Professional Documents
Culture Documents
Tetanus (Clostridium Tetani) : Mark R. Schleiss
Tetanus (Clostridium Tetani) : Mark R. Schleiss
Uploaded by
eagame gamersOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tetanus (Clostridium Tetani) : Mark R. Schleiss
Tetanus (Clostridium Tetani) : Mark R. Schleiss
Uploaded by
eagame gamersCopyright:
Available Formats
Chapter 238 ◆ Tetanus (Clostridium tetani) 1549
Chapter 238
Tetanus (Clostridium
tetani)
Mark R. Schleiss
ETIOLOGY
Tetanus is an acute, spastic paralytic illness caused by a neurotoxin
produced by Clostridium tetani. Thus, tetanus can be considered more
as a toxin-mediated process than an acute infectious process, since
there are few, if any, symptoms elicited by the presence of replicating
microorganisms or host inflammatory response. Unlike other pathogenic
clostridia species, C. tetani is not a tissue-invasive organism and instead
causes illness through the toxin, tetanospasmin, more commonly referred
to as tetanus toxin. Tetanospasmin is the 2nd most poisonous substance
known, surpassed in potency only by botulinum toxin. The human
lethal dose of tetanus toxin is estimated to be 10−5 mg/kg.
Clostridium tetani is a motile, gram-positive, spore-forming obligate
anaerobe. The organism’s natural habitat worldwide is soil, dust, and
the alimentary tracts of various animals. C. tetani forms spores terminally,
with a classic morphologic appearance resembling a drumstick or tennis
racket microscopically. The formation of spores is a critical aspect of
the organism’s persistence in the environment. Spores can survive boiling
but not autoclaving, whereas the vegetative cells are killed by antibiotics,
heat, and standard disinfectants.
EPIDEMIOLOGY
Tetanus occurs worldwide and is endemic in many developing countries,
although its incidence varies considerably. Public health efforts in recent
years have had an impressive impact on tetanus-associated mortality,
although many challenges remain. Approximately 57,000 deaths were
caused by tetanus globally in 2015. Of these, approximately 20,000 deaths
occurred in neonates and 37,000 in older children and adults. Most
mortality from neonatal (or umbilical) tetanus occurs in South Asia
and Sub-Saharan Africa (Fig. 238.1). Mortality in adults is largely caused
by maternal tetanus, which results from postpartum, postabortal, or
postsurgical wound infection with C. tetani. Reported tetanus cases
in the United States have declined >95% since 1947, and deaths from
tetanus have declined by >99% in that same period. From 2009 through
2015, a total of 197 cases and 16 deaths from tetanus were reported in
the United States. The majority of U.S. childhood cases of tetanus have
occurred in unimmunized children whose parents objected to vaccination.
Most non-neonatal cases of tetanus are associated with a traumatic
injury, often a penetrating wound inflicted by a dirty object such as a
nail, splinter, fragment of glass, or unsterile injection. Tetanus may also
occur in the setting of illicit drug injection. The disease has been associ-
ated with the use of contaminated suture material and after intramuscular
injection of medicines, most notably quinine for chloroquine-resistant
falciparum malaria. The disease may also occur in association with
animal bites, abscesses (including dental abscesses), ear and other body
piercing, chronic skin ulceration, burns, compound fractures, frostbite,
gangrene, intestinal surgery, ritual scarification, infected insect bites,
and female circumcision. Rarely, cases may present to clinical attention
without an antecedent history of trauma.
PATHOGENESIS
Tetanus typically occurs after spores (introduced by traumatic injury)
germinate, multiply, and produce tetanus toxin. A plasmid carries the
toxin gene. Toxin is produced only by the vegetative cell, not the spore.
It is released after the vegetative phase of replication, with replication
occurring under anaerobic conditions. The low oxidation-reduction
potential of an infected injury site therefore provides an ideal environment
for transition from the spore to the vegetative stage of growth. Following
bacterial cell death and lysis, tetanospasmin is produced. The toxin has
) E 1 @ 0., .1 1AA1@ A C 1 1 0 D @A F .CA , A1 @ ( 1 F 2F A D @ .1@
@ @A 1 CA F @ CA A E C @ AA ( F@ A D @, @ A @ A @D
1549.e2 Part XVI ◆ Infectious Diseases
Keywords
Arthus reaction
C. tetani
immunization
lockjaw
maternal tetanus
neonatal tetanus
opisthotonos
rabies
risus sardonicus
tetanus toxin
TIG
trismus
umbilical tetanus
) E 1 @ 0., .1 1AA1@ A C 1 1 0 D @A F .CA , A1 @ ( 1 F 2F A D @ .1@
@ @A 1 CA F @ CA A E C @ AA ( F@ A D @, @ A @ A @D
1550 Part XVI ◆ Infectious Diseases
Elimination status
MNT eliminated since 2000
MNT not eliminated
Eliminated prior to 2000
Fig. 238.1 Global elimination status of maternal and neonatal tetanus (MNT). (From World Health Organization: Maternal and neonatal tetanus
(MNT) elimination. http://www.who.int/immunization/diseases/MNTE_initiative/en.)
no known function for clostridia in the soil environment where they with the head and the heels bent backward and the body bowed forward.
