Professional Documents
Culture Documents
ICU One Pager Hypoxemia
ICU One Pager Hypoxemia
Uploaded by
Nicholas HelmstetterCopyright:
Available Formats
You might also like
- Prehospital Emergency Pharmacology 8Th Edition Full ChapterDocument21 pagesPrehospital Emergency Pharmacology 8Th Edition Full Chapterlouise.guerrero88396% (25)
- اسئلة علي فاينل مقرر طوارئ نظري2023HHDocument119 pagesاسئلة علي فاينل مقرر طوارئ نظري2023HHalshamyb309No ratings yet
- ACORN TrialDocument11 pagesACORN TrialsaramabulolaNo ratings yet
- Flight For Life 81M.01 Mechanical Ventilation 2022-07-01Document4 pagesFlight For Life 81M.01 Mechanical Ventilation 2022-07-01Bryan WinchellNo ratings yet
- IV Study Guide 2013Document78 pagesIV Study Guide 2013Kaloy KamaoNo ratings yet
- Hemodynamic Monitoring Made Incredibly Visual!Document2 pagesHemodynamic Monitoring Made Incredibly Visual!Artaria NurainiNo ratings yet
- Super V+ ManualDocument20 pagesSuper V+ ManualStepan BorisovichNo ratings yet
- Surgery Final NotesDocument81 pagesSurgery Final NotesDETECTIVE CONANNo ratings yet
- Updated BLS Provider ManualDocument24 pagesUpdated BLS Provider ManualRaquel Bregita-RasNo ratings yet
- Guide To Oxygen Delivery SystemDocument3 pagesGuide To Oxygen Delivery Systemsheirlyazhari56530% (1)
- Cardiac/Cardiogenic Shock: Clinical Practice GuidelinesDocument3 pagesCardiac/Cardiogenic Shock: Clinical Practice GuidelinesAnonymous Yo0mStNo ratings yet
- 2011 Understanding Pharmacology Essentials For Medication SafetyDocument1 page2011 Understanding Pharmacology Essentials For Medication SafetygloriyaNo ratings yet
- ICU One Pager ECMO FundamentalsDocument1 pageICU One Pager ECMO FundamentalsNicholas Helmstetter100% (1)
- EEM496 Communication Systems Laboratory - Experiment 4 - Digitally Modulated Signals Using Matlab, Pam (Ask), PSK, and QamDocument4 pagesEEM496 Communication Systems Laboratory - Experiment 4 - Digitally Modulated Signals Using Matlab, Pam (Ask), PSK, and Qamdonatello84No ratings yet
- The Alveolar Gas EquationDocument4 pagesThe Alveolar Gas Equationstewart_fNo ratings yet
- Ards Pocket Card 4.7 QRDocument1 pageArds Pocket Card 4.7 QRGenghis SupnetNo ratings yet
- ABCs of Thoracic TraumaDocument5 pagesABCs of Thoracic TraumaAlice S ChangNo ratings yet
- Cardiovascular & Hematologic SystemDocument163 pagesCardiovascular & Hematologic SystemRellie CastroNo ratings yet
- Chapter 6 Care of The Patient Experiencing Shock or Heart FailureDocument49 pagesChapter 6 Care of The Patient Experiencing Shock or Heart FailureJennifer KellerNo ratings yet
- Textbook ReadingDocument275 pagesTextbook ReadingNovitasari EkaNo ratings yet
- Using The ACLS Primary Survey For A Patient in Respiratory ArrestDocument34 pagesUsing The ACLS Primary Survey For A Patient in Respiratory Arrest강기연100% (1)
- ABCDEF Bundle WebcastDocument42 pagesABCDEF Bundle WebcastsoulstakersNo ratings yet
- Sirs & ModsDocument5 pagesSirs & Modsmarlou agananNo ratings yet
- ST ND RD THDocument8 pagesST ND RD THLuvleen KaurNo ratings yet
- Nursing Pharmacology (Chapter 1 - Introduction)Document1 pageNursing Pharmacology (Chapter 1 - Introduction)Jemima GasconNo ratings yet
- Pre Hos TraumaDocument11 pagesPre Hos TraumaGel OmugtongNo ratings yet
- 01 - Decision Making in Emergency MedicineDocument4 pages01 - Decision Making in Emergency MedicineSlvdrPlgrnNo ratings yet
- Avoiding Common Errors in The Emergency Department-1002-1280Document280 pagesAvoiding Common Errors in The Emergency Department-1002-1280Hernando CastrillónNo ratings yet
