Professional Documents
Culture Documents
Hemodialysis Unit Preparedness During and After Covid 19 Pandemic
Hemodialysis Unit Preparedness During and After Covid 19 Pandemic
Uploaded by
yanuar esthoCopyright:
Available Formats
You might also like
- NURSING CARE PLAN Risk For InfectionDocument3 pagesNURSING CARE PLAN Risk For InfectionEvelyn Lampios100% (1)
- MCNDocument23 pagesMCNJASTINE NICOLE SABORNIDONo ratings yet
- When To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsDocument9 pagesWhen To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsepraetorianNo ratings yet
- Shivan Sarna 10 Signs Your Mouth Could Be Making You SickDocument13 pagesShivan Sarna 10 Signs Your Mouth Could Be Making You SickViolet VioletNo ratings yet
- FMEA Audits - Why Do We Need Them?: Empirical Ranking of A FMEADocument2 pagesFMEA Audits - Why Do We Need Them?: Empirical Ranking of A FMEAyanuar esthoNo ratings yet
- 10 1016@j Breast 2020 04 006Document9 pages10 1016@j Breast 2020 04 006Alberto AlexandruNo ratings yet
- COVIDDocument9 pagesCOVIDryan smithNo ratings yet
- Global Guidance For Surgical Care During The COVID-19 PandemicDocument7 pagesGlobal Guidance For Surgical Care During The COVID-19 PandemicSergio Losada AmayaNo ratings yet
- Covid 19 ProgramDocument12 pagesCovid 19 ProgramBAGUIO CATSNo ratings yet
- Scope and LimitationsDocument4 pagesScope and LimitationsRey Dela PeñaNo ratings yet
- Mitigating Risk of COVID-19 in Dialysis Facilities: Alan S. Kliger and Jeffrey SilberzweigDocument3 pagesMitigating Risk of COVID-19 in Dialysis Facilities: Alan S. Kliger and Jeffrey SilberzweigRChofiyana OchiNo ratings yet
- Mitigating Isolation Study 2021.12.23.21268326v1.fullDocument10 pagesMitigating Isolation Study 2021.12.23.21268326v1.fullmart0830No ratings yet
- World Health Organization (WHO) Information Note Tuberculosis and COVID-19Document10 pagesWorld Health Organization (WHO) Information Note Tuberculosis and COVID-19WasimNo ratings yet
- Coronavirus Disease 2019 (Covid-19) and Hiv: Key Issues and ActionsDocument8 pagesCoronavirus Disease 2019 (Covid-19) and Hiv: Key Issues and ActionsnasratullahNo ratings yet
- Patient Management During COVID 19 AsrmDocument10 pagesPatient Management During COVID 19 AsrmDivisi FER MalangNo ratings yet
- Kidney InternationalDocument5 pagesKidney InternationalZara AkbariNo ratings yet
- COVID-19 Maternity Services TB Package UPDATE 2 14072020 SBZDocument58 pagesCOVID-19 Maternity Services TB Package UPDATE 2 14072020 SBZSalomeNo ratings yet
- COVID-19 Global Pandemic: Options For Management of Gynecologic CancersDocument4 pagesCOVID-19 Global Pandemic: Options For Management of Gynecologic CancersMuhammad FaisalNo ratings yet
- Goh2020 Article PreparingYourIntensiveCareUnitDocument19 pagesGoh2020 Article PreparingYourIntensiveCareUnitBAGUIO CATSNo ratings yet
- Covid-19: Guide On Home-Based Care, Screening & Isolation Ward Set UpDocument9 pagesCovid-19: Guide On Home-Based Care, Screening & Isolation Ward Set Upvimalraj vtNo ratings yet
- PIIS0003999320302951Document3 pagesPIIS0003999320302951Adiel CarrascoNo ratings yet
- Approaches To The Management of Patients in Oral and Maxillofacial Surgery During COVID-19 PandemicDocument21 pagesApproaches To The Management of Patients in Oral and Maxillofacial Surgery During COVID-19 PandemicYahul MazfarNo ratings yet
- Apexa NO 8Document5 pagesApexa NO 8Apexa YadavNo ratings yet
- Minimally Invasive Urologic Surgery Is Safe During COVID 19: Experience From Two High Volume Centers in ItalyDocument3 pagesMinimally Invasive Urologic Surgery Is Safe During COVID 19: Experience From Two High Volume Centers in ItalyMasrun FatanahNo ratings yet
- The Pandemic Hits Us Hard, But We Don't Lose HopeDocument4 pagesThe Pandemic Hits Us Hard, But We Don't Lose HopeLasa SiahaanNo ratings yet
- PCX - ReportDocument16 pagesPCX - Reportgowtham thakutNo ratings yet
- PCX - ReportDocument16 pagesPCX - Reportgowtham thakutNo ratings yet
- The Journal For Nurse PractitionersDocument5 pagesThe Journal For Nurse Practitionersagstri lestariNo ratings yet
- Research Paper For The Effectivity of Ultraviolet Lights in Containing COVID-19Document6 pagesResearch Paper For The Effectivity of Ultraviolet Lights in Containing COVID-19Angelyn MarquezNo ratings yet
- Guidance On The Use of Personal Protective Equipment Ppe in Hospitals During The Covid 19 OutbreakDocument9 pagesGuidance On The Use of Personal Protective Equipment Ppe in Hospitals During The Covid 19 OutbreakGerlan Madrid MingoNo ratings yet
- National Guidance For The Recovery of Elective Surgery in ChildrenDocument50 pagesNational Guidance For The Recovery of Elective Surgery in ChildrenJulia RamirezNo ratings yet
- Safari - 12 May 2020 10.04Document1 pageSafari - 12 May 2020 10.04tenun witaNo ratings yet
- First Case Report of A Successfully Managed Severe COVID-19 Infectionin MalawiDocument4 pagesFirst Case Report of A Successfully Managed Severe COVID-19 Infectionin MalawiYoga PrabawaNo ratings yet
- Ijgo 13868Document8 pagesIjgo 13868rutujaNo ratings yet
- Ivermectin Interest Group v4Document41 pagesIvermectin Interest Group v4SundayTimesZA100% (1)
- American Society For Reproductive Medicine (Asrm) Patient Management and Clinical Recommendations During The Coronavirus (Covid-19) PandemicDocument8 pagesAmerican Society For Reproductive Medicine (Asrm) Patient Management and Clinical Recommendations During The Coronavirus (Covid-19) PandemicIoana Adina RugescuNo ratings yet
