Professional Documents
Culture Documents
IndianJPsychiatry632146-3947242 105752
IndianJPsychiatry632146-3947242 105752
Uploaded by
gion.nandOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IndianJPsychiatry632146-3947242 105752
IndianJPsychiatry632146-3947242 105752
Uploaded by
gion.nandCopyright:
Available Formats
[Downloaded free from http://www.indianjpsychiatry.org on Saturday, April 17, 2021, IP: 117.251.52.
169]
ORIGINAL ARTICLE
A comparative diffusion tensor imaging study of patients with and without
treatment‑resistant schizophrenia
Anisha Aggarwal, Sandeep Grover, Chirag Ahuja1, Subho Chakrabarti, Niranjan Khandelwal1, Ajit Avasthi
Department of Psychiatry and 1Radiodiagnosis and Neuroimaging, Postgraduate Institute of Medical Education and Research,
Chandigarh, India
ABSTRACT
Aim: The aim was to study the brain connectivity using diffusion tensor imaging (DTI) among patients with
treatment‑resistant schizophrenia (TRS) and compare the same with a group of patients without TRS.
Methods: Twenty‑three patients with TRS and 15 patients without TRS underwent DTI using a 3T magnetic resonance
imaging machine. DTI data were processed with the calculation of fractional anisotropy (FA) and apparent diffusion
coefficient. Patients were also assessed on Brief Psychiatric Rating Scale, Positive and Negative Symptom Scale, Global
Assessment of Functioning Scale, and Clinical Global Impression severity scale.
Results: Patients with TRS and non‑TRS differed significantly in the FA values in the region of right superior longitudinal
fasciculus and right uncinate fasciculus, with more integrity of tracts in the non‑TRS group. However, these differences
disappeared when Bonferroni correction was used for multiple comparisons.
Conclusion: The present study suggests lack of significant difference in DTI findings between patients with TRS and
non‑TRS.
Key words: Diffusion tensor imaging, schizophrenia, treatment resistance
INTRODUCTION respond to adequate treatment and are known to be suffering
from treatment‑resistant schizophrenia (TRS).[2] Patients with
Schizophrenia is arguably the most puzzling of psychiatric TRS are found to be highly symptomatic, require extensive
syndromes and one of the most debilitating psychiatric periods of hospitalization, and are responsible for the high
disorders. Despite the numerous studies aimed at share of total cost toward treating schizophrenia.[3,4]
understanding the disorder, its pathophysiology is largely
unknown, with available treatments showing only partial As one‑third of patients do not respond or show minimal
efficacy in treating this disorder.[1] Available data suggest response to available treatments, clinicians and investigators
that about one‑third of patients with schizophrenia do not have attempted to predict nonresponse to treatment as
early as possible, with an aim to possibly start clozapine
Address for correspondence: Dr. Sandeep Grover, before the treatment resistance evolves. One of the ways
Department of Psychiatry, Postgraduate Institute via which this prediction has been made in literature is
Medical Science, Rohtak ‑ 124 001, Haryana, India.
E‑mail: drsandeepg2002@yahoo.com
This is an open access journal, and articles are distributed under the terms of
Submitted: 23‑Feb‑2020, Revised: 14‑Jun‑2020, the Creative Commons Attribution‑NonCommercial‑ShareAlike 4.0 License,
Accepted: 17‑Sep‑2020, Published: 14-Apr-2021 which allows others to remix, tweak, and build upon the work non‑commercially,
as long as appropriate credit is given and the new creations are licensed under
the identical terms.
Access this article online
Quick Response Code For reprints contact: WKHLRPMedknow_reprints@wolterskluwer.com
Website:
www.indianjpsychiatry.org
How to cite this article: Aggarwal A, Grover S, Ahuja C,
Chakrabarti S, Khandelwal N, Avasthi A. A comparative
DOI:
diffusion tensor imaging study of patients with and without
treatment-resistant schizophrenia. Indian J Psychiatry
10.4103/psychiatry.IndianJPsychiatry_147_20
2021;63:146-51.
146 © 2021 Indian Journal of Psychiatry | Published by Wolters Kluwer - Medknow
[Downloaded free from http://www.indianjpsychiatry.org on Saturday, April 17, 2021, IP: 117.251.52.169]
Aggarwal, et al.: DTI study of patients with and without TRS
through neuroimaging, which highlights the structural among patients with and without TRS. It was hypothesized
or functional changes in brain, possibly contributing to that individuals with TRS would not differ significantly in
etiopathogenesis of treatment resistance in schizophrenia. terms of brain circuitry involving the white matter compared
Most of the available studies have focused on patients with to patients with non‑TRS.
chronic schizophrenia using techniques such as computed
tomography (CT), magnetic resonance imaging (MRI), or METHODS
functional MRI, with meager data on studying cases of TRS
using diffusion tensor imaging (DTI).[4,5] Among the various This study was carried out in a tertiary care teaching
neuroimaging techniques, DTI can be considered as more hospital in North India. The ethics committee of the
useful than CT and MRI in schizophrenia as it provides institute approved the study, and all the study participants
direct information about the white‑matter neuroanatomical were recruited after obtaining written informed consent.
