Professional Documents
Culture Documents
Skeletal Diseases in Cushing's Syndrome: Osteoporosis Versus Arthropathy
Skeletal Diseases in Cushing's Syndrome: Osteoporosis Versus Arthropathy
Uploaded by
kuro hanabusa0 ratings0% found this document useful (0 votes)
21 views5 pagesOriginal Title
314298
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
21 views5 pagesSkeletal Diseases in Cushing's Syndrome: Osteoporosis Versus Arthropathy
Skeletal Diseases in Cushing's Syndrome: Osteoporosis Versus Arthropathy
Uploaded by
kuro hanabusaCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 5
Neuroendocrinology 2010;92(suppl 1):60–64 Published online: September 10, 2010
DOI: 10.1159/000314298
Skeletal Diseases in Cushing’s Syndrome:
Osteoporosis versus Arthropathy
Gregory Kaltsas Polyzois Makras
Department of Pathophysiology, National University of Athens, Athens, Greece
Key Words osteoporotic fractures. Bisphosphonates can induce a more
Osteoporosis ⴢ Cushing’s syndrome ⴢ Avascular necrosis ⴢ rapid improvement in BMD than cortisol normalization
Bisphosphonates ⴢ Cortisol ⴢ Bone mineral density alone and can be used in patients with increased risks for
further fractures and/or persistent hypercortisolemia to pre-
vent further bone loss. Anabolic agents have not as yet been
Abstract systemically used. Avascular necrosis, mainly of the femoral
Structural and functional impairment of the skeletal system neck, and growth arrest in children are the most common
remains an important cause of morbidity and disability in skeletal disorders unrelated to osteoporosis encountered in
patients with Cushing’s syndrome (CS). Glucocorticoid (GC) patients with endogenous hypercortisolism.
excess inhibits bone formation and calcium absorption from Copyright © 2010 S. Karger AG, Basel
the gut, increases bone resorption, and alters the secretion
of gonadotropin and growth hormones, cytokines and
growth factors influencing bone. Both overt and subtle en- Introduction
dogenous hypercortisolism affect bone, leading to vertebral
fractures in up to 70% of patients. Fracture risk is related to Glucocorticoids (GCs) exert multiple effects on bone
age at onset, duration and severity of the disease and indi- and GC-induced osteoporosis is the commonest cause of
vidual susceptibility to GCs that is genetically determined. secondary osteoporosis. However, the effects that GCs
Bone mineral density (BMD) measurement at the lumbar exert on bone metabolism are hampered by the specific
spine should be performed as a screening test in all patients effects of the underlying disease that GCs are prescribed
with CS due to the preferential loss of trabecular bone in- for. Recently, a substantial amount of data has been gath-
duced by GCs. The higher risk of fractures at comparable ered from studies looking at the effects that GC excess
BMD values with controls suggests that bone quality fea- exerts on bone denoted of any other confounding factors
tures, not assessed by routine BMD approaches, are also im- such as in cases of endogenous hypercortisolism (Cush-
portant and should be addressed when indicated applying ing’s syndrome; CS). This paper addresses the pathogen-
specific radiological means. Successful treatment of GC ex- esis, incidence, prediction and treatment of osteoporosis
cess is associated with improvement in bone mass which, in patients with CS and discusses other less common, re-
although delayed and often incomplete, reduces the risk of lated arthropathies encountered in such patients.
© 2010 S. Karger AG, Basel Gregory Kaltsas
0028–3835/10/0925–0060$26.00/0 Department of Pathophysiology
Fax +41 61 306 12 34 University of Athens, Mikras Asias 75
E-Mail karger@karger.ch Accessible online at: GR–11527 Athens (Greece)
www.karger.com www.karger.com/nen Tel. +30 210 746 2513, Fax +30 210 746 2664, E-Mail gkaltsas @ endo.gr
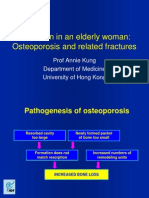
Skeletal growth
factors synthesis Osteoblast number
and activity ↓ and function ↓
↓ LH, FSH sex steroids ↑ RANK-L or
↓ GH, IGF-I, TGF- ↓ blunted OPG
activity
↓ Bone formation ↓BMD and bone
↑ Bone resorption strength
↑ PTH, altered dynamics + activity
↓ Ca absorption from the gut Osteoblast PTH-R
↑ Ca excretion from the kidneys
Fig. 1. Pathogenesis of GC-induced bone
loss.
