Professional Documents
Culture Documents
Enteral Vitamin A For Reducing Severity of Bronchopulmonary Dysplasia: A Randomized Trial
Enteral Vitamin A For Reducing Severity of Bronchopulmonary Dysplasia: A Randomized Trial
Uploaded by
laurencia aliminOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Enteral Vitamin A For Reducing Severity of Bronchopulmonary Dysplasia: A Randomized Trial
Enteral Vitamin A For Reducing Severity of Bronchopulmonary Dysplasia: A Randomized Trial
Uploaded by
laurencia aliminCopyright:
Available Formats
Enteral Vitamin A for Reducing Severity
of Bronchopulmonary Dysplasia: A
Randomized Trial
Abhijeet A. Rakshasbhuvankar, FRACP,a,b,c,d Karen Simmer, FRACP, PhD,a,b,c Sanjay K. Patole, FRACP, DrPH,a,b,c
Benjamin Stoecklin, MD,a,c,d,e Elizabeth A. Nathan, MBiostate,f,g Michael W. Clarke, PhD,h,i J. Jane Pillow, FRACP, PhDc,d
Evidence suggests that intramuscular vitamin A reduces the risk of
BACKGROUND AND OBJECTIVES: abstract
bronchopulmonary dysplasia (BPD) in preterm infants. Our objective was to compare enteral
water-soluble vitamin A with placebo supplementation to reduce the severity of BPD in
extremely preterm infants.
METHODS:We conducted a double-blind randomized controlled trial in infants ,28 weeks’
gestation who were to receive either enteral water-soluble vitamin A (5000 IU per day) or
a placebo. Supplementation was started within 24 hours of introduction of feeds and
continued until 34 weeks’ postmenstrual age (PMA). The primary outcome was the severity of
BPD, assessed by using the right shift of the pulse oximeter saturation versus the inspired
oxygen pressure curve.
A total of 188 infants were randomly assigned. The mean 6 SD birth weight (852 6
RESULTS:
201 vs 852 6 211 g) and gestation (25.8 6 1.49 vs 26.0 6 1.39 weeks) were comparable
between the vitamin A and placebo groups. There was no difference in the right shift (median
[25th–75th percentiles]) of the pulse oximeter saturation versus inspired oxygen pressure
curve (in kilopascals) between the vitamin A (11.1 [9.5–13.7]) and placebo groups (10.7
[9.5–13.1]) (P = .73). Enteral vitamin A did not affect diagnosis of BPD or other clinical
outcomes. Plasma retinol levels were significantly higher in the vitamin A group versus the
placebo group on day 28 and at 34 weeks’ PMA.
CONCLUSIONS: Enteral water-soluble
vitamin A supplementation improves plasma retinol levels in
extremely preterm infants but does not reduce the severity of BPD.
a
Neonatal Clinical Care Unit and fWomen and Infants Research Foundation, King Edward Memorial Hospital, WHAT’S KNOWN ON THIS SUBJECT: Evidence suggests
Subiaco, Western Australia, Australia; bNeonatal Clinical Care Unit, Perth Children’s Hospital, Perth, Western that intramuscular vitamin A improves plasma vitamin A
Australia, Australia; cCentre for Child Health Research, Medical School, The University of Western Australia and levels and reduces the risk of bronchopulmonary
Telethon Kids Institute, Perth, Western Australia, Australia; gDivision of Obstetrics and Gynaecology, Faculty of dysplasia (BPD) in extremely low birth weight infants.
Health and Medical Sciences, hMetabolomics Australia, Centre for Microscopy, Characterization, and Analysis,
i
Enteral vitamin A supplementation for the prevention of
School of Biomedical Sciences, Faculty of Health and Medical Sciences, and dDivision of Anatomy and Human
Biology, School of Human Sciences, Faculty of Science, The University of Western Australia, Perth, Western
BPD has not been investigated adequately.
Australia, Australia; and eDepartment of Neonatology, University Children’s Hospital Basel, Basel, Switzerland WHAT THIS STUDY ADDS: Enteral water-soluble vitamin A
Dr Rakshasbhuvankar contributed to the protocol, database development, enrollment, outcome supplementation in extremely preterm infants improves
measurement, laboratory work, and first and final drafts of the manuscript; Drs Simmer and Patole plasma vitamin A levels but does not reduce the severity
contributed to the protocol and first and final drafts of the manuscript; Dr Stoecklin contributed to of BPD, as assessed by the right shift of the pulse
the outcome measurement and the final draft of the manuscript; Ms Nathan contributed to oximeter saturation versus inspired oxygen
statistical analysis and the final draft of the manuscript; Dr Clarke contributed to the laboratory pressure curve.
work and the final draft of the manuscript; Dr Pillow acquired funding for the project and
contributed to the protocol, database development, and first and final drafts of the manuscript; and To cite: Rakshasbhuvankar AA, Simmer K, Patole SK, et al.
all authors approved the final manuscript as submitted and agree to be accountable for all aspects Enteral Vitamin A for Reducing Severity of
of the work. Bronchopulmonary Dysplasia: A Randomized Trial.
Pediatrics. 2021;147(1):e2020009985
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
PEDIATRICS Volume 147, number 1, January 2021:e2020009985 ARTICLE
Bronchopulmonary dysplasia (BPD) The 2 randomized controlled trials ratio is the predominant mechanism
is one of the most common (RCTs) investigating enteral vitamin of impaired gas exchange in BPD and
complications of extremely preterm A supplementation for the can be measured on a continuous
birth and is associated with increased prevention of BPD revealed no scale by using the shift test.24,25
short- and long-term morbidities. significant benefit.15,16 Poor Hence, the shift test offers better
BPD increases the risk of absorption by the enteral route could sensitivity and discriminatory
rehospitalization from respiratory explain these findings and may relate capacity compared to BPD defined as
causes, and the need for inhaled to decreased hydrolysis of retinyl a categorical outcome. We reported
pulmonary medications and esters, reduced availability of bile the discriminatory capacity of shift25
tracheostomy in the first 2 years of salts required for the formation of for the widely used 2001 National
life, impairs lung function in children micelles, or inadequate availability of Institutes of Health Eunice Kennedy
and young adults and likely carrier proteins needed for the Shriver National Institute of Child
predisposes preterm infants to absorption of vitamin A in Health and Human Development
chronic obstructive pulmonary enterocytes.17 We postulated that (NICHD) BPD definition.26 Shift
disease in older age.1–4 Additionally, the smaller particle size of vitamin A offers the additional benefit of being
BPD is associated with adverse long- in the water-soluble form might be unaffected by variations in clinician-
term neurodevelopmental outcomes.5 advantageous for improved prescribed saturation targets
BPD is the most important perinatal- absorbance by passive diffusion affecting the use of supplemental
neonatal factor associated with lower compared with the larger particle oxygen.
IQ seen in very and extremely size of the fat-soluble preparations We hypothesized that compared with
preterm infants.6 The effect of BPD on that require carrier-mediated placebo, enteral water-soluble
infants’ cognitive abilities may persist transport.18 Very low birth weight vitamin A supplementation would
lifelong, affecting their higher infants supplemented with the decrease the severity of BPD, as
education and employment water-soluble form of vitamin A have measured by the right shift in the
prospects.7 increased serum retinol levels.19 The SpO2 versus PIO2 curve.
