Professional Documents
Culture Documents
Discussions: Comparative Computational Study of Nipah Virus Drugs
Discussions: Comparative Computational Study of Nipah Virus Drugs
Uploaded by
DAMBALECopyright:
Available Formats
You might also like
- Microorganisms As Bio Indicators and BiosensorsDocument42 pagesMicroorganisms As Bio Indicators and BiosensorsJAFFER YOUSUF85% (13)
- Snurfle Meiosis Another WSDocument2 pagesSnurfle Meiosis Another WSAdriana IzquierdoNo ratings yet
- Prediction of Potential Commercially Inhibitors Against Sars-Cov-2 by Multi-Task Deep ModelDocument8 pagesPrediction of Potential Commercially Inhibitors Against Sars-Cov-2 by Multi-Task Deep ModelamyzeevshelaNo ratings yet
- In Silico Identification of Clinically Approved Medicines Against The Main Protease of Sars-Cov-2, Causative Agent of Covid-19Document17 pagesIn Silico Identification of Clinically Approved Medicines Against The Main Protease of Sars-Cov-2, Causative Agent of Covid-19Rakesh DavellaNo ratings yet
- Virtual Screening of Phytochemical Compounds As Potential Inhibitors Against HIV-1 Resistance To Protease InhibitorDocument6 pagesVirtual Screening of Phytochemical Compounds As Potential Inhibitors Against HIV-1 Resistance To Protease InhibitorZoya AmjadNo ratings yet
- Marroqui2008 Efecto de Inhinidor IPNVDocument7 pagesMarroqui2008 Efecto de Inhinidor IPNVandrea nettle bareaNo ratings yet
- Literature Review On PCRDocument6 pagesLiterature Review On PCRafdtzfutn100% (1)
- Clarke - 2002 - Molecular Diagnosis of HIVDocument7 pagesClarke - 2002 - Molecular Diagnosis of HIVSebastianNo ratings yet
- Biochemical and Biophysical Research CommunicationsDocument6 pagesBiochemical and Biophysical Research CommunicationslilisasaiNo ratings yet
- 1 s2.0 S0377123720300988 MainDocument6 pages1 s2.0 S0377123720300988 MainautomationenggNo ratings yet
- 4699-Article Text-8003-1-10-20220919Document8 pages4699-Article Text-8003-1-10-20220919Efrin SitumorangNo ratings yet
- 42 Han 2012 BMCBioinformaticsDocument10 pages42 Han 2012 BMCBioinformaticsrammhtoNo ratings yet
- Computational Analysis of Protein Interactions Between HIV-1 and Homo SapiensDocument5 pagesComputational Analysis of Protein Interactions Between HIV-1 and Homo SapiensFaiza MalikNo ratings yet
- Oral Antiviral Newsletter Yan Versi 2 - Dec 2021Document7 pagesOral Antiviral Newsletter Yan Versi 2 - Dec 2021YanMardianNo ratings yet
- Sadianaz 2018Document25 pagesSadianaz 2018Laísa BarséNo ratings yet
- Potential Therapeutic Agents For COVID-19 Based On The Analysis of Protease and RNA Polymerase DockingDocument7 pagesPotential Therapeutic Agents For COVID-19 Based On The Analysis of Protease and RNA Polymerase DockingJoseGarciaNo ratings yet
- 2020-Joshi-In Silico Screening of Natural Compounds Against COVID-19 by Targeting Mpro and ACE2 Using Molecular DockingDocument8 pages2020-Joshi-In Silico Screening of Natural Compounds Against COVID-19 by Targeting Mpro and ACE2 Using Molecular DockingAdriana SantosNo ratings yet
- SPIN BindingSiteAnalysisOfPotentialDocument6 pagesSPIN BindingSiteAnalysisOfPotentialnishiNo ratings yet
- Biochem Term Paper Reporting - DISCUSSIONDocument1 pageBiochem Term Paper Reporting - DISCUSSIONShakira AntiquinaNo ratings yet
- Bioorganic & Medicinal ChemistryDocument9 pagesBioorganic & Medicinal ChemistryJunaid KhanNo ratings yet
- tmp9EA0 TMPDocument5 pagestmp9EA0 TMPFrontiersNo ratings yet
- Test 11Document14 pagesTest 11CiprianNo ratings yet
- Dissertation HCVDocument8 pagesDissertation HCVWriteMyPaperForMeIn3HoursCanada100% (1)
- Iddt 226ap2Document8 pagesIddt 226ap2pooja pandeyNo ratings yet
- Yunnan Key 2014Document9 pagesYunnan Key 2014crpen87No ratings yet
- Comparing Genetic Evolutionary Algorithms On Three Enzymes of HIV-1: Integrase, Protease, and Reverse TranscriptomeDocument13 pagesComparing Genetic Evolutionary Algorithms On Three Enzymes of HIV-1: Integrase, Protease, and Reverse TranscriptomeAI Coordinator - CSC JournalsNo ratings yet
- Sars Cov 2 Tratamentos Artigo NatureDocument6 pagesSars Cov 2 Tratamentos Artigo NaturesandraNo ratings yet
- A Antisense Technology 2Document2 pagesA Antisense Technology 2Gourav JainNo ratings yet
- CORVELVA Metagenomic Analysis Report On Gardasil 9Document9 pagesCORVELVA Metagenomic Analysis Report On Gardasil 9Gene XeneNo ratings yet
- Prediction of Interactions Between Hiv-1 and Human ProteinsDocument5 pagesPrediction of Interactions Between Hiv-1 and Human ProteinsDipyaman KunduNo ratings yet
- Iin Silicoi Screening and Molecular Docking of Bioactive Agents Towards Human CoronavirusDocument5 pagesIin Silicoi Screening and Molecular Docking of Bioactive Agents Towards Human CoronavirusSuresh KumarNo ratings yet
- 10 1016@j Molstruc 2020 129433Document25 pages10 1016@j Molstruc 2020 129433sananaveed.akberNo ratings yet
- Emerging Therapies in Hepatitis C. Dawn of The Era of The Direct Acting Antivirals (2011)Document14 pagesEmerging Therapies in Hepatitis C. Dawn of The Era of The Direct Acting Antivirals (2011)drheayNo ratings yet
- Is Oseltamivir Suitable For Fighting Against COVID-19 in Silico Assessment, in Vitro and Retrospective StudyDocument1 pageIs Oseltamivir Suitable For Fighting Against COVID-19 in Silico Assessment, in Vitro and Retrospective Studychristian bataNo ratings yet
- CH 15. Understanding The Statistical Analysis of Resistance Data - Antiretroviral Resistance in Clinical Practice - NCBI BookshelfDocument6 pagesCH 15. Understanding The Statistical Analysis of Resistance Data - Antiretroviral Resistance in Clinical Practice - NCBI BookshelfntnquynhproNo ratings yet
- Inhibition of The SARS-CoV-2 RNA-Dependent RNA Polymerase by Natural BioactiveDocument13 pagesInhibition of The SARS-CoV-2 RNA-Dependent RNA Polymerase by Natural BioactiveLuis MartinezNo ratings yet
- Construction and Application of A Protein Interaction - 2014 - Molecular - CelluDocument14 pagesConstruction and Application of A Protein Interaction - 2014 - Molecular - CelluTanIsmNo ratings yet
- Drugs For Hepatitis CDocument3 pagesDrugs For Hepatitis CIrvan PutraNo ratings yet
- Tied Down by Its Own Receptor: News & ViewsDocument2 pagesTied Down by Its Own Receptor: News & ViewsSimoné S SimonNo ratings yet
- Dissertation RT PCRDocument5 pagesDissertation RT PCRBuyAcademicPapersSingapore100% (1)
- Molecular Docking Analysis of Peptide-Based Antiviral Agents Against Sars-Cov-2 Main Protease: An Approach Towards Drug RepurposingDocument12 pagesMolecular Docking Analysis of Peptide-Based Antiviral Agents Against Sars-Cov-2 Main Protease: An Approach Towards Drug RepurposinguttamNo ratings yet
- Using Improved Non Ri - Maprec Assay To Detect Virulence Mutations in Poliomyelitis Vaccine Viruses: Advantages Over 40 TestDocument7 pagesUsing Improved Non Ri - Maprec Assay To Detect Virulence Mutations in Poliomyelitis Vaccine Viruses: Advantages Over 40 TestBa Trần VănNo ratings yet
- Bepridil Is Potent Against SARS-CoV-2 in VitroDocument28 pagesBepridil Is Potent Against SARS-CoV-2 in VitrosovalaxNo ratings yet
- Policresulen, A Novel NS2BNS3 Protease Inhibitor, PDFDocument11 pagesPolicresulen, A Novel NS2BNS3 Protease Inhibitor, PDFFernando cisneros prietoNo ratings yet
- tmpB794 TMPDocument13 pagestmpB794 TMPFrontiersNo ratings yet
- Potential Antiviral Agents for Coronaviruses: Compounds, Herbal Products, and Drug TargetsFrom EverandPotential Antiviral Agents for Coronaviruses: Compounds, Herbal Products, and Drug TargetsNo ratings yet
- Molecules Paper - CompressedDocument15 pagesMolecules Paper - CompressedkaviNo ratings yet
- 1 s2.0 S147692712200055X MainDocument18 pages1 s2.0 S147692712200055X Mainjipir64332No ratings yet
- 1 s2.0 S0223523421007522 MainDocument16 pages1 s2.0 S0223523421007522 Mainjipir64332No ratings yet
- Use of Monoclonal Antibodies Against Hendra and Nipah Viruses in An Antigen Capture ElisaDocument8 pagesUse of Monoclonal Antibodies Against Hendra and Nipah Viruses in An Antigen Capture ElisaThamizh Kumaran RNo ratings yet
- 2020 01 29 20019448v1 FullDocument27 pages2020 01 29 20019448v1 Fulljhonny12321No ratings yet
- Vaccine: Mitchell Tyler, Ebenezer Tumban, Agnieszka Dziduszko, Michelle A. Ozbun, David S. Peabody, Bryce ChackerianDocument8 pagesVaccine: Mitchell Tyler, Ebenezer Tumban, Agnieszka Dziduszko, Michelle A. Ozbun, David S. Peabody, Bryce ChackerianElizabeth CollinsNo ratings yet
- Journal of Molecular Graphics and ModellingDocument13 pagesJournal of Molecular Graphics and ModellingPencari IlmuNo ratings yet
- Heterotypic Interactions Drive Antibody Synergy Against A Malaria Vaccine CandidateDocument12 pagesHeterotypic Interactions Drive Antibody Synergy Against A Malaria Vaccine CandidateSamer ShamshadNo ratings yet
- Srep 42769Document12 pagesSrep 42769ara.lv007No ratings yet
- Journal Pre-Proof: Phytomedicine PlusDocument35 pagesJournal Pre-Proof: Phytomedicine PlusMohammed Shuaib AhmedNo ratings yet