Osteoporosis GC Effects on Bone at the Cellular Level
The initial event of GC effect on bone is stimulation of
Pathogenesis (fig. 1) osteoblastic cells to increase the production of RANKL
The multifactorial pathogenesis of bone loss in CS de- (receptor activator of NF-kappa B-RANK-ligand, which
pends on direct and indirect effects of GCs on bone that enhances osteoclastogenesis) and reduce the production
are not restricted to bone mineral density (BMD) alone, of osteoprotegerin, the natural antagonist of RANKL [1].
but also involve bone architecture, geometry and the rate Furthermore, GCs may act directly or through the
of bone remodeling units (BRU), important components increased expression of macrophage-colony-stimulating
that together determine bone strength [1]. factor on the osteoclasts, prolonging their life span, ex-
Sustained and prolonged hypercortisolism leads to a plaining the early rapid phase of bone loss [1]. However,
rapid early phase of BMD decline due to excessive bone the most detrimental effect of GCs on bone metabolism
resorption, which is followed later on by a slower and is a profound reduction in osteoblast number and func-
more progressive phase of impaired bone formation [2]. tion, leading to suppression of bone formation and sub-
Besides their direct effect on BRU, GCs also reduce cal- sequent reduction of the amount of bone replaced in each
cium absorption from the gastrointestinal tract due to remodeling cycle [1]. GC excess impairs osteoblastic cell
opposition of vitamin D action and inhibition of renal differentiation by inhibiting Wnt--catenin signaling,
tubular calcium reabsorption [2]. GCs also influence the and inducing the overexpression of Notch receptors
production and action of other hormones that regulate thereby enhancing apoptosis of osteoblasts and osteo-
bone and calcium metabolism such as gonadotropins, cytes by activating caspase 3 [6]. Osteocyte apoptosis may
growth hormone (GH) and insulin-like growth factor-I be an additional important mechanism in GC induced
(IGF-I) [2, 3]. In patients with CS, a significant reduction fractures while the disruption of the osteocyte-canalicu-
of lumbar spine bone density develops before involve- lar network may result in a detection failure of signals
ment of the peripheral skeleton [4] because of a rapid loss that normally stimulate the replacement of damaged
of the trabecular bone [5]. The catabolic effects of GCs on bone [7]. Thus, a substantial effect of GCs on osteocytes
muscle also contributes to fracture risk due to an in- might account for a disproportionate loss of bone strength
creased incidence of falls secondary to muscle weakness, in relation to bone mass. Recent evidence has also impli-
and loss of the stimulatory effect of muscular contraction cated the GC-induced leukine zipper gene transcription-
on bone formation [2]. al factor as a crucial factor by regulating osteoblast matu-
ration and bone turn-over [8].
Skeletal Involvement in Endogenous Neuroendocrinology 2010;92(suppl 1):60–64 61
Hypercortisolism
Risk of Fractures Bone Mass
Approximately 30–67% of patients with CS develop In CS there is uncoupling between bone apposition
fractures, mainly at the vertebrae, leading to back pain, (reduced) and resorption (normal/increased) leading to
kyphosis and loss of height [9]. The number of collapsed severe bone loss, especially in trabecular sites, with an
vertebral bodies is correlated to age at disease onset, dis- estimated risk of osteoporosis of 60–70% [9]. Measure-
ease duration, and urinary free cortisol levels at diagnosis ment of BMD by DEXA, particularly at the lumbar spine,
even in patients with long-term cured CS [9]. In a signif- presents the initial method of assessment. Vertebral CT
icant number of patients, fractures may be completely scan can also be used to assess osteoporosis in these pa-
asymptomatic and even develop in those with normal tients [5].
BMD values [10]. Men appear to be more susceptible than
women, with the crucial period of developing a fracture Bone Architecture
being 2 years prior diagnosis [11]. Although it was ini- Fracture risk among prior GC users can be partly ex-
tially suggested that the risk was higher in patients with plained by BMD and the thresholds of BMD for vertebral
adrenal CS this finding has not been replicated by subse- fractures are higher in patients treated with oral GC, sug-
quent studies [1]. gesting that other factors besides BMD may also operate
Besides clinically obvious CS, a significant number of [16]. Indeed, bone strength is also determined by instinct
patients are increasingly being identified with alterations properties of bone tissue such as microdamage accumula-
of cortisol secretory dynamics without exhibiting the tion, bone matrix proteins and degree of mineralization,
classical signs or symptoms of CS. These patients consti- and bone turn over effects. These features are currently
tute the so-called subclinical CS (SCS), mainly due to best accessed by peripheral quantitative computed to-
functioning adrenal adenomas, with an estimated preva- mography which can distinguish cortical from trabecular
lence higher than that of clinically obvious CS (0.8/1,000 bone, measure the geometric properties of long bones,
vs. 1/500,000) [1]. Although not replicated consistently, and estimate bone strength by calculating polar strength
several studies have documented that patients with SCS strain index [16]. When this method was recently applied
have reduced BMD and that this is more prominent in in 10 women with CS, it revealed that all these indices
postmenopausal women [1, 12]. were lower in patients with CS compared to controls but
only in premenopausal women, suggesting a strength loss
Individual Susceptibility to Osteoporosis mechanism and explaining the presence of fractures even
Not all individuals exposed to endogenous hypercor- in patients with normal BMD [16]. Since the ultrasound
tisolism develop osteoporosis and fractures [2]. Between velocity is influenced both by the organic and nonorganic
the speculated mechanisms subjects carrying the N363S bone compounds, quantitative ultrasound could be a use-
GC receptor polymorphism are thought to exhibit a high- ful tool for assessing the multifactorial bone involvement
er sensitivity to GCs [13]. Alternatively, the activity of in CS; however, longitudinal studies are lacking [5].
