Professional Documents
Culture Documents
Vincent 1993
Vincent 1993
Uploaded by
Jhuliana CabreraOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vincent 1993
Vincent 1993
Uploaded by
Jhuliana CabreraCopyright:
Available Formats
Epidural Anesthesia for
Postpartum Tubal
Using Epidural C
Pla&d during Labor
Robert D. Vincent, Jr., MD,* Robert W. Reid, MDT
Department of Anesthesia, University of Iowa College of Medicine, Iowa City, IA.
Study Objectives: To evaluate the success of epidural anesthesia for postpartum tubal
ligation using epidural catheters placed during labor and to determine whether patient
characteristics, timing of surgery, or technical factors (‘e.g., length of epidural catheter
inserted into the epidural space) influenced the success of subsequent epidural anesthesia.
Design: Retrospective stud..
Setting: University hospital labor and delivery suite.
Patients: 90 consecutive women scheduledfor postpartum tubal ligation usingepidural
catheters placed during labor.
Interventions: Epidural catheters were reinjected with 1.5% to 2% lidocaine with
epinephrine 5 pglml or 2% to 3% 2-chloroprocaine immediately before surgery.
Measurements and Main Results: 74% of the women received satisfato9 intrqer-
ative anesthesia using in situ epidural catheters. Reinjecting the catheter within 4 hours
of delivery was associated with a greater frequency of successful epidural anesthesia for
tubal ligation (95% vs. 67%; p = 0.029). There was no significant difference between
the two groups in the length of catheter inserted into the epidural space.
Conclusions: Although other factors may influence the timing of postpartum tubal
ligation after delivery, the success of epidural anesthesia for tubal ligation using in
situ epidural catheters is greater if surgery is performed shortly after delivery.
Keywords: Anesthesia, obstetric; anesthetic techniques, epidural; catheter,
epidural; postpartum tubal ligation.
Introduction
An advantage of epidural anesthesia for pain relief during labor in women
who desire sterilization after delivery is that the epidural catheter may be left in
place and reinjected later to provide anesthesia for postpartum tubal ligation.
*AssistantProfessor Unfortunately, we have observed that epidural anesthesia often is unsuccessful
tResident when these in situ catheters are reinjected just before surgery. The purpose
of this study was to evaluate the success of epidural anesthesia for postpartum
Address reprint requests to Dr. Vincent at tubal ligation using epidural catheters placed during labor and to determine
the Department of Anesthesia, University
whether patient characteristics, technical factors (e.g., length of epidural cathe-
of Iowa College of Medicine, Iowa City, IA
ter inserted into the epidural space), or the interval between placement and
52242, USA.
delivery or delivery and surgery influenced the success of subsequent epidural
Received for publication January 11, 1993; anesthesia.
revised manuscript accepted for publication
March 2, 1993. - - -
Materials and Methods
0 1993 Butterworth-Heinemann
The protocol was approved by the University of Iowa Institutional Review
J. Clin. Ant&h. 5:499491, 1993. Board for research involving human subjects. Medical records were reviewed
J. Clin. Anesth., vol. 5, July/August 1993 289
Original Contributions
Table 1. Patient Demographic Data was not significantly different between groups (Table 2).
But the time between delivery and tubal ligation was
Successful Unsuccessful significantly less (P = 0.023) in the successful group than
(n = 64) (n = 23) in the unsuccessful group (Table 2). Also, the chance of
successful epidural anesthesia was greater (p = 0.029) if
Age (yr) 29 28 the catheter was reinjected within 4 hours of delivery
Parity 3 3
(Figure I). Finally, epidural anesthesia for tubal ligation
Weight (kg) 79 * 1 a3 z? 3
was successful on each of ten occasions when attempted
BMI (kg/m2) 29.0 f 0.5 30.2 2 1.2
Height (cm) 165 * 1 165 + 1 before regression of sensory blockade (median level =
Tt,, prior to reinjection).
