Professional Documents
Culture Documents
Long Term Complications and Rehabilitation of COVID-19 Patients
Long Term Complications and Rehabilitation of COVID-19 Patients
Uploaded by
mathias kosasihCopyright:
Available Formats
You might also like
- Current Procedural Terminology (CPT CODING)Document5 pagesCurrent Procedural Terminology (CPT CODING)Rabindra P.Singh50% (2)
- James Tin Yau So - Treatment of Disease With AcupunctureDocument397 pagesJames Tin Yau So - Treatment of Disease With Acupuncturearyaa202096% (26)
- PUD QuestionsDocument5 pagesPUD QuestionsAmira Paguyo QuilapioNo ratings yet
- Long COVID: Post-Acute Sequelae of COVID-19 With A Cardiovascular FocusDocument22 pagesLong COVID: Post-Acute Sequelae of COVID-19 With A Cardiovascular FocusPhitsanu SuntornpiyapanNo ratings yet
- COVID ProlongadoDocument22 pagesCOVID ProlongadoSMIBA MedicinaNo ratings yet
- Long COVID: Post-Acute Sequelae of COVID-19 With A Cardiovascular FocusDocument22 pagesLong COVID: Post-Acute Sequelae of COVID-19 With A Cardiovascular FocusWalter ReyesNo ratings yet
- Post Acute Coronavirus (COVID-19) Syndrome - StatPearls - NCBI BookshelfDocument13 pagesPost Acute Coronavirus (COVID-19) Syndrome - StatPearls - NCBI BookshelfThành Tài TrầnNo ratings yet
- Post-COVID Syndrome Incidence, Clinical SpectrumDocument7 pagesPost-COVID Syndrome Incidence, Clinical SpectrumJeane ClaudiaNo ratings yet
- Long Covid 1Document5 pagesLong Covid 1lakshminivas PingaliNo ratings yet
- A Clinic Blueprint For Post-Coronavirus Disease 2019 RECOVERY Learning From The Past, Looking To The FutureDocument11 pagesA Clinic Blueprint For Post-Coronavirus Disease 2019 RECOVERY Learning From The Past, Looking To The FutureCARLA CRISTINA DE ARAUJONo ratings yet
- 14- COVID-19 - RISKS TO THE CENTRAL NERVOUS SYSTEM AND CARDIOVASCULAR DAMAGEDocument4 pages14- COVID-19 - RISKS TO THE CENTRAL NERVOUS SYSTEM AND CARDIOVASCULAR DAMAGEDaniel lipphausNo ratings yet
- Unraveling The Mystery Surrounding Post-Acute Sequelae of COVID-19Document16 pagesUnraveling The Mystery Surrounding Post-Acute Sequelae of COVID-19Ricardo Pariona LlanosNo ratings yet
- Long COVID19 Syndrome ADocument19 pagesLong COVID19 Syndrome Arbatjun576No ratings yet
- A Review of Respiratory Post-Acute Sequelae of COVID-19 (PASC)Document5 pagesA Review of Respiratory Post-Acute Sequelae of COVID-19 (PASC)elieser toding mendilaNo ratings yet
- Aspectos Autonómicos Post CovidDocument7 pagesAspectos Autonómicos Post Covidtavo570No ratings yet
- Updates On Clinical Trials Evaluating The Regenerative Potential of Allogenic Mesenchymal Stem Cells in COVID-19Document11 pagesUpdates On Clinical Trials Evaluating The Regenerative Potential of Allogenic Mesenchymal Stem Cells in COVID-19diana.alyNo ratings yet
- Mechanisms of Long COVID An Updated ReviewDocument10 pagesMechanisms of Long COVID An Updated Reviewemmanuel AndemNo ratings yet
- Geriatric Patient With Osteoarthritis and Obesity Survived From Critically Ill of COVID-19: A Case ReportDocument5 pagesGeriatric Patient With Osteoarthritis and Obesity Survived From Critically Ill of COVID-19: A Case Reportnadila raudhani pNo ratings yet
- Long COVID or post-COVID-19 Syndrome Putative Pathophysiology, Risk FactorsDocument18 pagesLong COVID or post-COVID-19 Syndrome Putative Pathophysiology, Risk FactorsVane SchulzeNo ratings yet
- Paper 8842Document7 pagesPaper 8842IJARSCT JournalNo ratings yet
- Effects of SARS-COVID-19 Infection On The Cardiovascular SystemDocument5 pagesEffects of SARS-COVID-19 Infection On The Cardiovascular SystemSabrina JonesNo ratings yet
- Covid-19: What Do We Need To Know About Icu Delirium During The Sars-Cov-2 Pandemic?Document7 pagesCovid-19: What Do We Need To Know About Icu Delirium During The Sars-Cov-2 Pandemic?bayu bagusNo ratings yet
- Int J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaDocument12 pagesInt J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaRebeca EscutiaNo ratings yet
- Progress: Pathological Inflammation in Patients With COVID-19: A Key Role For Monocytes and MacrophagesDocument8 pagesProgress: Pathological Inflammation in Patients With COVID-19: A Key Role For Monocytes and MacrophagesagenwongNo ratings yet
- Reviews: COVID-19 and Cardiovascular Disease: From Basic Mechanisms To Clinical PerspectivesDocument16 pagesReviews: COVID-19 and Cardiovascular Disease: From Basic Mechanisms To Clinical PerspectivesLAURA ALEJANDRA PARRA GOMEZNo ratings yet
- COVID-19: Pathophysiology of Acute Disease 1: SeriesDocument21 pagesCOVID-19: Pathophysiology of Acute Disease 1: SeriesMyatnoe KhinNo ratings yet
- Diabetes Mellitus in The Context of COVID-19 La Diabetes Mellitus en El Contexto de La COVID-19Document8 pagesDiabetes Mellitus in The Context of COVID-19 La Diabetes Mellitus en El Contexto de La COVID-19Tatiana Belén García MogollónNo ratings yet
- Mesenchymal Stem Cell Immunomodulation and Regeneration TherapeuticsDocument13 pagesMesenchymal Stem Cell Immunomodulation and Regeneration TherapeuticswiwiNo ratings yet
- International Immunopharmacology: Mohammad Shah Alam, Daniel M. Czajkowsky, Md. Aminul Islam, Md. Ataur RahmanDocument12 pagesInternational Immunopharmacology: Mohammad Shah Alam, Daniel M. Czajkowsky, Md. Aminul Islam, Md. Ataur RahmanJimena Vásquez RodríguezNo ratings yet
- Severe Covid-19: Clinical PracticeDocument10 pagesSevere Covid-19: Clinical PracticejoelNo ratings yet
- Long-COVID: An Evolving Problem With An Extensive Impact: Clinical UpdateDocument3 pagesLong-COVID: An Evolving Problem With An Extensive Impact: Clinical UpdateArif wicaksonoNo ratings yet
