Professional Documents
Culture Documents
Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva Susanti
Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva Susanti
Uploaded by
danaagus81Copyright:
Available Formats
You might also like
- Michael Grant Anaesthetics Emergency Medicine Notes PDFDocument70 pagesMichael Grant Anaesthetics Emergency Medicine Notes PDFMimansaDixit100% (1)
- ChorioretinitisDocument13 pagesChorioretinitisrada tri rosi kurniaNo ratings yet
- Diagnosis AndtreatmentofallergicrhinitisinchildrenDocument6 pagesDiagnosis AndtreatmentofallergicrhinitisinchildrenIRANo ratings yet
- New Schatz2018 OldDocument44 pagesNew Schatz2018 Oldabhijeet abhijeetNo ratings yet
- New Schatz2018Document44 pagesNew Schatz2018abhijeet abhijeetNo ratings yet
- 011AADocument8 pages011AAAtef AlbooqNo ratings yet
- Probiotic Therapy On Children With Allergic RhinitisDocument4 pagesProbiotic Therapy On Children With Allergic RhinitisSus Retha Mona ArdianiNo ratings yet
- Schatz 2018Document44 pagesSchatz 2018abhijeet abhijeetNo ratings yet
- Ijerph 12 10984 v2Document11 pagesIjerph 12 10984 v2Nurjanah PutriNo ratings yet
- Allergic Rhinitis in ChildrenDocument7 pagesAllergic Rhinitis in ChildrenTina MorleyNo ratings yet
- Efficacy of Probiotic in Perennial Allergic Rhinitis Under Five Year Children: A Randomized Controlled TrialDocument6 pagesEfficacy of Probiotic in Perennial Allergic Rhinitis Under Five Year Children: A Randomized Controlled TrialBezoNo ratings yet
- Pi Is 1081120622006536Document11 pagesPi Is 1081120622006536Niken KuncorowatiNo ratings yet
- Allergen Immunotherapy Expert ExchangeDocument4 pagesAllergen Immunotherapy Expert ExchangeAnna LiachenkoNo ratings yet
- Out 4Document3 pagesOut 4Musthafa Afif WardhanaNo ratings yet
- Medical News in The World of Atopic Dermatitis First Quarter 2016Document5 pagesMedical News in The World of Atopic Dermatitis First Quarter 2016anon_384025255No ratings yet
- Perbedaan Imunoterapi Alergen Spesifik (ITS) Dengan Vaksinasi BCG Dalam Meningkatkan Kualitas Hidup Penderita Rinitis AlergiDocument12 pagesPerbedaan Imunoterapi Alergen Spesifik (ITS) Dengan Vaksinasi BCG Dalam Meningkatkan Kualitas Hidup Penderita Rinitis AlergiThya Alif KahfNo ratings yet
- Sublingual Immunotherapy To House Dust Mite in Pediatric Patients With Allergic Rhinitis and Asthma: A Retrospective Analysis of Clinical Course Over A 3-Year Follow-Up PeriodDocument4 pagesSublingual Immunotherapy To House Dust Mite in Pediatric Patients With Allergic Rhinitis and Asthma: A Retrospective Analysis of Clinical Course Over A 3-Year Follow-Up PeriodPeter SalimNo ratings yet
- Research ArticleDocument6 pagesResearch ArticleReffy AdhaNo ratings yet
- Vitamin D Deficiency and Its Relation To Allergic Diseases A Cross Sectional Study Among Allergic Patients From Jeddah City Saudi ArabiaDocument17 pagesVitamin D Deficiency and Its Relation To Allergic Diseases A Cross Sectional Study Among Allergic Patients From Jeddah City Saudi ArabiaAthenaeum Scientific PublishersNo ratings yet
- Comparison of Sublingual Immunotherapy in Patients With Allergic Rhinitis Sensitive To House Dust Mites in KoreaDocument8 pagesComparison of Sublingual Immunotherapy in Patients With Allergic Rhinitis Sensitive To House Dust Mites in Koreafm_askaNo ratings yet
- Nutrients 10 01678Document11 pagesNutrients 10 01678zulfa nadiaNo ratings yet
- Probiotics in Late Infancy Reduce The Incidence of Eczema: A Randomized Controlled TrialDocument6 pagesProbiotics in Late Infancy Reduce The Incidence of Eczema: A Randomized Controlled TrialarditaNo ratings yet
- Effect of Oral Vitamin E On Atopic DermatitisDocument4 pagesEffect of Oral Vitamin E On Atopic DermatitisYusufTaqwaMuladiNo ratings yet
- Probioticos Rinitis AlergicaDocument8 pagesProbioticos Rinitis AlergicaFlavio GuillenNo ratings yet
- Diagnosing Allergic Rhinitis - Is There A Need?Document3 pagesDiagnosing Allergic Rhinitis - Is There A Need?Alfa Suryani ArdliNo ratings yet
- Nurmatov Et Al-2012-Cochrane Database of Systematic ReviewsDocument4 pagesNurmatov Et Al-2012-Cochrane Database of Systematic ReviewsfiskaderishaNo ratings yet
- Andosan™-An Anti-Allergic and Anti-Inflammatory Ingredient Prepared From Agaricus Blazei MushroomDocument11 pagesAndosan™-An Anti-Allergic and Anti-Inflammatory Ingredient Prepared From Agaricus Blazei MushroomMartinaNo ratings yet
- Evaluation of Six Years Allergen ImmunotherapyDocument12 pagesEvaluation of Six Years Allergen ImmunotherapyArifin I. OputuNo ratings yet
- Sintha nug,+6.+CR+5+-+RAZIV+FINISHDocument7 pagesSintha nug,+6.+CR+5+-+RAZIV+FINISHFyiaaa02No ratings yet
- Pharmacoeconomics of allergy immunotherapy versus pharmacotherapyDocument14 pagesPharmacoeconomics of allergy immunotherapy versus pharmacotherapyjladinoNo ratings yet
- 1 s2.0 S1684118218301816 Main PDFDocument28 pages1 s2.0 S1684118218301816 Main PDFPrasetyaNo ratings yet
- Allergy - 2022 - Farraia - Allergen Immunotherapy For Asthma Prevention A Systematic Review and Meta Analysis ofDocument17 pagesAllergy - 2022 - Farraia - Allergen Immunotherapy For Asthma Prevention A Systematic Review and Meta Analysis ofpedrotiagosilvaNo ratings yet
- Prevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisDocument6 pagesPrevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisKevinFeraldyNo ratings yet
- DermatitisDocument6 pagesDermatitisAmalia Zulfa AmandaNo ratings yet
- High-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialDocument15 pagesHigh-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialHendra EfendiNo ratings yet