Note: Mean and median values are given for age and parity, respec- The length of epidural catheter inserted into the epi-
tively. Measured data are expressed as means f SEM. There were dural space was not significantly different between the
no significant differences between the groups. successful and unsuccessful groups (4.1 + 0.1 cm and
BMI = body mass index. 3.9 f 0.2 cm, respectively). The length of epidural cathe-
ter at the skin was recorded at placement and again
before surgery in 11 women. In 2 women, the catheter
for 90 consecutive women scheduled for elective postpar- position was unchanged at the skin. In the remaining 9
tum tubal ligation between January 1989 and September patients, the catheter migrated outward to a more super-
1992 using epidural catheters placed during labor (in ficial position (median length of migration = 2 cm; range
situ catheters). Twenty-gauge, closed-tip, triple-orifice = 1 to 6 cm). Also, 3 epidural catheters were completely
epidural catheters (Burron, Bethlehem, PA) were placed dislodged from the skin between delivery and surgery.
during labor in all parturients. All catheters were secured
to the patient’s back with plastic tape. Immediately before Discussion
surgery, the epidural catheters were incrementally rein-
jetted with 1.5% to 2% lidocaine with epinephrine 5 kg/ Gastric emptying slows during labor.‘** Opioids given for
ml or 2% to 3% 2-chloroprocaine. analgesia during labor also delay gastric emptying.z+s This
Subsequent epidural anesthesia was defined as suc- is of concern in postpartum women for fear that gastro-
cessful [i.e., adequate patient analgesia was achieved with esophageal incompetence places them at greater risk for
epidural local anesthetic alone or in combination with regurgitation of gastric contents.4 Thus, some anesthesi-
intravenous (IV) opioids and/or benzodiazepines] or un- ologists prefer to delay at least 8 hours after delivery
successful (i.e., the epidural catheter became accidentally before anesthetizing women for postpartum tubal liga-
dislodged before surgery; the catheter was reinjected, tion to allow for more complete gastric emptying.5 Al-
but a potent inhalation drug was required to achieve though one would expect that this practice would reduce
adequate intraoperative anesthesia; or spinal anesthesia the risk factors associated with aspiration pneumonitis,
was given for surgery). In several patients, the length of James et al6 found no relationship between the time
epidural catheter visible at the skin recorded at place- interval after delivery and the volume and acidity of
ment and again just before surgery. Epidural catheter stomach contents when measured during tubal ligation.
migration was defined as the difference between these Therefore, our results support the administration of epi-
two measurements. dural anesthesia for postpartum tubal ligation soon after
Statistical analysis of continuous data was by unpaired delivery in the hope that the success of subsequent epi-
t-tests. The Mann-Whitney U test and the chi-square dural anesthesia will be optimized.
test with contingency correction were used to compare We hypothesized that epidural anesthesia for tubal li-
nonparametric data between groups. A value of p < 0.05 gation would be more reliable in women whose epidural
was considered statistically significant. catheters were inserted to a greater depth. We anticipated
that this would be especially true in larger women because
of the tendency to overestimate the length of the catheter
in the epidural space in obese patients.' Although our data
Results
did not support these hypotheses, we did observe that
Successful epidural anesthesia for postpartum tubal liga- many catheters migrated to a more superficial position in
tion was achieved in 64 of 87 women (74%) using epidural the epidural space after the initial placement. For this rea-
catheters placed during labor. We excluded 3 patients son, we always advance the catheter at least 4 cm into the
who had adequate sensory levels of anesthesia docu- epidural space in women who are considering tubal liga-
mented in the chart but were given nitrous oxide in tion after delivery. But we acknowledge that this practice
oxygen via face mask during surgery. (One of these may increase the frequency of unilateral blockade and epi-
women also received IV boluses of thiopental sodium). dural venous cannulation.8.9
There were no significant demographic differences Postpartum tubal ligation is a semiurgent surgical pro-
between the two groups (Table I). However, patients in cedure that should not take priority over the obstetric
the successful group tended to weigh slightly less than and anesthetic care of women in active labor. However,
patients in the unsuccessful group. if staffing requirements and obligations to other patients
The time from epidural catheter placement to delivery permit, one should consider reinjecting in situ epidural
290 1. Clin. Anesth.. vol. 5. lulv/Auaust 1993
Reinjection of epidural catheters for postpartum tubal ligation: Vincent and Reid
Table 4. Success of Subsequent Epidural Anesthesia versus Time Intervals between Epidural Catheter Placement, Delivery, and
Postpartum Tubal Ligation
Successful Unsuccessful
(n = 64) (n = 23) p-value
Epidural catheter placement to delivery (hr) 3.6 t 0.4 2.8 * 0.4 NS
Second stage of labor (min) 42 + 6 40 + 9 NS
Epidural catheter placement to surgery (hr) 14.1 + 1.1 17.6 + 1.4 NS
Delivery to surgery (hr) 10.6 f 1.0 14.8 t 1.4 0.023
Note: Data are means f SEM.
