Professional Documents
Culture Documents
NakatoIJP Volume6 Issue9 Pages8215-8223
NakatoIJP Volume6 Issue9 Pages8215-8223
Uploaded by
Siti HumairahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NakatoIJP Volume6 Issue9 Pages8215-8223
NakatoIJP Volume6 Issue9 Pages8215-8223
Uploaded by
Siti HumairahCopyright:
Available Formats
http:// ijp.mums.ac.
ir
Original Article (Pages: 8215-8223)
Analysis of Respiratory Behavior and Clinical Parameters for
Successful Extubation in Premature Infants
*Adriane Muller Nakato1, Regina P. G. V. Cavalcante da Silva1, Nelson Rosario Filho11
1
Department of Pediatrics, Hospital de Clínicas, Federal University of Paraná, Curitiba, Brazil.
Abstract
Background
The weaning process is complex and needs to be done carefully. The success of extubation in
premature babies is associated with brain maturity and adequate function of the lungs. We aimed to
identify the ventilator parameters and clinical conditions related to extubation success and failure in
premature infants.
Materials and Methods
This is an observational study, analytical and non-comparative cohort. We selected all premature
infants, into inclusion criterion, admitted to the Neonatal Intensive Care Unit (NICU) of Hospital de
Clínicas, Curitiba, Brazil in Invasive mechanical ventilation (IMV). The fifty-one premature infants
were evaluated every day until tracheal extubation and the data of the day of extubation were used.
Results
Thirty-nine premature infants had extubation success and the majority of them 32(82.05%) were
appropriated for gestational age (AGA). The parameters that showed a statistical difference between
success and failure group were Positive end-expiratory pressure (p = 0.03), plate pressure (p = 0.03),
Partial pressure oxygen (p = 0.04), pH (p = 0.04), end-tidal CO2 (p = 0.01) and heart rate (p = 0.04).
The use of caffeine periextubation and the permanence in Continuous positive airway pressure
(CPAP) during the post-extubation period was higher in the success group (46.15% and 87.18%,
respectively). The presence of piratory distress syndrome (RDS) was high in both groups, success
group, 82.05% and failure group 100%.
Conclusion
The pressure values, the arterial blood gas analyses, and capnometry are important parameters to
evaluate in the weaning process, checking these values closer to reference values. Supports before and
after endotracheal extubation, such as the use of caffeine and CPAP, are important to avoid the need
for reintubation.
Key Words: Brazil, Endotracheal extubation, Infants, Neonatal Prematurity.
*Please cite this article as: Nakato AM, Cavalcante da Silva R, Rosario Filho N. Analysis of Respiratory
Behavior and Clinical Parameters for Successful Extubation in Premature Infants. Int J Pediatr 2018; 6(9): 8215-
23. DOI: 10.22038/ijp.2018.31384.2774
*Corresponding Author:
Adriane Muller Nakato, Address: Rua General Carneiro 181, 80060-900 Curitiba, Brazil.
Email: drmsrezaii@yahoo.com
Received date: Mar.10, 2018; Accepted date: Apr. 22, 2018
Int J Pediatr, Vol.6, N.9, Serial No.57, Sep. 2018 8215
Ventilator Weaning in Premature Infants
1- INTRODUCTION other factors may influence the success of
extubation, such as weight, gestational age,
The mechanical ventilation (MV) is
length of MV, type of respiratory support
considered an advantage in neonatal
used after endotracheal tube removal,
medicine, especially in extremely preterm
medications used prior to extubation, for
infants (1). However, there is progress in
example, caffeine and surfactant
the non-invasive respiratory support to
administration (12, 13). There are
minimize the injuries caused by invasive
recommendations and protocols in the
mechanical ventilation (IMV). Most
weaning process for adults, but in pediatric
premature infants require endotracheal
and neonatal patients this information is
intubation for a long time, and the longer
still not clear. This study aimed to identify
this time in the IMV the higher the
the ventilator parameters and clinical
morbidity and mortality, so that extubation
conditions related to extubation success
is indicated as soon as possible (1, 2). In
and failure in premature infants and thus,
2010 the World Health Organization
prevent mortality and morbidity risk in
(WHO) estimated 14.5 million babies were
these babies and reduce hospital costs.
born preterm, it represented a preterm birth
rate of 11.1% (3). The mortality rate
2- MATERIALS AND METHODS
increases with the decrease of gestational
age, but medical innovations can decrease 2-1. Method
this rate (3, 4). This was an observational study, an
The weaning process is complex and needs analytical and non-comparative cohort,
to be done carefully. Before the conducted to investigate the respiratory
endotracheal tube is removed, the parameters and clinical conditions
ventilator is gradually weaned until associated with extubation success in
spontaneous respiration commences. Some premature babies admitted in the neonatal
evaluation methods can help to monitor intensive care unit (NICU) of Hospital de
this transition from the ventilator to Clínicas, Curitiba, Brazil from July 2014
ambient air, as blood gas parameters, to November 2016. The study was
oxygen saturation, and ventilator settings. approved by the Ethics Committee of the
Extubation success is considered by many Federal University of Parana, Curitiba,
authors without reintubation within 24 to Brazil. All parents were informed and
72 hours (5–9). The decision to remove the formally agreed to have their infants
MV is based on the clinical experience of included in the study.
