Professional Documents
Culture Documents
Implant Esthetics: Review Article
Implant Esthetics: Review Article
Uploaded by
Sahana RangarajanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Implant Esthetics: Review Article
Implant Esthetics: Review Article
Uploaded by
Sahana RangarajanCopyright:
Available Formats
Review Article
Implant esthetics
Ritu Batra, mds*, Sanjay Kalra, mds**, Hemant Batra, mds†
*Senior Lecturer, **Principal and Head, Department of Prosthodontics, BRS Dental College and Hospital, Sultanpur, Panchkula, †Professor and Head,
Department of Oral and Maxillofacial Surgery, Dr HS Judge Institute of Dental Sciences, Punjab University, Chandigarh, India.
Abstract
The recent concepts of implant dentistry are not only to restore the function of mastication, but the newly applied surgical and prosthetic
techniques are enabling dentists to fulfill patients’ esthetic expectations as well. A diagnostic wax-up of planned final restoration is crucial
as it establishes the final goal toward which all treatment is directed. The esthetic restoration must possess a form that compliments the sur-
rounding tissues and facilitates proper plaque control and occlusal function. It often presents reconstructive and restorative challenges and
requires a comprehensive treatment plan. Implants used to replace missing teeth in the esthetic zone have many advantages ranging from
preservation of unrestored adjacent teeth, halting the resorption of edentulous spaces to provide support for the prosthesis. Advanced papilla
reconstruction procedures can enable the dentist in achieving the ultimate and most sophisticated goal of ideal esthetic restoration both in
anterior and in posterior regions of human dentition. Hence, this is helping patients smile with confidence and dignity.
Keywords: Abutments, emergence profile, implant esthetics
INTRODUCTION Scientific investigations have resulted in the formulation
and verification of a set of laws or principles of visual per-
In a population that is becoming increasingly aware of the ception. These provide a basis for an introduction to the ele-
benefits of esthetic surgery, implant dentistry is among the ments of esthetics that are part of essential and natural
most frequently requested procedures for both esthetic and beauty. These principles were first introduced to the dental
functional purposes. The recent concepts of implant den- fraternity by Richard E Lombardi1,6; by combining artistic
tistry are not restricted to the basic needs, but newly applied creativity with scientific discretion, an esthetically appeal-
surgical and prosthetic techniques are enabling dentists to ing smile window can emerge4,7:
approach patients’ esthetic expectations. The philosophy 1. Composition: The relationships existing between objects
behind successful esthetic implant restoration is restoration- made visible by contrasts in color, line, and texture is
driven implant placement. Thus, the restoration itself becomes called composition; it is the dental composition, dentofa-
immediately involved in the correct development of soft- cial composition, and facial composition.
tissue profile, similar to conventional prosthetic restoration in 2. Unity: It gives the different parts of the composition the
which the restoration on remaining tooth structure is involved effects of a whole, which can be
in soft-tissue support.1–3 A diagnostic wax-up of planned final (a) Static: As seen in inanimate objects such as snow-
restoration is crucial as it establishes the final goal toward flakes and crystals. They are passive and inert based
which all treatment is directed. The esthetic restoration must on a regular, repetitive pattern.
possess a form that compliments the surrounding tissues and (b) Dynamic: Active, living, and growing as in plants
facilitates proper plaque control and occlusal function.4,5 and animals.
It often presents reconstructive and restorative challenges 3. Cohesive and segregative forces:
and requires a comprehensive treatment plan. (a) Cohesive forces: Elements that tend to unify a com-
position, represented by elements arranged according
Correspondence: Ritu Batra, Senior Lecturer, Department of to a principle.
Prosthodontics, BRS Dental College and Hospital, Sultanpur, Panchkula, (b) Segregative forces: Elements that break the monotony
India. of the composition to provide a variety in the unity.
E-mail: ritubatra71@gmail.com
Received: 05.08.2011
These are required to make a design effective.
Accepted: 16.11.2011 Harmony depends on the equilibrium created by
doi: 10.1016/S0975-962X(12)60006-9 cohesive and segregative forces.
© 2012 Indian Journal of Dentistry. Published by Elsevier Ltd. 15
Batra, et al
4. Symmetry: The regularity in the arrangement of forces or interdental papillae and often a couple of millimeters of the
objects. free gingival margin.
(a) Horizontal/running: Occurs when a design contains
similar elements from left to right in a regular sequence. Low Lip Line
(b) Radiating: Occurs as a result of the design of objects
extending from a central point with the left and right Less than 75% of the anterior teeth are displayed. The inter-
sides being mirror images; it is used to create a posi- face between implant and restoration is hidden behind the
tive psychologic response. drape of the lip. Thus, it is not that critical.
5. Proportion and repeated ratio: It is the percentage or Once the perimeter has been defined and smile is designed
measure in its numerical determination. Various philoso- with harmony and symmetry, the esthetic workup should be
phers have desired to prove the hypothesis that beauty focused on matching the tooth in its most natural form, that
could also be expressed mathematically.8–11 is, shade (e.g. value, hue, and chroma), shape, surface, tex-
For example, ture, and luster of the restoration to that of the adjacent natu-
Golden proportion (Pythagoras): 1/1.618 = 0.618 ral teeth.13 The success or failure also depends on the
Beautiful proportion (Plato): 1/1.733 = 0.577 emergence profile—the transition zone from the top of the
6. Balance: The causative element must be moved toward implant shoulder through the soft-tissue to the margin area.
the line of forces or midline to relieve visual tension. An
opposite element must be introduced along the same line Diagnostic Keys for Predicting Peri-implant Esthetics
of forces to promote equilibrium.
