Professional Documents
Culture Documents
Hepatopulmonary
Hepatopulmonary
Uploaded by
ademato4real576Copyright:
Available Formats
You might also like
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtFrom EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtRating: 5 out of 5 stars5/5 (1)
- Pulmonary HypertensionDocument63 pagesPulmonary HypertensionChrishan Shivanthan100% (4)
- Management of Cyanotic Child BivinDocument48 pagesManagement of Cyanotic Child BivinChippy BivinNo ratings yet
- 8) Chronic Cor PulmonaleDocument2 pages8) Chronic Cor PulmonaleAris PaparisNo ratings yet
- Pulmonary HypertensionDocument36 pagesPulmonary HypertensionDiana_anca6100% (2)
- COR PULMONALE - MahasiswaDocument14 pagesCOR PULMONALE - MahasiswaGalih Maygananda PutraNo ratings yet
- Resp 180214084710Document72 pagesResp 180214084710Karla Geraldine Carhuas VeliNo ratings yet
- Pulmonary HTNDocument59 pagesPulmonary HTNapi-3757039No ratings yet
- Cor PulmonaleDocument27 pagesCor PulmonaleumapathisivanNo ratings yet
- 10 1016@j CCL 2020 04 008Document12 pages10 1016@j CCL 2020 04 008Linda Silvana SariNo ratings yet
- Resp N41Document11 pagesResp N41ashafernandesssNo ratings yet
- HAP Pulmonar 19Document106 pagesHAP Pulmonar 19jorge corolla montesNo ratings yet
- HTPAnnals 2005Document12 pagesHTPAnnals 2005api-3703544No ratings yet
- Cardiology Notes by Wasim AhmadDocument28 pagesCardiology Notes by Wasim AhmadAshna moeenNo ratings yet
- Primary Pulmonary Hypertension: A Case ReportDocument4 pagesPrimary Pulmonary Hypertension: A Case ReportaknbdgNo ratings yet
- Respiratory Failure Workup: Approach ConsiderationsDocument8 pagesRespiratory Failure Workup: Approach Considerationsjeanie mae PangapalanNo ratings yet
- 1 FullDocument4 pages1 FullMuli YamanNo ratings yet
- Pulmonary Embolism: DR A Hammangabdo Fwacp Professor and Cosultant PulmonologistDocument28 pagesPulmonary Embolism: DR A Hammangabdo Fwacp Professor and Cosultant PulmonologistAdamu Muhammad Dumbulwa100% (1)
- SDL 19 Cor Pulmonale - BMS16091064Document6 pagesSDL 19 Cor Pulmonale - BMS16091064Jonathan YeohNo ratings yet
- Cor PulmonaleDocument62 pagesCor PulmonaleAlbert NixonNo ratings yet
- Dyspnoea 2Document1 pageDyspnoea 2Shubham TarapureNo ratings yet
- Ratheesh R.LDocument23 pagesRatheesh R.LvaishnaviNo ratings yet
- KP 2.5.5.3 Cor PulmonaleDocument17 pagesKP 2.5.5.3 Cor Pulmonalenurul ramadhiniNo ratings yet
- Acute Pulmonary OedemaDocument4 pagesAcute Pulmonary OedemaTze SiangNo ratings yet
- Pulmo HPNDocument36 pagesPulmo HPNAlexander Santiago ParelNo ratings yet
- Jurnal FisioDocument8 pagesJurnal Fisiorizkya amanahNo ratings yet
- Css JantungDocument12 pagesCss JantungRegi FauzanNo ratings yet
- Respiratory FaillureDocument45 pagesRespiratory FaillureRika AmaliyaNo ratings yet
- Cor PulmonaleDocument8 pagesCor PulmonaleAymen OmerNo ratings yet
- Pulmonary Hypertension: and Its Implications For AnaesthesiaDocument31 pagesPulmonary Hypertension: and Its Implications For AnaesthesiaMay LeongNo ratings yet
- Cor PulmonaleDocument3 pagesCor PulmonaleKhalid Mahmud ArifinNo ratings yet
- AJAB CAR Pulmonary HypertensionDocument51 pagesAJAB CAR Pulmonary HypertensionAjabsingh ChoudharyNo ratings yet
- Dr. Adel Hamada: Chest Diseases SymptomsDocument20 pagesDr. Adel Hamada: Chest Diseases SymptomsAdel HamadaNo ratings yet
- Pulmonary EmbolismDocument21 pagesPulmonary EmbolismChoga Ilham ArlandoNo ratings yet
- Neonatal Central CyanosisDocument4 pagesNeonatal Central CyanosisRosdiana Elizabeth SiburianNo ratings yet
