Professional Documents
Culture Documents
Airway Management
Airway Management
Uploaded by
Baebee LouOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Airway Management
Airway Management
Uploaded by
Baebee LouCopyright:
Available Formats
Airway Management in COVID 19 Patients Guidelines
I. Introduction:
A. Background:
Severe acute respiratory syndrome-corona virus-2 (SARS-CoV-2), which causes
COVID-19, is a single-stranded ribonucleic acid -encapsulated corona virus and
is highly contagious.
Transmission is thought to be predominantly by droplet spread (i.e. relatively
large particles that settle from the air), and direct contact with the patient or
contaminated surfaces (fomites), rather than airborne spread, in which smaller
particles remain in the air longer.
Initial airway management procedures in Emergency & Intensive Care
Departments may generate aerosols which will increase risk of transmission.
Healthcare workers (HCW) treating patients with COVID-19 are at increased risk
of contracting the illness.
B. Aim of the Scope:
The aim of this guidelines is to provide HCWs with a well-organized approach to
manage airway for the COVID 19 patients in Emergency & Intensive Care
Departments, to protect them and optimize and increase the chances of
successful first attempt intubation. The guideline was developed by doing a
literature review by 3 reviewers and coming up with the written document. The
next step was having a meeting with 20 ICU consultant to review the final
version. Conflicts were solved by discussion and voting.
C. Purpose:
(1) Reduce risk of a viral airborne spread.
(2) Maximize first attempt success.
(3) Encourage use of Indirect glottic visualization with video
laryngoscopy (VL).
(4) Reduce personnel exposure.
D. Targeted Population:
All adult COVID 19 patients who are requiring airway management in the ED,
hospital wards, and ICUs.
E. Targeted End User:
(1) Adult Emergency Medicine physicians
(2) Adult Critical Care Medicine physicians
(3) Adult Anesthetist physicians.
F. Conflict of interest:
No conflict of interest.
G. Funding:
None.
Modified: 13 / May / 2020
II. Airway Management:
A. Tracheal intubation in Critically ill Patients:
This is a high-risk procedure with physiological difficulty. Around 10% of patients
in this setting develop severe hypoxemia (SpO2) and 2% experience cardiac
arrest. The increased risk of HCW infection during multiple airway manipulations
necessitates the use of airway techniques which are reliable and maximize first-
time success. This applies equally to rescue techniques if tracheal intubation
fails at first attempt. All COVID 19 patients requiring airway management should
be considered as a difficult airway and all preparation should take into
consideration this point.
B. Aerosol Generating Procedure:
Aerosol-generating procedures (AGP) are procedures that stimulate coughing
and promote the generation of aerosols. Additional infection prevention and
control precautions are required for some AGP where an increased risk of
infection has been identified. A systematic review of infection risk to HCWs,
based on limited literature, ranked airway procedures in descending order of risk
as:
(1) Tracheal intubation.
(2) Cricothyroidotomy.
(3) Tracheostomy.
(4) Non-invasive ventilation (NIV).
(5) High Flow Nasal Cannula Oxygenation (HFNO).
(6) Mask ventilation.
Other potentially AGPs include disconnection of ventilatory circuits during use;
tracheal extubation; cardiopulmonary resuscitation (before tracheal intubation);
bronchoscopy and tracheal suction without a closed in-line system.
C. Indication for Intubation in COVID 19:
(1) Increase work of breathing & signs of organ failure (e.g. altered mental
status, low BP, increase lactate, signs of cardiac ischemia).
(2) Acute hypoxic respiratory failure not responding to HFNO nor BiPAP for 2
hours.
(3) Hypoxia with acute decrease level of conscious and cannot protect his
airway.
(4) Hypoxia with large copious secretions.
(5) Hypercapnic respiratory failure not responding to HFNO nor BiPAP.
(6) Hemodynamically unstable.
(7) Consider in patient on HFNO or BiPAP therapy and for transfer by
ambulance.
D. Patient who are in respiratory distress and need assistance, a trial of HFNO
should be strongly considered prior to intubation if available (see figure in next
page).
Modified: 13 / May / 2020
E. If HFNO is not available, and oxygenation and ventilation support is needed,
intubation is recommended instead of attempts to primarily manage with
noninvasive positive pressure ventilation (NIPPV).