7. Lines: The parallel relationship between two lines is the The ultimate aim is for the implant restoration to harmonize
most harmonious as it does not exhibit conflict com- with the frame of the smile, face, and more importantly the
monly used as the equals sign. The strongest psychologic individual. Treatment planning must address hard and soft-
relationship that lines can engender is a perpendicular tissue deficiencies and combine this with the precision in
relationship as a plus or a cross sign. implant placement. Only with this approach can implant res-
8. Dominance: Implies the presence of subsequent similar toration be undistinguished from the adjacent teeth. To more
elements. The stronger the subsequent element, the stron- accurately predict the peri-implant esthetic outcome before
ger the dominating element and more vigorous the com- removing a failing tooth, an understanding of five diagnostic
position will be. Color, shape, and lines are factors that keys (smile line, relative tooth position [implant position],
can create dominance. form and biotype of the periodontium, emergence profile,
This can be achieved by increasing the size of the tooth in and position of the osseous crest) are essential.14 The diag-
question, making it lighter or placing it forward.12 nostic keys are described below:
Smile Line: The ultimate esthetics at smile depends on the
UNDERSTANDING THE NORMAL ESTHETIC ZONE interplay among the three components of esthetic zone, that
is, the teeth, the lips, and the gingiva. It is the lip line which
The ultimate esthetics at smile depends on the interplay among in turn determines the extent of display of teeth and the
the three components of esthetic zone, that is, the teeth, the gums. Depending upon this, it is categorized whether a par-
lips, and the gingiva. It is the lip line which in turn deter- ticular smile has a high, medium, or a low lip line.
mines the extent of display of teeth and the gums depending A high smile line poses considerable challenges when
upon this; it is categorized whether a particular smile has a planning for implant supported restorations because the res-
high, medium, or a low lip line. toration and gingival tissues are completely displayed.
High Lip Line Relative Tooth Position (Implant Position): Dictates the
emergence profile of the tooth to be replaced. The apico-
A lip line is high, if it reveals the total cervico-incisal length coronal position of the implant should be evaluated in rela-
of the maxillary anterior teeth and a continuous band of gin- tion to the adjacent teeth. A hopeless tooth for extraction
giva. It is most critical during smiling, as patient exposes the should be orthodontically extruded to migrate the marginal
entire restoration, the restorative gingival frame, the implant gingiva coronally prior to extraction so that gingival level is
prosthetic interface, and the extent of soft-tissue below the in harmony and prevent metal display. Faciolingual defi-
inferior border of the upper lip. It becomes more demanding ciency in the labial bone can be either augmented with a
area to restore if lost in such patients. graft or implant can be placed more palatally with ovate
pontic so that the health of the facial free gingival margin
Medium Lip Line may be preserved. Mesiodistal deficiency in this dimension
can be addressed through the use of orthodontics, enamelo-
It reveals 75–100% of the maxillary anterior teeth and the plasty, or restorations, as there is likelihood that black tri-
interproximal gingiva. Teeth are entirely visible, along with angles may occur if there is discrepancy in this relation teeth
16 © Indian Journal of Dentistry 2012/Volume 3/Issue 1
Implant esthetics
with root proximity also possess very little interproximal Position of the Osseous Crest: Position of the crestal bone
bone; this thin bone creates a great risk of lateral resorption is a determining factor for implant placement as it deter-
which will decrease the vertical bone height. mines the soft-tissue architecture after healing.18,19 Pro-
fessional acceptance of implants in the esthetic zone can be
Form and Biotype of the Periodontium: Implants should increased with better presurgical planning guidelines, under-
be inserted keeping in mind the form (scalloped or straight) standing options in the diameter of implant fixtures, know-
of the periodontal structures. The type of periodontium or ing variety of abutments, ensuring better fit of the abutment
periodontal biotype should be determined before surgery as to the implant fixture, ensuing better placement of the fix-
it has got a direct bearing on the esthetics owing to factors tures accurately with surgical guides, using better techniques
like the display of metal through the gums, response to sur- for preparing the edentulous site and employing prosthetic
gical insult and filling up of interimplant/dental spaces. techniques to produce a highly esthetic final restoration.
Broadly, periodontal biotypes can be thin and translucent, Deficient alveolar crest width will require a bone aug-
scalloped and thick, opaque, and flat. mentation procedure to allow the implant to be placed in
The thin scalloped periodontium reacts to insult by reces- an ideal position. Mesiodistal space should be equal to the
sion, facially, and interproximally. This type of periodontium is contralateral tooth.18
more demanding and tends to recede after implant placement.1 Use of a diagnostic template highlights the proposed
Thick, opaque, and flat periodontium is dense, fibrotic gingival margin of the implant restoration. Measuring the
soft-tissue curtain of periodontium and a flat, thick underly- distance from the free gingival margin to the osseous crest
ing osseous form tends to be more forgiving and favorable prior to extraction is an important diagnostic predictor of the
for implant placement and health and integration of peri- anticipated final position of the free gingival margin.
implant tissues. The important diagnostic factor in the predictability of
A thick biotype is prone to pocket formation, whereas a the post-placement level of the papillae is the crestal bone of
thin biotype is prone to gingival recession following surgical the teeth adjacent to the edentulous site.19,20 It has been
manipulation. A study by Kan and colleagues in 2003 has shown that the papillae will predictably form and maintain
stated that the implant papilla may be maintained at or re- if the distance between the crest of the bone and the inter-
established to the normal level (4.5 mm from the underlying proximal contact area is 5 mm or less. Inadequate interim-
bone) with the thick biotype, but it can seldom be created plant spacing (<3 mm) may result in exaggerated bone loss
beyond 4 mm with the thin biotype. and increased distance from the proximal contact points to
the associated alveolar bone crests.15 This may result in
Emergence Profile: Implant restorations in the esthetic decreased papillary volume and accompanying ‘black tri-
zone should mimic the emergence profile (flat) of the natu- angles’ within the esthetic zone.