11-hydroxysteroid dehydrogenase type 1 enzyme, which
acts to convert inactive cortisone to cortisol and is ex- Risk Factor Stratification
pressed in osteoblasts, is enhanced by GCs and leads to The number of collapsed vertebrae was reported to di-
osteoblastic dysfunction [14]. rectly relate to age at disease onset, disease duration and
severity based on urinary free cortisol levels, even in
Biochemical Markers of Bone Turnover cured patients [5]. These parameters along with lumbar
The net effect of bone apposition markers in patients BMD measurements and possible means of assessing
with CS reveals a picture of reduced synthesis of new bone quality, and the cortisol-to-DHEAS ratio should be
bone. Markers of bone formation, particularly osteocal- taken into consideration to identify patients at high risk
cin, are substantially reduced, correlate with disease ac- and offer appropriate intervention [17]. Assessment of
tivity and increase with restoration of eucortisolism. muscular strength is also highly important as muscular
Other markers of bone formation have shown greater weakness is associated with increased fracture risk.
variability [15], while bone resorption markers exhibit
substantial variation and thus are not used routinely [1]. Therapy
The ultimate target is to prevent fractures. Appropri-
ate interventions include calcium and vitamin D intake
of 1,500 mg and 800 IU daily, respectively. Urinary cal-
62 Neuroendocrinology 2010;92(suppl 1):60–64 Kaltsas/Makras
cium excretion has to be considered to avoid the develop- Table 1. Skeletal manifestation of Cushing’s syndrome
ment of nephrolithiasis. Administration of sex steroids
has a place in the management of hypogonadal patients Osteoporosis, predominantly of trabecular bones
receiving GCs and particularly in those with SCS [1, 2]. Spontaneous symptomless fractures of ribs, pubic and ischial
Similarly, GH replacement may exert a beneficial effect rami, foot bones and vertebrae
on bone turnover in significant number of patients with Healing of fracture with abundant pseudocallus formation
CS and GH deficiency [5]. However, this particular treat- Osteonecrosis (avascular necrosis) of head of femur and
ment has not been extensively used. Due to the increased humerus, distal femur and vertebrae
fracture risk, a proactive preventing approach including
Suppression of growth velocity in children
lifestyle changes, such as tobacco cessation and reduction
in alcohol consumption, exercise program, and restric-
tion of sodium intake in the presence of hypercalciuria
should be undertaken [2]. The cure of CS is reported to
restore normally coupled bone metabolism and remark- the ribs, pelvis and end plates of collapsed vertebrae and
ably improve BMD [1]. However, normalization may take is considered the hallmark of GC-induced osteoporosis
several years and may not always be complete although [19]. Microscopically, there is a reduction in osteoblastic
the fracture risk is substantially reduced over the first activity and production of a cartilaginous callus that be-
years following treatment [1]. In order to shorten the time comes highly mineralized in an amorphous fashion [20].
of BMD recovery, particularly in high-risk patients, the Such fractures can also develop in the feet, pubic and is-
use of aledronate and clodronate exhibit a higher BMD chial rami and uncommonly in long bones resembling
increase compared to untreated patients, suggesting that pseudofractures of osteomalacia [19]. Osteonecrosis of
these drugs may induce a more rapid improvement in the femoral head is most commonly encountered follow-
bone density than cortisol normalization alone [1]. As pa- ing exogenous GC administration although cases follow-
tients with GC induced osteoporosis have a higher risk ing endogenous hypercortisolism are increasingly being
for fractures, it has been recommended that treatment recognized; occasionally both femurs and several other
with bisphosphonates should be started with T-scores joints may be involved [1, 19]. Growth failure, weight gain
lower than –1 SD [2]. Estrogens are a reasonable approach and pubertal arrest are the hallmarks of CS in children
in hypogonadal premenopausal women and in combina- and growing adolescents leading to reduced final adult
tion with bisphosphonates have additive effects on osteo- height [5]. Children with hypercortisolism also develop a
cyte survival, acting synergistically on the same trans- reduction in peak bone mass, which presents a major de-
duction pathway although at different levels [2]. terminant of long-term risk of osteoporosis [5].
