Professional Documents
Culture Documents
Ocs P Screening Guidelines
Ocs P Screening Guidelines
Uploaded by
Ali HusseinOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ocs P Screening Guidelines
Ocs P Screening Guidelines
Uploaded by
Ali HusseinCopyright:
Available Formats
Ontario Cervical Screening
Guidelines Summary
Revised October 2016—based on current (2012) screening guidelines
Ontario Cervical Special screening
Screening Program circumstances
Screening initiation
• Women who have sex with women
Women should begin screening for cervical cancer at age 21 if they are
should follow the same cervical
or have ever been sexually active. Women who are not sexually active
screening regimen as women who
by age 21 should delay cervical cancer screening until they are sexually
have sex with men.
active. Sexual activity includes intercourse, as well as digital or oral
sexual activity involving the genital area with a partner of either sex. • Pregnant women should be screened
according to the guidelines. Pregnancy
Screening interval does not alter the recommended screening
interval. Only conduct Pap tests during
If a woman’s cytology is normal, she should be screened every three
pre- and post-natal care if a woman
years. The absence of transformation zone is not a reason to repeat a Pap
is due for regular screening.
test earlier than the recommended interval. See reverse for management
of abnormal cytology. • Women who have undergone subtotal
hysterectomy and retained their cervix
Screening cessation should continue screening according
to the guidelines.
A woman may discontinue screening at age 70 if she has an adequate
and negative cytology screening history in the previous 10 years • Women who are immunocompromised
(i.e., three or more negative cytology tests). (e.g., HIV-positive or on long-term
immunosuppressants) should
receive annual screening.
Notes:
• Any visible cervical abnormalities or abnormal symptoms must be • Transgender men who have retained
investigated by a specialist (e.g., colposcopist, gyne-oncologist, their cervix should be screened according
gynecologist) regardless of cytology findings. to the guidelines.
• Cancer Care Ontario is working with the Ministry of Health and
Long-Term Care to implement HPV testing in the Ontario Cervical
Screening Program.
For more information and resources
Visit: cancercare.on.ca/pcresources | Call: 1-866-662-9233
Email: screenforlife@cancercare.on.ca
Ontario Guidelines for Follow-Up of Abnormal Cytology
Revised October 2016—recommendations for referral to colposcopy unchanged from
May 2012 guidelines summary
Refer directly to colposcopy for the following cytology report:
• High-grade squamous intraepithelial lesion (HSIL)
• Atypical squamous cells, cannot exclude HSIL (ASC-H)
• Atypical glandular cells (AGC), atypical endocervical cells, atypical endometrial cells (also consider endometrial sampling)
• Squamous carcinoma, adenocarcinoma, other malignant neoplasms.
Any visible cervical abnormalities or abnormal symptoms must be investigated by a specialist (e.g. colposcopist, gyne-oncologist,
gynecologist) regardless of cytology findings.
Diagnosis Recommended management
For women <30 years old (HPV triage is not recommended)
Repeat cytology Result: Normal Routine screening in 3 years
Result: Normal
Repeat cytology in 6 months in 6 months Result: ≥ASCUS Colposcopy
Result: ≥ASCUS Colposcopy
For women ≥30 years old
Atypical squamous
cells of undetermined HPV testing for oncogenic strains* Result: Negative Routine screening in 3 years
significance (ASCUS) Result: Positive Colposcopy
If HPV status is not known
Repeat cytology Result: Normal Routine screening in 3 years
Result: Normal
Repeat cytology in 6 months in 6 months Result: ≥ASCUS Colposcopy
Result: ≥ASCUS Colposcopy
Repeat cytology Result: Normal Routine screening in 3 years
Low-grade squamous Result: Normal
Repeat cytology in 6 months in 6 months Result: ≥ASCUS Colposcopy
intraepithelial lesion
(LSIL) † Result: ≥ASCUS Colposcopy
Or refer to colposcopy
Unsatisfactory for evaluation Repeat cytology in 3 months
• Pre-menopausal women who are asymptomatic require no action (continue to follow usual screening guidelines)
Benign endometrial
• Post-menopausal women require investigation, including adequate endometrial tissue sampling
cells on Pap tests
• Abnormal vaginal bleeding in any woman requires investigation, which should include adequate endometrial tissue sampling
* HPV testing is not currently funded by the Ministry of Health and Long-Term Care.