the medical team, and there is no protocol The premature infants were selected
that could guide clinicians during this according to the gestational age (between
weaning period, which is why it may 24 and 36 weeks + 6 days), and in the
sometimes be considered successful or presence of invasive mechanical
failed by some researchers (1, 10). ventilation (IMV) on the first day in
In general, extubation process begins when NICU. Premature infants with neurological
the respiratory insufficiency that caused impairment, airway malformation,
the indication to MV starts to improve and accidentally extubated, transferred to other
the premature infants are hospitals, early death, big instabilities and
hemodynamically stable, with spontaneous those who we could not obtain the consent
breathing, good ventilation, and from their parents were excluded from this
oxygenation (9, 11). The success of study. A non-probabilistic sample was
extubation in premature babies is used, in the convenience and systematic
associated with brain maturity and form that includes all the premature
adequate function of the lungs, but some newborns in IMV within the inclusion and
Int J Pediatr, Vol.6, N.9, Serial No.57, Sep. 2018 8216
Nakato et al.
exclusion criteria. The intubation criteria syndromes, irregular breathing frequency
followed the routine practice manual of the and accidentally extubated infants were
NICU of the Clinical Hospital of the excluded. For blood gas analysis,
Federal University of Paraná in 2014 (14), heparinized arterial blood samples from
and considered these criteria: the radial artery were used and analyzed
with the GEM Premier equipment 3000®
Recurrent apnea associated with
(Instrumentation Laboratory, Lexington,
bradycardia (<80 to 100/min),
MA), which was calibrated daily. The end-
requiring a ventilation mask more
tidal of carbon dioxide (EtCO2) in the
than once every 12 hours;
exhaled air was measured by a mainstream
Hypoventilation with pH < 7.25 and portable Capnometer Monitor (EMMA
Partial pressure oxygen [PaCO2] > Emergency Capnometer, Phase in AB,
55-60 mmHg; Danderyd, Sweden) placed between the
Hypoxemia with PaO2< 50 with an endotracheal tube and the circuit of the
inspired fraction of oxygen (FiO2) in mechanical ventilator.
70%;
The values of heart rate and oxygen
The anticipation of imminent
saturation were used in the pulse oximetry
cardiovascular collapse (as in severe
monitor (OxiMax® N-560, Covidien,
sepsis), or ventilatory instability
Mansfield, USA), and for the temperature
(frequent unsaturation in Persistent
values they were used from the medical
Pulmonary Hypertension [PPH]);
records. The analyses started on the first
Frequent apneas, even without the day of the mechanical ventilation until the
need for Positive Pressure removal of the endotracheal tube and the
Ventilation (PPV), in a newborn with data from the day of extubation were used
necrotizing enterocolitis and the need and only the first attempt at extubation was
for ventilatory support, periventric included. Successful extubation was
Intraventricular hemorrhage; and considered without reintubation within 72
Sepsis. hours.
The criterion for extubation also followed
2-2. Ethics Approval
those recommended by the manual of the
routine practice of the NICU/ HC-UFPR This study was approved by Ethics
(the neonatal intensive care unit / Hospital Committee of the Federal University of
de Clínicas- Universidade Federal do Parana, Curitiba, Brazil.
Paraná) of 2014, except those with
2-3. Statistical Analysis
accidental extubation and the decision of
the clinical team to maintain the The data were analyzed using the SPSS
extubation. Statistical package®, version 10.0. The
premature Infants were divided into two
The criteria for extubation are: having a groups, successful and failed extubation.
regular spontaneous breathing and cough Student’s paired t-test was used to analyze
reflex; FiO2 ≤ 40% to maintain saturation the differences between groups, for
≥ 90%; the peak inspiratory pressures continuous variables. The Mann-Whitney
(PIP) <15-18 cm H2O and respiratory rate test was used for the abnormally
of 15-20/min; pH above 7.25 and PaCO2 distributed variable. The data are presented
below 50 mmHg (14). The ventilator used as mean (± standard deviation) or median
was Puritan Bennett™ 840®, Carlsbad, (range). A p-value < 0.05 was considered
California. Premature infants with severe significant.
hemodynamic instability, airway
congenital malformation, neurological
Int J Pediatr, Vol.6, N.9, Serial No.57, Sep. 2018 8217
Ventilator Weaning in Premature Infants
3- RESULTS associated with extubation failure or died
before the first attempt of extubation. Only
Between July 2014 and November
one infant was large for gestational age
2016, 507 premature infants with
(LGA) (Figure.2). The ventilatory
gestational age between 24 to 36 weeks
threshold and arterial blood gas parameters
were born, 177 premature infants were in
that showed statistical differences between
MV and 125 fitted in exclusion criteria.
successful and failed groups were positive
Fifty-one premature infants were into
end-expiratory pressure [PEEP] (p = 0.03),
inclusion criteria and were selected for the
plate pressure (p = 0.03), PaCO2 (p =
research. Some reasons for the exclusion
0.04), pH (p = 0.04), and end-tidal carbon
after the intubation were the transfer to
dioxide [EtCO2] (p = 0.01). Infants who
others hospitals, malformation, babies with
failed extubation had lower pressure value
neurological disease, big hemodynamics
and higher CO2 values. The heart rate also
instability, accidentally extubated, death in
showed statistically significant differences
the first day in MV, researcher absence
(p = 0.04), and it was higher in failed
and the ones without parent`s
groups (Table.2).
