Professional Documents
Culture Documents
Routine Prostate Biopsies Following Radiotherapy For Prostate Cancer: Results For 226 Patients
Routine Prostate Biopsies Following Radiotherapy For Prostate Cancer: Results For 226 Patients
Uploaded by
StirOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Routine Prostate Biopsies Following Radiotherapy For Prostate Cancer: Results For 226 Patients
Routine Prostate Biopsies Following Radiotherapy For Prostate Cancer: Results For 226 Patients
Uploaded by
StirCopyright:
Available Formats
ROUTINE PROSTATE BIOPSIES FOLLOWING
RADIOTHERAPY FOR PROSTATE CANCER:
RESULTS FOR 226 PATIENTS
J.M. CROOK, M.D.
G.A. PERRY, M.D.
S. ROBERTSON, M.D.
B.A. ESCHE, M.D.
From the Department of Radiation Oncology, Ottawa Regional Cancer Centre,
and the Department of Pathology, Ottawa General Hospital, Ottawa, Canada
ABSTRACT-Objectives. To determine the time course of histologic resolution of
prostate cancer following radiotherapy (RT) and to correlate biopsy results with clinical
outcome.
Methods. Since July 1990, all patients treated with radical external beam RT for
prostate cancer at the General Division of the Ottawa Regional Cancer Centre have had
systematic transrectal ultrasound (TRUS) and TRUS-guided biopsies beginning 12
months after RT and then every 6 months until negative or until clinical failure. Thus,
226 patients have had 375 TRUS with four to seven specimens per examination. Stage
distribution was Tl b: 32, Tl c: 1 1, T2a: 45, T2b: 82, T3: 50, and T4: 6. Median fol-
low-up was 33 months.
Results. Biopsy results were negative in 69.5% of patients by 30 months of follow-
up. Thirty-two (14%) had local failure (Tl b: 12.5%, Tl c: 0%, T2a: 1 1 %, T2b: 15%, T3:
18%, T4: 33%). Seven (3%) had chemical failure, and 47 (21%) had biopsy-only fail-
ure. Median follow-up for the biopsy-only failure group is only 19.5 months and mean
prostate-specific antigen (PSA) is 1 .O ng/mL. Thirty-nine patients, initially with biopsy-
only failure, have converted to negative biopsies at a median of 26 months. Nadir PSA
for patients with local failure was 3.9 ng/mL at 14 months versus 0.7 ng/mL at 23
months for those without failure. Patients with late conversion to negative biopsy re-
sults had a later nadir PSA of 1.3 ng/mL at 27.3 months. \ ~\_ \
Conclusions. Routine prostate biopsy specimens after RT in an unselected ‘population
show tumor clearance that is in agreement with long-term clinical follow-up, although
tumor may take more than 30 months to resolve. Nadir PSA can be used to predict
outcome.
External beam radiotherapy CRT) is the most Clinical follow-up after RT may be unreliable.
commonly used potentially curative treatment for The use of prostate-specific antigen (PSA) is rou-
carcinoma of the pr0state.i In general, patients se- tine, but a rising PSA may signal either local or
lected for radiation are 5 to 10 years older than distant recurrence. Prostate biopsy is logically the
those selected for radical prostatectomy,2 have gold standard for determination of local failure
more advanced local disease, and are of unknown but both the indications and interpretation of
nodal status. Despite a clearly less favorable pa- biopsy specimens are controversial.4 Several re-
tient population, clinical results at 10 years are ports on selective post-RT biopsies, often includ-
equivalent to those for surgery.lm3 ing patients who had biopsies a few months after
treatment or in whom residual disease is sus-
Submitted (Rapid Communication): November 17, 1994, pected, have shown very high positive biopsy
accepted (with revisions): December 5, 1994 rates.5-7 Such reports cast doubts on the efficacy
624 U ROLOGP /APRIL 1995 I VOLUME45, NUMBER4
TABLE I. TNM staging for prostate cancer (1 992)21
Stage Definition or Criteria for Inclusion
Tl Clinically inapparent tumor, not palpable nor visible by imaging
Tla Tumor an incidental histologic finding; <5% of tissue resected
Tlb Tumor an incidental histologic finding; > 5% of tissue resected
Tic Tumor identified by needle biopsy (eg, because of elevated serum PSA)
T2 Confined within the prostate
T2a Tumor involves half of a lobe or less
T2b Tumor involves more than half of a lobe but not both lobes
T2c Tumor involves both lobes
T3 Tumor extends through the prostate capsule
T3a Unilateral extracapsular extension
T3b Bilateral extracapsular extension
T3c Tumor invades seminal vesicle(s)
T4 Tumor is fixed or invades adjacent structures other than seminal vesicles
T4a Tumor invades bladder neck and/or external sphincter and/or rectum
T4b Tumor invades levator muscles and/or is fixed to pelvic wall
of radiation in the curative management of pros- to correlate biopsy results at intervals following
tate cancer. RT with clinical outcome.
Positive biopsy specimens are of concern because
they are associated with distant failure and death MATERIAL AND METHODS
from prostate cancer. 8-13However, the difficulty in In July 1990, a policy of obtaining routine post-
interpretation of post-RT biopsy results is often un- RT-TRUS-guided prostate biopsy specimens was
derstated. Histologic clearance of tumor following introduced at the General Division of the Ottawa
RT may take 18 months or longer.gv14-16Even when Regional Cancer Centre for all prostate cancer pa-
biopsies are performed at an appropriate interval tients treated by pelvic RT with curative intent.
following treatment, major pitfalls exist. Biopsies were scheduled 12 months following RT,
Radiation atypia in benign prostate glands may then every 6 months until negative or until the
be confused with residual or recurrent tumor, development of clinical recurrence. Patients with
leading to overcall of positive biopsy resu1ts.l’ initial negative biopsy results at 12 months had
Immunohistochemical stains for high molecular another biopsy at 36 months. We report the re-
weight keratin can differentiate radiation atypia sults on 226 patients aged 49 to 87 years (median,
from residual tumor, since the basal cell layer of 70), treated from July 1987 to February 1993, all
benign glands stains positive, whereas malignant with histologically confirmed adenocarcinoma of
glands are negative. l8 Most series, however, do the prostate. Data were updated in March 1994
not document staining for high molecular weight and analyzed with the Kwikstat 3.3 statistical data
keratin. analysis program (TexaSoft).
Tumor resolution after RT may leave scattered All patients had a complete history and physi-
nests of cells showing marked radiation change. cal examination at the time of initial consulta-
Since there is no identifiable glandular morphol- tion. Local tumor stage was determined by digi-
ogy, these remnants would be given a high Glea- tal rectal examination (DRE), performed by both
son score. Recently developed immunohisto- the radiation oncologist and the referring urolo-
chemical stains can differentiate between rapidly gist. If hormonal intervention had been initiated
proliferating poorly differentiated residual tumor before referral, the tumor stage assigned was as
and degenerated nonproliferating cells. Prolifera- described by the referring urologist. Investiga-
tive cell nuclear antigen (PCNA) is a nonhistone tions included complete hlood count, renal and
nuclear protein elaborated on the nuclear mem- hepatic function tests, serum alkaline and acid
brane of actively cycling cells, but absent in those phosphatases, PSA (since November 1989, Abbot
cells that are not proliferating. Levels correlate IMX assay: normal range to 5.3 ng/mL), chest ra-
well with other indices of proliferative activity, diograph, technetium-99m bone scan, and pelvic
such as in vivo 5bromodeoxyuridine (BuDR) computed tomography (CT) scan. Thirty-three
staininglg and tumor grade.20 patients (14.6%) had a staging pelvic lymphade-
In this prospective study, routine transrectal ul- nectomy. Staging is according to International
trasound (TRUS)-guided biopsies were done sys- Union Against Cancer-TNM classification of
tematically on 226 unselected patients to deter- 199221 (Table I). Distribution by stage and grade
mine the time course of histologic resolution and is shown in Table II.