normally reside. Tetanus toxin is a 150 kDa simple protein consisting In severe cases, only the back of the head and the heels of the patient
of a heavy (100 kDa) and a light (50 kDa) chain joined by a single are noted to be touching the supporting surface. Opisthotonos is an
disulfide bond. Tetanus toxin binds at the neuromuscular junction and equilibrium position that results from unrelenting total contraction of
enters the motor nerve by endocytosis, after which it undergoes retrograde opposing muscles, all of which display the typical boardlike rigidity of
axonal transport, facilitated by dyneins, to the cytoplasm of the tetanus. Laryngeal and respiratory muscle spasm can lead to airway
α-motoneuron. In the sciatic nerve, the transport rate was found to be obstruction and asphyxiation. Because tetanus toxin does not affect
3.4 mm/hr. The toxin exits the motoneuron in the spinal cord and next sensory nerves or cortical function, the patient unfortunately remains
enters adjacent spinal inhibitory interneurons, where it prevents release conscious, in extreme pain, and in fearful anticipation of the next tetanic
of the neurotransmitters glycine and γ-aminobutyric acid (GABA). seizure. The seizures are characterized by sudden, severe tonic contrac-
Tetanus toxin thus blocks the normal inhibition of antagonistic muscles tions of the muscles, with fist clenching, flexion, and adduction of the
on which voluntary coordinated movement depends; as a consequence, arms and hyperextension of the legs. Without treatment, the duration
affected muscles sustain maximal contraction and cannot relax. This of these seizures may range from a few seconds to a few minutes in
aspect of pathogenesis led to the term lockjaw, classically applied to length with intervening respite periods. As the illness progresses, the
the clinical manifestations of tetanus in the affected individual. The spasms become sustained and exhausting. The smallest disturbance by
autonomic nervous system is also rendered unstable in tetanus. sight, sound, or touch may trigger a tetanic spasm. Dysuria and urinary
The phenomenal potency of tetanus toxin is enzymatic. The 50 kDa retention result from bladder sphincter spasm; forced defecation may
light chain (A-chain) of tetanus toxin is a zinc-containing endoprotease occur. Fever, occasionally as high as 40°C (104°F), is common and is
whose substrate is synaptobrevin, a constituent protein of the docking caused by the substantial metabolic energy consumed by spastic muscles.
complex that enables the synaptic vesicle to fuse with the terminal Notable autonomic effects include tachycardia, dysrhythmias, labile
neuronal cell membrane. The cleavage of synaptobrevin is the final hypertension, diaphoresis, and cutaneous vasoconstriction. The tetanic
target of tetanus toxin, and even in low doses the neurotoxin will inhibit paralysis usually becomes more severe in the 1st wk after onset, stabilizes
neurotransmitter exocytosis in the inhibitory interneurons. The blockage in the 2nd wk, and ameliorates gradually over the ensuing 1-4 wk.
of GABA and glycine causes the physiologic effects of tetanus toxin. Neonatal tetanus, the infantile form of generalized tetanus, typically
The 100 kDa heavy chain (B-chain) of the toxin contains its binding manifests within 3-12 days of birth. It presents as progressive difficulty
and internalization domains. It binds to disialogangliosides (GD2 and in feeding (sucking and swallowing), associated hunger, and crying.
GD1b) on the neuronal membrane. The translocation domain aids the Paralysis or diminished movement, stiffness and rigidity to the touch,
movement of the protein across that membrane and into the neuron. and spasms, with or without opisthotonos, are characteristic. The
Because C. tetani is not an invasive organism, its toxin-producing umbilical stump, which is typically the portal of entry for the microorgan-
vegetative cells remain where introduced into the wound, which may ism, may retain remnants of dirt, dung, clotted blood, or serum, or it
display local inflammatory changes and a mixed bacterial flora. may appear relatively benign.
Localized tetanus results in painful spasms of the muscles adjacent to
CLINICAL MANIFESTATIONS the wound site and may precede generalized tetanus. Cephalic tetanus
Tetanus is most often generalized but may also be localized. The incuba- is a rare form of localized tetanus involving the bulbar musculature
tion period typically is 2-14 days but may be as long as months after that occurs with wounds or foreign bodies in the head, nostrils, or
the injury. In generalized tetanus the presenting symptom in about face. It also occurs in association with chronic otitis media. Cephalic
half of cases is trismus (masseter muscle spasm, or lockjaw). Headache, tetanus is characterized by retracted eyelids, deviated gaze, trismus,
restlessness, and irritability are early symptoms, often followed by stiffness, risus sardonicus, and spastic paralysis of the tongue and pharyngeal
difficulty chewing, dysphagia, and neck muscle spasm. The so-called musculature.
sardonic smile of tetanus (risus sardonicus) results from intractable
spasms of facial and buccal muscles. When the paralysis extends to DIAGNOSIS
abdominal, lumbar, hip, and thigh muscles, the patient may assume an The picture of tetanus is one of the most dramatic in medicine, and
arched posture of extreme hyperextension of the body, or opisthotonos, the diagnosis may be established clinically. The typical setting is an
) E 1 @ 0., .1 1AA1@ A C 1 1 0 D @A F .CA , A1 @ ( 1 F 2F A D @ .1@
@ @A 1 CA F @ CA A E C @ AA ( F@ A D @, @ A @ A @D
Chapter 238 ◆ Tetanus (Clostridium tetani) 1551
unimmunized patient (and/or mother) who was injured or born within of patients given the usual dose of TAT will experience serum sickness.
