Professional Documents
Culture Documents
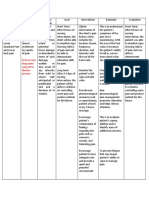
Subjective Cues: Short Term Goal: Short Term Goal
Subjective Cues: Short Term Goal: Short Term Goal
Uploaded by
Larr Sumalpong0 ratings0% found this document useful (0 votes)
26 views4 pagesThe nursing care plan is for an 8-year-old patient named Therese experiencing acute pain related to muscle spasms. The short term goals are for the patient to verbalize pain at a level less than 3-4 on a scale of 0-10 and display improved vital signs and muscle tone after 8 hours. The long term goal is for the patient to use pharmacological and nonpharmacological pain relief strategies after a month. The plan includes interventions like assessing pain level, immobilizing the affected area, explaining procedures, monitoring vital signs, providing comfort measures, exercises, and relaxation techniques to help meet these goals.
Original Description:
Original Title
NCPPPP
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe nursing care plan is for an 8-year-old patient named Therese experiencing acute pain related to muscle spasms. The short term goals are for the patient to verbalize pain at a level less than 3-4 on a scale of 0-10 and display improved vital signs and muscle tone after 8 hours. The long term goal is for the patient to use pharmacological and nonpharmacological pain relief strategies after a month. The plan includes interventions like assessing pain level, immobilizing the affected area, explaining procedures, monitoring vital signs, providing comfort measures, exercises, and relaxation techniques to help meet these goals.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
26 views4 pagesSubjective Cues: Short Term Goal: Short Term Goal
Subjective Cues: Short Term Goal: Short Term Goal
Uploaded by
Larr SumalpongThe nursing care plan is for an 8-year-old patient named Therese experiencing acute pain related to muscle spasms. The short term goals are for the patient to verbalize pain at a level less than 3-4 on a scale of 0-10 and display improved vital signs and muscle tone after 8 hours. The long term goal is for the patient to use pharmacological and nonpharmacological pain relief strategies after a month. The plan includes interventions like assessing pain level, immobilizing the affected area, explaining procedures, monitoring vital signs, providing comfort measures, exercises, and relaxation techniques to help meet these goals.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 4
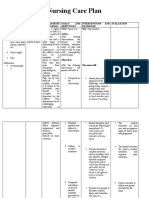
STUDENT NURSE’S NAME: L.
SUMALPONGFSUUSN Date: February 22, 2021
Client’s Name: Therese Age: 8-year-old
NURSING CARE PLAN
ASSESSMENT NURSING DIAGNOSIS PLANNING INTERVENTIONS EVALUATION
Subjective cues: Acute pain related to muscle spasms Short term Goal: 1. Assess and record the patient’s Short term Goal:
as evidenced by expression of pain After 8 hours of nursing level of pain utilizing pain intensity After 8 hours of nursing
through crying. interventions the patient will: rating scale including Wong Baker interventions the patient is able to:
Objectives cues: FACES pain rating scale, visual
Crying -Verbalize pain at a level less than 3 analog scale, and FLACC scale. Note -Verbalize pain at a level less than 3
to 4 on a rating scale of 0 to 10. relieving and aggravating factors, to 4 on a rating scale of 0 to 10.
and nonverbal pain cues such as
-Display improved well-being such changes in vital signs, emotions, and-Display improved well-being such
as baseline levels for pulse, BP, behavior. as baseline levels for pulse, BP,
respirations, and relaxed muscle respirations, and relaxed muscle
tone or body posture. Rationale: Influences the tone or body posture.
effectiveness of interventions. Many
factors, including the level of
Long term Goal: anxiety, may affect the perception Long term Goal:
After a month of nursing of pain. After a month of nursing
interventions the patient will: interventions the patient is able to:
-Use pharmacological and 2. Maintain immobilization of -Use pharmacological and
nonpharmacological pain-relief affected part by means of bed rest, nonpharmacological pain-relief
strategies. cast, splint, traction. strategies.
Rationale: Relieves pain and
prevents bone displacement and
extension of tissue injury.
3. Evaluate pain regularly (every 2
hrs. noting characteristics, location,
and intensity. Emphasize patient’s
responsibility for reporting pain/
relief of pain completely.
Rationale: Provides information
about need for or effectiveness of
interventions. Note: It may not
always be possible to eliminate
pain; however, analgesics should
reduce pain to a tolerable level.