- Emergency Ortho BCS 2017Document80 pagesEmergency Ortho BCS 2017Priza Razunip100% (1)
- Hypertonic Saline and Mannitol Therapy in Critical Care NeurologyDocument9 pagesHypertonic Saline and Mannitol Therapy in Critical Care NeurologyRonAlNo ratings yet
- Medical Surgical Nursing Mnemonics and TipsDocument36 pagesMedical Surgical Nursing Mnemonics and TipsAniki OniiNo ratings yet
- Nursing Pharma (Chapter 2 - Pharmaco & Pharmady)Document1 pageNursing Pharma (Chapter 2 - Pharmaco & Pharmady)Jemima GasconNo ratings yet
- Brain Sheet2011Document1 pageBrain Sheet2011nursekatieNo ratings yet
- FundamentalsDocument115 pagesFundamentalsMichelle Dona MirallesNo ratings yet
- Family Medicine M3 Clerkship Hypertensive Disorders: Joy Shen-Wagner MDDocument35 pagesFamily Medicine M3 Clerkship Hypertensive Disorders: Joy Shen-Wagner MDJT Thomas100% (1)
- MED 1.17 - Gastrointestinal CancersDocument6 pagesMED 1.17 - Gastrointestinal CancersZazaNo ratings yet
- Therapeutic Hypothermia ChillOutDocument38 pagesTherapeutic Hypothermia ChillOutJason RodmanNo ratings yet
- Prehospital Anesthesia HandbookDocument46 pagesPrehospital Anesthesia HandbookoscarNo ratings yet
- Cardiovascular System: By: Marc Anthony Liao RNDocument59 pagesCardiovascular System: By: Marc Anthony Liao RNloveseeker06No ratings yet
- ANTIBIOTICS Pharmacology NursingDocument10 pagesANTIBIOTICS Pharmacology NursingRalph Alfonse De JesusNo ratings yet
- Assessment of The Chest and LungsDocument46 pagesAssessment of The Chest and LungsSumathi GopinathNo ratings yet
- Pharmacology Quick HitsDocument6 pagesPharmacology Quick HitsHuma Hameed DogarNo ratings yet
- Empress' Dragoons Officer Part 1Document34 pagesEmpress' Dragoons Officer Part 1Luca de Fabbris100% (1)
- 7 Suggestions Paramedic Airway ANAM22 WMDocument5 pages7 Suggestions Paramedic Airway ANAM22 WMcedivadeniaNo ratings yet
- Pharmacology Midterm TestDocument19 pagesPharmacology Midterm Testmarie curryNo ratings yet
- Management of ArrhythmiasDocument4 pagesManagement of ArrhythmiasAray Al-AfiqahNo ratings yet
- Senior Center StudyDocument117 pagesSenior Center StudyIulian TNo ratings yet
- Emergency MnemonicDocument5 pagesEmergency Mnemonicanon_549623261No ratings yet
- Sepsis Quick Reference GuideDocument1 pageSepsis Quick Reference GuideRavin DebieNo ratings yet
- Anatomy RespDocument57 pagesAnatomy RespGunawan SamosirNo ratings yet
- Heart Failure Express Card HMCDocument2 pagesHeart Failure Express Card HMCalexNo ratings yet
- Ventilator Modes - WEANINGDocument3 pagesVentilator Modes - WEANINGAlaa OmarNo ratings yet
- Basic Drug Computations Part 1Document8 pagesBasic Drug Computations Part 1Carl Elexer Cuyugan Ano100% (4)
- Nursing CS Angina-Pectoris-medications 03Document1 pageNursing CS Angina-Pectoris-medications 03Mahdia akterNo ratings yet
- Neonatal SkinDocument384 pagesNeonatal SkinErnestas ViršilasNo ratings yet
- Calc Drip Rates 2Document2 pagesCalc Drip Rates 2Charisse Nicole DiazNo ratings yet
- Print Foundations - Fundamentals of Nursing, Chapter 48 Skin Integrity and Wound Care Flashcards - Easy NotecardsDocument6 pagesPrint Foundations - Fundamentals of Nursing, Chapter 48 Skin Integrity and Wound Care Flashcards - Easy NotecardsMark M. AlipioNo ratings yet
- Maternal Medications - Uterotonic (Induction/Augmentation of Labor And/or Prevention/Treatment of Hemorrhage)Document19 pagesMaternal Medications - Uterotonic (Induction/Augmentation of Labor And/or Prevention/Treatment of Hemorrhage)SariahNo ratings yet
