Professional Documents
Culture Documents
EMPHYSEMA
EMPHYSEMA
Uploaded by
Jerick DaangCopyright:
Available Formats
You might also like
- Renaissance Woman: Fat Loss, Muscle Growth & Performance Through Scientific EatingDocument20 pagesRenaissance Woman: Fat Loss, Muscle Growth & Performance Through Scientific EatingBenedict Ray Andhika33% (3)
- Obstructive Disease of Lung and Physiotherapy ManagementDocument76 pagesObstructive Disease of Lung and Physiotherapy Managementphysio43100% (1)
- List of Documents NBA PfilesDocument48 pagesList of Documents NBA PfilesDr. A. Pathanjali Sastri100% (1)
- Remembering, Bartlett (1932)Document11 pagesRemembering, Bartlett (1932)andreea4etc100% (1)
- Emphysema Is A LongDocument54 pagesEmphysema Is A LongryemoralesNo ratings yet
- CopdDocument4 pagesCopdapi-3739910100% (2)
- CR Patho SummaryDocument22 pagesCR Patho SummaryDNAANo ratings yet
- EmphysemaDocument27 pagesEmphysemaDiana Laura LeiNo ratings yet
- COPDDocument18 pagesCOPDMae CalicaNo ratings yet
- Emphysema Fall 2019Document3 pagesEmphysema Fall 2019Mary MarshNo ratings yet
- Asthma and The COPDsDocument133 pagesAsthma and The COPDsShania robertsNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument12 pagesChronic Obstructive Pulmonary Diseasejisoo100% (1)
- Chronic Obstructive Pulmonary DiseaseDocument10 pagesChronic Obstructive Pulmonary DiseaseZinya RobinsonNo ratings yet
- Emphysema A D A7Document13 pagesEmphysema A D A7Ahmed DsoukiNo ratings yet
- Textbuk DiscussionDocument5 pagesTextbuk Discussionapi-3717941No ratings yet
- Oxygenation NotesDocument23 pagesOxygenation NoteschikaycNo ratings yet
- Copd 200412082048Document139 pagesCopd 200412082048Richard ArceNo ratings yet
- EmphysemaDocument2 pagesEmphysemaapi-322389115No ratings yet
- Breathlessness EdittedDocument2 pagesBreathlessness EdittedSalwani MohamedNo ratings yet
- Resp Objectives Adn 253Document4 pagesResp Objectives Adn 253christian_zarate_2No ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument12 pagesChronic Obstructive Pulmonary DiseaseibegbunamchinemeremNo ratings yet
- Obstructive DisordersDocument23 pagesObstructive DisordersMartha ChaseNo ratings yet
- COPDDocument7 pagesCOPDarminmercado7406No ratings yet
- Patholpgic Change in EmphysemiaDocument16 pagesPatholpgic Change in Emphysemiafenil1194No ratings yet
- Onchi & CopdDocument8 pagesOnchi & CopdAngellene GraceNo ratings yet
- CopdDocument30 pagesCopdsalmanhabeebekNo ratings yet
- Normal Changes of AgingDocument9 pagesNormal Changes of AgingGiselle EstoquiaNo ratings yet
- Nursing Care Management - 112Document67 pagesNursing Care Management - 112Ong KarlNo ratings yet
- Copd CaseDocument36 pagesCopd Casejho_No ratings yet
- Dyspnea Is An Uncomfortable Abnormal Awareness of Breathing. A Number of DifferentDocument4 pagesDyspnea Is An Uncomfortable Abnormal Awareness of Breathing. A Number of DifferentSita SifanaNo ratings yet
- Pathophysiology of EmphysemaDocument3 pagesPathophysiology of EmphysemaApple Maiquez Garcia100% (1)
- Pathophysiology of COPD: Heart Failure Respiratory DisordersDocument5 pagesPathophysiology of COPD: Heart Failure Respiratory DisordersKath DeguzmanNo ratings yet
- The Respiratory SystemDocument8 pagesThe Respiratory SystemJane Rose SuperadaNo ratings yet
- NCLEX Review NotesDocument36 pagesNCLEX Review NotesKyla Patricia RibanoNo ratings yet
