Professional Documents
Culture Documents
M.01 MNCHN (Part 1) (Dr. Hora) (03-04-21)
M.01 MNCHN (Part 1) (Dr. Hora) (03-04-21)
Uploaded by
VanessaCopyright:
Available Formats
You might also like
- NBME 14 - AnswersDocument208 pagesNBME 14 - Answersmerontesfaye51No ratings yet
- Fhsis Mop Ver. 2018 FinalDocument489 pagesFhsis Mop Ver. 2018 FinalJoyce100% (5)
- Safe Motherhood: Reproductive Health I Clinical Medicine ClassDocument32 pagesSafe Motherhood: Reproductive Health I Clinical Medicine Classmoreen kipkemoiNo ratings yet
- Birth Control Pill & Lupron Sample IVF CalendarDocument2 pagesBirth Control Pill & Lupron Sample IVF Calendarandi hamatajNo ratings yet
- MCHN Midterm NotesDocument27 pagesMCHN Midterm NotesSeungwoo ParkNo ratings yet
- NCM 109 Lec PrelimsDocument12 pagesNCM 109 Lec PrelimsAngel Kim MalabananNo ratings yet
- MNCH-FINAL. 2023pptxDocument28 pagesMNCH-FINAL. 2023pptxpritaneionNo ratings yet
- 5 - Maternal and Child Health MCV EditedDocument18 pages5 - Maternal and Child Health MCV Editedcantonecchi8142No ratings yet
- LGT-9 Introduction To Child Health CareDocument26 pagesLGT-9 Introduction To Child Health CareMazinNo ratings yet
- Philippines: At-A-Glance: PhilippinesDocument8 pagesPhilippines: At-A-Glance: PhilippinesGari LazaroNo ratings yet
- Prelim - MCN LecDocument17 pagesPrelim - MCN Leclaurynejoyce26No ratings yet
- Improving Perinatal and Neonatal Mortality in Sri Lanka: Is It Cost Effective?Document5 pagesImproving Perinatal and Neonatal Mortality in Sri Lanka: Is It Cost Effective?Vijayakanth VijayakumarNo ratings yet
- Inaugural Lecture-Maternal and Neonatal Health-A Global Overview-Soltani 2016Document49 pagesInaugural Lecture-Maternal and Neonatal Health-A Global Overview-Soltani 2016HasanalitaNo ratings yet
- MCH MPH-MSPH 2023Document95 pagesMCH MPH-MSPH 2023ArRa Za (Arra)No ratings yet
- FeDocument7 pagesFeWilfredo PesanteNo ratings yet
- Antenatal Care IsDocument19 pagesAntenatal Care IsShivani Shah100% (1)
- Care of Mother and Child at RiskDocument2 pagesCare of Mother and Child at RiskJane CuencaNo ratings yet
- Week 11 Framework For Maternal and Child Health Nursing Focusing On at Risk High Risk and Sick ClientsDocument15 pagesWeek 11 Framework For Maternal and Child Health Nursing Focusing On at Risk High Risk and Sick Clientss.tabaquin.edwardjrNo ratings yet
- Maternal CareDocument13 pagesMaternal CareHannan AliNo ratings yet
- An Analysis of Impact of Antenatl Care in Reducing Maternal Mortality RateDocument46 pagesAn Analysis of Impact of Antenatl Care in Reducing Maternal Mortality RateUsman Ahmad TijjaniNo ratings yet
- EMONCDocument17 pagesEMONCJessie OranoNo ratings yet
- Maternal Health in NigeriaDocument8 pagesMaternal Health in NigeriaprofangieNo ratings yet
- MCNDocument47 pagesMCNSamantha DiegoNo ratings yet
- Lec Framework Care of MotherDocument27 pagesLec Framework Care of MotherRica ParcasioNo ratings yet
- 09-9 Child&Maternal HealthDocument43 pages09-9 Child&Maternal HealthAhmad SobihNo ratings yet
- I. Framework For Maternal and Child Health Nursing (MCN) Focusing On At-Risk, High Risk, and Sick ClientsDocument5 pagesI. Framework For Maternal and Child Health Nursing (MCN) Focusing On At-Risk, High Risk, and Sick ClientsSophia Loraine Dorone Jesura100% (1)
- 11.21 - Maternal Health Status in The PhilippinesDocument7 pages11.21 - Maternal Health Status in The PhilippinesJøshua CruzNo ratings yet
- Neonatal Survival 1: SeriesDocument10 pagesNeonatal Survival 1: Seriesoyunbileg tudevNo ratings yet
- 1PRELIMSDocument37 pages1PRELIMSJohn marc TolentinoNo ratings yet
- Part 2 MCHDocument30 pagesPart 2 MCHademabdella38No ratings yet
- Maternal Child Health 2Document4 pagesMaternal Child Health 2chiaramaemakilalaapatNo ratings yet
- MCHN PrelimDocument17 pagesMCHN PrelimantoynetteaNo ratings yet
- Obstetrics and Gynecology: in PH in Relation To Health CareDocument22 pagesObstetrics and Gynecology: in PH in Relation To Health Carejean de los santosNo ratings yet
- Obstetrics 1Document35 pagesObstetrics 1HUTALLA CezanneNo ratings yet
- Awareness of The Impact of Ante-Natal Care (Anc) Services in PreventingDocument8 pagesAwareness of The Impact of Ante-Natal Care (Anc) Services in PreventingUsman Ahmad TijjaniNo ratings yet
- CopyDesign 632 25 Bed Hospital1Document5 pagesCopyDesign 632 25 Bed Hospital1Derick DelacruzNo ratings yet
- Womens HealthDocument23 pagesWomens Healthtaty jatyNo ratings yet
- Maternal and Child Nursing - Essential Intrapartum Newborn CareDocument8 pagesMaternal and Child Nursing - Essential Intrapartum Newborn CareSofia Resol100% (1)