- COVID-19 and Diabetes MellitusDocument6 pagesCOVID-19 and Diabetes MellitusUlysses GamayonNo ratings yet
- Long COVID19 Syndrome As A Fourth Phase of SARSCoV2 Infection - 2022 - EDIMES Edizioni Medico ScientificheDocument8 pagesLong COVID19 Syndrome As A Fourth Phase of SARSCoV2 Infection - 2022 - EDIMES Edizioni Medico ScientificheftasiaNo ratings yet
- Koc 2022Document14 pagesKoc 2022John GoranitisNo ratings yet
- Background To Coronavirus (COVID-19) - ICM Anaesthesia COVID-19Document2 pagesBackground To Coronavirus (COVID-19) - ICM Anaesthesia COVID-19kajelchaNo ratings yet
- Reviews: Immunity, Endothelial Injury and Complement-Induced Coagulopathy in COVID-19Document19 pagesReviews: Immunity, Endothelial Injury and Complement-Induced Coagulopathy in COVID-19Edo RezaprasgaNo ratings yet
- Patfis Covid 6Document6 pagesPatfis Covid 6mayaNo ratings yet
- Role of Homoeopathy in Management of Covid-19 Complications: ISSN 2515-8260 Volume 7, Issue 2, 2020Document8 pagesRole of Homoeopathy in Management of Covid-19 Complications: ISSN 2515-8260 Volume 7, Issue 2, 2020mubbunNo ratings yet
- MAY 2020 SINTOMAS Gastrointestinal Symptoms Associated WithDocument14 pagesMAY 2020 SINTOMAS Gastrointestinal Symptoms Associated WithMayaraNo ratings yet
- BernasDocument17 pagesBernasYezekael Sebastian QuintinusNo ratings yet
- Cells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Document29 pagesCells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Yoni LinggaNo ratings yet
- Brain SciencesDocument13 pagesBrain SciencesRuhana Sk Abd RazakNo ratings yet
- Imaging in COVID 19 Related Myocardial InjuryDocument12 pagesImaging in COVID 19 Related Myocardial Injuryorkut verificationNo ratings yet
- Diagnosis of Sars-Cov-2 Infection in The Setting of The Cytokine Release SyndromeDocument12 pagesDiagnosis of Sars-Cov-2 Infection in The Setting of The Cytokine Release SyndromeTufik NaderNo ratings yet
- Banerjee 2021Document15 pagesBanerjee 2021georgeNo ratings yet
- EXPODocument18 pagesEXPOEstefy Cerda MoscosoNo ratings yet
- Pi Is 0003999321003269Document12 pagesPi Is 0003999321003269Amanda SchaefferNo ratings yet
- Astma Impact IncovidDocument9 pagesAstma Impact IncovidRosintchi MirsalNo ratings yet
- Neurobiologia Del COVID19Document25 pagesNeurobiologia Del COVID19paola coralNo ratings yet
- Jurnal DipsneaDocument7 pagesJurnal DipsneaAgnes AriscaNo ratings yet
- RESPIRO Role For Anti-Cytokine Therapies in Severe Coronavirus Disease 2019Document9 pagesRESPIRO Role For Anti-Cytokine Therapies in Severe Coronavirus Disease 2019Putu Surya SujanaNo ratings yet
- COVID-19: Pathophysiology of Acute Disease 1: SeriesDocument20 pagesCOVID-19: Pathophysiology of Acute Disease 1: SerieswiwiNo ratings yet
- Comprehensive Treatment COVID 19Document49 pagesComprehensive Treatment COVID 19ekoNo ratings yet
- 2023 Article 1194Document7 pages2023 Article 1194duraiezhilarasan.studiesNo ratings yet
- Type 1 Diabetes Triggered by Covid-19 Pandemic A Potential OutbreakDocument3 pagesType 1 Diabetes Triggered by Covid-19 Pandemic A Potential OutbreaksamuelNo ratings yet
- Joim 13091Document15 pagesJoim 13091sarabisimonaNo ratings yet
- Stroke As A Potential Complication of COVID-19-Associated Coagulopathy: A Narrative and Systematic Review of The LiteratureDocument11 pagesStroke As A Potential Complication of COVID-19-Associated Coagulopathy: A Narrative and Systematic Review of The LiteraturedenisNo ratings yet
- Estado Del Arte CoronavirusDocument17 pagesEstado Del Arte CoronavirusJosé AñorgaNo ratings yet
- 10 1002@oby 22849Document14 pages10 1002@oby 22849Hajon 1234No ratings yet
- Immunological Reviews - 2021 - John - COVID 19 and Pulmonary Fibrosis A Potential Role For Lung Epithelial Cells andDocument13 pagesImmunological Reviews - 2021 - John - COVID 19 and Pulmonary Fibrosis A Potential Role For Lung Epithelial Cells andemmanuel AndemNo ratings yet
- Sanford Consensus COVIDDocument11 pagesSanford Consensus COVIDCristina BoaventuraNo ratings yet
- 2020 June JOI COVID-19 As An Acute Inflammatory DiseaseDocument9 pages2020 June JOI COVID-19 As An Acute Inflammatory DiseaseOctavio GamezNo ratings yet
- CASE STUDY A Scarcity of Life-Saving Resources During The COVID-19 PandemicDocument2 pagesCASE STUDY A Scarcity of Life-Saving Resources During The COVID-19 Pandemicmadiha fatimaNo ratings yet
- MHS Profiles Uniformed Services UniversityDocument10 pagesMHS Profiles Uniformed Services UniversityMilitary Health SystemNo ratings yet
- Bio Mechanics of Tooth MovementDocument25 pagesBio Mechanics of Tooth MovementMohammad NimerNo ratings yet
- Introduction - To - Low - Dose - Naltrexone - LDN - 2!23!2019 - PDF - PDF Filename Utf-8introduction To Low Dose Naltrexone (LDN) 2 23 2019 PDFDocument6 pagesIntroduction - To - Low - Dose - Naltrexone - LDN - 2!23!2019 - PDF - PDF Filename Utf-8introduction To Low Dose Naltrexone (LDN) 2 23 2019 PDFRora11No ratings yet
- Aspek Legal & Etik Keperawatan Komplementer. Hengky IrawanDocument40 pagesAspek Legal & Etik Keperawatan Komplementer. Hengky IrawanBella OctaviaNo ratings yet
- Equity in Health Care Financing: The Case of MalaysiaDocument15 pagesEquity in Health Care Financing: The Case of MalaysiaViorentina YofianiNo ratings yet
- Philippine NLE Board Exam: Community Health Nursing Question & Answer W/ RationaleDocument22 pagesPhilippine NLE Board Exam: Community Health Nursing Question & Answer W/ RationaleTisyl BebzNo ratings yet
- Junaid Ahmad DarDocument12 pagesJunaid Ahmad Dar7ywtyc8rr7No ratings yet
