Professional Documents
Culture Documents
Contemporary Analysis of The Intraoperative and Perioperative Complications of Neurosurgical Procedures Performed in The Sitting Position
Contemporary Analysis of The Intraoperative and Perioperative Complications of Neurosurgical Procedures Performed in The Sitting Position
Uploaded by
Lloyd AllenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Contemporary Analysis of The Intraoperative and Perioperative Complications of Neurosurgical Procedures Performed in The Sitting Position
Contemporary Analysis of The Intraoperative and Perioperative Complications of Neurosurgical Procedures Performed in The Sitting Position
Uploaded by
Lloyd AllenCopyright:
Available Formats
CLINICAL ARTICLE
J Neurosurg 127:182–188, 2017
Contemporary analysis of the intraoperative and
perioperative complications of neurosurgical procedures
performed in the sitting position
Benjamin T. Himes, MD,1 Grant W. Mallory, MD,1 Arnoley S. Abcejo, MD,2 Jeffrey Pasternak, MD,2
John L. D. Atkinson, MD,1 Fredric B. Meyer, MD,1 W. Richard Marsh, MD,1 Michael J. Link, MD,1
Michelle J. Clarke, MD,1 William Perkins, MD,2 and Jamie J. Van Gompel, MD1
Departments of 1Neurologic Surgery and 2Anesthesiology, Mayo Clinic, Rochester, Minnesota
OBJECTIVE Historically, performing neurosurgery with the patient in the sitting position offered advantages such as
improved visualization and gravity-assisted retraction. However, this position fell out of favor at many centers due to
the perceived risk of venous air embolism (VAE) and other position-related complications. Some neurosurgical centers
continue to perform sitting-position cases in select patients, often using modern monitoring techniques that may improve
procedural safety. Therefore, this paper reports the risks associated with neurosurgical procedures performed in the
sitting position in a modern series.
METHODS The authors reviewed the anesthesia records for instances of clinically significant VAE and other complica-
tions for all neurosurgical procedures performed in the sitting position between January 1, 2000, and October 8, 2013. In
addition, a prospectively maintained morbidity and mortality log of these procedures was reviewed for instances of sub-
dural or intracerebral hemorrhage, tension pneumocephalus, and quadriplegia. Both overall and specific complication
rates were calculated in relation to the specific type of procedure.
RESULTS In a series of 1792 procedures, the overall complication rate related to the sitting position was 1.45%, which
included clinically significant VAE, tension pneumocephalus, and subdural hemorrhage. The rate of any detected VAE
was 4.7%, but the rate of VAE requiring clinical intervention was 1.06%. The risk of clinically significant VAE was highest
in patients undergoing suboccipital craniotomy/craniectomy with a rate of 2.7% and an odds ratio (OR) of 2.8 relative to
deep brain stimulator cases (95% confidence interval [CI] 1.2–70, p = 0.04). Sitting cervical spine cases had a compara-
tively lower complication rate of 0.7% and an OR of 0.28 as compared with all cranial procedures (95% CI 0.12–0.67, p <
0.01). Sitting cervical cases were further subdivided into extradural and intradural procedures. The rate of complications
in intradural cases was significantly higher (OR 7.3, 95% CI 1.4–39, p = 0.02) than for extradural cases. The risk of VAE
in intradural spine procedures did not differ significantly from sitting suboccipital craniotomy/craniectomy cases (OR
0.69, 95% CI 0.09–5.4, p = 0.7). Two cases (0.1%) had to be aborted intraoperatively due to complications. There were
no instances of intraoperative deaths, although there was a single death within 30 days of surgery.
CONCLUSIONS In this large, modern series of cases performed in the sitting position, the complication rate was low.
Suboccipital craniotomy/craniectomy was associated with the highest risk of complications. When appropriately used
with modern anesthesia techniques, the sitting position provides a safe means of surgical access.
https://thejns.org/doi/abs/10.3171/2016.5.JNS152328
KEY WORDS sitting position; venous air embolism; posterior fossa surgery; surgical technique
U
se of the sitting position in neurosurgery has long outlet pressure, improved visualization of the surgical field,
been a matter of some debate.32 Interest in its use and reduced need for cerebellar retraction in posterior fossa
stems from a number of perceived advantages rela- cases.15,32 In some instances, specifically deep brain stimu-
tive to other positions, particularly for procedures involv- lator (DBS) implantation, the use of the sitting position is
ing the posterior fossa and cervical spine. These advantages preferred to ensure appropriate access and patient comfort
include improved venous drainage due to reduced thoracic as well as to minimize brain shift during the procedure.
ABBREVIATIONS ACLS = advanced cardiovascular life support; CI = confidence interval; DBS = deep brain stimulator; OR = odds ratio; PFO = patent foramen ovale; TEE
= transesophageal echocardiography; VAE = venous air embolism.
SUBMITTED October 6, 2015. ACCEPTED May 17, 2016.
INCLUDE WHEN CITING Published online August 5, 2016; DOI: 10.3171/2016.5.JNS152328.
182 J Neurosurg Volume 127 • July 2017 ©AANS, 2017
Unauthenticated | Downloaded 09/05/20 03:42 PM UTC
Contemporary complications in the sitting position
These benefits must be weighed against perceived traoperatively. This diagnosis was made at the discretion
complications inherent to the sitting position. Venous of the documenting physician based on clinical findings
air embolism (VAE), postoperative quadriplegia, tension and intraoperative fluctuations in the patient’s vital signs.
pneumocephalus, and subdural hematomas have been re- Cases of VAE were not diagnosed retrospectively. Cases
ported.15,28,37 In much of the reported literature, these com- of VAE were retrospectively classified as mild (requiring
plications occur at very low rates, but the results can be no intervention), moderate (a significant drop in end-tidal
devastating when they do occur. However, modern tech- CO2 or hemodynamic instability requiring support with va-
niques to prevent, monitor, diagnose, and rapidly treat sopressors), or severe (moderate criteria with the addition
these complications can potentially improve outcome.14 of emergency repositioning or use of Advanced Cardiovas-
This is supported by a number of recent series that have cular Life Support [ACLS] resuscitation). A case of VAE
demonstrated reduced rates of complications, particularly was deemed clinically significant if it was classified in the
VAE, relative to older studies.15,21,37 These results suggest moderate or severe categories.