water- versus fat-solubility of
Caffeine and vitamin A are the only vitamin A preparations may be
safe and effective drugs currently critical for interpreting the results of METHODS
available for the prevention of BPD.8,9 RCTs of enteral vitamin A: Wardle We conducted a double-blind
Mechanism of action of vitamin A for et al16 and Calisici et al15 did not placebo-controlled RCT in our
the prevention of BPD is likely to be report the form of vitamin A used in tertiary NICU. We recruited infants
multifactorial (Fig 1).10–14 Despite the their RCTs. Given these data, we who were born at ,28 weeks’
evidence, the use of vitamin A to aimed to investigate the efficacy of gestational age and ,72 hours of age
prevent BPD is limited because of enteral water-soluble vitamin A for after obtaining informed parental
reluctance to prescribe repeated reducing the severity of BPD in consent. Infants with major
intramuscular (IM) injections. Enteral extremely preterm infants. congenital gastrointestinal or
vitamin A may be an alternative respiratory tract abnormalities were
approach but has not been studied The severity of lung disease is excluded. The study was approved by
well in clinical trials. assessed by using the shift test, the hospital ethics committee
which detects a change in the pulse (2016028EW). The study was
oximetry saturation (SpO2) versus registered prospectively with the
inspired oxygen pressure (PIO2) Australian New Zealand Clinical Trial
curve.20–22 The change may be in the Registry (ACTRN12616000408482)
form of the right shift of the entire before recruitment commenced. The
curve (shift) or displacement of the study protocol was published in
top part of the curve downward a peer-reviewed journal for
(shunt) or a combination of the transparency.18 We followed
two.23 Shift is measured in Consolidated Standards of Reporting
kilopascals, whereas shunt is Trials guidelines for reporting the
measured in percentages. Shift results.27
indicates a decreased ventilation/
perfusion ratio, whereas shunt Primary Outcome
indicates a right-to-left intracardiac The primary outcome was the
FIGURE 1
Mechanism of action of vitamin A for the pre- or intrapulmonary shunt. A severity of BPD, as measured by the
vention of BPD. decreased ventilation/perfusion right shift of SpO2 versus PIO2 curve at
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
2 RAKSHASBHUVANKAR et al
36 weeks’ postmenstrual age (PMA). was performed at 38 weeks’ PMA Randomization was stratified for sex
Simultaneous measurements of SpO2 and reported as abnormal if it and gestational age (230–256 and
and PIO2 were obtained while the showed sequelae of IVH or 260–276 weeks’ PMA). Siblings of
PIO2 level was decreased stepwise in intracerebellar hemorrhage or white multiple births were randomly
2 kPa (15 mm Hg or 2% inspired matter loss. assigned individually.
oxygen at sea level) steps at 5-
minute intervals. At least 5 SpO2 Vitamin A Levels Blinding
measurements in the range of 86% We measured plasma retinol and The pharmacy dispensed vitamin A
to 97% were obtained; the lowest relative dose response (RDR) in 35 and the placebo in identical amber-
permissible PIO2 level was 14 kPa infants at day 28 of life. Plasma colored containers. Both preparations
(105 mm Hg or 14% inspired oxygen retinol and RDR were also measured were indistinguishable by their
at sea level). Paired measurements of in 36 consecutive infants at 34 weeks’ appearance, smell, and other physical
SpO2 versus PIO2 were plotted, and PMA. Measurements were obtained properties.
the right shift was determined by 24 hours after the last dose of the
using an algorithm described by trial medication in infants who had Intervention
Lockwood et al.24,28 not received steroids in the preceding The treatment group received enteral
2 weeks because steroids can water-soluble vitamin A (Bio-Logical
Secondary Outcomes influence blood retinol levels.32 A Vitamin A Solution; Biological
The following secondary clinical blood sample (0.5 mL) was collected Therapies, Braeside, Victoria,
outcomes were measured at the in a lithium heparin tube (BD Australia) containing 5000 IU (0.5
time of discharge or death: Microtainer; Becton, Dickinson and mL) of retinyl palmitate, which was
moderate to severe BPD (therapy Company, Franklin Lakes, NJ) by administered once daily through the
with supplemental oxygen for either heel prick or venipuncture. gastric tube, followed by a feed. The
$28 days plus requirement of The method of collection does preparation included pegylated
supplemental oxygen and/or not significantly influence plasma castor oil as an emulsifier. The
continuous positive airway pressure retinol values.33 Plasma for retinol osmolarity of the solution was 1025
[CPAP] and/or mechanical measurement was obtained mOsm/kg. To further reduce the
ventilation at 36 weeks’ PMA)29; immediately by centrifugation of osmolarity, the medication was
death; use of postnatal steroids for the collected blood at 3000 rpm administered with at least 1 mL of
BPD; durations (hours) of for 10 minutes. Plasma was stored breast milk. The control group
supplemental oxygen, mechanical at 280°C and protected from received an identical volume (0.5 mL)
ventilation, and positive pressure light until further analysis. We of the placebo solution (normal saline
support (mechanical ventilation measured plasma retinol levels mixed with a safe coloring agent:
plus CPAP plus humidified high using high-performance liquid 2.5 mg/dL quinoline yellow). The
flow); the proportion of infants chromatography–tandem mass study medications were started
discharged from the hospital with spectrometry. A plasma retinol level within 24 hours of commencement of
home oxygen; weight gain (grams of ,10 mg/dL suggests depleted enteral feeds and continued until 34
per day) during the period of study body stores, whereas levels between weeks’ PMA.
medication supplementation; 10 and 20 mg/dL are considered to
retinopathy of prematurity be low. An RDR value of .20% The attending neonatologist
requiring treatment in the form of indicates deficient liver vitamin A determined the day-to-day
laser ablation or bevacizumab stores.34 management of the infants. Routine
injection; diagnoses of culture- unit policies for preterm infants
positive (blood or cerebrospinal Randomization and Allocation ,28 weeks’ gestation include
fluid) or suspected sepsis Concealment the commencement of caffeine
(C-reactive protein level .25 mg/L Infants were randomly assigned by within 24 hours after birth and
and treatment with antibiotics for at a hospital pharmacist not involved in prescription of probiotics
least 5 days); grade 3 or 4 clinical care. Randomization followed alongside starting minimal
intraventricular hemorrhage (IVH) a computer-generated randomization enteral feeds.
or periventricular leukomalacia30; table using blocks of 6.
stage 2a or greater necrotizing Randomization was performed Other Sources of Vitamin A in the
enterocolitis (NEC)31; and vitamin A within the Research Electronic Data Study Infants
adverse effects (bulging fontanel in Capture randomization module, Separate to the prescribed medication
the absence of IVH, hepatomegaly, ensuring allocation concealment or placebo solution, all study infants
and skin changes). MRI of the brain throughout the study period.35 received 966 IU/kg per day of vitamin
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
PEDIATRICS Volume 147, number 1, January 2021 3
calculator available at https://
clincalc.com/stats/samplesize.aspx).
With a reported incidence of ∼40%
to 45% for moderate to severe BPD
in extremely preterm infants37,38 and
accounting for a 20% loss to follow-
up, we required 188 extremely
preterm infants to achieve a study
power of 80% with a two-tailed test
and 5% significance. The 20% loss to
follow-up estimate was based on our
hospital data: estimated mortality of
10% to 15% and transfer of 5% to
10% of the recruited infants before
36 weeks’ PMA.
Statistical Analysis
An intention-to-treat analysis was
performed. The SpO2 versus PIO2
curve shift measurements were not
normally distributed and were
compared between treatment groups
by using the Mann–Whitney U test
with Hodges-Lehman 95%
confidence intervals (CI). Outcomes
were compared by using
independent t tests, x2 tests, or
Fisher’s exact tests as appropriate.
The duration of respiratory support
outcomes was analyzed by using
survival techniques and compared
by using the log-rank test. Deaths
and transfers that occurred while
patients were on respiratory support
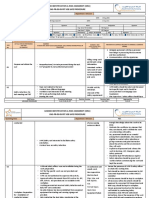
FIGURE 2 were censored in the analysis.
Study flow diagram.
