Professional Documents
Culture Documents
A Case Report of Rare Acute Ischemic Stroke Due To Meningeal Irritation
A Case Report of Rare Acute Ischemic Stroke Due To Meningeal Irritation
Uploaded by
Dayu Punik ApsariCopyright:
Available Formats
You might also like
- Intracerebral Haemorrhage: Disease PrimersDocument18 pagesIntracerebral Haemorrhage: Disease PrimersMarlon VillanuevaNo ratings yet
- Case Study On ManiaDocument30 pagesCase Study On ManiaIOM BNS78% (9)
- New HSV EraserDocument108 pagesNew HSV EraserDashar WilsonNo ratings yet
- A 19-Year-Old Man With Sickle Cell Disease Presenting With Spinal Infarction: A Case ReportDocument6 pagesA 19-Year-Old Man With Sickle Cell Disease Presenting With Spinal Infarction: A Case ReportJabber PaudacNo ratings yet
- Ischemic Cerebral Stroke Case Report, Complications and Associated FactorsDocument5 pagesIschemic Cerebral Stroke Case Report, Complications and Associated Factorsfaradilla wiyandaNo ratings yet
- Ischemic Cerebral Stroke Case Report, Complications and Associated FactorsDocument7 pagesIschemic Cerebral Stroke Case Report, Complications and Associated FactorsAlfa DexterNo ratings yet
- Acute Ischemic Stroke: Clinical PracticeDocument8 pagesAcute Ischemic Stroke: Clinical PracticeDorina FrunzeNo ratings yet
- Acute Ischaemic Stroke in Infective Endocarditis: Pathophysiology and Clinical Outcomes in Patients Treated With Reperfusion TherapyDocument13 pagesAcute Ischaemic Stroke in Infective Endocarditis: Pathophysiology and Clinical Outcomes in Patients Treated With Reperfusion TherapyPatrick NunsioNo ratings yet
- Biomedicines 10 02830 v2Document12 pagesBiomedicines 10 02830 v2Septi Dimas jamaludinNo ratings yet
- Vascular Instability and Neurological Morbidity in Sickle Cell Disease: An Integrative Framework.Document21 pagesVascular Instability and Neurological Morbidity in Sickle Cell Disease: An Integrative Framework.Arturo Martí-CarvajalNo ratings yet
- Oral Medicine: Editor: Martin S. GreenbergDocument12 pagesOral Medicine: Editor: Martin S. GreenbergSuseno AjiNo ratings yet
- Acute Stroke ArticleDocument10 pagesAcute Stroke ArticlenesredeNo ratings yet
- Ischemic Stroke in A Young Male Patient in Rural Uganda, Case Report.Document3 pagesIschemic Stroke in A Young Male Patient in Rural Uganda, Case Report.International Journal of Innovative Science and Research TechnologyNo ratings yet
- Hemato Si StrokeDocument6 pagesHemato Si Strokeseaside16girlNo ratings yet
- 1 s2.0 S2589238X23000098 Main PDFDocument4 pages1 s2.0 S2589238X23000098 Main PDFAnastasia ThaliaNo ratings yet
- Nervous SystemDocument62 pagesNervous Systemmyat252No ratings yet
- Cerebral Small Vessel Disease: Review ArticleDocument21 pagesCerebral Small Vessel Disease: Review ArticleSiklus AnakNo ratings yet
- Cerebral ToxoplasmaDocument4 pagesCerebral ToxoplasmaTheodoreNo ratings yet
- Infective EndocarditisDocument5 pagesInfective Endocarditismustafa malvi100% (1)
- Myocarditis Due To Systemic Lupus Erythematosus Associated With Cardiogenic ShockDocument3 pagesMyocarditis Due To Systemic Lupus Erythematosus Associated With Cardiogenic ShockAkbar IskandarNo ratings yet
- Are Acute Subdural Hematomas Possible Without Head Trauma?: Case SeriesDocument5 pagesAre Acute Subdural Hematomas Possible Without Head Trauma?: Case SeriesSucipto HartonoNo ratings yet
- Non Hemorrhagic Stroke (SNH) and Interleukin-6 (Il6) : A Literature ReviewDocument10 pagesNon Hemorrhagic Stroke (SNH) and Interleukin-6 (Il6) : A Literature ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cardiovascular Stroke Prevention and Management Using The Principles of Cellular MedicineDocument4 pagesCardiovascular Stroke Prevention and Management Using The Principles of Cellular MedicineInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Multi-Infarct Dementia With Acute Intra Cerebral Hemorrhage and Chronic Subdural Hygromas: A Case StudyDocument4 pagesMulti-Infarct Dementia With Acute Intra Cerebral Hemorrhage and Chronic Subdural Hygromas: A Case StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- What Is The Pathophysiology of Hemifacial Spasm?Document3 pagesWhat Is The Pathophysiology of Hemifacial Spasm?NabilaNo ratings yet
- Spontaneous Intracerebral Hemorrhage: Pathogenesis, Clinical Features, and DiagnosisDocument25 pagesSpontaneous Intracerebral Hemorrhage: Pathogenesis, Clinical Features, and DiagnosisBryan Tam ArevaloNo ratings yet
- HHS Public Access: Subarachnoid Hemorrhage Presenting With Second-Degree Type I Sinoatrial Exit Block: A Case ReportDocument15 pagesHHS Public Access: Subarachnoid Hemorrhage Presenting With Second-Degree Type I Sinoatrial Exit Block: A Case Reportcitra annisa fitriNo ratings yet
- Adolescent Onset of Acute Heart FailureDocument19 pagesAdolescent Onset of Acute Heart FailureVeronica Romero MouthonNo ratings yet
- MainDocument7 pagesMainSonia khanNo ratings yet
- Ischemic Stroke A Comparative Retrospective Study: Experience of Military Hospital of MeknesDocument20 pagesIschemic Stroke A Comparative Retrospective Study: Experience of Military Hospital of MeknesIJAR JOURNALNo ratings yet
- Cerebral Small Vessel DiseaseDocument11 pagesCerebral Small Vessel Diseaseyousra yatrebNo ratings yet
- Noninfectious Cerebral Vasculitis in Children: Indianapolis, IndianaDocument15 pagesNoninfectious Cerebral Vasculitis in Children: Indianapolis, IndianaNathaly LapoNo ratings yet
- Acute Viral Myocarditis: Epidemiology and Pathophysiology: Lara Shekerdemian, MD, MRCP Desmond Bohn, MB, MRCPDocument6 pagesAcute Viral Myocarditis: Epidemiology and Pathophysiology: Lara Shekerdemian, MD, MRCP Desmond Bohn, MB, MRCPMike ShufflebottomNo ratings yet
