Professional Documents
Culture Documents
Hypovolemic Shock - StatPearls - NCBI Bookshelf
Hypovolemic Shock - StatPearls - NCBI Bookshelf
Uploaded by
Roselyn VelascoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypovolemic Shock - StatPearls - NCBI Bookshelf
Hypovolemic Shock - StatPearls - NCBI Bookshelf
Uploaded by
Roselyn VelascoCopyright:
Available Formats
Books ?
Hypovolemic Shock
Taghavi S, Askari R.
Publication Details
Introduction
Patients with hypovolemic shock have severe
hypovolemia with decreased peripheral perfusion.
If left untreated, these patients can develop
ischemic injury of vital organs, leading to multi-
system organ failure. The first factor to be
considered is whether the hypovolemic shock has
resulted from hemorrhage or fluid losses, as this
will dictate treatment. When etiology of
hypovolemic shock has been determined,
replacement of blood or fluid loss should be
carried out as soon as possible to minimize tissue
ischemia. Factors to consider when replacing
fluid loss include the rate of fluid replacement
and type of fluid to be used. [1]
Etiology
The annual incidence of shock of any etiology is
0.3 to 0.7 per 1000, with hemorrhagic shock
being most common in the intensive care unit.
Hypovolemic shock is the most common type of
shock in children, most commonly due to
diarrheal illness in the developing world.
Hypovolemic shock occurs as a result of either
blood loss or extracellular fluid loss.
Hemorrhagic shock is hypovolemic shock from
blood loss. Traumatic injury is by far the most
common cause of hemorrhagic shock. Other
causes of hemorrhagic shock include
gastrointestinal (GI) bleed, bleed from an ectopic
pregnancy, bleeding from surgical intervention, or
vaginal bleeding.
Hypovolemic shock as a result of extracellular
fluid loss can be of the following etiologies:
Gastrointestinal Losses
GI losses can occur via many different etiologies.
The gastrointestinal tract usually secretes between
3 to 6 liters of fluid per day. However, most of
this fluid is reabsorbed as only 100 to 200 mL are
lost in the stool. Volume depletion occurs when
the fluid ordinarily secreted by the GI tract cannot
be reabsorbed. This occurs when there is
retractable vomiting, diarrhea, or external
drainage via stoma or fistulas.
Renal Losses
Renal losses of salt and fluid can lead to
hypovolemic shock. The kidneys usually excrete
sodium and water in a manner that matches
intake. Diuretic therapy and osmotic diuresis
from hyperglycemia can lead to excessive renal
sodium and volume loss. In addition, there are
several tubular and interstitial diseases beyond the
scope of this article that cause severe salt-wasting
nephropathy.
Skin Losses
Fluid loss also can occur from the skin. In a hot
and dry climate, skin fluid losses can be as high
as 1 to 2 liters/hour. Patients with a skin barrier
interrupted by burns or other skin lesions also can
experience large fluid losses that lead to
hypovolemic shock.
Third-Space Sequestration
Sequestration of fluid into a third-space also can
lead to volume loss and hypovolemic shock.
Third-spacing of fluid can occur in intestinal
obstruction, pancreatitis, obstruction of a major
venous system, or any other pathological
condition that results in a massive inflammatory
response. [1]
Epidemiology
While the incidence of hypovolemic shock from
extracellular fluid loss is difficult to quantify, it is
known that hemorrhagic shock is most commonly
due to trauma. In one study, 62.2% of massive
transfusions at a level 1 trauma center were due to
traumatic injury. In this study, 75% of blood
products used were related to traumatic injury.
Elderly patients are more likely to experience
hypovolemic shock due to fluid losses as they
have a less physiologic reserve.[1]
Pathophysiology
Hypovolemic shock results from depletion of
intravascular volume, whether by extracellular
fluid loss or blood loss. The body compensates
with increased sympathetic tone resulting in
increased heart rate, increased cardiac
contractility, and peripheral vasoconstriction. The
first changes in vital signs seen in hypovolemic
shock include an increase in diastolic blood
pressure with narrowed pulse pressure. As
volume status continues to decrease, systolic
blood pressure drops. As a result, oxygen delivery
to vital organs is unable to meet oxygen demand.