UROLOGY@ I APRIL 1995 I VOLUME 45, NUMBER 4 625
All biopsy results were reviewed by one pathol-
TABLE II. Distribution of patients by
ogist (S.R.) and stained for PSA and prostatic acid
stage and grade
phosphatase. Immunohistochemical stain for high
Grade molecular weight keratin (keratin 903) was used
Stage WD MD PD GX to distinguish residual carcinoma from radiation
Tl ti- 14 13 5 0 atypia in benign glands. Biopsies were considered
Tic 8 3 0 0 positive if hematoxylin and eosin staining showed
T2a 30 11 1 3 any evidence of residual malignancy, regardless of
T2b 33 40 4 5
the scarcity of malignant cells or the degree of ra-
T3 14 30 4 2
diation effect. Positive biopsies were then subdi-
T4 2 - 1 2 1
vided into “clearly positive” and “indeterminate”
Total 101 98 16 11
categories, based on the degree of radiation-
KEY: WD = well dif~ereerentiated (Gleason scow 2-4); MD = moderately induced degenerative change.
d$Jereerentiated (Gleason scox 5-7); PD = poorly differentiated (Gleason SCDIC
8-10); GX = unknown grade. Positive or indeterminate biopsies were also
processed with an immunohistochemical stain for
PCNA, using the NovoCastra PC10 antibody. Fix-
Forty-two percent of patients (94 of 226) had ation time in formalin was limited to 12 hours.
hormonal intervention (median duration, 5 PCNA staining was expressed as the percentage of
months; range, 1 to 60 months) before referral for tumor cells staining positive.
definitive RT. Hormonal treatment was discontin- Patient status was considered as no evidence of
ued before RT and not reinstituted except for doc- disease (NED) if both serum PSA and DRE were
umented failure. Patients with orchiectomy were normal and the biopsy results were negative. Pos-
excluded. Patients who failed distantly in the first itive and indeterminate biopsy results were classi-
year of follow-up also had a biopsy if they were fied as biopsy failures if both DRE and serum PSA
close to the 12-month mark. values were normal. If either PSA or DRE was ab-
All patients were treated with 18 MV photons normal, together with a positive or indeterminate
using a four-field box technique. The treatment biopsy result, the patient was classified as having
volume was limited to the prostate and seminal a local failure. An elevated PSA level, with no ev-
vesicles for small well-differentiated tumors and idence of tumor on either DRE or a biopsy spec-
those that were pathologically node negative. Most imen was deemed a chemical failure. Patients with
patients were treated to the first echelon (external distant metastases were classified as distant fail-
and internal iliac) nodes with fields extending su- ures only if the prostate biopsy result was normal;
periorly to the bottom of the sacroiliac joints. otherwise they were considered to have combined
Treatment to the whole pelvis was rarely used. local and distant failure, even if the DRE was clin-
Standard fractionation of 1.8 to 2.0 Gy/day was ically normal.
used. Lymph nodes received 45 to 46 Gy, the pros-
tate and seminal vesicles received 65 to 66 Gy R&ULTS
(range, 60 to 68 Gy). Three hundred seventy-five biopsies were per-
The mean follow-up is 33 months (range, 12 to formed on 226 patients: 117 patients had one
78 months). Patients were seen every 3 to 4 months biopsy, 76 patients had two biopsies, 26 patients
for the first 2 years, every 6 months until 5 years, had three biopsies, and seven patients had four
and yearly thereafter, with a PSA determination at biopsies. Status of the 226 patients as of March
each visit. The first post-treatment biopsy was 1994 is shown in Table III. Of the 226 patients,
scheduled 12 months after RT. Prostates with resid- 51% (115 of 226) had an abnormal initial biopsy
ual tumor had a biopsy every 6 months until nega- result at a median time of 13 months after RT. Sev-
tive or until clinical evidence of failure (rising PSA enty of the 115 (61%) showed malignant cells with
values or abnormal DRE). Repeat biopsies were also apparently minimal treatment effect. Of these, 24%
performed to investigate a rising PSA or abnormal (17 of 70) progressed to local failure at a median
DRE. All biopsies were performed under TRUS guid- of 30 months, and 33% (23 of 70) converted to
ance with antibiotic prophylaxis (ciprofloxacin, negative at a median of 26 months. Of 115 pa-
500 mg every 12 hours for three doses). All quad- tients, 45 (39%) were considered indeterminate
rants of the prostate were sampled, as well as the because of marked degenerative changes. Of these,
site of the original tumor, which was targeted for an only 9% (4 of 45) progressed to local failure and
additional two or three passes. In total four to seven 29% (13 of 45) converted to negative. Delayed
samples were taken per biopsy session. conversion to negative occurred in all T stages
626 LJ ROLOCY@ /APRIL 1995 i VOLUME 45, NUMBER 4
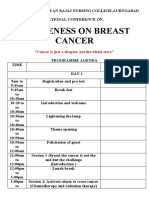
*Vander Wed Messing=
FIGURE 1. Percent positive
$-Herr rs biopsy versus time from comple-
*Crook (present series) tion of radiation therapy [RT).
14 [Modified from Crook et aLz2)
* cox
10
* Schellhammer
~0 3 6 9 12 15 18 21 24 27 30 33 i-5
Months post RT
TABLE III. Status of patients as of March 1994 according to stage
Stage NED BF CF LF* LF + DF DF+ Total
Tlb 21 5 1 2 2 1 32
Tic 6 5 0 0 0 0 11
T2a 28 9 1 4 1 2 45
T2b 46 15 3 10 2 6 82
T3 21 10 2 6 3 8 50
T4 0 3 0 0 2 1 6
Total 122 47 7 22 10 18 226
% 54.0 20.8 3.1 9.7 4.4 8 100
KEY: NED = no evidence of disease; BF = biopsy failure; CF = chemicaljaihue; LF = isolated local failure; DF = isolated
distant failure; L.F + DF = simultaneous local and distant failures.
“Total local failures were 32 (14%).
‘Total distant failures were28 (12.5%).