Median Kaplan-Meier survival
estimates and 25th to 75th
A (in lipid emulsion) while on interim test. Criteria for early percentiles were reported. The
parenteral nutrition and 1820 IU/kg stopping of the trial (P , .001) were relationship between plasma retinol
per day of vitamin A when entirely based on the Haybittle-Peto levels and RDR and the shift test was
fed with fortified maternal or donor approach.36 assessed by using the Spearman
human milk. correlation coefficient. Post hoc
sensitivity analyses were performed
Sample Size to assess the consistency of
Data Collection and Management The normal SpO2 versus PIO2 curve in treatment effects when the
Deidentified data were stored in adults is shifted to the right of the correlation between siblings was
a secure, Web-based, and password- oxygen-hemoglobin dissociation accounted for and when adjusting for
protected Research Electronic Data curve by 6 kPa.20 Preterm infants baseline imbalance. Stata Release 16
Capture system.35 An independent with (moderate to severe) BPD had (Stata Corp, College Station, TX)
data monitoring committee reviewed a mean (SD) shift of 16.5 (4.7) kPa at software was used for sensitivity
the trial periodically for adverse a mean (SD) PMA of 37.2 (0.62) analyses by using a generalized
effects. One formal interim analysis weeks.24 A 20% (3.3 kPa) change in estimating equations approach on
was performed after the recruitment the shift would require 64 infants log-transformed shift measurements.
of 100 infants; no correction was with moderate to severe BPD SPSS version 25.0 (IBM SPSS
made to the reported P value for this (calculated by using the sample size Statistics, IBM Corporation, Armonk,
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
4 RAKSHASBHUVANKAR et al
TABLE 1 Baseline Maternal and Neonatal Demographic and Clinical Characteristics participant. Eight infants in the
Vitamin A (n = 94) Placebo (n = 94) vitamin A group and 5 infants in the
Maternal characteristics
placebo group died before discharge
Ethnicity, n (%)a from the hospital. The causes of death
White 52 (55) 57 (60) are shown in Table 3.
Aboriginal or TSI 15 (16) 20 (21)
Other 27 (28) 17 (18) Plasma retinol levels were
Antenatal steroids, any dose, n (%) 79* (84) 93* (98) significantly higher in the vitamin A
Antenatal steroids, 2 doses, n (%) 64 (68) 66 (70) group compared with the placebo
Histologic chorioamnionitis, n (%)b 62 (72) 58 (66) group on day 28 and at 34 weeks’
Diabetes, n (%) 8 (8) 8 (8)
PMA (Table 4). Plasma vitamin A
Hypertension, n (%) 7 (7) 11 (11)
Cesarean delivery, n (%) 48* (51) 65* (69) levels and RDR at 28 days were not
Neonatal characteristics correlated with the right shift of the
Gestational age, wk, mean (SD) 25.8 (1.4) 26.0 (1.3) SpO2 versus PIO2 curve. The Spearman
Birth weight, g, mean (SD) 853 (201) 852 (211) correlation between plasma vitamin A
Birth weight z score, mean (SD) 0.35 (0.87) 0.25 (0.94)
levels at 28 days and the right shift
Male sex, n (%) 49 (52) 49 (52)
IUGR, n (%) 4 (4) 7 (7) was 0.259 (P = .139). The correlation
Apgar score ,7 at 5 min, n (%) 29 (31) 27 (28) between RDR at 28 days and the right
CRIB39 score, median (25th–75th percentiles) 4 (1–7) 4 (1–7) shift of SpO2 versus PIO2 curve was
SNAPPE-240 score, median (25th–75th percentiles) 32 (23–48) 32 (22–46) 0.010 (P = .955).
CRIB, Clinical Risk Index for Babies; IUGR, intrauterine growth restriction; SNAPPE-2, Score for Neonatal Acute
Physiology–Perinatal Extension 2; TSI, Torres Strait Islander. We performed additional analyses to
a Because no numbers beyond decimal points are reported, percentages may not add up to 100. account for clustering due to twins
b Placenta not available for 6 women in the placebo group and 9 women in the vitamin A group.
and baseline imbalance in antenatal
* P , .05.
steroids in the placebo and vitamin A
groups. A sensitivity analysis of the
primary outcome to allow for sibling
NY) statistical software was used in the step-down unit before 34 weeks’ cluster intracorrelation revealed no
all other data analyses. All PMA, and nil per os order. substantive change to results (mean
hypothesis tests were two-sided, and effect 1.06; 95% CI: 0.97 to 1.15; P =
P values ,.05 were considered Baseline maternal and neonatal
.204): a mean effect of 1.06
statistically significant. characteristics were comparable
represents a 6% increase (95% CI:
between treatment groups (Table 1).
3% decrease to 15% increase) in
The median (25th–75th percentiles)
shift in the treated group compared
postnatal age when vitamin A was
RESULTS with the placebo group. An
started was 2 (1–3) days, and the
adjustment for antenatal steroid use
A total of 188 infants were recruited median (25th–75th percentiles)
(yes or no) to assess the influence of
into the study between December duration of vitamin A
this baseline imbalance between the
2016 and May 2019 (Fig 2). Twenty- supplementation was 48 (42–57)
placebo and treatment groups did
seven infants did not have a shift days. No infant developed feed
not change the results (results not
test at 36 weeks’ PMA (15 in the intolerance with the study
shown).
vitamin A group and 12 in the medication, and the study medication
placebo group) for various reasons, was not stopped in any infant
as shown in Fig 2. The remaining 79 because of adverse effects. Exposures DISCUSSION
infants in the vitamin A group and to antenatal steroids and cesarean Our RCT revealed that
82 infants in the placebo group had delivery were less frequent in the supplementation of water-soluble
shift measurements and were vitamin A group than in the vitamin A did not reduce the severity
included in the analysis of the placebo group. of BPD, as assessed by the shift test,
primary outcome. More than 80% of despite the increased plasma vitamin
The shift did not differ between study
the expected doses of the study A levels. To our knowledge, this is the
groups (Table 2). The Hodges-
medications were administered in first RCT of enteral water-soluble
Lehman median difference estimate
vitamin A in extremely preterm
82% of the infants in the vitamin A was 0.10 (95% CI: 20.60 to 0.90; P =
group and 85% of the infants in the infants.
.730). Secondary clinical outcomes
placebo group. The reasons for not did not differ between groups Our trial is based on the encouraging
receiving doses were death, (Table 2). No adverse effects of finding in an adequately powered
withdrawal of consent, transfer to enteral vitamin A were seen in any RCT revealing decreased risk of BPD
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
PEDIATRICS Volume 147, number 1, January 2021 5
TABLE 2 Primary and Secondary Outcomes
Vitamin A (n = 94) Placebo (n = 94) P
Primary outcome
Right shift of SpO2 versus PIO2 curve, kPa, median (25th–75th percentiles)a 11.1 (9.5–13.7) 10.7 (9.5–13.1) .730
Secondary outcomes
Death before discharge, n (%) 8 (8) 5 (5) .388
Duration of oxygen, h, median (25th–75th percentiles)b 1195 (567–2461) 1156 (370–1911) .582
Duration of PP support, h, median (25th–75th percentiles)b 1597 (1205–2084) 1620 (1339–2024) .302
Duration of MV, h, median (25th–75th percentiles)b 66 (19–644) 80 (20–436) .422
Duration of CPAP and/or HHF, h, median (25th–75th percentiles)b 1432 (1126–1645) 1421 (1222–1598) .417
Moderate-severe BPD29 at 36 weeks’ gestation, n (%) 36 (38) 35 (37) .988
Postnatal steroids for BPD,29 n (%) 14 (15) 12 (13) .651
ROP requiring treatment, n (%) 6 (6) 6 (6) .898
Sepsis suspected or proven, n (%) 31 (33) 30 (32) .876
IVH30 grade 3 or 4 or PVL, n (%) 8 (8) 7 (7) .788
MRI, n (%)
Not abnormal 57 (61) 54 (58) .918
Abnormal 20 (21) 22 (24) .918
Scan not done 17 (18) 18 (19) .851
NEC31 stage 2a or more, n (%) 4 (4) 3 (3) .989
Shunt, median (25th–75th percentiles) 6 (0–12) 5 (0–12) .636
Oxygen support on discharge from the hospital, n (%)
No oxygen 49 (52) 53 (56) .825
Oxygen 8 (8) 8 (8) .825
Not discharged from the hospital 37 (39) 33 (35) .546
Wt gain, g/d, mean (95% CI) 22 (21 to 23) 23 (22 to 24) .702
Discharge wt, g, mean (95% CI) 3099 (2940 to 3260) 3081 (2930 to 324)0 .877
Discharge wt z score, mean (95% CI) 20.70 (20.90 to 20.49) 20.77 (20.95 to 20.58) .653
Duration of hospitalization, d, median (25th–75th percentiles)b 108 (89–129) 102 (87–126) .664
HHF, humidified high flow; MV, mechanical ventilation; PP, positive pressure (includes MV, CPAP, and HHF); PVL, periventricular leukomalacia; ROP, retinopathy of prematurity.