- Manejo Ambulatorio AdultosDocument18 pagesManejo Ambulatorio AdultosCarlos Huaman ZevallosNo ratings yet
- Ajbsr MS Id 001564Document3 pagesAjbsr MS Id 001564Rodrigo AlpizarNo ratings yet
- NOTTO Transplant Specific Guidelines With Reference To COVID-19Document5 pagesNOTTO Transplant Specific Guidelines With Reference To COVID-19Ashish MishraNo ratings yet
- Ajt.15876 NefroDocument7 pagesAjt.15876 Nefrobrissa senraNo ratings yet
- Covid19 - Physiotherapy - Management - Information - GuidanceDocument13 pagesCovid19 - Physiotherapy - Management - Information - GuidanceMasrov TukirovNo ratings yet
- Covid-19: Guide On Home-Based Care, Screening & Isolation Ward Set UpDocument9 pagesCovid-19: Guide On Home-Based Care, Screening & Isolation Ward Set UpTech Person 03No ratings yet
- © The Author(s) 2020. Published by Oxford University Press For The Infectious Diseases Society ofDocument13 pages© The Author(s) 2020. Published by Oxford University Press For The Infectious Diseases Society ofMastifa HanasitaNo ratings yet
- Preparing Your Intensive Care Unit For The COVID-19 Pandemic: Practical Considerations and StrategiesDocument12 pagesPreparing Your Intensive Care Unit For The COVID-19 Pandemic: Practical Considerations and Strategiesririn puspasariNo ratings yet
- LKS Virus CoronaDocument4 pagesLKS Virus Coronauciha.irfan80No ratings yet
- Teknik Resus BosaertDocument13 pagesTeknik Resus BosaertDADASDSANo ratings yet
- Maximizing The Calm Before The Storm: Tiered Surgical Response Plan For Novel Coronavirus (COVID-19)Document31 pagesMaximizing The Calm Before The Storm: Tiered Surgical Response Plan For Novel Coronavirus (COVID-19)drwagnerzaoNo ratings yet
- Guidance For Maternal Medicine Services in The Evolving Coronavirus (COVID-19) PandemicDocument46 pagesGuidance For Maternal Medicine Services in The Evolving Coronavirus (COVID-19) Pandemicadamu mohammadNo ratings yet
- Guidance For Return To Practice For Otolaryngology-Head and Neck SurgeryDocument10 pagesGuidance For Return To Practice For Otolaryngology-Head and Neck SurgeryLeslie Lindsay AlvarezNo ratings yet
- Brief Guideline For The Prevention of COVID-19Document8 pagesBrief Guideline For The Prevention of COVID-19wkzw779bxpNo ratings yet
- Lembar Kerja Peserta Didik Covid19Document6 pagesLembar Kerja Peserta Didik Covid19faraa dydasyrNo ratings yet
- COVID-19 - Infection Control For Persons With SARS-CoV-2 Infection - UpToDateDocument35 pagesCOVID-19 - Infection Control For Persons With SARS-CoV-2 Infection - UpToDateDuy Hùng HoàngNo ratings yet
- Sahwa Aisya SafitriDocument21 pagesSahwa Aisya SafitriSahwa Aisyah safitriNo ratings yet
- Lembar Kerja Siswa Virus CoronaDocument18 pagesLembar Kerja Siswa Virus CoronaChintiya PutriNo ratings yet
- LEMBAR KERJA SISWA Virus Corona OKDocument12 pagesLEMBAR KERJA SISWA Virus Corona OKAbdee74% (19)
- LEMBAR KERJA SISWA Virus Corona Salma Hamidah X Akl4Document16 pagesLEMBAR KERJA SISWA Virus Corona Salma Hamidah X Akl4Salma MuthmainahNo ratings yet
- Tugas BKDocument14 pagesTugas BKshakila azzaNo ratings yet
- (24!03!2020) LKS Pembelajaran Virus Corona Nisrina Nabila Azzahra X-TEI SMK PiramidaDocument43 pages(24!03!2020) LKS Pembelajaran Virus Corona Nisrina Nabila Azzahra X-TEI SMK PiramidaUne NuneNo ratings yet
- LEMBAR KERJA SISWA Fenny SA Virus Corona OKDocument20 pagesLEMBAR KERJA SISWA Fenny SA Virus Corona OKFenny Setya AyuNo ratings yet
- Preparing Your Intensive Care Unit For The COVID - ASLIDocument24 pagesPreparing Your Intensive Care Unit For The COVID - ASLIEven EdomekoNo ratings yet
- Amina AliDocument6 pagesAmina Alighada kamalNo ratings yet
- The Covid-19: Name: Yasin Nurrohman Class: Xi-Ipa 6Document9 pagesThe Covid-19: Name: Yasin Nurrohman Class: Xi-Ipa 632-Yasin Nurrohman-BaningNo ratings yet
- Lembar Kerja SiswaDocument25 pagesLembar Kerja SiswaMuhammad HaikalNo ratings yet
- China's Novel Coronavirus Response: Guidelines for Governments, Communities, Entities and Individuals to Combat COVID-19From EverandChina's Novel Coronavirus Response: Guidelines for Governments, Communities, Entities and Individuals to Combat COVID-19No ratings yet
- Care For Vulnerable Populations during COVID-19 Pandemic: Clinical Updates in COVID-19From EverandCare For Vulnerable Populations during COVID-19 Pandemic: Clinical Updates in COVID-19No ratings yet
- IC Data Risk Register 9419Document4 pagesIC Data Risk Register 9419yanuar esthoNo ratings yet
- 248291-Texto Del Artículo-1016521-1-10-20170612Document12 pages248291-Texto Del Artículo-1016521-1-10-20170612yanuar esthoNo ratings yet
- Prevalence of Restless Legs Syndrome in Haemodialysis PatientsDocument4 pagesPrevalence of Restless Legs Syndrome in Haemodialysis Patientsyanuar esthoNo ratings yet
- Hums Iejm v6n1p14 enDocument6 pagesHums Iejm v6n1p14 enyanuar esthoNo ratings yet
- Dialysis Treatment in Indonesia Focus On BaliDocument8 pagesDialysis Treatment in Indonesia Focus On Baliyanuar esthoNo ratings yet
- In Vitro Release Kinetics and Transferrin Saturation Study of Intravenous Iron Sucrose Entrapped in Poly (Ethylene Glycol) - Assisted Silica XerogelDocument12 pagesIn Vitro Release Kinetics and Transferrin Saturation Study of Intravenous Iron Sucrose Entrapped in Poly (Ethylene Glycol) - Assisted Silica Xerogelyanuar esthoNo ratings yet