- Ich Magistris, 2013Document8 pagesIch Magistris, 2013ignasachyntiaNo ratings yet
- Britton Et Al-2015-Internal Medicine JournalDocument14 pagesBritton Et Al-2015-Internal Medicine JournalfrizkapfNo ratings yet
- A Prospective Study of Prescribing Pattern in The Management of Stroke at A Tertiary Care HospitalDocument6 pagesA Prospective Study of Prescribing Pattern in The Management of Stroke at A Tertiary Care HospitalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Infective EndocarditisDocument13 pagesInfective EndocarditisIbrahimNo ratings yet
- Diabetes, Stroke, and Neuroresilience Looking BeyondDocument21 pagesDiabetes, Stroke, and Neuroresilience Looking BeyondMaudia IndrianiiNo ratings yet
- Intracerebral-hemorrhage-in-translational-research_2020_Brain-HemorrhagesDocument6 pagesIntracerebral-hemorrhage-in-translational-research_2020_Brain-HemorrhagesLeandro AntivilNo ratings yet
- StrokeDocument17 pagesStrokeluis sanchezNo ratings yet
- Bruce C V Campbell Ischaemic Stroke 2019Document22 pagesBruce C V Campbell Ischaemic Stroke 2019yiyecNo ratings yet
- Cerebellar Stroke in A COVID-19 Infected Patient. A Case ReportDocument6 pagesCerebellar Stroke in A COVID-19 Infected Patient. A Case ReportMuhammad Reza FirdausNo ratings yet
- The Risk Factor of Recurrence Stroke Among Stroke and Transient Ischemic Attack Patients in IndonesiaDocument11 pagesThe Risk Factor of Recurrence Stroke Among Stroke and Transient Ischemic Attack Patients in Indonesiafarah maulida martaNo ratings yet
- IJRPR15417Document2 pagesIJRPR15417Gleeware LimitedNo ratings yet
- StrokeDocument17 pagesStrokeJonathan Gutierrez RiosNo ratings yet
- HSA Aneurism+â-Ítica ICM 2014Document4 pagesHSA Aneurism+â-Ítica ICM 2014Ellys Macías PeraltaNo ratings yet
- Nihms 1873457Document15 pagesNihms 1873457Hanssel Viramontes CastroNo ratings yet
- 6 Giant Cell Arteritis Dan PolireumalgiaDocument8 pages6 Giant Cell Arteritis Dan PolireumalgiaRifqiNo ratings yet
- Hypertension in The Elderly: ArticleDocument14 pagesHypertension in The Elderly: Articleaulia nurfadilahNo ratings yet
- DownloadDocument7 pagesDownloadsitorus.family2009No ratings yet
- PICpediatricDocument14 pagesPICpediatricAtzi FNo ratings yet
- Demensia Vaskuler 2Document20 pagesDemensia Vaskuler 2Adam MochtarNo ratings yet
- Concise Clinical Review: Intracranial HemorrhageDocument9 pagesConcise Clinical Review: Intracranial HemorrhageWanda FlorenciaNo ratings yet
- Seminar: Epidemiology and Risk FactorsDocument17 pagesSeminar: Epidemiology and Risk FactorsNelly ElizabethNo ratings yet
- Vascular DementiaDocument8 pagesVascular Dementiaddelindaaa100% (1)
- Lupus Myocarditis A Rare CaseDocument3 pagesLupus Myocarditis A Rare Casea.rohman2700No ratings yet
- Challenges and Opportunities in Pediatric Heart Failure and TransplantationDocument15 pagesChallenges and Opportunities in Pediatric Heart Failure and TransplantationvijuNo ratings yet
- Cardiac Sarcoidosis: Abdul R Doughan, Byron R WilliamsDocument7 pagesCardiac Sarcoidosis: Abdul R Doughan, Byron R WilliamsBhagya Narayan PanditNo ratings yet
- Moyamoya Epidemiology, Presentation, and DiagnosisDocument9 pagesMoyamoya Epidemiology, Presentation, and DiagnosisshiloinNo ratings yet
- Cardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesFrom EverandCardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesNo ratings yet
- Comprehensive Insights into Acute Arterial Occlusion: Pathways, Prevention, and Holistic CareFrom EverandComprehensive Insights into Acute Arterial Occlusion: Pathways, Prevention, and Holistic CareNo ratings yet
- Arterial Disorders: Definition, Clinical Manifestations, Mechanisms and Therapeutic ApproachesFrom EverandArterial Disorders: Definition, Clinical Manifestations, Mechanisms and Therapeutic ApproachesAdel BerbariNo ratings yet
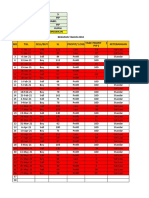
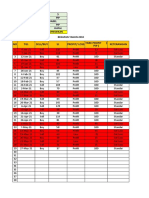
- NO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Document10 pagesNO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Dayu Punik ApsariNo ratings yet
- MM UnikDocument47 pagesMM UnikDayu Punik ApsariNo ratings yet
- NO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Document19 pagesNO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Dayu Punik ApsariNo ratings yet
- NO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Document12 pagesNO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Dayu Punik ApsariNo ratings yet
- BBMA Ibnu AdnanDocument32 pagesBBMA Ibnu AdnanDayu Punik ApsariNo ratings yet
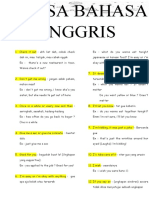
- Kata Sehari HariDocument3 pagesKata Sehari HariDayu Punik ApsariNo ratings yet
- Frasa Bahasa InggrisDocument19 pagesFrasa Bahasa InggrisDayu Punik ApsariNo ratings yet
- Research Article: Efficacy of Aloe Vera, Ananas Comosus, and SansevieriaDocument8 pagesResearch Article: Efficacy of Aloe Vera, Ananas Comosus, and SansevieriaDayu Punik ApsariNo ratings yet
- International Journal of Pharmaceutics: SciencedirectDocument11 pagesInternational Journal of Pharmaceutics: SciencedirectDayu Punik ApsariNo ratings yet
- Suffering: and Montreal THEDocument5 pagesSuffering: and Montreal THEDayu Punik ApsariNo ratings yet
- Metatrader DescriptionDocument1 pageMetatrader DescriptionDayu Punik ApsariNo ratings yet
- Definisi AsmaDocument12 pagesDefinisi AsmaDayu Punik ApsariNo ratings yet
- Government College of Nursing:, Jodhpur (Raj.)Document7 pagesGovernment College of Nursing:, Jodhpur (Raj.)priyankaNo ratings yet
- Anaplastic Thyroid CancerDocument40 pagesAnaplastic Thyroid Cancershita febrianaNo ratings yet