authorization. The flowchart shows the
infants selected (Figure.1). There is a considerable difference between
the failed and successful groups. One of
The demographic characteristic was
them is the size of the sample, with only
separated into successful and failed groups
six infants in failed extubation group. It is
and it is shown in Table.1. The gestational
important to consider the reason these
age, weight, and temperature were similar
infants failed even with some similar
in both groups and the presence of RDS
characteristics as gestational age, birth
was high in groups, 82.05% in the
weight, and temperature.
successful group, and 100% in the failed
group. The Apgar score was divided into 3 The characteristics that showed difference
groups and the score obtained at 5 minutes in successful and failed groups were length
was used in the analysis. Scores between 0 in mechanical ventilation 3 (1–31)/ 1.5 (1–
and 3 received punctuation 0, between 4 4), caffeine peri-extubation 18 (46.15%)/ 2
and 6 received 1 and above 6, were (33.33%), the permanence in continuous
classified as 2. positive airway pressure (CPAP) during
postextubation period 34 (87.18%)/ 2
The successful group had more babies in
(33.33%) and best score in Apgar 24
classification 2 (63.16%). These
(63.16%)/ 3 (50%).
characteristics in Table.1 did not show
statistically significant differences between Another feature that could influence
the groups. Six infants failed extubation successful extubation was 100 percent of
and six others died before the first attempt pulmonary disease (RDS, [respiratory
of extubation. In total thirty-nine distress syndrome]) in the failure group
premature infants had extubation success (Table.1).
and the majority of them were appropriate
for gestational age (AGA). The infants,
small for gestational age (SGA) were
Int J Pediatr, Vol.6, N.9, Serial No.57, Sep. 2018 8218
Nakato et al.
Fig.1: The flow chart of all the babies that were born between July 2014 and November 2016.
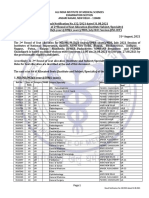
Table 1: Demographic characteristics of premature infants (n = 45).
Characteristics Successful group (n=39) Failed group (n = 6)
Number (%), Median (IQR) or Mean ± SD
Gender
Boys 19 (48.72) 5 (83.3)
Girls 20 (51.28) 1 (16.7)
Gestational age (weeks) 28 + 3.2 28.83 + 3.06
Birth weigth (g) 1102.2 (485 – 3.230) 1064.2 (610 – 1.790)
Apgar (5o minute) 38 (100) 6 (100)
<3 = 0 4 (10.52) 0 (0)
3-6 = 1 10 (26.32) 3 (50)
>6 = 2 24 (63.16) 3 (50)
Temperature (˚C)
Incubator 34.65 + 1.58 34.45 + 2.11
Body 36.39 + 1.13 36.67 + 0.48
Pulmonary Disease (RDS) 32 (82.05) 6 (100)
Days in MV 3 (1 – 31) 1.5 (1 – 4)
Periextubation caffeine 18 (46.15) 2 (33.33)
CPAP ostextubation 34 (87.18) 2 (33.33)
IQR: interquartile range; SD: standard deviation; RDS: respiratory distress syndrome; MV: mechanical
ventilation.
Int J Pediatr, Vol.6, N.9, Serial No.57, Sep. 2018 8219
Ventilator Weaning in Premature Infants
Fig.2: The characteristics of preterm infants selected.
Table-2: Extubation parameters premature infants (n = 45).
Characteristics Successful group (n = 39) Failed group (n = 6) P-value
Breath rate (bpm) 30.55 + 9.78 30.66 + 7.53 0.98
Heart rate (bpm) 149.79 + 17.96 167.8 + 7.85 0.04
Body Temperature oC 36.38 + 1.18 36.9 + 0.62 0.29
o
Incubator Temperature C 33.31 + 1.32 33.48 + 2.66 0.82
SatO2 (%) 94.84 + 2.85 95.17 + 4.02 0.81
PEEP (cmH2O) 5.37 + 0.54 4.8 + 0.44 0.03
PIP (cmH2O) 17.55 + 3.8 16 + 3.28 0.35
P plateau (cmH2O) 15.68 + 3.3 12.4 + 2.88 0.03
VT (ml/kg) 10 (4.9 – 29) 7.55 (4 – 25) 0.39
Cst (ml/cmH2O) 1.07 (0.61 – 3) 1 (0.4–3.57) 0.55
Cdyn (ml/cmH2O) 0.92 (0.54 – 2.2) 0.7 (0.37 – 2.08) 0.57
Tinp (s) 0.39 + 0.03 0.36 + 0.04 0.16
FiO2 32.5 (21 – 90) 37.66 + 11.43 0.92
PaO2/FiO2 182.54 (54.44 – 623.80) 153.42 (108 – 304.77) 0.36
Vol min (l/m) 0.55 (0.07 – 1.35) 0.41 (0.05 – 0.49) 0.08
PaO2 (mmHg) 66.5 (31 – 150) 65.33 + 16.46 0.47
PaCO2 (mmHg) 38 + 12.2 50.6 + 10.62 0.04
pH 7.36 + 0.09 7.24 + 0.23 0.04
HCO3 (mEq/L) 20.69 + 6.08 21.63 + 3.35 0.71
BE -3.4 (-22.10 – 8.7) -5.95 (-10.6 – 4.10) 0.73
EtCO2 (mmHg) 39.54 + 10.21 51.8 + 8.07 0.01
Abbreviations: VT - tidal volume; Vol min – minute volume; bpm – breaths per minute and beats per minute;
o
C: degree celsius; PIP – peak inspiratory pressure; Pplateau - plateau pressure; PEEP – positive end-expiratory
pressure; Cdyn - dynamic compliance; Cst - static compliance; pH - potential of ionic hydrogen; PaCO2 – partial
pressure of arterial carbon dioxide; PaO2 – partial pressure of arterial oxygen; HCO3- – bicarbonate; BE - base
excess; SpO2 – oxygen saturation; EtCO2 - end-tidal of carbon dioxide; mmHg - millimeters of mercury ; ml -
milliliter; mL/kg- milliliter per kilogram; s - seconds; cmH2O – water centimeter; l/min - liters per minute;
ml/cmH2O – milliliter per water centimeter; cm2 - square centimeter; mEq/L -milliequivalents per liter.