- Emergency Preparedness - Oops! I Got Caught With My Pants DownDocument12 pagesEmergency Preparedness - Oops! I Got Caught With My Pants Downyanuar esthoNo ratings yet
- Four Love StoriesDocument56 pagesFour Love Storiesyanuar esthoNo ratings yet
- Association Between Low Serum Ferritin and Restless Legs Syndrome in Patients With Attention Defi Cit Hyperactivity DisorderDocument8 pagesAssociation Between Low Serum Ferritin and Restless Legs Syndrome in Patients With Attention Defi Cit Hyperactivity Disorderyanuar esthoNo ratings yet
- 2019 Challenges of Professional Boundaries in The Medical SettingDocument7 pages2019 Challenges of Professional Boundaries in The Medical Settingyanuar esthoNo ratings yet
- Attitudes of Hemodialysis Patients, Medical and Nursing Staff Towards Patients' Physical ActivityDocument12 pagesAttitudes of Hemodialysis Patients, Medical and Nursing Staff Towards Patients' Physical Activityyanuar esthoNo ratings yet
- CMS Survey ProcessDocument16 pagesCMS Survey Processyanuar estho100% (1)
- Supportive Care: Integration of Patient-Centered Kidney Care To Manage Symptoms and Geriatric SyndromesDocument10 pagesSupportive Care: Integration of Patient-Centered Kidney Care To Manage Symptoms and Geriatric Syndromesyanuar esthoNo ratings yet
- Eds AgesDocument8 pagesEds Agesyanuar esthoNo ratings yet
- MSG83 Epidural Analgesia in Labour PDFDocument18 pagesMSG83 Epidural Analgesia in Labour PDFGrigore PopaNo ratings yet
- NCP Liver CirrhosisDocument7 pagesNCP Liver CirrhosisIris Jimenez-BuanNo ratings yet
- Dom Care InfoDocument3 pagesDom Care InfoAnakha AbeyNo ratings yet
- Septem 26 To October 82022Document7 pagesSeptem 26 To October 82022Nathaniel Karl Enin PulidoNo ratings yet
- Tract Gastrointestinal: AgingDocument70 pagesTract Gastrointestinal: Agingmin09hihi100% (1)
- 1683 5733 1 PB PDFDocument48 pages1683 5733 1 PB PDFindahNo ratings yet
- Terms of Reference: Mataasnakahoy Senior High SchoolDocument13 pagesTerms of Reference: Mataasnakahoy Senior High SchoolAngelica LindogNo ratings yet
- Alcohol and Drug Abuse Flow ChartDocument1 pageAlcohol and Drug Abuse Flow Chartboen jaymeNo ratings yet
- Feig 2017Document13 pagesFeig 2017Lembaga Pendidikan dan PelayananNo ratings yet
- Consent Form v2Document2 pagesConsent Form v2api-359651181No ratings yet
- 1 Helicobacter PyloriDocument7 pages1 Helicobacter PyloriNear MtzNo ratings yet
- Morbili 1Document5 pagesMorbili 1Dina MariyanaNo ratings yet
- MPhil Thesis Defence - Schedule of Presentation - October 2021Document1 pageMPhil Thesis Defence - Schedule of Presentation - October 2021Saheed AbdulkarimNo ratings yet
- Pandemic Preparedness PlanDocument40 pagesPandemic Preparedness PlanMurali Vallipuranathan100% (2)
- An Assignment On Autoimmunity: July 2012Document15 pagesAn Assignment On Autoimmunity: July 2012SudhakarNo ratings yet
- Mri Request FormDocument1 pageMri Request Formraad_alghamdi_1No ratings yet
- Young Workers' Occupational Safety: Catherine Loughlin and Michael R. FroneDocument19 pagesYoung Workers' Occupational Safety: Catherine Loughlin and Michael R. FroneStain HecNo ratings yet
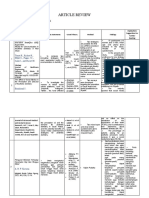
- Article Review - Mona Febiyola Azizah - J2a021043Document3 pagesArticle Review - Mona Febiyola Azizah - J2a021043Mona Febiyola AzizahNo ratings yet
- Aspects /component OF PharmacyDocument10 pagesAspects /component OF PharmacyAlanNo ratings yet
- Nurse Writing 003 OET Practice Letter by PASS OETDocument3 pagesNurse Writing 003 OET Practice Letter by PASS OETTwila Abuedo78% (9)
- Topic: at The Doctor Health Problems Topic: at The Doctor Health ProblemsDocument17 pagesTopic: at The Doctor Health Problems Topic: at The Doctor Health ProblemsEll'm AngelesNo ratings yet
- Inguinal and Anorectal Lymphogranuloma Venereum: A Case Series From A Sexually Transmitted Disease Center in Rome, ItalyDocument5 pagesInguinal and Anorectal Lymphogranuloma Venereum: A Case Series From A Sexually Transmitted Disease Center in Rome, ItalyLovely PoppyNo ratings yet
- ICU Without WallDocument6 pagesICU Without WallFahmi AuliaNo ratings yet
- Health Teaching Plan FormDocument2 pagesHealth Teaching Plan FormChadd Vyllmorr VillarinNo ratings yet
- Aspergillus and Other Respiratory Fungal Infections in The ICU Diagnosis and Management 2018Document7 pagesAspergillus and Other Respiratory Fungal Infections in The ICU Diagnosis and Management 2018ferrevNo ratings yet
- What Is The Effect of Swallowing Without Chewing Properly? What Happen With The Chewing Gum?Document15 pagesWhat Is The Effect of Swallowing Without Chewing Properly? What Happen With The Chewing Gum?Jorge Enrique Olaya LiévanoNo ratings yet
Hemodialysis Unit Preparedness During and After Covid 19 Pandemic
Hemodialysis Unit Preparedness During and After Covid 19 Pandemic
Uploaded by
yanuar esthoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hemodialysis Unit Preparedness During and After Covid 19 Pandemic
Hemodialysis Unit Preparedness During and After Covid 19 Pandemic
Uploaded by
yanuar esthoCopyright:
Available Formats
Hemodialysis Unit Preparedness During And
After COVID-19 Pandemic
COVID-19 Kidney Health Action Group
(v 1 date 19 April 2020)
INTRODUCTION
COVID-19, a respiratory illness caused by a newly discovered coronavirus, has become a
pandemic affecting over 1.9 million people with over 130,000 deaths in 210 countries.