(Tlb: 6, Tic: 1, T2a: 12, T2b: 14, T3: 6). The pro- 100
portion of normal and abnormal biopsies as a func-
tion of time is shown in Figure 1. By 30 months, 90
69.5% of patients had achieved a negative biopsy. a0
Eleven (7%) of the 150 patients with negative post-
treatment biopsy results progressed to local failure 70
at a median time of 36 months. 60
Overall, 14% of patients (32 of 226) had a local
50
failure. The local failure rate by stage is 12.5% %
Tlb, 0% Tic, 11% T2a, 15% TZb, 18% T3, and 40
33% T4. Of local failures, 28% (9 of 32) were 30
based on a positive biopsy and elevated PSA level
with a normal DRE, and were thus “preclinical.” 20
Actuarial local control is shown in Figure 2. 10
Twenty-one percent of patients (47 of 226) re-
main in the biopsy failure category, with a normal 0 I I I I I I I I
0 6 12 18 24 30 36 42 48
PSA and DRE. This has occurred in 16% of Tlb
(5 of 32), 45% of Tic (5 of ll), 20% of T2a (9 of Months
45), 17% of T2b (14 of 82), 20% of T3 (10 of 50), FIGURE 2. Actuarial local control by stage.
UROLOGY@ /APRIL 1995 I VOLUME 45, NUMBER 4
27.3 months, whereas those who progressed had
a nadir of 4.7 ng/mL at 14.9 months.
Staining for PCNA was attempted in all biopsies
suspicious for residual tumor. For the 39 patients
showing late conversion to negative, 27 (69%) of
the initial post-treatment biopsy specimens were
stained for PCNA and 18 of these (67%) were ini-
tially negative, indicating a loss of proliferative
capability. The 9 patients who had initially PCNA-
positive residual tumor showed decreasing PCNA
counts with subsequent biopsies (Fig. 3). All lo-
cal failures that could be stained for PCNA (26 of
32) were PCNA positive, with a mean count of
13.7 cells per 100 tumor cells, confirming their
biologic activity.
Forty-two percent of patients (94 of 226) had
hormonal treatment before RT. The effect on
local outcome was examined as a function of du-
12 18 24 ration of hormones. Negative biopsy rates at 18
TimepostRT (month) months are 53% (56 of 106) for those who did
FIGURE 3. Proliferative cell nuclear antigen (PCNA) not receive prior hormones and 74% for those
counts (number of PCNApositive nuclei per 100 tumor treated for more than 4 months (P = 0.047). Pa-
nuclei) in three consecutive biopsies for 2 individual tients with stage T2b or T3 disease showed no in-
patients. (Modified from Crook et a1.24) fluence of prior hormone therapy in the rate of
local failure.
and 50% of T4 (3 of 6). This includes both posi- COMMENT
tive and indeterminate biopsy results, regardless Prostate cancer is a disease with a long natural
of PCNA status or apparent tumor viability. The history. Overall survival is not an appropriate mea-
median follow-up on these patients is only 19.5 sure of treatment efficacy in an aging population
months, and the median PSA level is 1.0 ng/mL. with multiple competing causes of mortality.25
Only 30% (14 of 47) of the biopsy failure group Even disease-specific survival can be misleading,
has a PSA level of 1.5 ng/mL or greater. given the high risk of subclinical microscopic dis-
We classified the positive biopsies (clearly posi- semination at the time of diagnosis. Efficacy of lo-
tive versus indeterminate) based on the degree of cal therapy must be judged by local tumor eradi-
radiation effect, in order to predict eventual con- cation. Therefore, prostate biopsy should be the
version to negative. Forty-five patients had an ini- ultimate measure of treatment success. Unfortu-
tial indeterminate biopsy. Of these, 14 have had nately, the prolonged time to histologic tumor
only one biopsy, and 10 have continued to be clas- clearance and the microscopic changes caused by
sified as indeterminate after subsequent biopsies, irradiation of nonmalignant glands can make in-
for a total of 53% (24 of 45) who require further fol- terpretation of biopsy results difficult. Other series
low-up to determine outcome. Sixteen (36%) have that may not have taken these factors into account
resolved to negative at a mean time of 24 months have reported very high rates of residual tumor
after RT, and 5 (11%) have progressed to a clearly following RT.5-7 We have tried to eliminate selec-
positive biopsy result at a mean of 20 months tion bias by performing biopsies on all patients.
(4 with local failure). Thirty-two patients (14%) have had local fail-
The mean PSA nadir for the study population ures, 10 with concurrent distant metastases.
was 2.0 ng/mL at a mean time of 19.3 months. Twenty-eight percent of these local failures were
Nadir PSA was higher in patients with local fail- detected by the combination of a positive biopsy
ure (mean, 3.9 ng/mL) than those without failure and a rising PSA level without abnormality on
(mean, 0.7 ng/mL) (P <O.OOl). Time to nadir PSA DRE. Thus, although our follow-up is relatively
was 14.4 months in patients with local failure short, our criteria for local failure are strict, and
compared with 23.1 months in patients without failures are diagnosed earlier than they would be
failure (P = 0.012). Patients with abnormal biopsy clinically. Surgical series reporting results for rad-
result that resolved had a nadir of 1.3 ng/mL at ical prostatectomy show that biochemical failure
628 UROLOGY@ / APRK 1995 I VOWME 45, NUMBER 4
at 3 years is equivalent to clinical failure at 10 though some will undoubtedly fail, many of these
years26,27 and the same may be true for RT. biopsies may eventually convert to negative. The
The 7% false-negative rate (defined as patients median follow-up of this group is only 19.5 months,
with a negative post-treatment biopsy that later which is short compared with the time course for
converts to positive) is comparable to other se- tumor resolution, and the mean nadir PSA level is
ries9 and is likely due to sampling error. We have 1.0 ng/mL, which indicates an overall favorable
tried to minimize sampling error by using TRUS prognosis. However, 14 of the 47 patients (30%)
guidance, taking multiple samples, and preferen- presently have a serum PSA over 1.5 ng/mL and
tially targeting the original tumor site. this subgroup is at higher risk for eventual failure.
Biopsy failures, by definition, have no support- PCNA was found to correlate with tumor via-
ing evidence for biologically active disease. bility after radiotherapy The absence of PCNA in
Whether the biopsy shows apparently viable tu- residual tumor is predictive of eventual resolu-
mor or degenerated cells showing marked radia- tion, since no patient with negative PCNA had lo-
tion change, continued resolution over time may cal progression. Unfortunately, the converse is not
occur. So far, only 18% of patients (21 of 115) true, since PCNA positivity may decrease with
with an initially positive post-treatment biopsy time. RT causes postmitotic cell death, allowing
have developed local failure, whereas 34% (39 of fatally damaged prostate carcinoma cells to un-
115) have demonstrated delayed conversion to dergo a limited number of cell divisions.30,31 Since
negative at a mean of 26 months (range, 17 to 65 tumor doubling times are many months, residual
months). This rate of late tumor clearance agrees proliferative activity may be seen up to 24 months
well with Scardino’s16 rate of 32% of positive 12- after RT. All local failures showed high PCNA
month biopsy results becoming negative by 24 counts (mean, 13.7 per 100 tumor cells), indica-
months. For patients not achieving complete tu- tive of retained proliferative potential. Other
mor clearance, one can expect a continued toll of markers of cell proliferative capacity are available
local failures. Schellhammer et al.1° have reported (Ki-67, MoAb, AgNor)31-33 and are currently be-
local failures developing in 25% of patients with ing investigated.