Significant difference at a significance level of p < 0.05.
Int J Pediatr, Vol.6, N.9, Serial No.57, Sep. 2018 8220
Nakato et al.
4- DISCUSSION estimate of the PaCO2 (18), so the EtCO2
can be used as an indicator for a successful
In a cohort study, we were able to
extubation, too. In the periextubation
show during nearly two-year studies with
period, the pH and PaCO2 also showed
51 mechanically ventilated premature
statistically significant differences (p =
babies that the majority of them were
0.01) in the study done by Chawla et al. in
successfully extubated. The group showed
2017 (16). This results agree with the
similar features in gestational age, birth
present study and shows the importance of
weight, Apgar score, temperature, length
the arterial blood gas analysis, that is
in mechanical ventilation and appropriate
considered the gold-standard test and
for gestational age. Six infants died before
might be used to predict extubation
the first attempt at extubation and five of
outcomes (19). Autonomic nervous system
them were small for gestational age. The
through sympathetic and parasympathetic
extubation parameters, which showed
innervation work in balance to adapt to
statistically significant differences, were
different situations, but premature infants
heart rate, plateau pressure, PEEP, PaCO2,
don’t have their systems balance well
pH, and EtCO2, and the successful group
established, so some changes in
had the values closer to reference values.
intrathoracic pressure and lung volume
Currently, the decision of extubation is during weaning may induce changes in
based on clinical conditions, blood gas heart rate, because the autonomic nervous
variables, oxygen support and the level of system can induce alterations to maintain
ventilator support needed, but there is no cardiac output (20, 21). The heart rate
parameter that can show the extubation showed statistically significant differences
success, and it continues to be based on between the groups (p = 0.04), and in the
subjective assessments of premature babies failed group the heart rate was higher than
(15,16). Some weaning concepts have the successful groups, that could suggest
failed to show superiority over doctors' the attempt of the autonomic nervous
experience and clinical judgment, but system to adapt the changes in the
researchers showed that the combination respiratory mechanics.
of these variables, like respiratory
Another factor that may be associated with
mechanics, gas exchange, ability to
successful extubation is the administration
maintain the work of breathing and clinical
of caffeine during the pre-extubation
experience, is a good combination for a
period. Caffeine is usually used in neonatal
weaning success (17). Parameters that
intensive care units because it can reduce
showed statistically significant differences
the apnea, intermittent hypoxemia, avoid
between the groups were related to
extubation failure of the mechanical
pressure and arterial blood gas. A study by
ventilation, reduces the incidence of
Wang et al. (2017) showed the similar
bronchopulmonary and patent ductus
result in pH (p = 0.05), and bicarbonate
arteriosus in preterm infants (22). In the
level (p = 0.03), and in this case, arterial
present study, with 39 preterm infants that
blood gas analyze might be associated with
had successful extubation, 18 used caffeine
extubation outcomes (15). In our study, the
(46.15%), and only 2 (33.33%) premature
arterial blood gas parameters, pH, and
infants used caffeine in the failed group.
PaCO2 (p = 0.04), can also be used as an
Caffeine dosage has not been reported in
indicator for a successful extubation. The
our study, but other research shows that
EtCO2 showed statistically significant
the use of high dose of caffeine, in
differences (p = 0.01), this parameter is an
alternative noninvasive method to monitor comparison to low doses, may decrease the
chance of extubation failure in premature
CO2 values and has been showing a good
Int J Pediatr, Vol.6, N.9, Serial No.57, Sep. 2018 8221
Ventilator Weaning in Premature Infants
infants mechanically ventilated (23). One research on the comparison between
factor affecting successful extubation is successful and failed extubation for future
post-extubation respiratory support and the prospective studies.
most used is the continuous positive
airway pressure (CPAP). CPAP is a type 5- CONCLUSION
of flow used to generate the positive The decision of extubation involves
pressure and it is associated with lower many factors, such as the clinical
incidence of intubation and reintubation conditions of premature babies, arterial
because it prevents apnea and atelectasis blood gas, oxygen support, ventilator
(24, 25). In our study, the majority of support level and the experience of the
premature infants in the successful group clinical team; but in this study, we can
used CPAP in the post-extubation period consider the pressure values, the analyzes
(87.18%), and only 2 babies used in the of arterial blood gases and capnometry as
failed group (33,33%). In this study, important parameters to evaluate in the
comparing two type of CPAP, bi-level weaning process, verifying these values
nasal CPAP (NCPAP), and nasal closer to the reference values. Supports
intermittent positive pressure ventilation before and after endotracheal extubation,
(NIPPV) showed that both have high such as caffeine and CPAP, are important
extubation successful rates in the post- to avoid the need for reintubation.
extubation period (24).