Some people become infected with the virus but do not develop symptoms. When they
appear, symptoms are non-specific, with fever, cough, shortness of breath, sore throat,
fatigue, and headache being the most common. Symptoms are usually mild and benign in a
vast majority (>80%) and recede gradually, leading to a full spontaneous recovery.
A small number become seriously ill, develop difficulty in breathing and complications related
to other organs. They may require hospitalisation and a smaller subset need ICU care. The
mortality is relatively higher in the latter group. This risk goes up in the elderly and those with
co-morbidities (such as hypertension, diabetes, cardiac disease, kidney failure). Still, it is
essential to emphasise that everybody is at risk for severe disease (including the relatively
young and healthy dialysis staff).
The strategy of physical distancing, case finding, contact tracing and quarantine/isolation of
positive cases and high-risk contacts is critical to controlling the spread of this infection. This
strategy is being implemented through nationwide lockdown during the period of intense
transmission. Still, physical distancing is likely to remain in force after the end of the current
lockdown to prevent disease spread.
The virus spreads mainly from person-to-person
through droplets produced especially when an Patients with chronic conditions
infected person coughs or sneezes, and can be passed need to receive regular medical
on to others in close proximity (within about 6 feet) care. In particular, patients on
or through contact with the surfaces that have the maintenance in-center
virus on it followed by touching their face, mouth, hemodialysis need to come to
nose or eyes. Dialysis staff remains in close vicinity to their dialysis centers two to three
patients for long periods of time. Finally, dialysis times every week in order to
units have a lot of surfaces including beds, chairs, receive this life-saving therapy.
equipment etc that can get potentially contaminated.
In addition to dialysis units, patients are likely to get this infection in their communities as
well. In turn, one infected patient can pass on this infection to other patients and staff in the
unit. It is crucial, therefore, for the dialysis units to develop strategies that protect ALL
patients and staff.
A number of bodies, including the International and National Societies of Nephrology and
hospitals around the world have developed guidance for the operation of dialysis units. They
were sourced from journals, web portals and personal communications. These guidelines,
including those by the Indian Ministry of Health and Family Welfare, were reviewed by
members of this group, and a consensus was reached through a series of email exchanges
and videoconferences. In addition, the group also considered the challenges being faced
during the implementation of such guidance.
COVID-19 Pandemic and HD Unit Preparedness v 1.0 19 Apr 2020 2
During their review, the group recognised that guidance by the various expert groups/bodies
are broadly similar, suggesting that this checklist is valid and should be applied in all
circumstances.
It is currently believed that those who have recovered from COVID-19 would develop
antibodies that will confer protection from future infection. While this is likely to be the case,
the group felt that this still remains to be proven, more so for dialysis patients with impaired
immune response. Also, it is unknown how long such immunity will last. Finally, the virus
might mutate (like common influenza virus) and infect those who have had previous
infections with different strains. The hope is that a vaccine will allow generation of quick
immunity. Until then, all dialysis patients and staff should be considered at risk.
WHY THIS PREPAREDNESS CHECKLIST AND HOW TO USE IT?
Given the increased infection risk, and recognising that a coronavirus positive person can
spread the virus before developing symptoms, mitigation steps need to be in place and
followed in all dialysis units at all times.
As coronavirus spreads through our country, dialysis patients and staff will remain at risk of
exposure to the coronavirus in the course of their normal activities even after the initial peak.
Preventing disease spread will require a fundamental change in the way human interaction
takes place in dialysis units. Since patients and dialysis staff interact closely for extended
periods, units will need to be prepared for a ‘new normal’ where they always follow the
precautions described here.
Dialysis staff are used to following protocols. As with the WHO Safe Surgery Checklist, the
current preparedness checklist has been developed to standardise processes further, reduce
errors and avoidable complications, improve teamwork and increase communication,
thereby leading to consolidation of the culture change in response to the pandemic. This
checklist requires making changes in the way units operate currently, including a shift in
mindset, mainly by providing more clear role-definition and guidance around attention to
detail.
An added benefit of this checklist is a likely reduction in the risk of non-COVID infectious
complications in dialysis units, including catheter-related bacteremias.
In the opinion of the group, the checklist needs to be gone through at least once every day,
or more frequently (such as before and after every shift) if required. Each unit should
designate a leader who will go through this list at a pre-determined frequency (e.g. daily) and
monitor its implementation.
DIALYSIS FACILITIES
There is broad consensus that all cases with confirmed Coronavirus infection who need to be
in a healthcare facility should be managed in an isolated area, and should have dedicated staff
COVID-19 Pandemic and HD Unit Preparedness v 1.0 19 Apr 2020 3
without change in duty areas. This includes Coronavirus positive patients who need dialysis.
Since it can be anticipated that coronavirus infection will become widespread in the long run,
all units need to develop an isolation facility for COVID-19 patients. At this time patients are
being referred to designated hospitals for dialysis, which is impractical in the long run.
The issue of cohorting patients with suspected CoV infection was discussed. The group agreed
that since a substantial proportion are likely to test negative, they should not be dialyzed with
those confirmed to have the infection. It was agreed that dialysing them in a separate shift
or clear physical separation is the most feasible strategy at this time.
The In-charge of the Dialysis Unit must put together a working team consisting of physicians,
nursing staff, and technologists. They should receive training in updated clinical knowledge
of COVID-19, notification of cases, epidemic prevention tools, and guidelines. The list of staff
should be recorded and retained by dialysis units.
In the worst-case scenario, we can expect sick patients
with COVID-19 to develop kidney failure that will lead If the number of Coronavirus
to a surge in patients requiring dialysis. Some of this positive cases grows, shortage
surge will divert resources from ESKD patients on of resources is likely to present
chronic dialysis, leading to a forced reduction in service a major challenge. Resource
provision. Several interventions have been suggested to conservation, both manpower
manage this situation. For patients - these include and supplies, is therefore
enforcement of fluid restriction, use of potassium important.
binding resins and oral alkali (non-potassium
containing) or 'total-nephron blockade' (use of multiple diuretic combination with
complementary mechanisms of action to maximise urine output (in non-anuric patients).