the preceding 2 wk, who presents with trismus, dysphagia, generalized The human-derived immunoglobulins are much preferred because of
muscle rigidity and spasm, and a clear sensorium. their longer half-life (30 days) and the virtual absence of allergic and
Results of routine laboratory studies are usually normal. A peripheral serum sickness adverse effects. Results of studies examining the potential
leukocytosis may result from a secondary bacterial infection of the benefit of intrathecal administration of TIG are conflicting. The TIG
wound or may be stress-induced from the sustained tetanic spasms. preparation available for use in the United States is neither licensed
The cerebrospinal fluid analysis is normal, although the intense muscle nor formulated for intrathecal or intravenous use.
contractions may raise intracranial pressure. Serum muscle enzymes Oral (or intravenous) metronidazole (30 mg/kg/day, given at 6 hr
(creatine kinase, aldolase) may be elevated. Neither the electroencepha- intervals; maximum dose, 4 g/day) decreases the number of vegetative
logram nor the electromyogram shows a characteristic pattern, although forms of C. tetani and is currently considered the antibiotic of choice.
EMG may show continuous discharge of motor subunits and shortening, Parenteral penicillin G (100,000 U/kg/day, administered at 4-6 hr inter-
or absence of the silent interval normally observed after an action vals, with a daily maximum 12 million U) is an alternative treatment.
potential. An assay for antitoxin levels is not readily available, although Antimicrobial therapy for a total duration of 7-10 days is recommended.
a serum antitoxin level of ≥0.01 IU/mL is generally considered protective Supportive care and pharmacologic interventions targeted at control
and makes the diagnosis of tetanus less likely. C. tetani is not always of tetanic spasms are of critical importance in the management of tetanus.
visible on Gram stain of wound material and is isolated by culture in Toward this goal, all patients with generalized tetanus should receive
only approximately 30% of cases. The spatula test is a simple diagnostic muscle relaxants. Diazepam provides both relaxation and seizure control.
bedside test that involves touching the oropharynx with a spatula or The initial dose of 0.1-0.2 mg/kg every 3-6 hr intravenously is subse-
tongue blade. Normally this maneuver will elicit a gag reflex, as the quently titrated to control the tetanic spasms, after which the effective
patient tries to expel the spatula (negative test). If tetanus is present, dose is sustained for 2-6 wk before a tapered withdrawal. Magnesium
patients develop a reflex spasm of the masseter muscles and bite the sulfate, other benzodiazepines (midazolam), chlorpromazine, dantrolene,
spatula (positive test). This bedside diagnostic maneuver is said to have and baclofen are also used. Intrathecal baclofen produces such complete
a high sensitivity and specificity. muscle relaxation that apnea often ensues; as with most other agents
listed, baclofen should be used only in an intensive care unit setting.
Differential Diagnosis Favorable survival rates in generalized tetanus have been described
Florid and generalized tetanus is typically not mistaken for any other with the use of neuromuscular blocking agents such as vecuronium
disease. However, trismus may result from parapharyngeal, retropha- and pancuronium, which produce a general flaccid paralysis that is
ryngeal, or dental abscesses or rarely from acute encephalitis involving then managed by mechanical ventilation. Autonomic instability is
the brainstem. Either rabies or tetanus may follow an animal bite, and regulated with standard α- or β-adrenergic (or both) blocking agents;
rabies may manifest as trismus with seizures. Rabies may be distinguished morphine has also proved useful.
from tetanus by hydrophobia, marked dysphagia, predominantly clonic
seizures, and pleocytosis (see Chapter 300). Although strychnine SUPPORTIVE CARE
poisoning may result in tonic muscle spasms and generalized seizure Meticulous supportive care in a quiet, dark, secluded setting is most
activity, it seldom produces trismus, and unlike in tetanus, general desirable. Because tetanic spasms may be triggered by minor stimuli,
relaxation usually occurs between spasms. Hypocalcemia may produce the patient should be sedated and protected from all unnecessary sounds,
tetany that is characterized by laryngeal and carpopedal spasms, but sights, and touch, and all therapeutic and other manipulations must be
trismus is absent. Occasionally, epileptic seizures, narcotic withdrawal, carefully scheduled and coordinated. Endotracheal intubation may not
or other drug reactions may suggest tetanus. be required, but it should be done to prevent aspiration of secretions
before laryngospasm develops. A tracheostomy kit should be immediately
TREATMENT at hand for unintubated patients. Endotracheal intubation and suctioning
Management of tetanus requires eradication of C. tetani, correction of easily provoke reflex tetanic seizures and spasms, so early tracheostomy
wound environment conditions conducive to its anaerobic replication, should be considered in severe cases not managed by pharmacologically
neutralization of all accessible tetanus toxin, control of seizures and induced flaccid paralysis. Therapeutic botulinum toxin has been used
respiration, palliation, provision of meticulous supportive care, and to overcome trismus.
prevention of recurrences. Cardiorespiratory monitoring, frequent suctioning, and maintenance
Surgical wound excision and debridement are often needed to remove of the patient’s substantial fluid, electrolyte, and caloric needs are
the foreign body or devitalized tissue that created the anaerobic growth fundamental. Careful nursing attention to mouth, skin, bladder, and
conditions necessary for vegetative replication. Surgery should be bowel function is needed to avoid ulceration, infection, and obstipation.
performed promptly after administration of human tetanus immuno- Prophylactic subcutaneous heparin may be of value, but it must be
globulin (TIG) and antibiotics. Excision of the umbilical stump in the balanced with the risk of hemorrhage. Enoxaparin would be an alternative
neonate with tetanus is no longer recommended. for the patient for whom deep vein thrombosis prophylaxis is warranted.