NS = not significant.
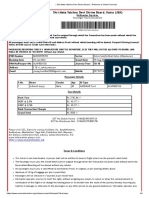
100 ’
80 -
60 -
40 -
20 -
0”
c4 4-8 8-12 >I2
(n=20) (n=12) (n=40) (n-15)
Delivery to surgery interval (h)
Figure 1. Percentage of successful epidural anesthetics for postpartum tubal ligation (PPTL) verszLs time interval between
delivery and surgery. Successful epidural anesthesia was more likely if the catheter was reinjected within 4 hours of delivery
(p = 0.029).
catheters and proceeding with postpartum tubal ligation JW, Moshal MC: Gastric and lower oesophageal sphincter (LOS)
shortly after delivery to improve the probability of suc- pressures in early pregnancy. Br J Anuesth 1981;53:381-4.
cessful epidural anesthesia. 5. Rolbin SH: Anesthesia for postpartum sterilization surgery. In:
Shnider SM, Levinson G, eds. Anesthesiafor Obstetrics. Baltimore:
Williams & Wilkins, 1993:247-58.
6. James CF, Gibbs CP, Banner T: Postpartum perioperative risk
References
of aspiration pneumonia. Anesthesiology 1984;61:756-9.
Davison JS, Davison MC, Hay DM: Gastric emptying time in 7. Webster SG: Migration of epidural catheters [Letter]. Anaesthesiu
late pregnancy and labour. J Obstet Gynoecol Br Communw 1986;41:654.
1970;77:37-41. 8. Shnider SM, Levinson G, Ralston DH: Regional anesthesia for
O’Sullivan GM, Sutton AJ, Thompson SA, Carrie LE, Bull- labor and delivery. In: Shnider SM, Levinson G, eds. Anesthesia
ingham RE: Noninvasive measurement of gastric emptying in for Obstekes. Baltimore: Williams & Wilkins, 1993:135-53.
obstetric patients. Anesth Analg 1987;66:505-11. 9. Cousins MJ, Bromage PR: Epidurai neural blockade. In: Cousins
Holdsworth JD: Relationship between stomach contents and an- MJ, Bridenbaugh PO, eds. Neural Blockade in Clinical Anesthka
algesia in labour. Br J Anuesth 1978;50: 1145-B. and Management of Pain. Philadelphia: J.B. Lippincott,
Brock-Utne JG, Dow TG, Dimopoulos GE, Welman S, Downing 1988:253-360.