- ASIA International Standards For Neurological Classification of Spinal Cord InjuryDocument2 pagesASIA International Standards For Neurological Classification of Spinal Cord InjuryMicah Tagle100% (1)
- Philosophy of NursingDocument8 pagesPhilosophy of Nursingapi-430575435No ratings yet
- Med Surg BurnsDocument8 pagesMed Surg BurnsawuahbohNo ratings yet
- Community Acquired Pneumonia CAP 1.28.21Document1 pageCommunity Acquired Pneumonia CAP 1.28.21Illaizah EdictoNo ratings yet
- ICU One Pager Massive Hemoptysis v11Document1 pageICU One Pager Massive Hemoptysis v11Nicholas HelmstetterNo ratings yet
- ICU One Pager NIPPVDocument1 pageICU One Pager NIPPVNicholas HelmstetterNo ratings yet
- Guide Beer Flavor Zymurgy-1987 PDFDocument21 pagesGuide Beer Flavor Zymurgy-1987 PDFNicholas HelmstetterNo ratings yet
- ICU One Pager Abdominal Compartment SyndromeDocument1 pageICU One Pager Abdominal Compartment SyndromeNicholas HelmstetterNo ratings yet
- Blood Flow Q: The Transmembrane Pressure (TMP) GradientDocument1 pageBlood Flow Q: The Transmembrane Pressure (TMP) GradientNicholas HelmstetterNo ratings yet
- ICU One Pager Lactic AcidosisDocument1 pageICU One Pager Lactic AcidosisNicholas Helmstetter100% (1)
- ICU One Pager Minnesota TubeDocument1 pageICU One Pager Minnesota TubeNicholas HelmstetterNo ratings yet
- 1001 Songs You Must Hear Before You Die 27526Document7 pages1001 Songs You Must Hear Before You Die 27526Nicholas HelmstetterNo ratings yet
- Movesets)Document158 pagesMovesets)Nicholas HelmstetterNo ratings yet
- How To... Select Multiple Values in A Dropdown BoxDocument15 pagesHow To... Select Multiple Values in A Dropdown Boxkalicharan13No ratings yet
- Allowable Span/Depth Ratio For High Strength Concrete BeamsDocument1 pageAllowable Span/Depth Ratio For High Strength Concrete BeamsbagmassNo ratings yet
- Chemical NamesDocument4 pagesChemical NamesSomesubhraDasNo ratings yet
- Lecture Notes 11-Euler Method-IIDocument59 pagesLecture Notes 11-Euler Method-IITesfaye Teferi ShoneNo ratings yet
- Garat2015 PDFDocument7 pagesGarat2015 PDFmanojkumarNo ratings yet
- MS, TMT, CTDDocument5 pagesMS, TMT, CTDAbdul BasitNo ratings yet
- Analyze Phase Workbook - FinalDocument151 pagesAnalyze Phase Workbook - FinalNicola100% (1)
- Chapter 2 (Electrostatic Potential and Capacitance) UnsolvedDocument8 pagesChapter 2 (Electrostatic Potential and Capacitance) UnsolvedMahendra ShahNo ratings yet
- Nemo Windcatcher: Industry-Leading Drive Test Data Post-Processing and AnalysisDocument2 pagesNemo Windcatcher: Industry-Leading Drive Test Data Post-Processing and AnalysistreejumboNo ratings yet
- Coleman RV 12 Volt Thermistat ACDocument18 pagesColeman RV 12 Volt Thermistat ACsthoma20100% (1)
- Electrical Protections: Presentation byDocument34 pagesElectrical Protections: Presentation bydjfffNo ratings yet
- NCP1002Document14 pagesNCP1002Ailton De JesusNo ratings yet
- 3 2systems AlgDocument20 pages3 2systems AlgSyeda Saman Zahra Zaidi/TCHR/GBFNo ratings yet
- Indefinite IntegralDocument18 pagesIndefinite IntegralMA LEAH I ABADNo ratings yet
- Pemanfaatan Ilmu Fisika Terhadap PeternakanDocument15 pagesPemanfaatan Ilmu Fisika Terhadap PeternakanSinta Sri RahayuNo ratings yet
- Fluidtecq Fluidtecq Fluidtecq Fluidtecq: Operation and Maintenance ManualDocument12 pagesFluidtecq Fluidtecq Fluidtecq Fluidtecq: Operation and Maintenance ManualmehtahemalNo ratings yet
- ESDU BrochureDocument3 pagesESDU BrochureWilhelm ThorleyNo ratings yet
- PRU Assembly Instruction User GuideDocument50 pagesPRU Assembly Instruction User GuideJános JuhászNo ratings yet