F. NIPPV or HFNO (if used) should be performed in a negative pressure room. If
negative pressure room is not available, then the room has to have at least a
HEPA filter. Prior SARS experience showed that BiPAP and manual bagging
both increase the risk of airborne viral particles and > 90% of patients ultimately
failed trials of NIPPV.
G. Intubate in a negative pressure room, and if not available, then HEPA filter
should be available in the room while intubating.
H. Avoid nebulized medication administration whenever possible.
I. Rapid sequence intubation (RSI) should be the method for intubation.
J. During RSI, use high-dose neuromuscular blocking agents (NMBA) for faster
and complete apnea with no residual cough. It is preferred to use rocuronium
1mg/kg rather than succinylcholine as it has a longer duration and will prevent
post intubation coughing on the mechanical ventilator until patient is well
sedated.
Modified: 13 / May / 2020
Modified: 13 / May / 2020
III. The 7 Ps approach should always be used in intubation:
A. Preparation:
(1) 3 HCW should be available during the procedure: 1 to intubate,
1 to assist [respiratory care practitioner (RCP) or a nurse], 1 to give the
medication (nurse).
(2) Full PPE should be applied before intubating: (surgical or yellow
gown, face shield, N95, double gloves, head cover, foot cover).
(3) Procedure should be done in a negative pressure room. If not
available, the room should have HEPA filter.
(4) The minimal number of health care workers should be in the
room.
(5) The most expert person should be the one who intubate the
patient (preferably anesthesia if available at time of intubation).
(6) The patient should have 2 large bore peripheral IV cannulas (14-
16 gauge) before intubation.
(7) An intubation trolley should be always prepared and ready in the
ICU or ED. This should include:
1. Oral Airways different sizes.
2. Nasal Airways different sizes.
3. Malleable ETT stylets.
4. Laryngoscope with size 3 and 4 Macintosh blade (preferable
disposable).
5. Different sized of ETT (from size 7.5-8.5).
6. Ambo Bag Adult Size.
7. Oxygen tubing.
8. Elastic bougie.
9. 10 or 15 cc syringe.
10. Yanker suction.
11. Suction tubing.
12. ETCO2 detector.
13. ETT securing device.
14. Stethoscope (preferred disposable).
(8) A difficult airway kit should be always ready on the ED or ICU
and should include laryngeal mask airways (LMAs) with different sizes,
elastic bougies, percutaneous cricothyroidotomy kit)
(9) Video Assisted Laryngoscopy (e.g. Glidoscope, MAC) should be
ready all the time with disposable blades.
B. Pre-Oxygenation:
(1) Preoxygenation should be done by non-rebreather oxygen mask
on 15L/min. Manual bagging and PPV should be avoided an only
performed if clinically required.
(2) Low volume and higher frequency approach if bagging is
required.
Modified: 13 / May / 2020
C. Pre-Medication:
(1) Atropine: if patient develops bradycardia secondary to intubation
(dose 0.5-1mg IV).
(2) Fentanyl: in case patient has high BP (SBP>180mmHg) before
intubation (dose: 0.5-1mcg/kg IV).
(3) Phenylephrine: in case of low BP (SBP< 90mmHg) during
intubation (dose 50- 100mcg IV), OR
(4) Ephedrine: in case of low BP (SBP<90 mmHg) during intubation
(5-25mg IV).
D. Paralysis & Sedation:
(1) Sedation (see Appendix 1):
• Option 1: Etomidate.
• Option 2: Propofol.
• Option 3: Midazolam & Fentanyl.
• Option 4: Ketamine.
(2) Paralysis agent (see Appendix 2):
1. Option 1: Rocuronium: 30-60 sec to have effect, longer duration,
dose 1mg/kg IV (preferred).\
2. Option 2: Succinylcholine: 5-15 sec to have effect, short
duration, dose 1.5mg/kg IV. Should avoid in:
• CRF patients.
• Burn patients.
• Neuromuscular disease patients.
• Large stroke patients.
• Malignant hyperthermia.
E. Put the tube (intubation):
(1) The most expert Intubator around should do the intubation.
(2) After assuring full PPEs, a cuffed ETT size 8-8.5 in male patients,
and 7-7.5 in female patient should be placed with video assisted
laryngoscopy (e.g. glidoscope).
(3) 10-15 cc syringe full of air should be used to inflate the ETT
balloon to secure it.