With these results, we assume that the 6- CONFLICT OF INTEREST: None.
gradual reduction of respiratory support 7- ACKNOWLEDGMENTS
can provide a better adaptation of the lung
and avoid reintubation. Though the The research was carried out in the
gestational age, weight, and temperature Neonatal Intensive Care Unit, Hospital de
were similar in both groups, the Apgar Clínicas. We thank the team of NICU and
score was better in successful groups, with Lilian Messias for the statistical support
24 (63.16%) premature infants with and assistance.
classification 2, but did not show
statistically significant differences between 8- REFERENCES
the failed group and the classifications. 1. Robles-rubio CA, Kaczmarek J,
Research comparing risk factors associated Chawla S, et al. Automated Analysis of
with extubation failure in newborns with Respiratory Behavior in Extremely Preterm
birth weight < 1,250 grams showed Infants and Extubation Readiness. Pediatric
statistically significant differences between Pulmonology 2015;486:479–86.
groups in the 5-minute Apgar score (p= 2. Dimitriou G, Greenough A, Endo A, et
0.01), which showed that higher Apgar al. Prediction of extubation failure in preterm
score can increase the chances of infants. Arch Dis Child Fetal Neonatal Ed
extubation success (26). 2002;86:F32–F35.
3. Blencowe H, Cousens S, Chou D, et
4-1. Limitations of the study al. Born Too Soon: The global epidemiology
This is an observational study to evaluate of 15 million preterm births. Reprod Health
the parameters associated with extubation 2013;10(Suppl 1):1–14.
success and these results match others 4. Glass HC, Costarino AT, Stayer SA,
researches already published. During the et al. Outcomes for Extremely Premature
study period, we had some limitations, as a Infants. Anesth Analg 2015;120(6):1337–51.
strike at the hospital and reform in NICU, 5. Mcconville JF, Kress JP. Weaning
which made it impossible to obtain a larger Patients from the Ventilator. N Engl J Med
sample. It is important to conduct more 2012;367(23):2233–39.
Int J Pediatr, Vol.6, N.9, Serial No.57, Sep. 2018 8222
Nakato et al.
6. Sant’Anna GM, Keszler M. 17. Rimensberger PC, Cheifetz IM,
Developing a neonatal unit ventilation Kneyber MCJ. The top ten unknowns in
protocol for the preterm baby. Early Hum Dev. pediatric mechanical ventilation. Intensive
Elsevier Ltd 2012;88(12):925–9. Care Med. Springer Berlin Heidelberg 2017.
7. A Collective Task Force Facilitated by 18. Bhat R, Abhishek N. Mainstream end-
the American College of Chest Physicians, the tidal carbon dioxide monitoring in ventilated
American Association for Respiratory Care, neonates Mainstream end-tidal carbon dioxide
and the American College of Critical Care monitoring in ventilated neonates. Singapore
Medicine: Evidence-Based Guidelines for Med J 2008;49(3):199–203.
Weaning and Discontinuing Ventilatory 19. Wu C, Chou H, Hsieh W, Chen W.
Support. Respir Care 2002;47(1):69–90. Good Estimation of Arterial Carbon Dioxide
8. Sant’Anna GM, Keszler M. Weaning by End-Tidal Carbon Dioxide Monitoring in
Infants from Mechanical ventilation. Clin the Neonatal Intensive Care Unit. Pediatr
Perinatol. Elsevier Inc 2012;39(3):543–62. Pulmonol 2003;30:292–5.
9. Chawla S, Natarajan G, Gelmini M, et 20. Hammash MH, Moser debra K,
al. Role of Spontaneous Breathing Trial in Frazier Susan K, et al. Heart Rate variability as
Predicting Successful Extubation in Premature a predictor of cardiac dysrhythmias during
Infants. Pediatric Pulmonology 2013;448:443– weaning from mechanical ventilation. Am J
8. Crit Care 2015;24(2):118–28.
10. Al-Mandari H, Shalish W, Dempsey 21. Shalish W, Kanbar LJ, Rao S, et al.
E, et al. International survey on periextubation Prediction of Extubation readiness in
practices in extremely preterm infants. Arch extremely preterm infants by the automated
Dis Child Fetal Neonatal Ed 2015;100: F428– analysis of cardiorespiratory behavior : study
31. protocol. BMC Pediatrics 2017;1–15.
11. Biban P, Gaffuri M, Spaggiari S, et al. 22. Abdel-hady H, Nasef N, Shabaan AE,
Weaning newborn infants from mechanical Nour I. Caffeine therapy in preterm infants.
ventilation. Journal of Pediatric and Neonatal World J Clin Pediatr 2015;4(4):81–94.
Individualized Medicine 2013;2(2):1–7. 23. Mohammed S, Nour I, Shabaan AE.
12. Thomas PE, Leflore J. Extubation High versus low-dose caffeine for apnea of
Success in Premature Infants Treated With Bi- prematurity : a randomized controlled trial.
Level Nasal Continuous. J Perinat Neonat Eur J Pediatr 2015;949–56.
Nurs 2013;27(4):328–34. 24. Thomas PE, LeFlore J. Extubation
13. Dehdashtian M, Malakian A, Aramesh success in premature infants with respiratory
MR, et al. The effectiveness of intratracheal distress syndrome treated with bi-level nasal
salbutamol in addition to surfactant on the continuous positive airway pressure versus
clinical course of newborns with respiratory nasal intermittent positive pressure ventilation.
distress syndrome: a clinical trial. Ital J Pediatr J Perinat Neonat Nurs 2013;27(4):324–8.