- Commercial Quality of Seed PotatoesDocument112 pagesCommercial Quality of Seed PotatoesPedro Daniel LeivaNo ratings yet
- Funda Reviewer CADocument33 pagesFunda Reviewer CARichie Marie BajaNo ratings yet
- Colon Cancer Case StudyDocument21 pagesColon Cancer Case StudyInfection QcghNo ratings yet
- Met 201Document9 pagesMet 201minamessak98No ratings yet
- 3.psychiatric HX and MSE (1) According To DSM-5Document96 pages3.psychiatric HX and MSE (1) According To DSM-5sopsychaNo ratings yet
- Ben20Diazepine Withdrawal Symptom Questionnaire: Yes ModerateDocument1 pageBen20Diazepine Withdrawal Symptom Questionnaire: Yes Moderatesharp8787No ratings yet
- Medicine For Mountaineering and Other Wilderness Activities (6th Edition) (2010) (James A. Wilkerson)Document2,899 pagesMedicine For Mountaineering and Other Wilderness Activities (6th Edition) (2010) (James A. Wilkerson)zaellixaNo ratings yet
- Asthma Brochure 2015Document2 pagesAsthma Brochure 2015Eliseo RamirezNo ratings yet
- Bleeding Disorders: LCDR Art GeorgeDocument54 pagesBleeding Disorders: LCDR Art GeorgepallavberiNo ratings yet
- Top 100 Diagnoses in Neurology Core Features, Synopses, IllustrationsDocument445 pagesTop 100 Diagnoses in Neurology Core Features, Synopses, IllustrationspondebernardoNo ratings yet
- DRUG+STUDY NaprexDocument2 pagesDRUG+STUDY NaprexJoevence Gazo CuaresmaNo ratings yet
- Case AnalysisDocument27 pagesCase AnalysisIrish Eunice FelixNo ratings yet
- The Gluten Connection - Walter VeithDocument5 pagesThe Gluten Connection - Walter VeithGabriela Rojas FusNo ratings yet
- Vitamin B6: Health and NutritionDocument16 pagesVitamin B6: Health and NutritionKreena PatelNo ratings yet
- 501MCQforclinicalpharmacylast IvrtjnDocument119 pages501MCQforclinicalpharmacylast Ivrtjnد.شەماڵ احمد : پزیشکی دەرمانساز100% (1)
- What Is The Difference Between The Mind and The Brain-1Document2 pagesWhat Is The Difference Between The Mind and The Brain-1Amir Nazir100% (1)
- Alfuzosin HCL (Xatral XL 10mg)Document6 pagesAlfuzosin HCL (Xatral XL 10mg)asdwasdNo ratings yet
- Drug Study #2Document3 pagesDrug Study #2Sarah Kaye BañoNo ratings yet
- HEALTH TALK of EncopresisDocument15 pagesHEALTH TALK of EncopresisAmit RanjanNo ratings yet
- RHD Poster - ODADocument1 pageRHD Poster - ODASinclair Broadcast Group - EugeneNo ratings yet
- Name: - Score: - Teacher: - DateDocument2 pagesName: - Score: - Teacher: - DatePauline Erika CagampangNo ratings yet
- Pathoma - Chapter 1Document13 pagesPathoma - Chapter 1Jonathan AiresNo ratings yet
- The Persistent Stigma and Disregard For Mental Health in Sri LankaDocument3 pagesThe Persistent Stigma and Disregard For Mental Health in Sri Lankadevmini herathNo ratings yet
- 2004 - Number Series For Psychological Normalization - Book1Document208 pages2004 - Number Series For Psychological Normalization - Book1Carla Perin67% (3)
- THE Health Emergency Management: Doh - Ro XiDocument58 pagesTHE Health Emergency Management: Doh - Ro XiCreativ Worx100% (3)
- Chapter 4 - Servsafe - 6e Edited PDFDocument4 pagesChapter 4 - Servsafe - 6e Edited PDFdevvy anneNo ratings yet
A Case Report of Rare Acute Ischemic Stroke Due To Meningeal Irritation
A Case Report of Rare Acute Ischemic Stroke Due To Meningeal Irritation
Uploaded by
Dayu Punik ApsariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Case Report of Rare Acute Ischemic Stroke Due To Meningeal Irritation
A Case Report of Rare Acute Ischemic Stroke Due To Meningeal Irritation
Uploaded by
Dayu Punik ApsariCopyright:
Available Formats
World Journal of Neuroscience, 2018, 8, 171-177
http://www.scirp.org/journal/wjns
ISSN Online: 2162-2019
ISSN Print: 2162-2000
A Case Report of Rare Acute Ischemic Stroke
Due to Meningeal Irritation
Reem AlSherooqi1, Jad Alkhoury1, Moiz Bakhiet1,2*
1
Department of Internal Medicine, King Hamad University Hospital Princess Al-Jawhara Center for Genetics and Inherited
Diseases, Arabian Gulf University, Manama, Bahrain
2
Department of Molecular Medicine, College of Medicine and Medical Sciences, Princess Al-Jawhara Center for Genetics and
Inherited Diseases, Arabian Gulf University, Manama, Bahrain
How to cite this paper: AlSherooqi, R., Abstract
Alkhoury, J. and Bakhiet, M. (2018) A Case
Report of Rare Acute Ischemic Stroke Due Stroke is a rapidly developing symptom or sign of loss of cerebral function
to Meningeal Irritation. World Journal of secondary to interruption of the blood supply due to a thrombus or hemorr-
Neuroscience, 8, 171-177. hage. These diseased vessels are usually affected by well-recognized risk fac-
https://doi.org/10.4236/wjns.2018.82015
tors, but in some cases other rare conditions may be related to stroke devel-
Received: March 30, 2018 opment. Herein, we introduce one of these rare stroke conditions in a
Accepted: May 4, 2018 37-year-old previously healthy male who presented to the emergency depart-
Published: May 7, 2018 ment with misleading symptoms and signs of reduced level of consciousness,
isolated medical 3rd nerve palsy and possible drug overdose. A thorough neu-
Copyright © 2018 by authors and
Scientific Research Publishing Inc. rological examination and investigation demonstrated a case of acute ischemic
This work is licensed under the Creative stroke as a consequence of meningeal irritation with an underlying inflam-
Commons Attribution International matory response. The patient was treated simultaneously for both conditions
License (CC BY 4.0). and responded dramatically with full recovery upon discharge. Thus, consid-
http://creativecommons.org/licenses/by/4.0/
eration of acute stroke in patients with no previous known risk factors is
Open Access
highly recommended especially with unusual neurological findings.