† Evidence suggests that either repeat cytology or colposcopy are acceptable management options after the first LSIL result. Although colposcopy may be useful for ruling out high-grade
lesions, low-grade abnormalities, particularly in young women, often regress on their own and may therefore be best managed by surveillance.
Screening/surveillance in primary care after discharge from colposcopy
The colposcopist should provide specific and individualized screening Screening/surveillance intervals
after discharge from colposcopy
recommendations when a woman is discharged from colposcopy:
• Women eligible for discharge from colposcopy who have normal, ASCUS or LSIL HPV status Recommended interval
cytology and a negative HPV test are at average risk and should be screened
Negative 3 years
every three years.
• Women eligible for discharge from colposcopy who have normal, ASCUS or LSIL cytology
and a positive HPV test are at elevated risk and should have annual surveillance. Positive Annual
• Women eligible for discharge from colposcopy, whose HPV status is not known, should
Follow recommendations
be screened according to risk-based recommendations made by the colposcopist. Unknown
from colposcopist
Re-referral to colposcopy should be based on screening results (cytology),
as per current guidelines.
For further information on coloposcopy, visit cancercare.on.ca/ocspresources
Need this information in an accessible format? 1-855-460-2647, TTY (416) 217-1815 publicaffairs@cancercare.on.ca
PCC2024
You might also like
- Clinical Internal Medicine Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2From EverandClinical Internal Medicine Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Rating: 4 out of 5 stars4/5 (2)
- Cancer ScreeningDocument37 pagesCancer ScreeningTomb RaiderNo ratings yet
- Pap TestDocument24 pagesPap TestAmirah MuhammadNo ratings yet
- Best Tarot Book 25Document5 pagesBest Tarot Book 25Classic Bobby100% (3)
- OCSPScreeningGuidelines June2020Document1 pageOCSPScreeningGuidelines June2020ixNo ratings yet
- Pap SmearDocument32 pagesPap SmearAmira Nasir100% (1)
- Pap Smear Guidelines: Baylor College of Medicine Anoop Agrawal, M.DDocument22 pagesPap Smear Guidelines: Baylor College of Medicine Anoop Agrawal, M.Dshygirl72No ratings yet
- Guidelines Colposcopy and Pap Smear Triage GuidelinesDocument12 pagesGuidelines Colposcopy and Pap Smear Triage Guidelinesbabarpdu100% (1)
- Management of Cervical Smears GoldenDocument47 pagesManagement of Cervical Smears GoldenFelixNo ratings yet
- Managment of Abnormal Pap SmearDocument78 pagesManagment of Abnormal Pap SmearMohammad AlrefaiNo ratings yet
- CYT 2113 Cytology I: Lesson 7: Introduction To Pap Smear TestDocument48 pagesCYT 2113 Cytology I: Lesson 7: Introduction To Pap Smear TestCarinaJongLeeNo ratings yet
- Abnormal Paps: DR Vidhi ChaudharyDocument29 pagesAbnormal Paps: DR Vidhi Chaudharyvidhi chaudharyNo ratings yet
- Pap Smear - Overview, Indications, PreparationDocument11 pagesPap Smear - Overview, Indications, PreparationBayu Surya DanaNo ratings yet
- CS-PUB-LAB-1 Cervical Cytology Management Recommendations Explanatory GuideDocument11 pagesCS-PUB-LAB-1 Cervical Cytology Management Recommendations Explanatory GuideMc Coral100% (1)
- P Ap SmearDocument4 pagesP Ap SmearKinjal VasavaNo ratings yet