- Bateria Sellada Agm Marca Magna Acceso Frontal 12v-150ah (Maf150-12)Document2 pagesBateria Sellada Agm Marca Magna Acceso Frontal 12v-150ah (Maf150-12)SOLUCIONES ENERGETICAS Y PROCESOS INNOVADORESNo ratings yet
- AnaDev - Building A Homebrew Load BoxDocument3 pagesAnaDev - Building A Homebrew Load BoxciccioNo ratings yet
- Appnote Operating SPL PLXX 03112004Document5 pagesAppnote Operating SPL PLXX 03112004interconnectfast4No ratings yet
- اسئلة كتاب البروتينات والاجبات -Document41 pagesاسئلة كتاب البروتينات والاجبات -Youssef AliNo ratings yet
- LegTech ReviewerDocument9 pagesLegTech ReviewerMaris Cay0% (1)
- Ch04Exp PDFDocument17 pagesCh04Exp PDFConstantin PopescuNo ratings yet
- Microbial NutritionDocument12 pagesMicrobial NutritionJosé Molineros100% (2)
- Generic Earth Directional Relay Io Dir, Io Dir (IOC, UMZ) RelayDocument2 pagesGeneric Earth Directional Relay Io Dir, Io Dir (IOC, UMZ) Relaybauhaus10No ratings yet
- Features Descriptio: Lt3503 1A, 2.2Mhz Step-Down Switching Regulator in 2Mm × 3Mm DFNDocument20 pagesFeatures Descriptio: Lt3503 1A, 2.2Mhz Step-Down Switching Regulator in 2Mm × 3Mm DFNBrett HufnagleNo ratings yet
- DSE Leaflet 22-23 Final - 0Document2 pagesDSE Leaflet 22-23 Final - 0NisAr AhmadNo ratings yet
ICU One Pager Hypoxemia
ICU One Pager Hypoxemia
Uploaded by
Nicholas HelmstetterOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ICU One Pager Hypoxemia
ICU One Pager Hypoxemia
Uploaded by
Nicholas HelmstetterCopyright:
Available Formats
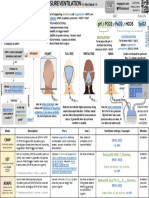
HYPOXIA & HYPOXEMIA by Nick Mark MD ONE
onepagericu.com Link to the
most current
@nickmmark version →
DEFINITIONS: 100% 20 13
Hypoxia – insufficient oxygen delivered to tissues to meet demands OXYGEN DELIVERY:
HB SATURATION SaO2
Tissue hypoxia occurs when DELIVERY OF OXYGEN (DO2) is inadequate to meet
O2 CONTENT CaO2
80% 16 11
Hypoxemia – low oxygen in the blood (most common type of hypoxia) P O2
metabolic demands. DO2 depends on CARDIAC OUTPUT (CO) & the
I
=140
60% 12 8
PIO2 – atmospheric oxygen (how much O2 is inspired) MIXED OXYGEN CONTENT OF BLOOD (CaO2)
PAO2 – alveolar oxygen (how much O2 reaches the alveoli) VENOUS ARTERIAL 8 5
40%
BLOOD
PaO2 – oxygen dissolved in arterial blood (measured on ABG) BLOOD PA O2 20% 4 3
𝐃𝑶𝟐 = 𝑯𝑹 × 𝑺𝑽 × 𝟏. 𝟑𝟒 × 𝑯𝒃 × 𝑺𝒂𝑶𝟐 + (𝑷𝒂𝑶𝟐 × 𝟎. 𝟎𝟎𝟑)
SaO2 – percent saturation of hemoglobin in arterial blood SvO2 = 70%
=100
SaO2 = 98%
@Hb = 10
@Hb = 15
20 40 60 80 100
CaO2 – oxygen content of art. blood (dissolved & Hb bound) CvO2 = 15 CaO2 = 20
DISSOLVED O2 PaO2 O2 bound to hemoglobin O2 dissolved in blood
PaO2 = 95 CO
HYPOXEMIC HYPOXIA ISCHEMIC HYPOXIA ANEMIC HYPOXIA CYTOPATHIC HYPOXIA
v1.0 (2020-12-06)
Insufficient oxygen in the blood Insufficient blood flow to tissues, Insufficient O2 carrying capacity Cells cannot use oxygen
CC BY-SA 3.0
(the most common type of hypoxia) also called stagnant hypoxia (e.g. severe blood loss) or abnormal (e.g. cyanide toxicity, maybe sepsis)
(e.g low cardiac output) hemoglobin (e.g. COHb, MetHb)
Low PaO2 Low SvO2 ! Low PaO2 Low CaO2 ! Low SvO2 ! Low PaO2 High PaO2, High SvO2
LOW INSPIRED OXYGEN (PIO2) ALVEOLAR HYPOVENTILATION V/Q MISMATCH SHUNT DIFFUSION LIMITATION
Fewer oxygen molecules enter the Fewer O2 molecules reach the alveoli Imbalance between regional lung Blood passes from the right side of Impaired O2 diffusion from alveoli to
lungs with respiration (low PAO2) due to decreased ventilation (low ventilation and perfusion (low V/Q). the heart to the left side without RBC, causing hypoxemia particularly
PAO2). Most common cause of hypoxemia. being oxygenated. in with increased cardiac outpu.