(4) Once tube is inserted in the airway, viral filter (or if not available
than HME filter) should be connected on the ETT before connecting to
the Ambo bag.
(5) ETCO2 should be connected to the Ambo bag to confirm
placement of ETT.
F. Post Intubation Care:
(1) Auscultation of the chest to confirm air entry in both lungs with
disposable stethoscopes if available.
(2) ETT should be immediately secured by ETT securing device.
(3) Assess patient vital signs and saturation immediately post
intubation.
(4) Start patient on sedation infusion immediately.
Modified: 13 / May / 2020
(5) Insert an NGT or OGT.
(6) Connect the patient to the ventilator with appropriate setting and
assure closed suctioning system.
(7) Order a CXR to confirm placement.
G. Reduce Personnel Contamination:
(1) Enhanced droplet PPE.
(2) Bonnet, N95 or PAPR, goggles, face shield, gown, and gloves
pulled over end of gown Sleeves.
(3) Follow all donning and doffing procedures with observer-ensured
compliance.
(4) Only clinicians that have completed PPE training can intubate.
(5) Minimize number of clinicians in the room needed to complete
the intubation.
(6) Limit to a 3-person intubation team when possible: Primary RN,
RT and MD.
(7) SARS experience revealed that cross contamination was highest
when > 3 people were in the room.
IV. References
A. T.M. Cook, K El-Boghdady, et al. Consensus guidelines for managing the airway
in patients with COVID- 19, Anesthesia 2020, doi:10.1111/anae.15054.
B. Zou M, Yuguang H, Wuhua M, et al. Expert Recommendations for Tracheal
Intubation in Critically Ill Patients with Novel. Coronavirus Disease 2019. Chinese
Medical Sciences Journal. Feb 2020 [epub ahead of print].
C. Wax RS, Christian MD. Practical recommendations for critical care and
anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J
Anesthesia. Feb 2020 [epub ahead of print].
D. Zucco L, Levy N, Ketchandji D, et al. Perioperative considerations for the 2019
Novel Coronavirus (COVID-19). Clinical communication from The Anesthesia
Patient Safety Foundation (APSF). Online publication Feb 2020.
E. Kamming D, Gardam M, Chung F. Anesthesia and SARS. Brit J of Anesth. 2003
Jun; 90(6):7158
F. COVID-19 Airway Management. Clinical communication from the European
Airway Management Society (EAMS).
Modified: 13 / May / 2020
APPENDIX 1
Sedative Medications for Induction During Intubation
Name Dose (IV) Advantages Disadvantages
Etomidate 0.3mg/kg Rapid onset, ultrashort duration, nausea and vomiting, adrenal
reduced ICP, no effect on insufficiency (rare)
hemodynamics
Propofol 1-1.5mg/kg Rapid onset, short duration, reduced Lower BP, pain at site of
ICP, anti-nausea, anti- seizure administration (use large bore
cannula in large peripheral veins),
allergy (very rare and in people
with anaphylaxis
secondary to Eggs)
Ketamine 1-1.5mg/kg Rapid onset, duration 10-15 min, Masseter muscle spasm, urgence
analgesic effect, bronchodilators, no hallucination.
effect on hemodynamics,
improved CPP
Midazolam 0.05- Rapid onset, short duration, Negative inotropic effect,
0.1mg/kg antiseizure variable effect
Fentanyl 1-2mcg/kg Analgesic, fast onset, duration 30- 60 Negative inotropic effect, acute
min, decrease sympathetic chest rigidity syndrome
stimulation
APPENDIX 2
Paralytic Agent for Intubation
Name Dose (IV) Advantage Disadvantage Antidote
Rocuronium 0.6-1mg/kg No side effects Longer action (30-60 sec). Sugammadex
Duration (30-60 min). (16mg/kg IV)
Succinylcholine 1-1.5mg/kg Rapid Onset (10-15 sec) Hyperkalemia. None
Short duration (6-10 min) Malignant hyperthermia.
Cardiac dysrhythmias.
Masseter muscle spasm.