- QI Basic Training Participant Hand Out 2021Document257 pagesQI Basic Training Participant Hand Out 2021drkefyalewtayeNo ratings yet
- WHO RHR 19.20 Eng PDFDocument4 pagesWHO RHR 19.20 Eng PDFElsa SembiringNo ratings yet
- 1.2 Current Aproaches - 2017Document30 pages1.2 Current Aproaches - 2017Abdella KesimNo ratings yet
- Lesson 1 - Global & National Health Situations, Definition & Focus, Public Health, and Community HealthDocument2 pagesLesson 1 - Global & National Health Situations, Definition & Focus, Public Health, and Community HealthA CNo ratings yet
- Maternal and Child MonitoringDocument10 pagesMaternal and Child MonitoringJoan VenidaNo ratings yet
- Maternal Note 1Document34 pagesMaternal Note 1JAN REY LANADONo ratings yet
- MCN Lec Group 1 Written ReportDocument51 pagesMCN Lec Group 1 Written ReportTrishNo ratings yet
- CHN SemifinalsDocument8 pagesCHN SemifinalsBAUZON, JANINE, C.No ratings yet
- 109 Midterms TransesDocument28 pages109 Midterms TransestumabotaboarianeNo ratings yet
- Hauwa'u - Chap-1-5Document51 pagesHauwa'u - Chap-1-5Usman Ahmad TijjaniNo ratings yet
- Excerpts From An Unpublished Thesis: WWW - Usaid.govDocument4 pagesExcerpts From An Unpublished Thesis: WWW - Usaid.govJaylen CayNo ratings yet
- The Current Maternal and Child Health and Health NutritionDocument12 pagesThe Current Maternal and Child Health and Health NutritionGiselle EstoquiaNo ratings yet
- MCN Reviewer 1STDocument10 pagesMCN Reviewer 1STAnthony Joseph ReyesNo ratings yet
- Maternal MortalityDocument32 pagesMaternal MortalityKristel AnneNo ratings yet
- ROLES RESPONSIBILITIES OF A MC NURSE IN CHALENGEING SITUATIONS Merged Compressed Merged MergedDocument53 pagesROLES RESPONSIBILITIES OF A MC NURSE IN CHALENGEING SITUATIONS Merged Compressed Merged MergedYuuki Chitose (tai-kun)No ratings yet
- Bemonc - S-Cort - SlidesDocument97 pagesBemonc - S-Cort - SlidesErrol LlanesNo ratings yet
- Unit 3.3 Safe Motherhood Doc (1-5)Document5 pagesUnit 3.3 Safe Motherhood Doc (1-5)mahesh thapaNo ratings yet
- Maternity Chapter 01 Framework For Maternal and Child Health Nursing PDFDocument9 pagesMaternity Chapter 01 Framework For Maternal and Child Health Nursing PDFChskNo ratings yet
- Framework For Maternal and Child Health NursingDocument10 pagesFramework For Maternal and Child Health NursingSHERYL TEMPLANo ratings yet
- SafeDocument18 pagesSafeSaripda JaramillaNo ratings yet
- Philippine Government Policies On Maternal, Newborn and Child Health and NutritionDocument20 pagesPhilippine Government Policies On Maternal, Newborn and Child Health and Nutritioncarlos-tulali-1309100% (34)
- Skilled Birth Attendance-Lessons LearntDocument9 pagesSkilled Birth Attendance-Lessons LearntTriksha GeorgeNo ratings yet
- On MCH and Maternal Health in BangladeshDocument46 pagesOn MCH and Maternal Health in BangladeshTanni ChowdhuryNo ratings yet
- NICU Journal: A Parent's JourneyFrom EverandNICU Journal: A Parent's JourneyNo ratings yet
- M.05 Palliative Care (Dr. Flores) (03-01-21)Document4 pagesM.05 Palliative Care (Dr. Flores) (03-01-21)VanessaNo ratings yet
- M.02 MNCHN (Part 2) (Dr. Hora) (03-04-21)Document4 pagesM.02 MNCHN (Part 2) (Dr. Hora) (03-04-21)VanessaNo ratings yet
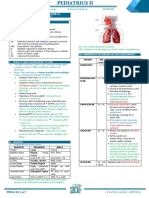
- M.03 Respiratory Disorders Part 3 (Dr. Tandoc) (10-26-2020)Document7 pagesM.03 Respiratory Disorders Part 3 (Dr. Tandoc) (10-26-2020)VanessaNo ratings yet
- Saint Louis University School of Medicine Mmxxii: Dr. Hora - 03/04/2021Document9 pagesSaint Louis University School of Medicine Mmxxii: Dr. Hora - 03/04/2021VanessaNo ratings yet
- M.04 IMCI (Part 2) (Dr. Hora) (03-03-21)Document5 pagesM.04 IMCI (Part 2) (Dr. Hora) (03-03-21)VanessaNo ratings yet
- M.03 Respiratory Disorders of Children Part 1 (Dr. Tandoc) (10-26-20)Document7 pagesM.03 Respiratory Disorders of Children Part 1 (Dr. Tandoc) (10-26-20)VanessaNo ratings yet
- Saint Louis University School of Medicine Mmxxii: Dr. Quitiquit - November 11, 2020Document9 pagesSaint Louis University School of Medicine Mmxxii: Dr. Quitiquit - November 11, 2020VanessaNo ratings yet
- M.04 Liver (Part 4) (Dr. Cinio) (10-29-20)Document8 pagesM.04 Liver (Part 4) (Dr. Cinio) (10-29-20)VanessaNo ratings yet
- M.04 MEDICAL ETHICS AND THE CHRISTIAN PHYSICIAN (Dr. Tolentino)Document9 pagesM.04 MEDICAL ETHICS AND THE CHRISTIAN PHYSICIAN (Dr. Tolentino)VanessaNo ratings yet
- Placenta PreviaDocument10 pagesPlacenta PreviaAdriane ComaNo ratings yet
- Sexual, Marital Perceivednihms199025Document16 pagesSexual, Marital Perceivednihms199025annisa habibullohNo ratings yet