Keywords
Meningitis, Weakness, Diplopia, Photophobia, EEG
1. Introduction
Stroke is recognized as the third leading cause of death worldwide and is asso-
ciated with permanent disability [1]. Traditional vascular risk factors affecting
blood vessels and circulation are the most common causes of stroke. These fac-
tors are common in young adults with ischemic stroke, which include Dyslipi-
demia, smoking, Hypertension, Patent Foramen Ovale, large-artery atheroscle-
rosis, small-vessel occlusion and cardioembolism [2].
DOI: 10.4236/wjns.2018.82015 May 7, 2018 171 World Journal of Neuroscience
R. AlSherooqi et al.
There are many less common causes of stroke which can be sub classified into
inflammatory and non-inflammatory vessel disorders, hematological disorders,
prothrombotic (clotting) disorders, Migraine-Related Stroke and Cerebral Ven-
ous Thrombosis (CVT). Examples of non-inflammatory blood vessel diseases
include Fibromuscular Dysplasia—a disorder that results in an abnormal devel-
opment of cells in the wall of arteries [3], Reversible Cerebral Vasoconstriction
Syndromes [4], radiation therapy for cancers of the head and neck [5], Moya-
moya disease—a rare disorder causing blocked arteries in the basal ganglia [6],
Fabry Disease—an X-linked rare genetic disorder causing lipids to deposit in the
internal lining of blood vessels [7]. On the other hand, the non-infectious and
inflammatory vasculitides that lead to stroke formation comprise Takayasu dis-
order, Giant Cell Arteritis, Churg-Strauss vasculitis, Wegener’s Granulomatosis,
Polyarteritis Nodosa, Buerger’s disease, Microscopic Polyangitis, Amylo-
id-β-related Angiitis, and isolated vasculitis of the central nervous system (CNS)
[8].
Ischemic stroke may also be associated with several blood coagulopathies af-
fecting the red blood cells, platelet function, clotting factors or fibrinolysis [9].
Antiphospholipid Antibody Syndrome and Sickle Cell Disease may also be asso-
ciated with the development of ischemic stroke [10] [11]. There is evidence that
migraine patients especially those with aura, may develop stroke through an
unknown mechanism. Nevertheless, migraine was also found to be associated
with platelet abnormalities and clotting disorders predisposing to ischemic
events [12]. Additionally, CVT is a rare cause of stroke [13].
Meningitis is the inflammation of the meninges due to bacterial, viral, or fun-
gal infections. Other causes may include carcinoma and drugs. Diagnosis can be
made clinically and biochemically through clinical symptoms including head-
ache and photophobia as well as signs such as Kernig’s and Brudzinski’s signs.
Detecting white blood cells (WBCs) in the CSF analysis can also aid our diagno-
sis. Meningitis can be classified into acute of chronic based on the onset of
symptoms, CSF analysis and underlying conditions. Acute meningitis presents
in hours or days [14].
This paper reports a rare case of acute ischemic stroke in a young healthy
male that occurred as a consequence of meningeal irritation thus presenting with
atypical signs and symptoms.
2. Case
A 37-year-old previously healthy male presented to the emergency room (ER)
with complaints of weakness and fatigue, double vision and photophobia of few
hours’ duration. It was not associated with fever, vomiting, abdominal pain or
any change in bowel habits. There was no chest pain, palpitations, shortness of
breath, paroxysmal nocturnal dyspnea or loss of consciousness. No recent me-
dications were started.
The patients’ past medical history (PMH), past surgical history (PSH) and
DOI: 10.4236/wjns.2018.82015 172 World Journal of Neuroscience
R. AlSherooqi et al.
family history (FH) were unremarkable. He was not on regular medications with
no allergies and denied any history of smoking.
On examination, the patient was vitally stable and afebrile. His abdominal,
respiratory and cardiovascular examinations were unremarkable. Neurological
examination was difficult to assess, as patient was very drowsy. However, plan-
tars were down going, and pupils were pinpoint bilaterally. There were no ob-
vious needle marks and lower limb examination was normal.
Laboratory investigations (hematological and biochemical) were all within
normal levels. CT Brain was also done at the level of the ER that was unremark-
able.
The patient was admitted to the ward with the initial impression of reduced
level of consciousness with isolated medical 3rd nerve palsy. Drug overdose was a
differential at the time of admission. Drug levels (Acetaminophen), urine toxi-
cology and MRI (Magnetic resonance imaging) brain were requested. The pa-
tient also received a dose of Naloxone that improved his level of consciousness
for a short period of time.
The Neurologist saw the patient the next day in the ward, and examination
showed response to painful stimuli. He was vitally stable with neck rigidity and
positive Kernig’s sign. The right pupil was constricted whereas the left one was
dilated. Plantars were down going bilaterally.
A differential diagnosis of absence seizure, meningitis and possible stroke was
made. The patient was kept in isolation and planned for lumbar puncture (LP).
He was also scheduled for an electroencephalogram (EEG), MRI brain and Ca-
rotid Doppler. After LP was done, he was started on Ceftriaxone 2 g once daily,
Vancomycin 1600 mg every 8 hours intravenously and Acyclovir 800 mg every 8
hours intravenously. He was also started on Keppra 1 g twice daily intravenously
as a prophylaxis for seizure disorder.
When patient was reviewed the next day, he was fully conscious. Laboratory
investigations including complete blood count (CBC), electrolytes and calcium,
C-reactive protein (CRP), hepatitis profile, Syphilis, HIV, Toxoplasmosis screen,
ANA and lipid profile were normal. However, Protein C and S were ele-
vated—>141% and >126% respectively. CSF analysis showed elevated protein
level (80 mg/dl). The gram stain showed no organism, acid-fast bacilli (AFB)
negative and cultures were negative.
MRI Brain showed acute infarcts in bilateral thalamus, meningeal irritation
(Figure 1) and bilateral sinusitis. There were sharp wave discharges in both
temporo-occipital regions on his EEG (Figure 2). Carotid Doppler showed no
stenosis or atherosclerotic plaques.
Day 3 of his admission, the patient was conscious, alert and oriented. Neck ri-
gidity improved and Kernig’s sign was negative. The patient was kept under ob-
servation for one week and was discharged in a good and stable condition.
3. Discussion
Per definition, meningitis is inflammation of the meninges of the CNS [14].