ral teeth. One method is by proper implant positioning and
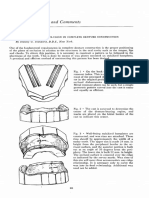
the use of a healing abutment or special gingival former with Implant Position: Mesiodistal position: The mesiodistal
coronal holes on which the flap is adapted at the desired position depends on the width of the coronal tooth to be
level with a single-knot suture. The second method is to use replaced; adjacent root proximity and the presence or absence
an ovate pontic or an acrylic resin restoration to sculpt the of diastema. It should approximate the position from which
gingival tissues. The third method is to employ a cervical the natural tooth originally emerged from the gingival sulcus.
contouring concept used in the case of an edentulous ridge, The mesiodistal implant axis should pass by the center of the
wherein cervical contouring is done on a model. Later, an future crown or the bisecting line angle of the adjacent roots.
acrylic resin crown is fabricated to fill the carved space A minimal mesiodistal, coronal, and radicular space must be
around the abutment and placed intra-orally to press against 1.5–2 mm from the root of the adjacent tooth (Figure 1).
the peri-implant soft-tissue to form the required emergence
profile. Moreover, the emergence profile of the final pros- Buccopalatal position: The body of the implant should be
thesis should be carefully created. If the profile is too nar- placed as far labially as the buccal bone allows. Orientation
row, no contralateral pressure or support for the gingiva will at 45° to the occlusal plane provides the best facial contour
exist, and the interdental papilla will diminish. If the profile and lip support and requires the fewest compromises in terms
is too wide, papillae will be vertically compressed, oral of oral hygiene and maintenance. The principle behind this
hygiene will be difficult or impossible to perform, and papil- requirement is that the implant angulations relates to the orig-
lae will collapse. The soft-tissue cast (gingival mimic) is inal tooth structure more than the original root of the tooth
used to finalize the emergence profile during the different and to some extent the type of restoration being planned
laboratory steps.12,15,16 Once this parameter has been defined (Figure 2).
and smile is designed with harmony and symmetry, the
esthetic workup should be focused on matching the tooth in Apico-coronal position: Implant can be placed 1.5–2 mm
its most natural form and profile, that is, shade (e.g. value, from cementoenamel junction (CEJ) of adjacent teeth, if
hue, and chroma), shape, surface, texture, and luster of the there is no gingival recession for better emergence profile
restoration to that of the adjacent natural teeth.17 and to accommodate the abutment and porcelain restoration
© Indian Journal of Dentistry 2012/Volume 3/Issue 1 17
Batra, et al
edentulous ridge because the abutment screw access needs
to be in the cingulum area to avoid the incisal edge and
facial aspect of the restoration. This palatal placement of
implant will lead to either a ridge-lap on the labial aspect of
the restoration or to more apical placement, which results in
a deeper peri-implant sulcus. Therefore, in most cases, ideal
implant placement in nonresorbed premaxilla may necessi-
tate the use of angled abutments to overcome the problems
associated with implant placement and its relationship to the
screw hole access. The cement retained restoration directs
long axis of implant toward incisal edge and the screw-
retained restoration directs long axis of implant toward the
cingulum. If the buccopalatal position of the implant is too
Figure 1 A minimal mesiodistal, coronal, and radicular space must be
palatal, the shape of the final restoration will be overcontoured;
1.5–2 mm from the root of the adjacent tooth. it will overlap the ridge, increase the cantilever and compli-
cate oral hygiene. In such cases, a ridge-lap pontic needs to
be fabricated to compensate for poor implant placement.
Steps to Achieve Desired Esthetic Outcome
Site Preservation: After the loss of an anterior tooth, the nor-
mal sequelae of wound healing will create an unfavorable
esthetic soft-tissue complex. The remaining facial mucosa
often recedes apically and palatally. Typically, this cervical
recession results in a restoration that appears too long and
may be compounded with the loss of the interdental papilla.
Optimal implant soft-tissue esthetics depends much on the
optimal implant site preservation after the extraction of the
natural tooth. In the simplest terms, site preservation involves
the use of surgical and prosthetic techniques to preserve
Figure 2 The implant angulations relate to the original tooth structure both the volume and the architecture of the hard and soft-
more than the original root of the tooth.
tissues at the implant site. Surgical factors including flap
design and surgical approaches applicable to the respective
case, thereby reducing further damage or shrinkage of the
soft-tissues, can be considered to be site preservation tech-
niques. Soft-tissue integration refers to the establishment
and long-term maintenance of soft-tissue health and esthetics.
Soft-tissue integration is influenced by several factors such
as surgical/clinical technique, macro- and micro-surface
design, biocompatibility of the transmucosal component
(Figure 4), as well as soft-tissue morphology, including bio-
type, papilla volume (fill), and degree of scalloped gingival
margin. Clinical handling may jeopardize the soft-tissue
integration, during repeated disconnection and reconnection
of the transmucosal abutment. This has been reported to
result in a more apical position of the connective tissue.