4. Explain procedures before
beginning them.
Rationale: Allows patient to prepare
mentally for activity and to
participate in controlling the level of
discomfort.
5. Assess vital signs, noting
tachycardia, hypertension, and
increased respiration, even if
patient denies pain.
Rationale: Changes in these vital
signs often indicate acute pain and
discomfort. Note: Some patients
may have a slightly lowered BP,
which returns to normal range after
pain relief is achieved.
6. Assess causes of possible
discomfort other than operative
procedure.
Rationale: Discomfort can be caused
or aggravated by presence of non-
patent indwelling catheters and
tubes.
7. Provide additional comfort
measures: backrub, heat or cold
applications.
Rationale: Improves circulation,
reduces muscle tension and anxiety
associated with pain. Enhances
sense of well-being.
8. Perform and supervise active and
passive ROM exercises.
Rationale: Maintains strength and
mobility of unaffected muscles and
facilitates resolution of
inflammation in injured tissues.
9. Encourage use of relaxation
techniques: deep-breathing
exercises, guided imagery,
visualization, music.
Rationale: Relieves muscle and
emotional tension; enhances sense
of control and may improve coping
abilities.
10. Evaluate the patient’s response
to pain and management strategies.
Rationale: It is essential to assist
patients to express as factually as
possible (i.e., without the effect of
mood, emotion, or anxiety) the
effect of pain relief measures.
You might also like
- A Detailed Lesson Plan in Mathematics 3 Q3Document5 pagesA Detailed Lesson Plan in Mathematics 3 Q3Lordiel Miasco94% (18)
- Nursing Care Plan Post Op & Intra OpDocument2 pagesNursing Care Plan Post Op & Intra OpLei Ortega85% (48)
- Septic Arthritis NCPDocument3 pagesSeptic Arthritis NCPMae Therese B. MAGNO0% (1)
- 4999EDN: The Griffith Education Internship Professional Learning PlanDocument7 pages4999EDN: The Griffith Education Internship Professional Learning Planapi-469331794No ratings yet
- Whistle and I'Ll Come To You. Susan Hill: For Edexcel IgcseDocument7 pagesWhistle and I'Ll Come To You. Susan Hill: For Edexcel IgcseMariam AlgaoudNo ratings yet
- NCP For ChronicPain PDFDocument2 pagesNCP For ChronicPain PDFjay kusainNo ratings yet
- UntitledDocument5 pagesUntitledJayelles Dixien JuguilonNo ratings yet
- Heart Clinic: Alternative Learning System Related Learning ExperienceDocument8 pagesHeart Clinic: Alternative Learning System Related Learning ExperienceEdson John DemayoNo ratings yet
- Brain Surgery Post Op NCPDocument6 pagesBrain Surgery Post Op NCPunnamed personNo ratings yet
- Patient NCPDocument8 pagesPatient NCPlouie john abilaNo ratings yet
- "Naga Pan Luya Lang Ang Lawas Ko"as Verbalized by The PatientDocument3 pages"Naga Pan Luya Lang Ang Lawas Ko"as Verbalized by The PatientJamie Grace AbitNo ratings yet
- No Diagnose Liver Cancer NOC NIC Nutrition Imbalance Less Body Requirements Nutrition ManagementDocument2 pagesNo Diagnose Liver Cancer NOC NIC Nutrition Imbalance Less Body Requirements Nutrition ManagementBobbye MardaNo ratings yet
- Manguiat, Ncma 111 RomeoDocument4 pagesManguiat, Ncma 111 RomeoCiara ManguiatNo ratings yet
- Group 9 Sickle Cell Anemia Case Study ActivityDocument4 pagesGroup 9 Sickle Cell Anemia Case Study ActivityJuliaNo ratings yet
- Nursing Care Plan: Western Mindanao State University College of NursingDocument11 pagesNursing Care Plan: Western Mindanao State University College of NursingPatricia VasquezNo ratings yet