- Obstructive Airway DiseasesDocument56 pagesObstructive Airway Diseaseskalanakariyawasam99No ratings yet
- Respiratory SystemDocument85 pagesRespiratory SystemDr:-Ustaad Aakass Ahmed Junejo SahabNo ratings yet
- Case Study For EmphysemaDocument5 pagesCase Study For EmphysemaGabbii CincoNo ratings yet
- (Respi) Lo Week 2 Tutorial 1Document10 pages(Respi) Lo Week 2 Tutorial 1KintanNo ratings yet
- Oxygenation and Airway Management: Quick LookDocument24 pagesOxygenation and Airway Management: Quick LookNining Komala SariNo ratings yet
- Emphysema Chronic Obstructive Pulmonary Disease (COPD) : Call Dasco Today For More Information 855-442-7912Document6 pagesEmphysema Chronic Obstructive Pulmonary Disease (COPD) : Call Dasco Today For More Information 855-442-7912Nazif Aiman IsmailNo ratings yet
- Acute Respiratory Failure-PRINTDocument5 pagesAcute Respiratory Failure-PRINTJan SicatNo ratings yet
- Adult - RespiratoryDocument14 pagesAdult - RespiratoryahmeddorostyNo ratings yet
- Systems Plus College Foundation Macarthur Highway, Balibago, Angeles CityDocument13 pagesSystems Plus College Foundation Macarthur Highway, Balibago, Angeles CityLeanne Princess GamboaNo ratings yet
- Bronchial Obstruction: Presenter Andrea Fagan 3 Year Student NurseDocument27 pagesBronchial Obstruction: Presenter Andrea Fagan 3 Year Student NurseAndrea FaganNo ratings yet
- COPD Treatment and ManagementDocument3 pagesCOPD Treatment and ManagementHydie Mae AlcabedosNo ratings yet
- Patho Exam 3: Deficiency in Alpha-1-Antitrypsin-Unchecked Elastase Destruction of The AlveoliDocument5 pagesPatho Exam 3: Deficiency in Alpha-1-Antitrypsin-Unchecked Elastase Destruction of The AlveoliTaran LuthraNo ratings yet
- Reviewer For Management of Common IllnessDocument27 pagesReviewer For Management of Common Illnessmarie vennis hamchawanNo ratings yet
- Epidemiology: Several Diseases Airflow ObstructionDocument11 pagesEpidemiology: Several Diseases Airflow ObstructionBharat Singh BanshiwalNo ratings yet
- Dr. Kamran - S PBLDocument12 pagesDr. Kamran - S PBLTaimoor Ul HassanNo ratings yet
- CopdDocument60 pagesCopdRizqy Shofianingrum100% (1)
- COPDDocument30 pagesCOPDAmila SirisingheNo ratings yet
- Pulmonary PathologyDocument46 pagesPulmonary PathologyMuostafa KamelNo ratings yet
- Day 5 Respiratory DiseaseDocument71 pagesDay 5 Respiratory DiseaseRamzen Raphael DomingoNo ratings yet
- COPD & RLDDocument17 pagesCOPD & RLDhis.thunder122No ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument4 pagesChronic Obstructive Pulmonary DiseaseSeraphina SolanNo ratings yet
- LP Dyspnea RevisiDocument12 pagesLP Dyspnea RevisiInsaniNo ratings yet
- EmphysemaDocument3 pagesEmphysemaKhalid Mahmud ArifinNo ratings yet
- Essay EmphysemaDocument6 pagesEssay EmphysemaChristopher EstevezNo ratings yet
- DR Ambreen Shams NephrologistDocument58 pagesDR Ambreen Shams NephrologistAamer NaeemNo ratings yet
- Interstitial Lung DiseaseDocument14 pagesInterstitial Lung DiseaseAzkaZulfiqarNo ratings yet
- Physical Rehabilitation For Asthmatic PatientsDocument54 pagesPhysical Rehabilitation For Asthmatic PatientsIjeoma Okpalla60% (5)
- Atelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesFrom EverandAtelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesNo ratings yet
- The Entrepreneurial and Entrepreneurial Mind: Week #2Document20 pagesThe Entrepreneurial and Entrepreneurial Mind: Week #2Mr.BaiGNo ratings yet
