Professional Documents
Culture Documents
Activity 7.1 Alhambra, Sophia
Activity 7.1 Alhambra, Sophia
Uploaded by
sophia alhambra0 ratings0% found this document useful (0 votes)
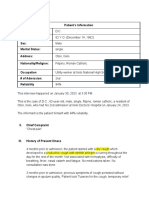
18 views8 pagesThe comprehensive geriatric assessment form summarizes an elderly patient's medical history and current condition. It includes assessments of [1] personal health planning, finances, and medical history; [2] vital signs, physical exam findings, and functional abilities; and [3] activities of daily living. The patient has fatigue and eye pain but is otherwise healthy and independent with daily activities.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe comprehensive geriatric assessment form summarizes an elderly patient's medical history and current condition. It includes assessments of [1] personal health planning, finances, and medical history; [2] vital signs, physical exam findings, and functional abilities; and [3] activities of daily living. The patient has fatigue and eye pain but is otherwise healthy and independent with daily activities.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
18 views8 pagesActivity 7.1 Alhambra, Sophia
Activity 7.1 Alhambra, Sophia
Uploaded by
sophia alhambraThe comprehensive geriatric assessment form summarizes an elderly patient's medical history and current condition. It includes assessments of [1] personal health planning, finances, and medical history; [2] vital signs, physical exam findings, and functional abilities; and [3] activities of daily living. The patient has fatigue and eye pain but is otherwise healthy and independent with daily activities.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 8
COMPREHENSIVE GERIATRIC ASSESSMENT FORM
Date of Assessment: _____________________
A. PERSONAL DATA ASSESSMENT Justification/ Pathophysiological basis
Advanced Health Directive Planning The patient haven’t secured any of the
DNR Directive: none documents mentioned because she
Living Will: none feels like “she is ready for whatever
Medical Power of Attorney: none may happen because she accepted the
fact that she going to die someday”.
Financial Health Planning Patient seeks financial health planning
Primary source of healthcare:Kiangan from the nearest medical care unit
Medical Care Dialysis Center and depending on condition.
Panopdopan District Hospital
Financial resources related to illness: PCSO, Senior citizen health care benefits is
PhilHealth, Senior Citizen, Children one of the financial resources related
to illness of the patient because she is
over 60 years old.
B. MEDICAL ASSESSMENT Justification/ Pathophysiological basis
Vital Signs Normal according to Armstrong
Temperature (2020)
Rate: 35.6 ̊ C
Route: axillary
Peripheral pulse Normal PR and rhythm: 60-100 bpm,
Rate: 80 bpm so Sinus Rhythm (Regular). Pulse
Rhythm: regular amplitude: absent 1+ = diminished,
Location: radial barely palpable, easy to obliterate 2+
Pulse amplitude: strong = easily palpable, normal 3+ = full,
increased 4+ = strong, bounding,
cannot be obliterated
Apical pulse *see above rationale There are two
Rate: 80 bpm types of murmurs (innocent and
Rhythm: regular abnormal) the former is commonly
Murmurs: none present in children and not worrisome.
However, the latter is commonly
present in adults with abnormal heart
conditions.
Respirations Normal RR and rhythm: 12-20 cpm,
Rate: 16 cpm so eupnea. No indication of labored
Rhythm: normal breathing, no use of
Use of accessory muscles: none sternocleidomastoid, spinal, and neck
Lung sounds:Bronchial, Vesicular, Bronchovesicular: muscles in respiration. Normal
no adventitious lung sounds sounds: Loud, high-pitched bronchial
breath sounds over the trachea.
Medium pitched bronchovesicular
sounds over the mainstream bronchi,
between the scapulae, and below the
clavicles. Soft, breezy, low-pitched
vesicular breath sounds over most of
the peripheral lung fields.
General appearance:patient lying in bed: fatigued The patient is lying in bed because she
just had her dialysis, also she is
feeling sleepy because of fatigue.