Tetanus toxin cannot be neutralized by TIG after it has begun its
axonal ascent to the spinal cord. However, TIG should be given as soon COMPLICATIONS
as possible, toward the goal of neutralizing toxin that diffuses from the The seizures and the severe, sustained rigid paralysis of tetanus predispose
wound into the circulation before the toxin can bind at distant muscle the patient to many complications. Aspiration of secretions with attendant
groups. The optimal dose of TIG has not been determined. Some experts pneumonia is an important complication to consider and may be present
recommend a single intramuscular injection of 500 units of TIG to at initial diagnosis. Maintaining airway patency often mandates endo-
neutralize systemic tetanus toxin, but total doses as high as 3,000-6,000 U tracheal intubation and mechanical ventilation with their attendant
are also recommended. Infiltration of part of the dose of TIG into the hazards, including pneumothorax and mediastinal emphysema. The
wound is recommended by the Red Book Committee of the American seizures may result in lacerations of the mouth or tongue, in intramuscular
Academy of Pediatrics, although the efficacy of this approach has not hematomas or rhabdomyolysis with myoglobinuria and renal failure,
been proved. If TIG is unavailable, use of human intravenous immu- or in long-bone or spinal fractures. Venous thrombosis, pulmonary
noglobulin may be necessary. IVIG contains 4-90 U/mL of TIG; the embolism, gastric ulceration with or without hemorrhage, paralytic
optimal dosage of IVIG for treating tetanus is not known, and its use ileus, and decubitus ulceration are described as complications. Excessive
is not approved for this indication. In parts of the world where it is use of muscle relaxants, which are an integral part of care, may produce
available, another alternative may be equine-derived tetanus antitoxin iatrogenic apnea. Cardiac arrhythmias, including asystole, unstable blood
(TAT). This product is no longer available in the United States. A dose pressure, and labile temperature regulation reflect disordered autonomic
of 1,500-3,000 U is recommended and should be administered after nervous system control that may be aggravated by inattention to
appropriate testing for sensitivity and desensitization, since up to 15% maintenance of intravascular volume needs.
) E 1 @ 0., .1 1AA1@ A C 1 1 0 D @A F .CA , A1 @ ( 1 F 2F A D @ .1@
@ @A 1 CA F @ CA A E C @ AA ( F@ A D @, @ A @ A @D
Table 238.1 Tetanus Vaccination and Immune Globulin Use in Wound Management
CLEAN, MINOR WOUNDS ALL OTHER WOUNDS*
HISTORY OF ABSORBED
† ‡
TETANUS TOXOID DTaP, Tdap, or Td TIG DTaP, Tdap, or TD† TIG‡
Uncertain or <3 doses Yes No Yes Yes
≥3 doses No if <10 yr since last dose of tetanus-containing No No if <5 yr since last tetanus-containing No
vaccine vaccine§
Yes if ≥10 yr since last dose of tetanus-containing No Yes if ≥5 yr since last tetanus-containing No
vaccine vaccine dose
*Such as, but not limited to, wounds contaminated with dirt, feces, and saliva; puncture wounds; avulsions; and wounds resulting from missiles, crushing, burns, and
frostbite.
†
DTaP is used for children <7 yr old. Tdap is preferred over Td for underimmunized children ≥7 yr old who have not received Tdap previously.
‡
Intravenous immune globulin should be used when TIG is unavailable.
§
More frequent boosters are not needed and can accentuate adverse events.
DT, Diphtheria and tetanus toxoid vaccine; DTaP, combined diphtheria toxoid–tetanus toxoid–acellular pertussis vaccine; Td, tetanus toxoid and reduced
diphtheria toxoid vaccine; Tdap, tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine; TIG, tetanus immune globulin.
Data from Tetanus (lockjaw). In Kimberlin DW, Brady MT, Jackson MA, Long SS, editors: Red book: 2015 report of the Committee on Infectious Diseases, ed 30, Elk
Grove Village, IL, 2015, American Academy of Pediatrics.
PROGNOSIS Tetanus toxoid should always be given after a dog or other animal
Recovery in tetanus occurs through regeneration of synapses within bite, even though C. tetani is infrequently found in canine mouth flora.
the spinal cord that results in restoration of muscle relaxation. Interest- Non-minor wounds require human TIG except those in a fully immunized
ingly, an episode of tetanus does not result in the production of toxin- patient (i.e., ≥3 doses of adsorbed tetanus toxoid). In any other circum-
neutralizing antibodies, presumably because the infinitesimally small stances (e.g., patients with an unknown or incomplete immunization
amounts of toxin required to cause disease are not sufficient to elicit history; crush, puncture, or projectile wounds; wounds contaminated
an immune response. Therefore, active immunization with tetanus toxoid with saliva, soil, or feces; avulsion injuries; compound fractures; or
during convalescence and/or at discharge, with provision for completion frostbite), TIG 250 units should be administered intramuscularly,
of the primary vaccine series, is mandatory. regardless of the patient’s age or weight. If TIG is unavailable, use of
The most important factor that influences outcome is the quality human IVIG may be considered. If neither of these products is available,
of supportive care. Mortality is highest in very young and very old 3,000-5,000 units of equine-derived TAT (in regions of the world where
patients. A favorable prognosis is associated with a long incubation it is available) may be given intramuscularly after testing for hypersensitiv-
period, absence of fever, and localized disease. An unfavorable prognosis ity. Serum sickness may occur with this agent.