a Seventy-nine infants in the vitamin A group and 82 infants in the placebo group had a shift test.
b Data summaries represent Kaplan-Meier survival estimates.
at 36 weeks’ PMA (relative risk: 0.85; Our findings are consistent with gestation: 30.5 weeks; only 26 of 196
95% CI: 0.73 to 0.98) in extremely these 2 studies, except we found infants ,28 weeks).
low birth weight infants treated with improved plasma retinol levels with
IM vitamin A (5000 IU, 3 times per The lack of benefit of enteral vitamin
vitamin A supplementation,
week for 4 weeks).41 However, this A for reducing the severity of BPD in
confirming that the water-soluble
parenteral treatment approach is our study is unlikely to be due to
preparation is absorbed in extremely inadequate plasma retinol levels for
routinely not used because it
preterm infants. Our findings are the following reasons: (1) the plasma
involves repeated IM injections in
consistent with those reported by retinol levels in our study were
preterm infants. Enteral vitamin A
Basu et al.19 Furthermore, they comparable to those after IM
offers an alternative approach to
preventing BPD. The RCTs by Wardle confirm that an increase in plasma supplementation in the study by
et al16 and Calisici et al15 revealed no retinol levels is achievable in Tyson et al,41 which revealed benefit;
benefit of enteral vitamin A for extremely preterm infants as (2) plasma retinol levels and RDR at
improving plasma retinol levels or opposed to the more mature infants day 28 were not correlated with the
prevention of BPD at 36 weeks’ PMA. reported by Basu et al19 (median severity of BPD; and (3) our duration
of vitamin A supplementation was
longer compared to that in previous
studies (6–11 weeks versus 4
TABLE 3 Causes of Death in the Study Groups weeks).16,41
Cause of Death Vitamin A Placebo
Group, n Group, n The ineffectiveness of vitamin A in
Severe BPD 2 0
our study compared to previous
Pulmonary hemorrhage 1 1 studies is more likely related to the
NEC 3 2 overall less severe lung disease in our
IVH 1 0 cohort, as indicated by values for the
Sepsis 1 2 right shift of the SpO2 versus PIO2
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
6 RAKSHASBHUVANKAR et al
TABLE 4 Subgroups of Infants Who had Vitamin A Levels Tested at Day 28 (n = 35) and 34 Weeks’ PMA measure the severity of BPD, and the
(n = 36) use of a water-soluble vitamin A in
Vitamin A Placebo P extremely preterm infants at highest
Median 25th–75th Median 25th–75th risk for BPD.
Percentiles Percentiles
The limitations of our study need to
Day 28a be acknowledged. These include the
Plasma retinol, µg/dL 26.4 18.1–33.3 14.9 9.8–27.3 .023
availability of plasma vitamin A levels
RDR, % 18.2 6.8–28.1 28.7 6.3–39.0 .271
34 wk PMAb in only a fraction of participants. We
Plasma retinol, µg/dL 21.5 18.4–23.5 18.1 11.8–19.7 .014 did not monitor vitamin A levels in all
RDR, % 9.0 6.9–17.9 12.9 5.6–27.7 .375 infants because of the safety of
a n = 20 in the vitamin A group; n = 15 in the placebo group. supplementation reported in
b n = 18 in the vitamin A group; n = 18 in the placebo group. previous studies, the uncertainty of
normal levels in extremely preterm
infants, the lack of clinical utility, the
curve. Indeed only 27 (34%) infants day), indicating optimal vitamin A
and increased risk of iatrogenic
in the vitamin A group and 26 (32%) intake as per the current
anemia.41 Another limitation was the
infants in the placebo group had shift guidelines.44–47
small sample size for the outcome of
values consistent with moderate to 3. The routine use of prophylactic moderate to severe BPD as per
severe BPD.25,26 Furthermore, the caffeine48,49: Details of caffeine NICHD criteria, with the NICHD
major vitamin A supplementation supplementation were not criteria being more widely used and
trials (by Tyson et al41 and Wardle reported by Tyson et al.41 Because more readily interpreted than the
et al16) for BPD were conducted 2 prophylactic caffeine has emerged shift test.26 However, the NICHD
decades ago. Four contemporary only over the last 15 years, the criteria for BPD have limitations, as
lung-protective management benefits of this intervention may discussed earlier.18,25 The shift test is
strategies adopted in our unit may not have been exploited in the trial suitable for use as an outcome
explain the lower severity of BPD in of Tyson et al.41,48,49 indicator of BPD severity in clinical
our study versus these earlier
4. Probiotic supplementation: trials given its scientific and proven
studies:
Considering the role of ability to discriminate from the
1. Routine use of a lung-protective inflammation in the pathogenesis semiquantitative NICHD disease
ventilation strategy (early of BPD, probiotics may reduce the severity classification at a population
preferential use of CPAP, risk of BPD by altering the gut level.23,24 It is being implemented
prophylactic or low threshold microbiota.50 Current evidence across Australian and New Zealand
(inspired oxygen #30%) for from systematic reviews of RCTs is Neonatal Network units for
surfactant administration, volume- inadequate for extremely low birth benchmarking.53. The process will
targeted ventilation, and early weight infants to support this provide data on the correlation
extubation)42,43: The median hypothesis.51 between the shift test with long-term
duration of ventilation in the developmental and respiratory
control group of our study was In summary, it is likely that improved outcomes.
80 hours (3.3 days). Although standards of care over the last 2
decades have reduced the severity of Our study does not provide
Tyson et al41 did not report the
BPD, making it difficult to replicate a direct comparison between IM
duration of ventilation or
the beneficial effects of IM vitamin A vitamin A and enteral vitamin A
ventilation strategy, 48% of infants
on BPD reported by Tyson et al.41 supplementation for the prevention
in their control group were
Adoption of lung-protective strategies of BPD. IM vitamin A was not
ventilated on day 28 of life. The
and an aggressive approach to the included as a third intervention for
increasing use of noninvasive the following reasons: (1) IM
nutrition of extremely preterm
ventilation and other lung- vitamin A for prevention of BPD is
infants may explain the findings of
protective strategies for preterm not widely practiced because of
a recent study in which a national
infants is reported in many parts discomfort and risk of trauma on
shortage of vitamin A was not
of the world.42,43 a background of only modest
associated with an increase in the
2. Optimal vitamin A intake: the incidence of BPD.52 benefit,54,55 (2) it would have been
baseline vitamin A intake was ethically challenging to include this
higher in our study (1820 IU/kg The strengths of our study include painful procedure as a control arm
per day) compared with the study a robust methodology, the use of the because IM vitamin A is not
by Tyson et al41 (1000 IU/kg per shift test as the objective scale to a routine practice in Australia, (3)
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
PEDIATRICS Volume 147, number 1, January 2021 7
blinding of the intervention would ACKNOWLEDGMENTS
have been difficult, and (4) we
ABBREVIATIONS
We acknowledge the Data and Safety
anticipated difficulty in obtaining BPD: bronchopulmonary dysplasia
Committee monitoring members:
parental consent and clinician CI: confidence interval
Associate Professor Shripada Rao
acceptance of the trial. CPAP: continuous positive airway
(neonatal consultant, Perth
pressure
Children’s Hospital), Dr André
IM: intramuscular
CONCLUSIONS Schultz (pediatric respiratory
IVH: intraventricular hemorrhage
Our study reveals that enteral water- consultant, Perth Children’s
NEC: necrotizing enterocolitis
soluble vitamin A improves plasma Hospital), and Ms Nabeelah
NICHD: Eunice Kennedy Shriver
retinol levels in extremely preterm Mukadam (senior pharmacist); the
National Institute of Child
infants but does not reduce the pharmacists: Ms Antonia Wong and
Health and Human
severity of BPD. The lack of benefit of Ms Sarah Woodland; the research
Development
enteral vitamin A is likely related to assistants: Ms Jane Choi, Ms
PIO2: inspired oxygen pressure
the overall low severity of BPD in our Christine Astell, and Ms Amanda
PMA: postmenstrual age
study population. Further studies of Woods; the neonatal nurses and
RCT: randomized controlled trial
enteral water-soluble vitamin A are doctors; and, most importantly, the
RDR: relative dose response
essential in preterm infants with participating infants and families,
SpO2: pulse oximeter saturation
suboptimal vitamin A intake and high without whom the study was not
severity of BPD. possible.