Due to the substantial reduction of bone formation,
treatment with an anabolic agent that promotes bone for-
mation and reduces vertebral and non-vertebral frac- Conclusion
tures, such as PTH, has also been suggested [2]. Although
the use of teriparatide has not been yet explored in endog- Endogenous hypercortisolism exerts a detrimental ef-
enous CS it has been repeatedly shown to be beneficial fect on bone and substantially increases the risk for spinal
in patients with exogenous GC-induced osteoporosis fractures secondary to osteoporosis. High-risk patients
[2]. Another potential therapeutic target is the RANK- need to be identified and offered appropriate treatment at
RANKL-OPG system particularly after the development an early stage.
of a human monoclonal antibody to RANKL (denosum-
ab) that has been shown to reduce all osteoporotic frac-
tures in postmenopausal patients [18]. Disclosure Statement
The authors have nothing to declare.
Arthropathies (table 1)
Arthopathies related to CS are relatively rare and usu-
ally accompany osteoporosis. Abundant pseudocallus
formation is frequently seen around stress fractures in
Skeletal Involvement in Endogenous Neuroendocrinology 2010;92(suppl 1):60–64 63
Hypercortisolism
References
1 Chiodini I, Torlontano M, Carnevale V, 9 Shaker JL, Lukert BP: Osteoporosis associ- 15 Osella G, Terzolo M, Reimondo G, Piovesan
Trischitta V, Scillitani A: Skeletal involve- ated with excess glucocorticoids. Endocrinol A, Pia A, Termine A, Paccotti P, Angeli A:
ment in adult patients with endogenous hy- Metab Clin North Am 2005;34:341–343ix. Serum markers of bone and collagen turn-
percortisolism. J Endocrinol Invest 2008; 31: 10 Tauchmanovà L, Pivonello R, Di SC, Rossi R, over in patients with Cushing’s syndrome
267–276. De Martino MC, Camera L, Klain M, Salva- and in subjects with adrenal incidentalomas.
2 Mazziotti G, Angeli A, Bilezikian JP, Canalis tore M, Lombardi G, Colao A: Bone demin- J Clin Endocrinol Metab 1997;82:3303–3307.
E, Giustina A: Glucocorticoid-induced os- eralization and vertebral fractures in endog- 16 Kaji H, Yamauchi M, Chihara K, Sugimoto
teoporosis: an update. Trends Endocrinol enous cortisol excess: role of disease etiology T: Glucocorticoid excess affects cortical
Metab 2006;17:144–149. and gonadal status. J Clin Endocrinol Metab bone geometry in premenopausal, but not
3 Manelli F, Giustina A: Glucocorticoid- 2006;91:1779–1784. postmenopausal, women. Calcif Tissue Int
induced osteoporosis. Trends Endocrinol 11 Vestergaard P, Lindholm J, Jorgensen JO, 2008;82: 182–190.
Metab 2000;11:79–85. Hagen C, Hoeck HC, Laurberg P, Rejnmark 17 Tauchmanovà L, Pivonello R, De Martino
4 Karavitaki N, Ioannidis G, Giannakopoulos L, Brixen K, Kristensen LO, Feldt-Rasmus- MC, Rusciano A, De LM, Ruosi C, Mainolfi
F, Mavrokefalos P, Thalassinos N: Evalua- sen U, Mosekilde L: Increased risk of osteo- C, Lombardi G, Salvatore M, Colao A: Ef-
tion of bone mineral density of the periph- porotic fractures in patients with Cushing’s fects of sex steroids on bone in women with
eral skeleton in pre- and postmenopausal syndrome. Eur J Endocrinol 2002;146:51–56. subclinical or overt endogenous hypercorti-
women with newly diagnosed endogenous 12 Torlontano M, Chiodini I, Pileri M, Gugliel- solism. Eur J Endocrinol 2007;157:359–366.
Cushing’s syndrome. Clin Endocrinol (Oxf) mi G, Cammisa M, Modoni S, Carnevale V, 18 Cummings SR, San MJ, McClung MR, Siris
2004;60:264–270. Trischitta V, Scillitani A: Altered bone mass ES, Eastell R, Reid IR, Delmas P, Zoog HB,
5 Mancini T, Doga M, Mazziotti G, Giustina A: and turnover in female patients with adrenal Austin M, Wang A, Kutilek S, Adami S,
Cushing’s syndrome and bone. Pituitary incidentaloma: the effect of subclinical hy- Zanchetta J, Libanati C, Siddhanti S, Chris-
2004;7:249–252. percortisolism. J Clin Endocrinol Metab tiansen C: Denosumab for prevention of
6 Canalis E: Mechanisms of glucocorticoid ac- 1999;84:2381–2385. fractures in postmenopausal women with
tion in bone. Curr Osteoporos Rep 2005; 3: 13 Huizenga NA, Koper JW, De Lange P, Pols osteoporosis. N Engl J Med 2009; 361: 756–
98–102. HA, Stolk RP, Burger H, Grobbee DE, Brink- 765.