connectivity between different areas of the brain. These
neuroanatomical connections could, therefore, be directly The study followed a cross‑sectional design, in which all
studied to understand the etiopathogenesis of schizophrenia the patients were assessed only once. The study sample
and the etiopathogenesis of treatment resistance as well. comprised of two groups, that is, Group I comprised of
A recent systematic review evaluated the neuroimaging 23 patients with TRS, whereas Group II comprised of
findings of patients refractory to treatment and compared 15 patients who did not fulfill the criteria of TRS (non‑TRS
the available data with healthy controls and those Group). Both the study groups were matched for age,
responding to treatment.[4] In contrast to healthy controls, gender, and total duration of illness. For this study, TRS
patients with TRS showed gray‑matter reductions, which is was defined on the basis of: (i) insufficient response to two
consistent with findings seen in schizophrenia in general. clinical trials of two different antipsychotics for at least
When patients with treatment resistance/refractoriness 6 weeks’ duration and no period of good functioning in
were compared with those responding to treatment, the the previous 2 years as determined by Global Assessment
finding, which was most, replicated included a greater for Functional Scale (GAF)[7] score of <59, score of ≥4 on
reduction in gray matter in resistant patients, predominantly 2 of the 4 Brief Psychiatric Rating Scale (BPRS)[8] items of
in the frontal areas. However, none of the studies included conceptual disorganization, suspiciousness, hallucinatory
in the review, compared patients with treatment resistance behavior, and unusual thought content, total BPRS‑18
with treatment responders or healthy controls, was based score ≥45, and Clinical Global Impression (CGI)[9] score
on DTI.[4] Another systematic review published in 2015, of ≥4 at the time of assessment. To be included in the study,
also dealt with neuroimaging findings in patients with the participants were required to be aged 18–65 years and
TRS.[5] CT‑based studies showed prefrontal atrophy in fulfill the diagnosis of schizophrenia as per the Diagnostic
patients with TRS.[5] MRI studies showed that compared to and Statistical Manual, fourth revision (DSM‑IV) criteria, as
healthy controls, patients with TRS have more widespread confirmed by using the Mini International Neuropsychiatric
reduction in cortical thickness in all the lobes of brain than Interview (MINI).[10] Additionally, to be considered for
patients with non‑TRS, who had reduced cortical thickness the non‑TRS group, participants were required to have
only in frontal area of the brain.[5] As per this review, only one a period of good functioning in the previous 2 years and
study was based on DTI, which compared patients with TRS total BPRS‑18 item scale score ≤35, CGI score of ≤3,
and healthy controls. This study showed that compared to score of <4 on 2 of the 4 BPRS items of conceptual
healthy controls, patients with TRS showed lower fractional disorganization, suspiciousness, hallucinatory behavior,
anisotropy (FA) in multiple white‑matter bundles. The areas and unusual thought content. Patients with the presence
involved included the genu, body, and splenium of the of organic brain syndrome, intellectual disability, comorbid
corpus callosum; inferior longitudinal fasciculus; superior drug dependence (other than tobacco dependence), history
longitudinal fasciculus (SLF); external capsule; uncinate of any brain disorder (e.g., head injury, stroke, epilepsy, and
fasciculus (UF); posterior limb of the internal capsule; the Parkinson’s disease), history of any illness which can cause
left anterior limb of internal capsule; fornix; cerebellar white‑matter damage (e.g., multiple sclerosis), comorbid
peduncles; and the corticospinal tract at the level of the severe medical conditions which could influence the
brainstem. There was no voxel of increased FA in patients neuroimaging findings (e.g., poorly controlled diabetes or
compared with controls.[5] A recently published study based symptomatic coronary artery disease), and those receiving
on 1.5 T, voxel‑based statistical analysis using the tract‑based clozapine for more than 1 week just prior to assessment or
spatial statistics (TBSSv1.2) approach compared patients have received clozapine in the past were excluded from the
with treatment refractory schizophrenia and nonrefractory study. Similarly, patients with contraindication for MRI (i.e.,
schizophrenia. This study showed no differences in FA of those with pacemakers, aneurysm clip, cochlear implants,
white‑matter integrity between the two groups.[6] claustrophobia) were also excluded from the study. All the
patients were assessed on CGI Severity scale, BPRS, Positive
Considering the limited DTI data for patients with TRS, this and Negative Symptom Scale (PANSS),[11] and GAF scale. In
study aimed to compare the brain connectivity using DTI addition, using a semi‑structured interview, all the patients
Indian Journal of Psychiatry Volume 63, Issue 2, March-April 2021 147
[Downloaded free from http://www.indianjpsychiatry.org on Saturday, April 17, 2021, IP: 117.251.52.169]
Aggarwal, et al.: DTI study of patients with and without TRS
were evaluated for the presence or absence of auditory had significantly longer duration of untreated psychosis,
hallucinations in their lifetime. had significantly higher BPRS and PANSS total scores, had
higher scores in all the domains of BPRS and PANSS, had
Premorbid personality prior to onset of illness was assessed significantly higher CGI severity score, had significantly higher
by a semi‑structured interview conducted with the patient impairment in the level of functioning as assessed by GAF,
and family members and a review of treatment records. and had received significantly higher number of adequate
Presence of personality disorder was defined as per the antipsychotic trials [Table 1]. Most of the patients in the TRS
ICD‑10 criteria. group had continuous symptoms in the last 5 years.
DTI data were acquired using 3T MRI machine (60 slices; Only two patients (one borderline and one anxious avoidant
TE = 100 ms; TR = 15000 ms; 30 directions; voxel size: personality disorder) in the TRS group had evidence to
2.4 × 2.4 × 2.4; time of accuracy: 8.32 min; and slice suggest the presence of personality disorder prior to the
thickness = 2.4 mm). The DTI images were processed and onset of the schizophrenia, whereas only one patient had
analyzed on the Siemens work station (software Numaris, personality disorder (schizoid personality disorder) in the
version syngo MR B17). Motion and Eddy current‑induced non‑TRS group. Overall, majority of the patients in both the
geometric distortions were corrected automatically. groups had no diagnosable personality disorder prior to
onset of schizophrenia. In the TRS group, 30.4% (n = 7) of
DTI data were processed by a qualified neuroradiologist, the patients had lifetime diagnosis of tobacco dependence,
and the following steps were followed: (i) correction for of which 21.7% were still using tobacco in the dependence
motion and Eddy current‑induced geometric distortions pattern at the time of assessment for the study. About
with rotation of the b‑matrix to preserve the orientation one‑fifth (21.7%; n = 5) of the patients in the TRS group
information was ensured, (ii) diffusion tensor using a robust had lifetime diagnosis of alcohol dependence, of which 8.7%
nonlinear regression method was estimated, and (iii) FA fulfilled the diagnosis of alcohol dependence in the last
and apparent diffusion coefficient (ADC) were calculated. 2 years too. However, no patient was using alcohol in the
Subsequently, using the region of interest (ROI) approach, dependent pattern at the time of assessment for the study.
data were analyzed. When patients with and without TRS were compared, no
significant difference was seen in terms of substance use
The tensor data were loaded on the Neuro 3D platform pattern in the lifetime, last 5 years, and last 2 years.
to derive the FA and ADC maps. The FA/ADC maps were
subsequently fused with the 3D T1 MPRAGE high‑resolution Diffusion tensor imaging findings
images for better depiction and confirmation of the As is evident from Table 2, in terms of FA values, significant
white‑matter tracts. The tracts were identified as per the difference between the two groups was noted only in the
different cut sections, that is, sagittal, axial, or coronal right superior longitudinal fasciculus (SLF) and right uncinate
depending on the best visibility of the tract. Thereafter,
ROI‑based analysis was performed on the desired tracts. Up
to five ROIs were chosen to enclose tracts’ cross‑sections, and
a mean of the ROIs was calculated to improve the specificity
of the data. The radius of each ROI varied between 2 mm
and 10 mm, depending on the thickness of the white‑matter
bundle. Following this, a set of 22 values each depicting the
FA values and ADC values were obtained for further analysis.
Data were analyzed by using SPSS Inc. Released 2007.