Cells switch from aerobic metabolism to
anaerobic metabolism, resulting in lactic acidosis.
As sympathetic drive increases, blood flow is
diverted from other organs to preserve blood flow
to the heart and brain. This propagates tissue
ischemia and worsens lactic acidosis. If not
corrected, there will be worsening hemodynamic
compromise and, eventually, death. [2]
History and Physical
History and physical can often make the
diagnosis of hypovolemic shock. For patients
with hemorrhagic shock, a history of trauma or
recent surgery is present. For hypovolemic shock
due to fluid losses, history and physical should
attempt to identify possible GI, renal, skin, or
third-spacing as a cause of extracellular fluid loss.
Symptoms of hypovolemic shock can be related
to volume depletion, electrolyte imbalances, or
acid-base disorders that accompany hypovolemic
shock.
Patients with volume depletion may complain of
thirst, muscle cramps, and/or orthostatic
hypotension. Severe hypovolemic shock can
result in mesenteric and coronary ischemia that
can cause abdominal or chest pain. Agitation,
lethargy, or confusion may result from brain
malperfusion.
Although relatively nonsensitive and nonspecific,
physical exam can be helpful in determining the
presence of hypovolemic shock. Physical findings
suggestive of volume depletion include dry
mucous membranes, decreased skin turgor, and
low jugular venous distention. Tachycardia and
hypotension can be seen along with decreased
urinary output. Patients in shock can appear cold,
clammy, and cyanotic.[3]
Evaluation
Various laboratory values can be abnormal in
hypovolemic shock. Patients can have increased
BUN and serum creatinine as a result of prerenal
kidney failure. Hypernatremia or hyponatremia
can result, as can hyperkalemia or hypokalemia.
Lactic acidosis can result from increased
anaerobic metabolism. However, the effect of
acid-base balance can be variable as patients with
large GI losses can become alkalotic. In cases of
hemorrhagic shock, hematocrit and hemoglobin
can be severely decreased. However, with a
reduction in plasma volume, hematocrit and
hemoglobin can be increased due to
hemoconcentration.
Low urinary sodium is commonly found in
hypovolemic patients as the kidneys attempt to
conserve sodium and water to expand the
extracellular volume. However, sodium urine can
be low in a euvolemic patient with heart failure,
cirrhosis, or nephrotic syndrome. A fractional
excretion of sodium under 1% is also suggestive
of volume depletion. Elevated urine osmolality
can also suggest hypovolemia. However, this
number also can be elevated in the setting of
impaired concentrating ability by the kidneys.
Central venous pressure (CVP) is often used to
assess volume status. However, its usefulness in
determining volume responsiveness has recently
come into question. Ventilator settings, chest wall
compliance, and right-sided heart failure can
compromise CVPs accuracy as a measure of
volume status. Measurements of pulse pressure
variation via various commercial devices has also
been postulated as a measure of volume
responsiveness. However, pulse pressure
variation as a measure of fluid responsiveness is
only valid in patients without spontaneous breaths
or arrhythmias. The accuracy of pulse pressure
variation also can be compromised in right heart
failure, decreased lung or chest wall compliance,
and high respiratory rates.
Similar to examining pulse pressure variation,
measuring respiratory variation in inferior vena
cava diameter as a measure of volume
responsiveness has only been validated in patients
without spontaneous breaths or arrhythmias.