- Logging Best Practices Guide PDFDocument12 pagesLogging Best Practices Guide PDFbnanduriNo ratings yet
- Karriem Provet,: Background of This CaseDocument11 pagesKarriem Provet,: Background of This CaseJustia.comNo ratings yet
- APPLICATION FOR REGISTRATION/ACCREDITATION AS AN ECOZONE SERVICE ENTERPRISE (For Customs Broker, Freight Forwarder/Trucker and Security Agency)Document7 pagesAPPLICATION FOR REGISTRATION/ACCREDITATION AS AN ECOZONE SERVICE ENTERPRISE (For Customs Broker, Freight Forwarder/Trucker and Security Agency)Albert YsegNo ratings yet
- Worksheet 1: The Terms of An AgreementDocument2 pagesWorksheet 1: The Terms of An AgreementJulieta ImbaquingoNo ratings yet
- Grade 2 - 1ST Periodical TestDocument5 pagesGrade 2 - 1ST Periodical TestGAY IBANEZ100% (1)
- Unusual Ways Usual DestinationDocument3 pagesUnusual Ways Usual DestinationLina Saad0% (1)
- LEARNING THEORIES Ausubel's Learning TheoryDocument17 pagesLEARNING THEORIES Ausubel's Learning TheoryCleoNo ratings yet
- International Law: Savarkar CaseDocument15 pagesInternational Law: Savarkar CaseArunesh Chandra100% (1)
- New Microsoft Office Word DocumentDocument12 pagesNew Microsoft Office Word DocumentRamana VaralaNo ratings yet
- Care of Terminally IllDocument34 pagesCare of Terminally Illbemina jaNo ratings yet
- State of The Handloom Industry of BangladeshDocument8 pagesState of The Handloom Industry of BangladeshNoshin NawarNo ratings yet
- SOPDocument3 pagesSOPShreya BonteNo ratings yet
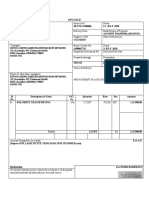
- Invoice: Qrt. No - : Cc-15, Civil Township Rourkela, Dist - (Sundargarh (Odisha) - 769012 GSTIN - 21ACWFS2234G1Z4Document2 pagesInvoice: Qrt. No - : Cc-15, Civil Township Rourkela, Dist - (Sundargarh (Odisha) - 769012 GSTIN - 21ACWFS2234G1Z4PUNYASHLOK PANDANo ratings yet
- Greece Education Foundation Courses and Gces 10 2010Document6 pagesGreece Education Foundation Courses and Gces 10 2010Stamatios KarapournosNo ratings yet
- Pengkarya Muda - Aliah BiDocument7 pagesPengkarya Muda - Aliah BiNORHASLIZA BINTI MOHAMAD MoeNo ratings yet
- Data Sheets Ecc I On AdoraDocument23 pagesData Sheets Ecc I On AdoraAlanAvtoNo ratings yet
- Proposal (Objective Jpurpose Jscope)Document3 pagesProposal (Objective Jpurpose Jscope)Lee ChloeNo ratings yet
- Index: Monthly Bulletin-Dec 2022Document46 pagesIndex: Monthly Bulletin-Dec 2022Sanif KhanNo ratings yet
- If ملخص قواعدDocument2 pagesIf ملخص قواعدAhmed GaninyNo ratings yet
- English Curriculum Reforminthe PhilippinesDocument18 pagesEnglish Curriculum Reforminthe PhilippinesLanping FuNo ratings yet
- Stacey Dunlap ResumeDocument3 pagesStacey Dunlap ResumestaceysdunlapNo ratings yet
- M HealthDocument81 pagesM HealthAbebe ChekolNo ratings yet
- Babst Vs CA PDFDocument17 pagesBabst Vs CA PDFJustin YañezNo ratings yet
- Ie 2e Level 4 Unit 9-4Document4 pagesIe 2e Level 4 Unit 9-4Stasya EgorovaNo ratings yet
- Dual-Band Wearable Rectenna For Low-Power RF Energy HarvestingDocument10 pagesDual-Band Wearable Rectenna For Low-Power RF Energy HarvestingbabuNo ratings yet
- Referee Report TemplateDocument2 pagesReferee Report TemplateAna Jufriani100% (1)
EMPHYSEMA
EMPHYSEMA
Uploaded by
Jerick DaangOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
EMPHYSEMA
EMPHYSEMA
Uploaded by
Jerick DaangCopyright:
Available Formats
Emphysema