- CastroDocument17 pagesCastrongoto88No ratings yet
- CorpulmonalefinalDocument37 pagesCorpulmonalefinalRay ReyesNo ratings yet
- PJ KritikalDocument38 pagesPJ KritikalnafisyarifahNo ratings yet
- Pulmonary HypertensionDocument10 pagesPulmonary HypertensionCkaye GansubinNo ratings yet
- CG VM Management of ARDSDocument31 pagesCG VM Management of ARDSVishnu ManglaNo ratings yet
- Cor Pulmonale IkaDocument19 pagesCor Pulmonale IkaIka Lukita SariNo ratings yet
- Case - 3Document20 pagesCase - 3abhiNo ratings yet
- Cardiopatias CianoticasDocument9 pagesCardiopatias CianoticasAngie CalderónNo ratings yet
- Approach To DyspneaDocument9 pagesApproach To DyspneaMuhammad LukmanNo ratings yet
- Acute Heart FailureDocument9 pagesAcute Heart FailureChen Briones100% (1)
- Cor Pulmonal and CHDDocument44 pagesCor Pulmonal and CHDamir iksanNo ratings yet
- Acute Respiratory FailureDocument8 pagesAcute Respiratory FailureCayunk NorlianaNo ratings yet
- P EmbolismDocument29 pagesP EmbolismCommandoCitotz100% (2)
- Approach To The Patient With Shortness of Breath: Colin EdwardsDocument37 pagesApproach To The Patient With Shortness of Breath: Colin EdwardsNur FadzilahNo ratings yet
- Pulmonary HypertensionDocument27 pagesPulmonary Hypertensionantonello picernoNo ratings yet
- Pulmonary Hypertension: 1. Identify Pulmonary Hypertension 2. Apply Required Collaborative and Nursing Care PlanDocument14 pagesPulmonary Hypertension: 1. Identify Pulmonary Hypertension 2. Apply Required Collaborative and Nursing Care PlanJeffrey KauvaNo ratings yet
- Pulmonary and Critical Care Medicine In-Training ObjectivesDocument12 pagesPulmonary and Critical Care Medicine In-Training ObjectiveshectorNo ratings yet
- Dypsnea - RevisedDocument19 pagesDypsnea - RevisedPrincella MonicaNo ratings yet
- Heart FailureDocument2 pagesHeart FailureDavid J. HernstadtNo ratings yet
- Bullets in Medical Surgical NursingDocument59 pagesBullets in Medical Surgical NursingDonna UyNo ratings yet
- Kuliah 16 Cor PulmonaleDocument41 pagesKuliah 16 Cor PulmonalecaturwiraNo ratings yet
- Pulmonary ThromboembolismDocument4 pagesPulmonary ThromboembolismValerrie NgenoNo ratings yet
- Cyanosis in The NewbornDocument32 pagesCyanosis in The Newbornimma_2014No ratings yet
- Diagram Myoma IIIDocument1 pageDiagram Myoma IIIJoann100% (2)
- Tetanus: Dr. Zubaida AimalDocument31 pagesTetanus: Dr. Zubaida AimalkhanmoinNo ratings yet
- Morning Report RakaDocument19 pagesMorning Report Rakaraka widhiartaNo ratings yet
- Candidiasis IDSA 2016Document23 pagesCandidiasis IDSA 2016Shihan HuqNo ratings yet
- VaccineDocument1 pageVaccinexmitchxNo ratings yet
- Discussion TextDocument1 pageDiscussion Textsamuel gunawanNo ratings yet
- Retinopati Diabetikum: Arso Pranindyo UtomoDocument14 pagesRetinopati Diabetikum: Arso Pranindyo Utomosusilo hadi wNo ratings yet
- 4.cough and Difficulty of BreathingDocument52 pages4.cough and Difficulty of BreathingLunaLureNo ratings yet
- Source VDocument2 pagesSource VArmelle HoungangNo ratings yet
- Reviewer - 1. Introduction To ZoonosesDocument4 pagesReviewer - 1. Introduction To ZoonosesGeriel QuidesNo ratings yet
- Infectious Diseases IIDocument57 pagesInfectious Diseases IIAhmad MakhloufNo ratings yet
- Feline PanleukopeniaDocument30 pagesFeline PanleukopeniaRenny BarriosNo ratings yet
- Screening IndustryDocument2 pagesScreening Industryrahaman.maNo ratings yet