- Screening of Cancer CervixDocument39 pagesScreening of Cancer CervixAnkur Yadav100% (1)
- Pap SmearDocument8 pagesPap Smearsmv2No ratings yet
- Management of The Abnormal Pap SmearDocument29 pagesManagement of The Abnormal Pap SmearMakWohWeiNo ratings yet
- Cervical Cancer ScreeningDocument1 pageCervical Cancer Screeningtavo823No ratings yet
- My Pap Smear Is Abnormal !Document70 pagesMy Pap Smear Is Abnormal !Alena JosephNo ratings yet
- Cervical Cancer Screening - AHS GuidelineDocument9 pagesCervical Cancer Screening - AHS GuidelineBasil al-hashaikehNo ratings yet
- 2021 Adult Preventive Health GuidelinesDocument8 pages2021 Adult Preventive Health GuidelinesAnthony El HageNo ratings yet
- 2019AdultPreventiveHealthGuidelines PDFDocument7 pages2019AdultPreventiveHealthGuidelines PDFvesvNo ratings yet
- The American Cancer Society Recommends The Following Guidelines For EarlyDocument2 pagesThe American Cancer Society Recommends The Following Guidelines For EarlyRatih Kusuma Dewi ArfaNo ratings yet
- Cervical CancerDocument4 pagesCervical CancerInomy Claudia Katherine ImbiriNo ratings yet
- 2021 Intraepithelial Neoplasia and Carcinoma of The Cervix (Document48 pages2021 Intraepithelial Neoplasia and Carcinoma of The Cervix (KarenNo ratings yet
- Gynae-L - MukundaDocument50 pagesGynae-L - MukundadocivirusNo ratings yet
- Pap SmearDocument4 pagesPap SmearRamy AsollaremNo ratings yet
- HMC Pap Guidelines November 2007Document1 pageHMC Pap Guidelines November 2007Nikki Mariz DepayNo ratings yet
- Management of Abnormal Pap Smears PresentationDocument17 pagesManagement of Abnormal Pap Smears Presentationapi-210786702100% (2)
- Cervical Cancer ScreeningDocument25 pagesCervical Cancer Screening6ixSideCreate MNo ratings yet
- PDFsam ObGynDocument4 pagesPDFsam ObGynAlessandro ZadraNo ratings yet
- N-Acetyl-Cysteine in Anovulatory Women: The Impact of Postcoital TestDocument4 pagesN-Acetyl-Cysteine in Anovulatory Women: The Impact of Postcoital TestRahma Evasari LubisNo ratings yet
- Faq085-Ervical Cancer ScreeningDocument3 pagesFaq085-Ervical Cancer ScreeningTjoema AsriNo ratings yet
- Cervical Cancer ScreeningDocument25 pagesCervical Cancer ScreeningDr VermaNo ratings yet
- Cancer Screening and Prevention:: Eliminating Deaths From Cervical CancerDocument45 pagesCancer Screening and Prevention:: Eliminating Deaths From Cervical CancerYingting ZooNo ratings yet
- Pendahuluan Pap SmearDocument14 pagesPendahuluan Pap SmearAyu NurlinaNo ratings yet
- ASCCP Management Guidelines - August 2014 PDFDocument24 pagesASCCP Management Guidelines - August 2014 PDFAnita BlazevskaNo ratings yet
- Gyn Screening PresentationDocument27 pagesGyn Screening Presentationapi-437704700100% (1)
- Approach To Breast..maha - PPTX 2Document38 pagesApproach To Breast..maha - PPTX 2Meno Ali50% (2)
- Unit 1 - Approach To The Patient - 30qDocument19 pagesUnit 1 - Approach To The Patient - 30qaeltee100% (1)
- FMcase 1Document24 pagesFMcase 1Ryan Townsend100% (2)
- Surabaya-Deteksi Dini Kanker Serviks UteriDocument32 pagesSurabaya-Deteksi Dini Kanker Serviks Uteripuskesmas manukan kulonNo ratings yet
- 22CRC 45new50 Brochure Trifold PRINTDocument2 pages22CRC 45new50 Brochure Trifold PRINTdingyshoreNo ratings yet
- Cervical Dysplasia and CancerDocument25 pagesCervical Dysplasia and CancerSarfarosh AhmadNo ratings yet