· Normal Aa difference · Normal Aa difference · Increased Aa difference · Increased Aa difference · Increased Aa difference
· PaO2 normalizes with supplemental · PaO2 normalizes with supplm. O2 · PaO2 normalizes with suppl. O2 · PaO2 does NOT normalize with · PaO2 normalizes with supplm. O2
oxygen · Increased PaCO2 supplemental oxygen
· Causes: low atmospheric pressure · Causes: decreased respiratory drive · Causes: obstructive lung diseases · Causes: anatomical (ASD, VSD, · Causes: pulmonary fibrosis, edema,
(e.g. high altitude), or low partial (opioids, brainstem stroke, OHVS), (COPD), pulmonary vascular disease pulm AVMs) & physiological shunts & inflammation that impair gas
pressure of oxygen (FiO2 < 0.21 e.g. neuromuscular weakness (GBS, ALS), (PE), alveolar filling processes (atelectasis, pneumonia, ARDS) exchange in the alveoli
confined space, low O2 gas mixtures) chest wall problems (kyphoscoliosis, (pneumonia, pulmonary edema), where blood bypasses alveoli
Borderline With increased blood
flail chest) or airflow obstruction interstitial disease & atelectasis without effective gas exchange
normoxemia at flow frank hypoxemia
(COPD, asthma) rest ensues
Low PAO2 due to Low PAO2 due to ↓ No O2 exchange
globally reduced ventilation relative to occurs and blood is
LOW MIXED VENOUS O2 (SVO2) ventilation perfusion in one area not oxygenated
(PAO2 & PaO2 will NL PA O2 ↓PA O2
(PAO2 & PaO2 will
↓↓PAO2
=0 (PaO2 will not fully
↓PA O2 ↓PA O2
Venous blood returning to the lungs normalize with normalize with normalize with SvO2 = 70% SaO2 = 95% SvO2 = 70% SaO2 = 85%
(SvO2) has very low O2 due to supplemental O2) supplemental O2) supplemental O2) CvO2 = 15 CaO2 = 19 CvO2 = 15 CaO2 = 17
increased extraction. Aa DIFFERENCE (aka Aa GRADIENT): 𝑨𝒈𝒆 𝒚𝒓𝒔 + 𝟏𝟎
𝑵𝒐𝒓𝒎𝒂𝒍 𝑨𝒂 𝒅𝒊𝒇𝒇𝒆𝒓𝒆𝒏𝒄𝒆 =
· Normal Aa difference The Aa DIFFERENCE is the ALVEOLAR OXYGEN TENSION 𝟒 Alveolar CO2 tension
· PaO2 normalizes with (PAO2) minus the ARTERIAL OXYGEN TENSION (PaO2), (assumed to be equal to
SvO2 = 50% SaO2 = 85% 𝑨𝒂 𝒅𝒊𝒇𝒇𝒆𝒓𝒆𝒏𝒄𝒆 = 𝑷𝑨 𝑶𝟐 − 𝑷𝒂 𝑶𝟐
arterial CO2)
supplemental oxygen CvO2 = 10 CaO2 = 17
reflecting the efficiency of oxygen exchange. It is
used to identify the etiology of hypoxemic hypoxia: 𝑷 𝑶 = 𝑭𝒊𝑶 × 𝑷 𝑷𝒂𝑪𝑶 𝟐
unable to fully 𝑨 𝟐 𝟐 𝒂𝒕𝒎 − 𝑷𝑯𝟐𝑶 −
Causes: severe anemia (low CaO2 oxygenate the pulmonary causes have ↑ Aa difference whereas 𝑸
rarely a problem unless Hb <5), low Respiratory
extremely extra-pulmonary etiologies (↓ PiO2, ↓SvO2, & Atmospheric pressure H2O vapor pressure
cardiac output, & extremely high deoxygenated (760 mmHg @ sea level, 630 mmHg @ Quotient
oxygen consumption venous blood
alveolar hypoventilation) have nl Aa difference. (47 mmHg in the lungs) (normally ~0.8)
1500m, 530 mmHg @ 3000m)
You might also like
- Prehospital Emergency Pharmacology 8Th Edition Full ChapterDocument21 pagesPrehospital Emergency Pharmacology 8Th Edition Full Chapterlouise.guerrero88396% (25)
- اسئلة علي فاينل مقرر طوارئ نظري2023HHDocument119 pagesاسئلة علي فاينل مقرر طوارئ نظري2023HHalshamyb309No ratings yet
- ACORN TrialDocument11 pagesACORN TrialsaramabulolaNo ratings yet
- Flight For Life 81M.01 Mechanical Ventilation 2022-07-01Document4 pagesFlight For Life 81M.01 Mechanical Ventilation 2022-07-01Bryan WinchellNo ratings yet
- IV Study Guide 2013Document78 pagesIV Study Guide 2013Kaloy KamaoNo ratings yet
- Hemodynamic Monitoring Made Incredibly Visual!Document2 pagesHemodynamic Monitoring Made Incredibly Visual!Artaria NurainiNo ratings yet
- Super V+ ManualDocument20 pagesSuper V+ ManualStepan BorisovichNo ratings yet
- Surgery Final NotesDocument81 pagesSurgery Final NotesDETECTIVE CONANNo ratings yet