- "Association Splitting" Versus Cognitive Remediation in Obsessive-Compulsive Disorder - A Randomized Controlled TrialDocument39 pages"Association Splitting" Versus Cognitive Remediation in Obsessive-Compulsive Disorder - A Randomized Controlled Trialmahashweta bhattacharyaNo ratings yet
- Public Health & Preventive Medicine - Toronto Notes 2022Document35 pagesPublic Health & Preventive Medicine - Toronto Notes 2022AbdullaNo ratings yet
- Green Book FinalDocument115 pagesGreen Book Finalechspckhammam pcNo ratings yet
- CHF LapsusDocument27 pagesCHF Lapsuseno46No ratings yet
- Thesis Title Role of Guidelines For Pregnant Women On Malaria Prevention and TreatmentDocument6 pagesThesis Title Role of Guidelines For Pregnant Women On Malaria Prevention and TreatmentPhillip TaylorNo ratings yet
- Enveloped and Non Enveloped VirusDocument10 pagesEnveloped and Non Enveloped ViruspixholicNo ratings yet
- Editor's Note: V Rama Med J Vol.43 No.1 January - March 2020Document2 pagesEditor's Note: V Rama Med J Vol.43 No.1 January - March 2020benznakupNo ratings yet
- Infection Control Assesment ToolDocument276 pagesInfection Control Assesment ToolHanan AhmedNo ratings yet
- UrosepsisDocument35 pagesUrosepsisdrasas690No ratings yet
- 2023-24 Community As ClientDocument81 pages2023-24 Community As Client7vjkgkw29xNo ratings yet
- First PrelimsDocument17 pagesFirst PrelimsLaish Christle CapiendoNo ratings yet
- Non Gynae CytologyDocument32 pagesNon Gynae CytologyfadoNo ratings yet
- 200-Article Text-744-1-10-20190121 PDFDocument4 pages200-Article Text-744-1-10-20190121 PDFJodi BoritnabanNo ratings yet
- Introduction To ParasitologyDocument2 pagesIntroduction To ParasitologyRomie SolacitoNo ratings yet
- Standard Precautions - Appendix A - Isolation Precautions - Guidelines Library - Infection Control - CDCDocument2 pagesStandard Precautions - Appendix A - Isolation Precautions - Guidelines Library - Infection Control - CDCKomite PPI RSUDPCNo ratings yet
- Graphic Organiser FactorDocument2 pagesGraphic Organiser FactorRogini SindhuNo ratings yet
- Newborn RashDocument20 pagesNewborn RashshamaaroubaNo ratings yet
Hepatopulmonary
Hepatopulmonary
Uploaded by
ademato4real576Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hepatopulmonary
Hepatopulmonary
Uploaded by
ademato4real576Copyright:
Available Formats
SJS Sept-03
HEPATOPULMONARY SYNDROME
Aboussouan LS, Stoller JK. The hepatopulmonary syndrome.
Baillieres Best Pract Res Clin Gastroenterol. 2000 Dec;14(6):1033-48.
Take home points:
1. Don’t confuse hepatopulmonary syndrome (shunting and V/Q mismatch due to arteriovenous malformations
in the lung) with portopulmonary hypertension (the development of pulmonary hypertension in a cirrhotic
patient with portal hypertension).
2. Look for platypnea and orthodeoxia; however, patients may be asymptomatic with only hypoxemia as a
clue.
3. Treatment = lung transplantation which cures hepatopulmonary syndrome in 80% of patients. However,
resolution can take up to 14 months.
Definition: look for the triad of liver disease, increased A-a gradient, and evidence of intrapulmonary vascular dilitations.
• Note that the liver dysfunction need not be severe.
• Intrinsic cardiopulmonary disease must be excluded.
• Pleural effusions and airflow obstruction can co-exist with the hepatopulmonary syndrome.
Clinical features:
• 8% of cirrhotics manifest true clinical features of the hepatopulmonary syndrome (PaO2 < 60 mmHg).
• The patient may be asymptomatic (only 18% have dyspnea). Look for hypoxemia which can lead to
clubbing and cyanosis.
• Platypnea: the opposite of orthopnea. Dyspnea improves when lying flat.
