Professional Documents
Culture Documents
Newborn Care 1
Newborn Care 1
Uploaded by
Francine LaxaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Newborn Care 1
Newborn Care 1
Uploaded by
Francine LaxaCopyright:
Available Formats
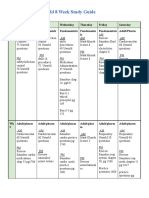
THE NEWBORN CARE 7-10 - indicates healthy newborn
3-6 - moderately depressed
The Nurses’ Role in MC Care 0-2 - severely depressed
• 1. PA of the NB If score is less than 7 at 5 minutes, the score should be performed in
a. transitional – immediately after birth (initial) 10 minutes.
b. physiologic adaptation
• 2. Physical/ Behavior APGAR Score Implementation:
• 3. Promote parent-infants bonding – be alert in any problems in 7-10 - very good; rarely needs resuscitation
attachment 3-6 - fair requires resuscitation, suctioning signify moderate difficulty
• 4. Prepares the family for discharge needs further assessment and medical intervention
a. demonstrate physical care of the NB 0-2 - poor, requires intensive resuscitation needs intensive medical
b. provide hx/discharge teaching/ info, anticipatory intervention
guidance
Ensure Newborn’s Proper Identification
Immediate Care of the Newborn 1. Check identification band
1. Dry the newborn immediately after delivery a. name of baby (e.g. Bb boy Fernando)
2. Clear airway PRN (as necessary) b. name of mother
3. Assess baby’s response to birth c. date and time of delivery
a. Check APGAR (1-5 mins after birth) d. Doctors (OB and Pedia)
4. Promote skin to skin contact 2. Footprints (depends on agency)
5. Ensure newborn’s identification 3. Baby tag and crib tag. Check always and should match at all
6. Take vital signs, anthropometric and do PA times.
7. Dress the umbilical cord 4. Take fingerprint of mother
8. Administer medication
9. Swaddle the baby and place in side-lying position. Identification of the Newborn
10. Give a full bath • Safety concerns related to newborn identification procedures
• Specific facility procedures
1.Dry newborn immediately • NCMEC: National Center for Missing and Exploited Children
- Wipe and dry using clean warmed blankets • “Profile” of abductor
- Place baby in a radiant warmer (put thermometer with probe)
- Remove wet linens Take Vital Signs
- Rub or flick soles of newborn if additional stimulation is required. • Maintain stable body temperature
- Do not slap buttocks (no beneficial effect) • 36.5 – 37.5◦C (99.7-99.5◦ F) axillary
- Stimulate baby to breathe • 36.5 – 37.6◦ C (97.7-99.7◦ F) rectal more accurate
- Stimulate crying by gentle friction • RR 30-60 breaths per minute
- Assess characteristic of cry (should be strong and lusty) • CR 120-160 beat per minute
- Assess for nasal flaring, retractions and abnormal respiration • BP seldom taken
Factors Predisposing the Newborn to Excessive Heat Loss Maintain Temperature Stability
• Large surface area results in heat loss to environment • Wrap newborn in a warm blanket and put in a stockinet cap on
• Newborn’s thin layer of adipose is poor insulator newborn’s head.
• Newborn cannot shiver to increase heat production • Usually unstable and takes 6-8 hours to stabilize (DOH
• Metabolizes brown fat stores to generate heat recommends after 24 hrs)
• Observe for hypothermia/ hyperthermia
2. Clear airway • Sign of infection, dehydration, inadequate clothing, prematurity
- Provide for patent airway
- Suction PRN Maintain Stable Body Temperature
- Newborns are obligatory nasal breather • Mechanisms of NB heat loss
- APGAR SCORE Developed by Virginia Apgar (1950), American - Evaporation
anesthesiologist - Radiation
- Conduction
Purpose of APGAR score: - Convection
1. She devised a scoring system that helped to evaluate a
newborn’s physical condition after birth help to determine any The Anthropometric Measurements of Newborn
urgent need for emergency or extra medical care (e.g. acidosis, • HC 33 – 35.5 cm (13-14 in) occipito-frontal
CPR) • CC 31- 33 cm measure at nipple line
2. 2.To evaluate how well the newborn adjust to extra uterine life. • AC 31-33 cm
3. Assess newborn’s response to birth • Length 48-53 cm (19-21 inches)
4. Performed and record at 1, 5 minutes and 10 minutes as needed • Body weight 2500-4000 grams
The CORD
• Apply cord clamp 1in from the base; cut above the cord clamp
• Cord is pearly white gelatinous
• Assess for the presence of the BV (2 Arteries, 1 vein AVA)
• Assess for intact cord and ensure that clamp is secured
• Cord should be clamped for at least the 1st 24 hours after birth
• Clamp can be removed when cord is dried (usually on day 2)
• Note for any bleeding or drainage from the cord
• Note for any foul odor from the cord
• Monitor cord meconium staining (green = baby stool discharge)
Administer medications
1. Give Crede’s prophylaxis
APGAR Score Interpretation: 2. Vitamin K
fcnlxa – St. Luke’s College of Nursing 1
3. Hepatitis B vaccination • Birth weight - 2500 – 4000 g (6 – 9 lbs)
4. BCG vaccine (optional/it depends) • Average weight 3400gms (7.5 lbs)
• 1. Crede’s Prophylaxis • Weight is taken soon after birth. WEIGHT LOSS occurs rapidly after
1. Application of ophthalmic medication to prevent birth. NEONATE LOSSES about 10 % of the BW by 3 -4 days of but
Ophthalmia Neonatorum usually regained by the 10th day of life.