J. Clin. Anesth., vol. 5, July/August 1993 491
You might also like
- US Not Useful For Low BMI and Easy Palpable PatientsDocument6 pagesUS Not Useful For Low BMI and Easy Palpable Patientscailin.hicuraNo ratings yet
- US For Epidural. Anesth Analg 2017Document6 pagesUS For Epidural. Anesth Analg 2017tarekabdelkarem927No ratings yet
- 2017 Intercostal Nerve Cryo Vs Thoracic Epidural Cath For Postop Analgesia 26 Cryo PatientsDocument6 pages2017 Intercostal Nerve Cryo Vs Thoracic Epidural Cath For Postop Analgesia 26 Cryo PatientsIevgen DanylchukNo ratings yet
- AshrafDocument5 pagesAshrafJennifer GNo ratings yet
- Graves 2017Document5 pagesGraves 2017hafidisara05No ratings yet
- IndianJPain 2021 35 3 254 334102Document3 pagesIndianJPain 2021 35 3 254 334102manoj majiNo ratings yet
- Continuous Versus Interrupted Sutures For Repair of Episiotomy or Second-DegreeDocument3 pagesContinuous Versus Interrupted Sutures For Repair of Episiotomy or Second-DegreeamilyapraditaNo ratings yet
- Miyazaki 2013Document6 pagesMiyazaki 2013Teja LaksanaNo ratings yet
- US Imaging For The Lumbar Spine in The Tranverse Plane - Correlation Between Est and Actual DepthDocument6 pagesUS Imaging For The Lumbar Spine in The Tranverse Plane - Correlation Between Est and Actual Depthcailin.hicuraNo ratings yet
- Continuous Versus Interrupted Sutures For Repairof Episiotomy or Second Degree Perineal Tearsa Randomised Controlled TriaDocument6 pagesContinuous Versus Interrupted Sutures For Repairof Episiotomy or Second Degree Perineal Tearsa Randomised Controlled TriaamilyapraditaNo ratings yet
- Hum. Reprod.-2003-Kroon-2323-7Document5 pagesHum. Reprod.-2003-Kroon-2323-7Jhony SatriaNo ratings yet
- Anesth Analg 2009 Lee 252 4Document3 pagesAnesth Analg 2009 Lee 252 4Ican DoitNo ratings yet
- Real-Time Ultrasound-Guided Paramedian Epidural Access: Evaluation of A Novel In-Plane TechniqueDocument10 pagesReal-Time Ultrasound-Guided Paramedian Epidural Access: Evaluation of A Novel In-Plane TechniqueANGELICANo ratings yet
- Anestesi Jurnal 2Document11 pagesAnestesi Jurnal 2dewi rahmanNo ratings yet
- Initial Experience With Application of Single Layer Modified Kugel Mesh For Inguinal Hernia Repair: Case Series of 72 Consecutive PatientsDocument6 pagesInitial Experience With Application of Single Layer Modified Kugel Mesh For Inguinal Hernia Repair: Case Series of 72 Consecutive Patientsnur hasnahNo ratings yet
- Avoidance of Wrong-Level Thoracic Spine Surgery: Intraoperative Localization With Preoperative PercutaneousDocument5 pagesAvoidance of Wrong-Level Thoracic Spine Surgery: Intraoperative Localization With Preoperative PercutaneousWinnie LiNo ratings yet
- CombinedDocument3 pagesCombinedSolape Akin-WilliamsNo ratings yet
- PII0028224394900779Document5 pagesPII0028224394900779AroelNo ratings yet
- Clinical Study: The Comparison of Lichtenstein Procedure With and Without Mesh-Fixation For Inguinal Hernia RepairDocument5 pagesClinical Study: The Comparison of Lichtenstein Procedure With and Without Mesh-Fixation For Inguinal Hernia RepairFikri AlfarisyiNo ratings yet
- A Comparative Study Between Erector Spinae Plane Block With General Anesthesia Versus Conventional Intravenous Analgesics With General Anesthesia inDocument8 pagesA Comparative Study Between Erector Spinae Plane Block With General Anesthesia Versus Conventional Intravenous Analgesics With General Anesthesia inrafiaNo ratings yet
- Bloqueo Pec 2 MamaDocument9 pagesBloqueo Pec 2 Mamapalomisgarcia1995No ratings yet