- Docking Study of Naringin Binding With COVID-19 Main ProteaseDocument8 pagesDocking Study of Naringin Binding With COVID-19 Main ProteaseLuis MartinezNo ratings yet
- s12900-018-0085-4Document13 pagess12900-018-0085-4Daniel FelipeNo ratings yet
- Virology Journal: Virus Detection and Identification Using Random Multiplex (RT) - PCR With 3'-Locked Random PrimersDocument11 pagesVirology Journal: Virus Detection and Identification Using Random Multiplex (RT) - PCR With 3'-Locked Random PrimersMarie Angeline CletoNo ratings yet
- Infant HIV TestsDocument5 pagesInfant HIV TestsProf Rakesh SharmaNo ratings yet
- In-Silico Pharmacophoric and Molecular Docking-Based Drug Discovery Against The Main Protease (M) of Sars-Cov-2, A Causative Agent Covid-19Document9 pagesIn-Silico Pharmacophoric and Molecular Docking-Based Drug Discovery Against The Main Protease (M) of Sars-Cov-2, A Causative Agent Covid-19sonyekanugrahaNo ratings yet
- Epilepsia - 2002 - Anderson - Children Versus Adults Pharmacokinetic and Adverse Effect DifferencesDocument7 pagesEpilepsia - 2002 - Anderson - Children Versus Adults Pharmacokinetic and Adverse Effect DifferencesDAMBALENo ratings yet
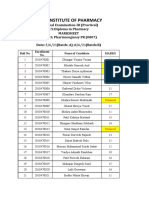
- PGY PR Attendance ReportDocument4 pagesPGY PR Attendance ReportDAMBALENo ratings yet
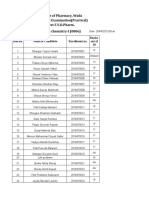
- Pgy PR Sessional-Iii MarksheetDocument3 pagesPgy PR Sessional-Iii MarksheetDAMBALENo ratings yet
- BLUEPRINT - Basic Principles of Toxicology Elective TYDocument2 pagesBLUEPRINT - Basic Principles of Toxicology Elective TYDAMBALENo ratings yet
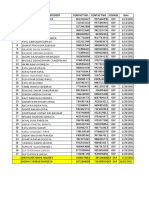
- PC-I, FY 2nd Sessional (PR) ReportDocument13 pagesPC-I, FY 2nd Sessional (PR) ReportDAMBALENo ratings yet
- PH-I Sessional 2. Exam MARKSHEETDocument3 pagesPH-I Sessional 2. Exam MARKSHEETDAMBALENo ratings yet
- 8TH Sem Project MarksheetDocument5 pages8TH Sem Project MarksheetDAMBALENo ratings yet
- SR - NO. Name of The Student Contact No. Contact No. Course DateDocument1 pageSR - NO. Name of The Student Contact No. Contact No. Course DateDAMBALENo ratings yet
- Tax Invoice: Shipping Address: Sold By: Invoice DetailsDocument1 pageTax Invoice: Shipping Address: Sold By: Invoice DetailsDAMBALENo ratings yet
- Blue Print PHARMACOLOGY-I (1) - 2Document1 pageBlue Print PHARMACOLOGY-I (1) - 2DAMBALENo ratings yet
- Ideal Institute of Pharmacy - Posheri - Wada B-Pharmacy Ii ND Year 2020-21Document12 pagesIdeal Institute of Pharmacy - Posheri - Wada B-Pharmacy Ii ND Year 2020-21DAMBALENo ratings yet
- Pharmaceutics - I (Theory) Set-ADocument1 pagePharmaceutics - I (Theory) Set-ADAMBALENo ratings yet
- University of Mumbai: Fourth Year B. of Pharmacy (Sem VIII) (CBCS)Document1 pageUniversity of Mumbai: Fourth Year B. of Pharmacy (Sem VIII) (CBCS)DAMBALENo ratings yet
- Pradnya - Sheet1Document1 pagePradnya - Sheet1DAMBALENo ratings yet
- BLUEPRINT - Basic Principles of Toxicology Elective TYDocument2 pagesBLUEPRINT - Basic Principles of Toxicology Elective TYDAMBALENo ratings yet
- Comparative Computational Study On Nipah Virus DrugsDocument10 pagesComparative Computational Study On Nipah Virus DrugsDAMBALENo ratings yet
- Comparativecomputational Study On Nipah Virus DrugsDocument10 pagesComparativecomputational Study On Nipah Virus DrugsDAMBALENo ratings yet
- Not Return Teachers Book ListDocument1 pageNot Return Teachers Book ListDAMBALENo ratings yet
- Website: WWW - Niperhyd.ac - in / WWW - Niperhyd.edu - In: TH THDocument24 pagesWebsite: WWW - Niperhyd.ac - in / WWW - Niperhyd.edu - In: TH THDAMBALENo ratings yet
- Siddhi Bhagwan Dalvi ....Document5 pagesSiddhi Bhagwan Dalvi ....DAMBALENo ratings yet
- Teaching AdvertisementDocument9 pagesTeaching AdvertisementDAMBALENo ratings yet
- Global Celiac Disease CD Market InsightsDocument3 pagesGlobal Celiac Disease CD Market InsightsericinsfNo ratings yet
- Controlled Release Technology and Design of Oral Controlled Released Dosage Forms Design and Scale Up of Drag Granulation ProcessDocument8 pagesControlled Release Technology and Design of Oral Controlled Released Dosage Forms Design and Scale Up of Drag Granulation ProcessYahya IsiedNo ratings yet
- O'Toole Et Al. (2017) Next Generation Probiotics Probiotics To Live BiotherapeuticsDocument19 pagesO'Toole Et Al. (2017) Next Generation Probiotics Probiotics To Live BiotherapeuticsTahir AliNo ratings yet
- Plant Immunology Lecture 9Document30 pagesPlant Immunology Lecture 9Lavander BlushNo ratings yet
- Top Ten Pharma Financials 2011Document136 pagesTop Ten Pharma Financials 2011Harjyot RandhawaNo ratings yet
- Unit 2 Part 2: Transgenic Animals Transgenic Fish Animal As BioreactorsDocument43 pagesUnit 2 Part 2: Transgenic Animals Transgenic Fish Animal As BioreactorsPraveen KumarNo ratings yet
- Classical (Mendelian) GeneticsDocument32 pagesClassical (Mendelian) GeneticsKOMAL FATIMANo ratings yet
- Cell Therapy: CGMP Facilities and Manufacturing: Mini ReviewDocument6 pagesCell Therapy: CGMP Facilities and Manufacturing: Mini ReviewMajin BooNo ratings yet
- 2 722597121924006461Document286 pages2 722597121924006461Shahul HameedNo ratings yet
- Lab 1Document1 pageLab 1AzharNo ratings yet
- Lecture 1: An Overview: Marine Biotechnology at Undip and Review of Undip-Ucsc CollaborationDocument52 pagesLecture 1: An Overview: Marine Biotechnology at Undip and Review of Undip-Ucsc CollaborationsaniyatlyNo ratings yet
- Linkage and Genetic Mapping EukaryotesDocument66 pagesLinkage and Genetic Mapping EukaryotesSITI BAZILAH BINTI BILAK KPM-GuruNo ratings yet
- Enzyme: Oleh Yana Cahyana Stp.,Dea.,Ph.DDocument21 pagesEnzyme: Oleh Yana Cahyana Stp.,Dea.,Ph.DDETA HARTININo ratings yet
- Lecture 01Document15 pagesLecture 01Tanvir FahimNo ratings yet
- The Study of Life BiologyDocument6 pagesThe Study of Life BiologyJokher BaliliNo ratings yet
- HB 1927 1090923 LL Quantinova Probe RT PCR Kit 0315 WWDocument4 pagesHB 1927 1090923 LL Quantinova Probe RT PCR Kit 0315 WWnbiolab6659No ratings yet
- Bio Two Ses Chapter 6Document12 pagesBio Two Ses Chapter 6azizrafeeqNo ratings yet
- Kuliah S2 Transport IntraselulerDocument27 pagesKuliah S2 Transport IntraselulerDwi Retna LestariNo ratings yet
- Pathology of The Bile Duct 2017 - Yasuni Nakanuma PDFDocument215 pagesPathology of The Bile Duct 2017 - Yasuni Nakanuma PDFHîrjoabă IoanNo ratings yet
- Name: - PeriodDocument3 pagesName: - PeriodMia HopkinsNo ratings yet
- Biology 102 SyllabusDocument2 pagesBiology 102 Syllabusapi-285160591No ratings yet
- AQA Biology 2 Revision Notes PDFDocument31 pagesAQA Biology 2 Revision Notes PDFRajashree MuNo ratings yet
- (Methods in Molecular Biology 1644) Vladimir V. Didenko (Eds.) - Fast Detection of DNA Damage - Methods and Protocols-Springer New York (2017) PDFDocument213 pages(Methods in Molecular Biology 1644) Vladimir V. Didenko (Eds.) - Fast Detection of DNA Damage - Methods and Protocols-Springer New York (2017) PDFMauro Porcel de PeraltaNo ratings yet
- NCM 212 - Drug Approval ProcessDocument8 pagesNCM 212 - Drug Approval ProcessLYRIZZA LEA BHEA DESIATANo ratings yet
- Transient Reprogramming of Crop Plants For Agronomic PerformanceDocument16 pagesTransient Reprogramming of Crop Plants For Agronomic PerformanceSELNo ratings yet
- Artikel Kesehatan Dalam Bahasa Inggris Dan Terjemahannya TerbaruDocument3 pagesArtikel Kesehatan Dalam Bahasa Inggris Dan Terjemahannya TerbaruRafaelDimasRizky67% (3)
- Clonagem Animal A Sobrevivência Dos Mais Aptos 2012Document19 pagesClonagem Animal A Sobrevivência Dos Mais Aptos 2012Felipe JuniorNo ratings yet
- Topic 3.2 Karyogram PracticeDocument2 pagesTopic 3.2 Karyogram PracticeAleksandra LukanovskaNo ratings yet
Discussions: Comparative Computational Study of Nipah Virus Drugs
Discussions: Comparative Computational Study of Nipah Virus Drugs
Uploaded by
DAMBALEOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Discussions: Comparative Computational Study of Nipah Virus Drugs
Discussions: Comparative Computational Study of Nipah Virus Drugs
Uploaded by
DAMBALECopyright:
Available Formats
Comparative computational study of Nipah Virus Drugs
Discussions
NiV is a deadly zoonotic virus with a mortality rate of 72% and 86% in Bangladesh
and India respectively. There is no known drugs/therapeutics against NiV. The
overarching aim of this study is to computationally design inhibitors and predict
small molecule drugs against NiV proteins. To design/predict therapeutic molecules
to act against NiV, we characterized all of its proteins. As a part of this effort, we
constructed partial models of 5 NiV proteins viz., M, L, V, W proteins along with the
post fusion conformation of the F protein. The structure of the post-fusion
conformation of the F protein is modeled for the first time in this study. Our model
is based on the post-fusion structures of another class I fusion protein from Human
Parainfluenza virus 3.