- Probiotics in Pregnant Women To Prevent Allergic Disease: A Randomized, Double-Blind TrialDocument8 pagesProbiotics in Pregnant Women To Prevent Allergic Disease: A Randomized, Double-Blind TrialarditaNo ratings yet
- Probiotics For The Prevention of Allergy A Systematic ReviewDocument10 pagesProbiotics For The Prevention of Allergy A Systematic ReviewadhyNo ratings yet
- The Efficiency and Safety of Olopatadine Against Rupatadine in Chronic Urticaria of Idiopathic Origin: A Comparative StudyDocument6 pagesThe Efficiency and Safety of Olopatadine Against Rupatadine in Chronic Urticaria of Idiopathic Origin: A Comparative StudyArezoo JamNo ratings yet
- Probiotic Allergic RhinitsDocument7 pagesProbiotic Allergic Rhinitscharoline gracetiani nataliaNo ratings yet
- PIIS1939455119301723Document5 pagesPIIS1939455119301723Yeol LoeyNo ratings yet
- Treatment of Allergic Rhinitis: DENISE K. SUR, MD, and STEPHANIE SCANDALE, MD, David Geffen School of MedicineDocument7 pagesTreatment of Allergic Rhinitis: DENISE K. SUR, MD, and STEPHANIE SCANDALE, MD, David Geffen School of MedicineM Isyhaduul IslamNo ratings yet
- Atopic DermatitisDocument5 pagesAtopic DermatitisUlung PrayogoNo ratings yet
- IgM Pada ThypoidDocument4 pagesIgM Pada ThypoidririlibertiNo ratings yet
- Abrahamsson 2013Document6 pagesAbrahamsson 2013Anja LjiljaNo ratings yet
- Clinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiaDocument6 pagesClinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiamariaprincesitaNo ratings yet
- Jurnal THTDocument14 pagesJurnal THTLaras Asri FatahaniNo ratings yet
- Jurnal RhinitisDocument6 pagesJurnal RhinitisdwiNo ratings yet
- Sinovac 3Document7 pagesSinovac 3Lukas ZamudioNo ratings yet
- Sublingual ImmunotherapyDocument4 pagesSublingual ImmunotherapyAnonymous eZqDZbObRiNo ratings yet
- Use of Superoxide Dismutase in Accelerating Symptom PDFDocument7 pagesUse of Superoxide Dismutase in Accelerating Symptom PDFWilliam JavierNo ratings yet
- Infections in Children Aged 6 Months To 5 Years Treated With Dupilumab in A Placebo-Controlled Clinical Trial of Moderate-To-Severe Atopic DermatitisDocument11 pagesInfections in Children Aged 6 Months To 5 Years Treated With Dupilumab in A Placebo-Controlled Clinical Trial of Moderate-To-Severe Atopic Dermatitisjennylau0809No ratings yet
- Effect of Amoxicillin Dose and Treatment Duration On The Need For Antibiotic Re-Treatment in Children With Community-Acquired PneumoniaDocument140 pagesEffect of Amoxicillin Dose and Treatment Duration On The Need For Antibiotic Re-Treatment in Children With Community-Acquired Pneumoniajennylau0809No ratings yet
- Check Unit 555 November Immunology V3 PDFDocument25 pagesCheck Unit 555 November Immunology V3 PDFdragon66No ratings yet
- erdle2017Document9 pageserdle2017tesis covidNo ratings yet
- Effectiveness of Regionally-Specific ImunotherapyDocument6 pagesEffectiveness of Regionally-Specific ImunotherapyLarissa AlonsoNo ratings yet
- Preventive Effect of Pleuran Glucan From Pleurotus Ostreatus in Children With Recurrent Respiratory Tract Infections OpenlabelproDocument6 pagesPreventive Effect of Pleuran Glucan From Pleurotus Ostreatus in Children With Recurrent Respiratory Tract Infections OpenlabelproRodolfo DelgadoNo ratings yet
- Choosing Wisely Canada Collection of Lists July 6 2022Document205 pagesChoosing Wisely Canada Collection of Lists July 6 2022Dila KavameNo ratings yet
- Atopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseFrom EverandAtopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseRating: 5 out of 5 stars5/5 (1)
- Pediatric Food Allergy: A Clinical GuideFrom EverandPediatric Food Allergy: A Clinical GuideRuchi S. GuptaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Fast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseFrom EverandFast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseNo ratings yet
- Sarcopenia 2Nd Edition John E Morley Full Download ChapterDocument51 pagesSarcopenia 2Nd Edition John E Morley Full Download Chapterdawn.payne642100% (16)
- Cattle RaisingDocument15 pagesCattle RaisingJoey Dumaluan100% (1)
- A 25yr Old Male Presented With Skin Rash Involving Both Hands and Feet For 2 DaysDocument234 pagesA 25yr Old Male Presented With Skin Rash Involving Both Hands and Feet For 2 DaysAli LashhabNo ratings yet
- Check List For Flood PreparednessDocument10 pagesCheck List For Flood Preparednesssnehakumar275No ratings yet
- HIRARC On Fertilisation - SI - 2022Document6 pagesHIRARC On Fertilisation - SI - 2022noor khairaniNo ratings yet
- Emergency Preparedness For Brgy. PoblacionDocument40 pagesEmergency Preparedness For Brgy. PoblacionMario N. MariNo ratings yet
- ผื่นแพ้ยาDocument26 pagesผื่นแพ้ยาKururin Kookkai KurukuruNo ratings yet
- Mount Litera Zee School: Subject: EVS Class: VDocument3 pagesMount Litera Zee School: Subject: EVS Class: VPrakhar SinghNo ratings yet
- Case Study 2Document6 pagesCase Study 2Rahmani MuharimNo ratings yet
- August 7, 2015 Strathmore Times PDFDocument28 pagesAugust 7, 2015 Strathmore Times PDFStrathmore TimesNo ratings yet
- Hospital Case StudyDocument38 pagesHospital Case Studyanannya jhaNo ratings yet
- Multi-Unit Implant Impression Accuracy: A Review of The LiteratureDocument13 pagesMulti-Unit Implant Impression Accuracy: A Review of The LiteratureRafaela VillamaguaNo ratings yet
- Hypnotics SedDocument13 pagesHypnotics SedSamantha ReyesNo ratings yet
- Amazon FBA Small and Light Program Everything To Know in 2022Document12 pagesAmazon FBA Small and Light Program Everything To Know in 2022natig samedovNo ratings yet
- CM Infant Weighing Scale PPDocument16 pagesCM Infant Weighing Scale PPMani DhamodharanNo ratings yet
- X FEDEX EIDocument13 pagesX FEDEX EINISREEN WAYANo ratings yet