Measuring the effect of passive leg raises on
cardiac contractility by echo appears to be the
most accurate measurement of volume
responsiveness, although it is also subject to
limitations. [3][[4]
Treatment / Management
For patients in hemorrhagic shock, early use of
blood products over crystalloid resuscitation
results in better outcomes. Balanced transfusion
using 1:1:1 or 1:1:2 of plasma to platelets to
packed red blood cells results in better
hemostasis. Anti-fibrinolytic administration to
patients with severe bleed within 3 hours of
traumatic injury appears to decrease death from
major bleed as shown in the CRASH-2 trial.
Research on oxygen-carrying substitutes as an
alternative to packed red blood cells is ongoing,
although no blood substitutes have been approved
for use in the United States.
For patients in hypovolemic shock due to fluid
losses, the exact fluid deficit cannot be
determined. Therefore, it is prudent to start with 2
liters of isotonic crystalloid solution infused
rapidly as an attempt to quickly restore tissue
perfusion. Fluid repletion can be monitored by
measuring blood pressure, urine output, mental
status, and peripheral edema. Multiple modalities
exist for measuring fluid responsiveness such as
ultrasound, central venous pressure monitoring,
and pulse pressure fluctuation as described above.
In general, for hypovolemic shock, vasopressors
should not be used because they can worsen
tissue perfusion.
Crystalloid fluid resuscitation is preferred over
colloid solutions for severe volume depletion not
due to bleeding. The type of crystalloid used to
resuscitate the patient can be individualized based
on the patients’ chemistries, estimated volume of
resuscitation, acid/base status, and physician or
institutional preferences. Isotonic saline is
hyperchloremic relative to blood plasma, and
resuscitation with large amounts can lead to a
hyperchloremic metabolic acidosis. Several other
isotonic fluids with lower chloride concentrations
exist, such as lactated Ringer's solution or
PlasmaLyte. These solutions are often referred to
as buffered or balanced crystalloids. Some
evidence suggests that patients who need large
volume resuscitation may have a less renal injury
with restrictive chloride strategies and use of
balanced crystalloids. Crystalloid solutions are
equally as effective and much less expensive than
colloid. Commonly used colloid solutions include
those containing albumin or hyperoncotic starch.
Studies examining albumin solutions for
resuscitation have not shown improved outcomes,
while other studies have shown resuscitation with
hyperoncotic starch leads to increased mortality
and renal failure.[5][6][7][8][9]
Di!erential Diagnosis
Femoral shaft fractures in emergency
medicine
Gastrointestinal bleeding
Hemorrhagic shock in emergency medicine
Iron toxicity
Pelvic fracture in emergency medicine
Pregnancy trauma
Peptic ulcer disease
Placental previa imaging
Thoracic aneurysm
Pearls and Other Issues
In patients with hypovolemic shock due to
extracellular fluid loss, the etiology of fluid
loss must be identified and treated.
Monitoring electrolytes and acid/base status
in patients in hypovolemic shock is of
utmost importance.
Trauma is the leading cause of hemorrhagic
shock.
The hemorrhagic shock should be treated
with balanced transfusion of packed red
blood cells, plasma, and platelets.
Determining whether patients will be
responsive to volume resuscitation should
not rely on a single modality such as
ultrasound, pulse pressure wave variation,
passive leg raises, or central venous
pressure. The decision for fluid
administration should be based on the entire
clinical presentation, laboratory values, and
the aforementioned modalities.
For patients with hypovolemic shock due to
fluid loss, the crystalloid solution is
preferred over colloid.
Enhancing Healthcare Team
Outcomes
The management of hypovolemic shock requires
an interprofessional team including ICU nurses.
For patients with hypovolemic shock due to fluid
loss, the crystalloid solution is preferred over
colloid.These patients need monitoring of their
fluid input and output and should be in an ICU
setting. The outcomes depend on the cause of
shock, the patient age, comorbidities and presence
of renal failure.
Continuing Education / Review
Questions
Access free multiple choice questions on
this topic.
Earn continuing education credits
(CME/CE) on this topic.
Comment on this article.