2. Give eye medications • BW & BL are very important because they provide a baseline for
3. Ophthalmia neonatorum is an infectious conjunctivitis in assessment of future growth
newborn • Assess for SGA (Small for Gestational age), AGA (Appropriate),
4. An infection contracted in the birth canal of mother w/ LGA (Large)
gonorrhea or chlamydia
5. Given within1st hour after birth Vital signs:
6. Rx: ophthalmic ointment or drops • Measure VS when the infant is still quiet
- Erythromycin (0.5%) • CR, RR, BP fluctuates with stress, crying,
- Tetracycline (1%) / Gentamicin • movements and sleep wake cycles
- Silver nitrate solution (used infrequently)
7. Parental right to waive Heart
8. How to apply Opthalmic medication? • Heart Rate: 120-160 beats per min
• the child is placed in a supine position: • Low & high
a. Eye drops • Assess for 1 full minute (due to some irregularities)
• to instill the medication, the lower lid is pulled to form a • Auscultation of heart sounds difficult
pocket and the solution is dropped into the pocket o Murmurs
b. Eye Ointment o S1, S2 should be clear
• applied to inner to outer canthus • PMI: Point of maximum impulse
Take note: make sure that the tip of tube/dropper will o *Rhythm regular at 4th to 5th intercostal space
not touch the eye - Slightly left of midclavicular line
• 2. Vitamin K injection (Aquamephyton, Phytonadione) • Rapid & irregular and with slight murmur
o Route: IM (single dose) o Murmur normal
o Site: Vastus lateralis (or Rectus Femoris) - Foramen Ovale still open
o Dose: 0.5 to 1 mg (0.1 ml term / 0.05ml preterm) - adjustment period
o Given to prevent hemorrhagic bleeding o Tachycardia – RDS (Respiratory Distress Syndrome)
o Catalyze the synthesis of prothrombin in the liver which is o Bradycardia – CHD (Coronary Heart Disease)
needed for blood clotting and coagulation. • Pulses sites: Apical, Brachial, femoral, pedal
• 3. Hepatitis B Vaccine o Check for equality and strength
o Hepatitis B (HBV) Vaccine Administration o Femoral – check if absent, COA (Contraction of Aorta)
o Recommended by CDC (Center for Ds. Control) for all • Dextrocardia – heart on right side
newborns before they leave the hospital
o decrease the incidence HBV in children and its serious Blood Pressure
consequences (e.g cirrhosis, liver Ca) • Normal: at birth systolic 60-80 mm Hg; diastolic 40- 50 mm Hg
o Given IM • at 10th DOL (day of life) systolic 95 – 100 mm Hg diastolic slightly
o If infant is born to HBsAg + they should be immunized w/ HBV increased
& HBIG w/in 12 hours. BCG • Not routinely checked in healthy newborn
o BCG can be given.it depends on the institution. • Only if problem is suspected (e.g Cardiac Problem) e.g COA –
- Swaddle the Baby all 4 extremities BP is taken
- Place right side lying • Varies with changes in NB’s activity and blood volume
o Swaddling the baby will keep them from hypothermia • More accurate if NB is resting
o Putting them on right side to drain out secretions
Respiratory Rate:
Bath • 30-60 breaths / minute. Assess for 1 full minute
• Give Full bath • Irregular, rapid, shallow, quiet, unlabored, symmetrical
• To clean the baby and remove blood and mucus • With short periods of apnea (5- 10 secs), with slight retractions
• Use lukewarm water and anti-microbial soap that is hypo • Breath sounds present, equal, clear
allergenic • Diaphragmatic and abdominal
• Take note: full bath should be done under radiant warmer and • Check and observe RR and effort
when temperature is already stable (between 12-24 hrs, 24hrs • Bradypnea – Narcosis from analgesics, anesthetics, trauma
suggested by DOH) • Tachypnea – RDS, MAP (Meconium Aspiration), CDH
II. Physical Assessment Lungs
• Basic Principles: • Pauses >20 seconds suggestive of apnea
1. Review perinatal history • Auscultate lungs when infant quiet
2. Keep newborn warm during the examination. • Check for: breath sounds
3. Begin with the general observations. Then perform - crackles, rhonchi, wheezes (fluid in lungs)
assessment that are least disturbing. - expiratory grunting (narrowing of bronchi nasal flaring,
a. Assess the infant’s color retractions, labored breathing (RDS)
b. Auscultate only in a quiet environment
4. Take note of the life-threatening abnormalities that require Temperature:
immediate attention. • Axillary is the preferred site
5. Calm the infant before doing the examination • Rectal temperature more accurate.
6. Have the necessary tools at hand • Temperature is taken per anal INITIALLY TO CHECK FOR PATENCY
7. Handle the infant gently OF ANUS! (Insert 1 inch)
8. Initiate nursing interventions for abnormal findings. Assess for • Succeeding temperature is taken by axillary
gross anomalies • ROUTINE USE OF RECTAL TEMP IS AVOIDED because of POSSIBLE
9. Document all findings (normal and abnormal) for legal INTESTINAL PERFORATION / ANAL MUCOSAL PERFORATION
purposes, document what has really been done because of thermometer insertion and may also cause vagal
nerve stimulation.