- School Grade Level 9 Teacher Learning Area English Teaching Dates / Time Quarter 2ndDocument5 pagesSchool Grade Level 9 Teacher Learning Area English Teaching Dates / Time Quarter 2ndJOHN CHRISTIAN TAPARANONo ratings yet
- Ha SL PrelimsDocument11 pagesHa SL PrelimsEthel May GranilNo ratings yet
- CPA16: Ingeus-Deloitte - PTD Q&ADocument17 pagesCPA16: Ingeus-Deloitte - PTD Q&AWork_Programme_DWPNo ratings yet
- Acute Appendicitis ReportDocument66 pagesAcute Appendicitis ReportSamantha PaulinoNo ratings yet
- Summer FInal Proof All PagesDocument16 pagesSummer FInal Proof All PagesJRidgellNo ratings yet
- Albrink 1968Document6 pagesAlbrink 1968Guido HerreraNo ratings yet
- Form-12 Accident Report From EmployerDocument2 pagesForm-12 Accident Report From Employersupriya100% (2)
- Wernestrup Syndrome or Variant of Vacterl Association - Case ReportDocument2 pagesWernestrup Syndrome or Variant of Vacterl Association - Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Research ProposalDocument25 pagesResearch ProposaladerindNo ratings yet
- Non-Specific Immune Response, and Resistance To Vibrio Alginolyticus in Pacific White, Chang 2012Document7 pagesNon-Specific Immune Response, and Resistance To Vibrio Alginolyticus in Pacific White, Chang 2012afandi saputraNo ratings yet
- M WM 501rl Pumphead enDocument21 pagesM WM 501rl Pumphead enMarcelo SilvaNo ratings yet
- Essay Writing For ECPE and C2 EFL Exams: Fullspate - 2014Document58 pagesEssay Writing For ECPE and C2 EFL Exams: Fullspate - 2014María Belén ButtilerNo ratings yet
Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva Susanti
Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva Susanti
Uploaded by
danaagus81Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva Susanti
Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva Susanti
Uploaded by
danaagus81Copyright:
Available Formats
Paediatrica Indonesiana
p-ISSN 0030-9311; e-ISSN 2338-476X; Vol.58, No.6(2018). p. 280-5; doi: http://dx.doi.org/10.14238/pi58.6.2018.280-5
Original Article
Immunotherapy and probiotic treatment for allergic
rhinitis in children
Sumadiono1, Cahya Dewi Satria1, Nurul Mardhiah2, Grace Iva Susanti2
A
Abstract llergic respiratory diseases are major health
Background Allergic rhinitis is a global health problem that is in- problems in the pediatric population due
creasing in prevalence. Many kinds of therapy have been tried, such to their high prevalence and chronicity,
as antihistamines, probiotics, and immunotherapy. Immunotherapy
may restore the patient’s normal immunity against the specific al-
as well as the costs for treatment and
lergen, while probiotics may modify the natural course of allergy. effect on quality of life. One of the most important
Objective To evaluate probiotics and immunotherapy for improving risk factors for the development of airway diseases
clinical symptoms of allergic rhinitis. in children and adolescents is atopy.1 This condition
Methods This randomized controlled trial (RCT) involved 64 pa-
tients, aged 3-18 years, and diagnosed with persistent allergic rhinitis predominates during the childhood years, with 25%
in the Department of Child Health, Sardjito General Hospital from classified as having severe allergic rhinitis.2 The
April 2016 until May 2017. Patients were randomly allocated into prevalence of asthma and allergies has increased
three therapy groups: group A (standard therapy/cetirizine only), over the last few decades. Allergic diseases are multi-
group B (standard and probiotic therapy), and group C (standard
therapy and immunotherapy). Clinical symptoms of allergic rhinitis factorial illnesses determined by a complex interplay
including sneezing, rhinorrhea, and itchy nose, were evaluated for 7 between genetic and environmental factors. 3 A
weeks and classified as improved or not improved. The significance prevalence and comorbidity study of allergy in children
of the data was analyzed using proportion test. in our previous study on 2014 revealed that 33.8%
Results Sixty-four patients completed 7 weeks of therapy, 15
subjects in group A, 26 in group B, and 23 in group C. Group C were diagnosed with allergic rhinitis, 17.3% with
showed significantly more improvement of sneezing and rhinor- atopic dermatitis, and 9.1% with asthma.4 House dust
rhea compared to both group A (Z=5.71; Z=7.57, respectively) mites were the most common aeroallergen.5
and group B (Z=2.82; Z=6.90, respectively). However, itchy nose Allergic rhinitis is defined as a type I hypersensiti
was not significantly improved in group C compared to group B
(Z=0.50), but was significantly improved in group C compared vity allergic reaction with the predominance of
to group A (Z=10.91). Group B had significant improvement of Th2 cells and characterized by high IgE levels. 6
sneezing, rhinorrhea, and itchy nose compared to group A (Z=3.81, The standard therapy for allergic rhinitis is second
Z=2.86, and Z=10.91, respectively).
generation antihistamines, but additional therapy
Conclusion The combined standard-immunotherapy group has
significantly superior improvement compared to the combined
standard-probiotic group and the standard therapy group, in terms From the Department of Child Health1 and Department of Public Health
of sneezing and rhinorrhea in children with persistent allergic and Nursing2, Universitas Gadjah Mada Medical, Public Health & Nursing
rhinitis. [Paediatr Indones. 2018;58:280-5; doi: http://dx.doi. School/Dr. Sardjito Hospital, Yogyakarta, Central Java, Indonesia.
org/10.14238/pi58.6.2018.280-5].
Corresponding author: Sumadiono, Department of Child Health,
Universitas Gadjah Mada/Dr. Sardjito Hospital. Jalan Kesehatan No.