that rather than abandoning this procedure as has occurred
at many centers, modern techniques aimed at recognizing Intraoperative Monitoring
VAE may mitigate complications associated with the sit- Intraoperative monitoring to aid in the diagnosis of VAE
ting position, improving its safety. In this paper we report was case-dependent. Sitting cranial cases typically includ-
a modern series of 1792 procedures performed in the sit- ed precordial Doppler ultrasonography, transesophageal
ting position from January 1, 2000, to October 8, 2013. echocardiography (TEE), and placement of a central line
for central venous pressure monitoring. Anesthesia was
Methods maintained with isoflurane, with or without nitrous oxide
Study Population or desflurane and short-acting narcotics. Cervical spine
Institutional Review Board approval was obtained cases used similar monitoring and anesthesia to cranial
prior to data collection. Patients undergoing DBS elec- cases but without central venous pressure monitoring. DBS
trode placement, suboccipital craniotomy/craniectomy, cases were monitored with precordial Doppler ultrasonog-
and procedures involving the posterior cervical spine in raphy only. DBS cases typically proceeded under moni-
the sitting position between January 1, 2000, and October tored sedation with dexmedetomidine; in cases in which
8, 2013, were included. Patients undergoing percutaneous general anesthesia was required, maintenance proceeded
procedures or refusing consent for research were exclud- with isoflurane or sevoflurane with or without nitrous ox-
ed. Morbidity and mortality logs, operative reports, and ide. The typical intraoperative positioning of a patient,
electronic medical records were reviewed for instances as well as the intraoperative monitoring configuration, is
of detected VAE, clinically significant VAE (defined as presented in Fig. 1. A retrospective review of the intraop-
those cases requiring anesthetic intervention), subdural erative anesthesia record was undertaken to assess the in-
hematoma, tension pneumocephalus, and postoperative cidence of VAE based on precordial Doppler monitoring,
quadriplegia. The morbidity and mortality log represents changes in end-expired CO2, and changes in hemodynamic
a prospectively maintained database of immediate and stability. Preoperative risk assessment, such as with bubble
near-term postoperative complications (within 30 days echocardiography, was not routinely undertaken.
of the procedure) as recorded by providers in the Depart-
ment of Neurological Surgery. Preoperatively, there were Statistical Analysis
no predetermined criteria as to what cases were to be per- Statistical analysis was performed using Microsoft Ex-
formed in the sitting position. Surgeon preference was the cel and MedCalc online to calculate the odds ratio (OR),
deciding factor, with consultation with the anesthesiolo- 95% confidence interval (CI), and statistical significance
gist at the time of surgery. of complications during a given type of procedure. Cases
Postoperative hemorrhages, including subdural hema- were broadly divided into sitting suboccipital craniotomy/
tomas, were part of the analysis if listed as an immediate craniectomy, DBS, or cervical spine procedures. Compli-
or short-term complication in the morbidity and mortality cations in sitting suboccipital cases were compared with
log during the acute hospital period. Cases of tension pneu- those in DBS procedures. Cervical spine procedures were
mocephalus were included if intervention was required in further categorized as either intradural or extradural, and
the form of twist-drill evacuation. The overall incidence of the risk of VAE was compared between these two groups.
complications as well as individual complication rates was
analyzed. Further subset analysis was performed accord-
ing to procedure type.
Results
Demographics
Data Collection A total of 1792 procedures were identified during the time
Cases of VAE were identified based on specific docu- interval of the study. The overall series consisted of 41% fe-
mentation in the anesthesia record. This was performed via male patients with a median age of 54 years (range 3–92
a database query of the included cases for the terms “VAE,” years). Further demographic data can be found in Table 1.
“venous air embolism,” “air embolism,” “air emb-,” “air
he-,” “air se-,” “air id-,” and “air bu-.” The results of the Events
query were manually reviewed to ensure the accuracy of The overall complication rate related to the procedure
the included cases. The diagnosis of VAE was made in- was 1.45% (26/1792 procedures). The incidence rates of
J Neurosurg Volume 127 • July 2017 183
Unauthenticated | Downloaded 09/05/20 03:42 PM UTC
B. T. Himes et al.
and 0.5%, respectively (Table 3). The lone case of tension
pneumocephalus noted in a sitting cervical procedure oc-
curred in an intradural case. No neurological deficits were
directly attributable to patient positioning in any of the in-
cluded cases. Sitting cervical procedures were overall as-
sociated with fewer complications than cranial procedures
(OR 0.28, 95% CI 0.12–0.67, p = 0.0042).
The occurrence of clinically significant VAE (OR 9.07,
95% CI 1.17–70.09, p = 0.035) was more strongly associ-
ated with suboccipital procedures as compared with DBS
implantation, but overall complication rates were compa-
rable (OR 2.83, 95% CI 0.93–8.6, p = 0.67; Table 2). There
was no significant difference in the risk of hemorrhage
or tension pneumocephalus between the two groups (p =
0.435 and p = 0.626, respectively), although there were no
incidences of tension pneumocephalus occurring in DBS
cases in this series.
In cervical spine cases, intradural procedures (n = 54)
were more strongly associated with mild (clinically insig-
nificant) VAE compared with extradural cervical spine
cases (n = 956; OR 6.87, 95% CI 2.38–19.38, p = 0.0004;
Table 4). However, when limited to clinically significant
VAE (moderate or severe), there was no significant dif-
ference (OR 3.59, 95% CI 0.41–31.27, p = 0.247; Table 3).
Intradural cases were also associated with a significantly
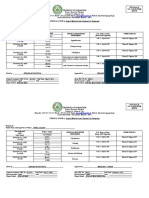
FIG. 1. Illustrative setup for sitting procedure. The patient is placed in a higher risk of tension pneumocephalus relative to extradu-
Mayfield pinion, the table is maximally flexed (A and B), and the patient ral procedures (OR 53.64, 95% CI 2.16–1332.35, p = 0.015;
secured to a Mayfield cross bar adapter (C). An antebrachial peripheral-
ly inserted central catheter is also placed prior to positioning (D). Figure
Table 3). When compared with sitting suboccipital cranial
is available in color online only. procedures, there was not a statistically significant differ-
ence in the risk of clinically significant VAE in intradural
cervical procedures (p = 0.723; Table 3). There was no in-
clinically significant (moderate or severe) VAE, tension cidence of clinically significant postoperative hemorrhage
pneumocephalus, and subdural or remote hemorrhage in either group.
were 1.06%, 0.11%, and 0.28%, respectively, inclusive of No deaths resulted from any of the observed complica-
all procedures. There were no intraoperative deaths; how- tions; the single death within 30 days of the procedure was
ever, 1 patient died within 30 days of the procedure. unrelated to the procedure performed. Two procedures
(2/1792) were aborted due to intraoperative VAE.