Allergic reactions on As per the patient
Medication: none
Food: none
Environment: Dust and animal scurf
Vaccinations: The patient’s vaccines were mostly
1. Hepatitis B from neonate to childhood.
2. Influenza
Health promotion activities: All measures aforementioned were
1.Visit optometrist every year given to suit the patient need as well
2. Eating only allowed food. as her condition.
3.Moving around the house as a form of
exercise.
Long term conditions: ---
1. Myopia
2. N/A
Recurring conditions: ---
1. N/A
2. N/A
Regular clinics and therapies: Due to current condition
1. Dr. Sandra Bonay
2. N/A
3. N/A
Surgical history: ---
1. Breast Cyst
2. N/A
Eyes/ Vision Normal as per Weber and Kelley
Eyes: redness and swelling of the eye (2018)
Pupil:Pupils are equally round but the right
pupil does not react properly to light, and has
also problems with accommodation in right
pupil.
Use of glasses: Yes
Ears/ Hearing Normal as per Kozier and Erb (2015)
Hearing: responds appropriately
Hearing aid: none
Skin integrity
Sacar/s: None
Wound/s: None
Surgical incisions/s: None
Mucous membranes: Oral cavity is moist and intact
Lips are well hydrated
Airway clearance Normal as per Kozier and Erb (2015)
Mouth: clear airway clearance without
obstruction
Nose: clear airway clearance without
obstruction
Color Patient’s skin is tan because she is
Skin: brown Filipino. Assessments regarding the
Nails: pinkish color of the nails and lips reveal
Lips: pinkish normal as per Kozier&Erb (2015).
Capillary refill:color returns within 2-3 seconds Normal: In the Blanch Test, the color
of the nail of the patient in the index
finger returned to usual color in 2-3
seconds.
Oxygen therapy: none ---
C. PHYSICAL AND FUNCTIONAL Justification/ Pathophysiological basis
ASSESSMENT
Current Activity: lying in bed: sedentary lifestyle Unhealthy, but the patient is fatigued.
Sleep: 5-8 hrs. Normal
Body Frame: mesomorph Normal
Gait: movements are coordinated Normal
Coordination: well-coordinated Normal
Balance: able to balance Normal
Muscle Strength 1-Visible muscle contraction with no
Right upper extremity:4/5 or trace movement.
Left upper extremity: 4/5 2-Limb movement, but not against
Right lower extremity: 4/5 gravity.
Left lower extremity: 4/5 3-Movement against gravity but not
resistance.
4-Movement against at least some
resistance supplied by the examiner.
5-Full strength.
Motor
Fine: can hold pen and write in paper Positive
Gross: can get and hold bottle of water Positive
Range of Motion 1-Visible muscle contraction with no
Abduction: 4/5 or trace movement.
Adduction: 4/5 2-Limb movement, but not against
Flexion: 4/5 gravity.
Extension: 4/5 3-Movement against gravity but not
resistance.
4-Movement against at least some
resistance supplied by the examiner.
5-Full strength.
Pain: none
Provocation:when eyes are blinking
Palliation:when eyes are blin king
Quality:shooting pain
Region:eyes are
Radiation:Yes. Pain to headache
Severity scale:6
Time onset/ timing: Gradual pain felt,
Basic Activities of the Daily Living
Activity Score Justification/ Pathophysiological basis
1. Bathing 1 Can bath self, yet needs assistance in
washing her back.
2. Dressing 1 Can do all the dressing by herself.
3. Toileting 1 Goes to toilet, gets on and off,
arranges clothes, washes genitalia by
herself.
4. Transferring 1 Moves in and out of bed or chair
unassisted
5. Continence 1 Exercises complete self-control over
urination and defecation.
6. Feeding 1 Can feed herself, route is oral.
Total 6
Interpretation Independent
Morse Scale (Falls Risk) Score
Age 0
Fall History 0
Mobility 0
Elimination 0
Medications 0
Patient care equipment (IV, Feeding Tubes, 0
Indwelling Catheters, etc.)
Total 0
Interpretation
Instrumental Activities of the Daily Living
Activity Score Justification/ Pathophysiological basis
1. Telephone 1 Was seen using her phone on initiative
2. Traveling 1 Able to travel
3. Shopping 1 Takes care of all shopping need
independently
4. Preparing meals 1 Plan, prepare, and serves adequate
meals independently
5. Housework 1 Able to do majority of housework’s
6. Medication 1 Is responsible for taking medication in
correct dosages at correct time.