Increase IOP
*IOP: intraocular pressure
Modified: 13 / May / 2020
You might also like
- LSVT Loud Patient Lecture Handout 2014Document12 pagesLSVT Loud Patient Lecture Handout 2014pancho_enNo ratings yet
- Aerosol Generating Medical ProceduresDocument6 pagesAerosol Generating Medical Proceduresdhira anindita100% (1)
- HadLock BPD ShapeDocument6 pagesHadLock BPD ShapePippo KennedyNo ratings yet
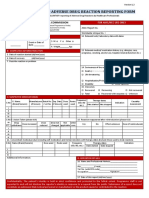
- ADR Reporting FormDocument2 pagesADR Reporting FormApoorva Tatti100% (1)
- Mechanical Ventilition COVID GuidelinesDocument7 pagesMechanical Ventilition COVID Guidelinesheba abuhelwaNo ratings yet
- Prone Position Guidelines-2Document14 pagesProne Position Guidelines-2SAMINo ratings yet
- 1b. Conduct of AnesthesiaDocument29 pages1b. Conduct of AnesthesiaMoayad NawaflehNo ratings yet
- European Resuscitation Council COVID-19 Guidelines: 24 April 2020Document49 pagesEuropean Resuscitation Council COVID-19 Guidelines: 24 April 2020raluNo ratings yet
- April 21st 2020 Muhc Code BlueDocument20 pagesApril 21st 2020 Muhc Code BlueS DNo ratings yet
- Annex 35 Guidelines of IPC and Clinical MX of SARI and PNEUMONIA TRO COVID19 3.11.2020Document4 pagesAnnex 35 Guidelines of IPC and Clinical MX of SARI and PNEUMONIA TRO COVID19 3.11.2020Yeoh Zi-NingNo ratings yet
- Use of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaDocument10 pagesUse of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaLingga AniNo ratings yet
- CCJM 87a ccc033 FullDocument4 pagesCCJM 87a ccc033 FullKamar Operasi Hermina BogorNo ratings yet
- Jurnal 1Document5 pagesJurnal 1RianNo ratings yet
- Webinar Kuliah Umum Anestesi Joglo Semar 17 Juni 2020Document95 pagesWebinar Kuliah Umum Anestesi Joglo Semar 17 Juni 2020izaNo ratings yet
- Weaning Francesas AICM 2019Document7 pagesWeaning Francesas AICM 2019Ana Miryam Pérez ZavalaNo ratings yet
- CCR3 10 E05756Document5 pagesCCR3 10 E05756MARSELLA MICHELLE ERIKA SUMANGKUTNo ratings yet
- Anest, 12 ChaiwatDocument4 pagesAnest, 12 ChaiwatHainey GayleNo ratings yet
- Therapeutics - para COVID - Junho 2020 - HavardDocument28 pagesTherapeutics - para COVID - Junho 2020 - HavardRenato GrinbaumNo ratings yet
- Rapid Sequence Intubation PMGDocument3 pagesRapid Sequence Intubation PMGjaggaNo ratings yet
- Guidelines For Safe ENT Practice in COVID 19Document12 pagesGuidelines For Safe ENT Practice in COVID 19muzeebur rahmanNo ratings yet
- Entcovid0306 PDFDocument12 pagesEntcovid0306 PDFPriyanka KolluruNo ratings yet
- Guía 2019 de Intubación y Extubación Francesa 2019Document7 pagesGuía 2019 de Intubación y Extubación Francesa 2019Rafael Edgar Aguilar Bandala ChaparrinNo ratings yet
- ICU Management of COVID Patients: PreventionDocument13 pagesICU Management of COVID Patients: PreventionYuri SadewoNo ratings yet
- BTSICS Guideline For The Ventilatory Management of Acute Hypercapnic Respiratory Failure in Adults.Document21 pagesBTSICS Guideline For The Ventilatory Management of Acute Hypercapnic Respiratory Failure in Adults.Madalina TalpauNo ratings yet
- Thorax 2016BTS/ICS Guideline For The Ventilatory Management of Acute Hypercapnic Respiratory Failure in Adults Davidson Ii1 Ii35Document36 pagesThorax 2016BTS/ICS Guideline For The Ventilatory Management of Acute Hypercapnic Respiratory Failure in Adults Davidson Ii1 Ii35danelvNo ratings yet