Other considerations to augment capacity include using peritoneal dialysis, preparing locally-
made replacement fluids for CRRT, and reducing frequencies of intermittent therapies (HD,
SLED).
As the sick COVID-19 patients are likely to receive multiple pharmacological interventions -
including novel antiviral agents - considerations about drug dose adjustment and interaction
should be kept in mind. Many of these drugs have
Closure of even one dialysis unit likely not been tested in dialysis patients and
places an undue burden on the therefore carry unpredictable toxicities.
patients who needs to find another
facility (which is likely to be already Information should be provided in a way that
full). Therefore, shutting down a prevents panic and undue burdening of dialysis
dialysis unit should be a measure of staff. All units should have a protocol for testing
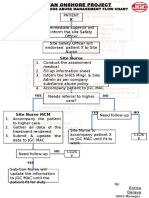
last resort. staff or patients. A suggested flow is shown in the
figure on the following page.
COVID-19 Pandemic and HD Unit Preparedness v 1.0 19 Apr 2020 4
Suggested algorithm for COVID screening in a dialysis unit
COVID-19 Pandemic and HD Unit Preparedness v 1.0 19 Apr 2020 5
An important question is what to do when a
dialysis patient or dialysis staff is found to be In case a dialysis patient or staff is found
COVID-19 positive. In usual healthcare to be COVID-19 positive, the unit should
settings, the contacts of the patient are undergo full disinfection over 24 hours
quarantined and tested if symptomatic. and then resume dialysis. All patients &
However, in the context of a dialysis centre, staff should be tested for COVID-19, but
this means shutting down the dialysis centre ONLY those who test positive and/or are
or significantly scaling down services. The considered as ‘high risk’ contacts (directly
group does not recommend quarantining all involved in care of the positive person)
staff or closing down of dialysis units as they should be quarantined. Staff who test
provide essential and lifesaving treatment negative can come back to work and be
for which there is no alternative. The closely monitored for symptoms
likelihood of a staff not involved in direct suggestive of COVID-19.
care of such a patient being at risk of getting
this infection is very low. India does not have
extra dialysis capacity to accommodate closure of dialysis units. Moreover, this situation can
be repeated in the next unit. The likelihood of death from coronavirus for a dialysis patient is
likely in the 1-10% range. However, the possibility of death from missing dialysis is 100%.
DIALYSIS STAFF
Dialysis staff is the most valuable resource for ensuring the continued operation of units. The
administrators must provide all staff with the necessary protective gear. Because PPE likely
will need to be deployed for many weeks or months in this current pandemic, care must be
taken to establish policies that will not exhaust available supplies of these precious resources.
• Dialysis staff should be instructed to maintain physical distancing and wear masks
when interacting with colleagues and patients at all times, including when they come
to and leave work.
• Staff should not sit in close proximity while eating or drinking.
• If the dialysis units are arranging living quarters for their HCW then they need to be
given individual quarters and not cohorted in one hall.
In case of shortages, acceptable alternatives
Several personal and societal should be agreed upon and sourced. For
consequences of COVID-19 have been example, waterproof rain pants and jackets
noticed, including the impact on mental can be worn under a standard reusable or
health and social stigmatisation. Creating disposable sterile gown along with a shower
awareness and support for prevention cap, shoe covers, a home-made face shield
and countering myths and social stigma is and N95 mask. In case of shortage of N95
important. The most important support, masks, they should be prioritised for those
however, is the provision of full and role- taking care of positive or suspected patients
appropriate PPEs. and/or during aerosol-generating procedures.
COVID-19 Pandemic and HD Unit Preparedness v 1.0 19 Apr 2020 6
It is important to emphasise that even during While supplies can be replenished
shortages, all efforts should continue to procure relatively rapidly but it is hard to find
proper PPEs (as described in the checklist) at the a substitute for skilled workforce
earliest. engaged in providing dialysis. It is
important, to optimize staffing and
HD patient scheduling and cross-
PATIENTS training staff in multiple tasks.
Transport to and from dialysis units is a crucial issue for patients. While the choice of transport
will depend upon the resources available, it should be guided by the principle of distancing
and avoidance of coming in close contact with someone who cannot be traced. Patients
should be advised not to take public transport since reliable physical distancing is difficult.
Patients should come unaccompanied whenever possible and not bring any personal items
with them. Eating is not allowed in the dialysis room since it requires the removal of masks
and generates aerosols.
Patients should be advised not to visit a healthcare facility unless essential. Units should
extend teleconsultation services, using telephones, social media or other online platforms.
All patients need to have regular access to essential medicines needed to manage their
health. Where possible, refilling of supplies should be coordinated with dialysis visits.
COVID-19 Pandemic and HD Unit Preparedness v 1.0 19 Apr 2020 7
About COVID-19 Kidney Health Action Group
This document was developed and will be maintained by the COVID-19 Kidney Health Action
Group, a voluntary group of nephrologists committed to improving the care of patients with
and at risk of kidney disease in India. Members of the group are:
• Divya Bajpai, Seth GS Medical College and KEM Hospital, Mumbai
• Natarajan Gopalakrishnan, Madras Medical College, Chennai
• Noble Gracious, Government Medical College, Trivandrum
• Ajay Kher, Max Hospital, Vaishali, Uttar Pradesh
• Vijay Kher, Medanta the Mediciti, Gurgaon. Past-President, Indian Society of
Nephrology
• Dinesh Khullar, Max Hospital, Saket, New Delhi
• Valentine Lobo, KEM Hospital, Pune
• Sandeep Mahajan, All India Institute of Medical Sciences, New Delhi
• Gopesh Modi, Samarpan Kidney Center, Bhopal
• Ajit S Narula, Fortis Escorts Kidney Institute, New Delhi
• Sreejith Parameswaran, Jawaharlal Institute of Medical Education and Research,
Puducherry
• Narayan Prasad, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow.