Procedure-Specific Data Cases of VAE were subdivided into mild, moderate, and
Among sitting suboccipital procedures (450 cases), the severe categories, based on changes in end-expired CO2
rates of clinically significant VAE, tension pneumocepha- or hemodynamic instability requiring intervention. Mild
lus, and hemorrhage (1 subdural and 1 remote) were 2.7%, cases required no intervention; moderate cases involved a
0.2%, and 0.4%, respectively, with an overall complication significant decrease in end-expired CO2 requiring use of
rate of 3.3% (Table 2). In 332 DBS cases, there was a 0.3% vasopressor support; and severe cases required emergency
incidence of clinically significant VAE and a 0.9% inci- repositioning or ACLS resuscitation. Mild cases of VAE
dence of subdural hemorrhage, with no cases of tension were significantly associated with suboccipital cranioto-
pneumocephalus. Within the 1010 included cervical spine my/craniectomy relative to DBS procedures (p = 0.001,
cases, there was a 0.7% incidence of clinically significant Table 4). Similarly, mild cases of VAE were also signifi-
VAE and 0.1% rate of tension pneumocephalus, with no cantly more frequent in intradural cervical spine cases (5
instances of significant postoperative hemorrhage. When of 54) as compared with extradural procedures (14 of 956;
separated into intradural and extradural cervical spine p = 0.0004, Table 4). There was not a significant associa-
cases, the rates of clinically significant VAE were 1.8% tion between moderate or severe VAE in comparing either
TABLE 1. Demographic data
Age in Yrs (range)
Procedure No. of Cases Women (%) Median Males Females
Overall 1792 736 (41) 54 (3–92) 56 (3–92) 51 (7–92)
Cervical 1010 354 (35) 54 (17–92) 55 (17–92) 51 (23–92)
DBS 332 125 (38) 62 (9–84) 62 (9–84) 64 (9–83)
Suboccipital 450 257 (57) 45 (3–83) 47 (3–81) 43 (7–83)
184 J Neurosurg Volume 127 • July 2017
Unauthenticated | Downloaded 09/05/20 03:42 PM UTC
Contemporary complications in the sitting position
TABLE 2. Overall and specific complication rates for sitting TABLE 3. Risk of complications in intradural cervical procedures
suboccipital craniotomies and DBS cases* compared with extradural cervical cases and sitting suboccipital
craniotomy/craniectomy cases
Complications p
Cranial Cases (%) OR 95% CI Value Complications p
Cervical Spine Cases (%) OR 95% CI Value
Overall 24 (3.1) 2.83 0.93–8.6 0.067
Suboccipital 15 (3.3) Overall 7 (0.7) 7.32 1.39–38.61 0.019
DBS 4 (1.2) Intradural 2 (3.7)
Moderate/severe VAE 9.07 1.17–70.09 0.035 Extradural 5 (0.5)
Suboccipital 12 (2.7) Moderate/severe VAE 3.59 0.41–31.27 0.247
DBS 1 (0.3) Intradural 1 (1.8)
Tension pneumo- 2.22 0.09–54.65 0.626 Extradural 5 (0.5)
cephalus Tension pneumo- 53.64 2.16–1332.35 0.015
Suboccipital 1 (0.2) cephalus
DBS 0 (0) Intradural 1 (1.8)
Hemorrhage 0.49 0.08–2.95 0.435 Extradural 0 (0)
Suboccipital 2 (0.4) Risk of moderate/ 0.69 0.09–5.40 0.723
DBS 3 (0.9) severe VAE
Intradural 1 (1.8)
* Odds ratios are presented comparing suboccipital craniotomy/craniectomy
to DBS for each complication and overall, along with a 95% CI and associated Suboccipital 12 (2.7)
p values.
extradural with intradural cervical cases or suboccipital cervical spine procedures and evaluated the incidence of
craniotomy/craniectomy with DBS cranial cases (Table 4). VAE as defined by a decrease in end-expired CO2 of more
than 4 mm Hg, characteristic sounds on Doppler ultraso-
Discussion nography, or any sign of air on TEE. The overall incidence
in their series was 19%. However, the incidence of VAE
Despite the potential advantages of the sitting position, causing hemodynamic or respiratory compromise was
hesitancy regarding its implementation persists among 3.3%, and only 1 in 200 cases had to be terminated due
some neurosurgeons and anesthesiologists, precluding its to VAE.15 Using a similar definition, Leslie et al. (2006)
widespread use. This negative stigma is partially due to in- found an overall incidence of 9%, also in a mixture of cer-
creased risk of VAE, but also due to other rare and severe vical and suboccipital cases.24 In contrast, Papadopoulos et
complications that have been attributed to sitting proce- al. (1994) prospectively reviewed 22 posterior fossa cases
dures. Our institution has an extensive history of perform- and 40 cervical spine cases, defining VAE solely by using
ing neurosurgical procedures in the sitting position.3,7,11 To TEE, and reported an incidence of 76% and 25%, respec-
better ascertain the true nature of these risks, we reviewed tively.31 However, the incidence of VAE detected in this
a large modern series (n = 1792, from January 1, 2000, manner is not known for other surgical positions.
until October 8, 2013) of various neurosurgical procedures Perhaps the most comprehensive study using variable
performed in the sitting position. The overall incidence definitions of VAE is that conducted by Feigl et al., who
of complications attributable to the sitting position was reviewed 200 consecutive semisitting neurosurgical cases
1.45%. The overall incidence of VAE requiring intraoper- in 2014. Using a graded scale, they found the incidence to
ative treatment was 1.1%. The incidence of VAE increased be 42.3% if a definition of the presence of air bubbles on
to 4.7% when all cases of VAE were included; however, TEE was used, compared with 3.8% if a decrease in end-
these additional occurrences responded to minimal field expired CO2 of more than 3 mm Hg was used and 1.9% if
interventions such as waxing bone edges, cauterizing ves- clinically significant changes (drop in mean arterial pres-
sels, or copious irrigation. No deaths resulted from any sure > 20% or increase in heart rate > 40%) were used.
of the observed complications, and only 2 procedures No VAEs resulted in hemodynamic instability requiring
(2/1794) were aborted due to intraoperative VAE. resuscitation.13 While series that use the most stringent of
definitions for VAE reveal that air passes into systemic
Venous Air Embolism circulation with no small frequency, it is worthy of note
The reported incidence of VAE during sitting neurosur- that comparably few VAEs involve adverse consequenc-
gical procedures is extremely variable in the literature and es. A review of 430 posterior fossa cases by Bithal et al.
largely depends on the way that VAE was defined, as well showed that 37% of VAEs (defined as a sustained decrease
as the patient population. The methods used to detect VAE in end-tidal CO2 by > 0.7 kPa) in adults and 33% in chil-
have also evolved over time.8,25 In our series, we empha- dren resulted in hypotension, and only in one instance was
sized clinically significant VAE, meaning a VAE resulting it necessary to abort a procedure.2 Furthermore, VAE is
in hemodynamic or respiratory compromise, or alteration a risk of any procedure in which the head is above the
of the course of the case. Recently, Ganslandt and col- heart, and there is scant literature to determine what the
leagues (2013) reviewed more than 600 suboccipital and exact incidence of VAE is in these cases. As reverse Tren-
J Neurosurg Volume 127 • July 2017 185
Unauthenticated | Downloaded 09/05/20 03:42 PM UTC
B. T. Himes et al.
TABLE 4. Severity of VAE stratified by procedure type*
Severity of Cervical
VAE Suboccipital DBS OR 95% CI p Value Intradural Extradural OR 95% CI p Value
Mild 38 8 3.74 1.72–8.12 0.001 5 14 6.87 2.38–19.83 0.0004
Moderate 9 1 6.75 0.85–53.58 0.071 1 5 3.59 0.41–31.27 0.247
Severe 3 0 5.2 0.28–101.04 0.276 0 0 — — —
* Cases were stratified as mild, moderate, or severe based on the following criteria: mild = diagnosis of VAE without clinical significance or need for pharmacological,
anesthetic, or surgical intervention; moderate = diagnosis of VAE with significant drop in end-tidal CO2 or requiring pressor support; severe = moderate criteria in addi-
tion to emergency repositioning or requiring ACLS resuscitation.
