grad- medications, based on their severity,
through play therapy, whereby the ually titrating the child’s exposure to although the value of medications for
child acts out several roles, includ- materials and discussions related to the children with PTSD is at best unclear.
ing that of the survivor, the parent trauma. In fact, the caregiver may
(who may have been absent at the require treatment and desensitization
time of the trauma), the teacher, in order to support and comfort the For relatively asymptomatic children
Other considerations
the perpetrator, and perhaps other child during this stage of therapy. and parents, psychoeducation, screen-
helpers such as police officers or Throughout the process, it is impor- ing, and prevention awareness may be
paramedics. tant to monitor the caregiver’s reac- adequate as long as further assistance
• Address the “ripple” effects of trau- tions. Psychoeducation of family can be arranged as needed. Duration of
ma (e.g., negative behavior with members may involve helping them treatment will vary with the severity
other children at preschool and with recognize their own trauma and need and duration of the trauma, and to the
extended family). Help the family to for individual or group therapies (or individual characteristics of the child
understand and not punish the both). Marital difficulties, when rec- and family.
child’s new behaviors, which may ognized during treatment, should be In the special case of trauma com-
be oppositional or isolative. addressed. bined with grief, an individualized
• Support the family/caregivers. Reinforcement of the child and approach is required. Both Eth and
Prevention of PTSD is actually the caregiver’s adaptive behaviors is very Pynoos22 and Cohen and Mannarino23
first point in treatment. 19 Ideally, a safer important. This and focusing on the have specifically addressed this issue.
society would permit primary preven- positive can serve to remind the child There seems to be consensus that not
tion, but more commonly we see sec- and family of the things that they still all family losses constitute trauma per
ondary prevention occurring with soci- have in their lives. Children and care- se. In the cases where there is “trau-
ety’s early response to disasters, child givers who appear to be doing well matic grief” (e.g., after a child wit-
protection awareness at all levels, and should still be monitored for delayed nesses a sudden death) it is recom-
screening of large populations of trau- effects of trauma, as these have been mended that the trauma be dealt with
matized individuals, such as children documented. first so that the child will be able to
who have survived disasters. At more advanced developmental retrieve positive feelings and memo-
Depending on the severity of trau- levels, the cues that can trigger trauma ries of the deceased.
VOL. 49 NO. 3, APRIL 2007 BC MEDICAL JOURNAL 137
Posttraumatic stress disorder in infants, toddlers, and preschoolers
bites in children. J Pediatr 2004;144:121- New York: Basic Books; 1980.
Posttraumatic stress disorder undoubt-
Conclusions 122. 17. Boris NW, Zeanah CH; Work Group on
edly presents unique challenges in our
5. Freud A, Burlingham D. Infants without Quality Issues. Practice parameter for
youngest patients, especially in in-
Families (1943). In: Freud A. The Writings the assessment and treatment of chil-
fants and toddlers. We need to increase
of Anna Freud, Vol. 3. New York: Interna- dren and adolescents with reactive
awareness of this diagnosis in the pre-
tional Universities Press; 1967. attachment disorder of infancy and early
verbal and early verbal years, and to
6. Spitz RA. Hospitalism. Psychoanal Study childhood. J Am Acad Child Adolesc psy-
keep assessment and referral in mind.
Child 1945;1:53-74. chiatry 2005;44:1206-1219.