- Cases On InflammationDocument3 pagesCases On InflammationAijan Murzalieva0% (1)
- About Cervical CancerDocument18 pagesAbout Cervical Canceramilaa.jNo ratings yet
- Role of A Pediatric Nurse in Child CareDocument14 pagesRole of A Pediatric Nurse in Child Carepraywin100% (2)
- Poor Water Supply and SanitationDocument1 pagePoor Water Supply and SanitationDienizs Labini TadenaNo ratings yet
- QMMC History - PE FormDocument1 pageQMMC History - PE FormPrisbert W. AlejoNo ratings yet
- Urinary Tract Infection (UTI)Document39 pagesUrinary Tract Infection (UTI)Sabita TripathiNo ratings yet
- NCP - Impaired Urinary EliminationDocument3 pagesNCP - Impaired Urinary EliminationFretzgine Lou ManuelNo ratings yet
- Daftar PustakaDocument9 pagesDaftar PustakaRicky RinaldiNo ratings yet
- Escasinas Docx 2Document3 pagesEscasinas Docx 2LEICETER ESCASINASNo ratings yet
- The United Insurance Company of Pakistan LTDDocument2 pagesThe United Insurance Company of Pakistan LTDAli RiazNo ratings yet
- Global Atlas of Palliative CareDocument111 pagesGlobal Atlas of Palliative CareAlexandra Raluca PepelanNo ratings yet
- Personalized AyurvedDocument13 pagesPersonalized AyurvedAtul WaghNo ratings yet
- PNPK PNPKDocument3 pagesPNPK PNPKPutri JunitasariNo ratings yet
- HEC's Policy On Drugs and Tobacco Control at HEIsDocument14 pagesHEC's Policy On Drugs and Tobacco Control at HEIsJaweria RasoolNo ratings yet
- Ethanol Intoxication in Adults - UpToDateDocument16 pagesEthanol Intoxication in Adults - UpToDateBogdanBudusanNo ratings yet
- The Basic Principles of Food SafetyDocument2 pagesThe Basic Principles of Food SafetyPaola GuayaNo ratings yet
- LHB2017Document238 pagesLHB2017haslinda84100% (2)
- Logig P Transducer Guide PDFDocument4 pagesLogig P Transducer Guide PDFbajarNo ratings yet
- Point-Of-care Ultrasonography N Engl J Med 3648749Document10 pagesPoint-Of-care Ultrasonography N Engl J Med 3648749Andreas Natan100% (1)
Long Term Complications and Rehabilitation of COVID-19 Patients
Long Term Complications and Rehabilitation of COVID-19 Patients
Uploaded by
mathias kosasihOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Long Term Complications and Rehabilitation of COVID-19 Patients
Long Term Complications and Rehabilitation of COVID-19 Patients
Uploaded by
mathias kosasihCopyright:
Available Formats
COVID-19: Transforming Global Health S-131
COMMENTARY
Long term complications and rehabilitation of COVID-19 patients
Arundhati Dasgupta,1 Atul Kalhan,2 Sanjay Kalra3
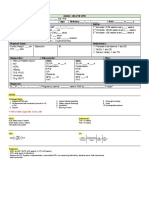
Abstract Table-1: Probable long-term complications of COVID-19.
With the ongoing pandemic of COVID-19 having caught A. Cardiorespiratory Complications
the world almost unaware millions of people across the 1. Cardiological Complications-
globe are presently grappling to deal with its acute effects *Increased Cardiovascular Disease
. Our previous experience with members of the same 2. Pulmonary Complications-
corona virus family (SARS and MERS) which have caused * Intralobular and Interlobular Septum Thickening
two major epidemics in the past albeit of much lower * Impaired FEV 25-75
* Reduced Diffusion Capacity
magnitude , has taught us that the harmful effect of such
outbreaks are not limited to acute complications alone B. Glucometabolic Complications
.Long term cardiopulmonary, glucometabolic and 1. Increased Risk of Dyslipidemia
neuropsychiatric complications have been documented 2. Increased Risk of Hyperglycaemia
following these infections .In the given circumstance it is 3. Endocrinological Complications
therefore imperative to keep in mind the possible *Hypocortisolism
complications that may occur after the acute phase of the *Primary and Central Hypothyroidism
disease subsides and to prepare the healthcare system for
such challenges. C. Neuropsychiatric Complications
1. Neuromusculoskeletal
Keywords: COVID 19, Long Term Complications, *Persistent Musculoskeletal Aches and Pains
Cardiopulmonary, Glucometabolic, Neuropsychiatric. *Femoral Head Necrosis
2. Psychiatric Complications
DOI: https://doi.org/10.5455/JPMA.32 *Depression
*Post-Traumatic Stress Disorder
Introduction *Somatoform Pain Disorder
*Panic Disorder
In December 2019, an aggressive and atypical viral
*Chronic Fatigue Syndrome
pneumonia was described with its origin *Compromised Quality Of Life
epidemiologically pin-pointed to Huanan seafood
market in Wuhan, China.1 A new human-infecting virus
of the coronavirus family was subsequently identified respectively. Although, the scale of morbidity and
with the use of next-generation sequencing, which was mortality noticed in the previous corona virus epidemics
provisionally named 2019 novel coronavirus or COVID does not match the ferocious and unprecedented havoc
19 (2019-nCoV). Till the date of writing this article almost induced by ongoing COVID19 pandemic. Genomic
27,00,000 individuals have been infected by the virus sequence studies of COVID-19 have shown that this virus
and around 1,90,000 people have succumbed to it with has nearly 50% and 77% similarity to MERS-CoV and
the case fatality reported to be close to 5%. There have SARS COV respectively.[2 Like the SARS-CoV-, the SARS-
been 2 previous outbreaks of coronavirus epidemics, CoV-2 also binds to Angiotensin converting enzyme
namely, severe acute respiratory syndrome (SARS-COV) (ACE)2 to gain entry to its host cell receptor, although it
in 2003 and Middle East respiratory syndrome (MERS - has a higher binding affinity for ACE2 as compared to
CoV) in 2012 caused by SARS and MERS viruses, the former.