delenburg positioning is very commonly employed to re- air.10 A larger study conducted by Standefar et al. of 488
duce brain swelling, VAE has been reported in horizontal cases found that only 8 patients (1.6%) developed symp-
neurosurgical cases, although the incidence is higher with tomatic pneumocephalus, none of whom required twist-
sitting procedures.12 drill bur hole and aspiration through a subdural catheter
Interestingly, the incidence of VAE appears to differ to relieve pressure.37
with the type of procedure as well. We found that cranial
cases, both suboccipital craniotomies (2.7%) and intradural Subdural and Remote Hemorrhages
cervical spine cases (1.8%), had higher incidences of clini- The development of subdural hemorrhage was exceed-
cally significant VAE compared with DBS cases (0.3%) ingly rare in the present series. No subdural hematomas
and extradural cervical cases (0.5%). While the reasons for occurred after cervical cases, and 5 patients developed a
these findings are not entirely clear, they have also been subdural hematoma after a cranial case (3 DBS cases and
borne out in other series.12,15 In a meta-analysis of more 2 posterior fossa cases). Standefar et al. also reported a low
than 4000 cases, Fathi et al. found a nearly 3-fold increase subdural hematoma rate (0.6% after all cases and 1.3%
in the incidence of VAE during posterior fossa procedures
after posterior fossa cases) following sitting procedures.37
compared with cervical cases.12 The incidence in 467 DBS
Presumably, the cause for subdural hematomas is related
cases was 1.3% as reported by Chang et al.6 Additionally,
the type of suboccipital craniotomy may also play a role, to mechanical displacement of the brain resulting in tear-
as Yonekawa and colleagues reported higher rates with lat- ing of bridging veins. While this appears to be a logical
eral approaches (21% vs 8%).43 The incidence rate may also explanation, it does not fully explain the findings of re-
vary with operative time, as 1 study that reviewed the util- mote intraparenchymal or epidural hemorrhages that have
ity of image guidance with lateral suboccipital craniotomy been observed after sitting procedures.4,22,30 Furthermore,
found lower incidences of VAE (8% vs 19%) and faster op- it is debatable as to whether the sitting position truly leads
erative times (21 vs 39 minutes) in cases that used image to an increase in these complications, as these complica-
guidance compared with cases in which this technology tions are observed in more conventional positions as well.
was not used.16 However, it should be noted that cases us- Although Brisman et al. found that 87% of remote hemor-
ing image guidance had lower rates of venous sinus injury rhages occurred in the sitting procedures in his review of
that may also account for this difference. The difference in the literature, a large series by Kalfas and Little that re-
risks may in part be explained by lower degrees of inva- viewed nearly 5000 supratentorial and infratentorial cases
siveness given that craniotomies/craniectomies have great- did not find an increased risk with the sitting position.4,22
er risk than DBS procedures. Cerebrospinal fluid egress
also likely plays a role as the cervical cases in this series Other Neurological and Rare Complications
were mostly decompressive laminectomies and forami- Although no neurological complications were directly
notomies, with a smaller representation of intradural pro- attributable to the sitting position in our series, a variety
cedures in which a higher, but not statistically significant, of neurological complications have been described as a re-
rate of clinically significant VAE was observed. sult of its use.19,23,27,29,38,41 Sciatic nerve palsies have been
described with the use of the sitting position.23,41 Other
Pneumocephalus cranial nerve palsies have also been described such as
Pneumocephalus is a common occurrence with any delayed lateral rectus palsies and anosmia.34,38 These re-
cranial procedure, and is a gravity-dependent phenom- ported complications range from minor complications
enon. Thus, it is not surprising that the reported incidence such as peripheral and cranial nerve palsies to devastat-
of pneumocephalus after sitting procedures is higher than ing complications such as cervical quadriplegia. Periph-
procedures performed in the horizontal position.40 Howev- eral nerve palsies that have been described due to the sit-
er, tension pneumocephalus, a potential expanding volume ting position include sciatic nerve injury.34,35,38 One of the
of air that results in an increase in intracranial pressure, is most feared complications is cervical quadriplegia due
rare and is not necessarily unique to sitting neurosurgical to cord stretch.42 Both cord infarction and quadriparesis
cases.20,33,39 Di Lorenzo conducted a prospective study of have been described.19,27,29 While such complications are
30 cases and found a 100% occurrence of pneumocepha- likely exceedingly rare, they do emphasize the necessity
lus, although no patient suffered tension pneumocephalus for meticulous positioning and support the use of monitor-
or any neurological symptom as the result of intracranial ing (motor and somatosensory evoked potentials) for pre-
186 J Neurosurg Volume 127 • July 2017
Unauthenticated | Downloaded 09/05/20 03:42 PM UTC
Contemporary complications in the sitting position
vention. Other rare complications that have been reported is higher in suboccipital cases relative to DBS procedures.
after sitting procedures include acute parotitis, pyriformis While a higher rate of clinically significant VAE was ob-
syndrome, and tension pneumoventricle.1,5,18 We did not served in intradural cervical cases relative to extradural
observe these complications in this series, and our series ones, it did not reach statistical significance. There was,
likely represents a more modern approach to these cases however, a significantly higher rate of mild VAE in intra-
compared with the prior report. Additionally, consequenc- dural cases. When appropriately used, the sitting position
es of VAE such as paradoxical emboli in the presence of provides a safe means of surgical access.
patent foramen ovale (PFO) or due to right-to-left intra-
pulmonary shunting and fatal coagulopathy have been de- Acknowledgments
scribed.12,17,26,36 Due to the risk of paradoxical emboli, the
We would like to acknowledge Dr. Guiseppe Lanzino and Dr.
presence of PFO is considered a contraindication to the Kendall Lee, who contributed cases to this series and aided in the
sitting position by some, and efforts have been undertaken preparation of this paper.