- a long-term, progressive disease of the lungs that primarily causes shortness of breath. In people with emphysema,
the tissues necessary to support the physical shape and function of the lungs are destroyed. It is included in a group of
diseases called chronic obstructive pulmonary disease or COPD (pulmonary refers to the lungs). Emphysema is called
an obstructive lung disease because the destruction of lung tissue around smaller sacs, called alveoli, makes these air
sacs unable to hold their functional shape upon exhalation. It is often caused by smoking or long-term exposure to air
pollution.
The term means swelling and comes from the Greek ἐμφυσᾶν emhysan meaning inflate, itself composed of
ἐν en meaning in and φυσᾶν physan meaning breath, blast
- a condition in which chronic inflammation of the lungs leads to destruction of alveoli and decreased elasticity of
the lungs. As a result, air is trapped and lungs hyperinflate.
INSPECTION: SOB, especially on exertion, barrel chest, pursed lip breathing, use of accessory muscles, cyanosis,
clubbing of fingers, tripod posture.
PALPATION: decreased chest expansion, decreased tactile fremitus (palpable vibration on the chest wall when the
client speaks)
PERCUSSION: hyperresonance : abnormally loud auscultatory tone that is low & long duration (ex. Lungs filled with air)
AUSCULTATION: decreased vesicular sounds and possible wheeze (whistling/high pitched)
Classification
Emphysema can be classified into primary and secondary. However, it is more commonly classified by location into
panacinary and centroacinary (or panacinar and centriacinar, or centrilobular and panlobular).
Panacinar (or panlobular) emphysema: The entire respiratory acinus, from respiratory bronchiole to
alveoli, is expanded. Occurs more commonly in the lower lobes, especially basal segments, and anterior margins of the
lungs.
Centriacinar (or centrilobular) emphysema: The respiratory bronchiole (proximal and central part of the
acinus) is expanded. The distal acinus or alveoli are unchanged. Occurs more commonly in the upper lobes.
Other types include distal acinar and irregular. A special type is congenital lobar emphysema (CLE).
Congenital lobar emphysema - CLE results in overexpansion of a pulmonary lobe and resultant compression of the
remaining lobes of the ipsilateral lung, and possibly also the contralateral lung. There is bronchial narrowing because of
weakened or absent bronchial cartilage. There may be congenital extrinsic compression, commonly by an abnormally
large pulmonary artery. This causes malformation of bronchial cartilage, making them soft and collapsible. CLE is
potentially reversible, yet possibly life-threatening, causing respiratory distress in the neonate.
Paraseptal emphysema - Paraseptal emphysema is a type of emphysema which involves the alveolar ducts and sacs
at the lung periphery. The emphysematous areas are subpleural in location and often surrounded by interlobular septa
(hence the name). It may be an incidental finding in young adults, and may be associated with
spontaneous pneumothorax. It may also be seen in older patients with centrilobular emphysema. Both centrilobular and
paraseptal emphysema may progress to bullous emphysema. A bulla is defined as being at least 1cm in diameter, and
with a wall less than 1mm thick. Bullae are thought to arise by air trapping in emphysematous spaces, causing local
expansion.