- TAP Vs QL CesareanDocument7 pagesTAP Vs QL CesareanEmmanuel FortalezaNo ratings yet
- The Optimal Distance That A Multiorifice Epidural.16Document4 pagesThe Optimal Distance That A Multiorifice Epidural.16Mahavir GemavatNo ratings yet
- Novel Technique For Safe Primary Trocar InsertionDocument5 pagesNovel Technique For Safe Primary Trocar InsertionPrameita Rahmawati MITNo ratings yet
- TAP Paper PublishedDocument8 pagesTAP Paper PublishedMotaz AbusabaaNo ratings yet
- Initial Experience Using Incisional Anesthetic Catheter in Abdominal Wall Ambulatory SurgeryDocument6 pagesInitial Experience Using Incisional Anesthetic Catheter in Abdominal Wall Ambulatory SurgeryilhamNo ratings yet
- Single-Knot Versus Multiple-Knot Technique of Perineal Repair - A Randomised Controlled TrialDocument8 pagesSingle-Knot Versus Multiple-Knot Technique of Perineal Repair - A Randomised Controlled TrialDR RISKA WAHYUNo ratings yet
- IndianJAnaesth6311924-2183535 060355Document8 pagesIndianJAnaesth6311924-2183535 060355Abhijeet ThakurNo ratings yet
- Ease of Lumbar Epidural Catheter Insertion With.11Document5 pagesEase of Lumbar Epidural Catheter Insertion With.11jagadish aNo ratings yet
- Evidence Based Nursing General QuestionDocument3 pagesEvidence Based Nursing General QuestionLeo FrivaldoNo ratings yet
- Touhy y CateterDocument8 pagesTouhy y CateterhumildementeanestesiosNo ratings yet
- The Modified Misgav-Ladach Versus The Pfannenstiel-Kerr Technique For Cesarean Section A Randomized Trial PDFDocument6 pagesThe Modified Misgav-Ladach Versus The Pfannenstiel-Kerr Technique For Cesarean Section A Randomized Trial PDFAntonio TovarNo ratings yet
- Jms 50 061 Chandrashekar OutcomeDocument6 pagesJms 50 061 Chandrashekar OutcomeAripinSyarifudinNo ratings yet
- Modified Prepuce Unfurling For Buried Penis: A Report of 12 Years of ExperienceDocument5 pagesModified Prepuce Unfurling For Buried Penis: A Report of 12 Years of ExperienceMuhammad NurzakkyNo ratings yet
- Refarat DHDocument5 pagesRefarat DHFahmil AgungNo ratings yet
- 1 SMDocument4 pages1 SMSyifarNo ratings yet
- Efficay TAP Block PDFDocument5 pagesEfficay TAP Block PDFMarius PapuricaNo ratings yet
- Labor Epidural Analgesia With Severe ThrombocytopeniaDocument2 pagesLabor Epidural Analgesia With Severe Thrombocytopeniasand52525No ratings yet
- Transversus Abdominis Plane Block For Laparoscopic SurgeryDocument2 pagesTransversus Abdominis Plane Block For Laparoscopic SurgeryFitri Kasmita SariNo ratings yet
- TAP BlockDocument5 pagesTAP BlockclaucardemilNo ratings yet
- Surgically Placed Rectus Sheath Catheters For Post-Laparotomy AnalgesiaDocument6 pagesSurgically Placed Rectus Sheath Catheters For Post-Laparotomy AnalgesiaKarthikNo ratings yet
- Al Sadek2014Document7 pagesAl Sadek2014AYŞE GÜLŞAH ATASEVERNo ratings yet
- The Erector Spinae Plane Block For Effective.9Document4 pagesThe Erector Spinae Plane Block For Effective.9Rully ZenNo ratings yet
- Role of Wound Drains VS Abdominal Binder and Percutaneous Aspiration After Open Repair of Ventral Hernia Using Polyprolene MeshDocument12 pagesRole of Wound Drains VS Abdominal Binder and Percutaneous Aspiration After Open Repair of Ventral Hernia Using Polyprolene MeshIJAR JOURNALNo ratings yet
- Right Open Nephrectomy Under Combined Spinal and Peridural Operative Anesthesia and Analgesia (CSE) : A New Anesthetic Approach in Abdominal SurgeryDocument2 pagesRight Open Nephrectomy Under Combined Spinal and Peridural Operative Anesthesia and Analgesia (CSE) : A New Anesthetic Approach in Abdominal SurgeryPablo Segales BautistaNo ratings yet