7. Money 1 Launders small items
Total 7
Interpretation Independent
D. NUTRITIONAL ASSESSMENT Justification/ Pathophysiological basis
Diet Restriction: DASH diet
Fluid Intake: limited fluid intake
Weight: 42.5 kg
Height: 150 cm
BMI: 18.89
Interpretation: normal
Skin turgor: intact, goes back immediately
Gag reflex: active
Swallow: able
Appetite: good appetite
Food likes: vegetables
Food dislikes: salty foods
Elimination- bowel:
Stool
Frequency: 2-3 times a week
Consistency: soft
Color: brown
Elimination- bladder: Voluntary control of the external
Urine sphincter muscles enables healthy
Frequency: 1-2 times a day adults to hold larger amounts within
Color: yellow the bladder until urination is
Amount: approximately 100 ml convenient. Most adults void between
Transparency: clear to transparent 6 and 10 times per day, but this may
vary greatly, depending on fluid
consumption, personal habits, and
emotional state.
Abdomen A scaphoid or boat-like abdomen
Contour: scaphoid suggests weight loss, with possible
malnutrition.
Bowel Sounds
Right lower: gurgles, 5-30/min
Right upper: gurgles, 5-30/min
Right upper: gurgles, 5-30/min
Left lower: gurgles, 5-30/min
Mini Nutritional Assessment- Screening
Screening Score Justification/ Pathophysiological basis
1. Has food intake declined over the 1 According to the patient there is
past 3 months due to loss of moderate decrease in food intake
appetite, digestive problems, because of the diet she follow.
chewing or swallowing
difficulties?
2. Weight loss during last 3 months 3 The patient did not lose weight
3. Mobility 2
4. Has suffered psychological stress 2 The patient did not suffered
or acute disease in the past 3 psychological stress or acute disease
months in the past 3 months
5. Neuropsychological problems 2 The patient has no psychological
problems
6. Body mass index (BMI) 0 The patient BMI is 18.89
Total 10
Interpretation Possible malnutrition—continue assessment
Mini Nutritional Assessment
Assessment Score Justification/ Pathophysiological basis
1. Lives independently 0 The patient lives with her husband and
grandchildren together.
2. Takes more than 3 prescription 1 The patient does not take more than 3
drugs per day drugs in a day.
3. Pressure sores or skin ulcers 1 There are no presence of pressure or
skin ulcers during the assessment.
4. How many full meals does the 1 According to the patient she eat one
patient eat daily? full meal daily.
5. Selected consumption markers for 0.5 The client eats oneor more servings
protein intake fish and small amount of meat
6. Consumes two or more servings 1 The client usually eats green leafy
of fruit or vegetables per day? vegetables like bitter gourd, Chinese
cabbage and the likes, fish and small
amount of meat when served in the
table.
7. How much fluid is consumed per 0 The patient consume less than 3 cups
day? per day
8. Mode of feeding 2 The patient feeds herself without any
problems
9. Self- view of nutritional status 2 According to the client, she views
herself as having no nutritional
problems
10. In comparison with other people 0 According to the patient her health
of the same age, how does the status is not good as other people of
patient consider his/ her health the same age.
status?
11. Mid- arm circumference (MAC) 1 The client's MAC is 22, which is a
measurement that helps medical staff
to easily assess whether a patient is
acutely malnourished.
12. Calf circumference (CC) 1 The patient's CC is 31, an
anthropometric parameter that has
been linked to the nutritional status of
the elderly population and is closely
related to whole-body muscle mass.