References
1. Hooper N, Armstrong TJ. StatPearls
[Internet]. StatPearls Publishing; Treasure
Island (FL): Jul 13, 2020. Hemorrhagic
Shock. [PubMed]
2. Gayet-Ageron A, Prieto-Merino D, Ker K,
Shakur H, Ageron FX, Roberts I.,
Antifibrinolytic Trials Collaboration. Effect
of treatment delay on the effectiveness and
safety of antifibrinolytics in acute severe
haemorrhage: a meta-analysis of individual
patient-level data from 40 138 bleeding
patients. Lancet. 2018 Jan
13;391(10116):125-132. [PMC free article]
[PubMed]
3. Annane D, Siami S, Jaber S, Martin C,
Elatrous S, Declère AD, Preiser JC, Outin H,
Troché G, Charpentier C, Trouillet JL,
Kimmoun A, Forceville X, Darmon M, Lesur
O, Reignier J, Régnier J, Abroug F, Berger P,
Clec'h C, Cle'h C, Cousson J, Thibault L,
Chevret S., CRISTAL Investigators. Effects
of fluid resuscitation with colloids vs
crystalloids on mortality in critically ill
patients presenting with hypovolemic shock:
the CRISTAL randomized trial. JAMA. 2013
Nov 06;310(17):1809-17. [PubMed]
4. Bentzer P, Griesdale DE, Boyd J, MacLean K,
Sirounis D, Ayas NT. Will This
Hemodynamically Unstable Patient Respond
to a Bolus of Intravenous Fluids? JAMA.
2016 Sep 27;316(12):1298-309. [PubMed]
5. Zarychanski R, Abou-Setta AM, Turgeon AF,
Houston BL, McIntyre L, Marshall JC,
Fergusson DA. Association of hydroxyethyl
starch administration with mortality and acute
kidney injury in critically ill patients requiring
volume resuscitation: a systematic review and
meta-analysis. JAMA. 2013 Feb
20;309(7):678-88. [PubMed]
6. Yunos NM, Bellomo R, Glassford N, Sutcliffe
H, Lam Q, Bailey M. Chloride-liberal vs.
chloride-restrictive intravenous fluid
administration and acute kidney injury: an
extended analysis. Intensive Care Med. 2015
Feb;41(2):257-64. [PubMed]
7. Self WH, Semler MW, Wanderer JP, Wang L,
Byrne DW, Collins SP, Slovis CM, Lindsell
CJ, Ehrenfeld JM, Siew ED, Shaw AD,
Bernard GR, Rice TW., SALT-ED
Investigators. Balanced Crystalloids versus
Saline in Noncritically Ill Adults. N Engl J
Med. 2018 Mar 01;378(9):819-828. [PMC
free article] [PubMed]
8. Better OS. Impaired fluid and electrolyte
balance in hot climates. Kidney Int Suppl.
1987 Aug;21:S97-101. [PubMed]
9. Miller TR, Anderson RJ, Linas SL, Henrich
WL, Berns AS, Gabow PA, Schrier RW.
Urinary diagnostic indices in acute renal
failure: a prospective study. Ann Intern Med.
1978 Jul;89(1):47-50. [PubMed]
Publication Details
Author Information
Authors
Sharven Taghavi1; Reza Askari2.
A"liations
1 Tulane University School of Medicine
2 Harvard Medical School
Publication History
Last Update: July 20, 2020.
Copyright
Copyright © 2020, StatPearls Publishing LLC.
This book is distributed under the terms of the Creative
Commons Attribution 4.0 International License
(http://creativecommons.org/licenses/by/4.0/), which
permits use, duplication, adaptation, distribution, and
reproduction in any medium or format, as long as you
give appropriate credit to the original author(s) and the
source, a link is provided to the Creative Commons
license, and any changes made are indicated.