SPSS for Windows, Version 16.0. (Chicago, SPSS Inc.). The
mean and standard deviation with range were calculated
for continuous variables and frequency and percentages
were calculated for categorical variables. Comparisons
were done by using Student’s t‑test, Mann–Whitney test,
and Chi‑square test. Bonferroni correction was applied to
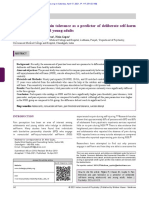
address multiple comparisons, and P = 0.002 (0.05/22) was Figure 1: The tract superior longitudinal fasciculus (yellow
arrowhead), an association fiber tract well represented in
considered statistically significant.
the color green. Uncinate fibers (blue arrow) are forming a
loop and turning around the lateral sulcus; in turn connecting
RESULTS inferior frontal and temporal lobes. The ellipsoids depict
anisotropy in both the tracts, with higher fractional anisotropy
The demographic profile of the study sample is shown in in the right superior longitudinal fasciculus and right uncinate
Table 1. Compared to non‑TRS group, patients with TRS fasciculus in the control group
148 Indian Journal of Psychiatry Volume 63, Issue 2, March-April 2021
[Downloaded free from http://www.indianjpsychiatry.org on Saturday, April 17, 2021, IP: 117.251.52.169]
Aggarwal, et al.: DTI study of patients with and without TRS
Table 1: Comparison of demographic and clinical variables of treatment‑resistant schizophrenia and
nontreatment‑resistant schizophrenia group
Parameters TRS group I (n=23) Non‑TRS group II (n=15) T‑test/χ2 (P)
Age in years 35.26 (10.85) 33.47 (8.74) t=0.54 (0.59)
Sex, male (%) 11 (47.8) 6 (40) χ2=0.22 (0.63)
Education in years, mean (SD); range 11.65 (4.02) 11.87 (2.90) t=−0.18 (0.86)
Marital status ‑ currently single (%) 13 (56.5) 5 (33.3) χ2=1.96 (0.17)
Occupation ‑ on paid employment (%) 3 (13) 3 (20) F.E=0.44
Type of schizophrenia ‑ paranoid (%) 19 (82.6) 11 (73.3) FE=0.38
Age of onset (in years) 24.65 (8.81) 22.67 (6.31) t=0.75 (0.46)
Duration of untreated psychosis (in days) 1262.35 (1682.43) 234.60 (396.8) U=97.5 (0.02)*
Total duration of illness (in years) 11.17 (8.12) 11.93 (5.92) t=−0.31 (0.76)
Comorbid physical illness ‑ presenta 5 (21.74%) 4 (26.67%) χ2b=0.0 (1)
Comorbid psychiatric illnessb 9 (39.13%) 2 (13.3%) χ2b=1.82 (0.18)
PANSS
Positive subscale score 27.13 (7.21) 7.27 (0.59) t=10.59 (<0.001)***
Negative subscale score 28.22 (11.83) 10.8 (2.57) t=5.59 (<0.001)***
General Psychopathology subscale score 49.70 (10.88) 21.07 (2.60) t=9.96 (<0.001)***
Total PANSS Score 105.04 (23.07) 39.13 (4.60) t=10.87 (<0.001)***
Insight score as assessed from PANSS (G12) 5.56 (1.37) 2.27 (1.10) t=6.69 (<0.001)***
Depression as per PANSS‑D 12.43 (5.95) 6 (1.51) t=4.08 (<0.001) ***
Depression as per PANSS‑D ‑ present (%) 19 (82.60) 5 (33.33) χ2=9.47 (0.002)**
BPRSc
Depression/anxiety/affect 9.70 (5.90) 4.2 (0.56) t=3.58 (0.001)***
Psychosis/thinking disorder 18.04 (3.76) 5.67 (0.90) t=12.46 (<0.001)***
Negative symptoms/withdrawal/retardation 9.17 (6.03) 3.6 (1.40) t=3.50 (0.001)***
Activation 6.65 (3.01) 3.87 (0.83) t=3.48 (<0.001)***
Resistance 10 (3.27) 3.27 (0.46) t=5.84 (<0.001)***
Total BPRS score 53.56 (10.68) 20.6 (2.03) t=11.76 (<0.001)***
GAF
GAF score 21 (11.27) 79.73 (7.36) t=−17.81 (<0.001)***
CGI
CGI severity 5.48 (0.59) 1.13 (0.35) t=25.52 (<0.001)***
Number of adequate trials received 3.78 (1.594) 1.73 (0.59) t=4.75 (<0.001)***
Course of illness in the last 5 years
Continuous illness with no improvement in symptoms (%) 14 (60.87) 0 χ2=14.46 (<0.001***)
Continuous illness with no or minimal symptoms 0 1 (6.7%) FE=0.39
Episodic illness in lifetime with no improvement in symptoms in last 5 years (%) 9 (39.13) 0 χ2b=0.02*
*P≤0.05; **P≤0.01; ***P≤0.001. AComorbid physical illnesses in TRS: diabetes mellitus (n=2), asthma (n=1), anemia (n=1), Acomorbid physical illnesses in
non‑TRS: diabetes mellitus (n=2), hypothyroidism (n=1), hypertension (n=1), Marfan syndrome (n=1); Bcomorbid psychiatric illnesses in TRS: moderate depressive
episode (n=4), tobacco dependence, currently using (n=6); Bcomorbid psychiatric Illnesses in non‑TRS: Moderate depressive episode (n=1), Tobacco dependence,
currently using (n=1); cItems of Brief Psychiatric Rating Scale were categorized into various domains as per.[12] χ2 – Chi‑square value; χ2b – Chi‑square value
with Yate’s correction; U – Mann-Whitney value; t – T test; SD – standard deviation; FE – Fisher’s exact value; PANSS – Positive and Negative Syndrome Scale,
BPRS – Brief Psychiatric Rating Scale; GAF – Global Assessment of Functioning; CGI – Clinical Global Impression; TRS – Treatment‑resistant schizophrenia
fasciculus (UF), with higher FA values for the right SLF and response to treatment. The other hypothesis, which can be
right UF for the non‑TRS group [Figures 1 and 2]. However, considered, is the categorical hypothesis, which suggests
when duration of untreated psychosis was used as a covariate, that patients with TRS have a fundamentally different
only significant difference persisted for right UF. Lack of pathophysiology compared to those showing response
significant difference persisted even after using duration of to treatment, and thus current treatments are ineffective
untreated psychosis as a covariate. However, when we used as they target the wrong processes.[12] The present study
the Bonferroni correction, no significant difference was seen. attempted to understand the etiopathogenesis of TRS on
In terms of ADC values, no significant difference emerged the basis of these hypotheses.
between both the groups on any of the tracts [Table 2].