7 Manolagas SC: Corticosteroids and frac- mann AO, De Jong FH, Lamberts SW: A 19 Adachi JD, Papaioannou A: Corticosteroid-
tures: a close encounter of the third cell kind. polymorphism in the glucocorticoid recep- Induced osteoporosis: detection and man-
J Bone Miner Res 2000; 15:1001–1005. tor gene may be associated with and in- agement. Drug Saf 2001;24:607–624.
8 Lekva T, Bollerslev J, Kristo C, Olstad OK, creased sensitivity to glucocorticoids in vivo. 20 Adachi JD: Corticosteroid-induced osteopo-
Ueland T, Jemtland R: The glucocorticoid- J Clin Endocrinol Metab 1998;83:144–151. rosis. Am J Med Sci 1997;313:41–49.
induced leucine zipper gene (GILZ) expres- 14 Tomlinson JW, Walker EA, Bujalska IJ,
sion decreases after successful treatment of Draper N, Lavery GG, Cooper MS, Hewison
patients with endogenous Cushing’s syn- M, Stewart PM: 11beta-hydroxysteroid dehy-
drome and may play a role in glucocorticoid- drogenase type 1: a tissue-specific regulator
induced osteoporosis. J Clin Endocrinol of glucocorticoid response. Endocr Rev
Metab 2010;95:246–255. 2004;25:831–866.
64 Neuroendocrinology 2010;92(suppl 1):60–64 Kaltsas/Makras
You might also like
- 5 - Introduction To Communicable DiseaseDocument32 pages5 - Introduction To Communicable DiseaseGetom Ngukir100% (1)
- Parameter Settings For Electrically Stimulated Muscle ContractionDocument3 pagesParameter Settings For Electrically Stimulated Muscle Contractionpallen100% (5)
- (MI) Patient Profile DatabaseDocument11 pages(MI) Patient Profile DatabaseMurathi Mwangi100% (1)
- FNCPDocument1 pageFNCPkristel_nicole18yahoNo ratings yet
- Gluco Induced OsteopDocument13 pagesGluco Induced Osteopmatheus galvãoNo ratings yet
- Capture The Fracture - Use of Bone Turnover MarkerDocument7 pagesCapture The Fracture - Use of Bone Turnover MarkergusdeNo ratings yet
- Pathophysiology of Bone MetastasesDocument5 pagesPathophysiology of Bone MetastasesdyahNo ratings yet
- Bone Disease in Chronic Kidney Disease and Kidney TransplantDocument27 pagesBone Disease in Chronic Kidney Disease and Kidney TransplantBhanu KumarNo ratings yet
- Group Ii: Harni Sartika Sandrawati Nangsih S. Slamet Rusman Hasanuddin Yusnita UsmanDocument17 pagesGroup Ii: Harni Sartika Sandrawati Nangsih S. Slamet Rusman Hasanuddin Yusnita UsmanYusnitaUsmanNo ratings yet
- Glucocorticoid-Induced Osteoporosis: Pathophysiology and TherapyDocument10 pagesGlucocorticoid-Induced Osteoporosis: Pathophysiology and TherapyMuhammad Isnaini ZuhriNo ratings yet
- L36 - Back Pain in An Elderly Woman - 2012Document46 pagesL36 - Back Pain in An Elderly Woman - 2012edwinfy123No ratings yet
- ESO Spesifik Pada Organ SpesifikDocument44 pagesESO Spesifik Pada Organ SpesifikLidwina Margaretha LakaNo ratings yet
- Arthrosis of KneeDocument30 pagesArthrosis of Kneebiomechy oktomalioputriNo ratings yet
- Arthrosis of KneeDocument30 pagesArthrosis of Kneebiomechy oktomalioputriNo ratings yet
- Effects of Microgravity On Bone DensityDocument9 pagesEffects of Microgravity On Bone DensityAffan Nadeem QaziNo ratings yet
- OsteoporosisDocument13 pagesOsteoporosisclaudyNo ratings yet
- Denosumab: An Emerging Therapy in Pediatric Bone Disorders: Pediatrics (L Ward and E Imel, Section Editors)Document10 pagesDenosumab: An Emerging Therapy in Pediatric Bone Disorders: Pediatrics (L Ward and E Imel, Section Editors)Dita Putri DamayantiNo ratings yet
- Biology of BoneDocument30 pagesBiology of BoneChris Jardine LiNo ratings yet
- Pathophysiology-Pathomechanics Dan Penegakan Diagnosis OsteoporosisDocument90 pagesPathophysiology-Pathomechanics Dan Penegakan Diagnosis Osteoporosissingle_ladyNo ratings yet
- Fimmu 13 1005665Document14 pagesFimmu 13 1005665sopha seyhaNo ratings yet
- OsteoporosisDocument35 pagesOsteoporosisFarida Abo ElmagdNo ratings yet