Keywords: allergic rhinitis; immunotherapy; 1, Sinduadi, Mlati, Sleman, Special District of Yogyakarta 55281. Telp.
probiotics +6281904186380. Email: smdnygy@gmail.com.
280 • Paediatr Indones, Vol. 58, No. 6, November 2018
Sumadiono et al.: Immunotherapy and probiotic treatment for allergic rhinitis in children
may be needed in persistent or severe cases.7 Probiotic allergic rhinitis and treated as outpatients in the
treatment has a unique, disease-modifying effect, Allergy and Immunology Division, Department of
as it manipulates the normal flora ecosystem in the Child Health, Dr. Sardjito General Hospital. The
gastrointestinal tract, induces the stability of Th1 and inclusion criteria were children aged 3-18 years
Th2 immune responses, and stimulates T-regulators to with persistent allergic rhinitis, at least one positive
inhibit excessive Th1 and Th2 reactivity.8 Probiotic skin prick test result, and parental written informed
supplementation was shown to be beneficial for consent. Diagnoses were based on the 2016 Allergic
decreasing nasal eosinophil percentages in children Rhinitis and Its Impact on Asthma (ARIA) classification
with allergic rhinitis.9 with symptoms present at least 4 days/week for at
Immunotherapy is given with the aim of least 4 weeks.21 We excluded those who did not
modifying the pathogenesis of allergic rhinitis. By complete 7 weeks of therapy, those with unusual
giving increasing amounts of allergens to modify skin prick test results (wide skin lesions or severe
the biological response, long-term tolerance may be dermatographism), antihistamin-dependent,20 and
induced, even after the treatment has ended. This uncooperative patients.
treatment approach has been shown to decrease Subjects were allocated into three groups using a
symptoms and improve quality of life, while being randomized block design and followed up until the 7th
cost-effective for a large number of patients. In week of therapy. The 3 groups were group A (standard
addition, it is considered to be the only treatment therapy/cetirizine only), group B (standard and
that can influence the natural course of the disease probiotic therapy), and group C (standard therapy and
by targeting the cause of the allergic inflammatory immunotherapy). We used cetirizine 10mg as standard
response.9,10 In allergic rhinitis, the effectiveness therapy, a sachet of Protexin® for probiotic and a
of immunotherapy has been demonstrated in many house dust mite allergen with 0.001 concentration
carefully conducted placebo-controlled trials.11 Skin form Pharmacy in Dr. Soetomo General Hospital. The
test sensitivity decreases and allergen-specific IgG improvement of each clinical symptom was evaluated
increases with immunotherapy.12 Immunotherapy by comparing the frequency of the symptom before
has also been demonstrated to be quite effective and after 7 weeks of therapy. The significance of the
in both seasonal and perennial allergic rhinitis.10,13 data was analyzed using the proportion test. The study
Immunotherapy treatment using house dust mite protocol was approved by the Medical Research Ethics
allergen has been used widely in developed countries Committee of the Universitas Gadjah Mada Medical,
for treating allergic rhinitis and asthma, but rarely used Public Health, and Nursing School.
in Indonesia.14,15 The frequency of symptoms has been
used as a predictor of immunotherapy effectiveness in
asthma patients.15 Administration of immunotherapy Results
and probiotic adjuvants can improve clinical scores
and quality of life in asthmatic children, despite a lack A total of 64 subjects aged 3 to 18 years were included
of significant differences in immunological parameters in the study and randomly allocated into three groups:
such as IFNgand eosinophils.17-19 These treatments 15 in group A, 26 in group B, and 23 in group C. Most
may increase the CD4+/CD8+ T-cell ratio as well, subjects were male (10 in group A, 16 in group B, and
which may lead to remarkable improvement of clinical 16 in group C). The subjects were predominantly
symptoms in asthmatic children.14 This study aimed to between 3 and 12 years of age in group A (12) and
evaluate probiotics and immunotherapy for improving group B (20), but group C subjects were mostly
clinical symptoms of allergic rhinitis. >12-18 years of age. Most subjects had a history
allergic rhinitis prior to the study, with symptoms of
sneezing, rhinorrhea, and itchy nose. The baseline
Methods characteristics of subjects are shown in Table 1.
The improvement of each clinical symptom was
This RCT was conducted from April 2016 to May evaluated by comparing the frequency before and after
2017, on subjects who were diagnosed with persistent the 7th week of therapy. The comparisons of clinical
Paediatr Indones, Vol. 58, No. 6, November 2018 • 281
Sumadiono et al.: Immunotherapy and probiotic treatment for allergic rhinitis in children
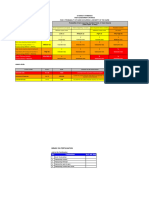
Table 1. Baseline characteristics of study subjects
Characteristics Group A Group B Group C
(n=15) (n=26) (n=23)
Sex, n
Male 10 16 16
Female 5 10 7
Age, n
3-12 years 12 20 10
>12-18 years 3 6 13
Nutritional status, n
Underweight 0 1 1
Normal 15 21 21
Overweight 0 4 1
History of sneezing, n
Present 12 24 23
Not present 3 2 0
History of rhinorrhea, n
Present 10 19 20
Not present 5 7 3
History of itchy nose, n
Present 8 20 18
Not present 7 6 5
History of atopy, n
Present 12 22 18
Not present 3 4 5
Table 2. Clinical symptom improvement after 7 weeks of therapy in the
standard vs. combined standard-probiotic (groups A and B)
Parameter Standard (A) Standard+probiotic Z score
(n=15) (n=26)
Sneezing, n
Improved 9 18 3.81
Not improved 6 8
Rhinorrhea, n
Improved 10 19 2.86
Not improved 5 7
Itchy nose, n
Improved 7 19 10.91
Not improved 8 7
symptom improvement between groups are shown in 18/26 group B (Z=2.82); rhinorrhea: 19/23 group C
Tables 2, 3, and 4. Table 2 shows that group B had vs. 19/26 group B (Z=6.90)]. However, while itchy
significantly improved clinical symptoms compared nose symptoms showed vast improvement in both
to group A. Sneezing improved in 18/26 of subjects groups B and C, there was no significant difference
in group B vs. 9/15 in group A (Z=3.81). Rhinorrhea between groups, with 17/23 of group C vs. 19/26 of
improved in 19/26 of subjects in group B vs. 10/15 in group B showing improvements (Z=0.50).