In the present study, in terms of FA values, when the
DISCUSSION comparison was done without statistical correction,
significant difference between the two groups was noted
Two main schools of thought exist regarding the neurobiology only in the right SLF and right UF, with higher FA values
of TRS. One, which can be characterized as the continuum for the non‑TRS group. However, this disappeared when
hypothesis, posits that the same pathophysiological the Bonferroni correction was applied. In terms of ADC
processes underlie symptoms in both treatment‑responsive findings of white‑matter tracts, no significant difference
and ‑resistant patients, but that these processes occur to a emerged between the two groups on any of the tracts.
greater degree in patients with TRS, which leads to poor There is only one study in the existing literature, which has
Indian Journal of Psychiatry Volume 63, Issue 2, March-April 2021 149
150
Table 2: Comparison of fractional anisotropy and apparent diffusion coefficient (×10‑6mm2/s) findings of white matter tracts of treatment‑resistant
schizophrenia group and nontreatment‑resistant schizophrenia group
Variables TRS group Non‑TRS T‑test/χ2 (P) Covariate TRS group I Non‑TRS group T‑test/χ2 (P) Covariate
I (n=23) group II (n=15) analysisa F (P) (n=23) II (n=15) analysisa F (P)
Fractional anisotropy Apparent diffusion coefficient
Anterior commissure 0.22 (0.10) 0.20 (0.15) t=0.51 (0.610) F=0.058 (0.811) 2078.39 (857.1) 1792.22 (689.65) t=1.08 (0.29) F=0.635 (0.431)
Genu 0.70 (0.21) 0.76 (0.21) t=−0.92 (0.365) F=0.819 (0.372) 1204.53 (1662.14) 734.05 (98.27) t=1.1 (0.28) F=1.494 (0.23)
Splenium 0.87 (0.07) 0.77 (0.26) t=1.6 (0.12) F=2.897 (0.098) 662.29 (106.66) 822.44 (463.64) t=−1.6 (0.12) F=2.852 (0.100)
Corpus callosum 0.70 (0.18) 0.66 (0.20) t=0.67 (0.51) F=0.489 (0.489) 873.52 (358.95) 826.11 (188.22) t=0.47 (0.64) F=0.970 (0.331)
Left anterior limb of internal capsule 0.53 (0.20) 0.48 (0.16) t=0.80 (0.43) F=0.342 (0.563) 653.03 (139.57) 724.97 (98.10) t=−1.73 (0.09) F=4.767 (0.036)
Left genu of internal capsule 0.67 (0.15) 0.68 (0.13) t=−0.88 (0.93) F=0.024 (0.878) 613.4 (90.33) 621.1 (82.68) t=−0.26 (0.79) F=0.299 (0.588)
Left posterior limb of internal capsule 0.72 (0.10) 0.73 (0.12) t=−0.21 (0.84) F=0.111 (0.741) 662.03 (70.42) 664.58 (51.89) t=−0.12 (0.90) F=0.003 (0.960)
Right anterior limb of internal capsule 0.61 (0.19) 0.56 (0.17) t=0.82 (0.41) F=0.044 (0.834) 687.48 (222.14) 725.79 (81.77) t=−0.64 (0.53) F=0.037 (0.849)
Right genu of internal capsule 0.65 (0.16) 0.68 (0.14) t=−0.65 (0.52) F=0.003 (0.958) 639.93 (100.23) 615.29 (96.48) t=0.75 (0.46) F=0.427 (0.518)
Right posterior limb of internal capsule 0.75 (0.12) 0.12 (0.11) t=0.81 (0.42) F=0.397 (0.533) 626.55 (75.10) 663.15 (63.28) t=−1.56 (0.13) F=0.698 (0.409)
Left cingulum 0.71 (0.09) 0.72 (0.07) t=−0.33 (0.75) F=0.141 (0.709) 704.87 (125.37) 701.87 (51.52) t=0.09 (0.93) F=0.456 (0.504)
Right cingulum 0.65 (0.13) 0.66 (0.04) t=−0.12 (0.90) F=1.013 (0.321) 698.62 (86.98) 717.33 (76.53) t=−0.68 (0.50) F=0.006 (0.636)
Left superior occipitofrontal fasciculus 0.44 (0.07) 0.48 (0.05) t=−1.73 (0.09) F=1.254 (0.270) 673.58 (59.34) 644.67 (38.20) t=1.71 (0.10) F=3.114 (0.086)
Right superior occipitofrontal fasciculus 0.44 (0.08) 0.46 (0.06) t=−0.93 (0.36) F=0.266 (0.609) 670.13 (88.63) 653.99 (35.20) t=1.05 (0.30) F=0.179 (0.675)
Left superior longitudinal fasciculus 0.41 (0.06) 0.42 (0.06) t=−0.80 (0.43) F=1.254 (0.270) 665.96 (43.14) 648.82 (33.38) t=1.30 (0.20) F=1.465 (0.234)
Right superior longitudinal fasciculus 0.41 (0.07) 0.45 (0.06) t=−2.05 (0.047)* F=0.266 (0.609) 662.19 (35.55) 653.99 (35.21) t=0.7 (0.49) F=0.718 (0.403)
Left inferior occipitofrontal fasciculus 0.54 (0.09) 0.57 (0.09) t=−1.10 (0.28) F=0.654 (0.424) 789.33 (105.16) 769.85 (86.18) t=0.6 (0.55) F=0.646 (0.427)
Right inferior occipitofrontal fasciculus 0.57 (0.11) 0.51 (0.09) t=1.71 (0.10) F=0.357 (0.067) 750.30 (78.76) 752.98 (56.20) t=−0.11 (0.91) F=0.253 (0.618)
[Downloaded free from http://www.indianjpsychiatry.org on Saturday, April 17, 2021, IP: 117.251.52.169]
Left inferior longitudinal fasciculus 0.39 (0.08) 0.40 (0.09) t=−0.19 (0.85) F=0.033 (0.856) 774.82 (94.58) 786.93 (116.79) t=−0.35 (0.73) F=2.045 (0.162)
Aggarwal, et al.: DTI study of patients with and without TRS
Right inferior longitudinal fasciculus 0.38 (0.10) 0.38 (0.11) t=0.12 (0.90) F=0.045 (0.833) 761.38 (96.90) 728.23 (66.70) t=1.16 (0.25) F=0.003 (0.958)
Left uncinate fasciculus 0.38 (0.10) 0.36 (0.10) t=0.64 (0.53) F=0.175 (0.678) 780.97 (102.04) 811.15 (89.13) t=−0.93 (0.36) F=0.403 (0.530)
Right uncinate fasciculus 0.36 (0.09) 0.44 (0.11) t=−2.46 (0.019)* F=6.122 (0.018)* 770.24 (95.71) 775.9 (69.74) t=−0.2 (0.84) F=0.119 (0.732)
*P≤0.05; **P≤0.01; ***P≤0.001. aCovariate: Duration of untreated psychosis. χ2 – Chi‑square value; χ2b – Chi‑square value with Yate’s correction; U – Mann-Whitney value; t – T test; SD – standard deviation;
FE – Fisher’s exact value; TRS – Treatment‑resistant schizophrenia
Indian Journal of Psychiatry Volume 63, Issue 2, March-April 2021
[Downloaded free from http://www.indianjpsychiatry.org on Saturday, April 17, 2021, IP: 117.251.52.169]
Aggarwal, et al.: DTI study of patients with and without TRS
present study did not involve the assessment of cognitive
functions and did not include a healthy control group. DTI
findings were assessed manually rather than using more
sophisticated techniques such as tract‑based spatial statistics.