• Orthodeoxia: hypoxemia worsens upon sitting up and improves when lying flat.
• Platypnea and orthodeoxia occur because the pulmonary AVMs occur predominantly in the bases of the
lung. Therefore, when sitting up or standing, blood pools at the bases of the lung with resultant
increased AV shunting.
Pathophysiology:
• Hypoxemia due to intrapulmonary vascular abnormalities akin to spider angiomata found on skin of
cirrhotics. This leads to AV shunting and V/Q mismatch.
• Note: unlike intracardiac shunting, 100% oxygen will (at least partially) correct the hypoxemia because
shunting is not the only factor leading to low oxygen saturation. Dilated vasculature also leads to
hypoxemia because of diffusion impairment. Increasing the oxygen level can overcome this problem.
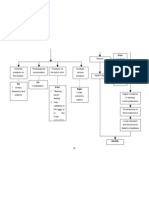
Hepatopulmonary syndrome (HPS) vs. portopulmonary hypertension (PPHTN):
HPS PPHTN
Pathophysiology Arteriovenous (AV) shunting in the lung, Similar to primary pulmonary hypertension
predominantly at the bases. “Spider with intense vasoconstriction of pulmonary
angiomata” in the lung. capillaries as well as remodeled, thickened
pulmonary vasculature
Symptoms Platypnea Dyspnea on exertion, syncope, orthopnea
Physical findings Hypoxemia, orthodeoxia Loud P2, RV heave, TR murmur,
hypoxemia worsens with exercise (normal
O2 saturation at rest is common)
Echocardiogram Positive bubble study Elevated pulmonary artery systolic pressure
Treatment Liver transplantation Same as primary pulmonary hypertension;
if mean PAP < 40 mmHg, can safely
undergo liver transplantation.
You might also like
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtFrom EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtRating: 5 out of 5 stars5/5 (1)
- Pulmonary HypertensionDocument63 pagesPulmonary HypertensionChrishan Shivanthan100% (4)
- Management of Cyanotic Child BivinDocument48 pagesManagement of Cyanotic Child BivinChippy BivinNo ratings yet
- 8) Chronic Cor PulmonaleDocument2 pages8) Chronic Cor PulmonaleAris PaparisNo ratings yet
- Pulmonary HypertensionDocument36 pagesPulmonary HypertensionDiana_anca6100% (2)
- COR PULMONALE - MahasiswaDocument14 pagesCOR PULMONALE - MahasiswaGalih Maygananda PutraNo ratings yet
- Resp 180214084710Document72 pagesResp 180214084710Karla Geraldine Carhuas VeliNo ratings yet
- Pulmonary HTNDocument59 pagesPulmonary HTNapi-3757039No ratings yet
- Cor PulmonaleDocument27 pagesCor PulmonaleumapathisivanNo ratings yet
- 10 1016@j CCL 2020 04 008Document12 pages10 1016@j CCL 2020 04 008Linda Silvana SariNo ratings yet
- Resp N41Document11 pagesResp N41ashafernandesssNo ratings yet
- HAP Pulmonar 19Document106 pagesHAP Pulmonar 19jorge corolla montesNo ratings yet
- HTPAnnals 2005Document12 pagesHTPAnnals 2005api-3703544No ratings yet
- Cardiology Notes by Wasim AhmadDocument28 pagesCardiology Notes by Wasim AhmadAshna moeenNo ratings yet
- Primary Pulmonary Hypertension: A Case ReportDocument4 pagesPrimary Pulmonary Hypertension: A Case ReportaknbdgNo ratings yet
- Respiratory Failure Workup: Approach ConsiderationsDocument8 pagesRespiratory Failure Workup: Approach Considerationsjeanie mae PangapalanNo ratings yet
- 1 FullDocument4 pages1 FullMuli YamanNo ratings yet
- Pulmonary Embolism: DR A Hammangabdo Fwacp Professor and Cosultant PulmonologistDocument28 pagesPulmonary Embolism: DR A Hammangabdo Fwacp Professor and Cosultant PulmonologistAdamu Muhammad Dumbulwa100% (1)