Figure 3 Implant can be placed 1.5–2 mm from cementoenamel junction
of adjacent teeth, if there is no gingival recession for better emergence Interdental Papillary Esthetics: Papillary volume is
profile. inversely proportional to the distance from the interproximal
contact area to the bone crest.19 At a distance of < 5 mm, the
subgingivally (Figure 3). But if gingival recession is observed, papillae fill 100% of the time; when the distance measures
then the implant head should be positioned 3 mm from the 5–7 mm, the papillae fill the space 56% of the time (Figure 5).
adjacent gingival margins. Successful implant placement Finally, when the distance exceeds 7 mm, the space is filled
must be accomplished in three planes. If a screw-retained only 27% of the time. Implants must be placed in the so-called
abutment is used, the implant needs to be placed on the pala- ‘safe zone’ for best esthetic results. In an apical–coronal
tal aspect of the extraction socket or more palatal within the position, it is recommended that the implant be positioned
18 © Indian Journal of Dentistry 2012/Volume 3/Issue 1
Implant esthetics
Figure 4 Soft-tissue integration influenced by biocompatibility of the Figure 6 Contact point position altered to give illusion to papilla.
transmucosal component.
Bone probing has been confirmed as a valid method of
reporting the papilla length.19 However, it is rather an invasive
method since administrating the local anesthesia is likely to
cause the patient some discomfort and pain. Radiography
on the other hand has been regarded a valuable diagnostic
method, noninvasive, and often requires minimum patient
cooperation.
The following four surgical choices provide a better
esthetic outcome for a particular implant treatment21–26:
1. Papilla saving incision (flap reflection).
2. Second-stage surgery: making the incisions exclusively
in the attached tissues, this definitely decreases scarring.
Transposing the palatal keratinized tissues labially
enhances the emergence contour.
Figure 5 Papillary volume is inversely proportional to the distance from
the interproximal contact area to the bone crest.
3. Soft-tissue grafting: free gingival grafting; subepithelial
connective tissue grafting; and coronally repositioning
flaps.
2–3 mm below the CEJ of adjacent teeth. When optimal 4. Gingival recontouring techniques: electrosurgery is uti-
implant positioning is achieved, the transitional tissue could lized to remove scarring and the gingivoplasty by using
be altered using a customized abutment to create an emer- a diamond bur to remove the excess tissue.
gence profile that mimics the natural teeth and provides Considerable knowledge has been gained in surgical
adequate support to the surrounding soft-tissue. This can be management of facial gingival recession. The procedures
performed with a provisional restoration at the time of described in the literature include free gingival grafts, coro-
uncovering the implant and could be transferred at a later nally positioned flaps, free gingival grafts combined with
stage to the definitive restoration. Using the patient’s natural coronally positioned flaps, different types of pedicle grafts,
tooth as a provisional can help maintain the volume and free connective tissue grafts combined with pedicle grafts,
support of the papilla. and the guided tissue regeneration procedure. Although
these techniques give predictable solutions to the coverage
Techniques to Achieve Optimum Soft-tissue Esthetics of the denuded roots, they are not directed to the reconstruc-
with Implants: To verify these results, different methods tion of truncated papillae.27
of measuring the lengths of papilla have been introduced.
Some authors used photographs to assess the length; others
introduced indices to measure the length. Few authors used CONCLUSION
a rather invasive technique called ‘bone sounding’ to relate
papilla with the interdental bone. Latest techniques rely on The change in dentistry from the need-based to elective den-
radiographic measurement of bone level, and measuring the tistry has made a significant impact on the profession and
height of papilla with respect to the pitch of the implant the public perception of dentists. It is estimated that up to
inserted. Modification includes placing a radio-opaque mate- one-half of the dentistry accomplished at this time is elective.
rial at the tip of the papilla before exposure to radiograph. Much of this treatment is what could be considered to be
© Indian Journal of Dentistry 2012/Volume 3/Issue 1 19
Batra, et al
esthetic dentistry including procedures like implant place- 10. Weinberg LA. Esthetic and the gingiva in full coverage. J Prosthet
ment. As health professionals have increased their ability to Dent 1960;10:737–44.
11. Snow SR. Esthetic smile analysis of maxillary anterior tooth width: the
change faces, the necessity to understand what is and is not golden percentage. J Esthet Dent 1999;11:177–84.
beautiful has intensified. 12. Lombardi RE. A method for the classification of errors in dental
Prosthetic-driven implantology has been suggestive of esthetics. J Prosthet Dent 1974;32:501.
more accurate depicter of the esthetic outcome. As with any 13. Sackstein M. Short communication: display of mandibular and maxil-
extensive oral rehabilitation, esthetic concerns will require lary anterior teeth during smiling and speech: age and sex correlations.
Int J Prosthodont 2008;21:149–51.
consideration both in treatment planning and in restoration 14. Sennerby L, Roos J. Surgical determinants of clinical success of osseo-
completion. The addition of an osseo-integrated component, integrated oral implants: a review of the literature. Int J Prosthodont
particularly in the esthetic zone, may both enhance ultimate 1998;11:408–20.
stability and provide the opportunity to utilize many of the 15. Tarnow DP, Cho SC, Wallace SS. The effect of the inter-implant dis-
esthetic concepts described previously.26 With better scien- tance on the height of inter-implant bone crest. J Periodontol 2000;
71:546–9.
tific approach and improved knowledge, what was impossi- 16. Nemocovsky CE, Moses O, Artzi Z. Interproximal papillae recon-
ble previously can be achieved in reality with ease in the struction in maxillary implants. J Periodontol 2000;71:308–14.
esthetic zone. 17. Tan PLB, Dunne JT. An esthetic comparison of a metal ceramic crown
Implants used to replace missing teeth in the esthetic and cast metal abutment with an all-ceramic crown and zirconia abut-
zone have many advantages from preservation of unrestored ment: a clinical report. J Prosthet Dent 2004;91:215–8.