- Updated BLS Provider ManualDocument24 pagesUpdated BLS Provider ManualRaquel Bregita-RasNo ratings yet
- Guide To Oxygen Delivery SystemDocument3 pagesGuide To Oxygen Delivery Systemsheirlyazhari56530% (1)
- Cardiac/Cardiogenic Shock: Clinical Practice GuidelinesDocument3 pagesCardiac/Cardiogenic Shock: Clinical Practice GuidelinesAnonymous Yo0mStNo ratings yet
- 2011 Understanding Pharmacology Essentials For Medication SafetyDocument1 page2011 Understanding Pharmacology Essentials For Medication SafetygloriyaNo ratings yet
- ICU One Pager ECMO FundamentalsDocument1 pageICU One Pager ECMO FundamentalsNicholas Helmstetter100% (1)
- EEM496 Communication Systems Laboratory - Experiment 4 - Digitally Modulated Signals Using Matlab, Pam (Ask), PSK, and QamDocument4 pagesEEM496 Communication Systems Laboratory - Experiment 4 - Digitally Modulated Signals Using Matlab, Pam (Ask), PSK, and Qamdonatello84No ratings yet
- The Alveolar Gas EquationDocument4 pagesThe Alveolar Gas Equationstewart_fNo ratings yet
- Ards Pocket Card 4.7 QRDocument1 pageArds Pocket Card 4.7 QRGenghis SupnetNo ratings yet
- ABCs of Thoracic TraumaDocument5 pagesABCs of Thoracic TraumaAlice S ChangNo ratings yet
- Cardiovascular & Hematologic SystemDocument163 pagesCardiovascular & Hematologic SystemRellie CastroNo ratings yet
- Chapter 6 Care of The Patient Experiencing Shock or Heart FailureDocument49 pagesChapter 6 Care of The Patient Experiencing Shock or Heart FailureJennifer KellerNo ratings yet
- Textbook ReadingDocument275 pagesTextbook ReadingNovitasari EkaNo ratings yet
- Using The ACLS Primary Survey For A Patient in Respiratory ArrestDocument34 pagesUsing The ACLS Primary Survey For A Patient in Respiratory Arrest강기연100% (1)
- ABCDEF Bundle WebcastDocument42 pagesABCDEF Bundle WebcastsoulstakersNo ratings yet
- Sirs & ModsDocument5 pagesSirs & Modsmarlou agananNo ratings yet
- ST ND RD THDocument8 pagesST ND RD THLuvleen KaurNo ratings yet
- Nursing Pharmacology (Chapter 1 - Introduction)Document1 pageNursing Pharmacology (Chapter 1 - Introduction)Jemima GasconNo ratings yet
- Pre Hos TraumaDocument11 pagesPre Hos TraumaGel OmugtongNo ratings yet
- 01 - Decision Making in Emergency MedicineDocument4 pages01 - Decision Making in Emergency MedicineSlvdrPlgrnNo ratings yet
- Avoiding Common Errors in The Emergency Department-1002-1280Document280 pagesAvoiding Common Errors in The Emergency Department-1002-1280Hernando CastrillónNo ratings yet
- Emergency Ortho BCS 2017Document80 pagesEmergency Ortho BCS 2017Priza Razunip100% (1)
- Hypertonic Saline and Mannitol Therapy in Critical Care NeurologyDocument9 pagesHypertonic Saline and Mannitol Therapy in Critical Care NeurologyRonAlNo ratings yet
- Medical Surgical Nursing Mnemonics and TipsDocument36 pagesMedical Surgical Nursing Mnemonics and TipsAniki OniiNo ratings yet
- Nursing Pharma (Chapter 2 - Pharmaco & Pharmady)Document1 pageNursing Pharma (Chapter 2 - Pharmaco & Pharmady)Jemima GasconNo ratings yet
- Brain Sheet2011Document1 pageBrain Sheet2011nursekatieNo ratings yet
- FundamentalsDocument115 pagesFundamentalsMichelle Dona MirallesNo ratings yet
- Family Medicine M3 Clerkship Hypertensive Disorders: Joy Shen-Wagner MDDocument35 pagesFamily Medicine M3 Clerkship Hypertensive Disorders: Joy Shen-Wagner MDJT Thomas100% (1)
- MED 1.17 - Gastrointestinal CancersDocument6 pagesMED 1.17 - Gastrointestinal CancersZazaNo ratings yet
- Therapeutic Hypothermia ChillOutDocument38 pagesTherapeutic Hypothermia ChillOutJason RodmanNo ratings yet
- Prehospital Anesthesia HandbookDocument46 pagesPrehospital Anesthesia HandbookoscarNo ratings yet