- Pathogenesis of Osteoporosis 2: Cli Ord J. RosenDocument13 pagesPathogenesis of Osteoporosis 2: Cli Ord J. RosenRonald TejoprayitnoNo ratings yet
- Nutritional Zinc Plays A Pivotal Role in Bone Health and Osteoporosis PreventionDocument14 pagesNutritional Zinc Plays A Pivotal Role in Bone Health and Osteoporosis PreventionDewi HenssaNo ratings yet
- Adverse Effects of Corticosteroids On BoneDocument6 pagesAdverse Effects of Corticosteroids On BoneDiego Rivas-VazquezNo ratings yet
- Effects of Glucosamine and Chondroitin Sulfate On Cartilage Metabolism in OA. Outlook On Other Nutrient Partners Especially Omega-3 Fatty AcidsDocument17 pagesEffects of Glucosamine and Chondroitin Sulfate On Cartilage Metabolism in OA. Outlook On Other Nutrient Partners Especially Omega-3 Fatty Acidsharvestmoon.harvestingtimeNo ratings yet
- Doosis KalsiumDocument8 pagesDoosis KalsiumNurul Kamilah SadliNo ratings yet
- Thiazolidinediones On PPARg The Roles in Bone RemoDocument9 pagesThiazolidinediones On PPARg The Roles in Bone RemoNguyễn Hoàng Thiên TânNo ratings yet
- Frontiers in Bioscience 4, d662-670, October 15, 1999Document9 pagesFrontiers in Bioscience 4, d662-670, October 15, 1999Aldo HoxhaNo ratings yet
- The Effect of Icariin On Bone Metabolism and Its Potential Clinical ApplicationDocument12 pagesThe Effect of Icariin On Bone Metabolism and Its Potential Clinical ApplicationBrenda MartinsNo ratings yet
- OsteoporosisDocument35 pagesOsteoporosisSanjeev MehtaNo ratings yet
- BP MecanismDocument14 pagesBP MecanismAdryana StefyNo ratings yet
- Normal Bone Formation and RemodelingDocument4 pagesNormal Bone Formation and RemodelingFernando AnibanNo ratings yet
- Secondary OsteoporosisDocument22 pagesSecondary OsteoporosisBenny Chris TantoNo ratings yet
- Update Osteoporosis Management (Listo)Document18 pagesUpdate Osteoporosis Management (Listo)Jossie AcuñaNo ratings yet
- Osseteointegration of Dental ImplantDocument24 pagesOsseteointegration of Dental ImplantFajar Kusuma Dwi KurniawanNo ratings yet
- 1042 FullDocument9 pages1042 Fulloki harisandiNo ratings yet
- Chondroprotective Effects of The Combination ChondroitinDocument9 pagesChondroprotective Effects of The Combination Chondroitincursotplo2021No ratings yet
- Regulatory Pathways Revealing New Approaches2008Document14 pagesRegulatory Pathways Revealing New Approaches2008Cami GutierrezNo ratings yet
- LID201112052004Document10 pagesLID201112052004Gia BảoNo ratings yet
- Pathophysiology of OsteoarthritisDocument3 pagesPathophysiology of OsteoarthritisHajar ToharNo ratings yet
- Non-Enzymatic Glycation of Bone Collagen Modifies Osteoclastic Activity and DifferentiationDocument28 pagesNon-Enzymatic Glycation of Bone Collagen Modifies Osteoclastic Activity and Differentiationdumboo21No ratings yet
- Yoon-Kyum Shin, Young Kwon Yoon, Kyung Bae Chung, Yumie Rhee, Sung-Rae ChoDocument6 pagesYoon-Kyum Shin, Young Kwon Yoon, Kyung Bae Chung, Yumie Rhee, Sung-Rae ChoRisky Ilona SaputraNo ratings yet
- Recent Advances in The Pathogenesis and Treatment of OsteoporosisDocument5 pagesRecent Advances in The Pathogenesis and Treatment of OsteoporosisAnil JohnNo ratings yet
- OSTEOPOROSISDocument39 pagesOSTEOPOROSISHapsari Wibawani 'winda'No ratings yet
- Secondary Osteoporosis - A Still Neglected ConditionDocument4 pagesSecondary Osteoporosis - A Still Neglected ConditionClaudiaGuerreroNo ratings yet
- Osteogenesi ImperfectaDocument8 pagesOsteogenesi ImperfectaAna Priscila RamirezNo ratings yet
- Tto de La Osteoporosis - 2020Document16 pagesTto de La Osteoporosis - 2020GilbertoNo ratings yet
- Bone Turnover Markers: Use in Fracture Prediction: Tatiane Vilaca, Fatma Gossiel, and Richard EastellDocument7 pagesBone Turnover Markers: Use in Fracture Prediction: Tatiane Vilaca, Fatma Gossiel, and Richard EastellPoramate PITAK-ARNNOPNo ratings yet