- Airway Management Guidelines of Suspected or Confirmed COVID-19 Patients (Outside of The Operating Rooms)Document19 pagesAirway Management Guidelines of Suspected or Confirmed COVID-19 Patients (Outside of The Operating Rooms)Alyssa GarciaNo ratings yet
- C 8 F 0 CF 2 F 9 C 13052842 DDocument11 pagesC 8 F 0 CF 2 F 9 C 13052842 DDewi Ji YongNo ratings yet
- Mechanical VentilationDocument4 pagesMechanical VentilationUntung SuropatNo ratings yet
- Sars P&P GuidelineDocument21 pagesSars P&P Guidelineyos_peace86No ratings yet
- Rapid Sequence Intubation W Checklist 2022Document4 pagesRapid Sequence Intubation W Checklist 2022drulilalbbNo ratings yet
- Annex 29 Intensive Care Preparedness & Management For Covid19 17062021Document8 pagesAnnex 29 Intensive Care Preparedness & Management For Covid19 17062021Danish SaneshNo ratings yet
- 4.assignment On Endo TubeDocument5 pages4.assignment On Endo Tubesantosh kumarNo ratings yet
- Covid 19 Iot de Emergencia 2021Document4 pagesCovid 19 Iot de Emergencia 2021anaNo ratings yet
- Percutaneous Tracheostomy Guideline - 3.26.14 - June 2014Document5 pagesPercutaneous Tracheostomy Guideline - 3.26.14 - June 2014joseL1994No ratings yet
- Rapid Training of Healthcare Staff For Protected Cardiopulmonary Resuscitation in The COVID-19 PandemicDocument3 pagesRapid Training of Healthcare Staff For Protected Cardiopulmonary Resuscitation in The COVID-19 PandemicRicardo BarreraNo ratings yet
- Via Aerea COVID 19Document3 pagesVia Aerea COVID 19zunarodriguezleoNo ratings yet
- Annex 40 INTERIM GUIDELINES ON RESUSCITATION DURING COVID19 PANDEMICDocument15 pagesAnnex 40 INTERIM GUIDELINES ON RESUSCITATION DURING COVID19 PANDEMICAzran Shariman HasshimNo ratings yet
- Tracheostomy in The COVID 19 PandemicDocument3 pagesTracheostomy in The COVID 19 PandemicKenjiNo ratings yet
- Airway Covid - 19Document37 pagesAirway Covid - 19Monica Herdiati Rukmana NaibahoNo ratings yet
- Intubation Guidelines SummaryDocument2 pagesIntubation Guidelines SummaryriccardoNo ratings yet
- Respiratory Support For Adult Patients With COVID-19Document7 pagesRespiratory Support For Adult Patients With COVID-19SekarNo ratings yet
- Airway Management: Intensive Care Unit, Prince of Wales Hospital, Chinese University of Hong KongDocument9 pagesAirway Management: Intensive Care Unit, Prince of Wales Hospital, Chinese University of Hong KongErwinRamadhaniNo ratings yet
- Implementation of A Non-Invasive Oxygenation Support Strategy During The COVID-19 Pandemic in An Ephemeral Respiratory Intermediate Care UnitDocument3 pagesImplementation of A Non-Invasive Oxygenation Support Strategy During The COVID-19 Pandemic in An Ephemeral Respiratory Intermediate Care UnitJHNo ratings yet
- COVID 19. 4 - 13 KashmerDocument42 pagesCOVID 19. 4 - 13 KashmerIshfaq GanaiNo ratings yet
- Covid-19: Negative Pressure Rooms: Anmf Evidence BriefDocument5 pagesCovid-19: Negative Pressure Rooms: Anmf Evidence BriefninesuNo ratings yet
- Non-Invasive Positive Pressure Ventilation (Nippv)Document4 pagesNon-Invasive Positive Pressure Ventilation (Nippv)docsandyy78No ratings yet
- COVID-19 Management in HongKongDocument1 pageCOVID-19 Management in HongKongShahzad KamranNo ratings yet
- Obesity and Anticipated Difficult Airway - A Comprehensive Approach With Videolaryngoscopy, Ramp Position, Sevoflurane and Opioid Free AnaesthesiaDocument8 pagesObesity and Anticipated Difficult Airway - A Comprehensive Approach With Videolaryngoscopy, Ramp Position, Sevoflurane and Opioid Free AnaesthesiaIJAR JOURNALNo ratings yet