18. Mish Carl E. Contemporary Implant Dentistry 2nd ed. Mosby Inc,
adjacent teeth, halting the resorption of edentulous spaces, St Louis, Missouri 1999.
and providing support. Restoratively by altering the position 19. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the
of contact points to give illusion of papilla can be done to contact point to the crest of bone on the presence or absence of the
achieve optimum esthetic outcome (Figure 6).28 interproximal dental papilla. J Periodontol 1992;63:995–6.
20. Jemt T. Regeneration of gingival papillae after single implant treatment.
Int J Periodont Rest Dent 1997;17:327–33.
21. Wheeler SL, Vogel RE, Casellini R. Tissue preservation and mainte-
REFERENCES nance of optimum esthetics: a clinical report. Int J Oral Maxillofac
Implants 2000;2:265–71.
1. Albino JE, Tedesco LA. Patient perception of dental-facial esthetics. 22. Becker W, Becker BE. Flap designs for minimization of recession
Shared concerns in prosthodontics and orthodontics. J Prosthet Dent adjacent to maxillary anterior implant sites: a clinical study. Int J Oral
1984;52:9. Maxillofac Implants 1996;11:46–54.
2. Croll BM. Emergence profiles in natural tooth contour. Part I: 23. Tinti C, Benfenati SP. The ramp mattress suture: a new suturing tech-
Photographic observations. J Prosthet Dent 1989;62:4–10. nique combined with a surgical procedure to obtain papillae between
3. Fonseca RJ. Oral and maxillofacial surgery. vol 7 (Implant and recon- implants in the buccal area. Int J Periodont Rest Dent 2002;22:63–9.
structive surgery). WB Saunders 2000. 24. Misch CE, Al-Shammari KF, Wang HL. Creation of interimplant papil-
4. Charles A. In: Babbush Dental Implants: The Art and Science. lae through a split-finger technique. Implant Dent 2004;13:20–7.
Philadelphia: WB Saunders, London 2001:335–50. 25. Ten Bruggenkate CM, Kraaijenhagen HA, van der Kwast WA,
5. Anthony HL Tjan, Gary D Miller, Josephine GP The. Some esthetic Krekeler G, Oosterbeek HS. Autogenous maxillary bone grafts in con-
factors in a smile. J Prosthet Dent 1984;51:24–8. junction with placement of ITI endosseous implants. A preliminary
6. Lombardi R. Visual perception and dental esthetics. J Prosthet Dent report. Int J Oral Maxillofac Surg 1992;21:181–4.
1973;29:352–82. 26. Campelo LD, Camara JRD. Flapless implant surgery: a 10-year clinical
7. Rufenacht CR. Fundamentals of Esthetics. Quintessence Publishing retrospective analysis. Int J Oral Maxillofac Implants 2002;17:271–6.
Co. Inc., Chicago, Illinois 1990:9–31. 27. Yehouda BA. Reconstruction of anterior papillae by interdental con-
8. Lombardi RE. Factors mediating against excellence in dental esthetics. nective tissue grafts. J Prosthet Dent 1997;11:111–3.
J Prosthet Dent 1977;38:243–8. 28. Jemt T. Restoring the gingival contour by means of provisional resin
9. Levin EI. Dental esthetics and the golden proportion. J Prosthet Dent crowns after single-implant treatment. Int J Periodont Rest Dent 1999;
1978;40:244–52. 19:20–9.
20 © Indian Journal of Dentistry 2012/Volume 3/Issue 1
You might also like
- Original PDF Phlebotomy Handbook 10th Edition PDFDocument41 pagesOriginal PDF Phlebotomy Handbook 10th Edition PDFnoe.simons469100% (47)
- Case Studies in Medical-Surgical NursingDocument154 pagesCase Studies in Medical-Surgical NursingAlvin Javier100% (9)
- Geometric Considerations in AnteriorDocument11 pagesGeometric Considerations in AnteriorSebastián BernalNo ratings yet
- Smile Design Concepts and RequirementsDocument7 pagesSmile Design Concepts and RequirementsZahra ZaNo ratings yet
- A Didactic Concept Of: Dental MorphologyDocument9 pagesA Didactic Concept Of: Dental MorphologyErick Brañes Espinoza100% (1)
- Factores Macroesteticos en El Diseño de SonrisaDocument7 pagesFactores Macroesteticos en El Diseño de SonrisaJassel DurdenNo ratings yet
- Esthetic - Considerations - in - Orthodontics - An - Overview SECOND YEAR JC (FIRST)Document6 pagesEsthetic - Considerations - in - Orthodontics - An - Overview SECOND YEAR JC (FIRST)VEENA k.aNo ratings yet
- EstheticsDocument119 pagesEstheticsRubina BansalNo ratings yet
- Smile Design Dental PhotographyDocument3 pagesSmile Design Dental Photographydranilshinde100% (2)
- JCDP 19 624Document4 pagesJCDP 19 624Priyanka GandhiNo ratings yet
- 12-Aesthetics in Removable Prosthodontics - MahmoudDocument39 pages12-Aesthetics in Removable Prosthodontics - Mahmoudhassan.h.h.elhusseinyNo ratings yet
- IPAnnProsthodontRestorDent-7-3-124-127 (2)Document4 pagesIPAnnProsthodontRestorDent-7-3-124-127 (2)Shreyakalyani PanikkerNo ratings yet
- Esthetic in Complete DentureDocument14 pagesEsthetic in Complete DentureNidhi KatochNo ratings yet
- Are Occulsion and Comprehensive Dentistry Really That ImportantDocument20 pagesAre Occulsion and Comprehensive Dentistry Really That ImportantAhmed HamzaNo ratings yet