- Clinical Aspects, Pathology and Pathophysiology of OsteoarthritisDocument3 pagesClinical Aspects, Pathology and Pathophysiology of OsteoarthritisOscar NgNo ratings yet
- Metabolic Bone DiseaseDocument6 pagesMetabolic Bone Diseasekartini ciatawiNo ratings yet
- Bone Erosion Rheumatoid Arthritis Mechanisms Diagnosis&TreatmentDocument9 pagesBone Erosion Rheumatoid Arthritis Mechanisms Diagnosis&TreatmentMaría RodríguezNo ratings yet
- Bones & Joints Pathology 4thDocument8 pagesBones & Joints Pathology 4thlovelyc95No ratings yet
- Osteoporosis After TransplantationDocument8 pagesOsteoporosis After TransplantationDennis KabuchwaNo ratings yet
- Nihms-1007745 TNF BoneDocument15 pagesNihms-1007745 TNF BoneAndyka YasaNo ratings yet
- Prof. Dr. Hazem Abd El-Azeem Professor of Orthopaedic Surgery Cairo UniversityDocument47 pagesProf. Dr. Hazem Abd El-Azeem Professor of Orthopaedic Surgery Cairo UniversitytarikeopsNo ratings yet
- Bone Grafts and Their SubstitutesDocument4 pagesBone Grafts and Their SubstitutesIndriastuti SoetomoNo ratings yet
- Lecture 31 Osteoporosis Pathophys FlattenedDocument3 pagesLecture 31 Osteoporosis Pathophys FlattenedAhmed Mashaly100% (1)
- Death&Birth 00Document23 pagesDeath&Birth 00kyz79No ratings yet
- Hyperphosphatemia CKDDocument9 pagesHyperphosphatemia CKDNico MirassoNo ratings yet
- CCCCCCCDocument4 pagesCCCCCCCGali Alfaro ZagalNo ratings yet
- Os 1 251Document7 pagesOs 1 251mukhlis akmalNo ratings yet
- Osteoporosis: Current Concepts: Ibrahim Akkawi Hassan ZmerlyDocument6 pagesOsteoporosis: Current Concepts: Ibrahim Akkawi Hassan ZmerlyDimas M IlhamNo ratings yet
- Module 4 HomeworkDocument4 pagesModule 4 HomeworkCj LinceNo ratings yet
- Reviseddd (Mia)Document16 pagesReviseddd (Mia)kuro hanabusaNo ratings yet
- MSE Research 1Document11 pagesMSE Research 1kuro hanabusaNo ratings yet
- Nursing - Assessment - (Mse) (Josol)Document5 pagesNursing - Assessment - (Mse) (Josol)kuro hanabusaNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Inference Goal Nursing Intervention Rationale EvaluationDocument1 pageNursing Care Plan Cues Nursing Diagnosis Inference Goal Nursing Intervention Rationale Evaluationkuro hanabusaNo ratings yet
- Nursing Care Plan 1Document5 pagesNursing Care Plan 1kuro hanabusaNo ratings yet
- Date Identified: July 13, 2021 Date Evaluated: July 20, 2021 TetengDocument5 pagesDate Identified: July 13, 2021 Date Evaluated: July 20, 2021 Tetengkuro hanabusaNo ratings yet
- Anxiety NCPDocument2 pagesAnxiety NCPkuro hanabusaNo ratings yet
- Drug Study (Acamprosate (Campral) and Bupropion)Document5 pagesDrug Study (Acamprosate (Campral) and Bupropion)kuro hanabusaNo ratings yet
- Quiz (Perfect)Document3 pagesQuiz (Perfect)kuro hanabusaNo ratings yet
- Drug Study (Loxapine, Haloperidol)Document5 pagesDrug Study (Loxapine, Haloperidol)kuro hanabusa100% (2)
- Program Design (Dance Therapy)Document3 pagesProgram Design (Dance Therapy)kuro hanabusaNo ratings yet
- Pre-Test (B)Document7 pagesPre-Test (B)kuro hanabusaNo ratings yet
- Psychoanalysis and Psychodynamic TherapiesDocument51 pagesPsychoanalysis and Psychodynamic Therapieskuro hanabusaNo ratings yet
- Journal Reflection On Nursing Care PlanDocument9 pagesJournal Reflection On Nursing Care Plankuro hanabusaNo ratings yet
- Journal Reflection On Mental Status Examination 1Document9 pagesJournal Reflection On Mental Status Examination 1kuro hanabusaNo ratings yet
- Journal Reflection On Therapeutic ModalitiesDocument23 pagesJournal Reflection On Therapeutic Modalitieskuro hanabusaNo ratings yet
- Psychoanalysis and Psychodynamic TherapiesDocument51 pagesPsychoanalysis and Psychodynamic Therapieskuro hanabusaNo ratings yet