- On Family WelfareDocument45 pagesOn Family WelfareSweety Yadav100% (2)
- Tosoh Series 2147Document3 pagesTosoh Series 2147ShahinNo ratings yet
- Vitamin D and PCOSDocument39 pagesVitamin D and PCOSsyafiraNo ratings yet
- Review of Literature Related To Low Birth Weight BabiesDocument4 pagesReview of Literature Related To Low Birth Weight BabiesgwfdurbndNo ratings yet
- GyaneDocument188 pagesGyaneSupekshya ShresthaNo ratings yet
- Case Report Iufd - RashifDocument32 pagesCase Report Iufd - RashifM Nur MuhammadNo ratings yet
- Twin Anemia Polycythemia SyndromesDocument67 pagesTwin Anemia Polycythemia SyndromesBhupendra GuptaNo ratings yet
- Midwifery Exam PracticeDocument12 pagesMidwifery Exam Practicekristel ludangcoNo ratings yet
- Week 12 13122022 015614pmDocument12 pagesWeek 12 13122022 015614pmJehanzaib AminNo ratings yet
- The Beautiful Mother - 1stdraftDocument254 pagesThe Beautiful Mother - 1stdraftMagus PrintNo ratings yet
- Science Module For Grade 10: Guagua National Colleges, Inc. Guagua, PampangaDocument62 pagesScience Module For Grade 10: Guagua National Colleges, Inc. Guagua, PampangaNorman Punla SantosNo ratings yet
- Abortion 150119000246 Conversion Gate02Document121 pagesAbortion 150119000246 Conversion Gate02chetankumarbhumireddyNo ratings yet
- Cow Calf CalendarDocument5 pagesCow Calf CalendarcapsfastNo ratings yet
- Puerperal PyrexiaDocument20 pagesPuerperal Pyrexiaهلا اكرم عقل طميزهNo ratings yet
- Quarter 2 Week 7-MAPEH8Document2 pagesQuarter 2 Week 7-MAPEH8Kimberly Ann Castro VitugNo ratings yet
- Biology Unit 1 Module 3 - Question and Answers 2013 To 2016Document20 pagesBiology Unit 1 Module 3 - Question and Answers 2013 To 2016Darion SinghNo ratings yet
- The Endometrial Factor A Reproductive Precision Medicine ApproachDocument275 pagesThe Endometrial Factor A Reproductive Precision Medicine ApproachErika Rosas100% (2)
- Oxytocin, Dinoprostone, Cefuroxime Drug StudyDocument3 pagesOxytocin, Dinoprostone, Cefuroxime Drug StudyMary Shane MoraldeNo ratings yet
- PubLSIS II Survey Finding Report June 2018Document620 pagesPubLSIS II Survey Finding Report June 2018Mao udangNo ratings yet
- Nutrition Through The Life Cycle 6Th Edition Brown Test Bank Full Chapter PDFDocument43 pagesNutrition Through The Life Cycle 6Th Edition Brown Test Bank Full Chapter PDFnhanselinak9wr16100% (11)
- Breast Care and Breast Feeding For CI, by DR Abera Sept 2021Document57 pagesBreast Care and Breast Feeding For CI, by DR Abera Sept 2021Kerod AbebeNo ratings yet
- Tosoh Bioscience Tosoh Bioscience: CL Aia-Pack ReagentsDocument2 pagesTosoh Bioscience Tosoh Bioscience: CL Aia-Pack ReagentsAleksandar MisicNo ratings yet
- Direct and Indirect SpeechDocument3 pagesDirect and Indirect SpeechImelda DayaNo ratings yet
- SaluEric New An Alluring Imp WPS Office 1Document7 pagesSaluEric New An Alluring Imp WPS Office 1Eric SaludaresNo ratings yet
- English8 Quarter3Document3 pagesEnglish8 Quarter3Knelle Rose TajoNo ratings yet
M.01 MNCHN (Part 1) (Dr. Hora) (03-04-21)
M.01 MNCHN (Part 1) (Dr. Hora) (03-04-21)
Uploaded by
VanessaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
M.01 MNCHN (Part 1) (Dr. Hora) (03-04-21)
M.01 MNCHN (Part 1) (Dr. Hora) (03-04-21)
Uploaded by
VanessaCopyright:
Available Formats
FAMILY AND COMMUNITY MEDICINE III
Saint Louis University School of Medicine MMXXII
M.01 MNCHN Part 1 (Maternal) • Lifetime risk of dying from maternal causes to Filipino
Dr. Nelson Hora | March 04, 2021 women of reproductive age is 1:120
• 14% of death among women of reproductive age is due to
OUTLINE maternal causes
I. MNCHN • Slow decline of Maternal Mortality Rate (MMR)
II. Epidemiology o 209/100,000 live births (1990)
III. MNCHN Core Package Services o 162/100,000 live births (2006)
IV. Maternal Care • Decline in UFMR and IMR but not in NMR
V. DOH Maternal Package o Under-Five Mortality Rate (UFMR)
VI. Delivery ▪ 61/1000 live births in 1990
VII. Postpartum Period ▪ 32/1000 live births in 2008
o Infant Mortality Rate (IMR)
I. Maternal, Newborn, Child Health and Nutrition (MNCHN) ▪ 42% in 1990
• DOH Administrative Order (A.O.) 2008-0029 ▪ 26% in 2006
o “Implementing Health Reforms for Rapid Reduction of o Neonatal Mortality Rate (NMR)
Maternal and Neonatal Mortality” ▪ 17/1000 live births in 2006
o Provides the strategy for rapidly reducing maternal and ▪ In 2000-2003, newborn death accounted for 37% of all
neonatal deaths through the provision of a package of UFMR. Most neonatal deaths occur within the first 2
maternal, newborn, child health, and nutrition (MNCHN) weeks after birth, half of which occur in the first 2 days
services. of life.