Take anthropometric measurements: o Other sites of temperature:
fcnlxa – St. Luke’s College of Nursing 2
a. Tympanic • Assymmetry of the head as a result of pressure in the birth canal
b. Skin - 36.5 – 37 C • Disappear in 72 hours
- Using probe; slightly lower than the core
• Temperature stabilizes in 8 – 10 hours after birth Sutures
• VS taken q 15 mins during the 1st hour and hourly during the next • Separating lines of the skull, may override at the birth because
few hours then q 4 (depends on hospital policy) thereafter if it of extreme pressure exerted by the passage through the birth
remains stable. canal, sort of overlap
• Stop development at 7 yrs old
General Appearance:
• yields valuable clues to the physical status of infant Anterior Fontanel
A. Posture: • At the junction of 2 parietal bones and the 2 fused frontal bones
• Infant assume a well flexed position (normal position in utero) • felt as soft spot, flat diamond shape
• Flexion decrease area of skin exposed to environment, thereby • 3-4 cm wide and 2-3 cm long
reducing heat loss • It closes at 12 to 18 months
• Fists are clenched, movement symmetrical • If > 5cm maybe a sign of HYDROCEPHALUS and CRETINISM
• With slight tremors during crying
• Hypotonic, limp, flaccid, “floppy” or rigid extremities are seen in Posterior Fontanel
preterm, hypoxia, medications, CNS trauma • Located between occipital and parietal bone
• Hypertonic – NAS (Neonatal Abstinence Syndrome), CNS • Triangular, 0.5 cm to 1 cm wide
damage • Small, not readily felt
• Jitteriness/tremors – low glucose / low calcium • Closes between birth and 2-3 months
• Opisthotonos, seizure, stiff neck – CNS damage
Caput Succedaneum
B. Behavior • Edema of the scalp
• Observe and monitor for alertness, drowsiness and irritability • This is due to the pressure of the presenting part during labor
(common signs of neurologic problems) some questions may be • Disappears after 3 days
ask:
a. Is the infant awakened easily by loud noise? Cephalhematoma
b. is the infant comforted by rocking, sucking, cuddling? • Rupture of periosteal capillary of the skull.
c. Do there seem to be periods of deep & light sleep? • This is due to pressure in birth canal
d. Does infant seem to be satisfied after feeding? • Usually absorbed in 6 weeks without treatment
• Behavior
a. Level of responsiveness to noxious stimuli Craniotabes
b. Transition of sleep states evident • Localized softening of the cranial bones
• Can be indented by pressure of a finger
C. Skin Color • Correct itself with treatment after some months
• Check color. Inspect and palpate. Use natural light • More common among 1st born because of early lightening
• Generally pinkish
• Depends on the racial and familial background Face
• With acrocyanosis (normal / chilled) • Check for symmetry
• Check for cyanosis: • No bell’s palsy (facial nerve paralysis/drooping of mouth to one
a. circum-oral – cyanosis of mouth & central side
b. areas (requires suctioning) • Due to use of forceps/ birth trauma
c. peripheral – due to cold environment o Permanent – CN7 is cut
d. infection, hypoglycemia, cardiopulmo, cardiac ds. o Temporary – pressure to CN7
• Dark red (phletora) – premature • Check for delivery history
• Pallor – CV, CNS, blood dyscrasia, blood loss, twin to twin,
nosocomial infection Eyes
• Petechiea (small rashes deep on the skin, possible bleeding) • Slate gray (light skin) or brown- gray (dark skin)
• Ecchymoses (manifestation of bleeding) • PERRLA – no keyhole (coloboma)
• Gray – hypotension, poor perfusion, infection • Symmetrical and clear
• Yellowish discoloration – jaundice • Cornea should be round and adult sized
• may have subconjunctival hemorrhage (small broken tiny
General Assessment: capillaries on sclera)
• Should be performed in cephalocaudal manner • Eyelids edematous for first days of life
• Drainage
Newborn Head: • Able to track and fixate momentarily
• 25% of the body length. Largest part of infant’s body • Eye cross because of weak extraocular muscles, normal
• Bones are not fused strabismus, tearless
• Sutures – palpable; may override (only at birth) • Nystagmus
• Assess for head circumference • Strabismus
o Microcephaly (cranial synostosis) • Corneal Reflex
o Macrocephaly (hydrocephalus) • Red reflex
• Anencephaly • Blink Reflex present
• Head lag COLOBOMA
• Assess contour of head (molding) EXOTROPIA STRABISMUS
• Assess fontanels—anterior, posterior ESOTROPIA STRABISMUS
• Degree of head control/head lag
• Result of birth trauma Ears
– Caput succedaneum • Pinna
– Cephalhematoma • Canals
– Physiologic craniotabes • Tympanic membrane
• Otoacoustic Emission
Molding • Auditory ability (ABR testing)
• Startle reflex
fcnlxa – St. Luke’s College of Nursing 3
• Well-formed notch of ears on straight line with outer canthus of • Femoral pulses palpable and equal, no bulges or nodes along
the eye (pinna aligned w/ outer canthus) bilateral inguinal areas.