This awareness may also be needed
7. Levy D. Psychic trauma of operations in 18. Perry BD, Pollard RA, Blakely TL, et al.
when it comes to the children of an
children. Am J Dis Child 1945;69:7-25. Childhood trauma, the neurobiology of
adult patient being treated for PTSD
8. Terr L. Chowchilla revisited: The effects of adaptation, and “use-dependent” devel-
by a psychiatrist or therapist.
trauma four years after a school-bus kid- opment of the brain: How “states”
It should be remembered that
napping. Am J Psychiatry 1983;140:1543- become “traits.” Infant Ment Health J
DSM-IV criteria are often not sensitive
1550. 1995;16:271-291.
enough to diagnose PTSD, and that
9. Terr L. What happens to early memories 19. Terr L. Childhood traumas: An outline and
even in the adult population, individ-
of trauma? A study of twenty children overview. Am J Psychiatry 1991;148:10-
uals with partial criteria are still
under age five at the time of document- 20.
referred for therapy if their symptoms
ed traumatic events. J Am Acad Child 20. Scheeringa MS, Zeanah CH. A relational
are debilitating. This should apply to
Adolesc Psychiatry 1988;27:96-104. perspective on PTSD in early childhood.
very young children as well. Infants,
10. Drell MJ, Siegel C, Gaensbauer TJ. Post- J Trauma Stress 2001;14:799-815.
toddlers, and preschoolers can all ben-
traumatic stress disorder. In: Zeanah CH 21. Harmon RJ, Riggs PD. Clonidine for post-
efit from the treatments described here,
(ed). Handbook of Infant Mental Health. traumatic stress disorder in preschool
which can be adjusted to the many
New York: Guilford Press; 1993: 291-304. children. J Am Acad Child Adolesc Psy-
forms PTSD may take.
11. Diagnostic Classification, 0-3. Diagnostic chiatry 1996;35:1247-1249.
When evaluating and treating chil-
Classification of Mental Health and 22. Eth S, Pynoos RS. Interaction of trauma
dren with a diagnosis of PTSD, we
Developmental Disorders of Infancy and and grief in childhood. In: Eth S, Pynoos
must always see the disorder within an
Early Childhood. Arlington, VA: Zero To RS (eds). Post-traumatic Stress Disorder
attachment context and take into
Three/National Center for Clinical Infant in Children. Washington, DC: American
account the developmental capacities
Programs; 1994. 134 pp. Psychiatric Press; 1985. 186 pp.
of the child.
12. Scheeringa MS, Zeanah CH, Drell MJ, et 23. Cohen JA, Mannerino AP. Treating trau-
al. Two approaches to the diagnosis of matic grief in children and adolescents.
posttraumatic stress disorder in infancy Presented at the 17th Annual Conference
Competing interests and early childhood. J Am Acad Child Ado- on Child and Family Maltreatment, San
None declared. lesc Psychiatry 1995;34:191-200. Diego, CA, 3-7 February 2003.
Table 13. Scheeringa MS, Zeanah CH, Myers L, et
References al. New findings on alternative criteria for
1. Diagnostic and Statistical Manual of PTSD in preschool children. J Am Acad
Mental Disorders: DSM-IV-TR. Washing- Child Adolesc Psychiatry 2003;42:561-
ton, DC: American Psychiatric Associa- 570.
tion; 2000. 943 pp. 14. DC: 0-3R: Diagnostic Classification of
2. Hidalgo RB, Davidson RT. Posttraumatic Mental Health and Developmental Disor-
stress disorder: Epidemiology and ders of Infancy and Early Childhood.
health-related considerations. J Clin Psy- Washington, DC: Zero To Three Press;
chiatry 2000;61(suppl 7):5-13. 2005. 75 pp.
3. Breslau N. The epidemiology of posttrau- 15. Schore A. Dysregulation of the right brain:
matic stress disorder. What is the extent A fundamental mechanism of traumatic
of the problem? J Clin Psychiatry attachment and the psychopathogenesis
2001;62(suppl 17):16-22. of posttraumatic stress disorder. Aust N
4. Peters V, Sottiaux M, Appelboom J, et al. Z J Psychiatry 2002;36:9-30.
Posttraumatic stress disorder after dog 16. Bowlby J. Attachment and Loss. Vol. I.