a positive post-treatment biopsy by 3 years, 50% The correct interpretation of post-RT prostate
by 5 years, and 65% by 8 years. biopsies requires a certain expertise. Pathologists
Histologic resolution correlates well with PSA should be encouraged to grade the therapy ef-
nadir. Patients with local failure had a higher PSA fect 34*35as this can be helpful in interpretation of
nadir, 3.9 ng/mL, and reached the nadir earlier (14 the ‘report. Gleason grading should be avoided,
months) than patients without failure (0.7 ng/mL since it was designed for untreated prostate can-
at 23 months). These values are similar to those re- cer and may not be applicable to irradiated can-
ported by Ritter et al. 28.. 2.9 ng/mL for patients with cers where tumor gland morphology can be
isolated local failure and 0.9 ng/mL for patients markedly altered. As with androgen deprivation
with no failure (Proschek assay: normal upper limit therapy, invasive cell clusters or single cells can
of 3.2 ng/mL). Our patients with delayed tumor mimic a high Gleason grade.36 Gleason grading
clearance reached a nadir PSA level of 1.3 ng/mL at may, however, be appropriate in biopsies showing
27 months, an interval almost identical to the mean no apparent therapy effect. Staining for high mo-
time for biopsy conversion. lecular weight keratin is essential to avoid mis-
It remains unclear what constitutes a normal taking radiation atypia in benign glands for resid-
PSA after RT. Since the prostate has not been re- ual tumor. Such overcall may have contributed to
moved, one cannot expect the serum PSA level to uncertainty about the clinical relevance of posi-
become undetectable or to fall below 0.6 ng/mL.2T29 tive biopsies,18 since patients with radiation atypia
Most authors continue to define chemical failure alone are unlikely to develop distant metastases
as a PSA level above the upper limits of normal for or die of prostate cancer.
their laboratory Levels associated with long-term There is no doubt that true residual tumor of
disease-free survival are 1.1 to 1.2 ng/mL,13,28,29 al- proven biologic activity (abnormal DRE or rising
though Stamey et al.ll reported stable values as PSA levels) will eventually progress and dissemi-
high as 2.9 ng/mL in radiation-treated patients. In nate. Prestidge et a1.37 report that the most im-
our series, the current median PSA in the patients portant predictive factor for the outcome of a pos-
with NED is 0.7 ng/mL. itive post-radiation prostate biopsy is the DRE. In
Forty-seven of our 226 patients (21%) are their series, 52% of patients with an abnormal
presently classified as biopsy failures. These pa- DRE developed distant metastases compared with
tients have no clinical or PSA abnormalities. Al- 26% of patients with no palpable abnormality. At
U ROLOCYO / APIUL 1995 I VOLUME 45, NUMBER 4 629
a median follow-up of 13.8 years, 50 of 116 pa- icity. Finally, cytoreduction prior to radiotherapy
tients (43%) are alive with no evidence of disease may reduce the number of clonogenic cells and
other than a positive prostate biopsy result. PSA improve the dose/response relationship.
levels for these patients were not reported.
Contrary to the experience of other authors,12 CONCLUSION
rapidly rising PSA values in our population of ir- Prostate biopsies following radical radiotherapy
radiated patients were seen only in those with dis- may take 2 l/2 to 3 years to resolve. Staining for
seminated disease. Local failures had a mean PSA proliferative cell nuclear antigen can help differ-
doubling time of 8.1 months compared with 3.4 entiate viable from nonviable tumor cells. Al-
months for patients with distant failure. Zagars though longer follow-up is required, it appears
amd Pollack38 reported mean doubling times of 6 that an abnormal prostate biopsy without other
months for metastatic disease and 10.8 months evidence of disease is insufficient to make the di-
for locoregional failure. Although PSA doubling agnosis of local failure.
times appear to be related more to grade than to
site of failure,25 higher grade tumors have a higher J. M. Crook, M.D.
metastatic potential. This may account for the Department of Radiation Oncology
consistently shorter doubling times for patients Ottawa Regional Cancer Centre
with metastases rather than isolated local failure. Ottawa, Canada
Cox et ~1.~~ have proposed an alternative theory
ACKNOWLEDGMENT. To Carolle Brazeau for secretarial as-
that, since the more rapidly dividing cells are more sistance, and to Dr. V. Zaleski for his expertise in ultra-
radiosensitive, radiation may select more slowly sonography and the Ottawa Regional urologists for referral
proliferating clones, accounting for the slower of patients, especially Dr. N. Futter, Dr. D. McKay, Dr. W.
rise in PSA levels with local failure. Walsh (Ottawa General Hospital), Dr. G. Chenard (Riverside
There was a higher rate of negative biopsies at 18 Hospital), Dr. N. Saliba and Dr. S. Faddoul (Centre hospi-
talier de Gatineau), Dr. G. Bourdeau and Dr. C. Lajeunesse
months in patients who received more than 4 (Montfort Hospital).
months of prior hormonal therapy (75%) compared
with no hormonal treatment (53%) (P = 0.047). REFERENCES
However, there was no corresponding difference in 1. Hanks GE: External beam radiation treatment for pros-
local failure rates. This should not be interpreted as tate cancer: still the gold standard. Oncology 6: 79-86, 1992.
a failure of cytoreductive therapy Patients receiving 2. Perez CA, Hanks GE, Leibel SA, Zietman AL, Fuks Z,
hormones before RT were selected for many reasons and Lee WR: Localized carcinoma of the prostate (Stages
and referred for RT at times often unrelated to op- Tlb, Tic, T2, and T3). Review of management with external
beam radiation therapy. Cancer 72: 31563173, 1993.
timal cytoreduction. Furthermore, the hormonal 3. Bagshaw MA, Kaplan ID, and Cox RC: Radiation ther-
therapy was not uniform. No conclusions should be apy for localized disease. Cancer 71: 939-952, 1993.
drawn when such heterogeneity exists. Prospective 4. Dugan TC, Shipley WU, Young RH, Verhey LJ, Al-
randomized trials of hormonal cytoreduction are thausen AF, Heney NM, McManus PL, and Abraham EH:
presently under way Biopsy after external beam radiation therapy for adenocarci-
noma of the prostate: correlation with original histological
We do not recommend routine post-treatment grade and current prostate specific antigen levels. J Urol 146:
biopsies in the follow-up of prostate cancer after 1313-1316, 1991.
RT. However, TRUS-guided biopsies may be use- 5. Kabalin JN, Hodge KK, McNeal JE, Freiha FS, and
ful if further local treatment is considered for lo- Stamey TA: Identification of residual cancer in the prostate
cal failure. A positive biopsy result after 30 following radiation therapy: role of transrectal ultrasound
guided biopsy and prostate specific antigen. J Urol 142:
months, especially one showing PCNA positivity, 326-331, 1989.
likely represents true local treatment failure. Al- 6. Scardino PT, and Wheeler TM: Prostatic biopsy after
though our follow-up is short, we recommend irradiation therapy for prostatic cancer. Urology 25: 39-46,
that treatment decisions should not be based on a 1985.
positive biopsy result alone, in the absence of ei- 7. Nachtsheim DA Jr, McAninch JW, Stutzman RE, and
Goebel JL: Latent residual tumor following external radiother-
ther a palpable abnormality or a rising PSA level. apy for prostate adenocarcinoma. J Urol 120: 312-314, 1978.