• Symmetrical • LIVER 2-3 cm BELOW RIGHT COSTAL MARGIN
• Firm cartilage with recoil • KIDNEYS 1-2 cm above umbilicus
• Can hear once amniotic fluid has been absorbed (e.g. Startle • SPLEEN left quadrant
Reflex)
• Assess for low set ears (associated with chromosomal defects) Gastrointestinal:
o Note: if set lower-abnormal • Assess for abnormalities (hernia, gastroschisis, omphalocele,
- Chromosomal defects- Down syndrome/Kidney Ds. scaphoid – diaphragmatic hernia)
- Patau syndrome • Assess for abdominal distention associated with obstruction,
- Edward disease mass or sepsis.
- Kidney defects • Monitor bowel sounds – occur within 1-2 hours after birth.
- Craniofacial defects
OMPHALOCELE
Nose GASTROSCHISIS
• Patency of nasal canals / No discharge
• Structure – flat, broad and at the center Anus
• Obligatory nasal breather • Check for anal opening
• Occasional sneezing to remove obstructions • Should be patent and well placed
• No septal deviation • Check for Imperforate Anus
• Check for congenital anomaly (e.g Choanal Atresia) • Meconium should pass within 24 hours
• Monitor for flaring, Observe for RDS • Take note: Strict monitoring of I & O important and should be
well documented.
Mouth and Throat
• Pink moist gums IMPERFORATE ANUS
• Tongue moves freely, symmetrical
• Sucking and crying movements symmetrical Female Genitalia
• Able to swallow – do test feeding • Labia majora edematous, clitoris enlarged
• Should open mouth evenly when crying • Labia minora may have vernix caseosa and smegma.
• Check for oral thrush – not common • Labia majora normally covers the minora and clitoris
• Check for tongue tie - not common • hymenal tag maybe visible
• Palate – soft and hard palates intactTEMP • Vaginal discharge/pseudomenstruation (blood- tinged mucus)
• Epstein pearls – small white cyst may be present in hard palate maybe present.
• Frenulum and lingual frenulum • Smegma (thick white mucus discharge)
• Reflexes present: sucking, rooting, gag swallowing • Take note: In preterm babies’ appearance is different: clitoris
• Uvula – at midline and minora larger than majora
• Natal teeth/neonatal teeth – not common
Male Genitalia
Neck • Scrotum edematous, pendulous with rugae
• Short and thick neck • Testes should be present & descended into scrotum
• Head held at the midline o Assess for Crytorchidism
• Trachea on midline • Urinary meatus at tip of penis.
• Good range of motion (ROM) and is able to extend. o Assess for epispadia / hypospadia
• Freely movable • Foreskin (prepuce) covers the glans penis and should be
• Thyroid gland not palpable retracted
• Reflex present: Tonic – neck reflex (Fencer Position) • Check for phimosis
• Check for any abnormalities (hydrocele / hernia)
Chest • Take note: Preterm male – appearance different
• Appears circular since anteroposterior and lateral o Small penis, lack for rugae on scrotum
• Dm are equal – barrel shaped chest w/ bilateral chest expansion • For both male and female 1st voiding should occur within 24
• Respirations diaphragmatic hours of life.
• Bronchial sounds heard on auscultation (BS clear) • Check for ambiguous genitalia:
• Clavicles straight and intact a. Hermaprodite
• HR auscultated at border of left sternum extending mid of b. Klinefelter’s syndrome
clavicle; regular rate and rhythm.
• Observe for abnormalities (appearance, BS) CRYPTOORCHIDISM
• Chest AP and lateral diameters are equal HYPOSPADIAS
• Ribs flexible—observe for S/S of RDS HYDROCELE
• Breasts – nipples are prominent and often edematous
o Supernumerary nipples
o “Witch’s milk” – small amt of milk present in newborn Back (Spine)
• Spine
Abdomen o Sacral dimple
• Contour o Sacral tuft
• Umbilical cord o Pilonidal sinus/cyst
• Liver o Spina bifida (occulta)
• Spleen • Straight and flexible
• Kidneys • Posture well flexed.