Our efforts have increased the coverage of existing structures of the G, N and P
proteins (by 13%, 8% and 8% respectively) by modeling a fraction of their
unresolved residues. No reliable models could be generated for the C protein.
Effectively, we doubled the number of amino acids in the NiV proteome that were
structurally characterized. While our aim is to use these models to predict/design
inhibitors, we believe that many of our models are by themselves quite insightful.
They could serve as templates for future structure-guided drug designing efforts
against members of the Paramyxoviridae family. We attempted to build complexes
of the viral and host protein (host cathepsin-L with NiV F protein and host AP3-B1
with NiV M protein) to target the interactions for inhibitor design. However, we
were unsuccessful in making reliable models of host-pathogen protein-protein
interaction complexes. With improvements to protein-protein docking methods, the
quality of such models of complexes could be improved, which in turn would help in
better targeting host-viral interactions.
We next used these models to design 4 peptide inhibitors against the F, M and G
proteins. The inhibitor against F protein would putatively prevent the pre to post
fusion transition of the F protein, a crucial step for viral entry. Our model of the post
fusion conformation of the F protein was crucial in designing this inhibitor. Another
inhibitor against the M protein was designed such that it would prevent the
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
dimerization of the protein, hence preventing the budding process. The two
inhibitors against the G proteins were selected such that they bind to the ephrin
receptor binding pocket, preventing viral attachment to the host cell. The peptides
here mimic the ephrin-B2 protein and an antibody (m102.3) that are bound at the
same site. We conjectured that these peptides would competitively inhibit the G
protein from binding the host ephrin receptors. All of these protein-peptide systems
were subjected to triplicate runs of 100 ns MD simulations to assess interaction
strengths. The distance of the center of the inhibitor and the peptide fluctuates with
a standard deviation of 0.03-0.09 nm from the mean distance, indicative of the
inhibitor remaining in the binding pocket. The inhibitors against the F and M
proteins also had stable hydrogen bond associations in the MD trajectories. Binding
affinity calculations suggest that three of the designed putative inhibitors bind tightly
(~100 kJ/mol) to their targets, making them promising leads against NiV proteins.
We screened a set of drug like molecules in a docking exercise to identify potential
small molecule inhibitors of NiV. The screen consisted of 22685 compounds of the
70% non-redundant set of clean drug like molecules of the ZINC library. The
docking onto the NiV proteins was done using two different docking programs,
Autodock4 and Dock6.8. Empirically, we chose the top 100 ligands from each of the
two methods and selected those that were common between them. This resulted in
70 compounds that bound the G, N, P, F and M proteins of NiV. As a more stringent
test, we whittled down this list to only include those molecules that were docked in
similar poses (empirically chosen RMSD of 0.15 nm or smaller) on the same binding
site. Hence, we predicted 10 compounds that would inhibit the N (5), P (4) and M (1)
proteins of NiV. In addition we also included 3 drugs to the list that did not clear the
criteria explained above. These drugs include one that binds the G protein on its
ephrin binding interface and two others which bind to P and M proteins. The most
important aspect of the docking study is that the molecular screen consists of known
drugs or drug like compounds. The implication is that a few of our proposed
inhibitors could be readily tested and repurposed. For instance, we have identified
Cyclopent-1-ene-1,2-dicarboxylic acid (ZINC04829362) as an inhibitor of the NiV N
protein. This compound is a known drug prescribed for antiasthmatic and
antopsoriatic among other disorders. Another example is Bicyclo[2.2.1]hepta-2,5-
diene-2,3-dicarboxylic acid (ZINC12362922) that we propose also inhibits the N
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
protein, is a drug prescribed against depression and Parkinson’s disease. We cannot
overemphasize the importance of these computational predictions, especially for
swift acting potent viruses as NiV where mortality rates are high.
Finally, we assessed the how effective our proposed inhibitors would be against
different strains of the virus and assess the risk of the virus getting drug resistant.
For this, we studied 3 Bangladeshi, 7 Malaysian and 5 Indian strains and inferred
the variations between the various strains from their multiple sequences alignment.
Further, we investigated whether such changes would affect inhibitor binding. Here,
we narrowed the changes only to those residues that were in direct contact (< 0.5
nm) from the inhibitors. We precluded the possibility of allosteric interactions. None
of the residues contacting the peptide inhibitors showed any variations in their
sequence. Only 5 residue positions that were involved in binding the drug like
inhibitors were changed between the different strains. 4 of these changes are
conservative substitutions where the nature of the mutated residue is not deemed to
change the binding property of the protein to its inhibitor. Only 1 amino acid change
of Asp252Gly of the F protein is a non-conservative change, however the Asp is not
involved in hydrogen bonding with the ligand. We conclude that it is likely that the
proposed inhibitors would be potent against all strains of the virus
Nipah and other zoonotic virus pose a serious epidemic threat. Computational
approaches can help identify/design inhibitors that could be rapidly tested or even
deployed as they may be drugs previously licensed for other uses. Our study also has
connotations for related viruses such as Hendra and other Paramyxoviruses.
Importantly, our models and the web pages we have created could be modified to
serve as portal to study the epidemiology of the virus should there be further
outbreaks.
The presence of antiviral prediction web servers is important for combating the
emerging viral infections speedily. It become more important, especially for the
viruses against which no treatment modality is available. Although, the limited
antiviral prediction algorihtms are available for the prediction of compounds
against viral infections, which includes the AVCpred, HIVprotI, and Anti-flavi
(Qureshi et al., 2017, 2018; Rajput and Kumar, 2018). The AVCpred is an antiviral
compound prediction server, especially for viruses HIV, HCV, HBV, HHV and also,
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
include a general prediction tool for 26 viruses. While HIVprotI is a dedicated
prediction server for compounds specifically targeting the integrase, protease and
reverse transcriptase of HIV. The Anti-flavi web based predcition algorithm is
helpful to predict and identify inhibitors against flaviviruses. However, in the
present study, we have developed the first QSAR based “anti-Nipah” prediction web
server for the screening of compounds having antiviral activity against NiV.
We have developed the first database (313 entries) with all the inhibitors of Nipah
Virus, which include 120 chemical inhbitors which are highly diverse and varies in
molecular weight from 182 to 1,000 g/mol. The maximally validated anti-nipah
inhibitor is Flavipiravir, which is a purine analog and one amongst the effective
broad-specturm antiviral effective against RNA viruses (Dawes et al., 2018).
Followed by, several novel antivirals designed to target the replication stage of NiV
(Aljofan et al., 2009a). Likewise, the user can get the details of all the NiV inhibitors
available in reseach artciles as well as patents at a platform using our web resource.
Further, using the experimentally validated data, we developed a robust QSAR
based prediction method. This is the first QSAR based web server (integrating
recursive regression model) dedicated to Nipah virus. The user can predict the anti-
NiV activity of any unknown compound with the PCC of 0.82. Thus, our predictor
would be very helpful to experimental biologists for speeding up their research
toward developing novel and effective anti-NiV scaffolds.