Signs and symptoms
Smoking is one major cause of this destruction, which causes the small airways in the lungs to collapse during forced
exhalation. As a result, airflow is impeded and air becomes trapped, just as in other obstructive lung diseases.
Symptoms include shortness of breath on exertion, and an expanded chest.
People with this disease do not get enough oxygen and cannot remove carbon dioxide from their blood; they therefore
exhibit dyspnea (shortness of breath). At first this occurs only during physical activity. Eventually it will occur after any
physical exertion. Later the patient may be dyspneic all the time, even when relaxing. Because breathing is difficult, the
patient must use accessory muscles to help them breathe; tachypnea (rapid breathing) may occur they try to extend
their exertion. They may have trouble coughing and lowered amounts of sputum. They may also lose weight.
The anteroposterior diameter of their chest may increase; this symptom is sometimes referred as "barrel chest." The
patient may lean forward with arms extended or resting on something to help them breathe.
When lung auscultation and chest percussion is performed a hyperresonant sound is heard (Mc Cance). The patient
may exhibit symptoms of cyanosis, lowered oxygen levels and increased carbon dioxide levels.
Diagnosis
The diagnosis is usually confirmed by pulmonary function testing (e.g. spirometry); however, X-ray radiography may aid
in the diagnosis. A DLCO test may be used to differentiate Emphysema from other types of Obstructive disorders such
as Chronic Bronchitis and Asthma. DLCO is a test that measures the ability of gases to diffuse across the alveolar-
capillary membrane. A DLCO will be decreased in Emphysema whereas it will be normal or increased in Asthma and
Chronic Bronchitis.
Management
Emphysema is also treated by supporting the breathing with anticholinergics, bronchodilators, steroid medication
(inhaled or oral), effective body positioning (High Fowlers), and supplemental oxygen as required. Treating the patient's
other conditions including gastric reflux and allergies may improve lung function. Supplemental oxygen used as
prescribed (usually more than 20 hours per day) is the only non-surgical treatment which has been shown to prolong life
in emphysema patients. There are lightweight portable oxygen systems which allow patients increased mobility.
Patients can fly, cruise, and work while using supplemental oxygen. Other medications are being researched.
Lung volume reduction surgery (LVRS) can improve the quality of life for certain carefully selected patients. It can be
done by different methods, some of which are minimally invasive. In July 2006 a new treatment, placing tiny valves in
passages leading to diseased lung areas, was announced to have good results, but 7% of patients suffered partial lung
collapse. The only known "cure" for emphysema is lung transplant, but few patients are strong enough physically to
survive the surgery. The combination of a patient's age, oxygen deprivation and the side-effects of the medications used
to treat emphysema cause damage to the kidneys, heart and other organs. Surgical transplantation also requires the
patient to take an anti-rejection drug regimen which suppresses the immune system, and can lead to
microbial infection of the patient. Patients who think they may have contracted the disease are recommended to seek
medical attention as soon as possible.
Emphysema is an irreversible degenerative condition. The most important measure to slow its progression is for the
patient to stop smoking and avoid all exposure to cigarette smoke and lung irritants.Pulmonary rehabilitation can be
very helpful to optimize the patient's quality of life and teach the patient how to actively manage his or her care.
Nursing Interventions
- If ordered, perform chest physiotherapy, including postural drainage and chest persussion and vibration
several times daily.
- Make sure the patient receives adequate fluids at least 3 liters per day to loosen secretions
- Monitor the patient’s RBC count for increases (warning signs of increasing lung and vascular congestion).
- Watch for complications, such as respiratory tract infections, cor pulmonale, spontaneous pneumothorax,
respiratory failure, and peptic ulcer disease.