2016;4–8. 25. Amatya S, Macomber M, Bhutada
14. Miyaki M. Manual da UTI Neonatal. A, Rastogi D, Rastogi S. Sudden versus
UTI Neonatal do HC/UFPR 2014;1–225. gradual pressure wean from Nasal CPAP in
15. Wang S, Liou J, Chen C, et al. Risk preterm infants: a randomized controlled trial.
Factors for Extubation Failure in Extremely J Perinatol 2017;37(6):662–7.
Low Birth Weight Infants. Pediatr Neonatol 26. Hermeto F, Martins BMR, Ramos
2017;58(2):145–50. JRM, Bhering CA, Sant'Anna GM. Incidence
16. Chawla S, Natarajan G, Shankaran S, and main risk factors associated with
et al. Markers of Successful Extubation in extubation failure in newborns with birth
Extremely Preterm Infants, and Morbidity weight <1, 250 grams.J Pediatr
After Failed Extubation. J Pediatr 2009;85(5):397–402.
2017;189:113–9.
Int J Pediatr, Vol.6, N.9, Serial No.57, Sep. 2018 8223
You might also like
- IAPD20 Virtual Abstract Book CompressedDocument991 pagesIAPD20 Virtual Abstract Book CompressedAnonymous NqTjEcNo ratings yet
- 101 Black Seed Oil Benefits, Uses & CuresDocument15 pages101 Black Seed Oil Benefits, Uses & CuresAli100% (3)
- AdenomyosisDocument16 pagesAdenomyosisWiwik'RatnaSariPratiwi'100% (2)
- Ajrcccm 2004Document9 pagesAjrcccm 2004kichilla1No ratings yet
- Impact of Prophylactic Continuous Positive Airway Pressure On Transient Tachypnea of The Newborn and Neonatal Intensive Care Admission in Newborns Delivered by Elective Cesarean SectionDocument8 pagesImpact of Prophylactic Continuous Positive Airway Pressure On Transient Tachypnea of The Newborn and Neonatal Intensive Care Admission in Newborns Delivered by Elective Cesarean SectionFabiano SilvaNo ratings yet
- TTNpublicationDocument5 pagesTTNpublicationVerushka CrespoNo ratings yet
- Jurnal Pubme 1 RdsDocument13 pagesJurnal Pubme 1 Rdsriri risna aNo ratings yet
- Australian Critical CareDocument9 pagesAustralian Critical CareLisa MaghfirahNo ratings yet
- 2019 A Phase II Randomized Controlled Trial For Lung and Diaphragm Protective VentilationDocument7 pages2019 A Phase II Randomized Controlled Trial For Lung and Diaphragm Protective VentilationwilsonmauriciolozanoNo ratings yet
- Klebsiella PDFDocument4 pagesKlebsiella PDFOscarEduardoNo ratings yet
- Lung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFDocument8 pagesLung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFcesar juarezNo ratings yet
- 1 ChestDocument5 pages1 ChestZakiyah Nur HaqqiNo ratings yet
- Journal NicuDocument4 pagesJournal NicuMargaret LlavorNo ratings yet
- Viral Respiratory Infections in Preterm Infants During andDocument9 pagesViral Respiratory Infections in Preterm Infants During andMariusNo ratings yet
- Risk Factors For Pediatric Extubation FailureDocument17 pagesRisk Factors For Pediatric Extubation FailureFabiola VaniaNo ratings yet
- Background: Corresponding AuthorDocument8 pagesBackground: Corresponding AuthorPratiwi UmbohNo ratings yet
- Clinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency DepartmentDocument5 pagesClinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency Departmentnavali rahmaNo ratings yet
- International Consensus On Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations (Costr)Document71 pagesInternational Consensus On Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations (Costr)Dr.Sushree Smita Behura100% (1)
- Buonsenso Et Al-2018-Pediatric PulmonologyDocument9 pagesBuonsenso Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- MD 0000000000012257Document5 pagesMD 0000000000012257Sykat ZamanNo ratings yet
- Journal ReadingDocument5 pagesJournal ReadingRoma WestNo ratings yet
- Articulo ViernesDocument6 pagesArticulo Viernesvelf5No ratings yet
- Umbilical Cord ClampingDocument10 pagesUmbilical Cord ClampingTika WulandariNo ratings yet
- E PDFDocument5 pagesE PDFKarolinaNo ratings yet
- Neonatal PneumoniaDocument8 pagesNeonatal PneumoniaAde Gustina SiahaanNo ratings yet
- Grafica 2 BiennDocument16 pagesGrafica 2 Biennwincu roNo ratings yet
- Dyke 2023 Ped Radiol PREFUL Lung MRI Ventilation NICUDocument9 pagesDyke 2023 Ped Radiol PREFUL Lung MRI Ventilation NICUJonathan DykeNo ratings yet
- Articulo Tesis 9Document8 pagesArticulo Tesis 9Lourdes MarcosNo ratings yet
- Neonatal Lung Ultrasonography To Evaluate Need For Surfactant and Mechanical VentilationDocument8 pagesNeonatal Lung Ultrasonography To Evaluate Need For Surfactant and Mechanical VentilationAlexandra NemesNo ratings yet