• Femoral pulses • Movements well-coordinated
• Soft, dome shaped, round, some laxness of muscles, moves with • No opening observed or felt on vertebral column
respirations • Pilonidal cyst /sinus– a small dimple at the base
• Bowel sounds present - of the spine no connection w/ S. Cord
• Liver, spleen and kidneys palpable at birth • Check for neural tube defect (Spina Bifida) e.g. meningocele
• Umbilical cord present – white gelatinous with 2 arteries and 1 /myelomeningocele encephalocele
vein, no foul odor.
fcnlxa – St. Luke’s College of Nursing 4
SPINA BIFIDA inguinal, and buttocks
o Serves as skin lubricant, protection from
Extremities and trunk o Infection and acts as insulator
• Trunk – short, flexed and synchronized movements o Seen 2-3 days of life
• Trunk incurvature reflex (Galant Reflex) • LANUGO
o Fine downy hair
Extremities: (Upper) o Seen upper arm, shoulder, back, forehead and ears
• Flexed with good muscle tone o Disappear in 2 weeks
• Full ROM; movements symmetrical o Common characteristic of premature babies
• Fists clenched • MILIA
• Equal in length o White, pinpoint spots seen on the cheek and bridge of nose
• Grasp reflex present caused by immature sebaceous glands
• Five digits on each hand w/ palmar creases, nails present, o Disappears in 2-4 weeks as sebaceous glands mature and
separated and in correct formation drain
• Assess for polydactyly, syndactyly • ERYTHEMA TOXICUM
• Reflex present: Grasp Reflex, Moro Reflex o Pink papules with superimposed vesicles
• Check for fracture / Erb’s Palsy o Common at the face, back and buttocks
• Erb Duchenne Paralysis / Erb’s Palsy – newborn unable to move o Self-limiting
upper arm or asymmetric more response maybe caused by
damage in 5th & 6th cervical roots of the brachial plexus NEWBORN RASH/FLEABITE RASH (Erythema Toxicum) Desquamation
• Assess skin turgor over the abdomen to determine hydration
ERBS PALSY status
• Observe for forcep marks
Legs (lower extremities) • Observe also for birth marks:
• Equal in length, bowed, well flexed a. Telangiectatic nevi
• symmetric skin folds (major gluteal folds even) b. Nevus flammeus (port –wine stain)
• Creases on soles of feet c. Nevus vasculosus (strawberry mark)
• pulses present (radial, brachial, femoral) d. Mongolian spots
• Assess for fractures (e.g. Hip disclocation) • STRAWBERRY MARKS (Nevus vasculosus)
o Ortolani’s sign / Barlow’s Test (clicking sound heard) o Elevated areas formed by immature capillaries
• Slight tremors are common but could be sign of a sign of o and endothelial tissues
hypoglycemia or drug withdrawal o Capillary hemangioma, raised clearly
o delineated dark red with rough surface
HIP DISLOCATION/DYSPLASIA o Common in head part
ORTOLANI TEST o Disappears at 7-9 years old
ALLIS/GALEAZZI • TELANGIECTASIS NEVI
o Pale pink or red dilated capillaries on eyelids, nose, lower
Feet occipital bone and nape of the neck
• Creases on soles o Disappear at 2 years of age Telangiectatic nevi
• May have “positional club foot” caused by intrauterine position
but should be able to turn toward midline Portwine Stains (Nevus Flammeus)
• Reflexes present: plantar grasp, babinski • A macular purple or dark red lesion or patches
• EQUINOVARUS • Non elevated, sharply demarcated, red to purple, dense areas
o Club foot of capillaries
o Characterized by: • Can be seen face, buttocks, thigh and genitals
- Plantar flexion (toes pointing down) • Does not fade in time
- Inversion (toes pointing inward) • May require surgery (cosmetic) in the future
- Other types:
- Eversion (toes pointing outward) Mongolian spot
- Calcaneus (toes pointing upward) • Bluish, greenish black, gray patches
• Caused by accumulation of melanocytes
PHOCOMELIA • Seen at shoulder, upper arm, back and buttocks
• Disappears at in a year (white skinned)
Skin • Pre-school (dark skinned)
• Color should be consistent with ethnic background
• Pinkish red (light skinned newborn to pinkish brown or pinkish
yellow (dark skinned newborn) Clinical Assessment of Gestational Age:
• Important criterion because perinatal morbidity & mortality r/t
• Different Colors: gestational age & BW
a. acrocyanosis • Ballard Scoring Tool / (Dubowitz scale)
b. pallor o An assessment that evaluates 6 neuromuscular and 6
c. gray color physical characteristics during the 1st few hours of birth.
d. jaundice o A score of 1 to 5 is assigned to each characteristic
e. dark red color – common in preterm
f. cyanosis Ballard Scoring
• Vernix Caseosa • Neuromuscular maturity
• Lanugo o During the 1st 24 hrs the Nervous system is unstable
• Milia o Reflexes and assessments dependent on his or her brain
• Desquamation centers.