is associated with onset of trismus <7 days after injury and onset of The wound should undergo immediate, thorough surgical cleansing
generalized tetanic spasms <3 days after onset of trismus. Sequelae and debridement to remove foreign bodies and any necrotic tissue in
of hypoxic brain injury, especially in infants, include cerebral palsy, which anaerobic conditions might develop. Tetanus toxoid should be
diminished mental abilities, and behavioral difficulties. Most fatalities given to stimulate active immunity and may be administered concurrently
occur within the 1st wk of illness. Reported case fatality rates for with TIG (or TAT) if given in separate syringes at widely separated
generalized tetanus are 5–35%, and for neonatal tetanus they extend sites. A tetanus toxoid booster (preferably Tdap) is administered to all
from <10% with intensive care treatment to >75% without it. Cephalic persons with any wound if the tetanus immunization status is unknown
tetanus has an especially poor prognosis because of breathing and or incomplete. A booster is administered to injured persons who have
feeding difficulties. completed the primary immunization series if (1) the wound is clean
and minor but ≥10 yr have passed since the last booster or (2) the
PREVENTION wound is more serious and ≥5 yr have passed since the last booster
Tetanus is an entirely and easily preventable disease. A serum antibody (Table 238.1). Persons who experienced an Arthus reaction after a dose
titer of ≥0.01 U/mL is considered protective. Active immunization should of tetanus toxoid–containing vaccine should not receive Td more fre-
begin in early infancy with combined diphtheria toxoid–tetanus quently than every 10 yr, even for tetanus prophylaxis as part of wound
toxoid–acellular pertussis (DTaP) vaccine at 2, 4, 6, and 15-18 mo of management. In a situation of delayed wound care, active immunization
age, with boosters at 4-6 yr (DTaP) and 11-12 yr (Tdap) of age, and at should be started at once.
10 yr intervals thereafter throughout adult life with tetanus and reduced
diphtheria toxoid (Td). Immunization of women with tetanus toxoid Bibliography is available at Expert Consult.
prevents neonatal tetanus, and pregnant women should receive 1 dose
of reduced diphtheria and pertussis toxoids (Tdap) during each pregnancy,
preferably at 27-36 wk of gestation. Recommended immunization
schedules are regularly updated (http://www.cdc.gov/vaccines/schedules).
Arthus reactions (type III hypersensitivity reactions), a localized
vasculitis associated with deposition of immune complexes and activation
of complement, are reported rarely after tetanus vaccination. Mass
immunization campaigns in developing countries have occasionally
provoked a widespread hysterical reaction.
Wound Management
Tetanus prevention measures after trauma consist of inducing active
immunity to tetanus toxin and of passively providing antitoxic antibody
(Table 238.1). Tetanus prophylaxis is an essential part of all wound
management, but specific measures depend on the nature of the injury
and the immunization status of the patient. Prevention of tetanus must
be included in planning for the consequences of bombings, natural
disasters, and other possible civilian mass-casualty events.
) E 1 @ 0., .1 1AA1@ A C 1 1 0 D @A F .CA , A1 @ ( 1 F 2F A D @ .1@
@ @A 1 CA F @ CA A E C @ AA ( F@ A D @, @ A @ A @D
Chapter 238 ◆ Tetanus (Clostridium tetani) 1552.e1
Bibliography Rossetto O, Scorzeto M, Megighian A, et al: Tetanus neurotoxin, Toxicon 66:59–63, 2013.
Centers for Disease Control and Prevention: Tetanus surveillance—United States, Sequist TD: Eliminating maternal and neonatal tetanus and closing the immunity
2001–2008, MMWR Morb Mortal Wkly Rep 60:365–369, 2011. gap, Lancet 389:1380–1381, 2017.
Fowkes FJ, McGready R, Johnstone-Robertson S, et al: Antibody boosting and longevity Skuby SO, Rhee E, Thilo EH: Tetanus and Occam’s razor: almost forgotten but not
following tetanus immunization during pregnancy, Clin Infect Dis 56:749–750, 2013. gone: a case report, Pediatrics 138(5):e20160298, 2017.
Grund JM, Toledo C, Davis SM, et al: Tetanus cases after voluntary medical male Thwaites CL, Beeching NJ, Newton CR: Maternal and neonatal tetanus, Lancet
circumcision for HIV prevention—Eastern and Southern Africa, 2012–2015, MMWR 385(9965):362–370, 2015.
Morb Mortal Wkly Rep 65(2):36–37, 2016. Thwaites CL, Loan HT: Eradication of tetanus, Br Med Bull 116:69–77, 2015.