Hon. Secretary, Indian Society of Nephrology
• Mohan M Rajapurkar, Muljibhai Patel Urological Hospital, Nadiad, Past-President,
Indian Society of Nephrology
• Raja Ramachandran, Postgraduate Institute of Medical Education and Research,
Chandigarh
• Manisha Sahay, Osmania General Hospital, Hyderabad
• Vivekanand Jha, George Institute for Global Health India, New Delhi
This checklist is not a guideline or an official document. It is intended to be used as a
constant reminder and practice guide, so that these practices and principles on which
they are based are internalised in the day-to-day working of the staff in the dialysis
unit, and by patients and their caregivers. It should be used in conjunction with local
policies and official guidance from health authorities or hospitals.
Please address any correspondence to vjha@georgeinstitute.org.in.
COVID-19 Pandemic and HD Unit Preparedness v 1.0 19 Apr 2020 8
You might also like
- NURSING CARE PLAN Risk For InfectionDocument3 pagesNURSING CARE PLAN Risk For InfectionEvelyn Lampios100% (1)
- MCNDocument23 pagesMCNJASTINE NICOLE SABORNIDONo ratings yet
- When To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsDocument9 pagesWhen To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsepraetorianNo ratings yet
- Shivan Sarna 10 Signs Your Mouth Could Be Making You SickDocument13 pagesShivan Sarna 10 Signs Your Mouth Could Be Making You SickViolet VioletNo ratings yet
- FMEA Audits - Why Do We Need Them?: Empirical Ranking of A FMEADocument2 pagesFMEA Audits - Why Do We Need Them?: Empirical Ranking of A FMEAyanuar esthoNo ratings yet
- 10 1016@j Breast 2020 04 006Document9 pages10 1016@j Breast 2020 04 006Alberto AlexandruNo ratings yet
- COVIDDocument9 pagesCOVIDryan smithNo ratings yet
- Global Guidance For Surgical Care During The COVID-19 PandemicDocument7 pagesGlobal Guidance For Surgical Care During The COVID-19 PandemicSergio Losada AmayaNo ratings yet
- Covid 19 ProgramDocument12 pagesCovid 19 ProgramBAGUIO CATSNo ratings yet
- Scope and LimitationsDocument4 pagesScope and LimitationsRey Dela PeñaNo ratings yet
- Mitigating Risk of COVID-19 in Dialysis Facilities: Alan S. Kliger and Jeffrey SilberzweigDocument3 pagesMitigating Risk of COVID-19 in Dialysis Facilities: Alan S. Kliger and Jeffrey SilberzweigRChofiyana OchiNo ratings yet
- Mitigating Isolation Study 2021.12.23.21268326v1.fullDocument10 pagesMitigating Isolation Study 2021.12.23.21268326v1.fullmart0830No ratings yet
- World Health Organization (WHO) Information Note Tuberculosis and COVID-19Document10 pagesWorld Health Organization (WHO) Information Note Tuberculosis and COVID-19WasimNo ratings yet
- Coronavirus Disease 2019 (Covid-19) and Hiv: Key Issues and ActionsDocument8 pagesCoronavirus Disease 2019 (Covid-19) and Hiv: Key Issues and ActionsnasratullahNo ratings yet
- Patient Management During COVID 19 AsrmDocument10 pagesPatient Management During COVID 19 AsrmDivisi FER MalangNo ratings yet
- Kidney InternationalDocument5 pagesKidney InternationalZara AkbariNo ratings yet
- COVID-19 Maternity Services TB Package UPDATE 2 14072020 SBZDocument58 pagesCOVID-19 Maternity Services TB Package UPDATE 2 14072020 SBZSalomeNo ratings yet
- COVID-19 Global Pandemic: Options For Management of Gynecologic CancersDocument4 pagesCOVID-19 Global Pandemic: Options For Management of Gynecologic CancersMuhammad FaisalNo ratings yet
- Goh2020 Article PreparingYourIntensiveCareUnitDocument19 pagesGoh2020 Article PreparingYourIntensiveCareUnitBAGUIO CATSNo ratings yet
- Covid-19: Guide On Home-Based Care, Screening & Isolation Ward Set UpDocument9 pagesCovid-19: Guide On Home-Based Care, Screening & Isolation Ward Set Upvimalraj vtNo ratings yet
- PIIS0003999320302951Document3 pagesPIIS0003999320302951Adiel CarrascoNo ratings yet
- Approaches To The Management of Patients in Oral and Maxillofacial Surgery During COVID-19 PandemicDocument21 pagesApproaches To The Management of Patients in Oral and Maxillofacial Surgery During COVID-19 PandemicYahul MazfarNo ratings yet
- Apexa NO 8Document5 pagesApexa NO 8Apexa YadavNo ratings yet
- Minimally Invasive Urologic Surgery Is Safe During COVID 19: Experience From Two High Volume Centers in ItalyDocument3 pagesMinimally Invasive Urologic Surgery Is Safe During COVID 19: Experience From Two High Volume Centers in ItalyMasrun FatanahNo ratings yet
- The Pandemic Hits Us Hard, But We Don't Lose HopeDocument4 pagesThe Pandemic Hits Us Hard, But We Don't Lose HopeLasa SiahaanNo ratings yet
- PCX - ReportDocument16 pagesPCX - Reportgowtham thakutNo ratings yet
- PCX - ReportDocument16 pagesPCX - Reportgowtham thakutNo ratings yet
- The Journal For Nurse PractitionersDocument5 pagesThe Journal For Nurse Practitionersagstri lestariNo ratings yet
- Research Paper For The Effectivity of Ultraviolet Lights in Containing COVID-19Document6 pagesResearch Paper For The Effectivity of Ultraviolet Lights in Containing COVID-19Angelyn MarquezNo ratings yet
- Guidance On The Use of Personal Protective Equipment Ppe in Hospitals During The Covid 19 OutbreakDocument9 pagesGuidance On The Use of Personal Protective Equipment Ppe in Hospitals During The Covid 19 OutbreakGerlan Madrid MingoNo ratings yet
- National Guidance For The Recovery of Elective Surgery in ChildrenDocument50 pagesNational Guidance For The Recovery of Elective Surgery in ChildrenJulia RamirezNo ratings yet