- Zgddekzz 23 11 1097Document6 pagesZgddekzz 23 11 1097arieza nur pratamaNo ratings yet
- CJRT 2019 011Document8 pagesCJRT 2019 011Siti HumairahNo ratings yet
- Does Antenatal Corticosteroid Therapy Improve Neonatal Outcomes in Late Preterm Birth?Document8 pagesDoes Antenatal Corticosteroid Therapy Improve Neonatal Outcomes in Late Preterm Birth?faikaoesmaniaNo ratings yet
- Pediatrics 1001 (Final)Document5 pagesPediatrics 1001 (Final)Paul HartingNo ratings yet
- Pi Is 0022347611006548Document7 pagesPi Is 0022347611006548Yudo PrabowoNo ratings yet
- Comparison of Saans Neonatal Continuous Positive Airway PressureDocument6 pagesComparison of Saans Neonatal Continuous Positive Airway Pressureemailtrinaya30No ratings yet
- DANI 2012 - Surfactant Replacement in Preterm Infants With RDSDocument4 pagesDANI 2012 - Surfactant Replacement in Preterm Infants With RDSRafael JustinoNo ratings yet
- Etiological Study of Respiratory Distress in Newborn: Original ResearchDocument5 pagesEtiological Study of Respiratory Distress in Newborn: Original ResearchNovia KurniantiNo ratings yet
- Mechanical Ventilation of The Premature NeonateDocument16 pagesMechanical Ventilation of The Premature NeonateHaitham HafezNo ratings yet
- Relationship Between Oxygenation Index and Extubation Outcome in Neonates Using Mechanical VentilatorDocument6 pagesRelationship Between Oxygenation Index and Extubation Outcome in Neonates Using Mechanical VentilatorInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Neonatal Tracheostomy - JonathanWalsh 2018Document12 pagesNeonatal Tracheostomy - JonathanWalsh 2018Ismael Erazo AstudilloNo ratings yet
- Journal Pone 0000192Document5 pagesJournal Pone 0000192TriponiaNo ratings yet
- Respiratory Distress in Term Babies, Can We Predict The Outcome?Document5 pagesRespiratory Distress in Term Babies, Can We Predict The Outcome?Dr. Nimesha GamhewageNo ratings yet
- Wright Et Al 2022 PDFDocument9 pagesWright Et Al 2022 PDFRadu CiprianNo ratings yet
- Use of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaDocument10 pagesUse of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaLingga AniNo ratings yet
- A Pilot Prospective Study On Closed Loop Controlled Ventilation and Oxygenation in Ventilated Children During The Weaning PhaseDocument9 pagesA Pilot Prospective Study On Closed Loop Controlled Ventilation and Oxygenation in Ventilated Children During The Weaning PhaseSiti HumairahNo ratings yet
- Causes and Outcomes of Respiratory Distress in NeonatesDocument8 pagesCauses and Outcomes of Respiratory Distress in NeonatesMohammad AlmuhaiminNo ratings yet
- NRDS国教班Document39 pagesNRDS国教班raj patelNo ratings yet
- Paediatrica IndonesianaDocument9 pagesPaediatrica IndonesianaAudina PutriNo ratings yet
- Lauder 2019Document12 pagesLauder 2019Julio AltamiranoNo ratings yet
- SDR Segun EdadDocument9 pagesSDR Segun EdadLuzbenia ChaparroNo ratings yet
- The Role of Delayed Cord Clamping in Improving The Outcome in Preterm BabiesDocument5 pagesThe Role of Delayed Cord Clamping in Improving The Outcome in Preterm BabiesJehangir AllamNo ratings yet
- 5882-PDF Galley-38159-1-10-20201216Document5 pages5882-PDF Galley-38159-1-10-20201216MF SNo ratings yet
- Neonatal Mechanical Ventilation Predictors of Mortality and OutcomesDocument8 pagesNeonatal Mechanical Ventilation Predictors of Mortality and OutcomesAthenaeum Scientific PublishersNo ratings yet
- Gruber2016 PDFDocument4 pagesGruber2016 PDFGiovanni HenryNo ratings yet
- Evaluation of Tracheal Intubations in A Paediatric Intensive Care UnitDocument10 pagesEvaluation of Tracheal Intubations in A Paediatric Intensive Care Unitan.mohammed.maisNo ratings yet
- A Framework For The Management of The Pediatric AirwayDocument23 pagesA Framework For The Management of The Pediatric AirwayDaniel GallegoNo ratings yet
- SPIROMETRYDocument9 pagesSPIROMETRYaeyousefNo ratings yet
- Artigo Ana e Frederico 2021Document10 pagesArtigo Ana e Frederico 2021CarolinaNo ratings yet
- DIT SoniyaRDocument4 pagesDIT SoniyaRLaelannie MagpayoNo ratings yet
- Intjprevmed6133-2704195 004504Document6 pagesIntjprevmed6133-2704195 004504Ade HabibieNo ratings yet
- Short-Acting Sedative-Analgesic Drugs Protect Against Development of Ventilator-Associated Events in Children: Secondary Analysis of The EUVAE StudyDocument8 pagesShort-Acting Sedative-Analgesic Drugs Protect Against Development of Ventilator-Associated Events in Children: Secondary Analysis of The EUVAE StudyevyNo ratings yet