Hassel B: Tetanus: pathophysiology, treatment, and the possibility of using botulinum Yaffee AQ, Day DL, Bastin G, et al: Notes from the field. Obstetric tetanus in an
toxin against tetanus-induced rigidity and spasms, Toxins (Basel) 5:73–83, 2013. unvaccinated woman after a home birth delivery—Kentucky, 2016, MMWR Morb
Johnson MG, Bradley KK, Mendus S, et al: Vaccine-preventable disease among home- Mortal Wkly Rep 66(11):307–308, 2017.
schooled children: two cases of tetanus in Oklahoma, Pediatrics 132(6):e1686–e1689,
2013.
) E 1 @ 0., .1 1AA1@ A C 1 1 0 D @A F .CA , A1 @ ( 1 F 2F A D @ .1@
@ @A 1 CA F @ CA A E C @ AA ( F@ A D @, @ A @ A @D
You might also like
- Sinclair Method AlcoholDocument24 pagesSinclair Method AlcoholToni ErdfeldNo ratings yet
- Assessment Inferen CE Plannin G Interve Ntion Rationa LE Evalua TionDocument4 pagesAssessment Inferen CE Plannin G Interve Ntion Rationa LE Evalua TionBg Celo33% (3)
- Nursing Care Plan AppendicitisDocument2 pagesNursing Care Plan Appendicitisderic95% (57)
- Crede's ProphyaxisDocument12 pagesCrede's ProphyaxisNikki M. Arapol100% (1)
- Tetanus: Andrew Michael Taylor FRCADocument4 pagesTetanus: Andrew Michael Taylor FRCAILHAM AMIENNo ratings yet
- Afshar 2011Document8 pagesAfshar 2011Kami LyaNo ratings yet
- Brook 2008Document10 pagesBrook 2008Kami LyaNo ratings yet
- Tetanus in Developing Countries: A Review and Case Series: Ingole KV, Mundhada SG, Powar RMDocument5 pagesTetanus in Developing Countries: A Review and Case Series: Ingole KV, Mundhada SG, Powar RMRizka ApNo ratings yet
- TetanusDocument35 pagesTetanusJulie FurioNo ratings yet
- Questions and Answers: TetanusDocument4 pagesQuestions and Answers: TetanusRhodjan RescoNo ratings yet
- K6 SLIDE-MANAGEMENT OF TETANUS IN PEDIATRIC-baruDocument69 pagesK6 SLIDE-MANAGEMENT OF TETANUS IN PEDIATRIC-baruRaja Alfian IrawanNo ratings yet
- Questions and Answers: TetanusDocument4 pagesQuestions and Answers: TetanusJahanzaib NiaziNo ratings yet
- Questions and Answers: TetanusDocument4 pagesQuestions and Answers: TetanuszippyzevenNo ratings yet
- Microbiology of Clostridium Tetani and Wound ClassificationDocument3 pagesMicrobiology of Clostridium Tetani and Wound ClassificationAZIZAH ARDINALNo ratings yet
- Clostridium Tetani: Scientific ClassificationDocument4 pagesClostridium Tetani: Scientific ClassificationGael Forbes RealNo ratings yet
- 388tetanus For WebsiteDocument51 pages388tetanus For Websitehafiz ikhsanNo ratings yet
- Management and Prevention of Tetanus: Abstract: THDocument16 pagesManagement and Prevention of Tetanus: Abstract: THFabian FabiansyahNo ratings yet
- Lovely Professional University: Term Paper of Advanced MicrobiologyDocument11 pagesLovely Professional University: Term Paper of Advanced Microbiology27AlokKumarNo ratings yet
- Tetanus: Maria Banica & Sophie NamDocument19 pagesTetanus: Maria Banica & Sophie NamSuwantin Indra SariNo ratings yet
- Tetanus Pathophysiology, Clinical Signs, DiagnosisDocument9 pagesTetanus Pathophysiology, Clinical Signs, DiagnosisJuris Isaac Perez VianaNo ratings yet
- Neonatal TetanusDocument44 pagesNeonatal TetanusJake MillerNo ratings yet
- TetanusDocument3 pagesTetanusmake_jajoeNo ratings yet
- TetanusDocument12 pagesTetanustinkerbell03No ratings yet
- The Pa Tho Physiology of TetanusDocument3 pagesThe Pa Tho Physiology of Tetanusmai_serpicNo ratings yet
- Brief: Tetanus Disease, Treatment, ManagementDocument5 pagesBrief: Tetanus Disease, Treatment, ManagementchindiaNo ratings yet
- Clostridia in CattleDocument6 pagesClostridia in Cattleamamùra maamarNo ratings yet
- Clostridium Tetan1Document4 pagesClostridium Tetan1Jul SkynEtNo ratings yet
- Tetanus: A Potential Public Health Threat in Times of DisasterDocument4 pagesTetanus: A Potential Public Health Threat in Times of DisasterNasriNo ratings yet
- Toxoplasmosis: A Global Infection, So Widespread, So NeglectedDocument6 pagesToxoplasmosis: A Global Infection, So Widespread, So NeglectedIndah Yulinda PramestyNo ratings yet
- Tetanu S: By: Reno WaisyahDocument18 pagesTetanu S: By: Reno WaisyahReno WaisyahNo ratings yet
- Status InternusDocument12 pagesStatus InternusPriscaNo ratings yet