- Appendicitis MattiotiDocument6 pagesAppendicitis MattiotiMedardo ApoloNo ratings yet
- Combined Spinal Epidural Anesthesia and Analgesia: March 2012Document21 pagesCombined Spinal Epidural Anesthesia and Analgesia: March 2012Elaine LaizaNo ratings yet
- Marzouk S.BDocument4 pagesMarzouk S.BVan DaoNo ratings yet
- A Retrospective Comparison of Spinal and General Anesthesia For Vaginal Hysterectomy: A Time AnalysisDocument3 pagesA Retrospective Comparison of Spinal and General Anesthesia For Vaginal Hysterectomy: A Time AnalysisWillie HicksNo ratings yet
- JOurnal Uro 2Document6 pagesJOurnal Uro 2Gladys AilingNo ratings yet
- Ultrasound Evaluation of The Uterine Scar After.13Document6 pagesUltrasound Evaluation of The Uterine Scar After.13Jessy MacNo ratings yet
- PBC ClassifiDocument5 pagesPBC ClassifiParvathy R NairNo ratings yet
- Wild-Regional Techniques For Thoracic Wall Surgery-2017-Current Anesthesiology ReportsDocument8 pagesWild-Regional Techniques For Thoracic Wall Surgery-2017-Current Anesthesiology Reportsmouxritsa_83No ratings yet
- Lidocaina en Tubo EndotraquealDocument4 pagesLidocaina en Tubo EndotraquealKane HopkinsNo ratings yet
- Pectus Escavatum NussDocument7 pagesPectus Escavatum NussCristi OgaruNo ratings yet
- Point-Of-Care Ultrasonography-Assisted Nasogastric Tube Placement in The Emergency Department: A Randomized Controlled TrialDocument6 pagesPoint-Of-Care Ultrasonography-Assisted Nasogastric Tube Placement in The Emergency Department: A Randomized Controlled TrialKhanh Ha NguyenNo ratings yet
- Ultrasound-Guided Continuous Erector Spinae Plane Block in Open Nephrectomy For Renal MalignancyDocument8 pagesUltrasound-Guided Continuous Erector Spinae Plane Block in Open Nephrectomy For Renal Malignancyindex PubNo ratings yet
- Jo (2003)Document5 pagesJo (2003)Елена КарпинскаяNo ratings yet
- To Evaluate The Efficacy of Ultrasonography Guided Pectoral Nerve Block For Postoperative Analgesia in Breast SurgeriesDocument4 pagesTo Evaluate The Efficacy of Ultrasonography Guided Pectoral Nerve Block For Postoperative Analgesia in Breast SurgeriesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Practice Modification For Pandemics: A Model For Surge Planning in ObstetricsDocument15 pagesPractice Modification For Pandemics: A Model For Surge Planning in ObstetricsJhuliana CabreraNo ratings yet
- Clinical Implications of Universal Severe Acute Respiratory Syndrome Coronavirus 2 (Sars-Cov-2) Testing in PregnancyDocument3 pagesClinical Implications of Universal Severe Acute Respiratory Syndrome Coronavirus 2 (Sars-Cov-2) Testing in PregnancyJhuliana CabreraNo ratings yet
- Articulo 1 PDFDocument8 pagesArticulo 1 PDFJhuliana CabreraNo ratings yet
- Esterilización de La MujerDocument8 pagesEsterilización de La MujerJhuliana CabreraNo ratings yet
- Ust HtaDocument5 pagesUst HtaSteven SantosNo ratings yet
- Security Guard Training & OSHA Training NY Guardian Group ServicesDocument1 pageSecurity Guard Training & OSHA Training NY Guardian Group ServicesLochard BaptisteNo ratings yet
- MR J, Close Fraktur 1,3 Medial Os Femur DextraDocument9 pagesMR J, Close Fraktur 1,3 Medial Os Femur DextraMuhammad SafaatNo ratings yet
- 3 2 1 Code It 6th Edition Green Solutions Manual DOWNLOAD YOUR FILES DownloadDocument131 pages3 2 1 Code It 6th Edition Green Solutions Manual DOWNLOAD YOUR FILES DownloadelizabethNo ratings yet