You might also like
- Renaissance Woman: Fat Loss, Muscle Growth & Performance Through Scientific EatingDocument20 pagesRenaissance Woman: Fat Loss, Muscle Growth & Performance Through Scientific EatingBenedict Ray Andhika33% (3)
- Obstructive Disease of Lung and Physiotherapy ManagementDocument76 pagesObstructive Disease of Lung and Physiotherapy Managementphysio43100% (1)
- List of Documents NBA PfilesDocument48 pagesList of Documents NBA PfilesDr. A. Pathanjali Sastri100% (1)
- Remembering, Bartlett (1932)Document11 pagesRemembering, Bartlett (1932)andreea4etc100% (1)
- Emphysema Is A LongDocument54 pagesEmphysema Is A LongryemoralesNo ratings yet
- CopdDocument4 pagesCopdapi-3739910100% (2)
- CR Patho SummaryDocument22 pagesCR Patho SummaryDNAANo ratings yet
- EmphysemaDocument27 pagesEmphysemaDiana Laura LeiNo ratings yet
- COPDDocument18 pagesCOPDMae CalicaNo ratings yet
- Emphysema Fall 2019Document3 pagesEmphysema Fall 2019Mary MarshNo ratings yet
- Asthma and The COPDsDocument133 pagesAsthma and The COPDsShania robertsNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument12 pagesChronic Obstructive Pulmonary Diseasejisoo100% (1)
- Chronic Obstructive Pulmonary DiseaseDocument10 pagesChronic Obstructive Pulmonary DiseaseZinya RobinsonNo ratings yet
- Emphysema A D A7Document13 pagesEmphysema A D A7Ahmed DsoukiNo ratings yet
- Textbuk DiscussionDocument5 pagesTextbuk Discussionapi-3717941No ratings yet
- Oxygenation NotesDocument23 pagesOxygenation NoteschikaycNo ratings yet
- Copd 200412082048Document139 pagesCopd 200412082048Richard ArceNo ratings yet
- EmphysemaDocument2 pagesEmphysemaapi-322389115No ratings yet
- Breathlessness EdittedDocument2 pagesBreathlessness EdittedSalwani MohamedNo ratings yet
- Resp Objectives Adn 253Document4 pagesResp Objectives Adn 253christian_zarate_2No ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument12 pagesChronic Obstructive Pulmonary DiseaseibegbunamchinemeremNo ratings yet
- Obstructive DisordersDocument23 pagesObstructive DisordersMartha ChaseNo ratings yet
- COPDDocument7 pagesCOPDarminmercado7406No ratings yet
- Patholpgic Change in EmphysemiaDocument16 pagesPatholpgic Change in Emphysemiafenil1194No ratings yet
- Onchi & CopdDocument8 pagesOnchi & CopdAngellene GraceNo ratings yet
- CopdDocument30 pagesCopdsalmanhabeebekNo ratings yet
- Normal Changes of AgingDocument9 pagesNormal Changes of AgingGiselle EstoquiaNo ratings yet
- Nursing Care Management - 112Document67 pagesNursing Care Management - 112Ong KarlNo ratings yet
- Copd CaseDocument36 pagesCopd Casejho_No ratings yet
- Dyspnea Is An Uncomfortable Abnormal Awareness of Breathing. A Number of DifferentDocument4 pagesDyspnea Is An Uncomfortable Abnormal Awareness of Breathing. A Number of DifferentSita SifanaNo ratings yet
- Pathophysiology of EmphysemaDocument3 pagesPathophysiology of EmphysemaApple Maiquez Garcia100% (1)
- Pathophysiology of COPD: Heart Failure Respiratory DisordersDocument5 pagesPathophysiology of COPD: Heart Failure Respiratory DisordersKath DeguzmanNo ratings yet
- The Respiratory SystemDocument8 pagesThe Respiratory SystemJane Rose SuperadaNo ratings yet
- NCLEX Review NotesDocument36 pagesNCLEX Review NotesKyla Patricia RibanoNo ratings yet