- The GENUS ClostridiumDocument28 pagesThe GENUS ClostridiumrohishaakNo ratings yet
- Tetanus: "Lock Jaw"Document10 pagesTetanus: "Lock Jaw"Atoillah IsvandiaryNo ratings yet
- TETANUSDocument17 pagesTETANUST. Chang100% (1)
- Tetanus PDFDocument10 pagesTetanus PDFVina MuspitaNo ratings yet
- !tetanus MDocument22 pages!tetanus MWendo yayahNo ratings yet
- Tetanus: Ma. Theresa Dj. YumangDocument28 pagesTetanus: Ma. Theresa Dj. YumangJean SarocamNo ratings yet
- Tetanus in Animals - Summary of Knowledge Malinovská, Z., Čonková, E., Váczi, PDocument7 pagesTetanus in Animals - Summary of Knowledge Malinovská, Z., Čonková, E., Váczi, PSophieNo ratings yet
- Tetanus 9 eDocument10 pagesTetanus 9 ea.hooker114No ratings yet
- Tetanus EmedicineDocument19 pagesTetanus EmedicineSapto SutardiNo ratings yet
- Group 2 TetanusDocument43 pagesGroup 2 TetanusDaymon, Ma. TeresaNo ratings yet
- Tetanus and BotulismDocument40 pagesTetanus and BotulismPatriceNo ratings yet
- Clinical Bacteriology: by Fawad Mahmood M.Phil. Medical Laboratory SciencesDocument26 pagesClinical Bacteriology: by Fawad Mahmood M.Phil. Medical Laboratory SciencesFawad SawabiNo ratings yet
- TetanusDocument4 pagesTetanuseagame gamersNo ratings yet
- TETAPOTADocument2 pagesTETAPOTArealme 6iNo ratings yet
- Pa Tho GenesisDocument11 pagesPa Tho GenesisBeth AvelinoNo ratings yet
- Tetanus: BackgroundDocument19 pagesTetanus: BackgroundYovita Devi KornelinNo ratings yet
- Clostridium Tetani: Infections in Newborn Infants: A Tetanus Neonatorum ReviewDocument8 pagesClostridium Tetani: Infections in Newborn Infants: A Tetanus Neonatorum ReviewNurul HikmahNo ratings yet
- Tetanus - The DiseaseDocument6 pagesTetanus - The Diseasemanjunath mamathaNo ratings yet
- Tetanus (Harrison's Principle of Internal Medicine)Document4 pagesTetanus (Harrison's Principle of Internal Medicine)Renz Mervin Rivera100% (1)
- Preventing Fetal Exposure To TETRATOGENSDocument6 pagesPreventing Fetal Exposure To TETRATOGENSEuna Patricia AguilarNo ratings yet
- Tetanus: C. L. ThwaitesDocument8 pagesTetanus: C. L. ThwaitesnurdiansyahNo ratings yet
- Acute Medicine Surgery - 2023 - Yamaguchi - The Threat of A New Tetanus Outbreak Due To Urban Flooding Disaster RequiresDocument9 pagesAcute Medicine Surgery - 2023 - Yamaguchi - The Threat of A New Tetanus Outbreak Due To Urban Flooding Disaster Requiresfitri dwiyantiNo ratings yet
- PEDIA Bacterial Infections Part 2 Dr. E. Lim FinalDocument5 pagesPEDIA Bacterial Infections Part 2 Dr. E. Lim FinalClaire DuNo ratings yet
- TetanusDocument23 pagesTetanusRiska PriyaniNo ratings yet
- TetanusDocument79 pagesTetanusSan MohapatraNo ratings yet
- Streptococcus Pneumoniae 2. Hemophilus Influenzae 3. Neisseria MeningitidesDocument4 pagesStreptococcus Pneumoniae 2. Hemophilus Influenzae 3. Neisseria Meningitidesa i r i e sNo ratings yet
- Tetanus Toxoid: Section TwoDocument1 pageTetanus Toxoid: Section TwoRaulimar Hernandez RamosNo ratings yet
- TTVDocument5 pagesTTVGlorious Tufon Neba EmmanuelNo ratings yet
- Zoonotic Infections 10Document21 pagesZoonotic Infections 10Chaudhary AjayNo ratings yet
- Brucellosis: The Short Textbook of PediatricsDocument3 pagesBrucellosis: The Short Textbook of PediatricsHosny M IsseNo ratings yet
- Tetanu S: Dr. MaslianiDocument74 pagesTetanu S: Dr. MaslianiHengky HanggaraNo ratings yet
- Cats and Toxoplasma: A Comprehensive Guide to Feline ToxoplasmosisFrom EverandCats and Toxoplasma: A Comprehensive Guide to Feline ToxoplasmosisNo ratings yet
- Familial Mediterranean FeverFrom EverandFamilial Mediterranean FeverMarco GattornoNo ratings yet
- JRCM 8 32Document4 pagesJRCM 8 32eagame gamersNo ratings yet
- Erythrasma Revisited: Diagnosis, Differential Diagnoses, and Comprehensive Review of TreatmentDocument7 pagesErythrasma Revisited: Diagnosis, Differential Diagnoses, and Comprehensive Review of Treatmenteagame gamersNo ratings yet
- Gastritis ManuscriptpresentationDocument12 pagesGastritis Manuscriptpresentationeagame gamersNo ratings yet
- Guillain-Barré Syndrome: Clinical ManifestationsDocument7 pagesGuillain-Barré Syndrome: Clinical Manifestationseagame gamersNo ratings yet
- Tetanus NeonatorumDocument1 pageTetanus Neonatorumeagame gamersNo ratings yet