- Safari - 12 May 2020 10.04Document1 pageSafari - 12 May 2020 10.04tenun witaNo ratings yet
- First Case Report of A Successfully Managed Severe COVID-19 Infectionin MalawiDocument4 pagesFirst Case Report of A Successfully Managed Severe COVID-19 Infectionin MalawiYoga PrabawaNo ratings yet
- Ijgo 13868Document8 pagesIjgo 13868rutujaNo ratings yet
- Ivermectin Interest Group v4Document41 pagesIvermectin Interest Group v4SundayTimesZA100% (1)
- American Society For Reproductive Medicine (Asrm) Patient Management and Clinical Recommendations During The Coronavirus (Covid-19) PandemicDocument8 pagesAmerican Society For Reproductive Medicine (Asrm) Patient Management and Clinical Recommendations During The Coronavirus (Covid-19) PandemicIoana Adina RugescuNo ratings yet
- Manejo Ambulatorio AdultosDocument18 pagesManejo Ambulatorio AdultosCarlos Huaman ZevallosNo ratings yet
- Ajbsr MS Id 001564Document3 pagesAjbsr MS Id 001564Rodrigo AlpizarNo ratings yet
- NOTTO Transplant Specific Guidelines With Reference To COVID-19Document5 pagesNOTTO Transplant Specific Guidelines With Reference To COVID-19Ashish MishraNo ratings yet
- Ajt.15876 NefroDocument7 pagesAjt.15876 Nefrobrissa senraNo ratings yet
- Covid19 - Physiotherapy - Management - Information - GuidanceDocument13 pagesCovid19 - Physiotherapy - Management - Information - GuidanceMasrov TukirovNo ratings yet
- Covid-19: Guide On Home-Based Care, Screening & Isolation Ward Set UpDocument9 pagesCovid-19: Guide On Home-Based Care, Screening & Isolation Ward Set UpTech Person 03No ratings yet
- © The Author(s) 2020. Published by Oxford University Press For The Infectious Diseases Society ofDocument13 pages© The Author(s) 2020. Published by Oxford University Press For The Infectious Diseases Society ofMastifa HanasitaNo ratings yet
- Preparing Your Intensive Care Unit For The COVID-19 Pandemic: Practical Considerations and StrategiesDocument12 pagesPreparing Your Intensive Care Unit For The COVID-19 Pandemic: Practical Considerations and Strategiesririn puspasariNo ratings yet
- LKS Virus CoronaDocument4 pagesLKS Virus Coronauciha.irfan80No ratings yet
- Teknik Resus BosaertDocument13 pagesTeknik Resus BosaertDADASDSANo ratings yet
- Maximizing The Calm Before The Storm: Tiered Surgical Response Plan For Novel Coronavirus (COVID-19)Document31 pagesMaximizing The Calm Before The Storm: Tiered Surgical Response Plan For Novel Coronavirus (COVID-19)drwagnerzaoNo ratings yet
- Guidance For Maternal Medicine Services in The Evolving Coronavirus (COVID-19) PandemicDocument46 pagesGuidance For Maternal Medicine Services in The Evolving Coronavirus (COVID-19) Pandemicadamu mohammadNo ratings yet
- Guidance For Return To Practice For Otolaryngology-Head and Neck SurgeryDocument10 pagesGuidance For Return To Practice For Otolaryngology-Head and Neck SurgeryLeslie Lindsay AlvarezNo ratings yet
- Brief Guideline For The Prevention of COVID-19Document8 pagesBrief Guideline For The Prevention of COVID-19wkzw779bxpNo ratings yet
- Lembar Kerja Peserta Didik Covid19Document6 pagesLembar Kerja Peserta Didik Covid19faraa dydasyrNo ratings yet
- COVID-19 - Infection Control For Persons With SARS-CoV-2 Infection - UpToDateDocument35 pagesCOVID-19 - Infection Control For Persons With SARS-CoV-2 Infection - UpToDateDuy Hùng HoàngNo ratings yet
- Sahwa Aisya SafitriDocument21 pagesSahwa Aisya SafitriSahwa Aisyah safitriNo ratings yet
- Lembar Kerja Siswa Virus CoronaDocument18 pagesLembar Kerja Siswa Virus CoronaChintiya PutriNo ratings yet
- LEMBAR KERJA SISWA Virus Corona OKDocument12 pagesLEMBAR KERJA SISWA Virus Corona OKAbdee74% (19)
- LEMBAR KERJA SISWA Virus Corona Salma Hamidah X Akl4Document16 pagesLEMBAR KERJA SISWA Virus Corona Salma Hamidah X Akl4Salma MuthmainahNo ratings yet
- Tugas BKDocument14 pagesTugas BKshakila azzaNo ratings yet
- (24!03!2020) LKS Pembelajaran Virus Corona Nisrina Nabila Azzahra X-TEI SMK PiramidaDocument43 pages(24!03!2020) LKS Pembelajaran Virus Corona Nisrina Nabila Azzahra X-TEI SMK PiramidaUne NuneNo ratings yet
- LEMBAR KERJA SISWA Fenny SA Virus Corona OKDocument20 pagesLEMBAR KERJA SISWA Fenny SA Virus Corona OKFenny Setya AyuNo ratings yet
- Preparing Your Intensive Care Unit For The COVID - ASLIDocument24 pagesPreparing Your Intensive Care Unit For The COVID - ASLIEven EdomekoNo ratings yet
- Amina AliDocument6 pagesAmina Alighada kamalNo ratings yet
- The Covid-19: Name: Yasin Nurrohman Class: Xi-Ipa 6Document9 pagesThe Covid-19: Name: Yasin Nurrohman Class: Xi-Ipa 632-Yasin Nurrohman-BaningNo ratings yet
- Lembar Kerja SiswaDocument25 pagesLembar Kerja SiswaMuhammad HaikalNo ratings yet
- China's Novel Coronavirus Response: Guidelines for Governments, Communities, Entities and Individuals to Combat COVID-19From EverandChina's Novel Coronavirus Response: Guidelines for Governments, Communities, Entities and Individuals to Combat COVID-19No ratings yet
- Care For Vulnerable Populations during COVID-19 Pandemic: Clinical Updates in COVID-19From EverandCare For Vulnerable Populations during COVID-19 Pandemic: Clinical Updates in COVID-19No ratings yet
- IC Data Risk Register 9419Document4 pagesIC Data Risk Register 9419yanuar esthoNo ratings yet
- 248291-Texto Del Artículo-1016521-1-10-20170612Document12 pages248291-Texto Del Artículo-1016521-1-10-20170612yanuar esthoNo ratings yet