Publisher
StatPearls Publishing, Treasure Island (FL)
NLM Citation
Taghavi S, Askari R. Hypovolemic Shock. [Updated 2020
Jul 20]. In: StatPearls [Internet]. Treasure Island (FL):
StatPearls Publishing; 2020 Jan-.
You might also like
- Muscular SystemDocument26 pagesMuscular Systemlubnab75% (4)
- Concept Map - HyponatremiaDocument9 pagesConcept Map - HyponatremiaElleNo ratings yet
- Gen. Biology 1: Quarter 1 - Module 1: Structure and Function of Animal TissueDocument27 pagesGen. Biology 1: Quarter 1 - Module 1: Structure and Function of Animal TissueMarianne Gonzales60% (5)
- Dapus 3Document7 pagesDapus 3Dhea NadhilaNo ratings yet
- Hypovolemic Shock 09Document58 pagesHypovolemic Shock 09Joanne Bernadette Aguilar100% (2)
- Hemorrhagic ShockDocument2 pagesHemorrhagic ShockPharhana PuterieNo ratings yet
- Third SpacingDocument4 pagesThird SpacingJelly BeanNo ratings yet
- Hemorrhagic ShockDocument11 pagesHemorrhagic ShockmuamervukNo ratings yet
- Pediatrics in Review 2013 HiponatremiaDocument5 pagesPediatrics in Review 2013 HiponatremiaCarlos Elio Polo Vargas100% (1)
- Electrolyte DisordersDocument10 pagesElectrolyte DisordersSlavicaNo ratings yet
- Medical Surgical Fluid and Electrolytes FVD FVEDocument7 pagesMedical Surgical Fluid and Electrolytes FVD FVEMichaelaKatrinaTrinidadNo ratings yet
- Fluid Deficit RevisedDocument6 pagesFluid Deficit RevisedShaira SariaNo ratings yet
- Fluid and Electrolyte Disorders: Dr. Chandra Kant Pandey Dr. R. B. SinghDocument8 pagesFluid and Electrolyte Disorders: Dr. Chandra Kant Pandey Dr. R. B. SinghMok Chu ZhenNo ratings yet
- Disorders of SodiumDocument13 pagesDisorders of SodiumteranrobleswaltergabrielNo ratings yet
- Kidney Failure Kelompok 3Document14 pagesKidney Failure Kelompok 3Devi FitrianaNo ratings yet
- Hipo e Hipernatremia en PediatriaDocument10 pagesHipo e Hipernatremia en PediatriaPao GonzalezNo ratings yet
- Pa Tho Physiology of Liver Cirrhosis - MercyDocument7 pagesPa Tho Physiology of Liver Cirrhosis - Mercymersenie_TheovercomerNo ratings yet
- Desqulibrio de LíqudosDocument5 pagesDesqulibrio de LíqudosadrianachavezhdzNo ratings yet
- Cardiovascular System Diseases Part 2Document9 pagesCardiovascular System Diseases Part 2Prince Rener Velasco PeraNo ratings yet
- Cardiovascular System Diseases Part 2Document9 pagesCardiovascular System Diseases Part 2Prince Rener Velasco PeraNo ratings yet
- Emergency Fluid Therapy in Companion Animals - PPitneyDocument9 pagesEmergency Fluid Therapy in Companion Animals - PPitneyUmesh GopalanNo ratings yet
- Now Get From Our Live Expert On Rea Ltime Basis Join Us and Get Homework HelpDocument24 pagesNow Get From Our Live Expert On Rea Ltime Basis Join Us and Get Homework HelplicservernoidaNo ratings yet
- Veterinary Clinics: Managing Fluid and Electrolyte Disorders in Renal FailureDocument21 pagesVeterinary Clinics: Managing Fluid and Electrolyte Disorders in Renal Failurecaesar nugrohoNo ratings yet
- Extracellular Fluid Volum DeficitDocument22 pagesExtracellular Fluid Volum DeficitKhushi Devgan SharmaNo ratings yet