Currently, efforts are under way to reduce the 8. Fuks Z, Leibel SA, Wallner KE, Begg CB, Fair WR,
failure rate. Fiducial markers inserted under ultra- Anderson LL, Hilaris BS, and Whitmore WF: The effect of lo-
sound guidance can be used to track prostate mo- cal control on metastatic dissemination in carcinoma of the
tion during RT and ensure optimal centering of prostate: long-term results in patients treated with lz51 im-
plantation. Int J Radiat Oncol Biol Phys 21: 537-547, 1991.
the radiation beam throughout therapy, reducing 9. Kuban DA, and El-Mahdi AM: Local control after ra-
the risk of geographic miss. Conformal therapy diation for prostatic carcinoma: significance and assessment.
may allow dose escalation without increasing tox- Semin Radiat Oncol 3: 221-229, 1993.
630 U ROLOCY@ /APRIL 1995 I VOLUME 45, NUMBER 4
10. Schellhammer PF, el-Mahdi AM, Higgins EM, 28. Ritter MA, Messing EM, Shanahan TG, Potts S, Chap-
Schultheiss TE, Ladaga LE, and Babb TJ: Prostate biopsy af- pell RJ, and Kinsella TJ: Prostate-specific antigen as a pre-
ter definitive treatment by interstitial ‘25iodine implant or dictor of radiotherapy response and patterns of failure in lo-
external beam radiation therapy. J Urol 137: 897-901, 1987. calized prostate cancer. J Clin Oncol 10: 1208-1217, 1992.
11. Stamey TA, Kabalin JN, and Ferrari M: Prostate spe- 29. Russell KJ, and Boileau MA: Current status of pros-
cific antigen in the diagnosis and treatment of adenocarci- tate-specific antigen in the radiotherapeutic management of
noma of the prostate. III. Radiation treated patients. J Urol prostatic cancer. Semin Radiat Oncol 3: 154-168, 1993.
141: 1084-1087, 1989. 30. Mostofi FK, Sesterhenn IA, and Davis CJ Jr: A pathol-
12. Stamey TA, Ferrari MK, and Schmid HP: The value of ogist’s view of prostatic carcinoma. Cancer 71 (suppl):
serial prostate specific antigen determinations 5 years after 906-932,1993.
radiotherapy: steeply increasing values characterize 80% of 31. Mostofi FK, Davis CJ Jr, and Sesterhenn IA: Pathology
patients. J Urol 150: 1856-1859, 1993. of carcinoma of the prostate. Cancer 70 (suppl): 235-253,
13. Zagars GK, vonEschenbach AC, Ayala AG, Schultheiss 1992.
TE, and Sherman NE: The influence of local control on meta- 32. Harper ME, Glynne-Jones E, Goddard L, Wilson DW,
static dissemination of prostate cancer treated by external beam Matenhelia SS, Conn IG, Peeling WB, and Griffiths K: Rela-
megavoltage radiation therapy. Cancer 68: 2370-2377, 1991. tionship of proliferating cell nuclear antigen (PCNA) in pros-
14. Cox JD, and Kline RW: The lack of prognostic signif- tatic carcinomas to various clinical parameters. Prostate 20:
icance of biopsies after radiotherapy for prostatic cancer. 243-253,1992.
Semin Urol 1: 237-242, 1983. 33. Sakr WA, Sarkar FH, Sreepathi P, Drozdowicz S, and
15. Herr HW, and Whitmore WF Jr: Significance of pros- Crissman JD: Measurement of cellular proliferation in hu-
tatic biopsies after radiation therapy for carcinoma of the man prostate by AgNOR, PCNA, and SPF. Prostate 22:
prostate. Prostate 3: 339-350, 1982. 147-154, 1993.
16. Scardino PT: The prognostic significance of biopsies 34. Dhom G, and Degro S: Therapy of prostatic cancer
after radiotherapy for prostatic cancer. Semin Urol 1: and histopathologic follow-up. Prostate 3: 531-542, 1982.
243-252,1983. 35. B&king A, and Auffermann W: Cytological grading of
17. Bostwick DG, Egbert BM, and Fajardo LF: Radiation therapy-induced tumor regression in prostatic carcinoma:
injury of the normal and neoplastic prostate. Am J Surg proposal of a new system. Diagn Cytopathol 3: 108-111,
Path01 6: 541-551, 1982. 1987.
18. Brawer MK, Nagle RB, Pitts W, Freiha F, and Gamble 36. Armas OA, Aprikian AG, Melamed J, Cordon-Card0
SL: Keratin immunoreactivity as an aid to the diagnosis of C, Cohen DW, Erlandson R, Fair WR, and Reuter VE: Clin-
persistent adenocarcinoma in irradiated human prostates. ical and pathobiological effects of neoadjuvant total andro-
Cancer 63: 454-460, 1989. gen ablation therapy on clinically localized prostatic adeno-
19. Carroll PR, Waldman FM, Rosenau W, Cohen MB, carcinoma. Am J Surg Path01 18: 979-991, 1994.
Vapnek JM, Fong P, Narayan P, and Maya11 BH: Cell prolif- 37. Prestidge BR, Kaplan I, Cox RS, and Bagshaw MA:
eration in prostatic adenocarcinoma: in vitro measurement Predictors of survival after a positive post-irradiation pros-
by S-bromodeoxyuridine incorporation and proliferating cell tate biopsy. Int J Radiat Oncol Biol Phys 28: 17-22, 1994.
nuclear antigen expression. J Urol 149: 403-407, 1993. 38. Zagars GK, and Pollack A: The fall and rise of pros-
20. Nemoto R, Kawamura H, Miyakawa I, Uchida K, Hat- tate-specific antigen. Kinetics of serum prostate-specific anti-
tori K, Koiso K, and Harada M: Immunohistochemical de- gen levels after radiation therapy for prostate cancer. Cancer
tection of proliferating cell nuclear antigen (PCNA)/cyclin in 72: 832-842,1993.
human prostate adenocarcinoma. J Urol149: 165-169,1993. 39. Cox RS, Kaplan ID, and Bagshaw MA: Prostate-spe-
21. Hermanek P, and Sobin LH (Eds): International Union cific antigen kinetics after external beam irradiation for car-
Against Cancer. TNM Classification ofMalignant Turnours, 4th cinoma of the prostate. Int J Radiat Oncol Biol Phys 28:
ed., 2nd rev. Berlin, Springer-Verlag, 1992. 23-31, 1994.
22. Crook J, Robertson S, Collin G, Zaleski V, and Esche
B: Clinical relevance of trans-rectal ultrasound, biopsy, and
serum prostate-specific antigen following external beam ra- EDITORIAL COMMENT
diotherapy for carcinoma of the prostate. Int J Radiat Oncol This study reports the results of a remarkable 6-year effort
Biol Phys 27: 31-37, 1993. by the authors to define the time course of histologic resolu-
23. van der Werf-Messing B: Prostatic cancer treated at tion of prostate cancer after radiotherapy. Of great importance
Rotterdam Radiotherapy Institute. Strahlentherapie 154: is that it was conducted prospectively in consecutive patients.