Total 10.5
Interpretation At risk for malnutrition
E. PSYCHOLOGICAL/ PSYCHIATRIC Justification/ Pathophysiological basis
ASSESSMENT
Level of Consciousness
E:open and blink eye spontaneously
V:converses normally, responds appropriately
M:follows instructions
Orientation
Person:knows husband’s name
Place:knows where she is
Time:knows what day today
Memory
Immediate:Patient is able to repeat Numbers
that is previously told
Recent:Patient knows what meal she had
eaten at breakfast
Remote:Patient knows her husband’s birthday
and death anniversary
Health attitude: positive attitude
Nonverbal Behaviors:Patient maintain eye contact
and nods when she agrees to a certain statement
Mini Mental State Examination
Questions Score Justification/ Pathophysiological basis
“What is the year? Season? Date? 5 The patient is oriented to date and
Day? Month?” time
“Where are we now? State? 5 The patient is oriented to place where
County? Town/city? Hospital? she/he is in.
Floor?”
The examiner names three unrelated 3 The patient’s registration is normal
objects clearly and slowly, then the
instructor asks the patient to name all
three of them. The patient’s response
is used for scoring. The examiner
repeats them until patient learns all of
them, if possible.
“I would like you to count backward 4 The patients attention and calculation
from 100 by sevens.” is in sync
Alternative: “Spell WORLD
backwards.”
“Earlier I told you the names of three 3 The patient’s recall is good
things. Can you tell me what those
were?”
Show the patient two simple objects, 2 The patient’s language is good
such as a wristwatch and a pencil,
and ask the patient to name them.
“Repeat the phrase: ‘No ifs, ands, or 1 The patient’s language is good
buts.’”
“Take the paper in your right hand, 3 The patient’s three stage command is
fold it in half, and put it on the floor.” good
“Please read this and do what it 0 The patient’s reading and writing is
says.” not good
“Make up and write a sentence about 0 The patient’s reading and writing is
anything.” not good
“Please copy this picture.” 1 The patient’s construction is good
TotalA total score of 27 indicates that the patient is normal
and has no cognitive impairment.
Interpretation Normal
Geriatric Depression Scale
Question Score Justification/ Pathophysiological basis
1. Are you basically satisfied with 0
your life?
2. Have you dropped many of your 0
activities and interests?
3. Do you feel that your life is 0
empty?
4. Do you often get bored? 0
5. Are you hopeful about the future? 0
6. Are you bothered by thoughts you 0
can't get out of your head?
7. Are you in good spirits most of 0
the time?
8. Are you afraid that something bad 1
is going to happen to you?
9. Do you feel happy most of the 0
time?
10. Do you often feel helpless? 0
11. Do you often get restless and 0
fidgety?
12. Do you prefer to stay at home 0
rather than go out and do things?
13. Do you frequently worry about 0
the future?
14. Do you feel you have more 0
problems with memory than
most?
15. Do you think it is wonderful to be 0
alive now?
16. Do you feel downhearted and 0
blue?
17. Do you feel worthless the way 0
you are now?
18. Do you worry a lot about the 0
past?
19. Do you find life very exciting? 0
20. Is it hard for you to get started on 0
new projects?
21. Do you feel full of energy? 0
22. Do you feel that your situation is 0
hopeless?
23. Do you think that most people are 0
better off than you are?
24. Do you frequently get upset over 0
little things?
25. Do you frequently feel like 0
crying?
26. Do you have trouble 0
concentrating?
27. Do you enjoy getting up in the 0
morning?
28. Do you prefer to avoid social 0
occasions?
29. Is it easy for you to make 1
decisions?
30. Is your mind as clear as it used to 1
be?
TotalA total of 3 indicates that the patient has no syptoms
of depression.