- Karthik ResumeDocument3 pagesKarthik Resumeshagy05No ratings yet
- All India Test Series: Concept Recapitulation Test - IDocument12 pagesAll India Test Series: Concept Recapitulation Test - IShreya DesaiNo ratings yet
- C9 ICT Full BookDocument122 pagesC9 ICT Full BookTajtiné Bondár KatalinNo ratings yet
- Experimental Investigation On Solar Absorption Refrigeration System in Malaysia PDFDocument5 pagesExperimental Investigation On Solar Absorption Refrigeration System in Malaysia PDFRana Abdul RehmanNo ratings yet
- Ma Galācarana Prayers: Sung During Shri Ram KathaDocument22 pagesMa Galācarana Prayers: Sung During Shri Ram Kathaashwin goswamiNo ratings yet
- Centre Province Relations Pakistan 1973Document27 pagesCentre Province Relations Pakistan 1973Ehtasham KhanNo ratings yet
- 04 Mata Heritage ConservationDocument10 pages04 Mata Heritage ConservationLannie MaiquezNo ratings yet
- Spare Parts Catalog: 6 WG 200 (555/5) Material Number: 4644.026.333 Current Date: 27.02.2020Document74 pagesSpare Parts Catalog: 6 WG 200 (555/5) Material Number: 4644.026.333 Current Date: 27.02.2020GeorgiNo ratings yet
- Iran (Persian) Architecture & Folk Arts: Shan Jasper O. TorresDocument24 pagesIran (Persian) Architecture & Folk Arts: Shan Jasper O. TorresGlenda DenosoNo ratings yet
- The Vaccine Adverse Event Reporting System (VAERS)Document356 pagesThe Vaccine Adverse Event Reporting System (VAERS)Josh SingerNo ratings yet
- How Long A Trip Is It From Here To Our Cairo Office?Document5 pagesHow Long A Trip Is It From Here To Our Cairo Office?Luyện TrầnNo ratings yet
- LCD TV Service Manual: Konka Group Co, LTDDocument18 pagesLCD TV Service Manual: Konka Group Co, LTDOliver Arenas Jones FENo ratings yet
- Form Euro.326 Rev.2 - Echo Preventive MaintenanceDocument6 pagesForm Euro.326 Rev.2 - Echo Preventive MaintenancesanazNo ratings yet
- Fronius Datamanager 2.0Document88 pagesFronius Datamanager 2.0JohnNo ratings yet
- Educational Marketing Strategies On The Market of Higher Education ServicesDocument11 pagesEducational Marketing Strategies On The Market of Higher Education ServicesGlobal Research and Development ServicesNo ratings yet
- Shri Mata Vaishno Devi Shrine Board - Welcome To Online ServicesDocument4 pagesShri Mata Vaishno Devi Shrine Board - Welcome To Online Servicesphool baghNo ratings yet
- NBD SyllabusDocument2 pagesNBD Syllabusbibby.higginsNo ratings yet
- Most Expensive Watch Brands 2024Document5 pagesMost Expensive Watch Brands 2024norahughes162No ratings yet
- Lembar Permintaan Obat Unit UgdDocument3 pagesLembar Permintaan Obat Unit Ugdpuskesmas anyarNo ratings yet
- Noah ArkDocument9 pagesNoah ArkbanuNo ratings yet
- SSR 2012-13Document146 pagesSSR 2012-13Madhu Sayari100% (1)
- ISO 11126-1 1998R Surface PrepDocument12 pagesISO 11126-1 1998R Surface PrepRejo V. MathewNo ratings yet
- Samsung Ue32es5500 Ue40es5500 Ue46es5500 Ue32eh5300 Ue40eh5300 Ue46eh5300 Ue26eh4500 Ue22es5400 TrainingDocument138 pagesSamsung Ue32es5500 Ue40es5500 Ue46es5500 Ue32eh5300 Ue40eh5300 Ue46eh5300 Ue26eh4500 Ue22es5400 TrainingytrisNo ratings yet
- The History of Computers: Done by - Anandhu Raj, Albin Raphy, Anirudh C. VinayanDocument42 pagesThe History of Computers: Done by - Anandhu Raj, Albin Raphy, Anirudh C. Vinayanarjun rajNo ratings yet
- TSX Cusb485Document2 pagesTSX Cusb485AurellioNo ratings yet
- One Week Online FDP, 21-27 March 2021 - REVISEDDocument9 pagesOne Week Online FDP, 21-27 March 2021 - REVISEDKanhaNo ratings yet