o To assess the health status of the community, look at the
vulnerable population mortality rates. B. FACTORS CONTRIBUTING TO MATERNAL AND NEONATAL
o Part of the Sustainable Developmental Goals (SDG) DEATHS
• The strategy aims to achieve the following intermediate results: 1. Mistimed, unplanned, unwanted, and unsupported
1. Every pregnancy is wanted, planned, and supported. pregnancy
2. Every pregnancy is adequately managed throughout its • Reason why family planning methods are promoted.
course. • Rape victims should be given a choice if they would want to take a
o Womb-to-womb: Conception until Delivery ‘morning-after-pill’.
o But ideally, pre-pregnant mothers should be given 2. Not securing adequate care during the course of pregnancy
supplements of iron and folate • Pregnant patients should be advised to seek Prenatal care at the
3. Every delivery is facility-based and managed by skilled time they become cognizant of their pregnancy.
birth attendants or skilled health professionals. • Most pregnant patients come only for consultation when they are
4. Every mother and newborn pair secures proper post- already in labor and preventable complications of pregnancy are
partum and newborn care with smooth transitions to the not addressed.
women’s health care package for the mother and child 3. Delivering without being attended to by skilled health
survival package for the newborn. professionals, and lack of access to emergency obstetric
o First 1000 days Program and newborn services
• ‘Hilots’, despite having the experience in assisting mothers, they
II. EPIDEMIOLOGY should still be regarded as the last choice because they are not
• Pregnancy-related death worldwide: 500,000/year using improved and scientifically proven techniques.
o 99% from developing countries 4. Not securing proper postpartum and newborn care for the
▪ Maternal mortality rate (WHO): 400/100,000pop mother and her newborn, respectively
▪ Developing countries are more burdened by diseases • Inappropriate postpartum care used by ‘hilots’ include applying ash
that contributes to these mortalities, however, majority and chewed guava leaves on the umbilical stump and immediately
of the world’s resources are concentrated to Developed giving the babies a bath.
countries
o Compounded by: III. MNCHN CORE PACKAGE OF SERVICES
▪ High fertility • Cuts across the following stages:
▪ Poor nutritional status 1. Pre-pregnancy
▪ Lack of basic health services 2. Pregnancy
• Infant mortality: 7.1 million/year 3. Delivery
o 50% die in the first 28 days after birth (neonatal period) 4. Post-partum
o 75% die in the first week after birth 5. Newborn care
o Neonatal and perinatal death are related to maternal 6. Child care
causes.
• Majority of these maternal and newborn deaths are preventable IV. MATERNAL CARE
with currently available technologies. • Focuses on the child-bearing function of the woman
• Goals:
A. PHILIPPINE SITUATION o Promotion of safe motherhood and women’s health
• 14 million Filipino women are in the reproductive age group (15-49 o Ensure healthy newborn
years old)
o 9 million are married or have partners PRIMARY CAUSES OF MATERNAL MORTALITY
o 6 million are considered to be at risk if they become Direct Causes Indirect Causes
pregnant because they: • Severe bleeding • Anemia
▪ are either too young (<20 years old) • Infection • Malaria
▪ or too old (>35 years old) • Consequences of unsafe • Poverty
▪ have >4 pregnancies abortions • Race, ethnic, or tribal
▪ have too close or unspaced pregnancies (<15 months) • Hypertensive disorders affiliation
▪ too sick (mostly anemic or underweight) such as pre-eclampsia and • Lack of education
• Average fertility rate: 3.7 (3-4 number of children per woman) eclampsia
• 2.3 million women are expected to get pregnant every year • Obstructed labor
o 2 million of those who become pregnant will deliver
FAMCOMM III |1 of 3 [HIPOLITO, GALAS]
FAMILY AND COMMUNITY MEDICINE III
Saint Louis University School of Medicine MMXXII
WHO. 1999 “Reduction of maternal mortality. A joint WHO/ UNFPA/
UNICEF/ World Bank Statement” PRENATAL CARE UPDATES
• Most direct causes can be addressed and prevented by skilled Before Now
Health Practitioners during the prenatal period. Risk scoring and prediction Recognizes that every
• Indirect causes are related to social (poverty) and environmental pregnancy is at risk
problems. PARADIGM SHIFT
• Every pregnancy faces risks
MAJOR DISABILITIES FROM PREGNANCY AND CHILDBIRTH • Therefore, at every AP visit we must be very careful in doing the
COMPLICATIONS history and physical exam of all pregnant women.
• These complications can be addressed appropriately if patients
deliver in a facility/hospital. Remember: Once a woman is pregnant, most serious complications
Severe bleeding Infection CANNOT be predicted or prevented, but they CAN be treated.
Pelvic inflammatory disease • That is why home deliveries or deliveries by traditional birth
Anemia
Chronic pelvic pain attendants are not advocated anymore.