DOI: 10.4236/wjns.2018.82015 173 World Journal of Neuroscience
R. AlSherooqi et al.
Axial Diffusion-weighted magnetic resonance imaging (ADW-MRI) revealing hyperintensities in bilateral thalamus (circle)
suggesting acute infarctions, because of restricted diffusion in the corresponding sites, and probably due to the early menin-
gitic vascular complications. Arrows depict meningeal irritation/inflammation.
Figure 1. Magnetic resonance imaging (MRI) of the brain.
A 21 channel digital video EEG recording performed in the EEG laboratory using the standard 10 - 20 International Elec-
trode Placement System. Hyperventilation and Photic stimulation was done. EEG was recorded in a wake stage. The post-
erior dominant rhythm consisted of well-organized and symmetrical 8 - 9 Hz alpha activity predominantly seen in the
posterior head region. This activity was reactive to eye opening. Photic stimulation induced the background activity bilate-
rally. Intermittent burst of sharp wave discharges in both the temporo-occipital regions were noted.
Figure 2. Electroencephalogram (EEG).
DOI: 10.4236/wjns.2018.82015 174 World Journal of Neuroscience
R. AlSherooqi et al.
Stroke—as stated by the American Stroke Association (ASA) and the American
Heart Association (AHA)—is a CNS (brain and/or spinal cord) infarction, or
death of retinal cells as a result of ischemia, established by clinical signs of per-
manent damage, neuroimaging and neuropathological evidence. Ischemic stroke
refers to a CNS infarction attended by obvious symptoms, whereas silent infarc-
tion produces no known symptoms [15].
The common causes of ischemic stroke are related to traditional risk factors
affecting the cerebrovascular circulation. Stroke was considered as symptoms
that are quickly arising or signs of nonappearance of cerebral function without
obvious reasons except for a vascular cause. The case presented in this study dis-
play a young adult male who was not known to have any medical condition (es-
pecially of vascular origin) or any risk factor for stroke. The only triggering fac-
tor for his stroke was the meningeal irritation that was most probably related to
an inflammatory process rather than an infection.
It has been reported previously that certain inflammatory processes of sys-
temic origin and infectious agents can lead to the development of stroke. Ionita
CC and colleagues have looked into different infections and their relationship to
acute ischemic stroke. They demonstrated that infectious endocarditis, menin-
goencephalitis, and human immunodeficiency virus infections were a direct
cause of stroke and concluded that infections, whether acute or chronic, can
cause acute ischemic stroke. The most likely explanation is the development of
enhanced immunohematologic changes and atherosclerosis [16]. However, in
our case there was no infectious agent isolated and no CSF abnormality was de-
tected to confirm bacterial or viral (aseptic) meningitis. High protein level was
suggestive of an inflammatory process which might have caused the meningeal
irritation. Meningitis was also evident with the clinical signs and symptoms. In
addition, EEG findings (Figure 2) and meningeal irritation on MRI also sup-
ported our diagnosis (Figure 1). The cause of inflammation that resulted in the
meningeal irritation is not clear to us, but it could be secondary to previous ex-
posure to an irritating agent or an infection that has resolved and the products of
that infectious agent such as endotoxin or viral protein has generated a
pro-inflammatory cytokine response. It is well known that inflammation leads to
activation of coagulation and that pro-inflammatory cytokines can activate the
coagulation system and down-regulate important physiologic anticoagulant
processes resulting in vascular complications thus leading to stroke [17]. In-
flammatory vasculitis subsequent to meningeal irritation/inflammation can
cause brain infarction as well [8]. The patient improved after a combination of
anti-viral, anti-bacterial and anti-epileptic medications that were all required in
the management and were given empirically as the underlying causative agent
and mechanism were not identified.
4. Conclusion
Acute stroke should be considered in all age groups with no previous acknowl-
DOI: 10.4236/wjns.2018.82015 175 World Journal of Neuroscience
R. AlSherooqi et al.
edged risk factors affecting blood vessels and circulation among other possible
differential diagnosis. Such factors may include inflammatory processes affecting
the meninges and/or the brain.
Acknowledgements
We gratefully acknowledge King Hamad University Hospital for supporting this
case study.
Funding
This work was supported by the Department of Internal Medicine, King Hamad
University Hospital.
Ethics Approval and Consent to Participate
This is a case report of standard treatment for an unusual presentation of a dis-
ease. There was no treatment given to the patient outside the standard of care.
We confirm that the case report was approved by the institute’s committee on
human research to be submitted for publication.
Consent to Publish
Written informed consent was obtained from the patient for his anonymized
information to be published in this article.
Availability of Data and Materials
Data supporting the conclusions of this article are presented in the manuscript.
Authors’ Contributions
RAS contributed to acquisition of data, analysis and interpretation of data. JA
was involved in drafting the manuscript and revising it critically for important
intellectual content. MB is the principle investigator (consultant) and wrote the
paper.
References
[1] Donnan, G.A., Fisher, M., Macleod, M. and Davis, S.M. (2008) Stroke. Lancet, 371,
1612-1623. https://doi.org/10.1016/S0140-6736(08)60694-7
[2] Renna, R., Pilato, F., Profice, P., Della Marca, G., Broccolini, A., Morosetti, R., et al.
(2014) Risk Factor and Etiology Analysis of Ischemic Stroke in Young Adult Pa-
tients. Journal of Stroke and Cerebrovascular, 23, e221-e227.
https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.10.008
[3] Kirton, A., Crone, M., Benseler, S., Mineyko, A., Armstrong, D., Wade, A., et al.
(2013) Fibromuscular Dysplasia and Childhood Stroke. Brain, 136, 1846-1856.
https://doi.org/10.1093/brain/awt111
[4] Miller, T.R., Shivashankar, R., Mossa-Basha, M. and Gandhi, D. (2015) Reversible
Cerebral Vasoconstriction Syndrome, Part 2: Diagnostic Work-Up, Imaging Evalu-
ation, and Differential Diagnosis. American Journal of Neuroradiology, 36, 1580-1588.
DOI: 10.4236/wjns.2018.82015 176 World Journal of Neuroscience
R. AlSherooqi et al.
https://doi.org/10.3174/ajnr.A4215
[5] Arthurs, E., Hanna, T.P., Zaza, K., Peng, Y. and Hall, S.F. (2016) Stroke after Radia-
tion Therapy for Head and Neck Cancer: What Is the Risk? International Journal of
Radiation Oncology, Biology, Physics, 96, 589-596.
https://doi.org/10.1016/j.ijrobp.2016.07.007
[6] Jang, D.K., Lee, K.S., Rha, H.K., Huh, P.W., Yang, J.H., Park, I.S., et al. (2014) Clin-
ical and Angiographic Features and Stroke Types in Adult Moyamoya Disease.