Deidentified individual participant data will be made available in addition to study protocols, the statistical analysis plan, and the informed consent form. The data
will be made available after publication to researchers who provide a methodologically sound proposal for use in achieving the goals of the approved proposal.
Proposals should be submitted to the corresponding author.
This trial has been registered with the Australian New Zealand Clinical Trials Registry (https://www.anzctr.org.au/) (identifier ACTRN12616000408482).
DOI: https://doi.org/10.1542/peds.2020-009985
Accepted for publication Sep 18, 2020
Address correspondence to Abhijeet A. Rakshasbhuvankar, FRACP, Neonatal Clinical Care Unit, King Edward Memorial Hospital, 374 Bagot Rd, Subiaco, WA 6008,
Australia. E-mail: abhijeet.rakshasbhuvankar@health.wa.gov.au
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright © 2021 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Pillow is funded the National Health and Medical Research Council Fellowship (RF1077691); the National Health and Medical Research Council Centres
of Research Excellence (GNT0157514) supported aspects of this study, and the Channel 7 Telethon Trust provided most of the funding for the study.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
REFERENCES
1. Gibson AM, Doyle LW. Respiratory adolescence and early adulthood in dysplasia: impact of the physiologic
outcomes for the tiniest or most individuals born very preterm or with definition. Early Hum Dev. 2012;88(7):
immature infants. Semin Fetal Neonatal very low birthweight compared with 509–515
Med. 2014;19(2):105–111 controls born at term or with normal
6. Twilhaar ES, Wade RM, de Kieviet JF, van
birthweight: a meta-analysis of
2. Gibson AM, Reddington C, McBride L, Goudoever JB, van Elburg RM,
individual participant data. Lancet
Callanan C, Robertson C, Doyle LW. Lung Oosterlaan J. Cognitive outcomes of
Respir Med. 2019;7(8):677–686
function in adult survivors of very low children born extremely or very
birth weight, with and without 4. Baraldi E, Filippone M. Chronic lung preterm since the 1990s and associated
bronchopulmonary dysplasia. Pediatr disease after premature birth. N Engl risk factors: a meta-analysis and meta-
Pulmonol. 2015;50(10):987–994 J Med. 2007;357(19):1946–1955 regression. JAMA Pediatr. 2018;172(4):
361–367
3. Doyle LW, Andersson S, Bush A, et al.; 5. Natarajan G, Pappas A, Shankaran S,
Adults Born Preterm International et al. Outcomes of extremely low birth 7. Beaudoin S, Tremblay GM, Croitoru D,
Collaboration. Expiratory airflow in late weight infants with bronchopulmonary Benedetti A, Landry JS. Healthcare
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
8 RAKSHASBHUVANKAR et al
utilization and health-related quality of interactions for absorption. Food Chem. 28. Lockwood GG, Fung NLS, Jones JG.
life of adult survivors of preterm birth 2015;172:155–160 Evaluation of a computer program for
complicated by bronchopulmonary non-invasive determination of
18. Rakshasbhuvankar A, Patole S, Simmer
dysplasia. Acta Paediatr. 2013;102(6): pulmonary shunt and ventilation-
K, Pillow JJ. Enteral vitamin A for
607–612 perfusion mismatch. J Clin Monit
reducing severity of bronchopulmonary
Comput. 2014;28(6):581–590
8. Mandell EW, Kratimenos P, Abman SH, dysplasia in extremely preterm infants:
Steinhorn RH. Drugs for the prevention a randomised controlled trial. BMC 29. Ehrenkranz RA, Walsh MC, Vohr BR,
and treatment of bronchopulmonary Pediatr. 2017;17(1):204 et al.; National Institutes of Child Health
dysplasia. Clin Perinatol. 2019;46(2): and Human Development Neonatal
19. Basu S, Khanna P, Srivastava R, Kumar
291–310 Research Network. Validation of the
A. Oral vitamin A supplementation in
National Institutes of Health consensus
9. Poets CF, Lorenz L. Prevention of very low birth weight neonates:
definition of bronchopulmonary
bronchopulmonary dysplasia in a randomized controlled trial. Eur
dysplasia. Pediatrics. 2005;116(6):
extremely low gestational age J Pediatr. 2019;178(8):1255–1265
1353–1360
neonates: current evidence. Arch Dis
20. Roe PG, Jones JG. Analysis of factors 30. Papile LA, Burstein J, Burstein R, Koffler
Child Fetal Neonatal Ed. 2018;103(3):
which affect the relationship between H. Incidence and evolution of
F285–F291
inspired oxygen partial pressure and subependymal and intraventricular
10. De Luca LM. Multiple mechanisms: the arterial oxygen saturation. Br hemorrhage: a study of infants with
example of vitamin A. Basic Life Sci. J Anaesth. 1993;71(4):488–494 birth weights less than 1,500 gm.
1993;61:17–25 J Pediatr. 1978;92(4):529–534
21. Sapsford DJ, Jones JG. The PIO2 vs.
11. Massaro D, Massaro GD. Lung SpO2 diagram: a non-invasive measure 31. Bell MJ. Neonatal necrotizing
development, lung function, and of pulmonary oxygen exchange. Eur enterocolitis. N Engl J Med. 1978;298(5):
retinoids. N Engl J Med. 2010;362(19): J Anaesthesiol. 1995;12(4):375–386 281–282
1829–1831
22. Smith HL, Jones JG. Non-invasive 32. Georgieff MK, Mammel MC, Mills MM,
12. Ozer EA, Kumral A, Ozer E, et al. Effect of assessment of shunt and ventilation/ Gunter EW, Johnson DE, Thompson TR.
retinoic acid on oxygen-induced lung perfusion ratio in neonates with Effect of postnatal steroid
injury in the newborn rat. Pediatr pulmonary failure. Arch Dis Child Fetal administration on serum vitamin A
Pulmonol. 2005;39(1):35–40 Neonatal Ed. 2001;85(2):F127–F132 concentrations in newborn infants with
13. James ML, Ross AC, Bulger A, Philips JB 23. Rowe L, Jones JG, Quine D, Bhushan SS, respiratory compromise. J Pediatr.
III, Ambalavanan N. Vitamin A and Stenson BJ. A simplified method for 1989;114(2):301–304
retinoic acid act synergistically to deriving shunt and reduced VA/Q in 33. Kennedy KA, Stoll BJ, Ehrenkranz RA,
increase lung retinyl esters during infants. Arch Dis Child Fetal Neonatal et al.; The NICHD Neonatal Research
normoxia and reduce hyperoxic lung Ed. 2010;95(1):F47–F52 Network. Vitamin A to prevent
injury in newborn mice. Pediatr Res. bronchopulmonary dysplasia in very-
24. Quine D, Wong CM, Boyle EM, Jones JG,
2010;67(6):591–597 low-birth-weight infants: has the dose
Stenson BJ. Non-invasive measurement
14. Ng-Blichfeldt JP, Alçada J, Montero MA, of reduced ventilation: perfusion ratio been too low? Early Hum Dev. 1997;
et al. Deficient retinoid-driven and shunt in infants with 49(1):19–31
angiogenesis may contribute to failure bronchopulmonary dysplasia: 34. Tanumihardjo SA. Vitamin A:
of adult human lung regeneration in a physiological definition of the disease. biomarkers of nutrition for
emphysema. Thorax. 2017;72(6): Arch Dis Child Fetal Neonatal Ed. 2006; development. Am J Clin Nutr. 2011;94(2):
510–521 91(6):F409–F414 658S–665S
15. Calisici E, Yarci E, Degirmencioglu H, 25. Svedenkrans J, Stoecklin B, Jones JG, 35. Harris PA, Taylor R, Thielke R, Payne J,
et al. The effects of early oral vitamin A Doherty DA, Pillow JJ. Physiology and Gonzalez N, Conde JG. Research
treatment on the prevention of predictors of impaired gas exchange in electronic data capture (REDCap)–a
bronchopulmonary displasia in the low infants with bronchopulmonary metadata-driven methodology and
birth weight infants [abstract]. Arch Dis dysplasia. Am J Respir Crit Care Med. workflow process for providing
Child. 2014;99(suppl 2):A494 2019;200(4):471–480 translational research informatics
16. Wardle SP, Hughes A, Chen S, Shaw NJ. 26. Jobe AH, Bancalari E. support. J Biomed Inform. 2009;42(2):
Randomised controlled trial of oral Bronchopulmonary dysplasia. Am 377–381
vitamin A supplementation in preterm J Respir Crit Care Med. 2001;163(7): 36. Schulz KF, Grimes DA. Multiplicity in
infants to prevent chronic lung disease. 1723–1729 randomised trials II: subgroup and
Arch Dis Child Fetal Neonatal Ed. 2001; interim analyses. Lancet. 2005;