Infertility
Reproductive organ damage
Hormonal damage
Infertility 2. TETANUS TOXOID
Obstructed or prolonged • Today, Tetanus toxoid is no longer available. Tdap combination
Unsafe abortion
labor is given instead and are given at government institutions
Incontinence Pelvic inflammatory disease because diphtheria protection is also needed for the mother.
Fistula Chronic pelvic pain • During first pregnancy, the woman is recommend
Genital prolapse Reproductive organ damage • ed to have at least 2 doses of TT.
Uterine rupture Reproductive tract infection • Ideally, the 1st dose should be given pre-pregnancy. If not, the
Nerve damage Infertility 1st dose will be given at the 2nd trimester.
Pregnancy-induced hypertension
Precursor to chronic hypertension TETANUS TOXOID IMMUNIZATION SCHEDULES
Kidney failure Infant’s
Protection
Nervous system problems Duration of
Vaccine Minimum Interval from
Lori Ashford. 2002. Hidden Suffering: Disabilities from Pregnancy and Protection Neonatal
Childbirth in Less Developed Countries. PRB. Tetanus
At first contact
NIL – No
V. DOH MATERNAL CARE PACKAGE with woman 15-49
protection
1. ANTENATAL REGISTRATION years (even if the
TT1 (Hence, 2nd dose is None
Antepartum Visits (Minimum Requirement) woman is not yet
really needed to
1st trimester 1 visit pregnant) or at first
acquire protection)
2nd trimester 1 visit AP visit.
3rd trimester 2 visits 3 years of
At least 4 weeks
But ideally: TT2 protection for the ✓
after TT1
• Monthly until the 30th week mother
• Every 2 weeks until the 36th week 5 years of
At least 6 months
• Weekly until Delivery TT3 protection for the ✓
after TT2
• Women can have as much consultation as needed mother
At least 1 year 10 years of
Purpose of prenatal check-ups: after TT3 or any protection for the
TT4 ✓
• Prepare and cope with the pregnancy time within the 10-yr mother
o The mother or couple should be counselled on what to do, period from TT3
not only medically, but also financially. Lifetime
At least 1 year
• Early detection and treatment of illnesses TT5 protection for the ✓
after TT4
• Know the estimate schedule of delivery or the expected date of mother
confinement.
o Use the Naegele’s Rule 3. NUTRITION
• Includes Vitamin A, Iron, Folate, and calcium supplementation
Danger signs of pregnancy: (Should be noted every AP visit) • 50.3% anemic pregnant women
• Vaginal bleeding – it can be a sign of abortion or problems in • 46% anemic lactating women
placental implantation • Supplements:
• Severe abdominal pain – symptom of impending abortion or o Vitamin A
infection ▪ Teratogenic in high doses
• Looks very ill and/or has fever – especially if patient is from o Iron
malarious areas ▪ Not tolerated during the 1st trimester due to morning
• Severe headache with visual disturbance – symptom of pre- sickness
eclampsia or pregnancy-induced hypertension ▪ Given preferably during the 2nd trimester
• Severe breathing difficulty o Folate
• Severe vomiting – may lead to dehydration of both mother and ▪ Given during the 1st trimester
child ▪ To prevent Neural Tube Defects
• Unconscious and/or has convulsions – manifestation of pre-
eclampsia 4. TREATMENT OF EXISTING DISEASES
• Diabetes
Risk factors: • Anemia
• Too young/old • Heart disease
• Too many (multigravida) • Refer to a specialist if needed.
• Too soon (early labor)
• Too sick
FAMCOMM III |2 of 3 [HIPOLITO, GALAS]
FAMILY AND COMMUNITY MEDICINE III
Saint Louis University School of Medicine MMXXII
5. RECOGNITION, EARLY DETECTION, AND MANAGEMENT OF • Fear of ill treatment at the facility
COMPLICATIONS BEFORE, DURING AND AFTER DELIVERY o Home Delivery is preferred mostly by patients because they
Prenatal tests: (Minimum laboratory examinations to be done) are personally cared by ‘hilots’. Care provided by ‘hilots’
• Urinalysis include washing soiled blankets and cooking home-cooked
• Complete Blood Count, Hemoglobin meals for the mother
• Blood typing • Culture
• VDRL/RPR test for syphilis • Poor decision making
• Hepatitis B screening • No person to take care of children and/or livestock
• HIV Screening • No companion when going to the facility
• FBS/ 2-hr Oral Glucose Tolerance Test (Standard to all pregnant • Address these problems during the prenatal period or
women) when doing the birth plan.
o Pregnant patients should not be required to fast, unless
Gestational Diabetes Mellitus is suspected 2. Delay in identifying and reaching the appropriate health
• Fecalysis facility
o Since parasitism is prevalent in the country, standard • Patient intends to go to a health facility but there is no available
deworming is done in the 2nd trimester. transportation
• Distance: woman’s home to the facility
BIRTH PLAN • Lack of roads or poor condition of roads
• A document prepared during the prenatal care which states: • No emergency transport
o The woman’s conditions during pregnancy • Unawareness regarding existing services
o Her preferences for her place of delivery • No referral system
o Her choice of birth attendant (midwife, physician) • Lack of communication with referral facility
o Her available resources for her childbirth and newborn baby • Lack of moral, financial, and logistic support from neighbors and
o Preparations needed should an emergency situation arise barangay officials
during pregnancy, childbirth, and postpartum (includes: o These officials are also involved because maternal health is
transportation, who will take care of the children when mother not just a personal problem, it is a problem of the community.
is in labor/give birth) It reflects the overall health community system. Maternal
mortality rate is one of the indicators if the health system is
working or not.
3. Delay in receiving appropriate and adequate care at the
health facility
• Patient is able to reach the facility, but it is not fully equipped.
• Lack of health care worker
• Non-professional attitudes of health workers
• Shortage of supplies (medicines, blood, etc.)