- Fluids Electrolytes Group 1 CompilationDocument41 pagesFluids Electrolytes Group 1 CompilationShaira SariaNo ratings yet
- Water Excess SyndromeDocument5 pagesWater Excess SyndromeQueenie Velasquez Reinoso JacksonNo ratings yet
- Hypovolemic ShockDocument10 pagesHypovolemic ShockUsran Ali BubinNo ratings yet
- NCP CKD From CaneDocument74 pagesNCP CKD From CaneSheela Khrystyn LeeNo ratings yet
- A Systematic Approach To The Hyponatremic Patient: Iva Ratkoviê-Gusiê, Petar Kes And Vanja Baπiê-KesDocument10 pagesA Systematic Approach To The Hyponatremic Patient: Iva Ratkoviê-Gusiê, Petar Kes And Vanja Baπiê-KesTio Prima SNo ratings yet
- Management of HemorrhageDocument11 pagesManagement of HemorrhageClara VerlinaNo ratings yet
- 3 Fluid and ElectrolyteDocument7 pages3 Fluid and ElectrolyteStephen HDNo ratings yet
- Hemorrhagic ShockDocument5 pagesHemorrhagic ShockGhina RahmadiantiNo ratings yet
- Pathophysiology of Hypovolemic ShockDocument5 pagesPathophysiology of Hypovolemic ShockIan Rama100% (1)
- Care Plan NRS 108Document10 pagesCare Plan NRS 108Don Prem LegaspiNo ratings yet
- Hipernatremia BDocument13 pagesHipernatremia BAchmad DainuriNo ratings yet
- The Hyponatremic Patient: A Systematic Approach To Laboratory DiagnosisDocument7 pagesThe Hyponatremic Patient: A Systematic Approach To Laboratory DiagnosisJuen LohNo ratings yet
- Fispatologjia e CreegullimeveDocument16 pagesFispatologjia e CreegullimeveArmar MendoNo ratings yet
- Fluid Therapy FinalDocument3 pagesFluid Therapy Finallaureeate100% (1)
- Management of Hyponatremia in Clinical Hepatology Practice: Liver (B Bacon, Section Editor)Document5 pagesManagement of Hyponatremia in Clinical Hepatology Practice: Liver (B Bacon, Section Editor)deltanueveNo ratings yet
- Lect 02Document5 pagesLect 02Iptysam Al-AlawiNo ratings yet
- Identifying Types of Shock in Dogs & Cats - Site - NameDocument8 pagesIdentifying Types of Shock in Dogs & Cats - Site - Namelara yaseenNo ratings yet
- Medscape Hypovolemic ShockDocument14 pagesMedscape Hypovolemic ShockSarah Ovinitha100% (1)
- StudyDocument23 pagesStudyK'winetoy Ra'llavNo ratings yet
- Pathophysiology and Etiology of Edema - IDocument9 pagesPathophysiology and Etiology of Edema - IBrandy MaddoxNo ratings yet
- M5 - Electrolyte AbnormalitiesDocument44 pagesM5 - Electrolyte AbnormalitiesVishal KumarNo ratings yet
- Hyponatremia and Hypernatremia in The ElderlyDocument15 pagesHyponatremia and Hypernatremia in The ElderlyStacey WoodsNo ratings yet
- Fluid Volume Deficit Nursing ManagementDocument5 pagesFluid Volume Deficit Nursing ManagementA.No ratings yet
- Hemorrhagic Shock - StatPearls - NCBI BookshelfDocument8 pagesHemorrhagic Shock - StatPearls - NCBI BookshelfRizqan Fahlevvi AkbarNo ratings yet
- Update On (Approach To) Anemia1 (Changes)Document39 pagesUpdate On (Approach To) Anemia1 (Changes)Balchand KukrejaNo ratings yet
- Fluid and Electrolytes Assignment 1. What Are The Different Processes of Body Fluid and Solutes Movement? and Give at Least 2 Examples EachDocument8 pagesFluid and Electrolytes Assignment 1. What Are The Different Processes of Body Fluid and Solutes Movement? and Give at Least 2 Examples EachAngelicaNo ratings yet