- Smile DesignDocument64 pagesSmile Designbaskarend67% (6)
- Review Article: Concepts of Complete Denture Occlusion: An Imperative Review of LiteratureDocument1 pageReview Article: Concepts of Complete Denture Occlusion: An Imperative Review of LiteratureSahana RangarajanNo ratings yet
- Faculty of Dentistry Prosthodontic DepartmentDocument23 pagesFaculty of Dentistry Prosthodontic DepartmentKarim MagdiNo ratings yet
- Aesthetics in Complete Denture - A REVIEWDocument2 pagesAesthetics in Complete Denture - A REVIEWInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Smiledesign 160716170541Document74 pagesSmiledesign 160716170541Aya Ibrahim YassinNo ratings yet
- ,ewwwwwwwwwwwwwDocument33 pages,ewwwwwwwwwwwwwDjoumana BentoumiNo ratings yet
- Evaluating Recurring Esthetic Dental Proportion REDocument6 pagesEvaluating Recurring Esthetic Dental Proportion REdanielaNo ratings yet
- Esthics in PDDocument5 pagesEsthics in PDMostafa Fayad100% (1)
- Principles of Smile DesignDocument2 pagesPrinciples of Smile DesignChristopher PriceNo ratings yet
- Aesthetics in Orthodontics: Six Horizontal Smile LinesDocument14 pagesAesthetics in Orthodontics: Six Horizontal Smile LinesPaulinaNo ratings yet
- Smile DesignDocument104 pagesSmile DesignEazhil Raj100% (3)
- Periodontal Considerations in Veneer CasesDocument7 pagesPeriodontal Considerations in Veneer CasesBethania CarolinaNo ratings yet
- 54.individualizing A Smile Makeover. Cur PDFDocument14 pages54.individualizing A Smile Makeover. Cur PDFEduardo AyubNo ratings yet
- Evaluation of Soft Tissue Parameters For Adults With Accepted Occlusion Using Legan and Burstone AnalysisDocument6 pagesEvaluation of Soft Tissue Parameters For Adults With Accepted Occlusion Using Legan and Burstone Analysismehdi chahrourNo ratings yet
- Orthodontic Treatment: The Soft Tissue Paradigm: ASE EportDocument4 pagesOrthodontic Treatment: The Soft Tissue Paradigm: ASE EportDrAshish KalawatNo ratings yet
- Principles For Establishment of Esthetics in Fixed Prosthodontics A ReviewDocument12 pagesPrinciples For Establishment of Esthetics in Fixed Prosthodontics A ReviewDjoumana BentoumiNo ratings yet
- Full Mouth ReconstructDocument5 pagesFull Mouth ReconstructMuaiyed Buzayan AkremyNo ratings yet
- Considerations For Establishing and Maintaining Proper Occlusion in The Aesthetic Zone - Dentistry TodayDocument12 pagesConsiderations For Establishing and Maintaining Proper Occlusion in The Aesthetic Zone - Dentistry Todayaziz2007No ratings yet
- Symmetry 13 00797 With CoverDocument15 pagesSymmetry 13 00797 With CoverNador AbdennourNo ratings yet
- Lechner. Placement of Artificial Teeth The Influence of Psyche and Illusion. (1997)Document9 pagesLechner. Placement of Artificial Teeth The Influence of Psyche and Illusion. (1997)Jose Enrique AvilaNo ratings yet
- 0 A 81Document11 pages0 A 81Sahana Rangarajan100% (1)
- Haptics - The Science of Touch in Dental TrainingDocument4 pagesHaptics - The Science of Touch in Dental TrainingInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- I015322838 PDFDocument11 pagesI015322838 PDFhinanaimNo ratings yet
- Dentist-Ceramist Communication Protocols For An Effective Esthetic Team Finkel2020Document12 pagesDentist-Ceramist Communication Protocols For An Effective Esthetic Team Finkel2020everaldocruzNo ratings yet
- Percepcion Desviaciones Faciales 2013 ChuDocument10 pagesPercepcion Desviaciones Faciales 2013 ChuAndres CurraNo ratings yet
- General Principles of Selection and Arrangement of Teeth A Literature Review - June - 2020 - 1591006696 - 5801245Document3 pagesGeneral Principles of Selection and Arrangement of Teeth A Literature Review - June - 2020 - 1591006696 - 5801245linaallakany2023No ratings yet
- Bioesthetic Dentistry, Part 1Document10 pagesBioesthetic Dentistry, Part 1suareztepper100% (1)
- b.10 Principles of Smile DesignDocument9 pagesb.10 Principles of Smile DesignbryamjbricenoNo ratings yet
- In Uence of Symmetry and Balance On Visual Perception of A White Female SmileDocument10 pagesIn Uence of Symmetry and Balance On Visual Perception of A White Female SmileSilpayNo ratings yet
- Goal Oriented Treatment MartinDocument8 pagesGoal Oriented Treatment Martindentist97No ratings yet
- Smile Characteristics in Orthodontics: A Concept ReviewDocument4 pagesSmile Characteristics in Orthodontics: A Concept Reviewjaganath venkatNo ratings yet
- Smile DesignDocument7 pagesSmile DesignDanilo Macam100% (1)
- Abutment Selection in Fixed Partial DentureDocument6 pagesAbutment Selection in Fixed Partial DentureheycoolalexNo ratings yet
- Abutment Selection in Fixed Partial Denture PDFDocument6 pagesAbutment Selection in Fixed Partial Denture PDFheycoolalexNo ratings yet
- Timeless Principles in Esthetic Dentistry JCD Fall 2012Document10 pagesTimeless Principles in Esthetic Dentistry JCD Fall 2012claudia360No ratings yet