group A (Z=2.86). Itchy nose improved in 19/26 of Table 4 shows the clinical symptom improve
group b vs. 7/15 in group A (Z=10.91). ments between groups A and C. Group C had
Table 3 shows that clinical symptoms of sneezing significantly more improvement of clinical symptoms
and rhinorrhea significantly improved in group C compared to group A [sneezing: 17/23 group C vs.
compared to group B [sneezing: 17/23 group C vs. 9/15 group A (Z=5.71); rhinorrhea: 19/23 group C
282 • Paediatr Indones, Vol. 58, No. 6, November 2018
Sumadiono et al.: Immunotherapy and probiotic treatment for allergic rhinitis in children
Table 3. Clinical symptom improvement after 7 weeks of therapy in the combined standard-
probiotic vs. combined standard-immunotherapy (groups B and C)
Parameter Standard+probiotic (B) Standard+immunotherapy (C) Z score
(n=26) (n=23)
Sneezing, n
Improved 18 17 2.82
Not improved 8 6
Rhinorrhea, n
Improved 19 19 6.90
Not improved 7 4
Itchy nose, n
Improved 19 17 0.50
Not improved 7 6
Table 4. Clinical symptom improvement after 7 weeks of therapy in the standard vs.
combined standard-immunotherapy (groups A and C)
Parameter Standard (A) Standard+immunotherapy (C) Z score
(n=15) (n=23)
Sneezing, n
Improved 9 17 5.71
Not improved 6 6
Rhinorrhea, n
Improved 10 19 7.57
Not improved 5 4
Itchy nose, n
Improved 7 17 10.91
Not improved 8 6
vs. 10/15 group A (Z=7.57); itchy nose: 17/23 group Similar study was done as well by Palma-Carlos et al.
C vs. 7/15 group A (Z=10.91)]. and showed significant improvement of rhinorrhea,
sneezing, and conjunctivitis compared with placebo
after one year therapy.24
Discussion Probiotic are beneficial microbes that give benefit
to the host, such as normalize the dysbiotic microbiota,
Children with persistent allergic rhinitis who received which will associate with immunopathology.9 It is
standard (antihistamine) therapy combined with described in a review by Hardy et al. in 2013 that probiotic
immunotherapy had significantly superior improvement has the ability as immunomodulatory on the cells,
of sneezing and rhinorrhea compared to those who molecules and immune response in the gut mucosae.7
received standard therapy combined with probiotics, Subcutaneous injection immunotherapy has been
and those who received standard therapy alone. demonstrated to be efficacacious in the management
Similarly, an RCT by Karakoc-Aydiner et al. concluded of allergic rhinitis and asthma, even in multi-allergen
that house dust mite-sensitized children with asthma situations. This therapy has been effective in the
and/or rhinitis treated with either subcutaneous prevention of new sensitizations and progression of
injection immunotherapy or sublingual immunotherapy rhinitis to asthma.13 Immunotherapy acts on the T
showed better clinical outcome improvements than helper cells type 1 (Th1/Th2) axis to shift the T cell
children who got antihistamine alone.22 Another phenotype away from the allergic Th2 phenotype. More
study by Smith et al. in 2004 also showed significant recently, some evidence has emerged to suggest that
improvement of reduction in runny nose and sneezing immunotherapy may promote regulatory T cells action
compared between immunotherapy and placebo.23 in attenuating allergic symptoms.10
Paediatr Indones, Vol. 58, No. 6, November 2018 • 283
Sumadiono et al.: Immunotherapy and probiotic treatment for allergic rhinitis in children
From our study, we conclude that immuno nutritional intake with fat content of Indonesian mothers’
therapy combined with antihistamine has better breast milk. Paediatr Indones. 2016;56:298-304.
improvement compared with antihistamine only or 10. Leung DYM, Szefler SJ, Bonilla FA, Akdis CA, Sampson HA.
antihistamine with probiotic. Pediatric allergy: principles and practice. 3rd ed. Edinburgh:
Elsevier; 2016. p.179.
11. Jacobsen L, Wahn U, Bilo MB. Allergen-specific immuno
Conflict of Interest therapy provides immediate, long-term and preventive
clinical effects in children and adults: the effects of
None declared. immunotherapy can be categorised by level of benefit -the
centenary of allergen specific subcutaneous immunotherapy.
Clin Transl Allergy. 2012;2:8.
Funding 12. Song Y, Long J, Wang T, Xie J, Wang M, Tan G. Long-term
efficacy of standardised specific subcutaneous immuno
This work was supported by “Dana Masyarakat” Funding from therapy in children with persistent allergic rhinitis due to
Universitas Gadjah Mada Medical, Public Health, and Nursing multiple allergens including house dust mites. J Laryngol
School. Otol. 2018;132:230-235.
13. El-sayed ZA, El-farghali OG. Allergen-specific immuno
therapy in children. Egyptian Journal of Pediatric Allergy
References and Immunology .2012;10:55-66.
14. Fattory H, Endharti AT, Barlianto W, Olivianto E, Kusuma
1. Mir E, Panjabi C, Shah A. Impact of allergic rhinitis in school HMSC. Efek imunoterapi, probiotik, Nigella sativa terhadap
going children. Asia Pac Allergy. 2012;2:93. rasio CD4+/CD8+, kadar imunoglobulin E, dan skoring
2. Cantani A. Allergic rhinitis. In: Heilmann U, editor. Pediatric asma. J Kedokt Brawijaya. 2015;28:328-33.
allergy, asthma and immunology. Berlin-Heidelberg: Springer- 15. Ratih I, Olivianto E, Barlianto W, Kusuma HMSC. Pengaruh
Verlag; 2008. p. 875-910. imunoterapi, probiotik dan jinten hitam terhadap CD4+IFNg
3. von Mutius E. Epidemiology of allergic diseases. In: Leung CD4 IFN, eosinofil, dan skor asma. J Kedokteran Brawijaya.
D, editor. Pediatric allergy: principles and practice. 2nd ed. 2015;28:187-94.