We are amidst an acute healthcare crisis evoked by
1Consultant Endocrinologist, Director, Rudraksh Superspeciality Care, Siliguri, highly pathogenic nature of COVID19 with precious
India, 2Consultant Diabetes and Endocrinology, Royal Glamorgan Hospital, resources of even advanced economies being
Wales, Honorary Consultant Endocrinologist, University Hospital Of Wales, stretched to the hilt. On the same account, it is of
Cardiff, 3President, Endocrine Society of India, Bharti Hospital & B.R.I.D.E., utmost importance to fathom the potential long-term
Karnal, India. complications of this novel virus so that healthcare
Correspondence: Arundhati Dasgupta. Email: drarundhatidg@gmail.com systems are geared up to meet up such challenges in
J Pak Med Assoc (Suppl. 3)
S-132 COVID-19: Transforming Global Health
not so distant future. .Keeping in mind the structural as intensive care unit (ICU) were noticed to be inferior to
pathogenic mechanistic similarities between the 3 those treated in medical wards, though no significant
viruses of the corona family, it is perfectly reasonable differences were found for other indices like 6 minute
to assume that the long-term complications of Covid walk distances and respiratory muscle strength.7 A 15-
19 pandemic should be on similar lines as its 2 year follow up from a prospective cohort study of SARS
predecessors (although at a much higher magnitude). recovered patients from 2003 to 2018 showed
The expected long-term complications can be divided improvement in pulmonary function tests and
into three sub-groups, namely — the cardiorespiratory, radiological parameters in CT during the first year post-
glucometabolic and neuropsychiatric complications illness. The pulmonological improvement plateaued
(Table-1). during the subsequent years with around 40% and
38.5% individuals having persistent impaired.
Cardiorespiratory Complications
FEF 25%-75% and diffusion capacity respectively at the
Cardiovascular (CVD) Risk — The viruses of corona
end of 15 years. 8 These studies highlight the
family induce a significant systemic inflammatory
importance of long term follow up of survivors
response along with localized vascular inflammation
specially for the individuals who developed moderate
leading to an increased risk of myocarditis and
to severe acute respiratory disease. The clinicians
thromboembolic events during the acute-phase of
should evaluate clinical functional respiratory
illness.3 On the other hand, the long term sequalae
parameters apart from considering formal pulmonary
associated with these group of viruses on cardiovascular
function testing on follow up visits. Chest
system are less well understood at this point of time. In
physiotherapy and functional rehabilitation could help
a study, hospitalization with pneumonia (not SARS) was
alleviate morbidity in individuals with residual
associated with subsequent increase in the risk of CVD
pulmonary functional impairment.
which remained approximately 1.5-fold higher after the
first year despite adjustment of confounding risk- Glucometabolic Complications
factors. Certain hypotheses have been put forward to
explain the increased risk including pro-inflammatory Risk of Dyslipidaemia
changes in the cellular composition of the An observational study which analysed the lipid
atherosclerotic lesions, persistent systemic metabolism parameters in recovered SARS patients 12
inflammatory activity, high circulating inflammatory years after the initial acute disease, noticed a rise in
markers, persistent pro coagulant state with higher triglyceride and very-low density lipoproteins (VLDL)
levels of coagulation markers and persistence of levels apart from a significant rise in the levels of serum
dysfunction in organs such as kidneys which can directly metabolomes, namely phosphatidylinositol and
or indirectly impair the CVD parameters.4 lysophosphatidylinositol (LPI). Dyslipidaemia was noted
in 68% of the survivors as compared to 40% of the healthy
Pulmonary Complications volunteers.9 The clinicians involved in long-term
The clinical and radiological imaging features of novel rehabilitation of individuals afflicted with moderate to
coronavirus disease 2019 (COVID-19) on pulmonary severe COVID-19 infection should remain mindful of
system reported so far show "significant overlap" with potential increased risk of dyslipidaemia in this cohort of
those of severe acute respiratory syndrome (SARS) and patients. Lifestyle modification including a balanced diet
Middle East respiratory syndrome (MERS).5 Based on it, and regular exercise remains the cornerstone of
one can extrapolate the respiratory sequelae of improving long term metabolic outcomes. LPI has been
COVID19 should be on similar lines as seen on long- found to have roles to play in the excitability of dorsal root
term follow up of individuals afflicted with SARS and ganglion neurons, intestinal inflammation, and the
MERS viruses. The Computed Tomography (CT) scan migration and orientation of human breast cancer
images of individuals affected during the previous through G-protein coupled receptor 55 expressed in
epidemics (SARS and MERS) have shown ground glass these tissues which could perhaps explain various
opacities (GGO) being the dominant radiological lesions symptoms observed in the recovered SARS patients.
at 6 months (from point of infection). Interestingly,
intralobular and interlobular septum thickening were Risk of Diabetes
more prominent radiological features when these Abnormal glucose metabolism has been reported in 60%
individuals were re-evaluated at 84 months.6 Indices of of post SARS survivors as compared to 16% of controls.
pulmonary function in SARS survivors admitted to Alteration in various biochemical parameters such as
Vol. 70, No. 5 (Suppl. 3), May 2020
COVID-19: Transforming Global Health S-133
hyperinsulinemia, insulin resistance and hyperglycaemia specially considering the identification of genome
has been reported in a significant proportion of sequences of the virus in the hypothalamus and cortex
recovered SARS patients. An association between of the brain during the acute stage of the disease.14
Lysophosphatidylinositols (LPI) and glucose metabolism Subacute thyroiditis is also a condition which needs to
in recovered SARS patients has been suggested as a be kept in mind given its close association with viral
possible pathogenic mechanism. LPI is believed to play a infections. There have been reports of drug interaction
critical role in glucose homeostasis based on their action between Lopinavir/Ritonavir combination (used as part
on insulin release with G-protein coupled receptor 55 of research treatment protocols) with levothyroxine in
(GPR55) potentially being an important factor.9 Increased patients with COVID-19. Patients who are on
rate of glycolysis has been observed in the recovered levothyroxine therapy may experience a rise in TSH
SARS patients. There have been reports of islet cell levels when given above mentioned anti-viral therapy.15
damage by SARS-CoV,10 although the long-term Keeping the complex and hitherto unknown impact of
sequelae of these viruses on pancreatic islet cell function COVID-19 virus on thyroid gland function, all survivors of
has not yet been studied. moderate to severe COVID-19 infection should be
clinically and biochemically evaluated for potential
Endocrinological Complications thyroid gland dysfunction during follow-up visit.