Future studies must attempt to overcome these limitations.
CONCLUSION
The present study demonstrates that white‑matter integrity
a
does not significantly differ between the patients with and
without TRS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
b 1. Keshavan MS, Nasrallah HA, Tandon R. Schizophrenia, “Just the Facts”
6. Moving ahead with the schizophrenia concept: From the elephant to the
Figure 2: (a) Fractional anisotropy at a point for the densest
mouse. Schizophr Res 2011;127:3‑13.
portion of uncinate fasciculus. (b) Fractional anisotropy at a 2. Molina JD, Jiménez‑González AB, López‑Muñoz F, Cañas F. Evolution of
point for the densest portion of superior longitudinal fasciculus the concept of treatment‑resistant schizophrenia: Toward a reformulation
for lack of an adequate response. J Exp Clin Med 2012;4:98‑102.
3. McGlashan TH. A selective review of recent North American long‑term
evaluated the white‑matter integrity in patients with TRS followup studies of schizophrenia. Schizophr Bull 1988;14:515‑42.
4. Mouchlianitis E, McCutcheon R, Howes OD. Brain‑imaging studies of
by using DTI and compared the same with patients without treatment‑resistant schizophrenia: A systematic review. Lancet Psychiatry
treatment refractoriness.[6] This study concluded that there 2016;3:451‑63.
5. Nakajima S, Takeuchi H, Plitman E, Fervaha G, Gerretsen P,
are no differences in FA values/white‑matter integrity Caravaggio F, et al. Neuroimaging findings in treatment‑resistant
between treatment refractory and nonrefractory groups schizophrenia: A systematic review: Lack of neuroimaging correlates of
following voxel‑wise analysis TBSS approach.[6] The findings treatment‑resistant schizophrenia. Schizophr Res 2015;164:164‑75.
6. Rodrigues JP, Reis Marques T, Picchioni MM, Ferragamo C, Lawrie S,
of the present study support the same. As per evidence, Sendt KV, et al. Poster #M178: White matter integrity in treatment-refractory
normal controls have asymmetry, with anisotropy on the schizophrenia: a diffusion tensor imaging study. NPJ SCHIZOPHRENIA.
2016;2. 16008. https://doi.org/10.1038/npjschz.2016.8.
left more than right in the UF and patients with chronic 7. Aas IH. Guidelines for rating Global Assessment of Functioning (GAF).
schizophrenia lack the normal left‑greater‑than‑right Ann Gen Psychiatry 2011;10:2.
8. Hunter EE, Murphy M. Brief Psychiatric Rating Scale. In: Kreutzer JS,
anisotropy asymmetry in the UF.[13‑15] DeLuca J, Caplan B, editors. Encyclopedia of Clinical Neuropsychology.
New York, NY: Springer; 2011.
9. Busner J, Targum SD. The clinical global impressions scale: Applying a
Findings of the present study must be interpreted in light research tool in clinical practice. Psychiatry (Edgmont) 2007;4:28‑37.
of its limitations in the form of small sample size and 10. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E,
et al. The Mini‑International Neuropsychiatric Interview (M.I.N.I.): The
cross‑sectional assessment. Cross‑sectional comparisons of development and validation of a structured diagnostic psychiatric interview
treatment‑resistant and ‑responsive patients can potentially for DSM‑IV and ICD‑10. J Clin Psychiatry 1998;59 Suppl 20:22‑33.
indicate differences that may underlie treatment resistance. 11. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome
scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261‑76.
They cannot, however, determine causality. In the present 12. Shafer A. Meta‑analysis of the brief psychiatric rating scale factor structure.
study, the study participants in the non‑TRS group were in Psychol Assess 2005;17:324‑35.
13. Kubicki M, Westin CF, Maier SE, Frumin M, Nestor PG, Salisbury DF,
clinical remission, whereas participants of the TRS group et al. Uncinate fasciculus findings in schizophrenia: A magnetic resonance
were symptomatic at the time of the assessment. Have diffusion tensor imaging study. Am J Psychiatry 2002;159:813‑20.
14. Highley JR, Walker MA, Esiri MM, Crow TJ, Harrison PJ. Asymmetry of the
a non‑TRS symptomatic group, could have been better. uncinate fasciculus: A post‑mortem study of normal subjects and patients
Furthermore, prospective studies will be required to evaluate with schizophrenia. Cereb Cortex 2002;12:1218‑24.
15. Burns J, Job D, Bastin ME, Whalley H, Macgillivray T, Johnstone EC, et al.
whether any neurobiological markers have the potential for Structural disconnectivity in schizophrenia: A diffusion tensor magnetic
clinically relevant prediction of treatment resistance. The resonance imaging study. Br J Psychiatry 2003;182:439‑43.