- Epidemiology and Definition: o Most Common Locations: o Acute PainDocument4 pagesEpidemiology and Definition: o Most Common Locations: o Acute PainJudy Ignacio EclarinoNo ratings yet
- Ns3a NCP and Drug StudyDocument9 pagesNs3a NCP and Drug StudyANNAMA3 SELMERNo ratings yet
- NCP FractureDocument7 pagesNCP FractureMacris BondocNo ratings yet
- NCP 2BCDocument6 pagesNCP 2BCPMG BrightNo ratings yet
- NCP Charm EditedDocument6 pagesNCP Charm EditedampogeNo ratings yet
- NPC5Document3 pagesNPC5Ahmed Mohammed SalamaNo ratings yet
- Nursing Care Plan 1Document2 pagesNursing Care Plan 1Justine Jean GuillermoNo ratings yet
- Care PlanDocument2 pagesCare PlanAnonymous 9QBCcNNo ratings yet
- NCP4Document4 pagesNCP4Noreen GyleNo ratings yet
- Disorders NCPDocument7 pagesDisorders NCPFaye Dianne Damian-BuenafeNo ratings yet
- Acute Pain TonsilitisncpDocument2 pagesAcute Pain Tonsilitisncpjustinekaye diongsonNo ratings yet
- No Data Problem Etiology Diagnosis: 1.pain Control 1. Pain ManagementDocument6 pagesNo Data Problem Etiology Diagnosis: 1.pain Control 1. Pain ManagementArjuna AnggaraNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanWinter SpringNo ratings yet
- Assessment Nursing Diagnosis Planning Interventions Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Planning Interventions Rationale EvaluationYamete KudasaiNo ratings yet
- "I Don't Have An Infection in My Gallbladder Which Is Good, But I Do Feel The Pain," As Verbalized by TheDocument2 pages"I Don't Have An Infection in My Gallbladder Which Is Good, But I Do Feel The Pain," As Verbalized by Theunnamed person100% (1)
- Di Ko To Sure Kung Tama Yung Rel To Disease ProcessDocument8 pagesDi Ko To Sure Kung Tama Yung Rel To Disease ProcessNyeam NyeamNo ratings yet
- JoeoeoeoeDocument31 pagesJoeoeoeoeBSRT1A BERBANO, IAN JEWEL M.No ratings yet
- Nursing Care Plan Preoperative Cues Nursing Diagnosis Objectives Nursing Interventions Rationale Evaluation SubjectiveDocument5 pagesNursing Care Plan Preoperative Cues Nursing Diagnosis Objectives Nursing Interventions Rationale Evaluation SubjectiveShamsa AfdalNo ratings yet
- Pleural EffusionDocument5 pagesPleural EffusionTerizla MobileNo ratings yet
- NCP Post OpDocument4 pagesNCP Post OpNIKKI CARYL ZAFRANo ratings yet
- Nursing Care Plan: Assessment Nursing Diagnosis Planning Nursing Interventi ON Rationale EvaluationDocument2 pagesNursing Care Plan: Assessment Nursing Diagnosis Planning Nursing Interventi ON Rationale EvaluationRaidis PangilinanNo ratings yet
- NCP - GeriaDocument4 pagesNCP - GeriaMarielle J GarciaNo ratings yet
- Nursing Care Plan - Cesarean SectionDocument1 pageNursing Care Plan - Cesarean SectionMarceline VueenNo ratings yet
- General Santos Doctors' Medical School Foundation Inc. NCM: Rle ExposureDocument3 pagesGeneral Santos Doctors' Medical School Foundation Inc. NCM: Rle ExposureEloisa Joy MaquidatoNo ratings yet
- Kusain - NCP in NCM 112 RleDocument2 pagesKusain - NCP in NCM 112 Rlejay kusainNo ratings yet
- Acute PainDocument2 pagesAcute PainNicole Genevie MallariNo ratings yet
- Rafin NCP and Drug StudyDocument7 pagesRafin NCP and Drug StudyCezanne CruzNo ratings yet
- NCP Drug Study, Ojoy Dan Joshua LDocument2 pagesNCP Drug Study, Ojoy Dan Joshua Ldan.ojoy18No ratings yet
- NCP3Document3 pagesNCP3Hanniel MontecalboNo ratings yet
- Effectiveness of Jacobson's Progressive Muscle Relaxation Technique For Pain Management in Post-Cesaerean WomenDocument5 pagesEffectiveness of Jacobson's Progressive Muscle Relaxation Technique For Pain Management in Post-Cesaerean Womennur aisahNo ratings yet
- Mga NCP For Preterm Birth Case 2Document9 pagesMga NCP For Preterm Birth Case 2John Rendel LopezNo ratings yet