138 BC MEDICAL JOURNAL VOL. 49 NO. 3, APRIL 2007
You might also like
- Kirschen2000 - The Royal London Space Planning - Part 1Document8 pagesKirschen2000 - The Royal London Space Planning - Part 1drgeorgejose7818100% (2)
- Childhood Traumas An Outline and Overview 1991 PDFDocument11 pagesChildhood Traumas An Outline and Overview 1991 PDFFrancisca AldunateNo ratings yet
- Din 50938 2000 2004Document5 pagesDin 50938 2000 2004Umer MuzammilNo ratings yet
- In Brief: Posttraumatic Stress DisorderDocument4 pagesIn Brief: Posttraumatic Stress DisorderDea PuspitaNo ratings yet
- Traumatic Events and Posttraumatic Stress in ChildhoodDocument8 pagesTraumatic Events and Posttraumatic Stress in ChildhoodcmdhanishNo ratings yet
- Risk Factors For Comorbid Psychopathology in Youth With Psychogenic Nonepileptic SeizuresDocument6 pagesRisk Factors For Comorbid Psychopathology in Youth With Psychogenic Nonepileptic SeizuresCecilia FRNo ratings yet
- 1010 4041 1 PBDocument3 pages1010 4041 1 PBblushing.lilithNo ratings yet
- Rao Chen 2009. DialoguesClinNeurosci-11-45Document18 pagesRao Chen 2009. DialoguesClinNeurosci-11-45Javiera Luna Marcel Zapata-SalazarNo ratings yet
- Depression in Children and Young People: Symposium: PsychiatryDocument8 pagesDepression in Children and Young People: Symposium: Psychiatry126 - Askandarnur riskisa PahleviNo ratings yet
- En V80n2sa05Document7 pagesEn V80n2sa05Imtiaz KhanNo ratings yet
- Metanalysis Prevalence PTDS PreeschoolDocument12 pagesMetanalysis Prevalence PTDS PreeschoolCesia Constanza Leiva GonzalezNo ratings yet
- NIH Public Access: Author ManuscriptDocument19 pagesNIH Public Access: Author ManuscriptIván CornuNo ratings yet
- Develpomental Trauma DisorderDocument9 pagesDevelpomental Trauma DisorderMariluzNo ratings yet
- Treating Childhood Traumatic Grief A Pilot StudyDocument9 pagesTreating Childhood Traumatic Grief A Pilot StudyAmanda PetinatiNo ratings yet
- Los Efectos Biológicos Del Trauma InfantilDocument39 pagesLos Efectos Biológicos Del Trauma InfantilFelipe Cáceres RiquelmeNo ratings yet
- Developmental Trauma Disorder Van Der Kolk 2005Document9 pagesDevelopmental Trauma Disorder Van Der Kolk 2005Sherina ChandraNo ratings yet
- Research Essay-RjDocument12 pagesResearch Essay-Rjapi-549236311No ratings yet
- Borderline and PTSDDocument11 pagesBorderline and PTSDContención Emocional CIASNo ratings yet
- Anxiety Disorders in Children and Adolescents Aetiology Diagnosis and TreatmentDocument10 pagesAnxiety Disorders in Children and Adolescents Aetiology Diagnosis and TreatmentCatalina Walker AlvarezNo ratings yet
- 2015 - Post-Traumatic Stress Disorder (Review)Document22 pages2015 - Post-Traumatic Stress Disorder (Review)Andrés Felipe SarmientoNo ratings yet
- Belindabombei,+5411 MAY JUNE 2021.v17 DepressionDocument8 pagesBelindabombei,+5411 MAY JUNE 2021.v17 DepressionBruno GonçalvesNo ratings yet
- The Role of Emotion Regulation As A Mediator Between Early Life Stress and Posttraumatic Stress Disorder, Depression and Anxiety in Syrian RefugeesDocument10 pagesThe Role of Emotion Regulation As A Mediator Between Early Life Stress and Posttraumatic Stress Disorder, Depression and Anxiety in Syrian RefugeesagathefuchsNo ratings yet