- Obstructive Airway DiseasesDocument56 pagesObstructive Airway Diseaseskalanakariyawasam99No ratings yet
- Respiratory SystemDocument85 pagesRespiratory SystemDr:-Ustaad Aakass Ahmed Junejo SahabNo ratings yet
- Case Study For EmphysemaDocument5 pagesCase Study For EmphysemaGabbii CincoNo ratings yet
- (Respi) Lo Week 2 Tutorial 1Document10 pages(Respi) Lo Week 2 Tutorial 1KintanNo ratings yet
- Oxygenation and Airway Management: Quick LookDocument24 pagesOxygenation and Airway Management: Quick LookNining Komala SariNo ratings yet
- Emphysema Chronic Obstructive Pulmonary Disease (COPD) : Call Dasco Today For More Information 855-442-7912Document6 pagesEmphysema Chronic Obstructive Pulmonary Disease (COPD) : Call Dasco Today For More Information 855-442-7912Nazif Aiman IsmailNo ratings yet
- Acute Respiratory Failure-PRINTDocument5 pagesAcute Respiratory Failure-PRINTJan SicatNo ratings yet
- Adult - RespiratoryDocument14 pagesAdult - RespiratoryahmeddorostyNo ratings yet
- Systems Plus College Foundation Macarthur Highway, Balibago, Angeles CityDocument13 pagesSystems Plus College Foundation Macarthur Highway, Balibago, Angeles CityLeanne Princess GamboaNo ratings yet
- Bronchial Obstruction: Presenter Andrea Fagan 3 Year Student NurseDocument27 pagesBronchial Obstruction: Presenter Andrea Fagan 3 Year Student NurseAndrea FaganNo ratings yet
- COPD Treatment and ManagementDocument3 pagesCOPD Treatment and ManagementHydie Mae AlcabedosNo ratings yet
- Patho Exam 3: Deficiency in Alpha-1-Antitrypsin-Unchecked Elastase Destruction of The AlveoliDocument5 pagesPatho Exam 3: Deficiency in Alpha-1-Antitrypsin-Unchecked Elastase Destruction of The AlveoliTaran LuthraNo ratings yet
- Reviewer For Management of Common IllnessDocument27 pagesReviewer For Management of Common Illnessmarie vennis hamchawanNo ratings yet
- Epidemiology: Several Diseases Airflow ObstructionDocument11 pagesEpidemiology: Several Diseases Airflow ObstructionBharat Singh BanshiwalNo ratings yet
- Dr. Kamran - S PBLDocument12 pagesDr. Kamran - S PBLTaimoor Ul HassanNo ratings yet
- CopdDocument60 pagesCopdRizqy Shofianingrum100% (1)
- COPDDocument30 pagesCOPDAmila SirisingheNo ratings yet
- Pulmonary PathologyDocument46 pagesPulmonary PathologyMuostafa KamelNo ratings yet
- Day 5 Respiratory DiseaseDocument71 pagesDay 5 Respiratory DiseaseRamzen Raphael DomingoNo ratings yet
- COPD & RLDDocument17 pagesCOPD & RLDhis.thunder122No ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument4 pagesChronic Obstructive Pulmonary DiseaseSeraphina SolanNo ratings yet
- LP Dyspnea RevisiDocument12 pagesLP Dyspnea RevisiInsaniNo ratings yet
- EmphysemaDocument3 pagesEmphysemaKhalid Mahmud ArifinNo ratings yet
- Essay EmphysemaDocument6 pagesEssay EmphysemaChristopher EstevezNo ratings yet
- DR Ambreen Shams NephrologistDocument58 pagesDR Ambreen Shams NephrologistAamer NaeemNo ratings yet
- Interstitial Lung DiseaseDocument14 pagesInterstitial Lung DiseaseAzkaZulfiqarNo ratings yet
- Physical Rehabilitation For Asthmatic PatientsDocument54 pagesPhysical Rehabilitation For Asthmatic PatientsIjeoma Okpalla60% (5)
- Atelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesFrom EverandAtelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesNo ratings yet