Interpretation Normal
F. SOCIAL- ENVIRONMENTASSESSMENT Justification/ Pathophysiological basis
Name of Caregiver: Mrs. P
Caregiver relationship: mother and daughter
Caregiver stress: none
Significant others: daughter
Social engagement: work
Current social support: family
Pets: 3 dogs
Personal safety concerns: none
Home safety concerns: none
Signs of neglect or abuse: none
Hobbies and favorite activities: watching
You might also like
- Case Write Up OphthalmologyDocument11 pagesCase Write Up OphthalmologyMuhammad HaziqNo ratings yet
- Care Plan On FractureDocument10 pagesCare Plan On Fracturesantosh kumarNo ratings yet
- Bronchial AsthmaDocument16 pagesBronchial AsthmaMOLINA, TANJA JAYNENo ratings yet
- Optic AtrophyDocument36 pagesOptic Atrophysajjad hossainNo ratings yet
- Ruptured Appendectomy - Docx 1Document7 pagesRuptured Appendectomy - Docx 1Rachel QuionNo ratings yet
- 01.06.2017-Congenital Cataract Case Presentation-Dr - LikithaDocument32 pages01.06.2017-Congenital Cataract Case Presentation-Dr - Likithamuhammed fouadNo ratings yet
- AGDHNDocument28 pagesAGDHNdomingrace65No ratings yet
- A Case Presentation Presented To The Faculty of St. Luke's College of NursingDocument14 pagesA Case Presentation Presented To The Faculty of St. Luke's College of Nursingim. EliasNo ratings yet
- 13 Areas of Assessment RevisedDocument9 pages13 Areas of Assessment RevisedPam RomeroNo ratings yet
- CaressssDocument18 pagesCaressssCallie ParkNo ratings yet
- National Board Examination - Kiki Dwi QoriDocument17 pagesNational Board Examination - Kiki Dwi QoriHendra WardhanaNo ratings yet
- Urinary Tract Infection: BSN Ii-C (PM Group)Document36 pagesUrinary Tract Infection: BSN Ii-C (PM Group)Joshua DulayNo ratings yet
- Case Study Medical WardDocument14 pagesCase Study Medical WardJoshNo ratings yet
- Mohammad Hamid Sabibi - 720621465Document11 pagesMohammad Hamid Sabibi - 720621465Farida Trinovita SariNo ratings yet
- Post Encephalitis PDFDocument24 pagesPost Encephalitis PDFJitendra bhargav bhargavNo ratings yet
- رنا عبدالله الصبيح كيس ستديDocument23 pagesرنا عبدالله الصبيح كيس ستديرنا عبداللهNo ratings yet
- Running Head: NURSING CASE STUDY/BONE FRACTURE DIP/2017/00451 1Document22 pagesRunning Head: NURSING CASE STUDY/BONE FRACTURE DIP/2017/00451 1Mur DerNo ratings yet
- Capitol University College of Nursing: in Partial Fulfillment in Related Learning Experince (RLE8)Document16 pagesCapitol University College of Nursing: in Partial Fulfillment in Related Learning Experince (RLE8)Jongjong Efondo RamosoNo ratings yet
- AGN 3B FinalDocument37 pagesAGN 3B FinalKristine Dela CruzNo ratings yet
- UtsaDocument17 pagesUtsaCallie ParkNo ratings yet
- Pcap D, CHF 2 CHDDocument78 pagesPcap D, CHF 2 CHDtrew_wertNo ratings yet
- Cesarean Section 2ndary To Fetal Distress Case PresentationDocument72 pagesCesarean Section 2ndary To Fetal Distress Case PresentationMhaii Ameril100% (1)
- Alas Dos Na Ya HAAH AADocument124 pagesAlas Dos Na Ya HAAH AATrizh MacatoNo ratings yet
- Stab Wound Case StudyDocument33 pagesStab Wound Case StudyAdrian MallarNo ratings yet
- National Board Examination - Kiki Dwi QoriDocument18 pagesNational Board Examination - Kiki Dwi QoriHendra WardhanaNo ratings yet
- Case Presentation 1 CopdDocument48 pagesCase Presentation 1 CopdPreeti ChouhanNo ratings yet