• Poor skills of healthcare providers
• Health is not a priority for officials in the LGU
• Lack of budget from the LGU
Gone are the days that women deliver at home because environment at
home is not that conducive especially in rural areas.
Skilled Birth Attendants include doctors, nurses, midwives who are
trained to respond to emergencies and complications that might arise
during delivery.
6. CLEAN AND SAFE DELIVERY
• 3% of the 3.5% expected antepartum women will progress to term
V. POSTPARTUM PERIOD
7. PROMOTION AND SUPPORT TO BREASTFEEDING AND Key Events
MANAGEMENT OF BREAST COMPLICATIONS 24 hours after delivery 1st postpartum visit
• We have to be advocates of breastfeeding because of the benefits 1 week after delivery 2nd postpartum visit
attached to it. Counselled to start their Family
Planning methods, whether artificial
Within 6 weeks after
8. HEALTH EDUCATION, COUNSELING, AND FAMILY or natural, since at this time, the
delivery
PLANNING SERVICES Mother’s menstrual cycle may come
back
9. STD/HIV PREVENTION AND MANAGEMENT Within a month after Vitamin A
delivery (200,000 IU supplementation)
10. DENTAL CARE For at least 3 months FeSO4 supplement
V. DELIVERY
• 14 % of deaths among women aged 15-49 are due to maternal
deaths.
3 DELAYS THAT CAUSE MATERNAL DEATH (WHO)
1. Delay in deciding to seek medical care
• Failure to recognize danger signs
• No skilled birth attendants in the area (assisted by whoever is
around)
• No money
• Unwanted pregnancy
• Poor services
FAMCOMM III |3 of 3 [HIPOLITO, GALAS]
You might also like
- NBME 14 - AnswersDocument208 pagesNBME 14 - Answersmerontesfaye51No ratings yet
- Fhsis Mop Ver. 2018 FinalDocument489 pagesFhsis Mop Ver. 2018 FinalJoyce100% (5)
- Safe Motherhood: Reproductive Health I Clinical Medicine ClassDocument32 pagesSafe Motherhood: Reproductive Health I Clinical Medicine Classmoreen kipkemoiNo ratings yet
- Birth Control Pill & Lupron Sample IVF CalendarDocument2 pagesBirth Control Pill & Lupron Sample IVF Calendarandi hamatajNo ratings yet
- MCHN Midterm NotesDocument27 pagesMCHN Midterm NotesSeungwoo ParkNo ratings yet
- NCM 109 Lec PrelimsDocument12 pagesNCM 109 Lec PrelimsAngel Kim MalabananNo ratings yet
- MNCH-FINAL. 2023pptxDocument28 pagesMNCH-FINAL. 2023pptxpritaneionNo ratings yet
- 5 - Maternal and Child Health MCV EditedDocument18 pages5 - Maternal and Child Health MCV Editedcantonecchi8142No ratings yet
- LGT-9 Introduction To Child Health CareDocument26 pagesLGT-9 Introduction To Child Health CareMazinNo ratings yet
- Philippines: At-A-Glance: PhilippinesDocument8 pagesPhilippines: At-A-Glance: PhilippinesGari LazaroNo ratings yet
- Prelim - MCN LecDocument17 pagesPrelim - MCN Leclaurynejoyce26No ratings yet
- Improving Perinatal and Neonatal Mortality in Sri Lanka: Is It Cost Effective?Document5 pagesImproving Perinatal and Neonatal Mortality in Sri Lanka: Is It Cost Effective?Vijayakanth VijayakumarNo ratings yet
- Inaugural Lecture-Maternal and Neonatal Health-A Global Overview-Soltani 2016Document49 pagesInaugural Lecture-Maternal and Neonatal Health-A Global Overview-Soltani 2016HasanalitaNo ratings yet
- MCH MPH-MSPH 2023Document95 pagesMCH MPH-MSPH 2023ArRa Za (Arra)No ratings yet
- FeDocument7 pagesFeWilfredo PesanteNo ratings yet
- Antenatal Care IsDocument19 pagesAntenatal Care IsShivani Shah100% (1)
- Care of Mother and Child at RiskDocument2 pagesCare of Mother and Child at RiskJane CuencaNo ratings yet
- Week 11 Framework For Maternal and Child Health Nursing Focusing On at Risk High Risk and Sick ClientsDocument15 pagesWeek 11 Framework For Maternal and Child Health Nursing Focusing On at Risk High Risk and Sick Clientss.tabaquin.edwardjrNo ratings yet
- Maternal CareDocument13 pagesMaternal CareHannan AliNo ratings yet
- An Analysis of Impact of Antenatl Care in Reducing Maternal Mortality RateDocument46 pagesAn Analysis of Impact of Antenatl Care in Reducing Maternal Mortality RateUsman Ahmad TijjaniNo ratings yet
- EMONCDocument17 pagesEMONCJessie OranoNo ratings yet
- Maternal Health in NigeriaDocument8 pagesMaternal Health in NigeriaprofangieNo ratings yet
- MCNDocument47 pagesMCNSamantha DiegoNo ratings yet
- Lec Framework Care of MotherDocument27 pagesLec Framework Care of MotherRica ParcasioNo ratings yet
- 09-9 Child&Maternal HealthDocument43 pages09-9 Child&Maternal HealthAhmad SobihNo ratings yet