Use of high doses of corticosteroids during the acute
infection phase of SARS can lead to subsequent Neuropsychiatric Complications
hypocortisolism. However, assessment of Neuromusculoskeletal Complications
endocrinological parameters of SARS survivors at one
Persistent neuromuscular abnormalities have been
year has revealed the presence of hypocortisolism in
observed amongst survivors of SARS. In a study involving
around 39% individuals even in the absence of steroid
128 health care workers with musculoskeletal complaints
use in around two-thirds of the studied population. This
-2-years after the SARS outbreak it was seen that
response has been attributed to be a delayed
difficulties in performing activities of daily living and work
pathological complication of SARS.11 The
tasks persisted in the patients despite receiving acute
hypocortisolism could possibly explain the persistence
rehabilitation measures.16 It has been suggested that
of symptoms seen in post SARS patients such as apathy,
bringing in force outcome measure assessment tools
lethargy, malaise, fatigue, weakness, orthostatic
which allow patients to identify specific limitations or
dizziness and anorexia.12
address overall health related quality of life (such as the
Based on observational data in SARS and MERS SF-36)17 may be helpful for the measurement of
survivors, it is imperative that individuals with moderate subjective improvement and thereby in planning proper
to severe COVID19 infection be evaluated clinically for rehabilitation measures. Femoral heads necrosis has been
potential dysfunction of adrenocorticotropin hormone reported in SARS patients which however unlike necrosis
(ACTH)-cortisol axis specially if the above-mentioned caused by other conditions such as long-term steroid use
symptoms are present. Measurement of 9 am cortisol or leukaemia, remains stable and even spontaneously
and a dynamic hormonal challenge testing (short reverse.8
synacthen test) should be carried out, if clinically
warranted. An explanation put forward to explain the Psychiatric Complications
hypothalamic-pituitary-adrenal (HPA) axis dysfunction, Psychiatric morbidities, chronic fatigue and resultant
considers it as a generic, transient adaptive functional disabilities have been persistently noted to
physiological response to the prolonged activation of be high and clinically significant amongst SARS
the HPA axis during the acute phase of the disease. This survivors. A 4-year study of SARS survivors has shown
school of thought advocates against using that active psychiatric illnesses was reported in more
supplementary steroids in such individuals considering than 40% and chronic fatigue was reported by 40.3%
this response to be an adaptive physiological state to (while 27.1% met the criterion for modified 1994
conserve energy.11 In a study of 61 survivors of SARS, Centers for Disease Control and Prevention criteria for
hypothyroidism was observed in 7% of the individuals.12 chronic fatigue syndrome.18 Another study reported
Histopathological studies have shown distortion, high incidence of depression, post-traumatic stress
dilatation, and collapse of follicular and parafollicular disorder, somatoform pain disorder, and panic disorder
architecture, apoptosis, and fibrosis.13 Hypophysitis in SARS survivors after 3 years.19 Interestingly a trend of
causing central hypothyroidism has also been progressive rise in psychiatric morbidities has been
postulated as a possible pathogenic mechanism noted after the event which continued to increase with
J Pak Med Assoc (Suppl. 3)
S-134 COVID-19: Transforming Global Health
the passage of time. Assessment by standardized As the magnitude of covid19 pandemic is at an
questionnaires showed figures around 10% to 35%20 in unprecedented scale, we can anticipate a far higher
the acute phase of the infection (acute stage to 1 surge in cardio-pulmonary dysfunction and
month) that increased to 64% at 1-year follow-up.21 A neuropsychiatric sequela in the survivors of this highly
role of immunological dysfunctions, including cytokine pathogenic novel corona virus. The experience gained
disturbances has also been suggested.22 During acute from observed long term impact of related viruses from
SARS infection, cytokine storm has been demonstrated the HuCoV family in both the physical and
and prospective studies among survivors will be psychological domains, could be used as a handy
needed to clearly understand their long-term role in checklist while planning rehabilitation of COVID19
such conditions. Alterations in the insertion/deletion survivors (Table-2). Early signal emerging from this
(I/D) polymorphism in the ACE gene have been pandemic suggests an increased case-fatality in
associated with increased risk of chronic fatigue individuals with multiple metabolic co-morbidities
syndrome and as SARS-CoV utilizes the angiotensin- including obesity, hypertension and diabetes. This
converting enzyme-2 ACE2 as a portal of cellular entry once again reinforces the importance of lifestyle
that could be a link in the explanation of association measures such as regular exercise and healthier diet to
between SARS and chronic fatigue syndrome.23 In view be adapted at individual, family, and social level to
of the high figures of long-term psychiatric dysfunction, mitigate the impact of pandemics in future.
it is important to optimize the diagnosis and treatment
of mental health morbidities by a multidisciplinary References
approach aimed at long-term rehabilitation. Adequate 1. Jung S-M, Kinoshita R, Thompson RN, Linton NM, Yang Y,
measures to dispel perceived social stigmatization and Akhmetzhanov AR et al. Epidemiological Identification of A Novel
Pathogen in Real Time: Analysis of the Atypical Pneumonia
proper functional rehabilitation would have strong Outbreak in Wuhan, China, 2019-2020. Journal of Clinical
roles to play in this context. Medicine. 2020; 9(3):637.
2. Kim JM, Chung YS, Jo HJ, Lee NJ, Kim MS, Woo SH et al.
Apart from these complications an association between Identification of Coronavirus Isolated from a Patient in Korea with
COVID 19 and a rise in cancer biomarkers like CYFRA21-1 COVID-19. Osong Public Health Res Perspect. 2020 Feb;11(1):3-7.
and HE4 have also been noted which raise an alarm of doi: 10.24171/j.phrp.2020.11.1.02. PMID: 32149036; PMCID:
PMC7045880.
potential malignancy in the future and need follow up.24 3. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential
Effects of Coronaviruses on the Cardiovascular System: A Review.
Conclusion JAMA Cardiol. Published online March 27, 2020.
doi:10.1001/jamacardio.2020.1286.
Although the COVID 19 virus was only reported for the
4. Corrales-Medina VF, Alvarez KN, Weissfeld LA, Angus DC, Chirinos
first time in December 2019, it has already transcended JA, Chang CC et al . Association between hospitalization for
continental borders posing catastrophic threat to pneumonia and subsequent risk of cardiovascular disease.JAMA.
healthcare systems and global economies during the 2015 Jan 20;313(3):264-74. doi: 10.1001/jama.2014.18229.
5. Melina Hosseiny, Soheil Kooraki, Ali Gholamrezanezhad, Sravanthi
acute phase of illness. The long term implications of
Reddy, Lee Myers. Radiology Perspective of Coronavirus Disease
Covid19 infection on morbidity and mortality are yet 2019 (COVID-19): Lessons From Severe Acute Respiratory
unknown although some basic deductions can be Syndrome and Middle East Respiratory Syndrome. American
made based on clinical experience gained from Journal of Roentgenology, 2020; 1 DOI: 10.2214/AJR.20.22969.
6. Wu. X, Dong. D, Ma. D. Thin-section computed tomography
residual long term effect of SARS and MERS epidemics.
manifestations during convalescence and long-term follow-up of
patients with severe acute respiratory syndrome (SARS). Med Sci.
Table-2: List of recommendations to identify and treat the anticipated long-term Monit. 22, 2793-2799 (2016).
7. Hui DS1, Wong KT, Antonio GE, Tong M, Chan DP, Sung JJ Long-
complications of COVID 19.
term sequelae of SARS: physical, neuropsychiatric, and quality-of-
life assessmentHong Kong Med J 2009;15(Suppl 8):S21-3.