537-541, 1978. Seventy percent of 226 patients achieved negative biopsy
24. Crook J, Robertson S, and Esche B: Proliferative cell status by 30 months follow-up and the conversion from early
nuclear antigen in post-radiotherapy prostate biopsies. Int J positivity to later negative biopsies was clearly shown. Im-
Radiat Oncol Biol Phys 30: 303-308, 1994. portantly, prostate-specific antigen (PSA) response predicted
25. Hanks GE: Treatment of early stage prostate cancer: biopsy outcome but conversion to late negative status was
radiotherapy, in Devita VT, Hellman S, and Rosenberg JB frequently accompanied by a later PSA response in those pa-
(Eds): Important Advances in Oncology, 1994. Philadelphia, tients. Rapidly rising PSAs after radiation failure were ob-
Lippincott, 1994. served only in a small group of patients with documented
26. Fair WR, Aprikian AG, Cohen D, Sogani P, and Reuter metastatic disease.
V: Use of neoadjuvant androgen deprivation therapy in clin- These data have established the new standard that extends
ically localized prostate cancer. Clin Invest Med 16: 516-522, and more accurately defines previous reports concerning the
1993. accuracy of postirradiation biopsies by Cox et al.’ and
27. Paulson DF, Moul JW, and Walther PJ: Radical pros- Scardino et nl.* They also show, along with other recent ar-
tatectomy for clinical stage Tl-ZNOMO prostatic adenocarci- ticles,3-5 that the previous statement by Kabalin et al.,‘j “Resid-
noma: long-term results. J Urol 144: 1180-1184, 1990. ual prostate cancer was proven by biopsy in 25 of 27 patients
U ROLOCY@ / APRIL 1995 / VOLUME 45, NUMBER 4 631
(93%) 18 months to 12 years after completion of radiation 2. Scardino PT: The prognostic significance of biopsies af-
therapy” and Stamey et al7 “...approximately 20% of the pa- ter radiotherapy for prostatic cancer. Semin Urol 1: 243-251,
tients...can be cured by irradiation therapy. The remaining 1985.
80% of the patients in whom radiotherapy fails appear to have 3. Hancock SL, Cox RS, and Bagshaw MA: Biochemical
an accelerated growth rate...” were observations made in highly control of prostate cancer and kinetics of prostate specific
selected patient groups that do not represent the results ob- antigen in recurrences in a cohort of patients treated by ex-
tained in unselected radiotherapy patients. Unfortunately, ternal beam irradiation. Int J Radiat Oncol Biol Phys 30: 217,
their comments have been interpreted by many physicians as 1994.
representing the results of radiation therapy as a whole. 4. Hanks GE, Lee WR, Corn B, and Schultheiss TE: Re-
Dr. Crook and her colleagues have reminded us that there sponse to “only 20% of irradiated prostate cancer patients are
is a role for institution-based clinical research where care- cured and the remainder may be made worse”. Int J Radiat
fully planned and conducted clinical studies in large groups Oncol Biol Phys 30: 217, 1994.
of consecutive patients can provide valuable information that 5. Zietman AL, Shipley WU, Coen JJ, Shipley JW, and Al-
can help to guide us in patient management. thausen AF: Long-term outcome for men with prostate can-
cer treated with radiation as sole therapy. Int J Radiat Oncol
Gerald E. Hanks, M.D. Biol Phys 30: 218, 1994.
Fox Chase Cancer Center 6. Kabalin JN, Hodge KK, McNeal JE, Freiha FS, and
Stamey TA: Identification of residual cancer in the prostate
7701 Burholme Avenue
following radiation therapy: role of transrectal ultrasound
Philadelphia, PA I91 I I guided biopsy and prostate specific antigen. J Urol 142:
326-331, 1989.
REFERENCES 7. Stamey TA, Ferrari MK, and Schmid H: The value of se-
1. Cox JD, and Stoffel TJ: The significance of needle rial prostate specific antigen determinations 5 years after ra-
biopsy after irradiation for the stage C adenocarcinoma of diotherapy: steeply increasing values characterize 80% of pa-
the prostate. Cancer 40: 156-160, 1977. tients. J Urol 150: 1856-1859, 1993.
632 UROLOGY@ /APRIL 1995 I VOLUME 45, NUMBER 4
You might also like
- ESMO Essentials Clinicians Genitourinary Tract Tumours 2020Document131 pagesESMO Essentials Clinicians Genitourinary Tract Tumours 2020Stir100% (3)
- Raphex 2011 PDFDocument29 pagesRaphex 2011 PDFcarlosqueiroz766975% (4)
- RT Urothelial Carcinomas Radu MitricaDocument37 pagesRT Urothelial Carcinomas Radu MitricaStirNo ratings yet
- Down-Staging of Early Stage Prostate Can PDFDocument9 pagesDown-Staging of Early Stage Prostate Can PDFNelma TuiranNo ratings yet
- 11 Preoperative - High - Neutrophil-Lymphocyte - Ratio - MayDocument8 pages11 Preoperative - High - Neutrophil-Lymphocyte - Ratio - MayBridia BogarNo ratings yet
- BladderDocument36 pagesBladderdrsumitavaNo ratings yet
- Tanum1991 (Biopsia A Todos)Document5 pagesTanum1991 (Biopsia A Todos)ouf81No ratings yet
- Correlation With Biochemical FailureDocument11 pagesCorrelation With Biochemical FailureStirNo ratings yet
- Lee2004 - 52.5 - 20sesDocument6 pagesLee2004 - 52.5 - 20sesMigue PerezNo ratings yet
- Sunaryo Hardjowijoto Wahjoe Djatisoesanto: Division Oncology Department of Urology Airlangga School of MedicineDocument33 pagesSunaryo Hardjowijoto Wahjoe Djatisoesanto: Division Oncology Department of Urology Airlangga School of MedicineAdith FileanugrahaNo ratings yet
- Radiotherapy of Oligometastatic Prostate Cancer Experience of The Mohamed VI Center For Cancer Treatment in Casablanca, MoroccoDocument7 pagesRadiotherapy of Oligometastatic Prostate Cancer Experience of The Mohamed VI Center For Cancer Treatment in Casablanca, MoroccoInternational Journal of Innovative Science and Research Technology100% (1)
- Soubra 2018Document5 pagesSoubra 2018nimaelhajjiNo ratings yet
- Yip Et Al 2015Document7 pagesYip Et Al 2015KasmiliawatyNo ratings yet
- Jurnal Radiologi 2Document21 pagesJurnal Radiologi 2Adelya Dwi AsyifaNo ratings yet