- HHS Public Access: Assessment and Treatment of Anxiety Disorders in Children and AdolescentsDocument19 pagesHHS Public Access: Assessment and Treatment of Anxiety Disorders in Children and Adolescentsayub01No ratings yet
- Annals Developmental TraumaDocument7 pagesAnnals Developmental TraumaMia Lawrence RuveNo ratings yet
- Clinical Significance of A Proposed Developmental Trauma Disorder Diagnosis - Results of An International Survey of Clinicians - 2020 11 09 232956Document14 pagesClinical Significance of A Proposed Developmental Trauma Disorder Diagnosis - Results of An International Survey of Clinicians - 2020 11 09 232956abelim01100% (1)
- Somatic Symptoms in Children and Adolescents With Anxiety DisordersDocument9 pagesSomatic Symptoms in Children and Adolescents With Anxiety DisordersDũng HồNo ratings yet
- 13.1 Undiagnosed or Diagnosed Mental Illness/complex Childhood trauma/PTSD Rachel Twelmeyer MDWF 3050 FALL 2020 Mel Smith-TourvilleDocument7 pages13.1 Undiagnosed or Diagnosed Mental Illness/complex Childhood trauma/PTSD Rachel Twelmeyer MDWF 3050 FALL 2020 Mel Smith-Tourvilleapi-384858632No ratings yet
- Negative Childhood Experiencies and Mental Health Theoretical Clinical and Prrimary Prevention ImplicationsDocument4 pagesNegative Childhood Experiencies and Mental Health Theoretical Clinical and Prrimary Prevention ImplicationsAnibal Silva Trabucco100% (1)
- WK 10 PTSD & TF-CBT Child Psychpath 2024 Tutorial HandoutsDocument24 pagesWK 10 PTSD & TF-CBT Child Psychpath 2024 Tutorial Handoutsisabellagallippi3No ratings yet
- 2020 Nemeroff - DeP ReviewDocument15 pages2020 Nemeroff - DeP Reviewnermal93No ratings yet
- Schore ANZJPDocument22 pagesSchore ANZJPGABRIEL PANDURO MUÑOZNo ratings yet
- Perinatal Psychiatric Disorders An OverviewDocument15 pagesPerinatal Psychiatric Disorders An OverviewZakkiyatus ZainiyahNo ratings yet
- Guided Imagery Treatment To BULIMIA NERVOSADocument17 pagesGuided Imagery Treatment To BULIMIA NERVOSAManoel SimaoNo ratings yet
- Pheonix Australia PTSD Guidelines - Children and AdolescentsDocument30 pagesPheonix Australia PTSD Guidelines - Children and AdolescentsMissDSKNo ratings yet
- No Health Without Perinatal Mental Health 2 MAGDocument2 pagesNo Health Without Perinatal Mental Health 2 MAGanadir1976No ratings yet
- Perinatal Psychiatric Disorders: An Overview: ObstetricsDocument15 pagesPerinatal Psychiatric Disorders: An Overview: ObstetricsAdolfoLaraRdzNo ratings yet
- Depresion en Adolescentes 2021 ReviewDocument5 pagesDepresion en Adolescentes 2021 ReviewDiana DuránNo ratings yet
- Postpartum Psychosis: Susan Hatters Friedman Eric Reed Nina E. RossDocument8 pagesPostpartum Psychosis: Susan Hatters Friedman Eric Reed Nina E. RossJesica MulyadiNo ratings yet
- 09 Art Originale Carmassi1Document7 pages09 Art Originale Carmassi1CongkrekNo ratings yet
- Egger Angold 2006emot Behav Problems in PreschoolerDocument25 pagesEgger Angold 2006emot Behav Problems in PreschoolerccarmogarciaNo ratings yet