- I. Framework For Maternal and Child Health Nursing (MCN) Focusing On At-Risk, High Risk, and Sick ClientsDocument5 pagesI. Framework For Maternal and Child Health Nursing (MCN) Focusing On At-Risk, High Risk, and Sick ClientsSophia Loraine Dorone Jesura100% (1)
- 11.21 - Maternal Health Status in The PhilippinesDocument7 pages11.21 - Maternal Health Status in The PhilippinesJøshua CruzNo ratings yet
- Neonatal Survival 1: SeriesDocument10 pagesNeonatal Survival 1: Seriesoyunbileg tudevNo ratings yet
- 1PRELIMSDocument37 pages1PRELIMSJohn marc TolentinoNo ratings yet
- Part 2 MCHDocument30 pagesPart 2 MCHademabdella38No ratings yet
- Maternal Child Health 2Document4 pagesMaternal Child Health 2chiaramaemakilalaapatNo ratings yet
- MCHN PrelimDocument17 pagesMCHN PrelimantoynetteaNo ratings yet
- Obstetrics and Gynecology: in PH in Relation To Health CareDocument22 pagesObstetrics and Gynecology: in PH in Relation To Health Carejean de los santosNo ratings yet
- Obstetrics 1Document35 pagesObstetrics 1HUTALLA CezanneNo ratings yet
- Awareness of The Impact of Ante-Natal Care (Anc) Services in PreventingDocument8 pagesAwareness of The Impact of Ante-Natal Care (Anc) Services in PreventingUsman Ahmad TijjaniNo ratings yet
- CopyDesign 632 25 Bed Hospital1Document5 pagesCopyDesign 632 25 Bed Hospital1Derick DelacruzNo ratings yet
- Womens HealthDocument23 pagesWomens Healthtaty jatyNo ratings yet
- Maternal and Child Nursing - Essential Intrapartum Newborn CareDocument8 pagesMaternal and Child Nursing - Essential Intrapartum Newborn CareSofia Resol100% (1)
- QI Basic Training Participant Hand Out 2021Document257 pagesQI Basic Training Participant Hand Out 2021drkefyalewtayeNo ratings yet
- WHO RHR 19.20 Eng PDFDocument4 pagesWHO RHR 19.20 Eng PDFElsa SembiringNo ratings yet
- 1.2 Current Aproaches - 2017Document30 pages1.2 Current Aproaches - 2017Abdella KesimNo ratings yet
- Lesson 1 - Global & National Health Situations, Definition & Focus, Public Health, and Community HealthDocument2 pagesLesson 1 - Global & National Health Situations, Definition & Focus, Public Health, and Community HealthA CNo ratings yet
- Maternal and Child MonitoringDocument10 pagesMaternal and Child MonitoringJoan VenidaNo ratings yet
- Maternal Note 1Document34 pagesMaternal Note 1JAN REY LANADONo ratings yet
- MCN Lec Group 1 Written ReportDocument51 pagesMCN Lec Group 1 Written ReportTrishNo ratings yet
- CHN SemifinalsDocument8 pagesCHN SemifinalsBAUZON, JANINE, C.No ratings yet
- 109 Midterms TransesDocument28 pages109 Midterms TransestumabotaboarianeNo ratings yet
- Hauwa'u - Chap-1-5Document51 pagesHauwa'u - Chap-1-5Usman Ahmad TijjaniNo ratings yet
- Excerpts From An Unpublished Thesis: WWW - Usaid.govDocument4 pagesExcerpts From An Unpublished Thesis: WWW - Usaid.govJaylen CayNo ratings yet
- The Current Maternal and Child Health and Health NutritionDocument12 pagesThe Current Maternal and Child Health and Health NutritionGiselle EstoquiaNo ratings yet
- MCN Reviewer 1STDocument10 pagesMCN Reviewer 1STAnthony Joseph ReyesNo ratings yet
- Maternal MortalityDocument32 pagesMaternal MortalityKristel AnneNo ratings yet
- ROLES RESPONSIBILITIES OF A MC NURSE IN CHALENGEING SITUATIONS Merged Compressed Merged MergedDocument53 pagesROLES RESPONSIBILITIES OF A MC NURSE IN CHALENGEING SITUATIONS Merged Compressed Merged MergedYuuki Chitose (tai-kun)No ratings yet
- Bemonc - S-Cort - SlidesDocument97 pagesBemonc - S-Cort - SlidesErrol LlanesNo ratings yet
- Unit 3.3 Safe Motherhood Doc (1-5)Document5 pagesUnit 3.3 Safe Motherhood Doc (1-5)mahesh thapaNo ratings yet
- Maternity Chapter 01 Framework For Maternal and Child Health Nursing PDFDocument9 pagesMaternity Chapter 01 Framework For Maternal and Child Health Nursing PDFChskNo ratings yet
- Framework For Maternal and Child Health NursingDocument10 pagesFramework For Maternal and Child Health NursingSHERYL TEMPLANo ratings yet
- SafeDocument18 pagesSafeSaripda JaramillaNo ratings yet
- Philippine Government Policies On Maternal, Newborn and Child Health and NutritionDocument20 pagesPhilippine Government Policies On Maternal, Newborn and Child Health and Nutritioncarlos-tulali-1309100% (34)
- Skilled Birth Attendance-Lessons LearntDocument9 pagesSkilled Birth Attendance-Lessons LearntTriksha GeorgeNo ratings yet
- On MCH and Maternal Health in BangladeshDocument46 pagesOn MCH and Maternal Health in BangladeshTanni ChowdhuryNo ratings yet
- NICU Journal: A Parent's JourneyFrom EverandNICU Journal: A Parent's JourneyNo ratings yet