- EAU Prostate Cancer 2004Document10 pagesEAU Prostate Cancer 2004Vinko GrubišićNo ratings yet
- Jurnal AjaDocument8 pagesJurnal AjaTiara Anggun NurartoNo ratings yet
- RRP Radical ProstatectomyDocument6 pagesRRP Radical ProstatectomybojanvuckovicNo ratings yet
- Papillary Microcarcinoma of The Thyroid-Prognostic Significance of Lymph Node Metastasis and MultifocalityDocument10 pagesPapillary Microcarcinoma of The Thyroid-Prognostic Significance of Lymph Node Metastasis and MultifocalityAZ RPNo ratings yet
- Ni Hms 519602Document21 pagesNi Hms 519602Nur Rissa MaharanyNo ratings yet
- JCO 2003 Lin 631 7Document7 pagesJCO 2003 Lin 631 7Adhika Manggala DharmaNo ratings yet
- Guidelines On Prostate Cancer: (Text Update February 2012)Document22 pagesGuidelines On Prostate Cancer: (Text Update February 2012)Julian Delgado BlancoNo ratings yet
- Improved Outcome by Adding Concurrent Chemotherapy ToDocument9 pagesImproved Outcome by Adding Concurrent Chemotherapy ToRaul Matute MartinNo ratings yet
- Ahmed 2011Document10 pagesAhmed 2011skribekbenjaminNo ratings yet
- EAU Pocket Guidelines Prostate Cancer 2019Document28 pagesEAU Pocket Guidelines Prostate Cancer 2019Madyurit RamírezNo ratings yet
- TNBC PMRTDocument7 pagesTNBC PMRTMed MedNo ratings yet
- Outcomes After Stereotactic Body Radiotherapy or Radiofrequency Ablation For Hepatocellular CarcinomaDocument10 pagesOutcomes After Stereotactic Body Radiotherapy or Radiofrequency Ablation For Hepatocellular CarcinomaRaul Matute MartinNo ratings yet
- Prostate CancerDocument58 pagesProstate CancerIsaac MwangiNo ratings yet
- FoXTRoT 2022Document15 pagesFoXTRoT 2022Ramez AntakiaNo ratings yet
- EAU EANM ESTRO ESUR ISUP SIOG Pocket On Prostate Cancer 2022Document33 pagesEAU EANM ESTRO ESUR ISUP SIOG Pocket On Prostate Cancer 2022Caio Vinicius SuartzNo ratings yet
- P. Wang Et Al.2019Document6 pagesP. Wang Et Al.2019Mai M. AlshalNo ratings yet
- Cas Clinique Colon DIU 2023 - M KAROUIDocument22 pagesCas Clinique Colon DIU 2023 - M KAROUIabirNo ratings yet
- Prostate+Ca Updated+Aug+2017 PDFDocument17 pagesProstate+Ca Updated+Aug+2017 PDFFlorencia GuerraNo ratings yet
- Cesium 131 Prostate BrachytherapyDocument7 pagesCesium 131 Prostate BrachytherapyPablo Del PozoNo ratings yet
- Fact de Pet n2Document6 pagesFact de Pet n2Pedro ChantaNo ratings yet
- Role of Radiotherapy For Hepatocellular CarcinomaDocument37 pagesRole of Radiotherapy For Hepatocellular CarcinomabahtiarhabibiNo ratings yet
- Livsey 2003Document6 pagesLivsey 2003Migue PerezNo ratings yet
- Aro 96-02auo Ap 0995Document8 pagesAro 96-02auo Ap 0995yingming zhuNo ratings yet
- Prostate CancerDocument67 pagesProstate CancerMalueth AnguiNo ratings yet
- EAU Pocket On Muscle Invasive and Metastatic Bladder Cancer 2022Document17 pagesEAU Pocket On Muscle Invasive and Metastatic Bladder Cancer 2022Caio Vinicius SuartzNo ratings yet
- EAU EANM ESTRO ESUR ISUP SIOG Pocket On Prostate Cancer 2024Document40 pagesEAU EANM ESTRO ESUR ISUP SIOG Pocket On Prostate Cancer 2024nadaelhaousNo ratings yet
- Metastatic Renal Cell Carcinoma in A Child: 11-Year Disease-Free Survival Following SurgeryDocument4 pagesMetastatic Renal Cell Carcinoma in A Child: 11-Year Disease-Free Survival Following SurgerySarly FebrianaNo ratings yet
- Dhondt Et Al 2022 90y Radioembolization Versus Drug Eluting Bead Chemoembolization For Unresectable HepatocellularDocument12 pagesDhondt Et Al 2022 90y Radioembolization Versus Drug Eluting Bead Chemoembolization For Unresectable HepatocellularNachchakorn DellNo ratings yet
- cn08015 PDFDocument5 pagescn08015 PDFadhityasdewiNo ratings yet
- Breast Cancer Clinical Case Presentation: ESMO Clinical Practice GuidelinesDocument18 pagesBreast Cancer Clinical Case Presentation: ESMO Clinical Practice GuidelinesNinaNo ratings yet
- Prognostic Model For Survival of Local Recurrent Nasopharyngeal Carcinoma With Intensity-Modulated RadiotherapyDocument7 pagesPrognostic Model For Survival of Local Recurrent Nasopharyngeal Carcinoma With Intensity-Modulated Radiotherapypp kabsemarangNo ratings yet
- Case Study: Low-Risk Organ-Confined Prostate CancerDocument4 pagesCase Study: Low-Risk Organ-Confined Prostate CancerAce VirtusioNo ratings yet
- UK Prostate Trials For 10th Uro-Onc Meeting 2013Document30 pagesUK Prostate Trials For 10th Uro-Onc Meeting 2013Prof_Nick_JamesNo ratings yet
- Carcinoma of UnknownDocument31 pagesCarcinoma of Unknownsamer falconNo ratings yet
- DTH 34 E14981Document9 pagesDTH 34 E14981Henry WijayaNo ratings yet
- C122 Early Post TURB Instillational Treatment in Ta, T1 Bladder CancersDocument1 pageC122 Early Post TURB Instillational Treatment in Ta, T1 Bladder CancersOkki Masitah Syahfitri NasutionNo ratings yet
- Protocol SummaryDocument4 pagesProtocol Summaryapi-631272802No ratings yet
- Jurnal Besar SampelDocument7 pagesJurnal Besar SampelepiloksaNo ratings yet
- Jco 2016 71 7397Document9 pagesJco 2016 71 7397brasilianaraNo ratings yet
- Corvera 2007Document9 pagesCorvera 2007Nikos SerifisNo ratings yet
- BiomedJ382173-2563889 070718 PDFDocument4 pagesBiomedJ382173-2563889 070718 PDFgrigmihNo ratings yet
- Ca MammaeDocument34 pagesCa MammaedarNo ratings yet
- Journal Reading Nasopharyngeal Carcinoma: Current Treatment Options and Future DirectionsDocument28 pagesJournal Reading Nasopharyngeal Carcinoma: Current Treatment Options and Future DirectionsyuliNo ratings yet
- The Significance of Neutrophil/lymphocyte Ratio As A Possible Marker of Underlying Papillary Microcarcinomas in Thyroidal Goiters: A Pilot StudyDocument6 pagesThe Significance of Neutrophil/lymphocyte Ratio As A Possible Marker of Underlying Papillary Microcarcinomas in Thyroidal Goiters: A Pilot StudyagusNo ratings yet
- Ou 2016Document8 pagesOu 2016tami widiatul azahraNo ratings yet