- Towards A Cognitive-Behavioral Model of PTSD in Children and AdolescentsDocument16 pagesTowards A Cognitive-Behavioral Model of PTSD in Children and Adolescentsivanka milićNo ratings yet
- Major Depressive Disorder in Children and Adolescents: Sandra Mullen, Pharmd, BCPPDocument9 pagesMajor Depressive Disorder in Children and Adolescents: Sandra Mullen, Pharmd, BCPPbogdancoticaNo ratings yet
- Davydow 2010 Psychiatric MorbidityDocument9 pagesDavydow 2010 Psychiatric MorbidityAndrew EdisonNo ratings yet
- Extended Essay - PsychologyDocument18 pagesExtended Essay - PsychologymihquanNo ratings yet
- Depresi 8Document11 pagesDepresi 8Kenny KenNo ratings yet
- 01 Somatization Disorders in Children and AdolescentsDocument10 pages01 Somatization Disorders in Children and AdolescentsValeria Olarte ManjarresNo ratings yet
- Depression in Adolescence: SeminarDocument12 pagesDepression in Adolescence: SeminarRachman BocayNo ratings yet
- 3 PTSD and Childhood TraumaDocument5 pages3 PTSD and Childhood TraumaMarvellous MunhuwaNo ratings yet
- Anxiety-Disorders-In-Children-And-Adolescents 140867Document2 pagesAnxiety-Disorders-In-Children-And-Adolescents 140867api-261471301No ratings yet
- Neuropsychological Function in Children With Maltreatment-Related Posttraumatic Stress DisorderDocument8 pagesNeuropsychological Function in Children With Maltreatment-Related Posttraumatic Stress DisorderKen SimonNo ratings yet
- Assignment - 1 07062023 122711pmDocument5 pagesAssignment - 1 07062023 122711pmaz.rah.e.khudiNo ratings yet
- Prior Juvenile Diagnosis in Adults With Mental DisorderDocument9 pagesPrior Juvenile Diagnosis in Adults With Mental DisorderAdhya DubeyNo ratings yet
- Var WWW HTML Wp-Content Uploads 2021-02-16131 Postpartum-Mood-Disorders-Diagnosis-Treatment-GuidelinesDocument7 pagesVar WWW HTML Wp-Content Uploads 2021-02-16131 Postpartum-Mood-Disorders-Diagnosis-Treatment-GuidelinesDewi NofiantiNo ratings yet
- Anxiety Disorders in Children and Their FamiliesDocument8 pagesAnxiety Disorders in Children and Their FamiliesPablo Padilla SolanoNo ratings yet
- PTSD en Adolesc PDFDocument17 pagesPTSD en Adolesc PDFmarielaNo ratings yet
- Module 5 Handout 5.3 PDFDocument21 pagesModule 5 Handout 5.3 PDFAnonymous KOYPvPUNo ratings yet
- Vargas, L., Et Al. - Trastorno Obsesivo-Compulsivo en Niños y Adolescentes - Una Actualización. Segunda Parte.Document8 pagesVargas, L., Et Al. - Trastorno Obsesivo-Compulsivo en Niños y Adolescentes - Una Actualización. Segunda Parte.Isi SproveraNo ratings yet
- Development of A Group and Family-Based Cognitive Behavioural Therapy Program For Youth at Risk For PsychosisDocument11 pagesDevelopment of A Group and Family-Based Cognitive Behavioural Therapy Program For Youth at Risk For PsychosisAneliz VargasNo ratings yet
- Artículo Tema 4 Tratamiento para La Depresión en Niños y PreescolaresDocument5 pagesArtículo Tema 4 Tratamiento para La Depresión en Niños y PreescolaresMariaAn DominguezNo ratings yet
- Children Who Are Anxious in Silent - A Review of Selective MutismDocument19 pagesChildren Who Are Anxious in Silent - A Review of Selective MutismNicole WilliamsNo ratings yet