American Journal of Neuroradiology, 35, 1124-1131.
https://doi.org/10.3174/ajnr.A3819
[7] Shi, Q., Chen, J., Pongmoragot, J., Lanthier, S. and Saposnik, G. (2014) Prevalence
of Fabry Disease in Stroke Patients—A Systematic Review and Meta-Analysis.
Journal of Stroke and Cerebrovascular Diseases, 23, 985-992.
https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.08.010
[8] Adams Jr., H.P. (2014) Cerebral Vasculitis. Handbook of Clinical Neurology, 119,
475-494. https://doi.org/10.1016/B978-0-7020-4086-3.00031-X
[9] Arboix, A., Jimenez, C., Massons, J., Parra, O. and Besses, C. (2016) Hematological
Disorders: A Commonly Unrecognized Cause of Acute Stroke. Expert Review of
Hematology, 9, 891-901. https://doi.org/10.1080/17474086.2016.1208555
[10] Okuma, H. and Kitagawa, Y. (2013) Diagnosis and Potential Treatment of Anti-
phospholipid Syndrome-Related Mainly on Ischemic Stroke. Brain and Nerves, 65,
1319-1332.
[11] Talahma, M., Strbian, D. and Sundararajan, S. (2014) Sickle Cell Disease and Stroke.
Stroke, 45, e98-e100. https://doi.org/10.1161/STROKEAHA.114.005144
[12] Sacco, S. and Kurth, T. (2014) Migraine and the Risk for Stroke and Cardiovascular
Disease. Current Cardiology Reports, 16, 524.
https://doi.org/10.1007/s11886-014-0524-1
[13] Coutinho, J.M. (2015) Cerebral Venous Thrombosis. Journal of Thrombosis and
Haemostasis, 13, S238-S244. https://doi.org/10.1111/jth.12945
[14] Putz, K., Hayani, K. and Zar, F.A. (2013) Meningitis. Prim Care, 40, 707-726.
https://doi.org/10.1016/j.pop.2013.06.001
[15] Sacco, R.L., Kasner, S.E., Broderick, J.P., Caplan, L.R., Connors, J.J., Culebras, A., et
al. (2013) An Updated Definition of Stroke for the 21st Century: A Statement for
Healthcare Professionals from the American Heart Association/American Stroke
Association. Stroke, 44, 2064-2089. https://doi.org/10.1161/STR.0b013e318296aeca
[16] Ionita, C.C., Siddiqui, A.H., Levy, E.I., Hopkins, L.N., Snyder, K.V. and Gibbons,
K.J. (2011) Acute Ischemic Stroke and Infections. Journal of Stroke and Cerebro-
vascular Diseases, 20, 1-9.
https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.09.011
[17] Jin, R., Liu, L., Zhang, S., Nanda, A. and Li, G. (2013) Role of Inflammation and Its
Mediators in Acute Ischemic Stroke. Journal of Cardiovascular Translational Re-
search, 6, 834-851. https://doi.org/10.1007/s12265-013-9508-6
DOI: 10.4236/wjns.2018.82015 177 World Journal of Neuroscience
You might also like
- Intracerebral Haemorrhage: Disease PrimersDocument18 pagesIntracerebral Haemorrhage: Disease PrimersMarlon VillanuevaNo ratings yet
- Case Study On ManiaDocument30 pagesCase Study On ManiaIOM BNS78% (9)
- New HSV EraserDocument108 pagesNew HSV EraserDashar WilsonNo ratings yet
- A 19-Year-Old Man With Sickle Cell Disease Presenting With Spinal Infarction: A Case ReportDocument6 pagesA 19-Year-Old Man With Sickle Cell Disease Presenting With Spinal Infarction: A Case ReportJabber PaudacNo ratings yet
- Ischemic Cerebral Stroke Case Report, Complications and Associated FactorsDocument5 pagesIschemic Cerebral Stroke Case Report, Complications and Associated Factorsfaradilla wiyandaNo ratings yet
- Ischemic Cerebral Stroke Case Report, Complications and Associated FactorsDocument7 pagesIschemic Cerebral Stroke Case Report, Complications and Associated FactorsAlfa DexterNo ratings yet
- Acute Ischemic Stroke: Clinical PracticeDocument8 pagesAcute Ischemic Stroke: Clinical PracticeDorina FrunzeNo ratings yet
- Acute Ischaemic Stroke in Infective Endocarditis: Pathophysiology and Clinical Outcomes in Patients Treated With Reperfusion TherapyDocument13 pagesAcute Ischaemic Stroke in Infective Endocarditis: Pathophysiology and Clinical Outcomes in Patients Treated With Reperfusion TherapyPatrick NunsioNo ratings yet
- Biomedicines 10 02830 v2Document12 pagesBiomedicines 10 02830 v2Septi Dimas jamaludinNo ratings yet
- Vascular Instability and Neurological Morbidity in Sickle Cell Disease: An Integrative Framework.Document21 pagesVascular Instability and Neurological Morbidity in Sickle Cell Disease: An Integrative Framework.Arturo Martí-CarvajalNo ratings yet
- Oral Medicine: Editor: Martin S. GreenbergDocument12 pagesOral Medicine: Editor: Martin S. GreenbergSuseno AjiNo ratings yet
- Acute Stroke ArticleDocument10 pagesAcute Stroke ArticlenesredeNo ratings yet
- Ischemic Stroke in A Young Male Patient in Rural Uganda, Case Report.Document3 pagesIschemic Stroke in A Young Male Patient in Rural Uganda, Case Report.International Journal of Innovative Science and Research TechnologyNo ratings yet
- Hemato Si StrokeDocument6 pagesHemato Si Strokeseaside16girlNo ratings yet
- 1 s2.0 S2589238X23000098 Main PDFDocument4 pages1 s2.0 S2589238X23000098 Main PDFAnastasia ThaliaNo ratings yet
- Nervous SystemDocument62 pagesNervous Systemmyat252No ratings yet
- Cerebral Small Vessel Disease: Review ArticleDocument21 pagesCerebral Small Vessel Disease: Review ArticleSiklus AnakNo ratings yet
- Cerebral ToxoplasmaDocument4 pagesCerebral ToxoplasmaTheodoreNo ratings yet
- Infective EndocarditisDocument5 pagesInfective Endocarditismustafa malvi100% (1)
- Myocarditis Due To Systemic Lupus Erythematosus Associated With Cardiogenic ShockDocument3 pagesMyocarditis Due To Systemic Lupus Erythematosus Associated With Cardiogenic ShockAkbar IskandarNo ratings yet
- Are Acute Subdural Hematomas Possible Without Head Trauma?: Case SeriesDocument5 pagesAre Acute Subdural Hematomas Possible Without Head Trauma?: Case SeriesSucipto HartonoNo ratings yet