The robustness of the prediction models were cross-checked using various statistical
approaches like using independent validation dataset, applicability domain
(William's plot), scatter plot, and decoy set. The independent validation dataset is
considered as the external validation of the model, and we got a good PCC of 0.92,
that showes that developed predictive model possess very high efficiency to predict
an unknown molecule efficiently. Further, the applicability domain showed that the
model is highly robust as majority of the datapoints lies within the cutoff threshold
of leverage and standard residuals. Likewise, the scatter plot between actual and
predicted accuracies further support the robustness of model with Spearman's and
Pearson's correlation coefficient of 0.80 and 0.82, respectively. Moreover, the low
predcition efficiency of decoy set further confirm the efficiency of prediction model.
Thus, all the multivariate analysis approach proves the relaibilty of the model.
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
The similarity analyses showed the diversity of the anti-NiV compounds. Highly
effective (low IC50) were clustered together, while the less effective/inactive (high
IC50) compounds are scattered throughout the dendrogram. Thus, the presence of
similar scaffold or chemical modifications might have resulted in the clustering of
the active compounds. Interstingly, while performing the chemical clustering
analysis, we found that in a few cases, highly efficient and less efficient compounds
were also clustered together. The chemical modifications in functional groups might
have increased their activity against NiV. Most of LJ series compounds, synthesized
using side chain modification, were found to be clustered together. A modification in
either carbon chain, carbon ring, or side group may have caused the transient shift
in the activity of these compound. Therefore, the construction of chemical libraries
using side group modifications can be useful for screening the effective antiviral
compounds against NiV. Thus, our anti-Nipah prediction tool will be useful in the
screening of such compounds against NiV. As NiV is a BSL-4 pathogen, therefore
large scale screening for NiV inhibitors is a limiting factor. Hence, this becomes the
limitation of our predictor as it is developed on the less number of chemicals
available in literature. However, it is the first initiative toward developing the NiV
dedicated computaional tool, but we will update our method as we get new updated
data of NiV inhibitors.
Epidemiology
Host
Pteropus fruit bats are considered to be the natural host of NiV infection and
are more commonly found in South East Asian & African countries. The
reactive and neutralizing antibodies to NiV were detected in Pteropus fruit
bats of Malaysia, Cambodia, Thailand, India, Bangladesh, and Papua New
Guinea and non-Pteropid bats of Madagascar, Ghana, and China [6]. NiV has
potential to cause infection that can be fatal in horses, pigs, cats, dogs, ferrets,
hamsters, guinea pigs, monkeys, and humans [7].
Modes of transmission
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
NiV outbreak in Malaysia occurred during 1998–1999 due to the spillage of
NiV from bats to pigs after consuming half eaten-fruits by bats [8]. Initially,
the outbreak was misapprehended as JE, but later the source of infection was
recognized as close contact with infected pigs and subsequent transmission to
humans. [6,[8], [9], [10], [11]]. Infection also spread to pig handlers in
Singapore, as pigs were imported from Malaysia [8].
First outbreak in Bangladesh occurred in 2001, where northwestern and
central parts of the country were affected due to date palm sap consumption
and person-to-person transmission [8,12]. An investigation suggested, washing
infected corpse before burial according to Islamic rituals could have
transmitted infection to family members [13]. Other risk factors such as
contact with domestic animals and tree climbing demonstrated fewer chances
of spreading infection [14].
In India, the initial NiV outbreak occurred in Siliguri, West Bengal (2001).
Investigations suggested person to person transmission via respiratory
secretions [8,15]. In the 2018 outbreak of Kerala, fruit bats were found as the
source of NiV infections, confirmed by Indian council of Medical Research
(ICMR) [16].
Clinical features
The median incubation period in case of raw date palm sap consumption was
10 days while in case of exposure to pigs, it ranged from 4 days to 2 months
[1,17]. Majority of the patients show symptoms related to central nervous
system, but respiratory pathology has also been reported [1,16,18]. Main
presenting features of NiV infection are acute encephalitis with fever,
dizziness or vomiting; more than half of the infected cases presented reduced
level of consciousness or prominent brain stem dysfunction in Singapore [1].
Similar features were also seen during the Kerala outbreak, India
[16]. Neurological signs such as behavioral changes, spasms, uncoordinated
gait and myoclonus were reported in patients from Bangladesh [8]. Cough
was the commonly presented respiratory symptom, while atypical
pneumonia was reported in 14% cases in Malaysian outbreak [1,8,19].
Complications of infection included acute or late onset encephalitis and
associated disorientation or coma [20]. Viral bronchopneumonia, acute
respiratory distress syndrome and myocarditis were also reported during the
Kerala outbreak [16].
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
Environmental factors
Interactions between animals, humans and environment played a significant
role during NiV outbreaks among South Asian countries [16,21]. There are
multiple reasons for human-animal interactions like prolonged droughts,
reduced animal habitats due to deforestations, anthropogenic forest fires in
Indonesia and pig farming mixed with agriculture [10,22]. Deforestation
and urbanization results in destruction of bat habitats which triggers them to
invade human habitats for food. Hunger increases stress level and weakens
immune system of bats due to which there is an increase in the viral load in
their systems spilled out through secretions such as urine, semen or saliva
[20]. “One Health" approach i.e. “an approach to designing and implementing
programmes, policies, legislation and research in which multiple sectors
communicate and work together to achieve better public health outcomes”
[23] was stressed during NiV outbreak to attain global health security by
mitigating the effects caused by deforestation and urbanization [20].
Increase in virus shedding can also be associated with seasonal preferences. A
study conducted in Thailand demonstrated an elevated viral load between
April–June, correlating with the time period when young bats begin to fly. It
has also been reported that all outbreaks occurred during December to May
(winter and spring season) in Southeast Asia [20].
Outbreaks
NiV outbreaks in various countries, starting from 1999, have led to high
number of fatalities among humans. Case fatality rate (Table 2) and country-
wise sequence of events during the outbreaks is given below:
Table 1. Different diagnostic techniques developed in various labs.
Technique Place
Rapid immune plaque assay for the detection of
CSIRO, Australia
Nipah virus and anti-virus antibodies
Solid-phase blocking ELISA (enzyme-linked
immunosorbent assay) for detection of DVS, Malaysia
antibodies to Nipah virus
Real-time Reverse transcription polymerase
Institut Pasteur, France
chain reaction (RT-PCR) (TaqMan)
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
Technique Place
MAb (Monoclonal Antibodies) against National Institute of
formalin-inactivated NiV Animal Health, Japan.
Recombinant nucleocapsid protein produced University Putra,
in Escherichia coli Malaysia
MAb-based immunohistochemical diagnosis National Institute of
NiV Animal Health, Japan
Recombinant glycoprotein produced in insect University Putra,
cells Malaysia
Recombinant nucleocapsid protein produced in University Putra,
insect cells Malaysia
University Putra,
Recombinant glycoprotein produced in E. coli
Malaysia
NCFAD (National Centre
Monoclonal antibodies against NiV (4 MAbs
for Foreign Animal
against “N” protein and 1 against “M” protein
Disease), Canada
Indirect ELISA for the detection of Henipavirus Chinese National
antibodies based on a recombinant nucleocapsid Diagnostic Centre for
protein expressed in E. coli Exotic Animal Diseases
Indirect IgG ELISA for human and swine sera
and an IgM capture-ELISA for human sera Institute of Tropical
using the recombinant NiV-N protein as an Medicine, Japan
antigen
Neutralization assays for differential
Henipavirus serology using Bio-Plex Protein CSIRO, Australia
Array Systems
Duplex nested RT-PCR for detection of Nipah Chulalongkorn
virus RNA (Ribonucleic acid) from urine University Hospital,
specimens of bats Thailand
Monoclonal antibodies against the nucleocapsid Institute of Veterinary
proteins Sciences, China
Neutralization test for specific detection of NiV National Inst. Inf.
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
Technique Place
antibodies using pseudo typed VSV (Vesicular
Diseases, Japan
stomatitis virus)
Recombinant matrix protein produced in E. University Putra
coli Malaysia, Malaysia
Neutralization assay using VSV pseudo type
particles expressing the F and G proteins of NiV CDC, Atlanta
as target antigens
MAb based antigen capture ELISAs for virus
detection and differentiation between NiV and CDC, Atlanta
Hendra Virus
Antigen capture ELISA using polyclonal
National Institute Inf.
antibodies obtained by DNA (Deoxyribonucleic
Diseases, Japan
acid) immunization
Second generation of pseudo type-based serum National Institute Inf
neutralization assay for NiV antibodies Diseases, Japan
Source: [1].
Table 2. Case fatality rate of NiV infection during outbreaks in different
countries.from 1999–2018.
Reported human Reported Case fatality
Country Year
cases deaths rate (%)
1998–
Malaysia 265 105 39.6
1999
Singapore 1999 11 1 9.1
Bangladesh 2001 13 9 69.0
India 2001 66 45 68.0
2003–
Bangladesh 109 77 70.6
2007
India 2007 5 5 100.0
Bangladesh 2008– 87 74 85.1
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
Reported human Reported Case fatality
Country Year
cases deaths rate (%)
2012
India 2018 19 17 89.0
Source: [4,16].
Malaysia
Febrile encephalitis cases were reported among pig farmers in September
1998. Initial deduction was JE, vaccine imported from Japan was
administered to farmers and people in close contact to pigs. By the end of 1998
only four of 28 samples were tested positive for anti-JE IgM, also, the virus
could not be isolated from postmortem brain tissue of patients. Due to
devastating effect of the outbreak, on 9th March, 1999 the presence of a novel
virus was announced by the ministries of health and agriculture.
Subsequently, the virus was named as Nipah, after the village from where the
virus was first isolated, Kampung Sungai Nipah [24]. The outbreak began
near Ipoh among pig farmers and spread to other major pig rearing areas,
resulting in 265 human cases including 105 deaths [1,24,25].