• Mottling o Maybe unreliable and need to be repeated in 24 hours
• Cutis marmorata o Components: Posture, Square window, Arm recoil, popliteal
• Erythema toxicum angle, scarf sign, heel to ear extension
• Harlequin Sign
• VERNIX CASEOSA Physical Maturity
o White cheesy substance seen in areas like back, armpit,
fcnlxa – St. Luke’s College of Nursing 5
• Not influenced by labor and birth and do not change
significantly within the 1st 24 hours after birth. 3. Skin to skin contact
• Components: Skin, Lanugo, Plantar surface, Breast, Eye/ear, After 40 mins take newborns temp again
male genitalia/ female genitalia
3. Bathing postponed
• Preterm = below 37 weeks Do not weight it must be performed 2 hrs after birth
• Term = 37-42 weeks Bathe 24 hrs after birth
• Post = above 42 weeks
4. Breastfeeding
Start within first hour of birth
TERM (37- 40 weeks) Do not force baby to latch
• SKIN: Smooth, pink, superficial, cracking, Less visible veins
• EARS: Formed and firm with instant recoil 5. Appropriate clothing
• BREAST NODULE: 3-5 mm Do not use tight and swaddling clothing
• GENITALS: Inform the mother to bring baby’s clothes before birth
o MALE: Partially descended, more swollen and rugae They should be warmed
o FEMALE: Partially covered by majora
• SOLE CREASE: 2/3 of the sole w/ creases 6. Mother and baby together
• LANUGO: Less Move the newborn while the mother is carrying it, skin to skin contact
Pre-term 7. Warm resuscitation
• PREMATURE (36 weeks & below)
• SKIN: Gelatinous, transparent, with visible BV 8. Training of health care professionals
• EAR CARTILAGE: Absent / Pliable
• BREAST NODULE: 1-2 mm
• GENITALS: Cord clamping
o MALE: TESTES- undescended AVA
- SCROTUM- Less swollen, few rugae KMC – Kangaroo Mother Care (used to prevent newborn from
o FEMALE: Clitoris and minor - PROMINENT persistent hypothermia
• SOLE CREASES: Anterior transverse
• LANUGO: abundant 1 inch above abdomen, then cut above cord clamp
• SCALP HAIR: Fine & Fussy
POST TERM (42 weeks & above)
• SKIN: Parchment, deep cracking, desquamates, no visible Blood
vessels
• EARS: thick cartilage and stiff
• BREAST NODULE: 6 TO 10 mm
• GENITALS:
o MALE: Fully descended, pendulous, marked swollen;
Extensive Rugae
o FEMALE: Majora completely covers minora and clitoris
• SOLE CREASE: ENTIRE SOLE
• LANUGO: None
Weight Related to Gestational Age
• Birth weight is poor indicator of gestational and fetal maturity
• Gestational age reflects fetal maturity
• AGA—growth between 10th and 90th percentile
• SGA—<10th percentile
• LGA—>90th percentile
NOTES:
Respiratory disorders
Convulsions
High glucose
The warm chain- prevents newborn hypothermia
Skipping one step breaks the chain, and increases the newborn’s
36.5 – 37.5 normal
36.5 below – hypothermia
1. Warm delivery room
Room should be warm, no air from open window, air or fan
Room should not be below 25 C
2. Immediate drying
Warm, dry towel
Socks, bonnet, warm blanket
23 C in infants = 0 C in adults
fcnlxa – St. Luke’s College of Nursing 6
You might also like
- BPT (Bachelor of Physiotherapy)Document8 pagesBPT (Bachelor of Physiotherapy)mmumullana0098No ratings yet
- Clinical Log Term II PDFDocument9 pagesClinical Log Term II PDFPriscilla S100% (1)
- Medical Terminology Systems A Body Systems Approach 8th Edition Gylys Test BankDocument25 pagesMedical Terminology Systems A Body Systems Approach 8th Edition Gylys Test Bankjasoncordovarojpamkcqe100% (31)
- ATI CompDocument9 pagesATI CompTee Wood100% (1)
- Blood Pressure SolutionDocument68 pagesBlood Pressure Solutionmgrfan100% (14)
- PB 20Document10 pagesPB 20Cheng CapunoNo ratings yet
- ATI Maternal Newborn Proctored Exam 2020Document4 pagesATI Maternal Newborn Proctored Exam 2020svetlanaNo ratings yet
- Fatime Sanogo Vsim Steps - HTMLDocument6 pagesFatime Sanogo Vsim Steps - HTMLJhunnieEy ReyesNo ratings yet
- First Semester Study Kits - The Nurse SamDocument5 pagesFirst Semester Study Kits - The Nurse SamRrgNo ratings yet
- Hesi Management of A Emergent Care UnitDocument5 pagesHesi Management of A Emergent Care UnitAna Bienne0% (1)
- Rounding Rules11!3!11Document1 pageRounding Rules11!3!11Sheldon SloanNo ratings yet
- ISBAR Worksheet Olivia Jones Jasgou1752Document1 pageISBAR Worksheet Olivia Jones Jasgou1752Jasmyn Rose100% (1)