- General Protocol of ICU Physical TherapyDocument15 pagesGeneral Protocol of ICU Physical Therapygeofrey burtonNo ratings yet
- PAHOPHEIHMCovid1920002 EngDocument5 pagesPAHOPHEIHMCovid1920002 EngfrehanyaqNo ratings yet
- Surfactant Final 2Document5 pagesSurfactant Final 2anuNo ratings yet
- Endotracheal intubation (Adult) (1)Document5 pagesEndotracheal intubation (Adult) (1)gourimsc1No ratings yet
- Aha RCP CovidDocument3 pagesAha RCP Covidalex zuluagaNo ratings yet
- Interim Guidance For Healthcare Providers During COVID-19 OutbreakDocument3 pagesInterim Guidance For Healthcare Providers During COVID-19 OutbreakDita Ambarsari SyafruddinNo ratings yet
- Guidelines For Patients With Covid in The Perioperative EnvironmentDocument4 pagesGuidelines For Patients With Covid in The Perioperative Environmentčrni ribezNo ratings yet
- Covid y TraqueostomíaDocument9 pagesCovid y TraqueostomíaCatalina Muñoz VelasquezNo ratings yet
- IV-C Safety Guidelines For Emergency Drugs, Endotracheal Set-Up and Defibrillator UseDocument21 pagesIV-C Safety Guidelines For Emergency Drugs, Endotracheal Set-Up and Defibrillator UseRio DanteNo ratings yet
- Post Extubation CoughDocument4 pagesPost Extubation CoughSana AbbasNo ratings yet
- Fresh H1N1 Guidelines 1 - 1-18Document15 pagesFresh H1N1 Guidelines 1 - 1-18Shahid IqbalNo ratings yet
- Respiratory Tract InfectionsDocument26 pagesRespiratory Tract InfectionsyousefismailrootNo ratings yet
- Long-Term Complications of Tracheal IntubationDocument24 pagesLong-Term Complications of Tracheal Intubationandi kurniawanNo ratings yet
- Standard Precautions: 1.1 Hand HygieneDocument9 pagesStandard Precautions: 1.1 Hand HygieneSandra Ann BijuNo ratings yet
- Pals With Bls 2017cDocument53 pagesPals With Bls 2017cBaebee LouNo ratings yet
- Pancrelipase - EnzymesDocument1 pagePancrelipase - EnzymesBaebee LouNo ratings yet
- Pediatric Hypoglycaemia Low Blood SugarDocument4 pagesPediatric Hypoglycaemia Low Blood SugarBaebee LouNo ratings yet
- Day 1. Mohd Sami 1Document67 pagesDay 1. Mohd Sami 1Baebee LouNo ratings yet
- Asthma - Patho, Signs & SymptomsDocument1 pageAsthma - Patho, Signs & SymptomsBaebee LouNo ratings yet
- Myopia & StrabismusDocument1 pageMyopia & StrabismusBaebee LouNo ratings yet
- Amblyopia, Astigmatism & HyperopiaDocument1 pageAmblyopia, Astigmatism & HyperopiaBaebee LouNo ratings yet
- Iron Deficiency AnemiaDocument1 pageIron Deficiency AnemiaBaebee LouNo ratings yet
- Abuse Assessment & SignsDocument1 pageAbuse Assessment & SignsBaebee LouNo ratings yet
- Saudi Nursing Licensure Examination Blueprint: (To Be Applied in January 2019)Document3 pagesSaudi Nursing Licensure Examination Blueprint: (To Be Applied in January 2019)Baebee LouNo ratings yet
- CPR 2Document3 pagesCPR 2Baebee Lou100% (1)
- ICU Criteria DuringDocument5 pagesICU Criteria DuringBaebee LouNo ratings yet
- Hospital Admission Criteria For COVID-19 Patients: MODIFIED: MAY 8, 2020Document2 pagesHospital Admission Criteria For COVID-19 Patients: MODIFIED: MAY 8, 2020Baebee LouNo ratings yet
- CoronavirusDocument3 pagesCoronavirusBaebee LouNo ratings yet
- AMI in Covid SCDC 1Document5 pagesAMI in Covid SCDC 1Baebee LouNo ratings yet
- Drugs Used in ICU, CCU, OTDocument11 pagesDrugs Used in ICU, CCU, OTBaebee LouNo ratings yet
- Nicholas Christakis Covid Coronavirus Pandemic Apollo's ArrowDocument20 pagesNicholas Christakis Covid Coronavirus Pandemic Apollo's ArrowEvan Sandhoefner100% (2)