- Treatment of Diff Thyroid CancersDocument28 pagesTreatment of Diff Thyroid CancersSameer FasihNo ratings yet
- Jco 20 03282Document10 pagesJco 20 03282AKNo ratings yet
- Trimodality Therapy in Bladder CancerDocument12 pagesTrimodality Therapy in Bladder CancerStirNo ratings yet
- RT Urothelial Carcinomas Radu MitricaDocument37 pagesRT Urothelial Carcinomas Radu MitricaStirNo ratings yet
- ImageGuided Radiation Therapy of Prostate CancerDocument318 pagesImageGuided Radiation Therapy of Prostate CancerStirNo ratings yet
- Therapy Associated Effects in The Prostate Gland 2012Document13 pagesTherapy Associated Effects in The Prostate Gland 2012StirNo ratings yet
- Radiotherapy in Prostate Cancer Innovative Techniques and Current ControversiesDocument288 pagesRadiotherapy in Prostate Cancer Innovative Techniques and Current ControversiesStirNo ratings yet
- (2017) Bladder BrachyDocument7 pages(2017) Bladder BrachyStirNo ratings yet
- Impact of Pathology Review For Decision Therapy inDocument4 pagesImpact of Pathology Review For Decision Therapy inStirNo ratings yet
- D'Amico Risk ClassificationDocument6 pagesD'Amico Risk ClassificationStirNo ratings yet
- Full Prescribing Information Boxed WarningDocument62 pagesFull Prescribing Information Boxed WarningStirNo ratings yet
- Characterization of Balance Control After Moderate To Severe Traumatic Brain Injury. A Longitudinal Recovery Study - ChapterDocument10 pagesCharacterization of Balance Control After Moderate To Severe Traumatic Brain Injury. A Longitudinal Recovery Study - ChapterStirNo ratings yet
- Correlation With Biochemical FailureDocument11 pagesCorrelation With Biochemical FailureStirNo ratings yet
- Transparenta Veniturilor Salariale La 31.03.2018Document12 pagesTransparenta Veniturilor Salariale La 31.03.2018StirNo ratings yet
- Clinical 20endocrinology 20finalDocument298 pagesClinical 20endocrinology 20finalStir100% (1)
- Ce Este Astmul?: Dr. Lavinia DavidescuDocument17 pagesCe Este Astmul?: Dr. Lavinia DavidescuStirNo ratings yet
- Copd Lab 2017Document42 pagesCopd Lab 2017StirNo ratings yet
- Full Prescribing Information Boxed WarningDocument62 pagesFull Prescribing Information Boxed WarningStirNo ratings yet
- CTS Radiology Technician - CTS - NSQF-5Document38 pagesCTS Radiology Technician - CTS - NSQF-5Ashish BharayNo ratings yet
- Lean Management Paradigm Shif DR ArbainDocument84 pagesLean Management Paradigm Shif DR ArbainazlizawatiNo ratings yet
- Traumatic Lesions of The Mucous MembranesDocument14 pagesTraumatic Lesions of The Mucous MembranesManar AlsoltanNo ratings yet
- National ConferenceDocument3 pagesNational Conferencelaveena aswaleNo ratings yet
- Oxaliplatin Monograph 1dec2016Document9 pagesOxaliplatin Monograph 1dec2016Nadial UzmahNo ratings yet
- Navy Diagnostic Imaging Equipment Performance Survey ManualDocument160 pagesNavy Diagnostic Imaging Equipment Performance Survey ManualTuankiet TruongNo ratings yet
- Biological Effects of Radiation IAEADocument87 pagesBiological Effects of Radiation IAEAkhushi786100% (1)
- Mini by Me - DR SuhilDocument188 pagesMini by Me - DR SuhilA L N O F E E ,TMNo ratings yet
- 2009 Rad Onc Inservice Exam Key - TXIT - RationalesDocument106 pages2009 Rad Onc Inservice Exam Key - TXIT - RationalesTed Ling100% (2)
- ), Mikhail F. Chernov, Motohiro Hayashi, Jeremy C. Ganz, Kintomo Takakura (Eds.) - Gamma Knife Neurosurgery in The Management of Intracranial-2Document216 pages), Mikhail F. Chernov, Motohiro Hayashi, Jeremy C. Ganz, Kintomo Takakura (Eds.) - Gamma Knife Neurosurgery in The Management of Intracranial-2juca1986100% (1)
- Flexifed 1 Elect Individual Option BrochureDocument25 pagesFlexifed 1 Elect Individual Option BrochurescannertplinkNo ratings yet
- Aman MarwadiDocument2 pagesAman MarwadiNitesh kuraheNo ratings yet
- Soft Tissue SarcomaDocument19 pagesSoft Tissue SarcomaEkvanDanangNo ratings yet
- Mosaiq Ro Emr BrochureDocument6 pagesMosaiq Ro Emr BrochureAdrián CejasNo ratings yet
- NESTAandPlSci Final RS BookletDocument89 pagesNESTAandPlSci Final RS BookletsaipathNo ratings yet
- Elekta BrochureDocument7 pagesElekta BrochurePartha ChaudhuryNo ratings yet
- 2 1 6 072016 enDocument29 pages2 1 6 072016 enbaglamaNo ratings yet
- Drugs Dosage Nursing Implications: Discharge PlanDocument2 pagesDrugs Dosage Nursing Implications: Discharge PlanCristina L. JaysonNo ratings yet
- TLTKDocument9 pagesTLTKTrương Tiến HòaNo ratings yet
- Cancer LungDocument95 pagesCancer LungAnonymous ylMpcDqNo ratings yet
- Infosys MaterialsDocument182 pagesInfosys Materialsrahul khandelwalNo ratings yet
- NANOTECHNOLOGY IN MEDICINE Assignment Final DraftDocument9 pagesNANOTECHNOLOGY IN MEDICINE Assignment Final DraftMadhumita KumarNo ratings yet
- UK Prostate Trials For 10th Uro-Onc Meeting 2013Document30 pagesUK Prostate Trials For 10th Uro-Onc Meeting 2013Prof_Nick_JamesNo ratings yet
- Treatment Strategies in Childhood CancerDocument3 pagesTreatment Strategies in Childhood CancerMary BurgosNo ratings yet
- Daruka Mahadevan - Handbook of Nutrition and Diet in Leukemia and Blood Disease TherapyDocument385 pagesDaruka Mahadevan - Handbook of Nutrition and Diet in Leukemia and Blood Disease TherapyAngelicaNo ratings yet
- Principii Constructive Si Functionale Ale Instalatiilor de Radioterapie ExternaDocument42 pagesPrincipii Constructive Si Functionale Ale Instalatiilor de Radioterapie ExternaCamiDavidNo ratings yet
- Colorectal: Understanding The Cancer ProcessDocument14 pagesColorectal: Understanding The Cancer ProcessSeli adalah SayaNo ratings yet
- Stomatitis: An Overview: Protecting The Oral Cavity During Cancer TreatmentDocument4 pagesStomatitis: An Overview: Protecting The Oral Cavity During Cancer TreatmentLenna IkawatiNo ratings yet
- Moderate and Extreme HypofractionationDocument32 pagesModerate and Extreme HypofractionationsamuelfsjNo ratings yet