27. Moher D, Hopewell S, Schulz KF, et al.
84(1):F9–F13 365(9471):1657–1661
CONSORT 2010 explanation and
17. Goncalves A, Roi S, Nowicki M, et al. Fat- elaboration: updated guidelines for 37. Stoll BJ, Hansen NI, Bell EF, et al.; Eunice
soluble vitamin intestinal absorption: reporting parallel group randomised Kennedy Shriver National Institute of
absorption sites in the intestine and trials. BMJ. 2010;340:c869 Child Health and Human Development
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
PEDIATRICS Volume 147, number 1, January 2021 9
Neonatal Research Network. Neonatal Neonatal Research Network. Trends in 50. Ryan FJ, Drew DP, Douglas C, et al.
outcomes of extremely preterm infants care practices, morbidity, and mortality Changes in the composition of the gut
from the NICHD Neonatal Research of extremely preterm neonates, 1993- microbiota and the blood
Network. Pediatrics. 2010;126(3): 2012. JAMA. 2015;314(10):1039–1051 transcriptome in preterm infants at
443–456 less than 29 weeks gestation diagnosed
44. Agostoni C, Buonocore G, Carnielli VP,
38. Chow SSW, Le Marsney R, Haslam R, Lui with bronchopulmonary dysplasia.
et al.; ESPGHAN Committee on Nutrition.
K. Report of the Australian and New mSystems. 2019;4(5):e00484-19
Enteral nutrient supply for preterm
Zealand Neonatal Network 2014. infants: commentary from the European 51. Villamor-Martínez E, Pierro M, Cavallaro
Sydney, Australia: Australian and New Society of Paediatric Gastroenterology, G, Mosca F, Kramer B, Villamor E.
Zealand Neonatal Network; 2016 Hepatology and Nutrition Committee on Probiotic supplementation in preterm
39. The International Neonatal Network. Nutrition. J Pediatr Gastroenterol Nutr. infants does not affect the risk of
The CRIB (clinical risk index for babies) 2010;50(1):85–91 bronchopulmonary dysplasia: a meta-
score: a tool for assessing initial analysis of randomized controlled
45. Adamkin DH, Radmacher PG. Current trials. Nutrients. 2017;9(11):1197
neonatal risk and comparing trends and future challenges in
performance of neonatal intensive care neonatal parenteral nutrition. 52. Tolia VN, Murthy K, McKinley PS, Bennett
units. [published correction appears in J Neonatal Perinatal Med. 2014;7(3): MM, Clark RH. The effect of the national
Lancet. 1993;342(8871):626]. Lancet. 157–164 shortage of vitamin A on death or
1993;342(8865):193–198 chronic lung disease in extremely low-
46. Ho MY, Yen YH. Trend of nutritional birth-weight infants. JAMA Pediatr.
40. Richardson DK, Corcoran JD, Escobar
support in preterm infants. Pediatr 2014;168(11):1039–1044
GJ, Lee SK. SNAP-II and SNAPPE-II:
Neonatol. 2016;57(5):365–370
simplified newborn illness severity and 53. Australian and New Zealand Neonatal
mortality risk scores. J Pediatr. 2001; 47. Cleminson JS, Zalewski SP, Embleton Network. Data dictionaries. Available at:
138(1):92–100 ND. Nutrition in the preterm infant: https://anznn.net/dataresources/
41. Tyson JE, Wright LL, Oh W, et al.; National what’s new? Curr Opin Clin Nutr Metab datadictionaries. Accessed May 12, 2020
Institute of Child Health and Human Care. 2016;19(3):220–225
54. Ambalavanan N, Kennedy K, Tyson J,
Development Neonatal Research 48. Dobson NR, Patel RM, Smith PB, et al. Carlo WA. Survey of vitamin A
Network. Vitamin A supplementation for Trends in caffeine use and association supplementation for extremely-low-
extremely-low-birth-weight infants. between clinical outcomes and timing birth-weight infants: is clinical practice
N Engl J Med. 1999;340(25):1962–1968 of therapy in very low birth weight consistent with the evidence? J Pediatr.
42. Owen LS, Manley BJ, Davis PG, Doyle LW. infants. J Pediatr. 2014;164(5): 2004;145(3):304–307
The evolution of modern respiratory 992–998.e3
55. Darlow BA, Graham PJ, Rojas-Reyes MX.
care for preterm infants. Lancet. 2017; 49. Schmidt B, Roberts RS, Davis P, et al.; Vitamin A supplementation to prevent
389(10079):1649–1659 Caffeine for Apnea of Prematurity Trial mortality and short- and long-term
43. Stoll BJ, Hansen NI, Bell EF, et al.; Eunice Group. Caffeine therapy for apnea of morbidity in very low birth weight
Kennedy Shriver National Institute of prematurity. N Engl J Med. 2006; infants. Cochrane Database Syst Rev.