- Long Case - Labiqatullubabah-En LokalDocument14 pagesLong Case - Labiqatullubabah-En LokalHendra WardhanaNo ratings yet
- NCP, InterviewDocument8 pagesNCP, Interviewim. EliasNo ratings yet
- Hashim Major LogDocument26 pagesHashim Major LogHashim AlsammawiNo ratings yet
- NUR 611 Case Study: Group DDocument17 pagesNUR 611 Case Study: Group DSheryl KumarNo ratings yet
- Bronchial Asthma Careplan BBDocument26 pagesBronchial Asthma Careplan BBKshayna 1234No ratings yet
- Bsn-Rs-Careplan 2Document9 pagesBsn-Rs-Careplan 2api-520841770No ratings yet
- ParacetamolDocument16 pagesParacetamolDan Dan ManaoisNo ratings yet
- Hypovolemic Shock Sample NCPDocument14 pagesHypovolemic Shock Sample NCPRENEROSE TORRES100% (1)
- 4 Abdominal+ExaminationDocument9 pages4 Abdominal+Examinationمرتضى حسين عبدNo ratings yet
- Cadisal MW 1ST Week RequiementsDocument36 pagesCadisal MW 1ST Week RequiementsJonathan GonzalesNo ratings yet
- DENGUEDocument21 pagesDENGUEHikari 光 ShidouNo ratings yet
- Care Plan 9 Substance Use DisorderDocument18 pagesCare Plan 9 Substance Use DisorderLokeshwari KatreNo ratings yet
- Case Presentation On Ectopoic PregnancyDocument15 pagesCase Presentation On Ectopoic PregnancyNisha FatmaNo ratings yet
- Bronchopneumonia: Prepared By: Bsn-3B-0Document64 pagesBronchopneumonia: Prepared By: Bsn-3B-0Mark Norriel CajandabNo ratings yet
- EN - Vita Pramatasari (Rev Miss Aini)Document20 pagesEN - Vita Pramatasari (Rev Miss Aini)Hendra WardhanaNo ratings yet
- Chapter IDocument8 pagesChapter IRahmakumalasariNo ratings yet
- CASE 1 Patient DCDocument6 pagesCASE 1 Patient DCDonnaLyssaReyesReunirNo ratings yet
- MW. Week 2 ReqsDocument39 pagesMW. Week 2 ReqsJoshuaNo ratings yet
- Electolyte ImbalanceDocument2 pagesElectolyte ImbalanceFouzia GillNo ratings yet
- Cholelithiasis (Case Presentation)Document19 pagesCholelithiasis (Case Presentation)Ian CiarNo ratings yet
- NURS 423 Case Scenario 2 - Heart FailureDocument9 pagesNURS 423 Case Scenario 2 - Heart FailureTeh DxjNo ratings yet
- Open I Tibia Fibula (R) Lacerated Wounded Leg: Our Lady of Fatima UniversityDocument21 pagesOpen I Tibia Fibula (R) Lacerated Wounded Leg: Our Lady of Fatima UniversityPOTENCIANA MAROMANo ratings yet
- 5 AssessmentDocument15 pages5 AssessmentDizerine Mirafuentes RolidaNo ratings yet
- Case Presentation On COPD FinalDocument26 pagesCase Presentation On COPD FinalShivani TiwariNo ratings yet
- Staphylococcal Scalded Skin Syndrome On Infant: Case Report Infection DivisionDocument25 pagesStaphylococcal Scalded Skin Syndrome On Infant: Case Report Infection DivisionAdhytio YasashiiNo ratings yet
- CASE STUDY Maladaptive G1Document39 pagesCASE STUDY Maladaptive G1BESA JERIC FLORESNo ratings yet
- Pedia 2017 Case ProtocolDocument14 pagesPedia 2017 Case ProtocolArjay Amba0% (1)
- CBD - Ebtesam AlmajedDocument38 pagesCBD - Ebtesam AlmajedEbtesamNo ratings yet
- II. AssessmentDocument13 pagesII. AssessmentIan Mizzel A. DulfinaNo ratings yet
- Cardiac Case StudyDocument44 pagesCardiac Case StudyNatalia Bernard100% (1)
- Pediatriccasepresentation1 170319164714Document30 pagesPediatriccasepresentation1 170319164714winadynamoNo ratings yet
- Nursing Health History ReyDocument10 pagesNursing Health History ReyNikki MarieNo ratings yet
- NCP 2009Document9 pagesNCP 2009louielean22No ratings yet
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicFrom EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicRating: 5 out of 5 stars5/5 (1)