- BJMP COVID-19 Advisory 01 COMMITMENT OF PDL FROM PNP AND OTHER AGENCIES LOCK UP CELLS OR DETENTION UNITSDocument2 pagesBJMP COVID-19 Advisory 01 COMMITMENT OF PDL FROM PNP AND OTHER AGENCIES LOCK UP CELLS OR DETENTION UNITSVin LanozoNo ratings yet
- Pharmacovigilance and Its Importance in Drug Regulation: An OverviewDocument16 pagesPharmacovigilance and Its Importance in Drug Regulation: An OverviewSarah ApriliaNo ratings yet
- Step 1 Estudio WORDDocument171 pagesStep 1 Estudio WORDdenisse moraNo ratings yet
- Extended Trochanteric Osteotomy in Revision Total Hip Arthroplasty - Contemporary Outcomes of 612 HipsDocument12 pagesExtended Trochanteric Osteotomy in Revision Total Hip Arthroplasty - Contemporary Outcomes of 612 Hips阿欧有怪兽No ratings yet
- Principles For Aseptic Technique - Information For Healthcare Workers - December 2021Document5 pagesPrinciples For Aseptic Technique - Information For Healthcare Workers - December 2021ebubechukwu echefuNo ratings yet
- Daftar Obat Apotek KumaraDocument36 pagesDaftar Obat Apotek KumaraYogi YogaswaraNo ratings yet
- CLM 104 C 12Document223 pagesCLM 104 C 12Hemant KumarNo ratings yet
- Nutrients 10 01568 PDFDocument13 pagesNutrients 10 01568 PDFمالك مناصرةNo ratings yet
- Castor Oil UsesDocument2 pagesCastor Oil UsesjayjonbeachNo ratings yet
- My ThesisDocument10 pagesMy Thesishinduja reddipilliNo ratings yet
- Abdominal Aortic AneurysmDocument14 pagesAbdominal Aortic AneurysmjialinNo ratings yet
- (One Step) : Whole Blood Serum Plasma Linear Range Specimen Type Mixture Reaction Time Product Class Diseases Test ItemDocument3 pages(One Step) : Whole Blood Serum Plasma Linear Range Specimen Type Mixture Reaction Time Product Class Diseases Test Itemقرآن كريمNo ratings yet
- Antepartum Haemorrhage - CTM Guideline 2020Document20 pagesAntepartum Haemorrhage - CTM Guideline 2020Kvy OngNo ratings yet
- Equine Facilitated TherapyDocument100 pagesEquine Facilitated TherapyBasil Donovan Fletcher100% (1)
- Guide To The Comprehensive, Adult Write-UpDocument6 pagesGuide To The Comprehensive, Adult Write-UpKeaira Kc100% (1)
- Breast SlingDocument9 pagesBreast SlingR2R ThailandNo ratings yet
- Advanced Herd Health Management, Sanitation and HygieneDocument28 pagesAdvanced Herd Health Management, Sanitation and Hygienejane entunaNo ratings yet
- Exam AnxietyDocument34 pagesExam AnxietyaashnasyalNo ratings yet
- Https Examinationservices - Nic.in Examsys22part2 Downloadadmitcard AdmitCardKVS - AspxDocument1 pageHttps Examinationservices - Nic.in Examsys22part2 Downloadadmitcard AdmitCardKVS - AspxReema SinghNo ratings yet
- NCM 107 Postpartum Assessment BenitezDocument2 pagesNCM 107 Postpartum Assessment BenitezJaye Aprile Adrianne KuizonNo ratings yet
- Drug Study - IbuprofenDocument7 pagesDrug Study - IbuprofenajNo ratings yet
- CNS Stimulants 2023Document10 pagesCNS Stimulants 2023ManWol JangNo ratings yet
- Changes in Barthel Index Outcomes As Result of Poststroke Rehabilitation Using NDT-Bobath MethodDocument5 pagesChanges in Barthel Index Outcomes As Result of Poststroke Rehabilitation Using NDT-Bobath MethodRommel AndresNo ratings yet
- Adult CardDocument4 pagesAdult CardagelsantosNo ratings yet
- Puerperium Q ADocument2 pagesPuerperium Q AMae Rose Charlene Mendoza100% (1)
- 1-Oral Diagnosis Involves:: D-All of The AboveDocument12 pages1-Oral Diagnosis Involves:: D-All of The AboveQalaq 02No ratings yet