- The Entrepreneurial and Entrepreneurial Mind: Week #2Document20 pagesThe Entrepreneurial and Entrepreneurial Mind: Week #2Mr.BaiGNo ratings yet
- Logging Best Practices Guide PDFDocument12 pagesLogging Best Practices Guide PDFbnanduriNo ratings yet
- Karriem Provet,: Background of This CaseDocument11 pagesKarriem Provet,: Background of This CaseJustia.comNo ratings yet
- APPLICATION FOR REGISTRATION/ACCREDITATION AS AN ECOZONE SERVICE ENTERPRISE (For Customs Broker, Freight Forwarder/Trucker and Security Agency)Document7 pagesAPPLICATION FOR REGISTRATION/ACCREDITATION AS AN ECOZONE SERVICE ENTERPRISE (For Customs Broker, Freight Forwarder/Trucker and Security Agency)Albert YsegNo ratings yet
- Worksheet 1: The Terms of An AgreementDocument2 pagesWorksheet 1: The Terms of An AgreementJulieta ImbaquingoNo ratings yet
- Grade 2 - 1ST Periodical TestDocument5 pagesGrade 2 - 1ST Periodical TestGAY IBANEZ100% (1)
- Unusual Ways Usual DestinationDocument3 pagesUnusual Ways Usual DestinationLina Saad0% (1)
- LEARNING THEORIES Ausubel's Learning TheoryDocument17 pagesLEARNING THEORIES Ausubel's Learning TheoryCleoNo ratings yet
- International Law: Savarkar CaseDocument15 pagesInternational Law: Savarkar CaseArunesh Chandra100% (1)
- New Microsoft Office Word DocumentDocument12 pagesNew Microsoft Office Word DocumentRamana VaralaNo ratings yet
- Care of Terminally IllDocument34 pagesCare of Terminally Illbemina jaNo ratings yet
- State of The Handloom Industry of BangladeshDocument8 pagesState of The Handloom Industry of BangladeshNoshin NawarNo ratings yet
- SOPDocument3 pagesSOPShreya BonteNo ratings yet
- Invoice: Qrt. No - : Cc-15, Civil Township Rourkela, Dist - (Sundargarh (Odisha) - 769012 GSTIN - 21ACWFS2234G1Z4Document2 pagesInvoice: Qrt. No - : Cc-15, Civil Township Rourkela, Dist - (Sundargarh (Odisha) - 769012 GSTIN - 21ACWFS2234G1Z4PUNYASHLOK PANDANo ratings yet
- Greece Education Foundation Courses and Gces 10 2010Document6 pagesGreece Education Foundation Courses and Gces 10 2010Stamatios KarapournosNo ratings yet
- Pengkarya Muda - Aliah BiDocument7 pagesPengkarya Muda - Aliah BiNORHASLIZA BINTI MOHAMAD MoeNo ratings yet
- Data Sheets Ecc I On AdoraDocument23 pagesData Sheets Ecc I On AdoraAlanAvtoNo ratings yet
- Proposal (Objective Jpurpose Jscope)Document3 pagesProposal (Objective Jpurpose Jscope)Lee ChloeNo ratings yet
- Index: Monthly Bulletin-Dec 2022Document46 pagesIndex: Monthly Bulletin-Dec 2022Sanif KhanNo ratings yet
- If ملخص قواعدDocument2 pagesIf ملخص قواعدAhmed GaninyNo ratings yet
- English Curriculum Reforminthe PhilippinesDocument18 pagesEnglish Curriculum Reforminthe PhilippinesLanping FuNo ratings yet
- Stacey Dunlap ResumeDocument3 pagesStacey Dunlap ResumestaceysdunlapNo ratings yet
- M HealthDocument81 pagesM HealthAbebe ChekolNo ratings yet
- Babst Vs CA PDFDocument17 pagesBabst Vs CA PDFJustin YañezNo ratings yet
- Ie 2e Level 4 Unit 9-4Document4 pagesIe 2e Level 4 Unit 9-4Stasya EgorovaNo ratings yet
- Dual-Band Wearable Rectenna For Low-Power RF Energy HarvestingDocument10 pagesDual-Band Wearable Rectenna For Low-Power RF Energy HarvestingbabuNo ratings yet
- Referee Report TemplateDocument2 pagesReferee Report TemplateAna Jufriani100% (1)