- M.05 Palliative Care (Dr. Flores) (03-01-21)Document4 pagesM.05 Palliative Care (Dr. Flores) (03-01-21)VanessaNo ratings yet
- M.02 MNCHN (Part 2) (Dr. Hora) (03-04-21)Document4 pagesM.02 MNCHN (Part 2) (Dr. Hora) (03-04-21)VanessaNo ratings yet
- M.03 Respiratory Disorders Part 3 (Dr. Tandoc) (10-26-2020)Document7 pagesM.03 Respiratory Disorders Part 3 (Dr. Tandoc) (10-26-2020)VanessaNo ratings yet
- Saint Louis University School of Medicine Mmxxii: Dr. Hora - 03/04/2021Document9 pagesSaint Louis University School of Medicine Mmxxii: Dr. Hora - 03/04/2021VanessaNo ratings yet
- M.04 IMCI (Part 2) (Dr. Hora) (03-03-21)Document5 pagesM.04 IMCI (Part 2) (Dr. Hora) (03-03-21)VanessaNo ratings yet
- M.03 Respiratory Disorders of Children Part 1 (Dr. Tandoc) (10-26-20)Document7 pagesM.03 Respiratory Disorders of Children Part 1 (Dr. Tandoc) (10-26-20)VanessaNo ratings yet
- Saint Louis University School of Medicine Mmxxii: Dr. Quitiquit - November 11, 2020Document9 pagesSaint Louis University School of Medicine Mmxxii: Dr. Quitiquit - November 11, 2020VanessaNo ratings yet
- M.04 Liver (Part 4) (Dr. Cinio) (10-29-20)Document8 pagesM.04 Liver (Part 4) (Dr. Cinio) (10-29-20)VanessaNo ratings yet
- M.04 MEDICAL ETHICS AND THE CHRISTIAN PHYSICIAN (Dr. Tolentino)Document9 pagesM.04 MEDICAL ETHICS AND THE CHRISTIAN PHYSICIAN (Dr. Tolentino)VanessaNo ratings yet
- Placenta PreviaDocument10 pagesPlacenta PreviaAdriane ComaNo ratings yet
- Sexual, Marital Perceivednihms199025Document16 pagesSexual, Marital Perceivednihms199025annisa habibullohNo ratings yet
- On Family WelfareDocument45 pagesOn Family WelfareSweety Yadav100% (2)
- Tosoh Series 2147Document3 pagesTosoh Series 2147ShahinNo ratings yet
- Vitamin D and PCOSDocument39 pagesVitamin D and PCOSsyafiraNo ratings yet
- Review of Literature Related To Low Birth Weight BabiesDocument4 pagesReview of Literature Related To Low Birth Weight BabiesgwfdurbndNo ratings yet
- GyaneDocument188 pagesGyaneSupekshya ShresthaNo ratings yet
- Case Report Iufd - RashifDocument32 pagesCase Report Iufd - RashifM Nur MuhammadNo ratings yet
- Twin Anemia Polycythemia SyndromesDocument67 pagesTwin Anemia Polycythemia SyndromesBhupendra GuptaNo ratings yet
- Midwifery Exam PracticeDocument12 pagesMidwifery Exam Practicekristel ludangcoNo ratings yet
- Week 12 13122022 015614pmDocument12 pagesWeek 12 13122022 015614pmJehanzaib AminNo ratings yet
- The Beautiful Mother - 1stdraftDocument254 pagesThe Beautiful Mother - 1stdraftMagus PrintNo ratings yet
- Science Module For Grade 10: Guagua National Colleges, Inc. Guagua, PampangaDocument62 pagesScience Module For Grade 10: Guagua National Colleges, Inc. Guagua, PampangaNorman Punla SantosNo ratings yet
- Abortion 150119000246 Conversion Gate02Document121 pagesAbortion 150119000246 Conversion Gate02chetankumarbhumireddyNo ratings yet
- Cow Calf CalendarDocument5 pagesCow Calf CalendarcapsfastNo ratings yet
- Puerperal PyrexiaDocument20 pagesPuerperal Pyrexiaهلا اكرم عقل طميزهNo ratings yet
- Quarter 2 Week 7-MAPEH8Document2 pagesQuarter 2 Week 7-MAPEH8Kimberly Ann Castro VitugNo ratings yet
- Biology Unit 1 Module 3 - Question and Answers 2013 To 2016Document20 pagesBiology Unit 1 Module 3 - Question and Answers 2013 To 2016Darion SinghNo ratings yet
- The Endometrial Factor A Reproductive Precision Medicine ApproachDocument275 pagesThe Endometrial Factor A Reproductive Precision Medicine ApproachErika Rosas100% (2)
- Oxytocin, Dinoprostone, Cefuroxime Drug StudyDocument3 pagesOxytocin, Dinoprostone, Cefuroxime Drug StudyMary Shane MoraldeNo ratings yet
- PubLSIS II Survey Finding Report June 2018Document620 pagesPubLSIS II Survey Finding Report June 2018Mao udangNo ratings yet
- Nutrition Through The Life Cycle 6Th Edition Brown Test Bank Full Chapter PDFDocument43 pagesNutrition Through The Life Cycle 6Th Edition Brown Test Bank Full Chapter PDFnhanselinak9wr16100% (11)
- Breast Care and Breast Feeding For CI, by DR Abera Sept 2021Document57 pagesBreast Care and Breast Feeding For CI, by DR Abera Sept 2021Kerod AbebeNo ratings yet
- Tosoh Bioscience Tosoh Bioscience: CL Aia-Pack ReagentsDocument2 pagesTosoh Bioscience Tosoh Bioscience: CL Aia-Pack ReagentsAleksandar MisicNo ratings yet
- Direct and Indirect SpeechDocument3 pagesDirect and Indirect SpeechImelda DayaNo ratings yet
- SaluEric New An Alluring Imp WPS Office 1Document7 pagesSaluEric New An Alluring Imp WPS Office 1Eric SaludaresNo ratings yet
- English8 Quarter3Document3 pagesEnglish8 Quarter3Knelle Rose TajoNo ratings yet