Edinburgh: Elsevier; 2010 p. 1-8. 16. Endaryanto A, Hikmah Z, Harsono A. Use of superoxide
4. Dina F, Satria CD, Sumadiono. Karakteristik klinis dan dismutase in accelerating symptom relief in asthmatic and
sensitisasi alergen pada anak dengan rinitis alergi di house dust mite allergic children receiving house dust mite
Yogyakarta [thesis]. [Yogyakarta]: Fakultas Kedokteran immunotherapy. Int J Integr Heal Sci. 2015;3:72-8.
Universitas Gadjah Mada; 2016. 17. Muhyi A, Barlianto W, Kuksuma HMSC. Efek pemberian
5. Raulf M, Bergmann KC, Kull S, Sander I, Hilger C, Bruning imunoterapi, probiotik, Nigella sativa terhadap Th17,
T, et al. Mites and other indoor allergens - from exposure to neutrofil, dan skoring asma. J Kedokt Brawijaya. 2015; 28:
sensitization and treatment. Allergo J Int. 2015; 24: 68-80. 334-9.
6. Deo SS, Mistry KJ, Kakade AM, Niphadkar PV. Role played 18. Nucifera C, Olivianto E, Barlianto W, Chandra HMS.
by Th2 type cytokines in IgE mediated allergy and asthma. Jumlah CD4+IL-5+, CD8+IL-5+, dan perbaikan kualitas
Lung India. 2010;27:66-71. hidup setelah pemberian probiotik dan Nigella sativa pada
7. Recto MT, Gabriel MT, Kulthanan K, Tantilipikorn P, Aw anak asma dengan imunoterapi fase rumatan. Sari Pediatri.
DC, Lee TH, et al. Selecting optimal second-generation 2015;16:379-84.
antihistamines for allergic rhinitis and urticaria in Asia. Clin 19. Endaryanto A, Irmawati M. Enhanced efficacy of sublingual
Mol Allergy. 2017;15:19. immunotherapy in childhood allergic asthma by probiotics.
8. Hardy H, Harris J, Lyon E, Beal J, Foey AD. Probiotics, Folia Medica Indonesiana. 2018;54:64-74.
prebiotics and immunomodulation of gut mucosal defences: 20. Hansen TK. Skin prick testing skin testing. 2006; 58: 1-5.
homeostasis and immunopathology. Nutrients. 2013; 29: 21. Brozek JL, Bousquet J, Agache I, Agarwal A, Bachert C,
1869-912. Bosnic-Anticevich S, et al. Allergic Rhinitis and its impact
9. Kurniati AM, SUnardi D, SUngkar A, Bardosono S, on Asthma (ARIA) Guidelines - 2016 Revision. J Allergy
Kartinah NT. Associations of maternal body composition and Clin Immunol. 2017;140: 950-8.
284 • Paediatr Indones, Vol. 58, No. 6, November 2018
Sumadiono et al.: Immunotherapy and probiotic treatment for allergic rhinitis in children
22. Smith H, White P, Annila I, Poole J, Andre C, Frew A. blind, placebo-controlled study. Clinical Allergy Immunology
Randomized controlled trial of high-dose sublingual Center. CAIC. 2006;34:195–8.
immunotherapy to treat seasonal allergic Rinitis. Journal of 24. Karakoc-Aydiner E, Eifan AO, Baris S, Gunay E, Akturk
Allergy and Clinical Immunology. 2004;114:831-7. H, Akkoc T, et al. Long-term effect of sSublingual and
23. Palma-Carlos AG, Santos AS, Branco-Ferreira M, Pregal subcutaneous immunotherapy in dust mite-allergic
AL, Palma-Carlos ML, Bruno ME, et al. Clinical efficacy and children with asthma/rhinitis: A 3-year prospective
safety of preseasonal sublingual immunotherapy with grass randomized controlled trial. J Investig Allergol Clin Immunol.
pollen carbamylated allergoid in rhinitic patient. double- 2015;25:334-42.
Paediatr Indones, Vol. 58, No. 6, November 2018 • 285
You might also like
- Michael Grant Anaesthetics Emergency Medicine Notes PDFDocument70 pagesMichael Grant Anaesthetics Emergency Medicine Notes PDFMimansaDixit100% (1)
- ChorioretinitisDocument13 pagesChorioretinitisrada tri rosi kurniaNo ratings yet
- Diagnosis AndtreatmentofallergicrhinitisinchildrenDocument6 pagesDiagnosis AndtreatmentofallergicrhinitisinchildrenIRANo ratings yet
- New Schatz2018 OldDocument44 pagesNew Schatz2018 Oldabhijeet abhijeetNo ratings yet
- New Schatz2018Document44 pagesNew Schatz2018abhijeet abhijeetNo ratings yet
- 011AADocument8 pages011AAAtef AlbooqNo ratings yet
- Probiotic Therapy On Children With Allergic RhinitisDocument4 pagesProbiotic Therapy On Children With Allergic RhinitisSus Retha Mona ArdianiNo ratings yet
- Schatz 2018Document44 pagesSchatz 2018abhijeet abhijeetNo ratings yet
- Ijerph 12 10984 v2Document11 pagesIjerph 12 10984 v2Nurjanah PutriNo ratings yet
- Allergic Rhinitis in ChildrenDocument7 pagesAllergic Rhinitis in ChildrenTina MorleyNo ratings yet
- Efficacy of Probiotic in Perennial Allergic Rhinitis Under Five Year Children: A Randomized Controlled TrialDocument6 pagesEfficacy of Probiotic in Perennial Allergic Rhinitis Under Five Year Children: A Randomized Controlled TrialBezoNo ratings yet
- Pi Is 1081120622006536Document11 pagesPi Is 1081120622006536Niken KuncorowatiNo ratings yet
- Allergen Immunotherapy Expert ExchangeDocument4 pagesAllergen Immunotherapy Expert ExchangeAnna LiachenkoNo ratings yet
- Out 4Document3 pagesOut 4Musthafa Afif WardhanaNo ratings yet
- Medical News in The World of Atopic Dermatitis First Quarter 2016Document5 pagesMedical News in The World of Atopic Dermatitis First Quarter 2016anon_384025255No ratings yet
- Perbedaan Imunoterapi Alergen Spesifik (ITS) Dengan Vaksinasi BCG Dalam Meningkatkan Kualitas Hidup Penderita Rinitis AlergiDocument12 pagesPerbedaan Imunoterapi Alergen Spesifik (ITS) Dengan Vaksinasi BCG Dalam Meningkatkan Kualitas Hidup Penderita Rinitis AlergiThya Alif KahfNo ratings yet