Child Health and Human Development 354(20):2112–2121 2016;(8):CD000501
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
10 RAKSHASBHUVANKAR et al
Enteral Vitamin A for Reducing Severity of Bronchopulmonary Dysplasia: A
Randomized Trial
Abhijeet A. Rakshasbhuvankar, Karen Simmer, Sanjay K. Patole, Benjamin
Stoecklin, Elizabeth A. Nathan, Michael W. Clarke and J. Jane Pillow
Pediatrics 2021;147;
DOI: 10.1542/peds.2020-009985 originally published online December 18, 2020;
Updated Information & including high resolution figures, can be found at:
Services http://pediatrics.aappublications.org/content/147/1/e2020009985
References This article cites 52 articles, 10 of which you can access for free at:
http://pediatrics.aappublications.org/content/147/1/e2020009985#BI
BL
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://www.aappublications.org/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
http://www.aappublications.org/site/misc/reprints.xhtml
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
Enteral Vitamin A for Reducing Severity of Bronchopulmonary Dysplasia: A
Randomized Trial
Abhijeet A. Rakshasbhuvankar, Karen Simmer, Sanjay K. Patole, Benjamin
Stoecklin, Elizabeth A. Nathan, Michael W. Clarke and J. Jane Pillow
Pediatrics 2021;147;
DOI: 10.1542/peds.2020-009985 originally published online December 18, 2020;
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pediatrics.aappublications.org/content/147/1/e2020009985
Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
has been published continuously since 1948. Pediatrics is owned, published, and trademarked by
the American Academy of Pediatrics, 345 Park Avenue, Itasca, Illinois, 60143. Copyright © 2021
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on April 16, 2021
You might also like
- Prep 2023Document909 pagesPrep 2023Imran A. Isaac100% (7)
- 100 IELTS Writing Sample Questions: Criminal JusticeDocument20 pages100 IELTS Writing Sample Questions: Criminal Justicebita bagheriNo ratings yet
- Principles and Practice of Gynecologic Oncology: Handbook ForDocument288 pagesPrinciples and Practice of Gynecologic Oncology: Handbook ForPeter Osundwa KitekiNo ratings yet
- Effect of Lactobacillus Rhamnosus On Serum Uremic Toxins (Phenol and P-Cresol) in Hemodialysis PatientsDocument7 pagesEffect of Lactobacillus Rhamnosus On Serum Uremic Toxins (Phenol and P-Cresol) in Hemodialysis PatientsOctavianus KevinNo ratings yet
- Iyengar RSL 2015Document7 pagesIyengar RSL 2015wisdom loverNo ratings yet
- Association Between Serum Vitamin A Levels and Recurrent Respiratory Tract Infections in ChildrenDocument9 pagesAssociation Between Serum Vitamin A Levels and Recurrent Respiratory Tract Infections in Childrenjulio cesarNo ratings yet
- Cormack 2021 - Neonatal Refeeding Syndrome and Clinical Outcome in ELBW Secondary Cohort Analysis ProVIDe TrialDocument14 pagesCormack 2021 - Neonatal Refeeding Syndrome and Clinical Outcome in ELBW Secondary Cohort Analysis ProVIDe TrialKarla LapendaNo ratings yet
- 2008 Fluid Regimens in The First Week of Life May Increase Risk of PDADocument6 pages2008 Fluid Regimens in The First Week of Life May Increase Risk of PDAyaritzaalviarezNo ratings yet
- RandomizedDocument7 pagesRandomizedmechi_ghisyaNo ratings yet
- Early Energy and Protein Intakes and AssociationsDocument7 pagesEarly Energy and Protein Intakes and Associationspaulo.freitas.machrentNo ratings yet
- ELZEN Et Al-2008-Alimentary Pharmacology & Therapeutics Vit B12Document7 pagesELZEN Et Al-2008-Alimentary Pharmacology & Therapeutics Vit B12jcNo ratings yet
- Oral Vitamin A Supplementation in Very Low Birth Weight Neonates: A Randomized Controlled TrialDocument11 pagesOral Vitamin A Supplementation in Very Low Birth Weight Neonates: A Randomized Controlled TrialNazihan Safitri AlkatiriNo ratings yet
- WRIGHT 2016 - Continuous Positive Airway Pressure To Prevent Neonatal Lung InjuryDocument10 pagesWRIGHT 2016 - Continuous Positive Airway Pressure To Prevent Neonatal Lung InjuryRafael JustinoNo ratings yet
- VITAMINB-12ANDFOLICACID AJCN July2013Document8 pagesVITAMINB-12ANDFOLICACID AJCN July2013afifahNo ratings yet
- Pi Is 1875957219305510Document10 pagesPi Is 1875957219305510madimadi11No ratings yet
- 2003 112 191 Committee On Fetus and NewbornDocument4 pages2003 112 191 Committee On Fetus and Newbornsherlin_de_wardanaNo ratings yet
- Intestinal - Rehabilitation - Programs - in - The Pediatric Failure and Shhort Bowel SyndromeDocument9 pagesIntestinal - Rehabilitation - Programs - in - The Pediatric Failure and Shhort Bowel SyndromeMinosska Pinto LazoNo ratings yet
- Impacto BrueDocument12 pagesImpacto BrueNATALIA LEMOS CALLENo ratings yet
- 09 2019 Pediatric Neonatology LAYOUT R2Document50 pages09 2019 Pediatric Neonatology LAYOUT R2khalid alharbiNo ratings yet
- Clinical Practice Guideline: The Diagnosis, Management, and Prevention of BronchiolitisDocument32 pagesClinical Practice Guideline: The Diagnosis, Management, and Prevention of BronchiolitisMarina LaquiseNo ratings yet
- Oxido NitricoDocument5 pagesOxido NitricoAmparito TitoNo ratings yet
- Journal ReadingDocument13 pagesJournal Readingayu amsariNo ratings yet
- 2008 PEDIATRICS Vitamin D Deficiency in Children and Its Management PediatricsDocument22 pages2008 PEDIATRICS Vitamin D Deficiency in Children and Its Management Pediatricssheyla alegreNo ratings yet
- Caffeine A Lung Drug For All Very Low Birth Weight PretermsDocument6 pagesCaffeine A Lung Drug For All Very Low Birth Weight PretermsSheila Cruz RodriguezNo ratings yet
- Malnutrition in Congenital Heart DiseaseDocument2 pagesMalnutrition in Congenital Heart DiseasenisaNo ratings yet
- Lodha 2014Document12 pagesLodha 2014madhuNo ratings yet
- Early Total Parenteral Nutrition in Very Low Birthweight Infants: Is It Safe? Is It Worth It?Document3 pagesEarly Total Parenteral Nutrition in Very Low Birthweight Infants: Is It Safe? Is It Worth It?YAKENLY YARENY MAZARIEGOS OROZCONo ratings yet
- Diet in Pregnancy - More Than Food: ReviewDocument7 pagesDiet in Pregnancy - More Than Food: ReviewDiego De Leon ZuritaNo ratings yet
- Lactobacillus Therapy For Acute Infectious Diarrhea in Children A Meta-AnalysisDocument9 pagesLactobacillus Therapy For Acute Infectious Diarrhea in Children A Meta-AnalysisfahrunisaNo ratings yet
- Acta PaediatricaDocument13 pagesActa PaediatricaDefranky TheodorusNo ratings yet
- Espen FQ NiñosDocument5 pagesEspen FQ NiñosCarla ANo ratings yet
- J Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The AdultDocument30 pagesJ Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The Adultsulemi castañonNo ratings yet
- 2005 ASSOCIATION BETWEEN FLUID INTAKE ANDWEIGHT LOSS DURING THE Ten DaysDocument5 pages2005 ASSOCIATION BETWEEN FLUID INTAKE ANDWEIGHT LOSS DURING THE Ten DaysyaritzaalviarezNo ratings yet
- Knowledge and Recommendations Vitamin D Deficiency in Children and Its Management: Review of CurrentDocument22 pagesKnowledge and Recommendations Vitamin D Deficiency in Children and Its Management: Review of Currentagatha febrinaNo ratings yet
- PIIS0022347617301828Document4 pagesPIIS0022347617301828adkhiatul muslihatinNo ratings yet
- Nicu 1Document7 pagesNicu 1PPDS ANAK FK USUNo ratings yet
- Indicaciones NP Onc PedDocument7 pagesIndicaciones NP Onc PedSebastian MarinNo ratings yet
- Pitfalls, Problems, and Progress in Bronchopulmonary DysplasiaDocument14 pagesPitfalls, Problems, and Progress in Bronchopulmonary Dysplasiatrixie2k7No ratings yet
- Cafeina DBPDocument6 pagesCafeina DBPVictoria Maslucán BorborNo ratings yet
- A. Brief Resume of Intended WorkDocument6 pagesA. Brief Resume of Intended WorkRabi DhakalNo ratings yet
- ChoosingWisely PHM PDFDocument2 pagesChoosingWisely PHM PDFAhraNo ratings yet