to identify patients undergoing sitting procedures where
there may be a PFO.9 However, in a series of 200 patients
undergoing semisitting procedures, 52 of whom had a References
PFO, no instances of paradoxical emboli were reported by 1. Berker M, Sahin A, Aypar U, Ozgen T: Acute parotitis fol-
Feigl et al. using modern protocols for VAE detection.13 lowing sitting position neurosurgical procedures: review of
five cases. J Neurosurg Anesthesiol 16:29–31, 2004
2. Bithal PK, Pandia MP, Dash HH, Chouhan RS, Mohanty B,
Limitations of the Study Padhy N: Comparative incidence of venous air embolism
The present series has value in its large sample size and associated hypotension in adults and children operated
and derivation from a prospectively collected morbidity for neurosurgery in the sitting position. Eur J Anaesthesiol
and mortality database. However, because the database is 21:517–522, 2004
maintained by neurosurgical staff, attention to anesthetic 3. Black S, Ockert DB, Oliver WC Jr, Cucchiara RF: Outcome
following posterior fossa craniectomy in patients in the sit-
complications (such as delayed extubation or macroglos- ting or horizontal positions. Anesthesiology 69:49–56, 1988
sia) would likely not be captured in this cohort. Thus, the 4. Brisman MH, Bederson JB, Sen CN, Germano IM, Moore F,
overall complication rate may well be higher if all anesthet- Post KD: Intracerebral hemorrhage occurring remote from
ic-related complications are considered. Additionally, our the craniotomy site. Neurosurgery 39:1114–1122, 1996
definition of VAE makes it difficult to compare incidences 5. Brown JA, Braun MA, Namey TC: Pyriformis syndrome in a
among other institutions or other series that may use more 10-year-old boy as a complication of operation with the pa-
stringent definitions. We did endeavor to separately review tient in the sitting position. Neurosurgery 23:117–119, 1988
the intraoperative anesthesia data to assess the incidence of 6. Chang EF, Cheng JS, Richardson RM, Lee C, Starr PA, Lar-
son PS: Incidence and management of venous air embolisms
VAE from a different perspective to address these issues. during awake deep brain stimulation surgery in a large clini-
The lack of any set criteria in the selection of patients to cal series. Stereotact Funct Neurosurg 89:76–82, 2011
undergo surgery in the sitting position may also present a 7. Cucchiara RF, Bowers B: Air embolism in children undergo-
confounding variable. Similarly, the variability of methods ing suboccipital craniotomy. Anesthesiology 57:338–339,
used to detect VAE (such as the use of TEE in suboccipital 1982
cases but not in DBS) may lead to some ascertainment bias 8. Cucchiara RF, Nugent M, Seward JB, Messick JM: Air em-
in the detection of mild VAE. However, this variation is un- bolism in upright neurosurgical patients: detection and local-
ization by two-dimensional transesophageal echocardiogra-
likely to obscure the detection of moderate or severe cases phy. Anesthesiology 60:353–355, 1984
of VAE as these cases involved some evidence of hemo- 9. Cucchiara RF, Seward JB, Nishimura RA, Nugent M, Faust
dynamic instability requiring intervention. Lastly, the het- RJ: Identification of patent foramen ovale during sitting posi-
erogeneity of procedures (cervical, suboccipital, and DBS tion craniotomy by transesophageal echocardiography with
cases) may also preclude direct comparisons to other prior positive airway pressure. Anesthesiology 63:107–109, 1985
series that did not include these specific types of procedures. 10. Di Lorenzo N, Caruso R, Floris R, Guerrisi V, Bozzao L,
We used data from a neurosurgical morbidity and mortality Fortuna A: Pneumocephalus and tension pneumocephalus
database, and events that may have occurred at a later time after posterior fossa surgery in the sitting position: a prospec-
tive study. Acta Neurochir (Wien) 83:112–115, 1986
(past the first 30 days postoperatively) were unlikely to be 11. Duke DA, Lynch JJ, Harner SG, Faust RJ, Ebersold MJ: Ve-
captured. Future study assessing the risk factors for compli- nous air embolism in sitting and supine patients undergoing
cations among different procedure types would be of value vestibular schwannoma resection. Neurosurgery 42:1282–
to better understand which subset of patients is truly at risk 1287, 1998
to further mitigate the risk of these complications. 12. Fathi AR, Eshtehardi P, Meier B: Patent foramen ovale and
neurosurgery in sitting position: a systematic review. Br J
Anaesth 102:588–596, 2009
Conclusions 13. Feigl GC, Decker K, Wurms M, Krischek B, Ritz R, Unertl
In this large, modern series of cases performed in the K, et al: Neurosurgical procedures in the semisitting position:
sitting position, the overall rate of complications was quite evaluation of the risk of paradoxical venous air embolism
in patients with a patent foramen ovale. World Neurosurg
low. No neurological deficits were observed directly as a 81:159–164, 2014
result of positioning (i.e., quadriplegia). While the risk of 14. Gale T, Leslie K: Anaesthesia for neurosurgery in the sitting
VAE has been shown to be higher in sitting procedures, position. J Clin Neurosci 11:693–696, 2004
the overall risk of clinically significant VAE in this study 15. Ganslandt O, Merkel A, Schmitt H, Tzabazis A, Buchfelder
was small at 1.1%. The risk of clinically significant VAE M, Eyupoglu I, et al: The sitting position in neurosurgery:
J Neurosurg Volume 127 • July 2017 187
Unauthenticated | Downloaded 09/05/20 03:42 PM UTC
B. T. Himes et al.
indications, complications and results. A single institution anosmia: a hitherto undescribed complication following sur-
experience of 600 cases. Acta Neurochir (Wien) 155:1887– gery of the posterior cranial fossa in the sitting position. Acta
1893, 2013 Neurochir (Wien) 139:482–483, 1997
16. Gharabaghi A, Rosahl SK, Feigl GC, Safavi-Abbasi S, 35. Ramsbacher J, Vesper J, Brock M: Permanent postoperative
Mirzayan JM, Heckl S, et al: Image-guided lateral suboccipi- anosmia: a serious complication of neurovascular decom-
tal approach: part 2-impact on complication rates and opera- pression in the sitting position. Acta Neurochir (Wien)
tion times. Neurosurgery 62 (3 Suppl 1):24–29, 2008 142:1259–1261, 2000
17. Girard F, Ruel M, McKenty S, Boudreault D, Chouinard P, 36. Schlundt J, Tzanova I, Werner C: A case of intrapulmonary
Todorov A, et al: Incidences of venous air embolism and transmission of air while transitioning a patient from a sitting
patent foramen ovale among patients undergoing selective to a supine position after venous air embolism during a crani-
peripheral denervation in the sitting position. Neurosurgery otomy. Can J Anaesth 59:478–482, 2012
53:316–320, 2003 37. Standefer M, Bay JW, Trusso R: The sitting position in neu-
18. Gonçalves MB, Nunes CF, Melo JO Jr, Guimarães RD, rosurgery: a retrospective analysis of 488 cases. Neurosur-
Klescoski J Jr, Landeiro JA: Tension pneumoventricle after gery 14:649–658, 1984
resection of a fourth ventricle choroid plexus papilloma: An 38. Stevens QE, Colen CB, Ham SD, Kattner KA, Sood S: De-
unusual postoperative complication. Surg Neurol Int 3:116, layed lateral rectus palsy following resection of a pineal cyst
2012 in sitting position: direct or indirect compressive phenom-
19. Haisa T, Kondo T: Midcervical flexion myelopathy after pos- enon? J Child Neurol 22:1411–1414, 2007
terior fossa surgery in the sitting position: case report. Neu- 39. Suri A, Mahapatra AK, Singh VP: Posterior fossa tension
rosurgery 38:819–822, 1996 pneumocephalus. Childs Nerv Syst 16:196–199, 2000
20. Hernández-Palazo NJ, Nuño de la Rosa-Carrillo V, Martinez- 40. Toung TJ, McPherson RW, Ahn H, Donham RT, Alano J,
Lage JF, López-Hernández F, Pérez-Espejo MA: [Tension Long D: Pneumocephalus: effects of patient position on the
pneumocephalus after intracranial surgery in the supine posi- incidence and location of aerocele after posterior fossa and
tion.] Neurocirugia (Astur) 15:596–599, 2004 (Span) upper cervical cord surgery. Anesth Analg 65:65–70, 1986
21. Hooper AK, Okun MS, Foote KD, Haq IU, Fernandez HH, 41. Wang JC, Wong TT, Chen HH, Chang PY, Yang TF: Bi-
Hegland D, et al: Venous air embolism in deep brain stimula- lateral sciatic neuropathy as a complication of craniotomy
tion. Stereotact Funct Neurosurg 87:25–30, 2009 performed in the sitting position: localization of nerve injury
22. Kalfas IH, Little JR: Postoperative hemorrhage: a survey of by using magnetic resonance imaging. Childs Nerv Syst
4992 intracranial procedures. Neurosurgery 23:343–347, 28:159–163, 2012
1988 42. Wilder BL: Hypothesis: the etiology of midcervical quad-
23. Konovalov AN, Lubnin AI, Shimanskiĭ VN, Kolycheva MV, riplegia after operation with the patient in the sitting position.