- Sublingual Immunotherapy To House Dust Mite in Pediatric Patients With Allergic Rhinitis and Asthma: A Retrospective Analysis of Clinical Course Over A 3-Year Follow-Up PeriodDocument4 pagesSublingual Immunotherapy To House Dust Mite in Pediatric Patients With Allergic Rhinitis and Asthma: A Retrospective Analysis of Clinical Course Over A 3-Year Follow-Up PeriodPeter SalimNo ratings yet
- Research ArticleDocument6 pagesResearch ArticleReffy AdhaNo ratings yet
- Vitamin D Deficiency and Its Relation To Allergic Diseases A Cross Sectional Study Among Allergic Patients From Jeddah City Saudi ArabiaDocument17 pagesVitamin D Deficiency and Its Relation To Allergic Diseases A Cross Sectional Study Among Allergic Patients From Jeddah City Saudi ArabiaAthenaeum Scientific PublishersNo ratings yet
- Comparison of Sublingual Immunotherapy in Patients With Allergic Rhinitis Sensitive To House Dust Mites in KoreaDocument8 pagesComparison of Sublingual Immunotherapy in Patients With Allergic Rhinitis Sensitive To House Dust Mites in Koreafm_askaNo ratings yet
- Nutrients 10 01678Document11 pagesNutrients 10 01678zulfa nadiaNo ratings yet
- Probiotics in Late Infancy Reduce The Incidence of Eczema: A Randomized Controlled TrialDocument6 pagesProbiotics in Late Infancy Reduce The Incidence of Eczema: A Randomized Controlled TrialarditaNo ratings yet
- Effect of Oral Vitamin E On Atopic DermatitisDocument4 pagesEffect of Oral Vitamin E On Atopic DermatitisYusufTaqwaMuladiNo ratings yet
- Probioticos Rinitis AlergicaDocument8 pagesProbioticos Rinitis AlergicaFlavio GuillenNo ratings yet
- Diagnosing Allergic Rhinitis - Is There A Need?Document3 pagesDiagnosing Allergic Rhinitis - Is There A Need?Alfa Suryani ArdliNo ratings yet
- Nurmatov Et Al-2012-Cochrane Database of Systematic ReviewsDocument4 pagesNurmatov Et Al-2012-Cochrane Database of Systematic ReviewsfiskaderishaNo ratings yet
- Andosan™-An Anti-Allergic and Anti-Inflammatory Ingredient Prepared From Agaricus Blazei MushroomDocument11 pagesAndosan™-An Anti-Allergic and Anti-Inflammatory Ingredient Prepared From Agaricus Blazei MushroomMartinaNo ratings yet
- Evaluation of Six Years Allergen ImmunotherapyDocument12 pagesEvaluation of Six Years Allergen ImmunotherapyArifin I. OputuNo ratings yet
- Sintha nug,+6.+CR+5+-+RAZIV+FINISHDocument7 pagesSintha nug,+6.+CR+5+-+RAZIV+FINISHFyiaaa02No ratings yet
- Pharmacoeconomics of allergy immunotherapy versus pharmacotherapyDocument14 pagesPharmacoeconomics of allergy immunotherapy versus pharmacotherapyjladinoNo ratings yet
- 1 s2.0 S1684118218301816 Main PDFDocument28 pages1 s2.0 S1684118218301816 Main PDFPrasetyaNo ratings yet
- Allergy - 2022 - Farraia - Allergen Immunotherapy For Asthma Prevention A Systematic Review and Meta Analysis ofDocument17 pagesAllergy - 2022 - Farraia - Allergen Immunotherapy For Asthma Prevention A Systematic Review and Meta Analysis ofpedrotiagosilvaNo ratings yet
- Prevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisDocument6 pagesPrevalence of Allergic Rhinitis Symptoms and Positive Skin Prick Test Results in Children With Recurrent EpistaxisKevinFeraldyNo ratings yet
- DermatitisDocument6 pagesDermatitisAmalia Zulfa AmandaNo ratings yet
- High-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialDocument15 pagesHigh-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialHendra EfendiNo ratings yet
- Probiotics in Pregnant Women To Prevent Allergic Disease: A Randomized, Double-Blind TrialDocument8 pagesProbiotics in Pregnant Women To Prevent Allergic Disease: A Randomized, Double-Blind TrialarditaNo ratings yet
- Probiotics For The Prevention of Allergy A Systematic ReviewDocument10 pagesProbiotics For The Prevention of Allergy A Systematic ReviewadhyNo ratings yet
- The Efficiency and Safety of Olopatadine Against Rupatadine in Chronic Urticaria of Idiopathic Origin: A Comparative StudyDocument6 pagesThe Efficiency and Safety of Olopatadine Against Rupatadine in Chronic Urticaria of Idiopathic Origin: A Comparative StudyArezoo JamNo ratings yet
- Probiotic Allergic RhinitsDocument7 pagesProbiotic Allergic Rhinitscharoline gracetiani nataliaNo ratings yet
- PIIS1939455119301723Document5 pagesPIIS1939455119301723Yeol LoeyNo ratings yet
- Treatment of Allergic Rhinitis: DENISE K. SUR, MD, and STEPHANIE SCANDALE, MD, David Geffen School of MedicineDocument7 pagesTreatment of Allergic Rhinitis: DENISE K. SUR, MD, and STEPHANIE SCANDALE, MD, David Geffen School of MedicineM Isyhaduul IslamNo ratings yet
- Atopic DermatitisDocument5 pagesAtopic DermatitisUlung PrayogoNo ratings yet
- IgM Pada ThypoidDocument4 pagesIgM Pada ThypoidririlibertiNo ratings yet
- Abrahamsson 2013Document6 pagesAbrahamsson 2013Anja LjiljaNo ratings yet
- Clinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiaDocument6 pagesClinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiamariaprincesitaNo ratings yet
- Jurnal THTDocument14 pagesJurnal THTLaras Asri FatahaniNo ratings yet
- Jurnal RhinitisDocument6 pagesJurnal RhinitisdwiNo ratings yet
- Sinovac 3Document7 pagesSinovac 3Lukas ZamudioNo ratings yet
- Sublingual ImmunotherapyDocument4 pagesSublingual ImmunotherapyAnonymous eZqDZbObRiNo ratings yet
- Use of Superoxide Dismutase in Accelerating Symptom PDFDocument7 pagesUse of Superoxide Dismutase in Accelerating Symptom PDFWilliam JavierNo ratings yet