- Cardiovascular System: By: Marc Anthony Liao RNDocument59 pagesCardiovascular System: By: Marc Anthony Liao RNloveseeker06No ratings yet
- ANTIBIOTICS Pharmacology NursingDocument10 pagesANTIBIOTICS Pharmacology NursingRalph Alfonse De JesusNo ratings yet
- Assessment of The Chest and LungsDocument46 pagesAssessment of The Chest and LungsSumathi GopinathNo ratings yet
- Pharmacology Quick HitsDocument6 pagesPharmacology Quick HitsHuma Hameed DogarNo ratings yet
- Empress' Dragoons Officer Part 1Document34 pagesEmpress' Dragoons Officer Part 1Luca de Fabbris100% (1)
- 7 Suggestions Paramedic Airway ANAM22 WMDocument5 pages7 Suggestions Paramedic Airway ANAM22 WMcedivadeniaNo ratings yet
- Pharmacology Midterm TestDocument19 pagesPharmacology Midterm Testmarie curryNo ratings yet
- Management of ArrhythmiasDocument4 pagesManagement of ArrhythmiasAray Al-AfiqahNo ratings yet
- Senior Center StudyDocument117 pagesSenior Center StudyIulian TNo ratings yet
- Emergency MnemonicDocument5 pagesEmergency Mnemonicanon_549623261No ratings yet
- Sepsis Quick Reference GuideDocument1 pageSepsis Quick Reference GuideRavin DebieNo ratings yet
- Anatomy RespDocument57 pagesAnatomy RespGunawan SamosirNo ratings yet
- Heart Failure Express Card HMCDocument2 pagesHeart Failure Express Card HMCalexNo ratings yet
- Ventilator Modes - WEANINGDocument3 pagesVentilator Modes - WEANINGAlaa OmarNo ratings yet
- Basic Drug Computations Part 1Document8 pagesBasic Drug Computations Part 1Carl Elexer Cuyugan Ano100% (4)
- Nursing CS Angina-Pectoris-medications 03Document1 pageNursing CS Angina-Pectoris-medications 03Mahdia akterNo ratings yet
- Neonatal SkinDocument384 pagesNeonatal SkinErnestas ViršilasNo ratings yet
- Calc Drip Rates 2Document2 pagesCalc Drip Rates 2Charisse Nicole DiazNo ratings yet
- Print Foundations - Fundamentals of Nursing, Chapter 48 Skin Integrity and Wound Care Flashcards - Easy NotecardsDocument6 pagesPrint Foundations - Fundamentals of Nursing, Chapter 48 Skin Integrity and Wound Care Flashcards - Easy NotecardsMark M. AlipioNo ratings yet
- Maternal Medications - Uterotonic (Induction/Augmentation of Labor And/or Prevention/Treatment of Hemorrhage)Document19 pagesMaternal Medications - Uterotonic (Induction/Augmentation of Labor And/or Prevention/Treatment of Hemorrhage)SariahNo ratings yet
- ASIA International Standards For Neurological Classification of Spinal Cord InjuryDocument2 pagesASIA International Standards For Neurological Classification of Spinal Cord InjuryMicah Tagle100% (1)
- Philosophy of NursingDocument8 pagesPhilosophy of Nursingapi-430575435No ratings yet
- Med Surg BurnsDocument8 pagesMed Surg BurnsawuahbohNo ratings yet
- Community Acquired Pneumonia CAP 1.28.21Document1 pageCommunity Acquired Pneumonia CAP 1.28.21Illaizah EdictoNo ratings yet
- ICU One Pager Massive Hemoptysis v11Document1 pageICU One Pager Massive Hemoptysis v11Nicholas HelmstetterNo ratings yet
- ICU One Pager NIPPVDocument1 pageICU One Pager NIPPVNicholas HelmstetterNo ratings yet
- Guide Beer Flavor Zymurgy-1987 PDFDocument21 pagesGuide Beer Flavor Zymurgy-1987 PDFNicholas HelmstetterNo ratings yet
- ICU One Pager Abdominal Compartment SyndromeDocument1 pageICU One Pager Abdominal Compartment SyndromeNicholas HelmstetterNo ratings yet
- Blood Flow Q: The Transmembrane Pressure (TMP) GradientDocument1 pageBlood Flow Q: The Transmembrane Pressure (TMP) GradientNicholas HelmstetterNo ratings yet
- ICU One Pager Lactic AcidosisDocument1 pageICU One Pager Lactic AcidosisNicholas Helmstetter100% (1)