- Non Hemorrhagic Stroke (SNH) and Interleukin-6 (Il6) : A Literature ReviewDocument10 pagesNon Hemorrhagic Stroke (SNH) and Interleukin-6 (Il6) : A Literature ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cardiovascular Stroke Prevention and Management Using The Principles of Cellular MedicineDocument4 pagesCardiovascular Stroke Prevention and Management Using The Principles of Cellular MedicineInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Multi-Infarct Dementia With Acute Intra Cerebral Hemorrhage and Chronic Subdural Hygromas: A Case StudyDocument4 pagesMulti-Infarct Dementia With Acute Intra Cerebral Hemorrhage and Chronic Subdural Hygromas: A Case StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- What Is The Pathophysiology of Hemifacial Spasm?Document3 pagesWhat Is The Pathophysiology of Hemifacial Spasm?NabilaNo ratings yet
- Spontaneous Intracerebral Hemorrhage: Pathogenesis, Clinical Features, and DiagnosisDocument25 pagesSpontaneous Intracerebral Hemorrhage: Pathogenesis, Clinical Features, and DiagnosisBryan Tam ArevaloNo ratings yet
- HHS Public Access: Subarachnoid Hemorrhage Presenting With Second-Degree Type I Sinoatrial Exit Block: A Case ReportDocument15 pagesHHS Public Access: Subarachnoid Hemorrhage Presenting With Second-Degree Type I Sinoatrial Exit Block: A Case Reportcitra annisa fitriNo ratings yet
- Adolescent Onset of Acute Heart FailureDocument19 pagesAdolescent Onset of Acute Heart FailureVeronica Romero MouthonNo ratings yet
- MainDocument7 pagesMainSonia khanNo ratings yet
- Ischemic Stroke A Comparative Retrospective Study: Experience of Military Hospital of MeknesDocument20 pagesIschemic Stroke A Comparative Retrospective Study: Experience of Military Hospital of MeknesIJAR JOURNALNo ratings yet
- Cerebral Small Vessel DiseaseDocument11 pagesCerebral Small Vessel Diseaseyousra yatrebNo ratings yet
- Noninfectious Cerebral Vasculitis in Children: Indianapolis, IndianaDocument15 pagesNoninfectious Cerebral Vasculitis in Children: Indianapolis, IndianaNathaly LapoNo ratings yet
- Acute Viral Myocarditis: Epidemiology and Pathophysiology: Lara Shekerdemian, MD, MRCP Desmond Bohn, MB, MRCPDocument6 pagesAcute Viral Myocarditis: Epidemiology and Pathophysiology: Lara Shekerdemian, MD, MRCP Desmond Bohn, MB, MRCPMike ShufflebottomNo ratings yet
- Ich Magistris, 2013Document8 pagesIch Magistris, 2013ignasachyntiaNo ratings yet
- Britton Et Al-2015-Internal Medicine JournalDocument14 pagesBritton Et Al-2015-Internal Medicine JournalfrizkapfNo ratings yet
- A Prospective Study of Prescribing Pattern in The Management of Stroke at A Tertiary Care HospitalDocument6 pagesA Prospective Study of Prescribing Pattern in The Management of Stroke at A Tertiary Care HospitalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Infective EndocarditisDocument13 pagesInfective EndocarditisIbrahimNo ratings yet
- Diabetes, Stroke, and Neuroresilience Looking BeyondDocument21 pagesDiabetes, Stroke, and Neuroresilience Looking BeyondMaudia IndrianiiNo ratings yet
- Intracerebral-hemorrhage-in-translational-research_2020_Brain-HemorrhagesDocument6 pagesIntracerebral-hemorrhage-in-translational-research_2020_Brain-HemorrhagesLeandro AntivilNo ratings yet
- StrokeDocument17 pagesStrokeluis sanchezNo ratings yet
- Bruce C V Campbell Ischaemic Stroke 2019Document22 pagesBruce C V Campbell Ischaemic Stroke 2019yiyecNo ratings yet
- Cerebellar Stroke in A COVID-19 Infected Patient. A Case ReportDocument6 pagesCerebellar Stroke in A COVID-19 Infected Patient. A Case ReportMuhammad Reza FirdausNo ratings yet
- The Risk Factor of Recurrence Stroke Among Stroke and Transient Ischemic Attack Patients in IndonesiaDocument11 pagesThe Risk Factor of Recurrence Stroke Among Stroke and Transient Ischemic Attack Patients in Indonesiafarah maulida martaNo ratings yet
- IJRPR15417Document2 pagesIJRPR15417Gleeware LimitedNo ratings yet
- StrokeDocument17 pagesStrokeJonathan Gutierrez RiosNo ratings yet
- HSA Aneurism+â-Ítica ICM 2014Document4 pagesHSA Aneurism+â-Ítica ICM 2014Ellys Macías PeraltaNo ratings yet
- Nihms 1873457Document15 pagesNihms 1873457Hanssel Viramontes CastroNo ratings yet
- 6 Giant Cell Arteritis Dan PolireumalgiaDocument8 pages6 Giant Cell Arteritis Dan PolireumalgiaRifqiNo ratings yet
- Hypertension in The Elderly: ArticleDocument14 pagesHypertension in The Elderly: Articleaulia nurfadilahNo ratings yet
- DownloadDocument7 pagesDownloadsitorus.family2009No ratings yet
- PICpediatricDocument14 pagesPICpediatricAtzi FNo ratings yet
- Demensia Vaskuler 2Document20 pagesDemensia Vaskuler 2Adam MochtarNo ratings yet
- Concise Clinical Review: Intracranial HemorrhageDocument9 pagesConcise Clinical Review: Intracranial HemorrhageWanda FlorenciaNo ratings yet
- Seminar: Epidemiology and Risk FactorsDocument17 pagesSeminar: Epidemiology and Risk FactorsNelly ElizabethNo ratings yet
- Vascular DementiaDocument8 pagesVascular Dementiaddelindaaa100% (1)
- Lupus Myocarditis A Rare CaseDocument3 pagesLupus Myocarditis A Rare Casea.rohman2700No ratings yet
- Challenges and Opportunities in Pediatric Heart Failure and TransplantationDocument15 pagesChallenges and Opportunities in Pediatric Heart Failure and TransplantationvijuNo ratings yet
- Cardiac Sarcoidosis: Abdul R Doughan, Byron R WilliamsDocument7 pagesCardiac Sarcoidosis: Abdul R Doughan, Byron R WilliamsBhagya Narayan PanditNo ratings yet