- Thinking Like A NurseDocument3 pagesThinking Like A Nurseapi-519359726No ratings yet
- NCLEX 2007 BulletinDocument44 pagesNCLEX 2007 Bulletinij22comNo ratings yet
- VATI Mental Health RemediationDocument2 pagesVATI Mental Health RemediationestberryNo ratings yet
- Exam 3 Review Med SurgDocument18 pagesExam 3 Review Med SurgCarol ReidNo ratings yet
- ATI Nursing ModulesDocument9 pagesATI Nursing ModulestgushikaNo ratings yet
- Hyperemesis Gravidarum: Bleeding Complications of PregnancyDocument6 pagesHyperemesis Gravidarum: Bleeding Complications of PregnancykirbsNo ratings yet
- NCLEXDocument11 pagesNCLEXPrince Charles AbalosNo ratings yet
- Answer: CDocument34 pagesAnswer: CLola OladapoNo ratings yet
- Ati Med-Surg Proctored Exam 2019 84 Questions and Answers With NGN Verified and Correct Explanations Graded A+Document41 pagesAti Med-Surg Proctored Exam 2019 84 Questions and Answers With NGN Verified and Correct Explanations Graded A+odhiambomanuel9No ratings yet
- Funds 2017A Answers QuizletDocument8 pagesFunds 2017A Answers QuizletHeather MoralesNo ratings yet
- Medical Surgical ATI Proctored Exam 2019 With Rationale Detailed AnswerDocument62 pagesMedical Surgical ATI Proctored Exam 2019 With Rationale Detailed Answerkinyuaboris990No ratings yet
- Hesi Management of A Medical UnitDocument2 pagesHesi Management of A Medical UnitAna Bienne100% (1)
- NCLEX Updates June 2010Document21 pagesNCLEX Updates June 2010erika_datu100% (1)
- Nursing BulletsDocument72 pagesNursing BulletsJoanna Mae Carolino100% (1)
- Quizlet (2) RRRRRDocument7 pagesQuizlet (2) RRRRRGina GiammalvoNo ratings yet
- Individual Performance Profile PN Nursing Care of Children 2011 Form BDocument4 pagesIndividual Performance Profile PN Nursing Care of Children 2011 Form BStan Tan67% (3)
- Asthma That Disappears Between Ages 6-8 - Bronchioles Grew & Resolved The AsthmaDocument27 pagesAsthma That Disappears Between Ages 6-8 - Bronchioles Grew & Resolved The Asthmasimonedarling100% (1)
- Basic Care and ComfortDocument35 pagesBasic Care and ComfortRebecca TapiaNo ratings yet
- Medsurge RationaleDocument8 pagesMedsurge RationaleRose Anne AbivaNo ratings yet
- Dysrhythmias: Se Admin Anticoagulante, Cardioversion As PrescribedDocument10 pagesDysrhythmias: Se Admin Anticoagulante, Cardioversion As Prescribedyaneidys perezNo ratings yet
- NURS 460 Nursing Licensure Examination Course: Jv7@hawaii - EduDocument5 pagesNURS 460 Nursing Licensure Examination Course: Jv7@hawaii - EduJeffrey ViernesNo ratings yet
- U World ReproductiveDocument5 pagesU World ReproductiveAce LabosNo ratings yet
- Jennifer Portillo Health Assessment VocabularyDocument9 pagesJennifer Portillo Health Assessment VocabularyJennifer PortilloNo ratings yet
- Fundamentals Quizzing TIPSDocument41 pagesFundamentals Quizzing TIPSmelissamichellleNo ratings yet
- Which Signs and Symptoms Would The Nurse Expect To Assess in A Newborn WithDocument1 pageWhich Signs and Symptoms Would The Nurse Expect To Assess in A Newborn WithjamesNo ratings yet
- Ati RN Comprehensive Predictor Exit Exam 2023Document30 pagesAti RN Comprehensive Predictor Exit Exam 2023ochienglavis100% (1)
- Amelia Sung MAternity VSIM Guided ReflectionDocument2 pagesAmelia Sung MAternity VSIM Guided Reflectionmeisha thompsonNo ratings yet
- GuideDocument5 pagesGuideHu Tao100% (1)
- ATI Comprehensive PredictorDocument34 pagesATI Comprehensive Predictorsimo.ouko100% (1)
- ATI Community Health Proctored Exam 2020Document7 pagesATI Community Health Proctored Exam 20204 u0% (1)
- AdultDocument295 pagesAdultKen WonNo ratings yet
- Medical Surgical Nursing - DiabetesDocument4 pagesMedical Surgical Nursing - Diabetestripj33100% (2)
- Med Surg MidtermDocument17 pagesMed Surg Midtermjhan grabierNo ratings yet
- Fall 2023, 1R8 - Maternal Newborn Study Guide (Comprehensive)Document16 pagesFall 2023, 1R8 - Maternal Newborn Study Guide (Comprehensive)Tia Liveandlearn0% (1)
- Task Delegations For NclexDocument3 pagesTask Delegations For Nclexjenn_028No ratings yet
- ATI Comprehensive: Study Online atDocument6 pagesATI Comprehensive: Study Online atVanessaMUeller100% (1)
- Open Pediatric ArcherDocument84 pagesOpen Pediatric Archerbaharada1979No ratings yet
- HESI Women's Health:Newborn DrugsDocument8 pagesHESI Women's Health:Newborn Drugsisapatrick8126No ratings yet