Ogurtsova AA, Grigorian AA: [Positional damage of the Neurosurgery 11:530–531, 1982
sciatic nerve during neurosurgical intervention into the pos- 43. Yonekawa Y: [Operative neurosurgery: personal view and
terior cranial fossa in the sitting position.] Anesteziol Reani- historical backgrounds (8) suboccipital craniotomy-sitting
matol 3:58–60, 2009 (Russian) position-linear incision.] No Shinkei Geka 39:789–809, 2011
24. Leslie K, Hui R, Kaye AH: Venous air embolism and the (Jpn)
sitting position: a case series. J Clin Neurosci 13:419–422,
2006
25. Michenfelder JD, Miller RH, Gronert GA: Evaluation of an
ultrasonic device (Doppler) for the diagnosis of venous air Disclosures
embolism. Anesthesiology 36:164–167, 1972 The authors report no conflict of interest concerning the materi-
26. Moningi S, Kulkarni D, Bhattacharjee S: Coagulopathy fol- als or methods used in this study or the findings specified in this
lowing venous air embolism: a disastrous consequence -a paper.
case report-. Korean J Anesthesiol 65:349–352, 2013
27. Morandi X, Riffaud L, Amlashi SF, Brassier G: Extensive Author Contributions
spinal cord infarction after posterior fossa surgery in the sit- Conception and design: Van Gompel, Himes, Mallory, Abcejo.
ting position: case report. Neurosurgery 54:1512–1516, 2004 Acquisition of data: Himes, Mallory, Abcejo, Pasternak, Atkin-
28. Mostafa RM, Mejadi A: Quadriplegia after interscalene son, Meyer, Marsh, Link, Clarke. Analysis and interpretation of
block for shoulder surgery in sitting position. Br J Anaesth data: Himes, Mallory, Abcejo. Drafting the article: Van Gompel,
111:846–847, 2013 Himes, Mallory, Abcejo, Pasternak. Critically revising the article:
29. Nitta H, Yamashita J, Nomura M, Igarashi N: Cervical spinal Van Gompel, Himes, Mallory, Abcejo, Pasternak, Atkinson,
cord infarction after surgery for a pineal region choriocar- Meyer, Clarke, Perkins. Reviewed submitted version of manu-
cinoma in the sitting position: case report. Neurosurgery script: Van Gompel, Himes, Mallory, Abcejo, Pasternak, Atkin-
40:1082–1086, 1997 son, Meyer, Marsh, Clarke, Perkins. Approved the final version of
30. Pandey P, Madhugiri VS, Sattur MG, Devi B I: Remote su- the manuscript on behalf of all authors: Van Gompel. Statistical
pratentorial extradural hematoma following posterior fossa analysis: Himes, Mallory.
surgery. Childs Nerv Syst 24:851–854, 2008
31. Papadopoulos G, Kuhly P, Brock M, Rudolph KH, Link J, Supplemental Information
Eyrich K: Venous and paradoxical air embolism in the sitting Previous Presentations
position. A prospective study with transoesophageal echocar-
diography. Acta Neurochir (Wien) 126:140–143, 1994 Portions of this work were presented as a platform presentation
32. Porter JM, Pidgeon C, Cunningham AJ: The sitting position at the 2014 AANS Annual Scientific Meeting in San Francisco,
in neurosurgery: a critical appraisal. Br J Anaesth 82:117– California, April 7, 2014.
128, 1999
33. Prabhakar H, Bithal PK, Garg A: Tension pneumocephalus Correspondence
after craniotomy in supine position. J Neurosurg Anesthe- Jamie J. Van Gompel, Department of Neurosurgery, Mayo Clinic,
siol 15:278–281, 2003 200 First St. SW, Rochester, MN 55905. email: vangompel.