- Andrian Dwi Herlambang (P17230181001) Acute PainDocument8 pagesAndrian Dwi Herlambang (P17230181001) Acute PainAndrian TakigawaNo ratings yet
- Sleep Deprivation Case PresDocument2 pagesSleep Deprivation Case Presjustinekaye diongsonNo ratings yet
- NCP Format 1Document4 pagesNCP Format 1Kylle AlimosaNo ratings yet
- Flank Pain, Anxiety...Document7 pagesFlank Pain, Anxiety...reneighdNo ratings yet
- Appendicitis - NCPDocument5 pagesAppendicitis - NCPEarl Joseph Deza100% (1)
- Appendicitis NCPDocument5 pagesAppendicitis NCPEarl Joseph DezaNo ratings yet
- NCPDocument6 pagesNCPKrishna Faith P. DelaraNo ratings yet
- Nursing Care Plan PainDocument2 pagesNursing Care Plan Painjanmarc goreroNo ratings yet
- Actual NCP Pt.Document2 pagesActual NCP Pt.Kate WeyganNo ratings yet
- Cholecystectomy Nursing Care PlanDocument1 pageCholecystectomy Nursing Care PlanJor Garcia100% (1)
- Subjective Data: Independent AssessDocument5 pagesSubjective Data: Independent AssessLadybelle GototosNo ratings yet
- Nursing Care Plan For Patient With PNEUMONIA (Geriatrics)Document4 pagesNursing Care Plan For Patient With PNEUMONIA (Geriatrics)CHRISTIE MONTANO0% (1)
- CaseDocument3 pagesCasebLessy_july16No ratings yet
- NCP Acute Pain RT CancerDocument3 pagesNCP Acute Pain RT CancerCharissa Magistrado De LeonNo ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Intervention Rationale Evaluation IndeoendentDocument3 pagesAssessment Nursing Diagnosis Scientific Explanation Planning Intervention Rationale Evaluation IndeoendentDiane Sarino CabonceNo ratings yet
- Assessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsFrom EverandAssessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsNo ratings yet
- Name: - Caring For A Patient On Isolation PrecautionDocument5 pagesName: - Caring For A Patient On Isolation PrecautionLarr SumalpongNo ratings yet
- Placenta Previa: The Exact Cause of Placenta Previa Is UnknownDocument3 pagesPlacenta Previa: The Exact Cause of Placenta Previa Is UnknownLarr SumalpongNo ratings yet
- Physical AssessmentDocument5 pagesPhysical AssessmentLarr SumalpongNo ratings yet
- The Following Questions Apply To The Scenario GivenDocument3 pagesThe Following Questions Apply To The Scenario GivenLarr SumalpongNo ratings yet
- There Are Three Elements Needed To Make A ManDocument1 pageThere Are Three Elements Needed To Make A ManLarr SumalpongNo ratings yet
- Part 1Document1 pagePart 1Larr SumalpongNo ratings yet
- The Health Belief Model Is A Theoretical Framework For Guiding Health Promotion and Disease Prevention Measures in Public HealthDocument3 pagesThe Health Belief Model Is A Theoretical Framework For Guiding Health Promotion and Disease Prevention Measures in Public HealthLarr SumalpongNo ratings yet
- Ukraine FinalDocument62 pagesUkraine FinalLarr SumalpongNo ratings yet
- Heliyon: Research ArticleDocument8 pagesHeliyon: Research ArticleLarr SumalpongNo ratings yet
- Inflation Differentials Between Austria, The Euro Area, Germany and ItalyDocument12 pagesInflation Differentials Between Austria, The Euro Area, Germany and ItalyLarr SumalpongNo ratings yet
- Framework Health-Generating: A For Prevention: ToDocument5 pagesFramework Health-Generating: A For Prevention: ToLarr SumalpongNo ratings yet
- Philippines FinalDocument36 pagesPhilippines FinalLarr SumalpongNo ratings yet
- Drug Study FormatDocument2 pagesDrug Study FormatLarr SumalpongNo ratings yet
- INFLATION ANALYSIS Macroeconomics Final 1Document2 pagesINFLATION ANALYSIS Macroeconomics Final 1Larr SumalpongNo ratings yet