- J Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The AdultDocument30 pagesJ Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The AdultPabloNo ratings yet
- Vitamin DDocument11 pagesVitamin DCastiglianoNo ratings yet
- Implementation of A Guideline To Decrease Use of Acid Suppresing Medications in The NicuDocument12 pagesImplementation of A Guideline To Decrease Use of Acid Suppresing Medications in The NicuNoviaNo ratings yet
- Jurnal Refrat Vitamin K PDFDocument4 pagesJurnal Refrat Vitamin K PDFTia Amalia Puti RenaeryNo ratings yet
- Vitamin D Birth Cohort StudyDocument9 pagesVitamin D Birth Cohort StudyRita ChatrinNo ratings yet
- Varuzza Et Al-2019-Environmental ToxicologyDocument10 pagesVaruzza Et Al-2019-Environmental ToxicologyCharles santos da costaNo ratings yet
- Litonjua 2014Document14 pagesLitonjua 2014odivarNo ratings yet
- (2019) Parenteral Nutrition in The ICU Lessons Learned Over The Past Few YearsDocument7 pages(2019) Parenteral Nutrition in The ICU Lessons Learned Over The Past Few YearsAnna Maria Ariesta PutriNo ratings yet
- How To Use Faecal Calprotectin in Management of PaDocument7 pagesHow To Use Faecal Calprotectin in Management of PauglyangelNo ratings yet
- 2014 Guideline For The Evaluation of Cholestatic Jaundice in InfantsDocument61 pages2014 Guideline For The Evaluation of Cholestatic Jaundice in InfantsHenry BarberenaNo ratings yet
- Acute Kidney Injury in ChildrenDocument8 pagesAcute Kidney Injury in ChildrenInfectologia ClinicaNo ratings yet
- Two Case Reports of Successful Treatment of Cholestasis With Steroids in Patients With PFIC-2Document9 pagesTwo Case Reports of Successful Treatment of Cholestasis With Steroids in Patients With PFIC-2AstiaNingrumSanjayaNo ratings yet
- RESEARCH ARTICLEOpen AccessChallenges of Acute Peritoneal Dialysis Inextremely-Low-Birth-Weight Infants - Aretrospective Cohort StudyDocument9 pagesRESEARCH ARTICLEOpen AccessChallenges of Acute Peritoneal Dialysis Inextremely-Low-Birth-Weight Infants - Aretrospective Cohort StudysavitageraNo ratings yet
- Hyperbilirubinemia, Phototherapy, and Childhood Asthma: ObjectivesDocument11 pagesHyperbilirubinemia, Phototherapy, and Childhood Asthma: ObjectivesrizaniaNo ratings yet
- Wright Et Al 2022 PDFDocument9 pagesWright Et Al 2022 PDFRadu CiprianNo ratings yet
- Probiotic Supplementation in CKD - Double-Blind, Randomized, Placebo TrialsDocument9 pagesProbiotic Supplementation in CKD - Double-Blind, Randomized, Placebo TrialsVinod KumarNo ratings yet
- With Bacterial Meningitis Effect of Antibiotic Pretreatment On Cerebrospinal Fluid Profiles of ChildrenDocument7 pagesWith Bacterial Meningitis Effect of Antibiotic Pretreatment On Cerebrospinal Fluid Profiles of ChildrenImelda Ika ApriliaNo ratings yet
- Bronchopulmonary DysplasiaDocument3 pagesBronchopulmonary Dysplasiabun_yulianaNo ratings yet
- Displasia BroncopulmonarDocument12 pagesDisplasia BroncopulmonarRaul VillacresNo ratings yet
- Probiotics For Preterm Infants Which Ones To ChooseDocument4 pagesProbiotics For Preterm Infants Which Ones To ChoosePETERNo ratings yet
- Protein in Neonatal and Infant Nutrition: Recent Updates: 86th Nestlé Nutrition Institute Workshop, Beijing, May 2015From EverandProtein in Neonatal and Infant Nutrition: Recent Updates: 86th Nestlé Nutrition Institute Workshop, Beijing, May 2015No ratings yet
- JJGR v1 1004Document5 pagesJJGR v1 1004laurencia aliminNo ratings yet
- Gorfinkel 2020 Oi 200521 1596736886.419Document11 pagesGorfinkel 2020 Oi 200521 1596736886.419laurencia aliminNo ratings yet
- Self Isolation A Significant Contributor To Cannabis Use During The COVID 19 PandemicDocument5 pagesSelf Isolation A Significant Contributor To Cannabis Use During The COVID 19 Pandemiclaurencia aliminNo ratings yet
- Impact of Acute and Chronic Cannabis Use On Stress Response Regulation: Challenging The Belief That Cannabis Is An Effective Method For CopingDocument11 pagesImpact of Acute and Chronic Cannabis Use On Stress Response Regulation: Challenging The Belief That Cannabis Is An Effective Method For Copinglaurencia aliminNo ratings yet
- Cannabis and Covid 19 Reason ForDocument6 pagesCannabis and Covid 19 Reason Forlaurencia aliminNo ratings yet
- Tender For EndoscopeDocument131 pagesTender For EndoscopeJasjit Singh100% (1)
- CME Upper GI BleedDocument46 pagesCME Upper GI Bleedfarah fadzilNo ratings yet
- Arya 2014Document15 pagesArya 2014pratyusha vallamNo ratings yet
- Anterior FPDDocument5 pagesAnterior FPDAnand KumarNo ratings yet
- Nurse RoleDocument1 pageNurse RolechoobiNo ratings yet
- EdemaDocument3 pagesEdemaUdaya SreeNo ratings yet
- Bhert EoDocument2 pagesBhert EoRosette Ramos100% (7)
- Incidence of Post Op Pain After 1 Appointment Endodontic Treatment of Asymptomatic Pulpal Necrosis in Single Rooted Teeth Mulhern 1982Document6 pagesIncidence of Post Op Pain After 1 Appointment Endodontic Treatment of Asymptomatic Pulpal Necrosis in Single Rooted Teeth Mulhern 1982abcder1234No ratings yet
- Activity Completion Report: District Brigada Eskwela Kick - Off CeremonyDocument13 pagesActivity Completion Report: District Brigada Eskwela Kick - Off CeremonyNoriza BocaboNo ratings yet
- Spirulina Blue Green AlgaeDocument7 pagesSpirulina Blue Green AlgaeshamttNo ratings yet
- Jack Newman Latching HandoutDocument3 pagesJack Newman Latching HandoutOctavia Raica100% (1)
- Table of Contents Iadc Safety Meeting TopicsDocument4 pagesTable of Contents Iadc Safety Meeting TopicsfarisNo ratings yet
- Bladder Pain SyndromeDocument385 pagesBladder Pain SyndromeansarijavedNo ratings yet
- OHS-PR-09-03-F07 JOB SAFE PROCEDURE (19) Installation of Conductor JumperDocument14 pagesOHS-PR-09-03-F07 JOB SAFE PROCEDURE (19) Installation of Conductor Jumpermohammed tofiqNo ratings yet
- Surviving Part V PDFDocument12 pagesSurviving Part V PDFFortune RubengoNo ratings yet
- Amputation Rehabilitation and Prosthetic Restoration. From Surgery To Community ReintegrationDocument7 pagesAmputation Rehabilitation and Prosthetic Restoration. From Surgery To Community ReintegrationGabriela Istrati-StanciugelNo ratings yet
- Care & Maintenance of Contact LenseDocument26 pagesCare & Maintenance of Contact LenseGurria NaheedNo ratings yet
- Var TMP TMP Generated AABBTechnicalManual18thEd2014 AABB Technical Manual 18th Ed 2014Document824 pagesVar TMP TMP Generated AABBTechnicalManual18thEd2014 AABB Technical Manual 18th Ed 2014Hoàng Nguyễn VănNo ratings yet
- Models of DisabilityDocument7 pagesModels of DisabilityAnime PHNo ratings yet
- 02-11-2012 EditionDocument32 pages02-11-2012 EditionSan Mateo Daily JournalNo ratings yet
- GelafusalinfDocument5 pagesGelafusalinfToni Dafia PutraNo ratings yet
- PDF Cognitive Communication Disorders of Dementia Definition Diagnosis and Treatment 3 Ed Edition Kathryn Bayles Ebook Full ChapterDocument53 pagesPDF Cognitive Communication Disorders of Dementia Definition Diagnosis and Treatment 3 Ed Edition Kathryn Bayles Ebook Full Chapteryolanda.schwartz402100% (2)
- Development and In-Vitro Evaluation of Catechin Loaded Ethosomal Gel For Topical DeliveryDocument6 pagesDevelopment and In-Vitro Evaluation of Catechin Loaded Ethosomal Gel For Topical DeliveryRAPPORTS DE PHARMACIENo ratings yet
- Pengaruh Body Massage Terhadap Tingkat Depresi Ibu Nifas Di Bidan Praktik Mandiri Siyamtiningsih KaranganyarDocument8 pagesPengaruh Body Massage Terhadap Tingkat Depresi Ibu Nifas Di Bidan Praktik Mandiri Siyamtiningsih KaranganyarEnzel LinaNo ratings yet
- Deviation Permit/ConcessionDocument3 pagesDeviation Permit/ConcessionUnni AlsvikNo ratings yet
- Ban The BanDocument4 pagesBan The BanHamada BakheetNo ratings yet
- Derm Summary Table PDFDocument33 pagesDerm Summary Table PDFVas LillaNo ratings yet
- TESDA Circular No. 082-2020Document3 pagesTESDA Circular No. 082-2020Aileen K. LigmayoNo ratings yet