34. Ramsbacher J, Brock M, Kombos T: Permanent postoperative jamie@mayo.edu.
188 J Neurosurg Volume 127 • July 2017
Unauthenticated | Downloaded 09/05/20 03:42 PM UTC
You might also like
- Carotid Endarterectomy: Experience in 8743 Cases.Document13 pagesCarotid Endarterectomy: Experience in 8743 Cases.Alexandre Campos Moraes AmatoNo ratings yet
- Anesthetic Management in Pediatric General Surgery: Evolving and Current ConceptsFrom EverandAnesthetic Management in Pediatric General Surgery: Evolving and Current ConceptsSusan T. VergheseNo ratings yet
- Anesthesia Management of Ophthalmic Surgery in Geriatric Patients PDFDocument11 pagesAnesthesia Management of Ophthalmic Surgery in Geriatric Patients PDFtiaraleshaNo ratings yet
- Anterior Cervical Discectomy and FusionDocument7 pagesAnterior Cervical Discectomy and FusionGeraldine Alvarez ANo ratings yet
- Cardiac Arrest in The Operating Room (2012)Document6 pagesCardiac Arrest in The Operating Room (2012)patricia.untoroNo ratings yet
- Medical Terminology - The Language of Health CareDocument670 pagesMedical Terminology - The Language of Health CareMisty TranquilNo ratings yet
- Urgent Repositioning After Venous Air Embolism During Intracranial Surgery in The Seated PositionDocument9 pagesUrgent Repositioning After Venous Air Embolism During Intracranial Surgery in The Seated PositionwprbpwsczzNo ratings yet
- Pi Is 0003497505009550Document7 pagesPi Is 0003497505009550pbchantaNo ratings yet
- Clinical Review: Management of Weaning From Cardiopulmonary Bypass After Cardiac SurgeryDocument18 pagesClinical Review: Management of Weaning From Cardiopulmonary Bypass After Cardiac SurgeryAdilZyaniNo ratings yet
- Pda Ev Ejtcs 04Document7 pagesPda Ev Ejtcs 04emmanuel le bretNo ratings yet
- Legnani 2013Document6 pagesLegnani 2013wedawisnawaNo ratings yet
- J Surneu 2005 04 039Document7 pagesJ Surneu 2005 04 039MohitNo ratings yet
- neurosurg-focus-article-pE2Document9 pagesneurosurg-focus-article-pE2whistle.blowersl.associationNo ratings yet
- Eco in Cardiac Sugrery Anesthesic 1-s2.0-S1053077020305875-MainDocument11 pagesEco in Cardiac Sugrery Anesthesic 1-s2.0-S1053077020305875-MainCésar Marriaga ZárateNo ratings yet
- Endarterectomia 2Document12 pagesEndarterectomia 2Andrea RangelNo ratings yet
- Readmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsDocument9 pagesReadmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsbobNo ratings yet
- 19 - Capítulo 4.2 - 2-Zhang e Colaboradores 2022Document13 pages19 - Capítulo 4.2 - 2-Zhang e Colaboradores 2022CharleneNo ratings yet
- Jnic 2019 00213 PDFDocument6 pagesJnic 2019 00213 PDFAwal13 ArigaNo ratings yet
- Minimally Invasive Perventricular Device Occlusion Versus Surgical Closure For Treating Perimembranous Ventricular Septal DefectDocument10 pagesMinimally Invasive Perventricular Device Occlusion Versus Surgical Closure For Treating Perimembranous Ventricular Septal DefectRinzyNo ratings yet
- Complications of Posterior Cranial Fossa PDFDocument7 pagesComplications of Posterior Cranial Fossa PDFemilio9fernandez9gatNo ratings yet
- Comparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourDocument9 pagesComparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourtasyadelizaNo ratings yet
- Laringo y BroncoespasmoDocument4 pagesLaringo y BroncoespasmoLUIS FERNANDO GOMEZ CANONo ratings yet
- Bernard D. Prendergast and Pilar Tornos: Surgery For Infective Endocarditis: Who and When?Document26 pagesBernard D. Prendergast and Pilar Tornos: Surgery For Infective Endocarditis: Who and When?om mkNo ratings yet
- Post MI VSD Article FinalDocument19 pagesPost MI VSD Article FinalPooja JakharNo ratings yet
- Complications Predicting Perioperative Mortality in Patients Undergoing Elective Craniotomy A Population Based StudyDocument11 pagesComplications Predicting Perioperative Mortality in Patients Undergoing Elective Craniotomy A Population Based Study49hr84j7spNo ratings yet
- Anesthesia For Carotid Endarterectomy: Where Do We Stand at Present?Document12 pagesAnesthesia For Carotid Endarterectomy: Where Do We Stand at Present?Lil_QuinceNo ratings yet
- 2 5373127936972950922Document6 pages2 5373127936972950922teguh sNo ratings yet
- Choi 2013Document6 pagesChoi 2013arun gowdaNo ratings yet
- Swanson 2007Document5 pagesSwanson 2007Giancarlo Maruri MunarettoNo ratings yet
- Perioperative Stroke BJA 2021Document7 pagesPerioperative Stroke BJA 2021lim sjNo ratings yet
- Eer 4 1 90 102Document13 pagesEer 4 1 90 102bakkouriyacineNo ratings yet
- Spinal vs. General Anesthesia For Percutaneous Nephrolithotomy: A Prospective Randomized TrialDocument5 pagesSpinal vs. General Anesthesia For Percutaneous Nephrolithotomy: A Prospective Randomized TrialDella Puspita SariNo ratings yet
- Munro Dan Christiansen, 2015Document33 pagesMunro Dan Christiansen, 2015Jonathan LucisNo ratings yet
- Percutaneous Aortic Valve Implantation: The Anesthesiologist PerspectiveDocument11 pagesPercutaneous Aortic Valve Implantation: The Anesthesiologist Perspectiveserena7205No ratings yet
- Pulmonary Endarterectomy: Experience and Lessons Learned in 1,500 CasesDocument8 pagesPulmonary Endarterectomy: Experience and Lessons Learned in 1,500 CasesRoxana Maria MunteanuNo ratings yet
- J Jpedsurg 2008 06 024Document1 pageJ Jpedsurg 2008 06 024afsdsaadsNo ratings yet
- Hefler Et Al., 2009Document4 pagesHefler Et Al., 2009Jonathan LucisNo ratings yet
- 8-3-353Document6 pages8-3-353houmaishag77No ratings yet
- Incidence of Venous Air Embolism During Craniectomy For Craniosynostosis RepairDocument4 pagesIncidence of Venous Air Embolism During Craniectomy For Craniosynostosis RepairFika Khulma SofiaNo ratings yet
- Endovascular Stentgraft Placement in Aortic Dissection A MetaanalysisDocument10 pagesEndovascular Stentgraft Placement in Aortic Dissection A MetaanalysisCiubuc AndrianNo ratings yet
- (10920684 - Neurosurgical Focus) Space-Occupying Cerebellar Infarction - Complications, Treatment, and OutcomeDocument13 pages(10920684 - Neurosurgical Focus) Space-Occupying Cerebellar Infarction - Complications, Treatment, and OutcomeDiệp TâmNo ratings yet
- Jurnal KardioDocument5 pagesJurnal KardiomadeNo ratings yet
- 2017 7 Peds17155Document7 pages2017 7 Peds17155Kiky Martha A.No ratings yet
- Kepler 2018Document12 pagesKepler 2018Dede NovHyNo ratings yet
- Nej MR A 1916801Document12 pagesNej MR A 1916801bagholderNo ratings yet