- 09 Ijss Sep Oa09 2015 PDFDocument5 pages09 Ijss Sep Oa09 2015 PDFIonela MadalinaNo ratings yet
- Esthetic Factors of Smile in Vertical Dimensions ADocument7 pagesEsthetic Factors of Smile in Vertical Dimensions Agheorghita.mihaelaaNo ratings yet
- Planning and Orthodontic Preparation For Maxillary Incisors ReshapingDocument39 pagesPlanning and Orthodontic Preparation For Maxillary Incisors ReshapingJuliana SalasNo ratings yet
- The Relationship of Facial and Dental Midlines With Various Anatomic Landmarks of Face and Oral CavityDocument9 pagesThe Relationship of Facial and Dental Midlines With Various Anatomic Landmarks of Face and Oral CavityNyxeNo ratings yet
- Implants in Esthetic ZoneDocument10 pagesImplants in Esthetic ZoneInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Minimally Invasive Endodontics A Promising Future Concept A Review Article - 2017Document7 pagesMinimally Invasive Endodontics A Promising Future Concept A Review Article - 2017izeldien5870No ratings yet
- Dental Dimensions PDFDocument28 pagesDental Dimensions PDFHugo MoralesNo ratings yet
- The Correlation Between Anterior Tooth Form and GeDocument10 pagesThe Correlation Between Anterior Tooth Form and GeGabriela AvilesNo ratings yet
- Abutment Selection in Fixed Partial Denture - A Review: Drug Invention Today January 2018Document6 pagesAbutment Selection in Fixed Partial Denture - A Review: Drug Invention Today January 2018Najeeb UllahNo ratings yet
- Multidisciplinary Approach For The Closure of Multiple Diastemata With Composite ResinDocument15 pagesMultidisciplinary Approach For The Closure of Multiple Diastemata With Composite ResinCentro Dental IntegralNo ratings yet
- Abutment Selection in Fixed Partial Denture - A Review: Drug Invention Today January 2018Document6 pagesAbutment Selection in Fixed Partial Denture - A Review: Drug Invention Today January 2018Anwar KurniawanNo ratings yet
- Fragment Reattachment After Complicated Crown-Root Fractures of Anterior Teeth: A Systematic ReviewDocument16 pagesFragment Reattachment After Complicated Crown-Root Fractures of Anterior Teeth: A Systematic ReviewARUNA BharathiNo ratings yet
- Dynamic Navigation in Dental Implantology: The Influence of Surgical Experience On Implant Placement Accuracy and Operating Time. An in Vitro StudyDocument9 pagesDynamic Navigation in Dental Implantology: The Influence of Surgical Experience On Implant Placement Accuracy and Operating Time. An in Vitro StudySahana RangarajanNo ratings yet
- Mandibular MovementDocument56 pagesMandibular MovementSahana RangarajanNo ratings yet
- Factors Affecting Shade of All Ceramic Restorations - A Literature ReviewDocument8 pagesFactors Affecting Shade of All Ceramic Restorations - A Literature ReviewSahana RangarajanNo ratings yet
- Support in Complete DentureDocument30 pagesSupport in Complete DentureSahana Rangarajan100% (2)
- Different Types of Tooth PreparationDocument56 pagesDifferent Types of Tooth PreparationSahana Rangarajan100% (1)
- Support in Complete DentureDocument16 pagesSupport in Complete DentureSahana RangarajanNo ratings yet
- Frankel Appliance Certified Fixed Orthodontic Courses by Indian Dental AcademyDocument76 pagesFrankel Appliance Certified Fixed Orthodontic Courses by Indian Dental AcademySahana RangarajanNo ratings yet
- Fulltext - Jda v5 Id1107Document3 pagesFulltext - Jda v5 Id1107Sahana RangarajanNo ratings yet
- Finishing and Polishing Agents: - Presented by DR Arpita DuttaDocument89 pagesFinishing and Polishing Agents: - Presented by DR Arpita DuttaSahana RangarajanNo ratings yet
- Clinical Report Rehabilitation of Maxillary Surgical Defect With A Cast Partial Denture ObturatorDocument4 pagesClinical Report Rehabilitation of Maxillary Surgical Defect With A Cast Partial Denture ObturatorSahana RangarajanNo ratings yet
- A Hollow Bulb Obturator For Maxillary Resection in A Completely Edentulous PatientDocument6 pagesA Hollow Bulb Obturator For Maxillary Resection in A Completely Edentulous PatientSahana RangarajanNo ratings yet
- 6.clinical Case ReportMultidisciplinary Approach For Rehabilitation of Debilitated Anterior ToothDocument6 pages6.clinical Case ReportMultidisciplinary Approach For Rehabilitation of Debilitated Anterior ToothSahana RangarajanNo ratings yet
- 7 Shreeprada Dash IJPHRDDecember 2018 IssueDocument7 pages7 Shreeprada Dash IJPHRDDecember 2018 IssueSahana RangarajanNo ratings yet
- Gothic Arch TrachingDocument7 pagesGothic Arch TrachingSahana RangarajanNo ratings yet
- Long-Term Follow-Up of Maxillary Fixed Retention: Survival Rate and Periodontal HealthDocument7 pagesLong-Term Follow-Up of Maxillary Fixed Retention: Survival Rate and Periodontal HealthSahana RangarajanNo ratings yet