- Infections in Children Aged 6 Months To 5 Years Treated With Dupilumab in A Placebo-Controlled Clinical Trial of Moderate-To-Severe Atopic DermatitisDocument11 pagesInfections in Children Aged 6 Months To 5 Years Treated With Dupilumab in A Placebo-Controlled Clinical Trial of Moderate-To-Severe Atopic Dermatitisjennylau0809No ratings yet
- Effect of Amoxicillin Dose and Treatment Duration On The Need For Antibiotic Re-Treatment in Children With Community-Acquired PneumoniaDocument140 pagesEffect of Amoxicillin Dose and Treatment Duration On The Need For Antibiotic Re-Treatment in Children With Community-Acquired Pneumoniajennylau0809No ratings yet
- Check Unit 555 November Immunology V3 PDFDocument25 pagesCheck Unit 555 November Immunology V3 PDFdragon66No ratings yet
- erdle2017Document9 pageserdle2017tesis covidNo ratings yet
- Effectiveness of Regionally-Specific ImunotherapyDocument6 pagesEffectiveness of Regionally-Specific ImunotherapyLarissa AlonsoNo ratings yet
- Preventive Effect of Pleuran Glucan From Pleurotus Ostreatus in Children With Recurrent Respiratory Tract Infections OpenlabelproDocument6 pagesPreventive Effect of Pleuran Glucan From Pleurotus Ostreatus in Children With Recurrent Respiratory Tract Infections OpenlabelproRodolfo DelgadoNo ratings yet
- Choosing Wisely Canada Collection of Lists July 6 2022Document205 pagesChoosing Wisely Canada Collection of Lists July 6 2022Dila KavameNo ratings yet
- Atopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseFrom EverandAtopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseRating: 5 out of 5 stars5/5 (1)
- Pediatric Food Allergy: A Clinical GuideFrom EverandPediatric Food Allergy: A Clinical GuideRuchi S. GuptaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Fast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseFrom EverandFast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseNo ratings yet
- Sarcopenia 2Nd Edition John E Morley Full Download ChapterDocument51 pagesSarcopenia 2Nd Edition John E Morley Full Download Chapterdawn.payne642100% (16)
- Cattle RaisingDocument15 pagesCattle RaisingJoey Dumaluan100% (1)
- A 25yr Old Male Presented With Skin Rash Involving Both Hands and Feet For 2 DaysDocument234 pagesA 25yr Old Male Presented With Skin Rash Involving Both Hands and Feet For 2 DaysAli LashhabNo ratings yet
- Check List For Flood PreparednessDocument10 pagesCheck List For Flood Preparednesssnehakumar275No ratings yet
- HIRARC On Fertilisation - SI - 2022Document6 pagesHIRARC On Fertilisation - SI - 2022noor khairaniNo ratings yet
- Emergency Preparedness For Brgy. PoblacionDocument40 pagesEmergency Preparedness For Brgy. PoblacionMario N. MariNo ratings yet
- ผื่นแพ้ยาDocument26 pagesผื่นแพ้ยาKururin Kookkai KurukuruNo ratings yet
- Mount Litera Zee School: Subject: EVS Class: VDocument3 pagesMount Litera Zee School: Subject: EVS Class: VPrakhar SinghNo ratings yet
- Case Study 2Document6 pagesCase Study 2Rahmani MuharimNo ratings yet
- August 7, 2015 Strathmore Times PDFDocument28 pagesAugust 7, 2015 Strathmore Times PDFStrathmore TimesNo ratings yet
- Hospital Case StudyDocument38 pagesHospital Case Studyanannya jhaNo ratings yet
- Multi-Unit Implant Impression Accuracy: A Review of The LiteratureDocument13 pagesMulti-Unit Implant Impression Accuracy: A Review of The LiteratureRafaela VillamaguaNo ratings yet
- Hypnotics SedDocument13 pagesHypnotics SedSamantha ReyesNo ratings yet
- Amazon FBA Small and Light Program Everything To Know in 2022Document12 pagesAmazon FBA Small and Light Program Everything To Know in 2022natig samedovNo ratings yet
- CM Infant Weighing Scale PPDocument16 pagesCM Infant Weighing Scale PPMani DhamodharanNo ratings yet
- X FEDEX EIDocument13 pagesX FEDEX EINISREEN WAYANo ratings yet
- School Grade Level 9 Teacher Learning Area English Teaching Dates / Time Quarter 2ndDocument5 pagesSchool Grade Level 9 Teacher Learning Area English Teaching Dates / Time Quarter 2ndJOHN CHRISTIAN TAPARANONo ratings yet
- Ha SL PrelimsDocument11 pagesHa SL PrelimsEthel May GranilNo ratings yet
- CPA16: Ingeus-Deloitte - PTD Q&ADocument17 pagesCPA16: Ingeus-Deloitte - PTD Q&AWork_Programme_DWPNo ratings yet
- Acute Appendicitis ReportDocument66 pagesAcute Appendicitis ReportSamantha PaulinoNo ratings yet
- Summer FInal Proof All PagesDocument16 pagesSummer FInal Proof All PagesJRidgellNo ratings yet
- Albrink 1968Document6 pagesAlbrink 1968Guido HerreraNo ratings yet
- Form-12 Accident Report From EmployerDocument2 pagesForm-12 Accident Report From Employersupriya100% (2)
- Wernestrup Syndrome or Variant of Vacterl Association - Case ReportDocument2 pagesWernestrup Syndrome or Variant of Vacterl Association - Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Research ProposalDocument25 pagesResearch ProposaladerindNo ratings yet
- Non-Specific Immune Response, and Resistance To Vibrio Alginolyticus in Pacific White, Chang 2012Document7 pagesNon-Specific Immune Response, and Resistance To Vibrio Alginolyticus in Pacific White, Chang 2012afandi saputraNo ratings yet
- M WM 501rl Pumphead enDocument21 pagesM WM 501rl Pumphead enMarcelo SilvaNo ratings yet
- Essay Writing For ECPE and C2 EFL Exams: Fullspate - 2014Document58 pagesEssay Writing For ECPE and C2 EFL Exams: Fullspate - 2014María Belén ButtilerNo ratings yet