Indian Journal of Psychiatry Volume 63, Issue 2, March-April 2021 151
You might also like
- Student Cell CommunicationDocument11 pagesStudent Cell Communicationapi-2620290510% (1)
- The Massachusetts General Hospital Guide to Depression: New Treatment Insights and OptionsFrom EverandThe Massachusetts General Hospital Guide to Depression: New Treatment Insights and OptionsBenjamin G. ShaperoNo ratings yet
- Obstetrics and Gynaecology History Taking TemplateDocument4 pagesObstetrics and Gynaecology History Taking TemplateMaruti100% (3)
- 10 1016@j JHT 2017 02 001 PDFDocument10 pages10 1016@j JHT 2017 02 001 PDFGusti Ayu KrisnayantiNo ratings yet
- The Neural Basis of Religious Cognition: Jordan Grafman, Irene Cristofori, Wanting Zhong, and Joseph BulbuliaDocument8 pagesThe Neural Basis of Religious Cognition: Jordan Grafman, Irene Cristofori, Wanting Zhong, and Joseph Bulbuliagion.nand100% (1)
- ndt-18-891Document7 pagesndt-18-891Julio DelgadoNo ratings yet
- Wisconsin Card Sorting Test Performance ImpairmentDocument6 pagesWisconsin Card Sorting Test Performance ImpairmentAbhishek kumarNo ratings yet
- IJPsyM 41 178Document4 pagesIJPsyM 41 178uml.beitsahourNo ratings yet
- Meisi Arisandi - Resume Jurnal Internasional Dan Nasional Keperawatan JiwaDocument6 pagesMeisi Arisandi - Resume Jurnal Internasional Dan Nasional Keperawatan JiwawendihiNo ratings yet
- Antipsychotic Treatment - A Systematic Literature Review and Meta-Analysis of Qualitative StudiesDocument12 pagesAntipsychotic Treatment - A Systematic Literature Review and Meta-Analysis of Qualitative StudiesPriti BhosleNo ratings yet
- Association Between Medication Adherence and Duration of Outpatient Treatment in Patients With SchizophreniaDocument7 pagesAssociation Between Medication Adherence and Duration of Outpatient Treatment in Patients With SchizophreniaazedaaNo ratings yet
- Clinical Correlates of Treatment Adherence and Insight in Patients With SchizophreniaDocument5 pagesClinical Correlates of Treatment Adherence and Insight in Patients With SchizophreniaArif IrpanNo ratings yet
- Risperidone Improves Interpersonal Perception and Executive Function in Patients With SchizophreniaDocument7 pagesRisperidone Improves Interpersonal Perception and Executive Function in Patients With SchizophreniaBuatlogin DoangNo ratings yet
- Good For QualitativeDocument9 pagesGood For QualitativeWassie TsehayNo ratings yet
- Factor Associated With Unfavourable Treatment Outcome Among Adult Tuberculosis Patients in Agra: A Cross-Sectional StudyDocument7 pagesFactor Associated With Unfavourable Treatment Outcome Among Adult Tuberculosis Patients in Agra: A Cross-Sectional StudyIJAR JOURNALNo ratings yet
- Impact of Antipsychotic Medication On Transcranial Direct Current Stimulation (TDCS) Effects in Schizophrenia PatientsDocument7 pagesImpact of Antipsychotic Medication On Transcranial Direct Current Stimulation (TDCS) Effects in Schizophrenia PatientsAlexis GrayNo ratings yet
- Antipsychotic Treatment A Systematic Literature Review and Meta Analysis of Qualitative StudiesDocument12 pagesAntipsychotic Treatment A Systematic Literature Review and Meta Analysis of Qualitative StudiesmafeNo ratings yet
- NDT 81677 Adherence and Re Hospitalizations in Patients With Schizophr 040115Document6 pagesNDT 81677 Adherence and Re Hospitalizations in Patients With Schizophr 040115Elsa OctaviaNo ratings yet
- Clinical Phenotypes of Icu Delirium and Long Term Cognitive ImpairmenetDocument22 pagesClinical Phenotypes of Icu Delirium and Long Term Cognitive ImpairmenetPsiquiatría CESAMENo ratings yet
- 2014 - Intelligence As A Predictor of Outcome in Short-And Long-Term PsychotherapyDocument9 pages2014 - Intelligence As A Predictor of Outcome in Short-And Long-Term PsychotherapyZayne CarrickNo ratings yet
- The Relationship of Cognitive Functions and Psychopathology On The Level of Insight in Patients With SchizophreniaDocument6 pagesThe Relationship of Cognitive Functions and Psychopathology On The Level of Insight in Patients With SchizophrenianandhaNo ratings yet
- Therapeutic Adherence in A Population of Patients Treated For Schizophrenia at The Hospital For Mental Health and Psychiatric Disorders in TangierDocument8 pagesTherapeutic Adherence in A Population of Patients Treated For Schizophrenia at The Hospital For Mental Health and Psychiatric Disorders in TangierIJAR JOURNALNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- (Astuti, Anggorowati & Johan, 2017) PDFDocument7 pages(Astuti, Anggorowati & Johan, 2017) PDFYuliaNo ratings yet
- Cognitive Behavior Therapy For Schizophrenia 2006Document9 pagesCognitive Behavior Therapy For Schizophrenia 2006Patri SanchezNo ratings yet
- Acta Psychiatr Scand - 2022 - Li - Estradiol and Raloxifene As Adjunctive Treatment For Women With Schizophrenia ADocument13 pagesActa Psychiatr Scand - 2022 - Li - Estradiol and Raloxifene As Adjunctive Treatment For Women With Schizophrenia AmarketinglobalsmNo ratings yet
- NDT 45697 Efficacy of Second Generation Antipsychotics in Patients at 061813Document8 pagesNDT 45697 Efficacy of Second Generation Antipsychotics in Patients at 061813twahyuningsih_16No ratings yet
- Long Term Vs Short TermDocument9 pagesLong Term Vs Short TermHerizko KusumaNo ratings yet
- NCM 115 Journal Article Review.2023Document2 pagesNCM 115 Journal Article Review.2023Hanniel Jufet GolosindaNo ratings yet
- Pi Is 2215036616303789Document11 pagesPi Is 2215036616303789U of T MedicineNo ratings yet
- 31022-Article Text-57704-1-10-20210727Document3 pages31022-Article Text-57704-1-10-20210727Manusia BiasaNo ratings yet
- First-Episode Psychosis in Treatment-Resistant Schizophrenia: A Cross-Sectional Study of A Long-Term Follow-Up CohortDocument10 pagesFirst-Episode Psychosis in Treatment-Resistant Schizophrenia: A Cross-Sectional Study of A Long-Term Follow-Up CohortagungratihsdNo ratings yet
- Psychotherapy For Chronic Treatment Non Responce Choose Change Trial - 2022Document9 pagesPsychotherapy For Chronic Treatment Non Responce Choose Change Trial - 2022Ericka RutledgeNo ratings yet
- Psychoeducation For Schizophrenia (Review) : CochraneDocument3 pagesPsychoeducation For Schizophrenia (Review) : CochraneKenny KenNo ratings yet