1. Clinical Screening for Symptoms Of Cardiovascular Complications, Neuromuscular 8. Zhang, P., Li, J., Liu, H.Han N, Ju J, Kou Y et al. Long-term bone and
Complications, Thyroid Disorders, Standardised Questionnaires For Assessment of lung consequences associated with hospital-acquired severe
Psychiatric Status. acute respiratory syndrome: a 15-year follow-up from a
prospective cohort study. Bone Res 8, 8 (2020).
2. Laboratory Investigations-Blood Sugar, Lipid Profile, Thyroid Function Tests, Se https://doi.org/10.1038/s41413-020-0084-5.
Cortisol (If Clinically Indicated), Pulmonary Function Tests 9. Wu. Q, Zhou. L, Sun, X. Yan, Z., Hu, C., Wu, J.et al. Altered Lipid
Metabolism in Recovered SARS Patients Twelve Years after
3. Adaptation of Healthy Lifestyle Measures Infection. Sci Rep 7, 9110 (2017). https://doi.org/10.1038/s41598-
017-09536-z.
10. Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its
4. Rehabilitation Measures Like Chest Physiotherapy, Psychiatric Counselling, receptor damages islets and causes acute diabetes.Acta Diabetol.
Functional Rehabilitation 2010 Sep;47(3):193-9. doi: 10.1007/s00592-009-0109-4. Epub
Vol. 70, No. 5 (Suppl. 3), May 2020
COVID-19: Transforming Global Health S-135
2009 Mar 31. 18. Lam MH, Wing YK, Yu MW, Leung CM, Ma RC, Kong AP et al.
11. Chrousos G.P., Kaltsas G. Post-SARS sickness syndrome Mental morbidities and chronic fatigue in severe acute respiratory
manifestations and endocrinopathy: how, why, and so what? Clin syndrome survivors: long-term follow-up. Arch Intern Med
Endocrinol (Oxf) 2005;63:363-365. 2009;169:2142-7.
12. Leow MK, Kwek DS, Ng DS, Ong KC, Kaw GJ, Lee LS. 19. Wing YK, Leung CM. Mental health impact of severe acute
Hypocortisolism in sur- vivors of severe acute respiratory respiratory syndrome: a prospective study. Hong Kong Med J
syndrome (SARS). Clin Endocrinol (Oxf ). 2005; 63(2):197-202 . 2012;18 Suppl 3:24-7.
13. Wei L, Sun S, Xu CH, Zhang J, Xu Y, Zhu H et al. Pathology of the 20. Wu KK, Chan SK, Ma TM. Posttraumatic stress after SARS. Emerg
thyroid in severe acute respiratory syndrome. Hum Pathol. 2007 Infect Dis. 2005;11(8):1297-1300.
Jan;38(1):95-102. doi: 10.1016/j.humpath.2006.06.011. Epub 2006 21. Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC
Sep 25. PMID: 16996569; PMCID: PMC7112059. et al. Stress and psychological distress among SARS survivors 1
14. Gu J., Gong E., Zhang B. Multiple organ infection and the year after the outbreak. Can J Psychiatry. 2007;52(4):233- 240.
pathogenesis of SARS. JEM. 2005;202:417-424. 22. Delahanty DL, Doug-all AL, Craig KJ, Jenkins FJ, Baum A. Chronic
15. Touzot M, Beller CL, Touzot F, Louet AL, Piketty C.Dramatic stress and natu- ral killer cell activity after exposure to traumatic
interaction between levothyroxine and lopinavir/ritonavir in a death. Psychosom Med. 1997; 59(5):467-476.
HIV-infected patient.AIDS. 2006 May 12;20(8):1210-2. 23. Vladutiu, G.D. & Natelson, B.H. Association of medically
16. Law RK, Lee EW, Poon PY ,Lau TC, Kwok KM, Chan AC. The unexplained fatigue with ACE insertion/deletion polymorphism
functional capacity of healthcare workers with history of severe inGulf War veterans. Muscle and Nerve, (2004) 30, 38 -43.
acute respiratory distress syndrome (SARS) complicated with 24. Wei, Xiuqi and Su, Jingyu and Lin, Yuqi and Wei, Jiazhou and Wan,
avascular necrosis - case report. Work. 2007; 30:17-26. Huimin and Cao, SARS-COV-2 Infection Causes Dyslipidemia and
17. Paterson C. Measuring outcomes in primary care: a patient Increases Levels of Cancer Biomarkers in COVID-19 Patients
generated measure, MYMOP, compared with the SF-36 health (3/10/2020). Available at SSRN: https://ssrn.com/abstract=3552854
survey. BMJ. 1996; 312:1016-1020 or http://dx.doi.org/10.2139/ssrn.3552854.
J Pak Med Assoc (Suppl. 3)
You might also like
- Current Procedural Terminology (CPT CODING)Document5 pagesCurrent Procedural Terminology (CPT CODING)Rabindra P.Singh50% (2)
- James Tin Yau So - Treatment of Disease With AcupunctureDocument397 pagesJames Tin Yau So - Treatment of Disease With Acupuncturearyaa202096% (26)
- PUD QuestionsDocument5 pagesPUD QuestionsAmira Paguyo QuilapioNo ratings yet
- Long COVID: Post-Acute Sequelae of COVID-19 With A Cardiovascular FocusDocument22 pagesLong COVID: Post-Acute Sequelae of COVID-19 With A Cardiovascular FocusPhitsanu SuntornpiyapanNo ratings yet
- COVID ProlongadoDocument22 pagesCOVID ProlongadoSMIBA MedicinaNo ratings yet
- Long COVID: Post-Acute Sequelae of COVID-19 With A Cardiovascular FocusDocument22 pagesLong COVID: Post-Acute Sequelae of COVID-19 With A Cardiovascular FocusWalter ReyesNo ratings yet
- Post Acute Coronavirus (COVID-19) Syndrome - StatPearls - NCBI BookshelfDocument13 pagesPost Acute Coronavirus (COVID-19) Syndrome - StatPearls - NCBI BookshelfThành Tài TrầnNo ratings yet
- Post-COVID Syndrome Incidence, Clinical SpectrumDocument7 pagesPost-COVID Syndrome Incidence, Clinical SpectrumJeane ClaudiaNo ratings yet
- Long Covid 1Document5 pagesLong Covid 1lakshminivas PingaliNo ratings yet
- A Clinic Blueprint For Post-Coronavirus Disease 2019 RECOVERY Learning From The Past, Looking To The FutureDocument11 pagesA Clinic Blueprint For Post-Coronavirus Disease 2019 RECOVERY Learning From The Past, Looking To The FutureCARLA CRISTINA DE ARAUJONo ratings yet
- 14- COVID-19 - RISKS TO THE CENTRAL NERVOUS SYSTEM AND CARDIOVASCULAR DAMAGEDocument4 pages14- COVID-19 - RISKS TO THE CENTRAL NERVOUS SYSTEM AND CARDIOVASCULAR DAMAGEDaniel lipphausNo ratings yet