Singapore Eleven cases and one death among pig abattoir workers was
reported in Singapore between 10–19 March, 1999, due to contact with live
pigs imported from Malaysia during NiV outbreak period [24,26].
Bangladesh
First NiV outbreak was identified in Meherpur district of Bangladesh between
April–May, 2001. Thereafter, districts affected by NiV infection between
January 2003 to February 2013 were: Naogoan, Rajbari, Faridpur, Tangail,
Thakurgaon, Kushtia, Pabna, Natore, Naogaon, Manikgonj, Rajbari,
Faridpur, Gaibandha, Rangpur, Nilphamari, Madaripur, Gopalganj,
Lalmohirhat, Dinajpur, Rangpur, Comilla, Joypurhat, Rajshahi, Gaibandha,
Rajshahi, Pabna, Jhenaidah and Mymensingh. Few districts of Bangladesh
observed repeated outbreaks [1]. A total of 209 human cases of NiV infection
were reported in Bangladesh from April 2001 to March 31, 2012, of which 161
(77%) died [20]. In 2001, 13 cases were diagnosed followed by multiple
outbreaks until 2013, with 193 reported cases. Fatality rate in 2001 was 69%
and in 2013 it increased to 83% which is depicted in Fig. 1 [1].
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
1. Download : Download high-res image (259KB)
2. Download : Download full-size image
Fig. 1. Graph showing number of cases, deaths and case fatality rate in
Bangladesh.
Source: [1].
India
Three outbreaks of NiV have been reported in India since 2001. First
outbreak was reported in Siliguri, West Bengal; between January and
February, 2001. Total 66 cases and 45 deaths were reported in this outbreak
[20,23]. Second outbreak occurred in Nadia, West Bengal in 2007; 30 cases
and 5 deaths were confirmed to be positive through real-time polymerase
chain reaction (RT - PCR) as depicted in Fig. 2 [20,27]. Outbreak in Kerala,
May 2018; reported 17 deaths with high case fatality. First index case was
reported in Perambra, Kozhikode district. The outbreak began with three
members of a family who died after cleaning an old well infected by bats.
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
1. Download : Download high-res image (104KB)
2. Download : Download full-size image
Fig. 2. Epidemic Curve by date of onset Siliguri, India outbreak 2001.
Source: [27].
Philippines
An outbreak of NiV or NiV like virus occurred in the southern part of
Philippines affecting two villages of Mindanao in 2014. Horses were the source
of infection and 17 cases were reported, seven of these were involved with
either butchering activities or consuming horse meat and around 10 horses
were reported to be dead [28].
Diagnosis
Laboratory diagnostic tests of NiV encephalitis consists of detecting anti-
NiV immunoglobulin M (IgM) and IgG antibody in the serum
and cerebrospinal fluid (CSF), with or without viral isolation. Most commonly
used diagnostic method is enzyme-linked immunosorbent assay (ELISA) test,
using monoclonal antibody-based antigen, for virus detection and for
differentiating NiV from Hendra virus [1,6,19,20]. Direct ELISA test was used
to detect anti-NiV-specific IgM, whereas, indirect IgG ELISA was used to
detect the IgG antibody [6,29]. Other methods like serum neutralizing tests
[6,30], RT-PCR for detection of viral RNA from serum, urine, and CSF
[6,16,19,20,30], virus isolation [1,20,30] and nucleic acid amplification tests
are available [1]. Magnetic resonance imaging (MRI) of the brain served as
sensitive diagnostic tool in acute and relapse/late-onset NiV encephalitis, as
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
the diagnostic sensitivity of ELISA was not reliable [6,20]. Different diagnostic
techniques used globally are mentioned in Table 1.
Prevention
Preventive strategies can be incorporated to prevent NiV transmission.
Patient to attendant transmission can be minimized through frequent hand
washing and avoiding sharing of food and bed with patients. Wearing gloves
and masks while handling of dead body is necessary to avoid corpse to human
transmission. If this is not feasible in low and middle income countries at least
thorough hand washing with soap and water immediately after the corpse
contact may prevent disease transmission [13,31]. Nosocomial transmission to
health care workers can be minimized by ensuring proper hand washing
facilities, use of personal protective equipment (PPE) and isolation of
the meningoencephalitis patients during NiV outbreaks [13].
Measures like bamboo skirt method can be used to prevent the contamination
of date palm sap. The method involves covering the shaved part and mouth of
the pot by hanging a bamboo skirt. Other methods include sap branch method
where the shaved part of the tree is covered with its own branches, cloth or
mosquito net [12,32]. Washing or peeling of fruits and thorough hand washing
while having fruits and preparing meals should be followed [33]. Strategies to
improve awareness regarding risk factors and significance of adopting
preventive measures can help in preventing the spread of infection [20].
Various communication strategies like local television or radio channels and
print media were used to create awareness among people [12].
Vaccines
Studies have demonstrated that after challenging with NiV, ferrets and Syrian
hamsters, vaccinated with recombinant vesicular stomatitis (rVSV) expressing
NiV glycoproteins (attachment protein) and F(fusion) protein, showed
complete protection against the lethal NiV infection, while animals in control
group showed characteristic clinical signs of the disease [34,35]. Single dose
rVSV vaccination has demonstrated to be effective when it was administered a
day before the challenge. It has shown to be partially protective when
administered at the early hours following the NiV infection in hamsters [36].
Single dose replication-defective vesicular stomatitis based-vaccine expressing
NiV G and F proteins, also showed complete protection in the Syrian golden
hamster model [37].
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
Effect of the vaccine, G glycoprotein of Hendra virus (HeVsG) has displayed
that ferrets were protected from acute NiV disease for a duration of at least 12
months post vaccination [38].
Immunization of recombinant measles vaccine (rMV) along with the
administration of the same amount of booster dose to both hamsters and
monkeys revealed that, there was no clinical signs of the disease in both the
animals and survived after challenging with NiV after 1 week of second
immunization [39]. Monoclonal antibody (m102.4) against the G glycoprotein
of the NiV, if administered pre-exposure or up to 10 h after exposure has
shown to prevent the disease condition in ferrets [7,25].
Control
After identification of the virus in Malaysia outbreak, agricultural labourers
were shifted from the place contaminated with NiV and suspected farms were
closed [23]. More than a million pigs were culled and strict quarantine
measures on pig movements were imposed [25]. Information regarding the
virus was broadcasted through media [23]. Education about personal safety in
case of contact with pigs and standard operating procedures were developed
for people who were handling the dead bodies of NiV cases [23]. Information,
education and communication in different languages was used to create
awareness in the community [40]. Dissemination of information regarding
NiV through official websites and hotline numbers were undertaken by the
government [23]. Slaughterhouse workers and people involved in handling
and management of pigs were suggested to use PPEs and proper handwashing
techniques [23]. All healthcare workers including relatives of infected persons
were recommended to use PPE as they were more prone to develop infection
[23]. A major control measure during this outbreak, was restricting import of
live pigs through Malaysia [41].
There were more than five rural hospitals in Bangladesh, which reported
maximum number of NiV cases. As mentioned in a commentary, there is a
need for infectious disease control infrastructure in the hospitals. As repeated
episodes of NiV outbreak were seen in Bangladesh during harvesting season of
date palm sap, the government emphasized on avoiding date palm sap or
boiling it for at least ten minutes before consumption [12]. Stringent isolation
procedures were followed at the treatment centers in Kerala, India, and
measures to prevent droplet infection were initiated [16].
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
Treatment
A broad spectrum antibiotic, Ribavirin was the drug of choice in Malaysian
outbreak for treating NiV encephalitis, leading to 36% reduction of mortality
among humans [42]. Ribavirin also delayed the death of NiV infected
hamsters by five days. Administration of chloroquine alone or combined with
ribavirin did not provide any protection against NiV disease [43].
Favipiravir (T-705) demonstrated inhibition of NiV replication and
transcription at the molecular concentration. In Syrian hamster model,
administration of favipiravir orally twice daily or subcutaneously once daily
for 14 days protected the animals [44]. Monoclonal antibody (m102.4) when
administered to African green monkeys twice post exposure to NiV beginning
on day 1, 3 or 5 and again after two days had shown to prevent the disease
condition even after they developed clinical signs of the disease [45].
Supportive treatment remains the most common mode of treatment for acute
Nipah encephalitis. Broad-spectrum antibiotic for nosocomial infections,
prevention of deep venous thrombosis, mechanical
ventilation and anticonvulsants for patients with seizures are some of the
treatment measures given to infected patients [6].
Surveillance
Surveillance helped in analyzing the viral strains and monitoring the changes
of viral factors. Cluster based surveillance helped to identify two types of
Nipah outbreaks with high fatality rate, whereas case based surveillance
identified sporadic NiV introductions in a study done in Bangladesh [46].
Another commentary on policy options for Bangladesh mentioned that early
detection of outbreaks was achieved by setting up a surveillance system in five
hospitals across the NiV belt [12]. A study done in Malaysia during 1999
outbreak conducted surveillance in human health sector, animal health sector
and for reservoir hosts. Three categories were covered under human health
sector such as disease surveillance, patient surveillance and high risk group
surveillance [23]. Data regarding the roosting behavior of bats, their access to
date palm sap and virus sequences among bats at different locations was
collected to give evidence that environmental factors played an important role
in NiV infection spread by Pteropus bats carrying the virus [[47], [48], [49]].
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
Economic burden
The NiV outbreak in Malaysia caused a tremendous economic loss because of
the culling of over 1.1 million pigs to control the outbreak [4]. A case study
done in Malaysia reported lowered standard of living mainly due to lack of
opportunities to work in pig farms. Lack of employment opportunities led to
out-migration of young labour force in affected areas which further
contributed to the economic burden. Out of pocket expenditure did not
contribute to economic burden as there was a robust public health system to
support the patients. [50].