- Fluid and Electrolytes Assignment 1. What Are The Different Processes of Body Fluid and Solutes Movement? and Give at Least 2 Examples EachDocument8 pagesFluid and Electrolytes Assignment 1. What Are The Different Processes of Body Fluid and Solutes Movement? and Give at Least 2 Examples EachAngelicaNo ratings yet
- HiponatremiaDocument8 pagesHiponatremiaMeidistya Ayu MardhianiNo ratings yet
- EdemaDocument4 pagesEdemaWanchung ZienNo ratings yet
- DehydrationDocument27 pagesDehydrationDivika ShilvanaNo ratings yet
- HyponatremiaDocument6 pagesHyponatremiaJaymart Saclolo CostillasNo ratings yet
- Dan L Ellsbury, MD, FAAPDocument8 pagesDan L Ellsbury, MD, FAAPfaruuukNo ratings yet
- Fluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsDocument17 pagesFluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsA.No ratings yet
- The Physical Examination To Assess For Anemia and HypovolemiaDocument10 pagesThe Physical Examination To Assess For Anemia and HypovolemiaAlejandro MaitaNo ratings yet
- Fluid Replacement GOODocument13 pagesFluid Replacement GOOMansoor TariqNo ratings yet
- Shock HypovolemicDocument16 pagesShock HypovolemicTitinNo ratings yet
- Hepatorenal Syndrome: Causes, Tests, and Treatment OptionsFrom EverandHepatorenal Syndrome: Causes, Tests, and Treatment OptionsRating: 4.5 out of 5 stars4.5/5 (2)
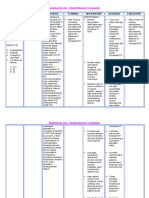
- Defining Characteristics Nursing Diagnosis Outcome Identification Nursing Interventions Rationale EvaluationDocument2 pagesDefining Characteristics Nursing Diagnosis Outcome Identification Nursing Interventions Rationale EvaluationRoselyn VelascoNo ratings yet
- ActDocument1 pageActRoselyn VelascoNo ratings yet
- Questions in CasesDocument10 pagesQuestions in CasesRoselyn VelascoNo ratings yet
- ISLAMDocument2 pagesISLAMRoselyn VelascoNo ratings yet
- 1 Data Gathering 1Document32 pages1 Data Gathering 1Roselyn VelascoNo ratings yet
- What Are The Common Causes of AGEDocument2 pagesWhat Are The Common Causes of AGERoselyn VelascoNo ratings yet
- DocumentDocument1 pageDocumentRoselyn VelascoNo ratings yet
- Case Presentation 4 AGEDocument33 pagesCase Presentation 4 AGERoselyn VelascoNo ratings yet
- Piaget and EriksonDocument4 pagesPiaget and EriksonRoselyn VelascoNo ratings yet
- Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationRoselyn Velasco100% (1)
- Daily Medication SheetDocument1 pageDaily Medication SheetRoselyn VelascoNo ratings yet
- Reproductive System PharmaDocument67 pagesReproductive System PharmaRoselyn VelascoNo ratings yet
- Business Plan: Forms of Small Business OwnershipDocument3 pagesBusiness Plan: Forms of Small Business OwnershipRoselyn VelascoNo ratings yet
- Hypovolemic Shock Nursing Care Management and Study GuideDocument1 pageHypovolemic Shock Nursing Care Management and Study GuideRoselyn VelascoNo ratings yet
- HydrocephalusDocument33 pagesHydrocephalusRoselyn VelascoNo ratings yet
- Routine RBC CountingDocument9 pagesRoutine RBC CountingWilmor BenedictosNo ratings yet