- Unraveling The Mystery Surrounding Post-Acute Sequelae of COVID-19Document16 pagesUnraveling The Mystery Surrounding Post-Acute Sequelae of COVID-19Ricardo Pariona LlanosNo ratings yet
- Long COVID19 Syndrome ADocument19 pagesLong COVID19 Syndrome Arbatjun576No ratings yet
- A Review of Respiratory Post-Acute Sequelae of COVID-19 (PASC)Document5 pagesA Review of Respiratory Post-Acute Sequelae of COVID-19 (PASC)elieser toding mendilaNo ratings yet
- Aspectos Autonómicos Post CovidDocument7 pagesAspectos Autonómicos Post Covidtavo570No ratings yet
- Updates On Clinical Trials Evaluating The Regenerative Potential of Allogenic Mesenchymal Stem Cells in COVID-19Document11 pagesUpdates On Clinical Trials Evaluating The Regenerative Potential of Allogenic Mesenchymal Stem Cells in COVID-19diana.alyNo ratings yet
- Mechanisms of Long COVID An Updated ReviewDocument10 pagesMechanisms of Long COVID An Updated Reviewemmanuel AndemNo ratings yet
- Geriatric Patient With Osteoarthritis and Obesity Survived From Critically Ill of COVID-19: A Case ReportDocument5 pagesGeriatric Patient With Osteoarthritis and Obesity Survived From Critically Ill of COVID-19: A Case Reportnadila raudhani pNo ratings yet
- Long COVID or post-COVID-19 Syndrome Putative Pathophysiology, Risk FactorsDocument18 pagesLong COVID or post-COVID-19 Syndrome Putative Pathophysiology, Risk FactorsVane SchulzeNo ratings yet
- Paper 8842Document7 pagesPaper 8842IJARSCT JournalNo ratings yet
- Effects of SARS-COVID-19 Infection On The Cardiovascular SystemDocument5 pagesEffects of SARS-COVID-19 Infection On The Cardiovascular SystemSabrina JonesNo ratings yet
- Covid-19: What Do We Need To Know About Icu Delirium During The Sars-Cov-2 Pandemic?Document7 pagesCovid-19: What Do We Need To Know About Icu Delirium During The Sars-Cov-2 Pandemic?bayu bagusNo ratings yet
- Int J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaDocument12 pagesInt J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaRebeca EscutiaNo ratings yet
- Progress: Pathological Inflammation in Patients With COVID-19: A Key Role For Monocytes and MacrophagesDocument8 pagesProgress: Pathological Inflammation in Patients With COVID-19: A Key Role For Monocytes and MacrophagesagenwongNo ratings yet
- Reviews: COVID-19 and Cardiovascular Disease: From Basic Mechanisms To Clinical PerspectivesDocument16 pagesReviews: COVID-19 and Cardiovascular Disease: From Basic Mechanisms To Clinical PerspectivesLAURA ALEJANDRA PARRA GOMEZNo ratings yet
- COVID-19: Pathophysiology of Acute Disease 1: SeriesDocument21 pagesCOVID-19: Pathophysiology of Acute Disease 1: SeriesMyatnoe KhinNo ratings yet
- Diabetes Mellitus in The Context of COVID-19 La Diabetes Mellitus en El Contexto de La COVID-19Document8 pagesDiabetes Mellitus in The Context of COVID-19 La Diabetes Mellitus en El Contexto de La COVID-19Tatiana Belén García MogollónNo ratings yet
- Mesenchymal Stem Cell Immunomodulation and Regeneration TherapeuticsDocument13 pagesMesenchymal Stem Cell Immunomodulation and Regeneration TherapeuticswiwiNo ratings yet
- International Immunopharmacology: Mohammad Shah Alam, Daniel M. Czajkowsky, Md. Aminul Islam, Md. Ataur RahmanDocument12 pagesInternational Immunopharmacology: Mohammad Shah Alam, Daniel M. Czajkowsky, Md. Aminul Islam, Md. Ataur RahmanJimena Vásquez RodríguezNo ratings yet
- Severe Covid-19: Clinical PracticeDocument10 pagesSevere Covid-19: Clinical PracticejoelNo ratings yet
- Long-COVID: An Evolving Problem With An Extensive Impact: Clinical UpdateDocument3 pagesLong-COVID: An Evolving Problem With An Extensive Impact: Clinical UpdateArif wicaksonoNo ratings yet
- COVID-19 and Diabetes MellitusDocument6 pagesCOVID-19 and Diabetes MellitusUlysses GamayonNo ratings yet
- Long COVID19 Syndrome As A Fourth Phase of SARSCoV2 Infection - 2022 - EDIMES Edizioni Medico ScientificheDocument8 pagesLong COVID19 Syndrome As A Fourth Phase of SARSCoV2 Infection - 2022 - EDIMES Edizioni Medico ScientificheftasiaNo ratings yet
- Koc 2022Document14 pagesKoc 2022John GoranitisNo ratings yet
- Background To Coronavirus (COVID-19) - ICM Anaesthesia COVID-19Document2 pagesBackground To Coronavirus (COVID-19) - ICM Anaesthesia COVID-19kajelchaNo ratings yet
- Reviews: Immunity, Endothelial Injury and Complement-Induced Coagulopathy in COVID-19Document19 pagesReviews: Immunity, Endothelial Injury and Complement-Induced Coagulopathy in COVID-19Edo RezaprasgaNo ratings yet
- Patfis Covid 6Document6 pagesPatfis Covid 6mayaNo ratings yet
- Role of Homoeopathy in Management of Covid-19 Complications: ISSN 2515-8260 Volume 7, Issue 2, 2020Document8 pagesRole of Homoeopathy in Management of Covid-19 Complications: ISSN 2515-8260 Volume 7, Issue 2, 2020mubbunNo ratings yet
- MAY 2020 SINTOMAS Gastrointestinal Symptoms Associated WithDocument14 pagesMAY 2020 SINTOMAS Gastrointestinal Symptoms Associated WithMayaraNo ratings yet
- BernasDocument17 pagesBernasYezekael Sebastian QuintinusNo ratings yet
- Cells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Document29 pagesCells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Yoni LinggaNo ratings yet
- Brain SciencesDocument13 pagesBrain SciencesRuhana Sk Abd RazakNo ratings yet
- Imaging in COVID 19 Related Myocardial InjuryDocument12 pagesImaging in COVID 19 Related Myocardial Injuryorkut verificationNo ratings yet
- Diagnosis of Sars-Cov-2 Infection in The Setting of The Cytokine Release SyndromeDocument12 pagesDiagnosis of Sars-Cov-2 Infection in The Setting of The Cytokine Release SyndromeTufik NaderNo ratings yet