- Reviewer C AnswersDocument39 pagesReviewer C AnswersDavis WhiteNo ratings yet
- Hesi Med Surg Study GuideDocument1 pageHesi Med Surg Study GuideGeorgeNo ratings yet
- Kaplan Focus ReviewDocument9 pagesKaplan Focus ReviewSaidel ElizondoNo ratings yet
- Select All That ApplyDocument10 pagesSelect All That ApplyJohnasse Sebastian NavalNo ratings yet
- Final Peds Concept MapDocument9 pagesFinal Peds Concept Mapapi-495456666No ratings yet
- Calc Drip Rates 2Document2 pagesCalc Drip Rates 2Charisse Nicole DiazNo ratings yet
- Immunity 1Document6 pagesImmunity 1Tori RolandNo ratings yet
- Ch. 1, Lesson 1: What Is The Next Gen NCLEXDocument4 pagesCh. 1, Lesson 1: What Is The Next Gen NCLEXChantel100% (1)
- 52 Nclex ReviewDocument1 page52 Nclex ReviewedobleNo ratings yet
- Nursing BulletsDocument83 pagesNursing BulletsgilissaNo ratings yet
- NCLEX Pregnancy NotesDocument3 pagesNCLEX Pregnancy NotesrustiejadeNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- The Newborn Care: Fcnlxa - St. Luke's College of NursingDocument11 pagesThe Newborn Care: Fcnlxa - St. Luke's College of NursingFrancine LaxaNo ratings yet
- Viruses and Prions: Fcnlxa - St. Luke's College of NursingDocument4 pagesViruses and Prions: Fcnlxa - St. Luke's College of NursingFrancine LaxaNo ratings yet
- Adjustment To Extrauterine LifeDocument4 pagesAdjustment To Extrauterine LifeFrancine LaxaNo ratings yet
- The Newborn Care: Fcnlxa - St. Luke's College of NursingDocument10 pagesThe Newborn Care: Fcnlxa - St. Luke's College of NursingFrancine LaxaNo ratings yet
- Community ProfilingDocument40 pagesCommunity ProfilingFrancine LaxaNo ratings yet
- AnswerDocument4 pagesAnswerRachel DominguezNo ratings yet
- 114 Final Brain Dump Part 2Document8 pages114 Final Brain Dump Part 2kelsey jacksonNo ratings yet
- Cardiology MCQDocument2 pagesCardiology MCQmohamed mowafeyNo ratings yet
- PathophysiologyDocument34 pagesPathophysiologyeunams_1195% (20)
- Echocardiography Juni 2018Document1 pageEchocardiography Juni 2018Prima Agung LNo ratings yet
- Acute Ischemic Heart DiseaseDocument27 pagesAcute Ischemic Heart DiseaseJaymee CachoNo ratings yet
- Guía de Usuario HOME 2020 - CompressedDocument45 pagesGuía de Usuario HOME 2020 - CompressedHelder GamaNo ratings yet
- Exploring Anatomy Circulatory System WorksheetDocument4 pagesExploring Anatomy Circulatory System WorksheetBrian MartinezNo ratings yet
- Systolic Heart FailureDocument66 pagesSystolic Heart FailureFerinaTarizaIINo ratings yet
- Nursing Care of Patients With HypertensionDocument13 pagesNursing Care of Patients With HypertensionDon Chiaw Manongdo100% (1)
- Slide JR UGD SaktaDocument39 pagesSlide JR UGD SaktaWayan GunawanNo ratings yet
- CPCRDocument36 pagesCPCRapi-19916399100% (1)
- DR Tejas Patel cv-1 PDFDocument18 pagesDR Tejas Patel cv-1 PDFnarasimhahanNo ratings yet
- ELSO Guideline Elso .1 PediatricDocument5 pagesELSO Guideline Elso .1 Pediatricyowewe7363No ratings yet
- Buret TerbaruDocument33 pagesBuret TerbaruEka Rahayu UtamiNo ratings yet
- NURSING-CARE-PLAN With AnswersDocument4 pagesNURSING-CARE-PLAN With AnswersTracy Malingin QuimqueNo ratings yet
- The Blood Pressure Solution Ebook 022318Document14 pagesThe Blood Pressure Solution Ebook 022318Rolando M Tabora100% (3)
- Textbook of MedicineDocument198 pagesTextbook of MedicineSoumyadip pradhanNo ratings yet
- Cot 1 Vital SignsDocument22 pagesCot 1 Vital Signscristine g. magatNo ratings yet
- ECG LictureDocument25 pagesECG LictureALi NursingNo ratings yet
- ReferralDocument1 pageReferralmanasabhavaniNo ratings yet
- ST IN Grade 9 ScienceDocument4 pagesST IN Grade 9 ScienceFatima Ybanez Mahilum-Limbaga0% (1)
- Worksheet Ap06Document7 pagesWorksheet Ap06liawijayaNo ratings yet
- Booklet 11º 2024 Unit 1Document28 pagesBooklet 11º 2024 Unit 1YELLOW BEENo ratings yet
- Myocardial Diseases: Marvi G. Dulnuan - Niog, MD, FPSPDocument94 pagesMyocardial Diseases: Marvi G. Dulnuan - Niog, MD, FPSPLianne LagayanNo ratings yet
- Course in The WardDocument7 pagesCourse in The WardlouielouielouieNo ratings yet
- Antitrombotik, PPT 7Document66 pagesAntitrombotik, PPT 7Rizky Saraswati IndraputriNo ratings yet
- Case Study Bago Neonatal Sepsis PikeDocument30 pagesCase Study Bago Neonatal Sepsis PikeAlex VarelaNo ratings yet