Strength & limitation
This narrative review summarizes the important scientific evidence available
on NiV. Limitation of this literature review was language restriction of
included articles to English.
Conclusion
Varied niv disease pattern in Malaysia–Singapore and Indo–Bangladesh
outbreaks was observed. In Malaysia and Singapore, niv was transmitted
from pig to humans whereas, in Bangladesh the cultural practices of
consuming date palm sap contaminated by the infected bats, led to the
repeated outbreaks. In India outbreak was observed in West Bengal region,
sharing border with Bangladesh, due to spillover of virus from Bangladesh.
The outbreak in Kerala, India started with direct contact of humans with bats
and consequent nosocomial infection. The authors conclude, environmental
factors play a vital role in the emergence of zoonotic disease in humans.
Climatic changes due to factors like drought or floods,
deforestation, urbanization, industrialization on large scale leads to
destruction of animal habitats causing starvation and low immunity,
increasing the viral load in their body, excreted in the secretions of bats,
thereby infecting the fruits, animals or humans who come in contact with
them. Hence, it is necessary to adopt ‘one health’ approach by considering
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
human, animal and environmental health into the same context to address this
particular disease. The niv outbreaks in Malaysia and Singapore in 1999
ended with the mass culling of pigs and did not recur, whereas, multiple
outbreaks have occurred in India and Bangladesh since 2001. The reasons for
multiple outbreaks may be varied, nevertheless, low healthcare system
capacity and lack of a robust surveillance strategy contribute substantially to
it. Interdisciplinary and multi sectoral approach is vital in preventing the
emergence of niv. Along with these aspects it is necessary to undertake
rigorous research for developing vaccines and medicines to prevent and treat
niv.
Over the past two decades, the Nipah virus pathogenesis along with the transmission
have been much well understand due to extensive research.
The understanding is going to be more advanced in the decade to come.
It is important to note in this regard that the practical utility of this understanding
will be reflected in the entry of Nipah virus vaccines into clinical trial in humans and
modification of risk factors in order to prevent infection.
Further, such understanding will be great aid in developing techniques along with
therapeutic for treatment of infected subjects for reduction of morbidity as well as
mortility.
Result
Computational miRNAs prediction depends on two approaches: ab-intio based and
homology based. Evolutionary conservation tracing is the main motive of homology
based approach and thus having limitation in finding novel miRNAs. But ab-intio
based approach which search for hair-pin loop structure topology in genomic
sequence is more of significance in locating novel pre-miRNAs and hence the
derivative miRNAs because pre-miRNAs tends to form hair-pin loop structures
during their biogenesis [53-55].
In our study we also used ab-intio based program, VMir for scanning the NiV
genome for possible pre-miRNAs prediction. Genome sequence was analysed on
both strands (Direct/Reverse) during pre-miRNAs prediction. We got nine pre-
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
miRNAs (Fig. 1) with high score at stringent parameters (min. hairpin size: 70, min.
score: 115 and min. window count: 35 in VMir viewer) as previously described [45]
to filter out imprecise candidate pre-miRNAs. Six pre-miRNAs predicted were on
direct strand and three were on reverse strand. The length of pre-miRNAs was in
the range 76-165 nucleotide. The genomic position, Vmir score and rank were
shown in Table 1.
Figure 1
Predicted pre-miRNAs structures. Hairpin loop structures of NiV predicted by m
fold, 5' arm of mature miRNAs indicated by cyan, 3' arm by pink whereas dark
green show overlapping region
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
Table 1
pre-miRNAs predicted by VMir False-positive pre-miRNAs prediction is common
limitation to all ab-intio prediction programs because of selection of the pseudo hair
pin loops structures [56, 57], therefore to validate and find reliable results we
examined all nine predicted pre-miRNAs by SVM based virus specific tool,
ViralmiR. All nine pre-miRNAs were found to be potential in yielding miRNAs.
Minimum free energy (MFE) calculation of pre-miRNAs sequence during folding is
one of the features that confer stability values to it [58]. We used Mfold web server
for MFE calculation (Table 2) and secondary structure prediction of pre-miRNAs.
Table 2
Potential pre-miRNAs validated by ViralMir and Minimum Free Energy (MFE)
calculated by Mfold After initial identification and validation, pre-miRNAs
sequences were subjected to Mature Bayes for retrieving the small mature miRNAs.
Large pre-miRNAs sequences were cleaved to short mature miRNAs of 22
nucleotide length. We got eighteen mature miRNAs from nine pre-miRNAs
sequences on 5’ and 3’ stem location as shown in Table 3. Because one or both
strands can serve as mature miRNA molecule depending on the assembly of RISC
complex [59], we kept both for further analysis.
Table 3
Mature miRNAs sequences predicted by MatureBayes miRNAs exerts their effects
by targeting the mRNA of protein coding gene of the cell, thus predicting the target
of miRNAs directly revealed their function in the cell [60]. Computational
predictions of target depend on the Watson-Crick base pairing between miRNA and
mRNA molecule and mostly used seed pairing approach [61, 62]. Target prediction
by miRDB for all mature miRNAs gave 769 target genes (supplementary Table) in
human genome. The server uses the MirTarget algorithm, which is based on 7-mer
seeding approach and custom predict miRNAs targets in human gene’s 3’ UTRs.
We selected target genes with miRDB score >80 because a predicted target with
prediction score >80 is most likely to be real and not required any other supporting
evidence [49].
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
Gene ontology analysis of the target genes by PANTHER revealed their involvement
in different clusters of molecular functions, cellular component, biological process
and pathway. The clustering approach proved to be significant in determination
target gene molecular function (Fig. 2a), cellular component (Fig. 2b), biological
process (Fig. 2c) and pathway (Fig. 2d) of large data set at once. In molecular
function cluster target genes products were depicted to play role in translation
regulator activity (GO:0045182), signal transducer activity (GO:0004871) binding
(GO:0005488) and receptor activity (GO:0004872), which shows that inhibition of
these gene product might lead to abnormal state in body. Biological process cluster
classification have proteins which are involved in immune system response
(GO:0002376), response to stimulus (GO:0050896), biological adhesion
(GO:0022610) and localization (GO:0051179) etc. Biological processes mentioned
are significant for defense against viral infection. Pathway clusters analysis showed
pathways that can mediate the disease in human. Interference in pathways like
Axon guidance mediated by netrin (P00009), Axon guidance mediated by
semaphorins (P00007), T cell activation (P00053), Nicotinic acetylcholine receptor
signaling pathway (P00044), Alzheimer disease-amyloid secretase pathway (P00003)
and Parkinson disease (P00049) can lead to acute encephalitis. Cellular component
classification also suggest the target gene products are part of synapse
(GO:0045202), cell junction (GO:0030054), extracellular region (GO:0005576) and
organelle (GO:0043226) etc. Significant results obtained through GO analysis
prompt us to uncover the encephalitis disease genes among the 769 target genes.
Manual screening of target genes with NCBI Gene database and OMIM
encephalitis disease genes identified five target genes. Literature mining results
(Table 4.) of five target genes discovered their role in normal brain functioning and
disorders.
Table 4
Screened target genes role and associated disorders
Go Analysis of target genes: Target genes were found to be involved in molecular
function (2a), cellular component (2b), biological process (2c) and pathways (2d)
Comparative computational study of Nipah Virus Drugs
Comparative computational study of Nipah Virus Drugs
TLR3 (Toll Like Receptor 3) expressed in human neurons during innate immune
response confirmed its role in the host defense against viruses. It works by
recognizing the molecular patterns specific to microorganisms [63]. Degradation of
TJP1 (Tight Junction Protein 1) during Japanese encephalitis virus and human
Immunodeficiency virus-1 infection caused breached in blood-brain barrier (BBB)
and hence results in neurological symptoms leads to encephalitis [64, 65]. NOTCH2
(Neurogenic Locus Notch Homolog Protein 2) participates in neurogenesis and is
key protein in adult brain, impairment in signaling of NOTCH2 contribute to
neurological disease manifestation [66, 67]. The expression evidences of FHL1 (Four
And A Half LIM Domains 1) in brain tissue and interaction with PLEKHG2
(Pleckstrin Homology And RhoGEF Domain Containing G2) revealed its role in
brain cells [68]. FHL1 mutation lead to muscular dystrophy is main disorder related
to this target gene [69]. Lastly, GRIA3 (Glutamate Ionotropic Receptor AMPA
Type Subunit 3) are the predominant excitatory neurotransmitter receptors in the
mammalian brain and are activated in a variety of normal neurophysiologic
processes. Diseases associated with GRIA3 include mental retardation and
Rasmussen encephalitis [70, 71].