- Clinical Review: Hemodynamic Monitoring in The Intensive Care UnitDocument8 pagesClinical Review: Hemodynamic Monitoring in The Intensive Care Unitmasfak97No ratings yet
- Epidermoid Cysts TNEDocument10 pagesEpidermoid Cysts TNEbello_england_209552No ratings yet
- 508 - 7 CardiologyDocument9 pages508 - 7 CardiologymlinaballerinaNo ratings yet
- 3 s2.0 B978032375929800040XDocument19 pages3 s2.0 B978032375929800040XClaudia IsabelNo ratings yet
- Ecocardiografia Monitoreo Hemodinamico en Critico..Document12 pagesEcocardiografia Monitoreo Hemodinamico en Critico..cositaamorNo ratings yet
- Evidence-Based Perioperative Medicine (EBPOM) : A Summary of The 8th EBPOM Conference 2009Document6 pagesEvidence-Based Perioperative Medicine (EBPOM) : A Summary of The 8th EBPOM Conference 2009ashut1No ratings yet
- Risk Model DialysiddssssDocument7 pagesRisk Model DialysiddssssDumitru GrozaNo ratings yet
- JTD 13 03 1886Document13 pagesJTD 13 03 1886Nongnapat KettungmunNo ratings yet
- Journal of Clinical Anesthesia: Original ContributionDocument6 pagesJournal of Clinical Anesthesia: Original Contributionpooria shNo ratings yet
- Short - and Long-Term Outcomes at A Single InstitutionDocument7 pagesShort - and Long-Term Outcomes at A Single InstitutionJonathan Frimpong AnsahNo ratings yet
- Performance and Safety of Diagnostic Procedures in Superior Vena Cava SyndromeDocument4 pagesPerformance and Safety of Diagnostic Procedures in Superior Vena Cava SyndromesukiyantoNo ratings yet
- Anestesia Espinal para Cirugía de Corta Estancia en Cirugía Plástica 9Document23 pagesAnestesia Espinal para Cirugía de Corta Estancia en Cirugía Plástica 9Paulo TorresNo ratings yet
- Bmri2016 3741426Document7 pagesBmri2016 3741426MandaNo ratings yet
- Contents OcnaDocument4 pagesContents OcnaGirish SubashNo ratings yet
- 05.03 - Interventional Neuroradiology PDFDocument113 pages05.03 - Interventional Neuroradiology PDFBivolaru AlinNo ratings yet
- Atlas of 3D Transesophageal Echocardiography in Structural Heart Disease Interventions: Cases and VideosFrom EverandAtlas of 3D Transesophageal Echocardiography in Structural Heart Disease Interventions: Cases and VideosNo ratings yet
- 2008 Article 9145-2 PDFDocument7 pages2008 Article 9145-2 PDFDeborah González GarcíaNo ratings yet
- Laser and Cryosurgery MADE EASYDocument6 pagesLaser and Cryosurgery MADE EASYMohammedNo ratings yet
- Tmi Lumbar Fusion Rehabilitation ProtocolDocument2 pagesTmi Lumbar Fusion Rehabilitation ProtocolJackyNo ratings yet
- Megagen AnyRidgeDocument87 pagesMegagen AnyRidgeFloare79No ratings yet
- CT of The Paranasal Sinuses Normal Anatomyvariants and PathologyDocument10 pagesCT of The Paranasal Sinuses Normal Anatomyvariants and PathologyAndi FirdaNo ratings yet
- Prospectus New India Floater Mediclaim 21012020 - 1Document20 pagesProspectus New India Floater Mediclaim 21012020 - 1mail2sranjanNo ratings yet
- Innervation of The Posterior Hip Capsule, A Cadaveric StudyDocument8 pagesInnervation of The Posterior Hip Capsule, A Cadaveric StudyValentín ThomasNo ratings yet
- Standard Operating Procedures For Hospitals (SOP) - 10Document1 pageStandard Operating Procedures For Hospitals (SOP) - 10AnonymousNo ratings yet
- Prognostic Factors Affecting The Mortality of Burn Injuries Patients in Dr. Sardjito General Hospital, Yogyakarta, IndonesiaDocument8 pagesPrognostic Factors Affecting The Mortality of Burn Injuries Patients in Dr. Sardjito General Hospital, Yogyakarta, IndonesiaYeni PuspitasariNo ratings yet
- Surgical Suture Materials Are Used in The Closure of Most Wound Types. The Ideal SutureDocument9 pagesSurgical Suture Materials Are Used in The Closure of Most Wound Types. The Ideal SutureToria053No ratings yet
- Colostomy Care ReviseDocument6 pagesColostomy Care ReviseMeryl Mae RamosNo ratings yet
- Reconstructive Plastic Surgery of PressuDocument291 pagesReconstructive Plastic Surgery of Pressurus gheorghe catalinNo ratings yet
- Open Bite Correction Made Easy PDFDocument3 pagesOpen Bite Correction Made Easy PDFVieussens JoffreyNo ratings yet
- Histology Report 10-06-2022Document2 pagesHistology Report 10-06-2022chloedee30No ratings yet
- Care of The Older Adult - SAS 3Document4 pagesCare of The Older Adult - SAS 3Gia Lourdes Camille AustriaNo ratings yet
- Maingot's Abdominal Operations, 8th Edition, Vol. 1 & 2: Annals of Surgery November 1986Document3 pagesMaingot's Abdominal Operations, 8th Edition, Vol. 1 & 2: Annals of Surgery November 1986Julio LeviNo ratings yet
- Nursing Documentation: Your License May Depend On It!Document146 pagesNursing Documentation: Your License May Depend On It!shenric16No ratings yet
- NABH QI ListDocument9 pagesNABH QI ListMangesh VirkarNo ratings yet
- Or-01-005 Surgical Safety ChecklistDocument3 pagesOr-01-005 Surgical Safety ChecklistOHHC ORNo ratings yet
- Book Review: Skull FractureDocument2 pagesBook Review: Skull FractureMohammad AkheelNo ratings yet
- NOE FractureDocument71 pagesNOE FractureAlex HaileyesusNo ratings yet
- Obeid Specialized Hospital - Riyadh: Key Performance Indiactors Second Quarter - 2019Document29 pagesObeid Specialized Hospital - Riyadh: Key Performance Indiactors Second Quarter - 2019LovelydePerioNo ratings yet
- Performance Outcomes After Surgical Repair of Achilles Tendon Rupture in WNBADocument6 pagesPerformance Outcomes After Surgical Repair of Achilles Tendon Rupture in WNBAJoan Obiol FiblaNo ratings yet
- Ethiopian Hospital Services Trasformation Guidelines (Ehstg)Document112 pagesEthiopian Hospital Services Trasformation Guidelines (Ehstg)Ezana50% (2)
- The Pattern of Branching and Intercommunications of The Musculocutaneous Nerve For Surgical Issues Anatomical StudyDocument9 pagesThe Pattern of Branching and Intercommunications of The Musculocutaneous Nerve For Surgical Issues Anatomical StudyProf. Hesham N. MustafaNo ratings yet
- Clinical Examination EyeDocument2 pagesClinical Examination EyeKirti JamwalNo ratings yet
- Diagnosis of Urethral Stricture On Dynamic Voiding Transvaginal Sonourethrography: A Case ReportDocument4 pagesDiagnosis of Urethral Stricture On Dynamic Voiding Transvaginal Sonourethrography: A Case ReportSri PertiwiNo ratings yet
- Sclerotherapy: Treatment of Varicose Telangiectatic Leg VeinsDocument439 pagesSclerotherapy: Treatment of Varicose Telangiectatic Leg VeinsjesussalvadorsuazaNo ratings yet
- University of Pangasinan Phinma Education Network Arellano ST., Dagupan CityDocument5 pagesUniversity of Pangasinan Phinma Education Network Arellano ST., Dagupan CitymyannbeguasNo ratings yet