- ENGL240 Paper 488Document11 pagesENGL240 Paper 488Love JovellanosNo ratings yet
- Health - Liver CleanseDocument4 pagesHealth - Liver CleanseVictorNo ratings yet
- Poptropica English STR - Scope and SequenceDocument2 pagesPoptropica English STR - Scope and SequenceD. Diana Esquivel InterianNo ratings yet
- Grammar Unit 7 1 Complete The Sentences With The Correct Form of The Verbs in BracketsDocument6 pagesGrammar Unit 7 1 Complete The Sentences With The Correct Form of The Verbs in BracketsCristina GarciaNo ratings yet
- Maps Office Present and FutureDocument3 pagesMaps Office Present and Futurecuong doNo ratings yet
- EE Sample 2Document43 pagesEE Sample 2Julius DennisNo ratings yet
- To 1 IngDocument11 pagesTo 1 IngKasmadNo ratings yet
- Speech On Indian Culture in EnglishDocument7 pagesSpeech On Indian Culture in EnglishjennaNo ratings yet
- Group 44 - 1906307201 - 1906300252 - 1906302693Document2 pagesGroup 44 - 1906307201 - 1906300252 - 1906302693howdy.daviNo ratings yet
- Agri Quiz 2 and 3Document2 pagesAgri Quiz 2 and 3jellah garciaNo ratings yet
- Finding Water When Lost in The Wilderness - Survival LifeDocument1 pageFinding Water When Lost in The Wilderness - Survival Lifekplumlee723No ratings yet
- Science Class 7thDocument298 pagesScience Class 7thbhat.sohail191No ratings yet
- BPD Startup BusinessDocument21 pagesBPD Startup BusinessvinaybioNo ratings yet
- Week 1: Name: - SectionDocument4 pagesWeek 1: Name: - SectionJohn Nelson PiconesNo ratings yet
- CCTEC Gets Big Boost: Professional. Friendly. LocalDocument20 pagesCCTEC Gets Big Boost: Professional. Friendly. LocalgrapevineNo ratings yet
- Nouns ExercisesDocument6 pagesNouns ExercisesHardik SomkuwarNo ratings yet
- 02 Lost SpringDocument10 pages02 Lost Springapi-240439386No ratings yet
- Buku Menu Zeito Update Jan 23 PDFDocument31 pagesBuku Menu Zeito Update Jan 23 PDFQory BaskoroNo ratings yet
- MOA - Punctuation and Capitalisation - Sample PaperDocument11 pagesMOA - Punctuation and Capitalisation - Sample PaperMelanie TaittNo ratings yet
- Pandemic: Week-3 Challenge Dedicated To Everyone Who Lost Their Lives in ThisDocument18 pagesPandemic: Week-3 Challenge Dedicated To Everyone Who Lost Their Lives in ThisSudhaNo ratings yet
- SHS Application Part 1Document15 pagesSHS Application Part 1ronald bantuganNo ratings yet
- ABE43 ReviewerDocument16 pagesABE43 ReviewerFrancine Ann AgapayNo ratings yet
- Ilihan Water System Development CORDOVADocument5 pagesIlihan Water System Development CORDOVAAnalinda Suril100% (3)
- Hindustan Unilever LimitedDocument13 pagesHindustan Unilever LimitedRakeshNo ratings yet
- David Ogilvy Aga CookerDocument18 pagesDavid Ogilvy Aga Cookerthiago cardoso vieira da costaNo ratings yet
- James and Juliett Fackrell Howard FamilyDocument171 pagesJames and Juliett Fackrell Howard FamilyNathan DavisNo ratings yet
- Environmental Law ProjectDocument17 pagesEnvironmental Law ProjectraaziqNo ratings yet
- Veg Manchurian Dry Recipe, How To Make Dry Vegetable ManchurianDocument22 pagesVeg Manchurian Dry Recipe, How To Make Dry Vegetable ManchurianSans QuestNo ratings yet
- Menu KawungDocument14 pagesMenu Kawungcynthia prastikaNo ratings yet
- Food Science and Human Nutrition OInformaionDocument2 pagesFood Science and Human Nutrition OInformaionEmily Duran FronteraNo ratings yet