- Mental Status Examination: Concerns and AddictionDocument2 pagesMental Status Examination: Concerns and Addictionkuro hanabusaNo ratings yet
- DocxDocument53 pagesDocxkuro hanabusaNo ratings yet
- Francisco Arcellana: 4 Life Lessons That Can Be Derived From The StoryDocument1 pageFrancisco Arcellana: 4 Life Lessons That Can Be Derived From The Storykuro hanabusaNo ratings yet
- Philippine Literature During American RegimeDocument13 pagesPhilippine Literature During American Regimekuro hanabusaNo ratings yet
- CNT Manual 7th EditionDocument85 pagesCNT Manual 7th EditionStoopidHead100% (1)
- Note TakingDocument57 pagesNote TakingLee이서영No ratings yet
- Drug Presentation On Anti-Hypertensive: All India Institute of Medical and Science New Delhi 2021-2022Document12 pagesDrug Presentation On Anti-Hypertensive: All India Institute of Medical and Science New Delhi 2021-2022Priya SinghNo ratings yet
- CLPNM PD Nursing Foot CareDocument9 pagesCLPNM PD Nursing Foot CareMourad LAKHOUADRANo ratings yet
- Pre AnestesiDocument64 pagesPre AnestesiKevin YonathanNo ratings yet
- Dry Eye Syndrome - Basic and Clinical PerspectivesDocument129 pagesDry Eye Syndrome - Basic and Clinical PerspectivesPutri kartiniNo ratings yet
- Cardiovascular Hypertensive Crisis Recent EvidenceDocument6 pagesCardiovascular Hypertensive Crisis Recent Evidenceagustinaw1981No ratings yet
- Incident Classification: Class I Incidents: DateDocument3 pagesIncident Classification: Class I Incidents: DateJuan Ernesto Benavides VNo ratings yet
- Rheumatoid Arthritis PathophysiologyDocument3 pagesRheumatoid Arthritis PathophysiologyArunNo ratings yet
- CC1 Lab Manual FinalDocument14 pagesCC1 Lab Manual FinalMelody PardilloNo ratings yet
- Review Article: Biliary Atresia: 50 Years After The First KasaiDocument16 pagesReview Article: Biliary Atresia: 50 Years After The First Kasaibela RachmanNo ratings yet
- Genacol Instant: The Most Complete Reference Booklet About CollagenDocument28 pagesGenacol Instant: The Most Complete Reference Booklet About CollagendiosesatomicsNo ratings yet
- Riqas Ri RQ9142 11aDocument6 pagesRiqas Ri RQ9142 11aGrescia Ramos VegaNo ratings yet
- BerirabDocument6 pagesBerirabfateme.tf.1999No ratings yet
- Chd. AmiDocument4 pagesChd. AmiDead shotNo ratings yet
- Therapeutic Communication Between Nurse - PatientDocument10 pagesTherapeutic Communication Between Nurse - PatientLucy P PutriNo ratings yet
- Diagnostic Test For Endocrine DisordersDocument15 pagesDiagnostic Test For Endocrine DisordersRichard Deo R. Alave100% (1)
- Neonatal Sepsis - A Review: January 2012Document9 pagesNeonatal Sepsis - A Review: January 2012Tiwi QiraNo ratings yet
- THE Beginner'S Guide To Earthing: Brought To You byDocument23 pagesTHE Beginner'S Guide To Earthing: Brought To You byPopescu AndreeaNo ratings yet
- The Fastest Way To Sleep?Document7 pagesThe Fastest Way To Sleep?NNorameenNo ratings yet
- WHO Global Pandemic Phases and The Stages For Federal Government ResponseDocument4 pagesWHO Global Pandemic Phases and The Stages For Federal Government ResponseMara Luisa PanopioNo ratings yet
- Proprioception, Vestibular & CoordinationDocument28 pagesProprioception, Vestibular & Coordinationzm2h8hpsq8No ratings yet
- Mesotherapy in The Treatment of MusculoskeletalDocument11 pagesMesotherapy in The Treatment of MusculoskeletalArmin ArceoNo ratings yet
- Pe AnswerssDocument9 pagesPe AnswerssAngela Ruth MoranNo ratings yet
- Hesi Comprehensive Review For The Nclex RN Examination 6E Oct 3 2019 - 0323582451 - Elsevier Hesi Full ChapterDocument67 pagesHesi Comprehensive Review For The Nclex RN Examination 6E Oct 3 2019 - 0323582451 - Elsevier Hesi Full Chaptertracy.zimmer564100% (17)
- Concept PaperDocument3 pagesConcept PaperNndaydna0% (1)