Comparative computational study of Nipah Virus Drugs
You might also like
- Microorganisms As Bio Indicators and BiosensorsDocument42 pagesMicroorganisms As Bio Indicators and BiosensorsJAFFER YOUSUF85% (13)
- Snurfle Meiosis Another WSDocument2 pagesSnurfle Meiosis Another WSAdriana IzquierdoNo ratings yet
- Prediction of Potential Commercially Inhibitors Against Sars-Cov-2 by Multi-Task Deep ModelDocument8 pagesPrediction of Potential Commercially Inhibitors Against Sars-Cov-2 by Multi-Task Deep ModelamyzeevshelaNo ratings yet
- In Silico Identification of Clinically Approved Medicines Against The Main Protease of Sars-Cov-2, Causative Agent of Covid-19Document17 pagesIn Silico Identification of Clinically Approved Medicines Against The Main Protease of Sars-Cov-2, Causative Agent of Covid-19Rakesh DavellaNo ratings yet
- Virtual Screening of Phytochemical Compounds As Potential Inhibitors Against HIV-1 Resistance To Protease InhibitorDocument6 pagesVirtual Screening of Phytochemical Compounds As Potential Inhibitors Against HIV-1 Resistance To Protease InhibitorZoya AmjadNo ratings yet
- Marroqui2008 Efecto de Inhinidor IPNVDocument7 pagesMarroqui2008 Efecto de Inhinidor IPNVandrea nettle bareaNo ratings yet
- Literature Review On PCRDocument6 pagesLiterature Review On PCRafdtzfutn100% (1)
- Clarke - 2002 - Molecular Diagnosis of HIVDocument7 pagesClarke - 2002 - Molecular Diagnosis of HIVSebastianNo ratings yet
- Biochemical and Biophysical Research CommunicationsDocument6 pagesBiochemical and Biophysical Research CommunicationslilisasaiNo ratings yet
- 1 s2.0 S0377123720300988 MainDocument6 pages1 s2.0 S0377123720300988 MainautomationenggNo ratings yet
- 4699-Article Text-8003-1-10-20220919Document8 pages4699-Article Text-8003-1-10-20220919Efrin SitumorangNo ratings yet
- 42 Han 2012 BMCBioinformaticsDocument10 pages42 Han 2012 BMCBioinformaticsrammhtoNo ratings yet
- Computational Analysis of Protein Interactions Between HIV-1 and Homo SapiensDocument5 pagesComputational Analysis of Protein Interactions Between HIV-1 and Homo SapiensFaiza MalikNo ratings yet
- Oral Antiviral Newsletter Yan Versi 2 - Dec 2021Document7 pagesOral Antiviral Newsletter Yan Versi 2 - Dec 2021YanMardianNo ratings yet
- Sadianaz 2018Document25 pagesSadianaz 2018Laísa BarséNo ratings yet
- Potential Therapeutic Agents For COVID-19 Based On The Analysis of Protease and RNA Polymerase DockingDocument7 pagesPotential Therapeutic Agents For COVID-19 Based On The Analysis of Protease and RNA Polymerase DockingJoseGarciaNo ratings yet
- 2020-Joshi-In Silico Screening of Natural Compounds Against COVID-19 by Targeting Mpro and ACE2 Using Molecular DockingDocument8 pages2020-Joshi-In Silico Screening of Natural Compounds Against COVID-19 by Targeting Mpro and ACE2 Using Molecular DockingAdriana SantosNo ratings yet
- SPIN BindingSiteAnalysisOfPotentialDocument6 pagesSPIN BindingSiteAnalysisOfPotentialnishiNo ratings yet
- Biochem Term Paper Reporting - DISCUSSIONDocument1 pageBiochem Term Paper Reporting - DISCUSSIONShakira AntiquinaNo ratings yet
- Bioorganic & Medicinal ChemistryDocument9 pagesBioorganic & Medicinal ChemistryJunaid KhanNo ratings yet
- tmp9EA0 TMPDocument5 pagestmp9EA0 TMPFrontiersNo ratings yet
- Test 11Document14 pagesTest 11CiprianNo ratings yet
- Dissertation HCVDocument8 pagesDissertation HCVWriteMyPaperForMeIn3HoursCanada100% (1)
- Iddt 226ap2Document8 pagesIddt 226ap2pooja pandeyNo ratings yet
- Yunnan Key 2014Document9 pagesYunnan Key 2014crpen87No ratings yet
- Comparing Genetic Evolutionary Algorithms On Three Enzymes of HIV-1: Integrase, Protease, and Reverse TranscriptomeDocument13 pagesComparing Genetic Evolutionary Algorithms On Three Enzymes of HIV-1: Integrase, Protease, and Reverse TranscriptomeAI Coordinator - CSC JournalsNo ratings yet
- Sars Cov 2 Tratamentos Artigo NatureDocument6 pagesSars Cov 2 Tratamentos Artigo NaturesandraNo ratings yet
- A Antisense Technology 2Document2 pagesA Antisense Technology 2Gourav JainNo ratings yet
- CORVELVA Metagenomic Analysis Report On Gardasil 9Document9 pagesCORVELVA Metagenomic Analysis Report On Gardasil 9Gene XeneNo ratings yet
- Prediction of Interactions Between Hiv-1 and Human ProteinsDocument5 pagesPrediction of Interactions Between Hiv-1 and Human ProteinsDipyaman KunduNo ratings yet
- Iin Silicoi Screening and Molecular Docking of Bioactive Agents Towards Human CoronavirusDocument5 pagesIin Silicoi Screening and Molecular Docking of Bioactive Agents Towards Human CoronavirusSuresh KumarNo ratings yet
- 10 1016@j Molstruc 2020 129433Document25 pages10 1016@j Molstruc 2020 129433sananaveed.akberNo ratings yet
- Emerging Therapies in Hepatitis C. Dawn of The Era of The Direct Acting Antivirals (2011)Document14 pagesEmerging Therapies in Hepatitis C. Dawn of The Era of The Direct Acting Antivirals (2011)drheayNo ratings yet
- Is Oseltamivir Suitable For Fighting Against COVID-19 in Silico Assessment, in Vitro and Retrospective StudyDocument1 pageIs Oseltamivir Suitable For Fighting Against COVID-19 in Silico Assessment, in Vitro and Retrospective Studychristian bataNo ratings yet
- CH 15. Understanding The Statistical Analysis of Resistance Data - Antiretroviral Resistance in Clinical Practice - NCBI BookshelfDocument6 pagesCH 15. Understanding The Statistical Analysis of Resistance Data - Antiretroviral Resistance in Clinical Practice - NCBI BookshelfntnquynhproNo ratings yet
- Inhibition of The SARS-CoV-2 RNA-Dependent RNA Polymerase by Natural BioactiveDocument13 pagesInhibition of The SARS-CoV-2 RNA-Dependent RNA Polymerase by Natural BioactiveLuis MartinezNo ratings yet
- Construction and Application of A Protein Interaction - 2014 - Molecular - CelluDocument14 pagesConstruction and Application of A Protein Interaction - 2014 - Molecular - CelluTanIsmNo ratings yet
- Drugs For Hepatitis CDocument3 pagesDrugs For Hepatitis CIrvan PutraNo ratings yet
- Tied Down by Its Own Receptor: News & ViewsDocument2 pagesTied Down by Its Own Receptor: News & ViewsSimoné S SimonNo ratings yet
- Dissertation RT PCRDocument5 pagesDissertation RT PCRBuyAcademicPapersSingapore100% (1)
- Molecular Docking Analysis of Peptide-Based Antiviral Agents Against Sars-Cov-2 Main Protease: An Approach Towards Drug RepurposingDocument12 pagesMolecular Docking Analysis of Peptide-Based Antiviral Agents Against Sars-Cov-2 Main Protease: An Approach Towards Drug RepurposinguttamNo ratings yet
- Using Improved Non Ri - Maprec Assay To Detect Virulence Mutations in Poliomyelitis Vaccine Viruses: Advantages Over 40 TestDocument7 pagesUsing Improved Non Ri - Maprec Assay To Detect Virulence Mutations in Poliomyelitis Vaccine Viruses: Advantages Over 40 TestBa Trần VănNo ratings yet
- Bepridil Is Potent Against SARS-CoV-2 in VitroDocument28 pagesBepridil Is Potent Against SARS-CoV-2 in VitrosovalaxNo ratings yet
- Policresulen, A Novel NS2BNS3 Protease Inhibitor, PDFDocument11 pagesPolicresulen, A Novel NS2BNS3 Protease Inhibitor, PDFFernando cisneros prietoNo ratings yet
- tmpB794 TMPDocument13 pagestmpB794 TMPFrontiersNo ratings yet
- Potential Antiviral Agents for Coronaviruses: Compounds, Herbal Products, and Drug TargetsFrom EverandPotential Antiviral Agents for Coronaviruses: Compounds, Herbal Products, and Drug TargetsNo ratings yet
- Molecules Paper - CompressedDocument15 pagesMolecules Paper - CompressedkaviNo ratings yet
- 1 s2.0 S147692712200055X MainDocument18 pages1 s2.0 S147692712200055X Mainjipir64332No ratings yet
- 1 s2.0 S0223523421007522 MainDocument16 pages1 s2.0 S0223523421007522 Mainjipir64332No ratings yet
- Use of Monoclonal Antibodies Against Hendra and Nipah Viruses in An Antigen Capture ElisaDocument8 pagesUse of Monoclonal Antibodies Against Hendra and Nipah Viruses in An Antigen Capture ElisaThamizh Kumaran RNo ratings yet
- 2020 01 29 20019448v1 FullDocument27 pages2020 01 29 20019448v1 Fulljhonny12321No ratings yet
- Vaccine: Mitchell Tyler, Ebenezer Tumban, Agnieszka Dziduszko, Michelle A. Ozbun, David S. Peabody, Bryce ChackerianDocument8 pagesVaccine: Mitchell Tyler, Ebenezer Tumban, Agnieszka Dziduszko, Michelle A. Ozbun, David S. Peabody, Bryce ChackerianElizabeth CollinsNo ratings yet