- SDL 19 Cor Pulmonale - BMS16091064Document6 pagesSDL 19 Cor Pulmonale - BMS16091064Jonathan YeohNo ratings yet
- Cor PulmonaleDocument62 pagesCor PulmonaleAlbert NixonNo ratings yet
- Dyspnoea 2Document1 pageDyspnoea 2Shubham TarapureNo ratings yet
- Ratheesh R.LDocument23 pagesRatheesh R.LvaishnaviNo ratings yet
- KP 2.5.5.3 Cor PulmonaleDocument17 pagesKP 2.5.5.3 Cor Pulmonalenurul ramadhiniNo ratings yet
- Acute Pulmonary OedemaDocument4 pagesAcute Pulmonary OedemaTze SiangNo ratings yet
- Pulmo HPNDocument36 pagesPulmo HPNAlexander Santiago ParelNo ratings yet
- Jurnal FisioDocument8 pagesJurnal Fisiorizkya amanahNo ratings yet
- Css JantungDocument12 pagesCss JantungRegi FauzanNo ratings yet
- Respiratory FaillureDocument45 pagesRespiratory FaillureRika AmaliyaNo ratings yet
- Cor PulmonaleDocument8 pagesCor PulmonaleAymen OmerNo ratings yet
- Pulmonary Hypertension: and Its Implications For AnaesthesiaDocument31 pagesPulmonary Hypertension: and Its Implications For AnaesthesiaMay LeongNo ratings yet
- Cor PulmonaleDocument3 pagesCor PulmonaleKhalid Mahmud ArifinNo ratings yet
- AJAB CAR Pulmonary HypertensionDocument51 pagesAJAB CAR Pulmonary HypertensionAjabsingh ChoudharyNo ratings yet
- Dr. Adel Hamada: Chest Diseases SymptomsDocument20 pagesDr. Adel Hamada: Chest Diseases SymptomsAdel HamadaNo ratings yet
- Pulmonary EmbolismDocument21 pagesPulmonary EmbolismChoga Ilham ArlandoNo ratings yet
- Neonatal Central CyanosisDocument4 pagesNeonatal Central CyanosisRosdiana Elizabeth SiburianNo ratings yet
- CastroDocument17 pagesCastrongoto88No ratings yet
- CorpulmonalefinalDocument37 pagesCorpulmonalefinalRay ReyesNo ratings yet
- PJ KritikalDocument38 pagesPJ KritikalnafisyarifahNo ratings yet
- Pulmonary HypertensionDocument10 pagesPulmonary HypertensionCkaye GansubinNo ratings yet
- CG VM Management of ARDSDocument31 pagesCG VM Management of ARDSVishnu ManglaNo ratings yet
- Cor Pulmonale IkaDocument19 pagesCor Pulmonale IkaIka Lukita SariNo ratings yet
- Case - 3Document20 pagesCase - 3abhiNo ratings yet
- Cardiopatias CianoticasDocument9 pagesCardiopatias CianoticasAngie CalderónNo ratings yet
- Approach To DyspneaDocument9 pagesApproach To DyspneaMuhammad LukmanNo ratings yet
- Acute Heart FailureDocument9 pagesAcute Heart FailureChen Briones100% (1)
- Cor Pulmonal and CHDDocument44 pagesCor Pulmonal and CHDamir iksanNo ratings yet
- Acute Respiratory FailureDocument8 pagesAcute Respiratory FailureCayunk NorlianaNo ratings yet
- P EmbolismDocument29 pagesP EmbolismCommandoCitotz100% (2)
- Approach To The Patient With Shortness of Breath: Colin EdwardsDocument37 pagesApproach To The Patient With Shortness of Breath: Colin EdwardsNur FadzilahNo ratings yet
- Pulmonary HypertensionDocument27 pagesPulmonary Hypertensionantonello picernoNo ratings yet
- Pulmonary Hypertension: 1. Identify Pulmonary Hypertension 2. Apply Required Collaborative and Nursing Care PlanDocument14 pagesPulmonary Hypertension: 1. Identify Pulmonary Hypertension 2. Apply Required Collaborative and Nursing Care PlanJeffrey KauvaNo ratings yet
- Pulmonary and Critical Care Medicine In-Training ObjectivesDocument12 pagesPulmonary and Critical Care Medicine In-Training ObjectiveshectorNo ratings yet
- Dypsnea - RevisedDocument19 pagesDypsnea - RevisedPrincella MonicaNo ratings yet
- Heart FailureDocument2 pagesHeart FailureDavid J. HernstadtNo ratings yet
- Bullets in Medical Surgical NursingDocument59 pagesBullets in Medical Surgical NursingDonna UyNo ratings yet