- How Patients' Characteristics Influence The Use of Coercive MeasuresDocument6 pagesHow Patients' Characteristics Influence The Use of Coercive Measuresmas royNo ratings yet
- Ashina2020 Article EfficacyTolerabilityAndSafetyODocument9 pagesAshina2020 Article EfficacyTolerabilityAndSafetyOFirjatullahNo ratings yet
- Background: Lancet Psychiatry 2017Document11 pagesBackground: Lancet Psychiatry 2017Manya DhuparNo ratings yet
- The Effect of Foot Re Exology On Hospital Anxiety and Depression in Female Older Adults: A Randomized Controlled TrialDocument7 pagesThe Effect of Foot Re Exology On Hospital Anxiety and Depression in Female Older Adults: A Randomized Controlled TrialZainal AbidinNo ratings yet
- The Efficacy of Psychological Interventions On Psoriasis Treatment: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument10 pagesThe Efficacy of Psychological Interventions On Psoriasis Treatment: A Systematic Review and Meta-Analysis of Randomized Controlled Trialsluthfianisa azhariNo ratings yet
- Is ItmeVerbalself MonitoringneuralnetworkandclinicalinsightDocument8 pagesIs ItmeVerbalself MonitoringneuralnetworkandclinicalinsightVictor CarrenoNo ratings yet
- Ayuda Al Diagnóstico Del Trastorno de Identidad Disociativo Estudio de Reconocimiento de Patrones de Biomarcadores CerebralesDocument9 pagesAyuda Al Diagnóstico Del Trastorno de Identidad Disociativo Estudio de Reconocimiento de Patrones de Biomarcadores CerebralesValentina RodriguezNo ratings yet
- Trivino Et Al 2017 Effectiventess of A Neuropsychological Treatment For ConfabulatinsDocument25 pagesTrivino Et Al 2017 Effectiventess of A Neuropsychological Treatment For ConfabulatinsJoNo ratings yet
- Long-Term Cognitive Impairment After Critical Illness: Original ArticleDocument11 pagesLong-Term Cognitive Impairment After Critical Illness: Original ArticleRendy ReventonNo ratings yet
- American J Addict - 2023 - Faltushanskiy - Personality Predicting Relapse A Facet Analysis of The NEO PI RDocument7 pagesAmerican J Addict - 2023 - Faltushanskiy - Personality Predicting Relapse A Facet Analysis of The NEO PI RniedobroNo ratings yet
- Application of Functional Analytic Psychotherapy To Manage SchizophreniaDocument12 pagesApplication of Functional Analytic Psychotherapy To Manage Schizophreniamasterking K9No ratings yet
- Depression and Anxiety in Patients With Chronic Kidney Disease Undergoing HemodialysisDocument5 pagesDepression and Anxiety in Patients With Chronic Kidney Disease Undergoing HemodialysisDani ursNo ratings yet
- Jurnal JiwaDocument6 pagesJurnal JiwaoldDEUSNo ratings yet
- 1 s2.0 S0969996118304947 MainDocument13 pages1 s2.0 S0969996118304947 Maincherish60126No ratings yet
- International Journal of Trend in Scientific Research and Development (IJTSRD)Document4 pagesInternational Journal of Trend in Scientific Research and Development (IJTSRD)Editor IJTSRDNo ratings yet
- Journal Homepage: - : IntroductionDocument8 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Study On Clinical Presentations, Level of Stress & Role of Family Environment Among Dissociative Disorder PatientsDocument10 pagesStudy On Clinical Presentations, Level of Stress & Role of Family Environment Among Dissociative Disorder PatientsIJAR JOURNALNo ratings yet
- Extrapyramidal Symptoms in 10 Years of Long Term Treatment of Schizophrenia: Independent of Psychopathology and OutcomeDocument5 pagesExtrapyramidal Symptoms in 10 Years of Long Term Treatment of Schizophrenia: Independent of Psychopathology and OutcomeSeiska MegaNo ratings yet
- A Study To Assess The Effectiveness of Art Therapy To Reduce Depression Among Old Age Clients Admitted in Saveetha Medical College and Hospital, Thandalam, ChennaiDocument5 pagesA Study To Assess The Effectiveness of Art Therapy To Reduce Depression Among Old Age Clients Admitted in Saveetha Medical College and Hospital, Thandalam, ChennaiEditor IJTSRDNo ratings yet
- 50 179 1 PBDocument6 pages50 179 1 PBAmir UnbrahNo ratings yet
- Depression in Patients With Multiple Sclerosis: A Review StudyDocument5 pagesDepression in Patients With Multiple Sclerosis: A Review StudyalirezanouriNo ratings yet
- Assessment of Prescription Pattern Among Patients Suffering From HeadacheDocument4 pagesAssessment of Prescription Pattern Among Patients Suffering From HeadachedrziaapollohospitalsNo ratings yet
- 10 1111@jcpt 13177Document8 pages10 1111@jcpt 13177opanocayNo ratings yet
- Efficacy of Cognitive Behaviour Therapy in ManagementDocument5 pagesEfficacy of Cognitive Behaviour Therapy in ManagementIrfan FauziNo ratings yet
- Jurnal SkizoafektifDocument7 pagesJurnal SkizoafektifkhairinanurulNo ratings yet
- Schizophrenia Research: Markku Lähteenvuo, Heidi Taipale, Antti Tanskanen, Ellenor Mittendorfer-Rutz, Jari TiihonenDocument6 pagesSchizophrenia Research: Markku Lähteenvuo, Heidi Taipale, Antti Tanskanen, Ellenor Mittendorfer-Rutz, Jari TiihonenIndrajatiNo ratings yet
- A Randomized Controlled Trial of A Mindfulness-Based Intervention Program For People With Schizophrenia: 6-Month Follow-UpDocument14 pagesA Randomized Controlled Trial of A Mindfulness-Based Intervention Program For People With Schizophrenia: 6-Month Follow-UpOrion OriNo ratings yet
- Reduction in Mental Health Treatment UtilizationDocument8 pagesReduction in Mental Health Treatment UtilizationAndrewsNo ratings yet
- Appi Ajp 2019 19010080Document8 pagesAppi Ajp 2019 19010080sarahNo ratings yet
- Schizotaxia - A Review - IJSP 2004Document8 pagesSchizotaxia - A Review - IJSP 2004gion.nandNo ratings yet
- IndianJPsychiatry632171-3970252 110142Document4 pagesIndianJPsychiatry632171-3970252 110142gion.nandNo ratings yet
- Awards CriteriaDocument4 pagesAwards Criteriagion.nandNo ratings yet
- Quality of Psychiatry Journals Published From.13Document5 pagesQuality of Psychiatry Journals Published From.13gion.nandNo ratings yet
- Das N Das S Medical Writers and GhostwriDocument6 pagesDas N Das S Medical Writers and Ghostwrigion.nandNo ratings yet
- IndianJPsychiatry618149-4008418 110804Document1 pageIndianJPsychiatry618149-4008418 110804gion.nandNo ratings yet
- Schizophrenia and EmploymentDocument13 pagesSchizophrenia and Employmentgion.nandNo ratings yet
- From The Desk of Vice President-Elect: Mrugesh VaishnavDocument1 pageFrom The Desk of Vice President-Elect: Mrugesh Vaishnavgion.nandNo ratings yet