- Banerjee 2021Document15 pagesBanerjee 2021georgeNo ratings yet
- EXPODocument18 pagesEXPOEstefy Cerda MoscosoNo ratings yet
- Pi Is 0003999321003269Document12 pagesPi Is 0003999321003269Amanda SchaefferNo ratings yet
- Astma Impact IncovidDocument9 pagesAstma Impact IncovidRosintchi MirsalNo ratings yet
- Neurobiologia Del COVID19Document25 pagesNeurobiologia Del COVID19paola coralNo ratings yet
- Jurnal DipsneaDocument7 pagesJurnal DipsneaAgnes AriscaNo ratings yet
- RESPIRO Role For Anti-Cytokine Therapies in Severe Coronavirus Disease 2019Document9 pagesRESPIRO Role For Anti-Cytokine Therapies in Severe Coronavirus Disease 2019Putu Surya SujanaNo ratings yet
- COVID-19: Pathophysiology of Acute Disease 1: SeriesDocument20 pagesCOVID-19: Pathophysiology of Acute Disease 1: SerieswiwiNo ratings yet
- Comprehensive Treatment COVID 19Document49 pagesComprehensive Treatment COVID 19ekoNo ratings yet
- 2023 Article 1194Document7 pages2023 Article 1194duraiezhilarasan.studiesNo ratings yet
- Type 1 Diabetes Triggered by Covid-19 Pandemic A Potential OutbreakDocument3 pagesType 1 Diabetes Triggered by Covid-19 Pandemic A Potential OutbreaksamuelNo ratings yet
- Joim 13091Document15 pagesJoim 13091sarabisimonaNo ratings yet
- Stroke As A Potential Complication of COVID-19-Associated Coagulopathy: A Narrative and Systematic Review of The LiteratureDocument11 pagesStroke As A Potential Complication of COVID-19-Associated Coagulopathy: A Narrative and Systematic Review of The LiteraturedenisNo ratings yet
- Estado Del Arte CoronavirusDocument17 pagesEstado Del Arte CoronavirusJosé AñorgaNo ratings yet
- 10 1002@oby 22849Document14 pages10 1002@oby 22849Hajon 1234No ratings yet
- Immunological Reviews - 2021 - John - COVID 19 and Pulmonary Fibrosis A Potential Role For Lung Epithelial Cells andDocument13 pagesImmunological Reviews - 2021 - John - COVID 19 and Pulmonary Fibrosis A Potential Role For Lung Epithelial Cells andemmanuel AndemNo ratings yet
- Sanford Consensus COVIDDocument11 pagesSanford Consensus COVIDCristina BoaventuraNo ratings yet
- 2020 June JOI COVID-19 As An Acute Inflammatory DiseaseDocument9 pages2020 June JOI COVID-19 As An Acute Inflammatory DiseaseOctavio GamezNo ratings yet
- CASE STUDY A Scarcity of Life-Saving Resources During The COVID-19 PandemicDocument2 pagesCASE STUDY A Scarcity of Life-Saving Resources During The COVID-19 Pandemicmadiha fatimaNo ratings yet
- MHS Profiles Uniformed Services UniversityDocument10 pagesMHS Profiles Uniformed Services UniversityMilitary Health SystemNo ratings yet
- Bio Mechanics of Tooth MovementDocument25 pagesBio Mechanics of Tooth MovementMohammad NimerNo ratings yet
- Introduction - To - Low - Dose - Naltrexone - LDN - 2!23!2019 - PDF - PDF Filename Utf-8introduction To Low Dose Naltrexone (LDN) 2 23 2019 PDFDocument6 pagesIntroduction - To - Low - Dose - Naltrexone - LDN - 2!23!2019 - PDF - PDF Filename Utf-8introduction To Low Dose Naltrexone (LDN) 2 23 2019 PDFRora11No ratings yet
- Aspek Legal & Etik Keperawatan Komplementer. Hengky IrawanDocument40 pagesAspek Legal & Etik Keperawatan Komplementer. Hengky IrawanBella OctaviaNo ratings yet
- Equity in Health Care Financing: The Case of MalaysiaDocument15 pagesEquity in Health Care Financing: The Case of MalaysiaViorentina YofianiNo ratings yet
- Philippine NLE Board Exam: Community Health Nursing Question & Answer W/ RationaleDocument22 pagesPhilippine NLE Board Exam: Community Health Nursing Question & Answer W/ RationaleTisyl BebzNo ratings yet
- Junaid Ahmad DarDocument12 pagesJunaid Ahmad Dar7ywtyc8rr7No ratings yet
- Cases On InflammationDocument3 pagesCases On InflammationAijan Murzalieva0% (1)
- About Cervical CancerDocument18 pagesAbout Cervical Canceramilaa.jNo ratings yet
- Role of A Pediatric Nurse in Child CareDocument14 pagesRole of A Pediatric Nurse in Child Carepraywin100% (2)
- Poor Water Supply and SanitationDocument1 pagePoor Water Supply and SanitationDienizs Labini TadenaNo ratings yet
- QMMC History - PE FormDocument1 pageQMMC History - PE FormPrisbert W. AlejoNo ratings yet
- Urinary Tract Infection (UTI)Document39 pagesUrinary Tract Infection (UTI)Sabita TripathiNo ratings yet
- NCP - Impaired Urinary EliminationDocument3 pagesNCP - Impaired Urinary EliminationFretzgine Lou ManuelNo ratings yet
- Daftar PustakaDocument9 pagesDaftar PustakaRicky RinaldiNo ratings yet
- Escasinas Docx 2Document3 pagesEscasinas Docx 2LEICETER ESCASINASNo ratings yet
- The United Insurance Company of Pakistan LTDDocument2 pagesThe United Insurance Company of Pakistan LTDAli RiazNo ratings yet
- Global Atlas of Palliative CareDocument111 pagesGlobal Atlas of Palliative CareAlexandra Raluca PepelanNo ratings yet
- Personalized AyurvedDocument13 pagesPersonalized AyurvedAtul WaghNo ratings yet
- PNPK PNPKDocument3 pagesPNPK PNPKPutri JunitasariNo ratings yet
- HEC's Policy On Drugs and Tobacco Control at HEIsDocument14 pagesHEC's Policy On Drugs and Tobacco Control at HEIsJaweria RasoolNo ratings yet
- Ethanol Intoxication in Adults - UpToDateDocument16 pagesEthanol Intoxication in Adults - UpToDateBogdanBudusanNo ratings yet
- The Basic Principles of Food SafetyDocument2 pagesThe Basic Principles of Food SafetyPaola GuayaNo ratings yet
- LHB2017Document238 pagesLHB2017haslinda84100% (2)
- Logig P Transducer Guide PDFDocument4 pagesLogig P Transducer Guide PDFbajarNo ratings yet
- Point-Of-care Ultrasonography N Engl J Med 3648749Document10 pagesPoint-Of-care Ultrasonography N Engl J Med 3648749Andreas Natan100% (1)