- Moyamoya Epidemiology, Presentation, and DiagnosisDocument9 pagesMoyamoya Epidemiology, Presentation, and DiagnosisshiloinNo ratings yet
- Cardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesFrom EverandCardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesNo ratings yet
- Comprehensive Insights into Acute Arterial Occlusion: Pathways, Prevention, and Holistic CareFrom EverandComprehensive Insights into Acute Arterial Occlusion: Pathways, Prevention, and Holistic CareNo ratings yet
- Arterial Disorders: Definition, Clinical Manifestations, Mechanisms and Therapeutic ApproachesFrom EverandArterial Disorders: Definition, Clinical Manifestations, Mechanisms and Therapeutic ApproachesAdel BerbariNo ratings yet
- NO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Document10 pagesNO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Dayu Punik ApsariNo ratings yet
- MM UnikDocument47 pagesMM UnikDayu Punik ApsariNo ratings yet
- NO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Document19 pagesNO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Dayu Punik ApsariNo ratings yet
- NO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Document12 pagesNO TGL Sell/Buy SL Profit/ Loss Keterangan Take Profit (Pip)Dayu Punik ApsariNo ratings yet
- BBMA Ibnu AdnanDocument32 pagesBBMA Ibnu AdnanDayu Punik ApsariNo ratings yet
- Kata Sehari HariDocument3 pagesKata Sehari HariDayu Punik ApsariNo ratings yet
- Frasa Bahasa InggrisDocument19 pagesFrasa Bahasa InggrisDayu Punik ApsariNo ratings yet
- Research Article: Efficacy of Aloe Vera, Ananas Comosus, and SansevieriaDocument8 pagesResearch Article: Efficacy of Aloe Vera, Ananas Comosus, and SansevieriaDayu Punik ApsariNo ratings yet
- International Journal of Pharmaceutics: SciencedirectDocument11 pagesInternational Journal of Pharmaceutics: SciencedirectDayu Punik ApsariNo ratings yet
- Suffering: and Montreal THEDocument5 pagesSuffering: and Montreal THEDayu Punik ApsariNo ratings yet
- Metatrader DescriptionDocument1 pageMetatrader DescriptionDayu Punik ApsariNo ratings yet
- Definisi AsmaDocument12 pagesDefinisi AsmaDayu Punik ApsariNo ratings yet
- Government College of Nursing:, Jodhpur (Raj.)Document7 pagesGovernment College of Nursing:, Jodhpur (Raj.)priyankaNo ratings yet
- Anaplastic Thyroid CancerDocument40 pagesAnaplastic Thyroid Cancershita febrianaNo ratings yet
- Commercial Quality of Seed PotatoesDocument112 pagesCommercial Quality of Seed PotatoesPedro Daniel LeivaNo ratings yet
- Funda Reviewer CADocument33 pagesFunda Reviewer CARichie Marie BajaNo ratings yet
- Colon Cancer Case StudyDocument21 pagesColon Cancer Case StudyInfection QcghNo ratings yet
- Met 201Document9 pagesMet 201minamessak98No ratings yet
- 3.psychiatric HX and MSE (1) According To DSM-5Document96 pages3.psychiatric HX and MSE (1) According To DSM-5sopsychaNo ratings yet
- Ben20Diazepine Withdrawal Symptom Questionnaire: Yes ModerateDocument1 pageBen20Diazepine Withdrawal Symptom Questionnaire: Yes Moderatesharp8787No ratings yet
- Medicine For Mountaineering and Other Wilderness Activities (6th Edition) (2010) (James A. Wilkerson)Document2,899 pagesMedicine For Mountaineering and Other Wilderness Activities (6th Edition) (2010) (James A. Wilkerson)zaellixaNo ratings yet
- Asthma Brochure 2015Document2 pagesAsthma Brochure 2015Eliseo RamirezNo ratings yet
- Bleeding Disorders: LCDR Art GeorgeDocument54 pagesBleeding Disorders: LCDR Art GeorgepallavberiNo ratings yet
- Top 100 Diagnoses in Neurology Core Features, Synopses, IllustrationsDocument445 pagesTop 100 Diagnoses in Neurology Core Features, Synopses, IllustrationspondebernardoNo ratings yet
- DRUG+STUDY NaprexDocument2 pagesDRUG+STUDY NaprexJoevence Gazo CuaresmaNo ratings yet
- Case AnalysisDocument27 pagesCase AnalysisIrish Eunice FelixNo ratings yet
- The Gluten Connection - Walter VeithDocument5 pagesThe Gluten Connection - Walter VeithGabriela Rojas FusNo ratings yet
- Vitamin B6: Health and NutritionDocument16 pagesVitamin B6: Health and NutritionKreena PatelNo ratings yet
- 501MCQforclinicalpharmacylast IvrtjnDocument119 pages501MCQforclinicalpharmacylast Ivrtjnد.شەماڵ احمد : پزیشکی دەرمانساز100% (1)
- What Is The Difference Between The Mind and The Brain-1Document2 pagesWhat Is The Difference Between The Mind and The Brain-1Amir Nazir100% (1)
- Alfuzosin HCL (Xatral XL 10mg)Document6 pagesAlfuzosin HCL (Xatral XL 10mg)asdwasdNo ratings yet
- Drug Study #2Document3 pagesDrug Study #2Sarah Kaye BañoNo ratings yet
- HEALTH TALK of EncopresisDocument15 pagesHEALTH TALK of EncopresisAmit RanjanNo ratings yet
- RHD Poster - ODADocument1 pageRHD Poster - ODASinclair Broadcast Group - EugeneNo ratings yet
- Name: - Score: - Teacher: - DateDocument2 pagesName: - Score: - Teacher: - DatePauline Erika CagampangNo ratings yet
- Pathoma - Chapter 1Document13 pagesPathoma - Chapter 1Jonathan AiresNo ratings yet
- The Persistent Stigma and Disregard For Mental Health in Sri LankaDocument3 pagesThe Persistent Stigma and Disregard For Mental Health in Sri Lankadevmini herathNo ratings yet
- 2004 - Number Series For Psychological Normalization - Book1Document208 pages2004 - Number Series For Psychological Normalization - Book1Carla Perin67% (3)
- THE Health Emergency Management: Doh - Ro XiDocument58 pagesTHE Health Emergency Management: Doh - Ro XiCreativ Worx100% (3)
- Chapter 4 - Servsafe - 6e Edited PDFDocument4 pagesChapter 4 - Servsafe - 6e Edited PDFdevvy anneNo ratings yet