- Activity Design MakinsgDocument5 pagesActivity Design MakinsgLarr SumalpongNo ratings yet
- Letter of Rec - Heidi RodriguezDocument1 pageLetter of Rec - Heidi Rodriguezapi-498791344No ratings yet
- Year 1 Civic Lesson Plan (August-Happiness) : By:MrapolDocument1 pageYear 1 Civic Lesson Plan (August-Happiness) : By:Mrapolsaifulefpandi7761No ratings yet
- Enterprise Resource Planning For Police DepartmentDocument27 pagesEnterprise Resource Planning For Police DepartmentAnshika ChaudharyNo ratings yet
- DLL - English 6 - Q2 - W9Document4 pagesDLL - English 6 - Q2 - W9Rolando Ogerio AtaNo ratings yet
- Dept Tests Results Eot Code 141 Results Held On December 2011Document252 pagesDept Tests Results Eot Code 141 Results Held On December 2011rmdirfantvNo ratings yet
- PerceptionDocument6 pagesPerceptionRohit Kumar100% (4)
- Grading Sheet - GRADE-7-10-TLEDocument21 pagesGrading Sheet - GRADE-7-10-TLEAyn RealosaNo ratings yet
- NCM 117 - Nurse Patient Interaction - April 2021Document58 pagesNCM 117 - Nurse Patient Interaction - April 2021kimberly dedaseNo ratings yet
- Sample Grant ProposalDocument16 pagesSample Grant ProposalSaundra100% (1)
- MODULE 6. Developmental Reading Topic 6. Comprehension - Theories and StrategiesDocument11 pagesMODULE 6. Developmental Reading Topic 6. Comprehension - Theories and StrategiesBeverly Panganiban CadacioNo ratings yet
- Long Quiz in Oral CommunicationDocument1 pageLong Quiz in Oral CommunicationMichelle MicheleNo ratings yet
- Weekly Accomplishment Report Date / Week Duration: April 18-22, 2022Document3 pagesWeekly Accomplishment Report Date / Week Duration: April 18-22, 2022Joana NavaresNo ratings yet
- Unsupervised Feature Extraction With Autoencoders For EEG Based Multiclass Motor Imagery BCIDocument10 pagesUnsupervised Feature Extraction With Autoencoders For EEG Based Multiclass Motor Imagery BCIforooz davoodzadehNo ratings yet
- Outside Sales Resume ExamplesDocument6 pagesOutside Sales Resume Examplesafdnarfmi100% (1)
- Unit 2 Essay Writing - Comparison and Contrast What ISA Comparison Essay?Document12 pagesUnit 2 Essay Writing - Comparison and Contrast What ISA Comparison Essay?Yu LiuNo ratings yet
- 1thesis Statement AnthroDocument3 pages1thesis Statement AnthroanaspirantNo ratings yet
- Equivalent Record Form: Republic of The Philippines Department of Education Region Vi - Western Visayas Division of CapizDocument1 pageEquivalent Record Form: Republic of The Philippines Department of Education Region Vi - Western Visayas Division of CapizJL D. Busia100% (1)
- 北京英语中考 2021Document11 pages北京英语中考 2021Yuanyuan MaNo ratings yet
- Detailed Lesson Plan (DLP) Format: Objectives: NowledgeDocument2 pagesDetailed Lesson Plan (DLP) Format: Objectives: NowledgeRed Zye UbayNo ratings yet
- Coaching Questions: Types of Helpful QuestionsDocument3 pagesCoaching Questions: Types of Helpful QuestionsDebora TorresNo ratings yet
- MM 01 Handout 5 Marketing ResearchDocument12 pagesMM 01 Handout 5 Marketing ResearchAsset DyNo ratings yet
- Transcriptional and Translational Regulation of Stem Cells BookDocument370 pagesTranscriptional and Translational Regulation of Stem Cells BookMaria Del Mar RoblesNo ratings yet
- Project Charter Template.2019Document10 pagesProject Charter Template.2019沈悦双No ratings yet
- Practical Research I: Quarter 4: Week 3 & 4 Module 2: Research MethodologyDocument21 pagesPractical Research I: Quarter 4: Week 3 & 4 Module 2: Research MethodologyCarlyne Guiang FijerNo ratings yet
- Lbes-Deped FilesDocument47 pagesLbes-Deped FilesKaraoke SongsNo ratings yet
- Assertion ReasonDocument3 pagesAssertion Reasonananya thakurNo ratings yet