- ICU One Pager Minnesota TubeDocument1 pageICU One Pager Minnesota TubeNicholas HelmstetterNo ratings yet
- 1001 Songs You Must Hear Before You Die 27526Document7 pages1001 Songs You Must Hear Before You Die 27526Nicholas HelmstetterNo ratings yet
- Movesets)Document158 pagesMovesets)Nicholas HelmstetterNo ratings yet
- How To... Select Multiple Values in A Dropdown BoxDocument15 pagesHow To... Select Multiple Values in A Dropdown Boxkalicharan13No ratings yet
- Allowable Span/Depth Ratio For High Strength Concrete BeamsDocument1 pageAllowable Span/Depth Ratio For High Strength Concrete BeamsbagmassNo ratings yet
- Chemical NamesDocument4 pagesChemical NamesSomesubhraDasNo ratings yet
- Lecture Notes 11-Euler Method-IIDocument59 pagesLecture Notes 11-Euler Method-IITesfaye Teferi ShoneNo ratings yet
- Garat2015 PDFDocument7 pagesGarat2015 PDFmanojkumarNo ratings yet
- MS, TMT, CTDDocument5 pagesMS, TMT, CTDAbdul BasitNo ratings yet
- Analyze Phase Workbook - FinalDocument151 pagesAnalyze Phase Workbook - FinalNicola100% (1)
- Chapter 2 (Electrostatic Potential and Capacitance) UnsolvedDocument8 pagesChapter 2 (Electrostatic Potential and Capacitance) UnsolvedMahendra ShahNo ratings yet
- Nemo Windcatcher: Industry-Leading Drive Test Data Post-Processing and AnalysisDocument2 pagesNemo Windcatcher: Industry-Leading Drive Test Data Post-Processing and AnalysistreejumboNo ratings yet
- Coleman RV 12 Volt Thermistat ACDocument18 pagesColeman RV 12 Volt Thermistat ACsthoma20100% (1)
- Electrical Protections: Presentation byDocument34 pagesElectrical Protections: Presentation bydjfffNo ratings yet
- NCP1002Document14 pagesNCP1002Ailton De JesusNo ratings yet
- 3 2systems AlgDocument20 pages3 2systems AlgSyeda Saman Zahra Zaidi/TCHR/GBFNo ratings yet
- Indefinite IntegralDocument18 pagesIndefinite IntegralMA LEAH I ABADNo ratings yet
- Pemanfaatan Ilmu Fisika Terhadap PeternakanDocument15 pagesPemanfaatan Ilmu Fisika Terhadap PeternakanSinta Sri RahayuNo ratings yet
- Fluidtecq Fluidtecq Fluidtecq Fluidtecq: Operation and Maintenance ManualDocument12 pagesFluidtecq Fluidtecq Fluidtecq Fluidtecq: Operation and Maintenance ManualmehtahemalNo ratings yet
- ESDU BrochureDocument3 pagesESDU BrochureWilhelm ThorleyNo ratings yet
- PRU Assembly Instruction User GuideDocument50 pagesPRU Assembly Instruction User GuideJános JuhászNo ratings yet
- Bateria Sellada Agm Marca Magna Acceso Frontal 12v-150ah (Maf150-12)Document2 pagesBateria Sellada Agm Marca Magna Acceso Frontal 12v-150ah (Maf150-12)SOLUCIONES ENERGETICAS Y PROCESOS INNOVADORESNo ratings yet
- AnaDev - Building A Homebrew Load BoxDocument3 pagesAnaDev - Building A Homebrew Load BoxciccioNo ratings yet
- Appnote Operating SPL PLXX 03112004Document5 pagesAppnote Operating SPL PLXX 03112004interconnectfast4No ratings yet
- اسئلة كتاب البروتينات والاجبات -Document41 pagesاسئلة كتاب البروتينات والاجبات -Youssef AliNo ratings yet
- LegTech ReviewerDocument9 pagesLegTech ReviewerMaris Cay0% (1)
- Ch04Exp PDFDocument17 pagesCh04Exp PDFConstantin PopescuNo ratings yet
- Microbial NutritionDocument12 pagesMicrobial NutritionJosé Molineros100% (2)
- Generic Earth Directional Relay Io Dir, Io Dir (IOC, UMZ) RelayDocument2 pagesGeneric Earth Directional Relay Io Dir, Io Dir (IOC, UMZ) Relaybauhaus10No ratings yet
- Features Descriptio: Lt3503 1A, 2.2Mhz Step-Down Switching Regulator in 2Mm × 3Mm DFNDocument20 pagesFeatures Descriptio: Lt3503 1A, 2.2Mhz Step-Down Switching Regulator in 2Mm × 3Mm DFNBrett HufnagleNo ratings yet
- DSE Leaflet 22-23 Final - 0Document2 pagesDSE Leaflet 22-23 Final - 0NisAr AhmadNo ratings yet