- 7 RetainerinorthodonticsDocument6 pages7 RetainerinorthodonticsSahana RangarajanNo ratings yet
- Cases and Comments: by Stanley G. Standard, D.D.S., New YorkDocument3 pagesCases and Comments: by Stanley G. Standard, D.D.S., New YorkSahana RangarajanNo ratings yet
- 3D Printing Industry Roadmap - India (Aerospace) Summit DocumentDocument19 pages3D Printing Industry Roadmap - India (Aerospace) Summit DocumentSahana RangarajanNo ratings yet
- Review: Types of Finish Lines or Gingival Margins Intooth PreparationDocument6 pagesReview: Types of Finish Lines or Gingival Margins Intooth PreparationSahana RangarajanNo ratings yet
- Significance of Facebow For Dental RestorationsDocument5 pagesSignificance of Facebow For Dental RestorationsSahana RangarajanNo ratings yet
- Mouth Guards in Dentistry-A Review: September 2018Document6 pagesMouth Guards in Dentistry-A Review: September 2018Sahana RangarajanNo ratings yet
- Elegant Galaxy Background Breakthrough by SlidesgoDocument48 pagesElegant Galaxy Background Breakthrough by SlidesgoSahana RangarajanNo ratings yet
- Prosthodontics Horizontal Jaw Relation: Dr. Firas AbdulameerDocument6 pagesProsthodontics Horizontal Jaw Relation: Dr. Firas AbdulameerSahana RangarajanNo ratings yet
- Sauser 1957Document9 pagesSauser 1957Sahana RangarajanNo ratings yet
- Certificate of Good Standing Application FormDocument1 pageCertificate of Good Standing Application Formroosteenee0% (1)
- The Implementation of Universal Health Law in TH PhilippinesDocument1 pageThe Implementation of Universal Health Law in TH PhilippinesMelchizeder Solis LumanogNo ratings yet
- 4 - Drug Product Design ParametersDocument7 pages4 - Drug Product Design ParametersVinz AlvarezNo ratings yet
- 5980 10143 1 SM PDFDocument11 pages5980 10143 1 SM PDFfaustinaNo ratings yet
- Cigna Medical Coverage Policy: Electrical Stimulation Therapy and DevicesDocument55 pagesCigna Medical Coverage Policy: Electrical Stimulation Therapy and DevicesDidik HariadiNo ratings yet
- Entry Level Ultrasound Tech Cover LetterDocument6 pagesEntry Level Ultrasound Tech Cover Letterafdlxeqbk100% (1)
- New Variants of CovidDocument2 pagesNew Variants of CovidAdrian Jay BeloyNo ratings yet
- Endovascular Aortic Aneurysm Repair (EVAR)Document5 pagesEndovascular Aortic Aneurysm Repair (EVAR)D FNo ratings yet
- Volume 1Document1,428 pagesVolume 1Luli Corvelo SarmentoNo ratings yet
- Bag Technique (Performance Checklist)Document1 pageBag Technique (Performance Checklist)Gia Espinosa OcbeñaNo ratings yet
- PharmacogeneticsDocument8 pagesPharmacogeneticskangaroocherryNo ratings yet
- Class II Treatment Efficiency in U4 Extraction & Non Extraction Protocols 2007Document9 pagesClass II Treatment Efficiency in U4 Extraction & Non Extraction Protocols 2007Maha Ahmed SolimanNo ratings yet
- Bon Test FrameworkDocument16 pagesBon Test FrameworkMaria Garcia Pimentel Vanguardia II100% (1)
- The Impact of Music Therapy On Anxiety in Cancer Patients Undergoing Simulation For Radiation TherapyDocument8 pagesThe Impact of Music Therapy On Anxiety in Cancer Patients Undergoing Simulation For Radiation TherapyWWMTNo ratings yet
- Hpe Year 9 Lifestyle Diseases Oral Presentation AssessmentDocument1 pageHpe Year 9 Lifestyle Diseases Oral Presentation Assessmentapi-247292404No ratings yet
- Case Study of MicrobiologyDocument4 pagesCase Study of MicrobiologyQaisrani Y9No ratings yet
- Multiple Choice Cloze 4Document3 pagesMultiple Choice Cloze 4Marla JailerNo ratings yet
- The Effect of Orthodontic Referral Guidelines: A Randomised Controlled TrialDocument6 pagesThe Effect of Orthodontic Referral Guidelines: A Randomised Controlled TrialishtiiiNo ratings yet
- Admission & DischargeDocument7 pagesAdmission & DischargernrmmanphdNo ratings yet
- Community Health Nursing Chapter 5Document2 pagesCommunity Health Nursing Chapter 5Audrie Allyson GabalesNo ratings yet
- National Drug Control Framework-The Experience of GhanaDocument29 pagesNational Drug Control Framework-The Experience of Ghanalovia mensahNo ratings yet
- Countr State: Katsina: NigeriaDocument17 pagesCountr State: Katsina: NigeriaSalihu MustaphaNo ratings yet
- KKM Policies & Procedures On Infection Prevention and Control 2019Document305 pagesKKM Policies & Procedures On Infection Prevention and Control 2019Noor AtiqahNo ratings yet
- Week 2 Session 3 and 4 I Am Your Nurse Worksheets For StudentsDocument6 pagesWeek 2 Session 3 and 4 I Am Your Nurse Worksheets For StudentsAlfredo TeurupunNo ratings yet
- Getokinawatonic ComDocument4 pagesGetokinawatonic Comoszkar69No ratings yet
- Revised OKD Form C - OK Sa DepEd Accomplishment ReportDocument10 pagesRevised OKD Form C - OK Sa DepEd Accomplishment ReportDarren CariñoNo ratings yet
- Day SurgeryDocument350 pagesDay SurgeryMohamed Fawzy100% (1)
- Abortion PillsDocument3 pagesAbortion PillsmailbabuNo ratings yet