- 2018.02.08 Trauma and Stressor Related DisordersDocument38 pages2018.02.08 Trauma and Stressor Related DisordersErin RyanNo ratings yet
- Brain Healing and Trauma How Dark Psychology is Highly Effective in Treating Adult Survivors of Childhood AbuseFrom EverandBrain Healing and Trauma How Dark Psychology is Highly Effective in Treating Adult Survivors of Childhood AbuseRating: 3 out of 5 stars3/5 (1)
- Use of Cannabis in the Treatment of Post-Traumatic Stress DisorderFrom EverandUse of Cannabis in the Treatment of Post-Traumatic Stress DisorderNo ratings yet
- Perry 2006Document26 pagesPerry 2006Francisca AldunateNo ratings yet
- Jones2015 Translational Pyschiatry ConceptsDocument11 pagesJones2015 Translational Pyschiatry ConceptsFrancisca AldunateNo ratings yet
- Effect of Oral Iron Administration On Mental State in Children With Low Serum Ferritin ConcentrationDocument5 pagesEffect of Oral Iron Administration On Mental State in Children With Low Serum Ferritin ConcentrationFrancisca AldunateNo ratings yet
- Jun-13-SAHM VitaminD Position FinalDocument3 pagesJun-13-SAHM VitaminD Position FinalFrancisca AldunateNo ratings yet
- Issue Paper On COVID-19 and Fundamental Principles and Rights at WorkDocument38 pagesIssue Paper On COVID-19 and Fundamental Principles and Rights at WorkFrancisca AldunateNo ratings yet
- Irnmunoneuroendocrine Role of Melatonin: Mini-ReviewDocument10 pagesIrnmunoneuroendocrine Role of Melatonin: Mini-ReviewFrancisca AldunateNo ratings yet
- Melatonin As A Chronobiotic: Josephine Arendt, Debra Jean SkeneDocument15 pagesMelatonin As A Chronobiotic: Josephine Arendt, Debra Jean SkeneFrancisca AldunateNo ratings yet
- Hardeland 2005Document12 pagesHardeland 2005Francisca AldunateNo ratings yet
- 7 Melatonin: Clinical Relevance: Russel J. ReiterDocument13 pages7 Melatonin: Clinical Relevance: Russel J. ReiterFrancisca AldunateNo ratings yet
- Treating OCD in Children and Adolescents: A Cognitive-Behavioral Approach Martin E. Franklin, PH.DDocument49 pagesTreating OCD in Children and Adolescents: A Cognitive-Behavioral Approach Martin E. Franklin, PH.DFrancisca AldunateNo ratings yet
- Chanen Youth-SIG 15feb12Document40 pagesChanen Youth-SIG 15feb12Francisca AldunateNo ratings yet
- Alcohol Withdrawal Syndrome: Mechanisms, Manifestations, and ManagementDocument14 pagesAlcohol Withdrawal Syndrome: Mechanisms, Manifestations, and ManagementFrancisca AldunateNo ratings yet
- Arthropod Borne Infections - MHA (12 Files Merged)Document377 pagesArthropod Borne Infections - MHA (12 Files Merged)MariaNo ratings yet
- Personal Hygiene: How To Keep Your Body CleanDocument13 pagesPersonal Hygiene: How To Keep Your Body CleanneleaNo ratings yet
- ELSci Q2 Lesson 6 - Organ Systems of Representative AnimalsDocument51 pagesELSci Q2 Lesson 6 - Organ Systems of Representative AnimalsItsClarence100% (2)
- Minutes of Meeting Sept 2, 2022Document11 pagesMinutes of Meeting Sept 2, 2022roseannurakNo ratings yet
- Journal of Adolescence: Nele Laporte, Bart Soenens, Katrijn Brenning, Maarten VansteenkisteDocument17 pagesJournal of Adolescence: Nele Laporte, Bart Soenens, Katrijn Brenning, Maarten Vansteenkisterisa agustinaNo ratings yet