- NHS Cervical Screening: Helping You DecideDocument16 pagesNHS Cervical Screening: Helping You DecideBoy100% (1)
- Screening For Colorectal CancerDocument13 pagesScreening For Colorectal CancerPeewee AisyNo ratings yet
- Sitologi PDFDocument31 pagesSitologi PDFNadila Putri MaharaniNo ratings yet
- Health Maintenance GuidelinesDocument2 pagesHealth Maintenance GuidelinesmtataNo ratings yet
- Belle Cervical DiseaseDocument7 pagesBelle Cervical DiseaseRashed ShatnawiNo ratings yet
- Cervical Screening NewDocument17 pagesCervical Screening NewmesseeeNo ratings yet
- Undescended Testicle PathwayDocument8 pagesUndescended Testicle PathwayJessa MaeNo ratings yet
- Do Cervical Cancer Screening Recommendations Differ Among Women at Different Age Groups?Document8 pagesDo Cervical Cancer Screening Recommendations Differ Among Women at Different Age Groups?Nico Angelo CopoNo ratings yet
- Breast LectureDocument98 pagesBreast LectureTopher ReyesNo ratings yet
- Incorrect. The Correct Answer Is (D)Document5 pagesIncorrect. The Correct Answer Is (D)samgeorgyNo ratings yet
- Converted - SCREENING FOR CANCER OF THE CERVIXDocument29 pagesConverted - SCREENING FOR CANCER OF THE CERVIXSihle SibekoNo ratings yet
- Ectopic PregnancyDocument55 pagesEctopic PregnancyDr-Saja O. DmourNo ratings yet
- Sheryl Ann Pedines Bsn-IvDocument4 pagesSheryl Ann Pedines Bsn-IvSheryl Ann Barit PedinesNo ratings yet
- Infertility: PGI Ira Mikkaella GenobisDocument49 pagesInfertility: PGI Ira Mikkaella GenobisIra Mikkaella GenobisNo ratings yet
- Screening For Cancer of The Cervix: An Office Manual For Health Care ProvidersDocument16 pagesScreening For Cancer of The Cervix: An Office Manual For Health Care ProvidersYosie Yulanda PutraNo ratings yet
- Guidelines Screening USADocument2 pagesGuidelines Screening USAAyu RahmaNo ratings yet
- Explaining History of RomeDocument154 pagesExplaining History of RomeAli HusseinNo ratings yet
- Khalid Alfaki PedDocument21 pagesKhalid Alfaki PedAli HusseinNo ratings yet
- Result of Fmge (Screening Test), June 2021 SessionDocument121 pagesResult of Fmge (Screening Test), June 2021 SessionAli HusseinNo ratings yet
- Morning Pharma Dose Day 4Document2 pagesMorning Pharma Dose Day 4Ali HusseinNo ratings yet
- Morning Pharma Dose Day 3Document2 pagesMorning Pharma Dose Day 3Ali HusseinNo ratings yet
- June 2021 MCQ Psychiatry at DAMSDocument61 pagesJune 2021 MCQ Psychiatry at DAMSAli HusseinNo ratings yet
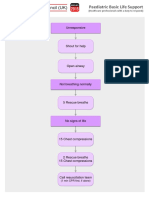
- Paediatric ALS A3Document1 pagePaediatric ALS A3Ali HusseinNo ratings yet
- Influenza Guideline 2015-16Document28 pagesInfluenza Guideline 2015-16Ali HusseinNo ratings yet
- Paediatric Basic Life Support: UnresponsiveDocument1 pagePaediatric Basic Life Support: UnresponsiveAli HusseinNo ratings yet
- How To Approach Any Cancer Patient: Levofloxacin)Document2 pagesHow To Approach Any Cancer Patient: Levofloxacin)Ali HusseinNo ratings yet
- Paediatric Choking Treatment-A3Document1 pagePaediatric Choking Treatment-A3Ali HusseinNo ratings yet
- G.R. No. 138774 March 8, 2001 Regina Francisco and Zenaida PASCUAL, Petitioners, Aida Francisco-ALFONSO, Respondent. Pardo, J.Document12 pagesG.R. No. 138774 March 8, 2001 Regina Francisco and Zenaida PASCUAL, Petitioners, Aida Francisco-ALFONSO, Respondent. Pardo, J.JuralexNo ratings yet
- Shangla Girls School: Summer Camp 2019Document5 pagesShangla Girls School: Summer Camp 2019Moyz RahmanNo ratings yet