- Prevalence of Restless Legs Syndrome in Haemodialysis PatientsDocument4 pagesPrevalence of Restless Legs Syndrome in Haemodialysis Patientsyanuar esthoNo ratings yet
- Hums Iejm v6n1p14 enDocument6 pagesHums Iejm v6n1p14 enyanuar esthoNo ratings yet
- Dialysis Treatment in Indonesia Focus On BaliDocument8 pagesDialysis Treatment in Indonesia Focus On Baliyanuar esthoNo ratings yet
- In Vitro Release Kinetics and Transferrin Saturation Study of Intravenous Iron Sucrose Entrapped in Poly (Ethylene Glycol) - Assisted Silica XerogelDocument12 pagesIn Vitro Release Kinetics and Transferrin Saturation Study of Intravenous Iron Sucrose Entrapped in Poly (Ethylene Glycol) - Assisted Silica Xerogelyanuar esthoNo ratings yet
- Emergency Preparedness - Oops! I Got Caught With My Pants DownDocument12 pagesEmergency Preparedness - Oops! I Got Caught With My Pants Downyanuar esthoNo ratings yet
- Four Love StoriesDocument56 pagesFour Love Storiesyanuar esthoNo ratings yet
- Association Between Low Serum Ferritin and Restless Legs Syndrome in Patients With Attention Defi Cit Hyperactivity DisorderDocument8 pagesAssociation Between Low Serum Ferritin and Restless Legs Syndrome in Patients With Attention Defi Cit Hyperactivity Disorderyanuar esthoNo ratings yet
- 2019 Challenges of Professional Boundaries in The Medical SettingDocument7 pages2019 Challenges of Professional Boundaries in The Medical Settingyanuar esthoNo ratings yet
- Attitudes of Hemodialysis Patients, Medical and Nursing Staff Towards Patients' Physical ActivityDocument12 pagesAttitudes of Hemodialysis Patients, Medical and Nursing Staff Towards Patients' Physical Activityyanuar esthoNo ratings yet
- CMS Survey ProcessDocument16 pagesCMS Survey Processyanuar estho100% (1)
- Supportive Care: Integration of Patient-Centered Kidney Care To Manage Symptoms and Geriatric SyndromesDocument10 pagesSupportive Care: Integration of Patient-Centered Kidney Care To Manage Symptoms and Geriatric Syndromesyanuar esthoNo ratings yet
- Eds AgesDocument8 pagesEds Agesyanuar esthoNo ratings yet
- MSG83 Epidural Analgesia in Labour PDFDocument18 pagesMSG83 Epidural Analgesia in Labour PDFGrigore PopaNo ratings yet
- NCP Liver CirrhosisDocument7 pagesNCP Liver CirrhosisIris Jimenez-BuanNo ratings yet
- Dom Care InfoDocument3 pagesDom Care InfoAnakha AbeyNo ratings yet
- Septem 26 To October 82022Document7 pagesSeptem 26 To October 82022Nathaniel Karl Enin PulidoNo ratings yet
- Tract Gastrointestinal: AgingDocument70 pagesTract Gastrointestinal: Agingmin09hihi100% (1)
- 1683 5733 1 PB PDFDocument48 pages1683 5733 1 PB PDFindahNo ratings yet
- Terms of Reference: Mataasnakahoy Senior High SchoolDocument13 pagesTerms of Reference: Mataasnakahoy Senior High SchoolAngelica LindogNo ratings yet
- Alcohol and Drug Abuse Flow ChartDocument1 pageAlcohol and Drug Abuse Flow Chartboen jaymeNo ratings yet
- Feig 2017Document13 pagesFeig 2017Lembaga Pendidikan dan PelayananNo ratings yet
- Consent Form v2Document2 pagesConsent Form v2api-359651181No ratings yet
- 1 Helicobacter PyloriDocument7 pages1 Helicobacter PyloriNear MtzNo ratings yet
- Morbili 1Document5 pagesMorbili 1Dina MariyanaNo ratings yet
- MPhil Thesis Defence - Schedule of Presentation - October 2021Document1 pageMPhil Thesis Defence - Schedule of Presentation - October 2021Saheed AbdulkarimNo ratings yet
- Pandemic Preparedness PlanDocument40 pagesPandemic Preparedness PlanMurali Vallipuranathan100% (2)
- An Assignment On Autoimmunity: July 2012Document15 pagesAn Assignment On Autoimmunity: July 2012SudhakarNo ratings yet
- Mri Request FormDocument1 pageMri Request Formraad_alghamdi_1No ratings yet
- Young Workers' Occupational Safety: Catherine Loughlin and Michael R. FroneDocument19 pagesYoung Workers' Occupational Safety: Catherine Loughlin and Michael R. FroneStain HecNo ratings yet
- Article Review - Mona Febiyola Azizah - J2a021043Document3 pagesArticle Review - Mona Febiyola Azizah - J2a021043Mona Febiyola AzizahNo ratings yet
- Aspects /component OF PharmacyDocument10 pagesAspects /component OF PharmacyAlanNo ratings yet
- Nurse Writing 003 OET Practice Letter by PASS OETDocument3 pagesNurse Writing 003 OET Practice Letter by PASS OETTwila Abuedo78% (9)
- Topic: at The Doctor Health Problems Topic: at The Doctor Health ProblemsDocument17 pagesTopic: at The Doctor Health Problems Topic: at The Doctor Health ProblemsEll'm AngelesNo ratings yet
- Inguinal and Anorectal Lymphogranuloma Venereum: A Case Series From A Sexually Transmitted Disease Center in Rome, ItalyDocument5 pagesInguinal and Anorectal Lymphogranuloma Venereum: A Case Series From A Sexually Transmitted Disease Center in Rome, ItalyLovely PoppyNo ratings yet
- ICU Without WallDocument6 pagesICU Without WallFahmi AuliaNo ratings yet
- Health Teaching Plan FormDocument2 pagesHealth Teaching Plan FormChadd Vyllmorr VillarinNo ratings yet
- Aspergillus and Other Respiratory Fungal Infections in The ICU Diagnosis and Management 2018Document7 pagesAspergillus and Other Respiratory Fungal Infections in The ICU Diagnosis and Management 2018ferrevNo ratings yet
- What Is The Effect of Swallowing Without Chewing Properly? What Happen With The Chewing Gum?Document15 pagesWhat Is The Effect of Swallowing Without Chewing Properly? What Happen With The Chewing Gum?Jorge Enrique Olaya LiévanoNo ratings yet