- Early Onset Bipolar Disorder, Stress, and Coping Responses of Mothers: A Comparative StudyDocument10 pagesEarly Onset Bipolar Disorder, Stress, and Coping Responses of Mothers: A Comparative Studygion.nandNo ratings yet
- Sexual Functioning During The Lockdown Period in India: An Online SurveyDocument8 pagesSexual Functioning During The Lockdown Period in India: An Online Surveygion.nandNo ratings yet
- IndianJPsychiatry632179-396519 110051Document5 pagesIndianJPsychiatry632179-396519 110051gion.nandNo ratings yet
- Pain Threshold and Pain Tolerance As A Predictor of Deliberate Self-Harm Among Adolescents and Young AdultsDocument4 pagesPain Threshold and Pain Tolerance As A Predictor of Deliberate Self-Harm Among Adolescents and Young Adultsgion.nandNo ratings yet
- IndianJPsychiatry631102-4698058 130300Document2 pagesIndianJPsychiatry631102-4698058 130300gion.nandNo ratings yet
- Telemedicine Practice Guidelines of India, 2020: Implications and ChallengesDocument5 pagesTelemedicine Practice Guidelines of India, 2020: Implications and Challengesgion.nandNo ratings yet
- Body (13-112)Document100 pagesBody (13-112)gion.nandNo ratings yet
- Ganser Syndrome: Intricacy in Diagnosis and ManagementDocument2 pagesGanser Syndrome: Intricacy in Diagnosis and Managementgion.nandNo ratings yet
- IndianJPsychiatry63135-466605 125740Document6 pagesIndianJPsychiatry63135-466605 125740gion.nandNo ratings yet
- Qualitative Research Methods in Psychiatry in India: Landscaping The TerrainDocument10 pagesQualitative Research Methods in Psychiatry in India: Landscaping The Terraingion.nandNo ratings yet
- Long Term Management of SchizophreniaDocument11 pagesLong Term Management of Schizophreniagion.nandNo ratings yet
- 13 Common Errors in Psychopharmacology: EditorialDocument8 pages13 Common Errors in Psychopharmacology: Editorialgion.nandNo ratings yet
- Newer Documentary Practices As Per Mental Healthcare Act 2017Document7 pagesNewer Documentary Practices As Per Mental Healthcare Act 2017gion.nandNo ratings yet
- IndianJPsychiatry 2019 61 4 423 262795Document2 pagesIndianJPsychiatry 2019 61 4 423 262795gion.nandNo ratings yet
- Mental Healthcare Act 2017: Preface To The Supplement: Shahul Ameen, Mahesh Gowda, G. S. RamkumarDocument3 pagesMental Healthcare Act 2017: Preface To The Supplement: Shahul Ameen, Mahesh Gowda, G. S. Ramkumargion.nandNo ratings yet
- Child Development Assessment Tools in Low-Income and Middle-Income CountriesDocument9 pagesChild Development Assessment Tools in Low-Income and Middle-Income Countriesalibaba1888No ratings yet
- PDF Medical Language Instant Translator 6 Ed Edition Davi Ellen Chabner Ebook Full ChapterDocument53 pagesPDF Medical Language Instant Translator 6 Ed Edition Davi Ellen Chabner Ebook Full Chapterdaniel.mann336100% (4)
- Power of The Pinch Pinch Lower Lid BlepharoplastyDocument6 pagesPower of The Pinch Pinch Lower Lid BlepharoplastyBFF BotoxNo ratings yet
- Ascari As IsDocument4 pagesAscari As IsHassan osmanNo ratings yet
- Female Urinary CatheterizationDocument4 pagesFemale Urinary CatheterizationArdiene Shallouvette GamosoNo ratings yet
- Education For Physically Challenged Children Set 1Document6 pagesEducation For Physically Challenged Children Set 1Ahmed KhanNo ratings yet
- ESMO Checklist Breast Cancer Patient Related Treatment WorkflowDocument1 pageESMO Checklist Breast Cancer Patient Related Treatment WorkflowsameeramwNo ratings yet
- Sexual Dysfunction in The United States: Prevalence and PredictorsDocument9 pagesSexual Dysfunction in The United States: Prevalence and Predictorscepavek196No ratings yet
- PT3 ROM-GonioDocument3 pagesPT3 ROM-Gonioim. EliasNo ratings yet
- Case Study (Adellia Irma P - 01.2.17.00590Document3 pagesCase Study (Adellia Irma P - 01.2.17.00590Anastasia Dewi AprillaNo ratings yet
- Application of Puerperal Healthy of Optimization of Postpartum Mother Knowledges That Given Effleurage Relaxation MassageDocument4 pagesApplication of Puerperal Healthy of Optimization of Postpartum Mother Knowledges That Given Effleurage Relaxation MassageInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Causes of AneurysmsDocument11 pagesCauses of AneurysmsMathew Ace M. OmilaNo ratings yet
- Heart Disease Prediction With Machine Learning ApproachesDocument5 pagesHeart Disease Prediction With Machine Learning ApproachesRony sahaNo ratings yet
- Added Sugars and Periodontal Disease in Young Adults: An Analysis of NHANES III DataDocument6 pagesAdded Sugars and Periodontal Disease in Young Adults: An Analysis of NHANES III DataNavaneethan GnanadesiganNo ratings yet
- Schneider, Meir - Handbook of Self-HealingDocument522 pagesSchneider, Meir - Handbook of Self-Healingavanzit5No ratings yet
- Hydrogen Peroxide Magic - Thacker.bDocument209 pagesHydrogen Peroxide Magic - Thacker.bMathieu ChautardNo ratings yet
- Risk Factors and Common Test of Genetic DisordersDocument29 pagesRisk Factors and Common Test of Genetic DisordersBianca Nicole Gacad FernandezNo ratings yet
- Hepatosplenomegaly: - Question: - AnswerDocument7 pagesHepatosplenomegaly: - Question: - AnswerSyximsh FPNo ratings yet
- Wound Healing Properties of Root Extract of Harungana Madagascariensis On Wistar Rat ModelDocument6 pagesWound Healing Properties of Root Extract of Harungana Madagascariensis On Wistar Rat ModelInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Mislim To Je ToDocument2 pagesMislim To Je ToIslami IsmailNo ratings yet
- Differences Between Men and Women BrainDocument1 pageDifferences Between Men and Women BrainHuiLingNo ratings yet
- Carpal Tunnel SyndromeDocument9 pagesCarpal Tunnel SyndromeMaha RajaNo ratings yet
- Logbook GIDocument15 pagesLogbook GIAna BorodinaNo ratings yet
- Philippine Adult Immunization Recommendation 2017 PDFDocument2 pagesPhilippine Adult Immunization Recommendation 2017 PDFLinius CruzNo ratings yet
- Sample Case Study-2-1Document4 pagesSample Case Study-2-1visiniNo ratings yet
- Comms 310 Strategic Message Planner Part 1Document7 pagesComms 310 Strategic Message Planner Part 1api-508434828No ratings yet
- Agnes MotuloDocument5 pagesAgnes MotuloFiLiOeiNo ratings yet
- Location: Map of Naga CityDocument2 pagesLocation: Map of Naga Citycatherine boragayNo ratings yet