- Doyle & Bradshaw - Sixty Golden MinutesDocument6 pagesDoyle & Bradshaw - Sixty Golden MinutesVillia DamayantieNo ratings yet
- MR Muu STHDocument13 pagesMR Muu STHSiti HumairahNo ratings yet
- CJRT 2019 011Document8 pagesCJRT 2019 011Siti HumairahNo ratings yet
- Assessment of Common Criteria For Awake Extubation in Infants and Young ChildrenDocument8 pagesAssessment of Common Criteria For Awake Extubation in Infants and Young ChildrenSiti HumairahNo ratings yet
- CC 3898Document10 pagesCC 3898Siti HumairahNo ratings yet
- A Pilot Prospective Study On Closed Loop Controlled Ventilation and Oxygenation in Ventilated Children During The Weaning PhaseDocument9 pagesA Pilot Prospective Study On Closed Loop Controlled Ventilation and Oxygenation in Ventilated Children During The Weaning PhaseSiti HumairahNo ratings yet
- Variability of Respiratory Parameters and Extubation Readiness in Ventilated NeonatesDocument6 pagesVariability of Respiratory Parameters and Extubation Readiness in Ventilated NeonatesSiti HumairahNo ratings yet
- Jurnal 4 SNDocument11 pagesJurnal 4 SNSiti HumairahNo ratings yet
- JClinNeonatol73158-3845905 104059Document4 pagesJClinNeonatol73158-3845905 104059Siti HumairahNo ratings yet
- Ocular Trauma: H. Amiruddin, DR., Spm. Rsud Arifin Achmad PekanbaruDocument22 pagesOcular Trauma: H. Amiruddin, DR., Spm. Rsud Arifin Achmad PekanbaruNovasiska Indriyani HutajuluNo ratings yet
- CBSE NCERT Solutions For Class 12 Science Chapter 4: Back of Chapter QuestionsDocument5 pagesCBSE NCERT Solutions For Class 12 Science Chapter 4: Back of Chapter QuestionsSatvik MishraNo ratings yet
- 2nd Round Seat Allotment Result MDMS MDS Final NET2Document52 pages2nd Round Seat Allotment Result MDMS MDS Final NET2SARKAR JAVED AKHTARNo ratings yet
- TamifluDocument20 pagesTamiflukiwikid718635No ratings yet
- DC Healthy People ReportDocument108 pagesDC Healthy People ReportChristina SturdivantNo ratings yet
- WorldAlzheimerReport2016 PDFDocument140 pagesWorldAlzheimerReport2016 PDFBinod मगरNo ratings yet
- 9 Essential CBT Techniques and Tools PsychotherapyDocument4 pages9 Essential CBT Techniques and Tools Psychotherapyآئمہ توصيف100% (1)
- Sodium Hyaluronate (Hyaluronic Acid) Promotes Migration of Human Corneal Epithelial Cells in VitroDocument2 pagesSodium Hyaluronate (Hyaluronic Acid) Promotes Migration of Human Corneal Epithelial Cells in VitroanamaghfirohNo ratings yet
- Clayton & Willihnganz: Basic Pharmacology For Nurses, 17th EditionDocument4 pagesClayton & Willihnganz: Basic Pharmacology For Nurses, 17th EditionabsianoNo ratings yet
- Contoh Artikel Buk RenoDocument5 pagesContoh Artikel Buk RenoDewita Wulan PratiwiNo ratings yet
- Narrative Report On Second Sem SyllabusDocument92 pagesNarrative Report On Second Sem SyllabusChristine Joy MolinaNo ratings yet
- 2.4.B DR Denni Clinical Evidence of Ribociclib Into Clinical PracticeDocument40 pages2.4.B DR Denni Clinical Evidence of Ribociclib Into Clinical Practicetepat rshsNo ratings yet
- Spine 2019 BrochureDocument10 pagesSpine 2019 BrochureLuciana AliceNo ratings yet
- Vitamin B12 InfographicDocument2 pagesVitamin B12 InfographicIan WynneNo ratings yet
- Report of Anp Icu PostingDocument5 pagesReport of Anp Icu PostingsimonjosanNo ratings yet
- Agents Used in Anemias 2Document25 pagesAgents Used in Anemias 2Raboha TawilNo ratings yet
- Henoch-Schonlein Purpura: An Update: Nutan Kamath, Suchetha RaoDocument7 pagesHenoch-Schonlein Purpura: An Update: Nutan Kamath, Suchetha RaoManjunath VaddambalNo ratings yet
- CurosurDocument2 pagesCurosuredNo ratings yet
- SOMATOM Definition AS Open 20 64 RadOncol PDFDocument20 pagesSOMATOM Definition AS Open 20 64 RadOncol PDFJorge LopezNo ratings yet
- CeftriaxoneDocument2 pagesCeftriaxonegaatgaatNo ratings yet
- Rapport Annuel Santé EuropéenDocument248 pagesRapport Annuel Santé EuropéennouvelobsNo ratings yet
- Paralytic Ileus: Prepared By: Laurence A. Adena, ManDocument43 pagesParalytic Ileus: Prepared By: Laurence A. Adena, ManJanah Beado PagayNo ratings yet
- EosinophiliaDocument8 pagesEosinophiliajohnNo ratings yet
- Terpinen 4 OlDocument8 pagesTerpinen 4 OlDouglas RussellNo ratings yet
- HysterectomyDocument24 pagesHysterectomypt.mahmoudNo ratings yet
- Kgmcta Membership List: Sl. No. Mem. No. Name Department CollegeDocument36 pagesKgmcta Membership List: Sl. No. Mem. No. Name Department CollegekgmctaNo ratings yet
- Fetal Hypoxia 2157 7420.1000e121Document1 pageFetal Hypoxia 2157 7420.1000e121Fian ChristoNo ratings yet