- Hemochron Hemochron Hemochron HemochronDocument2 pagesHemochron Hemochron Hemochron Hemochrontravieso1120% (1)
- Serologi ForensikDocument65 pagesSerologi ForensikbayuNo ratings yet
- NCP RosteDocument2 pagesNCP RosteRoyce Vincent TizonNo ratings yet
- Anemia 2024Document50 pagesAnemia 2024b9p6vmfnc4No ratings yet
- Healing of Tooth Extraction Socket: Dr. Pankaj Datta Dr. Shilpa Khullar Dr. Mittal ADocument3 pagesHealing of Tooth Extraction Socket: Dr. Pankaj Datta Dr. Shilpa Khullar Dr. Mittal AwatidinaNo ratings yet
- HistologyDocument65 pagesHistologyAlliana FlorenzaNo ratings yet
- Histology Structure of SkinDocument4 pagesHistology Structure of SkinLIEBERKHUNNo ratings yet
- Erythropoiesi S: by DR - Absar Ullah KhanDocument37 pagesErythropoiesi S: by DR - Absar Ullah KhanHassan AhmedNo ratings yet
- Virtual Long Bone DissectionDocument2 pagesVirtual Long Bone Dissectionapi-438810380No ratings yet
- Blood Specimen CollectionDocument20 pagesBlood Specimen CollectionChristian OleleNo ratings yet
- Membranes and FasciaeDocument18 pagesMembranes and FasciaeBurak KıvırcıkNo ratings yet
- Chapter 28Document7 pagesChapter 28MARCERA JERALDINE ALESSA P.No ratings yet
- Connective Tissue Slide #1Document19 pagesConnective Tissue Slide #1Faisal AbbasiNo ratings yet
- Islh 2009 Consensus RulesDocument10 pagesIslh 2009 Consensus RulesDanielIvanGuerreroNo ratings yet
- Dade Ci-Trol Coagulation Control Level 2Document6 pagesDade Ci-Trol Coagulation Control Level 2Lab BiosNo ratings yet
- Test Bank For Exercise Physiology Theory and Application To Fitness and Performance 10th Edition Scott Powers Edward Howley DownloadDocument7 pagesTest Bank For Exercise Physiology Theory and Application To Fitness and Performance 10th Edition Scott Powers Edward Howley Downloadjosephpereznqwsmfbcgp100% (33)
- Assessment of Musculoskeletal Function Assessment of Musculoskeletal FunctionDocument22 pagesAssessment of Musculoskeletal Function Assessment of Musculoskeletal FunctionKaushena LindsayNo ratings yet
- Bangalore Baptist Hospital: Laboratory ResultsDocument3 pagesBangalore Baptist Hospital: Laboratory ResultskavyaksNo ratings yet
- Important Questions For CBSE Class 7 Science Chapter 11Document7 pagesImportant Questions For CBSE Class 7 Science Chapter 11Atabuddin MondalNo ratings yet
- Blood BankingDocument1 pageBlood BankingFrancis ArciagaNo ratings yet
- Sandaletal UpdateonITPDocument18 pagesSandaletal UpdateonITPMarcellia AngelinaNo ratings yet
- Normal Erythrocyte1Document4 pagesNormal Erythrocyte1RonyArtoKapidaNo ratings yet
- Lab1 - RBCDocument4 pagesLab1 - RBCRamos, NicoleNo ratings yet
- Blood GroupsDocument28 pagesBlood GroupsKamran ZaheerNo ratings yet
- Cell SaverDocument8 pagesCell SaverFrank QuitianNo ratings yet
- (Prothrombin Time) : Intended UseDocument2 pages(Prothrombin Time) : Intended UseDharmesh PatelNo ratings yet
- Activity 11 Discussion Serum Plasma Preparation Centrifuging and TransferringDocument3 pagesActivity 11 Discussion Serum Plasma Preparation Centrifuging and TransferringErin De LaraNo ratings yet