- TetanusDocument4 pagesTetanuseagame gamersNo ratings yet
- Tetanus NeonatorumDocument6 pagesTetanus Neonatorumeagame gamersNo ratings yet
- Hyperbaric Oxygen in Critical CareDocument4 pagesHyperbaric Oxygen in Critical Careeagame gamersNo ratings yet
- Diving MedicineDocument14 pagesDiving Medicineeagame gamersNo ratings yet
- Atypical Antipsychotics and Newer AntidepressantsDocument21 pagesAtypical Antipsychotics and Newer Antidepressantseagame gamersNo ratings yet
- The Periodontal Index: A. L. Russell ExaminingDocument7 pagesThe Periodontal Index: A. L. Russell ExaminingVivek PatelNo ratings yet
- Poultry DiseasesDocument5 pagesPoultry DiseasesAnjum IslamNo ratings yet
- Level of Disease PreventionDocument16 pagesLevel of Disease Preventionenam professorNo ratings yet
- Reverse TrendelenburgDocument1 pageReverse TrendelenburgJamielyn BassigNo ratings yet
- Composite Vs Amalgam PowerpointDocument17 pagesComposite Vs Amalgam Powerpointapi-322463366100% (1)
- Colon, Rectum and Anus-Dr. SigitDocument121 pagesColon, Rectum and Anus-Dr. SigitYuliana Latif100% (1)
- Informed Consent: Lena Haygood (R) RT Radiology Instructor: Arizona Western Community College SourceDocument18 pagesInformed Consent: Lena Haygood (R) RT Radiology Instructor: Arizona Western Community College SourceJerry AbleNo ratings yet
- Acute AppendicitisDocument50 pagesAcute AppendicitisDeslia SupriyadiNo ratings yet
- AIIMS PG Jan 2015Document50 pagesAIIMS PG Jan 2015AnweshaBoseNo ratings yet
- Written Assignment Unit 2 EDUC 5420Document7 pagesWritten Assignment Unit 2 EDUC 5420RimaNo ratings yet
- Establishment Licenses Issued Under MDR, 2017 - FORM 4Document41 pagesEstablishment Licenses Issued Under MDR, 2017 - FORM 4AmberSattiNo ratings yet
- Department of Education: Annual Gender and Development (Gad) Plan and BudgetDocument6 pagesDepartment of Education: Annual Gender and Development (Gad) Plan and BudgetJaymar Padayao0% (1)
- BAXIE (M-UE-22) : Eight PathogensDocument1 pageBAXIE (M-UE-22) : Eight Pathogensray72roNo ratings yet
- School Form 2 Daily Attendance Report of Learners For Senior High School (SF2-SHS)Document3 pagesSchool Form 2 Daily Attendance Report of Learners For Senior High School (SF2-SHS)Jemarjo SalandananNo ratings yet
- Suicide in Children and Adolescents Cambridge Child and Adolescent PsychiatryDocument333 pagesSuicide in Children and Adolescents Cambridge Child and Adolescent PsychiatryFlorin Tudose100% (1)
- Autoimmune Hemolytic AnemiaDocument7 pagesAutoimmune Hemolytic AnemiaHoopmen SilaenNo ratings yet
- Control and RandomizationDocument18 pagesControl and RandomizationRARCHITA SHARMANo ratings yet
- Health Problem Family Nursing Problem Goal of Care Objectives of Care Intervention Plan Resources Required EvaluationDocument2 pagesHealth Problem Family Nursing Problem Goal of Care Objectives of Care Intervention Plan Resources Required EvaluationLuis WashingtonNo ratings yet
- Guidelines For Preventing Workplace Violence For Healthcare and Social Service WorkersDocument60 pagesGuidelines For Preventing Workplace Violence For Healthcare and Social Service WorkersSafety and Health magazineNo ratings yet
- Stroke Hemoragik: Yusi Rizky N 1 6 1 0 2 1 1 0 5 1Document19 pagesStroke Hemoragik: Yusi Rizky N 1 6 1 0 2 1 1 0 5 1Yusi RizkyNo ratings yet
- National Nursing Audit Ministry of Health Malaysia Version 3 April 2019 P5VSDocument4 pagesNational Nursing Audit Ministry of Health Malaysia Version 3 April 2019 P5VSmhd hasnanNo ratings yet
- Redacted Complaint Beaudoin V Baker FinalDocument25 pagesRedacted Complaint Beaudoin V Baker FinalKyle BeckerNo ratings yet
- Neonatal Mechanical Ventilation Predictors of Mortality and OutcomesDocument8 pagesNeonatal Mechanical Ventilation Predictors of Mortality and OutcomesAthenaeum Scientific PublishersNo ratings yet
- Lecture - Nutrition and Diet TherapyDocument9 pagesLecture - Nutrition and Diet TherapyLalaine Marie BianzonNo ratings yet
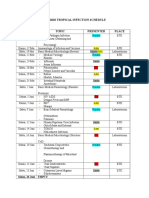
- Imo Tropical Infection ScheduleDocument3 pagesImo Tropical Infection ScheduleHendroMaleNo ratings yet
- Andrew Tran ResumeDocument2 pagesAndrew Tran Resumeapi-465054778No ratings yet