- Kuliah 16 Cor PulmonaleDocument41 pagesKuliah 16 Cor PulmonalecaturwiraNo ratings yet
- Pulmonary ThromboembolismDocument4 pagesPulmonary ThromboembolismValerrie NgenoNo ratings yet
- Cyanosis in The NewbornDocument32 pagesCyanosis in The Newbornimma_2014No ratings yet
- Diagram Myoma IIIDocument1 pageDiagram Myoma IIIJoann100% (2)
- Tetanus: Dr. Zubaida AimalDocument31 pagesTetanus: Dr. Zubaida AimalkhanmoinNo ratings yet
- Morning Report RakaDocument19 pagesMorning Report Rakaraka widhiartaNo ratings yet
- Candidiasis IDSA 2016Document23 pagesCandidiasis IDSA 2016Shihan HuqNo ratings yet
- VaccineDocument1 pageVaccinexmitchxNo ratings yet
- Discussion TextDocument1 pageDiscussion Textsamuel gunawanNo ratings yet
- Retinopati Diabetikum: Arso Pranindyo UtomoDocument14 pagesRetinopati Diabetikum: Arso Pranindyo Utomosusilo hadi wNo ratings yet
- 4.cough and Difficulty of BreathingDocument52 pages4.cough and Difficulty of BreathingLunaLureNo ratings yet
- Source VDocument2 pagesSource VArmelle HoungangNo ratings yet
- Reviewer - 1. Introduction To ZoonosesDocument4 pagesReviewer - 1. Introduction To ZoonosesGeriel QuidesNo ratings yet
- Infectious Diseases IIDocument57 pagesInfectious Diseases IIAhmad MakhloufNo ratings yet
- Feline PanleukopeniaDocument30 pagesFeline PanleukopeniaRenny BarriosNo ratings yet
- Screening IndustryDocument2 pagesScreening Industryrahaman.maNo ratings yet
- "Association Splitting" Versus Cognitive Remediation in Obsessive-Compulsive Disorder - A Randomized Controlled TrialDocument39 pages"Association Splitting" Versus Cognitive Remediation in Obsessive-Compulsive Disorder - A Randomized Controlled Trialmahashweta bhattacharyaNo ratings yet
- Public Health & Preventive Medicine - Toronto Notes 2022Document35 pagesPublic Health & Preventive Medicine - Toronto Notes 2022AbdullaNo ratings yet
- Green Book FinalDocument115 pagesGreen Book Finalechspckhammam pcNo ratings yet
- CHF LapsusDocument27 pagesCHF Lapsuseno46No ratings yet
- Thesis Title Role of Guidelines For Pregnant Women On Malaria Prevention and TreatmentDocument6 pagesThesis Title Role of Guidelines For Pregnant Women On Malaria Prevention and TreatmentPhillip TaylorNo ratings yet
- Enveloped and Non Enveloped VirusDocument10 pagesEnveloped and Non Enveloped ViruspixholicNo ratings yet
- Editor's Note: V Rama Med J Vol.43 No.1 January - March 2020Document2 pagesEditor's Note: V Rama Med J Vol.43 No.1 January - March 2020benznakupNo ratings yet
- Infection Control Assesment ToolDocument276 pagesInfection Control Assesment ToolHanan AhmedNo ratings yet
- UrosepsisDocument35 pagesUrosepsisdrasas690No ratings yet
- 2023-24 Community As ClientDocument81 pages2023-24 Community As Client7vjkgkw29xNo ratings yet
- First PrelimsDocument17 pagesFirst PrelimsLaish Christle CapiendoNo ratings yet
- Non Gynae CytologyDocument32 pagesNon Gynae CytologyfadoNo ratings yet
- 200-Article Text-744-1-10-20190121 PDFDocument4 pages200-Article Text-744-1-10-20190121 PDFJodi BoritnabanNo ratings yet
- Introduction To ParasitologyDocument2 pagesIntroduction To ParasitologyRomie SolacitoNo ratings yet
- Standard Precautions - Appendix A - Isolation Precautions - Guidelines Library - Infection Control - CDCDocument2 pagesStandard Precautions - Appendix A - Isolation Precautions - Guidelines Library - Infection Control - CDCKomite PPI RSUDPCNo ratings yet
- Graphic Organiser FactorDocument2 pagesGraphic Organiser FactorRogini SindhuNo ratings yet
- Newborn RashDocument20 pagesNewborn RashshamaaroubaNo ratings yet