- 02 IVD-R Deep-Dive Deck NewDocument215 pages02 IVD-R Deep-Dive Deck Newrajiveacharya100% (1)
- Technical Data BCC 1250P-50 BCC 1400S-50: 50 Hz Cos Φ = 0.8 3-PhaseDocument3 pagesTechnical Data BCC 1250P-50 BCC 1400S-50: 50 Hz Cos Φ = 0.8 3-PhaseHectrateNo ratings yet
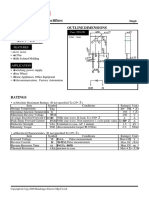
- Shindengen: Super Fast Recovery RectifiersDocument7 pagesShindengen: Super Fast Recovery Rectifiersjoroma58No ratings yet
- PARTY ROCKER ONE ManualDocument80 pagesPARTY ROCKER ONE ManualJustino BalancaNo ratings yet
- Literature Synopsis:: Brain-Based LearningDocument7 pagesLiterature Synopsis:: Brain-Based LearningJega SkyNo ratings yet
- Sheep Diseases - The Farmers Guide - 2nd Edition - July 2015Document84 pagesSheep Diseases - The Farmers Guide - 2nd Edition - July 2015Raghu NathaNo ratings yet
- Duke Plasto Technique PVTDocument25 pagesDuke Plasto Technique PVTVishnu Suthar100% (2)
- (19330693 - Journal of Neurosurgery) Estimating The Global Incidence of Traumatic Brain InjuryDocument18 pages(19330693 - Journal of Neurosurgery) Estimating The Global Incidence of Traumatic Brain InjuryIqra AlghifarihNo ratings yet
- Therbligs Are 18 Kinds of Elemental Motions Used in The Study of Motion Economy in The WorkplaceDocument2 pagesTherbligs Are 18 Kinds of Elemental Motions Used in The Study of Motion Economy in The WorkplaceManonmani Mani100% (2)
- Fruit Serving Calculation PureesDocument2 pagesFruit Serving Calculation PureesRuben ViegasNo ratings yet
- Quiz Chapter 2 3Document25 pagesQuiz Chapter 2 3THỊNH DƯƠNG GIANo ratings yet
- RG1 166Document8 pagesRG1 166tugceceran90No ratings yet
- The Role of Public Health Leadership (2) FinalDocument20 pagesThe Role of Public Health Leadership (2) FinalKing Mugitah18No ratings yet
- Sexuality Research in India An UpdateDocument5 pagesSexuality Research in India An UpdatekavalapparaNo ratings yet
- Basics of PLA - Bioplastics MAGAZINEDocument3 pagesBasics of PLA - Bioplastics MAGAZINEIsadora HenriquesNo ratings yet
- Average Average Set Ii Set I SampleDocument1 pageAverage Average Set Ii Set I Samplevenkateswara rao PothinaNo ratings yet
- Basics of HFFR ExtrusionDocument7 pagesBasics of HFFR ExtrusionYiğit IlgazNo ratings yet
- 7 - 1 - The - MoleDocument17 pages7 - 1 - The - Molenaziya begumNo ratings yet
- Quality Management Principles For Excellence: by - Sacchidanand Gogawale, Zen International SystemsDocument5 pagesQuality Management Principles For Excellence: by - Sacchidanand Gogawale, Zen International SystemsSanjeevani GogawaleNo ratings yet
- Riser Clamps SpecificationDocument36 pagesRiser Clamps SpecificationasaiNo ratings yet
- Diagnosisofmyasthenia Gravis: Mamatha Pasnoor,, Mazen M. Dimachkie,, Constantine Farmakidis,, Richard J. BarohnDocument14 pagesDiagnosisofmyasthenia Gravis: Mamatha Pasnoor,, Mazen M. Dimachkie,, Constantine Farmakidis,, Richard J. BarohnLilisNo ratings yet
- Drug Calculations Reviewer For NursesDocument6 pagesDrug Calculations Reviewer For NursesBreezy ReveloNo ratings yet
- Guptautkarsh@dsnlu Ac inDocument2 pagesGuptautkarsh@dsnlu Ac inUTKARSH GUPTANo ratings yet