- 55122505241#5852#55122505241#9 - 16 - 2022 12 - 00 - 00 AmDocument2 pages55122505241#5852#55122505241#9 - 16 - 2022 12 - 00 - 00 AmAdham ZidanNo ratings yet
- FN-LM07 Filipinos Conquering The WorldDocument3 pagesFN-LM07 Filipinos Conquering The WorldMichelle Em GerabanNo ratings yet
- Biomarkers of Bone Health and Osteoporosis Risk Symposium On Diet and Bone HealthDocument6 pagesBiomarkers of Bone Health and Osteoporosis Risk Symposium On Diet and Bone HealthDaniel SilvaNo ratings yet
- Assignment 2 Rahul Garg, 2020115006 IDocument8 pagesAssignment 2 Rahul Garg, 2020115006 ISrijan ChakrabortyNo ratings yet
- Details of Module and Its Structure: Ms. Kulwant KaurDocument14 pagesDetails of Module and Its Structure: Ms. Kulwant KaurAnkur TiwariNo ratings yet
- People Vs Rizal (1981)Document21 pagesPeople Vs Rizal (1981)Abigail DeeNo ratings yet
- Odeona Grecian Urn: by John KeatsDocument10 pagesOdeona Grecian Urn: by John KeatsjayeNo ratings yet
- How To Answer Stupid Job Interview Questions - LinkedInDocument17 pagesHow To Answer Stupid Job Interview Questions - LinkedInAnkur SharmaNo ratings yet
- NIT03 WAR Museurm PDFDocument78 pagesNIT03 WAR Museurm PDFDeepak SinghNo ratings yet
- Vaf PDFDocument11 pagesVaf PDFМаксим Ляшенко100% (1)
- Template For Repertoire ProposalDocument9 pagesTemplate For Repertoire ProposalAhmad SyabilNo ratings yet
- Exfoliative Respiratory Cytology (Part 1 of 2)Document15 pagesExfoliative Respiratory Cytology (Part 1 of 2)Jenn100% (2)
- Placement Exam FaqDocument2 pagesPlacement Exam FaqsglovescarsNo ratings yet
- EEE 209 Presentation 1 IntroductionDocument8 pagesEEE 209 Presentation 1 IntroductionMert YılmazNo ratings yet
- COT3 IDocument2 pagesCOT3 IKamsha Uy100% (1)
- Online Bike Parts Store and Rental SystemDocument4 pagesOnline Bike Parts Store and Rental SystemriysNo ratings yet
- 5564 Quantitative TechniquesDocument8 pages5564 Quantitative TechniquesTalat RaniNo ratings yet
- R. Molski, Polish Antitrust Law in Its Fight Against Cartels - Awaiting A BreakthroughDocument28 pagesR. Molski, Polish Antitrust Law in Its Fight Against Cartels - Awaiting A Breakthroughcsair1No ratings yet
- Particle Physics (Physics Factsheet)Document27 pagesParticle Physics (Physics Factsheet)Utsav Dhakal83% (6)
- Grade 9: Research Quiz: Citation FormatsDocument20 pagesGrade 9: Research Quiz: Citation Formatsvia macario100% (1)
- Self Incompatibility: Dr. L.K.GangwarDocument38 pagesSelf Incompatibility: Dr. L.K.GangwarSiddhant Singh100% (1)
- Powerpoint By: Mohamad Sepehri, Ph.D. Jacksonville UniversityDocument31 pagesPowerpoint By: Mohamad Sepehri, Ph.D. Jacksonville UniversityNilesh DhakeNo ratings yet
- Marketing Management AssessmentDocument5 pagesMarketing Management AssessmentMajdi SuleimanNo ratings yet
- Proof by Induction - FactorialsDocument1 pageProof by Induction - FactorialsejlflopNo ratings yet
- Pengaruh Otago Exercise Dan Gaze Stability Exercise Terhadap Keseimbangan Pada Lanjut UsiaDocument10 pagesPengaruh Otago Exercise Dan Gaze Stability Exercise Terhadap Keseimbangan Pada Lanjut UsiaBimo AnggoroNo ratings yet
- Periodic Safety Update Reports: Adel Alrwisan B.SC, M.SC, PPCDocument16 pagesPeriodic Safety Update Reports: Adel Alrwisan B.SC, M.SC, PPCHala MohamedNo ratings yet
- 1Document11 pages1Amjad PiroutiNo ratings yet