- Journal of Molecular Graphics and ModellingDocument13 pagesJournal of Molecular Graphics and ModellingPencari IlmuNo ratings yet
- Heterotypic Interactions Drive Antibody Synergy Against A Malaria Vaccine CandidateDocument12 pagesHeterotypic Interactions Drive Antibody Synergy Against A Malaria Vaccine CandidateSamer ShamshadNo ratings yet
- Srep 42769Document12 pagesSrep 42769ara.lv007No ratings yet
- Journal Pre-Proof: Phytomedicine PlusDocument35 pagesJournal Pre-Proof: Phytomedicine PlusMohammed Shuaib AhmedNo ratings yet
- Docking Study of Naringin Binding With COVID-19 Main ProteaseDocument8 pagesDocking Study of Naringin Binding With COVID-19 Main ProteaseLuis MartinezNo ratings yet
- s12900-018-0085-4Document13 pagess12900-018-0085-4Daniel FelipeNo ratings yet
- Virology Journal: Virus Detection and Identification Using Random Multiplex (RT) - PCR With 3'-Locked Random PrimersDocument11 pagesVirology Journal: Virus Detection and Identification Using Random Multiplex (RT) - PCR With 3'-Locked Random PrimersMarie Angeline CletoNo ratings yet
- Infant HIV TestsDocument5 pagesInfant HIV TestsProf Rakesh SharmaNo ratings yet
- In-Silico Pharmacophoric and Molecular Docking-Based Drug Discovery Against The Main Protease (M) of Sars-Cov-2, A Causative Agent Covid-19Document9 pagesIn-Silico Pharmacophoric and Molecular Docking-Based Drug Discovery Against The Main Protease (M) of Sars-Cov-2, A Causative Agent Covid-19sonyekanugrahaNo ratings yet
- Epilepsia - 2002 - Anderson - Children Versus Adults Pharmacokinetic and Adverse Effect DifferencesDocument7 pagesEpilepsia - 2002 - Anderson - Children Versus Adults Pharmacokinetic and Adverse Effect DifferencesDAMBALENo ratings yet
- PGY PR Attendance ReportDocument4 pagesPGY PR Attendance ReportDAMBALENo ratings yet
- Pgy PR Sessional-Iii MarksheetDocument3 pagesPgy PR Sessional-Iii MarksheetDAMBALENo ratings yet
- BLUEPRINT - Basic Principles of Toxicology Elective TYDocument2 pagesBLUEPRINT - Basic Principles of Toxicology Elective TYDAMBALENo ratings yet
- PC-I, FY 2nd Sessional (PR) ReportDocument13 pagesPC-I, FY 2nd Sessional (PR) ReportDAMBALENo ratings yet
- PH-I Sessional 2. Exam MARKSHEETDocument3 pagesPH-I Sessional 2. Exam MARKSHEETDAMBALENo ratings yet
- 8TH Sem Project MarksheetDocument5 pages8TH Sem Project MarksheetDAMBALENo ratings yet
- SR - NO. Name of The Student Contact No. Contact No. Course DateDocument1 pageSR - NO. Name of The Student Contact No. Contact No. Course DateDAMBALENo ratings yet
- Tax Invoice: Shipping Address: Sold By: Invoice DetailsDocument1 pageTax Invoice: Shipping Address: Sold By: Invoice DetailsDAMBALENo ratings yet
- Blue Print PHARMACOLOGY-I (1) - 2Document1 pageBlue Print PHARMACOLOGY-I (1) - 2DAMBALENo ratings yet
- Ideal Institute of Pharmacy - Posheri - Wada B-Pharmacy Ii ND Year 2020-21Document12 pagesIdeal Institute of Pharmacy - Posheri - Wada B-Pharmacy Ii ND Year 2020-21DAMBALENo ratings yet
- Pharmaceutics - I (Theory) Set-ADocument1 pagePharmaceutics - I (Theory) Set-ADAMBALENo ratings yet
- University of Mumbai: Fourth Year B. of Pharmacy (Sem VIII) (CBCS)Document1 pageUniversity of Mumbai: Fourth Year B. of Pharmacy (Sem VIII) (CBCS)DAMBALENo ratings yet
- Pradnya - Sheet1Document1 pagePradnya - Sheet1DAMBALENo ratings yet
- BLUEPRINT - Basic Principles of Toxicology Elective TYDocument2 pagesBLUEPRINT - Basic Principles of Toxicology Elective TYDAMBALENo ratings yet
- Comparative Computational Study On Nipah Virus DrugsDocument10 pagesComparative Computational Study On Nipah Virus DrugsDAMBALENo ratings yet
- Comparativecomputational Study On Nipah Virus DrugsDocument10 pagesComparativecomputational Study On Nipah Virus DrugsDAMBALENo ratings yet
- Not Return Teachers Book ListDocument1 pageNot Return Teachers Book ListDAMBALENo ratings yet
- Website: WWW - Niperhyd.ac - in / WWW - Niperhyd.edu - In: TH THDocument24 pagesWebsite: WWW - Niperhyd.ac - in / WWW - Niperhyd.edu - In: TH THDAMBALENo ratings yet
- Siddhi Bhagwan Dalvi ....Document5 pagesSiddhi Bhagwan Dalvi ....DAMBALENo ratings yet
- Teaching AdvertisementDocument9 pagesTeaching AdvertisementDAMBALENo ratings yet
- Global Celiac Disease CD Market InsightsDocument3 pagesGlobal Celiac Disease CD Market InsightsericinsfNo ratings yet
- Controlled Release Technology and Design of Oral Controlled Released Dosage Forms Design and Scale Up of Drag Granulation ProcessDocument8 pagesControlled Release Technology and Design of Oral Controlled Released Dosage Forms Design and Scale Up of Drag Granulation ProcessYahya IsiedNo ratings yet
- O'Toole Et Al. (2017) Next Generation Probiotics Probiotics To Live BiotherapeuticsDocument19 pagesO'Toole Et Al. (2017) Next Generation Probiotics Probiotics To Live BiotherapeuticsTahir AliNo ratings yet
- Plant Immunology Lecture 9Document30 pagesPlant Immunology Lecture 9Lavander BlushNo ratings yet
- Top Ten Pharma Financials 2011Document136 pagesTop Ten Pharma Financials 2011Harjyot RandhawaNo ratings yet
- Unit 2 Part 2: Transgenic Animals Transgenic Fish Animal As BioreactorsDocument43 pagesUnit 2 Part 2: Transgenic Animals Transgenic Fish Animal As BioreactorsPraveen KumarNo ratings yet
- Classical (Mendelian) GeneticsDocument32 pagesClassical (Mendelian) GeneticsKOMAL FATIMANo ratings yet
- Cell Therapy: CGMP Facilities and Manufacturing: Mini ReviewDocument6 pagesCell Therapy: CGMP Facilities and Manufacturing: Mini ReviewMajin BooNo ratings yet
- 2 722597121924006461Document286 pages2 722597121924006461Shahul HameedNo ratings yet
- Lab 1Document1 pageLab 1AzharNo ratings yet
- Lecture 1: An Overview: Marine Biotechnology at Undip and Review of Undip-Ucsc CollaborationDocument52 pagesLecture 1: An Overview: Marine Biotechnology at Undip and Review of Undip-Ucsc CollaborationsaniyatlyNo ratings yet
- Linkage and Genetic Mapping EukaryotesDocument66 pagesLinkage and Genetic Mapping EukaryotesSITI BAZILAH BINTI BILAK KPM-GuruNo ratings yet
- Enzyme: Oleh Yana Cahyana Stp.,Dea.,Ph.DDocument21 pagesEnzyme: Oleh Yana Cahyana Stp.,Dea.,Ph.DDETA HARTININo ratings yet
- Lecture 01Document15 pagesLecture 01Tanvir FahimNo ratings yet
- The Study of Life BiologyDocument6 pagesThe Study of Life BiologyJokher BaliliNo ratings yet
- HB 1927 1090923 LL Quantinova Probe RT PCR Kit 0315 WWDocument4 pagesHB 1927 1090923 LL Quantinova Probe RT PCR Kit 0315 WWnbiolab6659No ratings yet
- Bio Two Ses Chapter 6Document12 pagesBio Two Ses Chapter 6azizrafeeqNo ratings yet
- Kuliah S2 Transport IntraselulerDocument27 pagesKuliah S2 Transport IntraselulerDwi Retna LestariNo ratings yet
- Pathology of The Bile Duct 2017 - Yasuni Nakanuma PDFDocument215 pagesPathology of The Bile Duct 2017 - Yasuni Nakanuma PDFHîrjoabă IoanNo ratings yet
- Name: - PeriodDocument3 pagesName: - PeriodMia HopkinsNo ratings yet
- Biology 102 SyllabusDocument2 pagesBiology 102 Syllabusapi-285160591No ratings yet
- AQA Biology 2 Revision Notes PDFDocument31 pagesAQA Biology 2 Revision Notes PDFRajashree MuNo ratings yet
- (Methods in Molecular Biology 1644) Vladimir V. Didenko (Eds.) - Fast Detection of DNA Damage - Methods and Protocols-Springer New York (2017) PDFDocument213 pages(Methods in Molecular Biology 1644) Vladimir V. Didenko (Eds.) - Fast Detection of DNA Damage - Methods and Protocols-Springer New York (2017) PDFMauro Porcel de PeraltaNo ratings yet
- NCM 212 - Drug Approval ProcessDocument8 pagesNCM 212 - Drug Approval ProcessLYRIZZA LEA BHEA DESIATANo ratings yet
- Transient Reprogramming of Crop Plants For Agronomic PerformanceDocument16 pagesTransient Reprogramming of Crop Plants For Agronomic PerformanceSELNo ratings yet
- Artikel Kesehatan Dalam Bahasa Inggris Dan Terjemahannya TerbaruDocument3 pagesArtikel Kesehatan Dalam Bahasa Inggris Dan Terjemahannya TerbaruRafaelDimasRizky67% (3)
- Clonagem Animal A Sobrevivência Dos Mais Aptos 2012Document19 pagesClonagem Animal A Sobrevivência Dos Mais Aptos 2012Felipe JuniorNo ratings yet
- Topic 3.2 Karyogram PracticeDocument2 pagesTopic 3.2 Karyogram PracticeAleksandra LukanovskaNo ratings yet