Professional Documents
Culture Documents
Mannitol For Reduce IOP
Mannitol For Reduce IOP
Uploaded by
HerryantoThomassawaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mannitol For Reduce IOP
Mannitol For Reduce IOP
Uploaded by
HerryantoThomassawaCopyright:
Available Formats
Mannitol Infusion to Reduce Intraocular Pressure
DANIEL I. WEISS, M.D., New York; ROBERT N. SHAFFER, M.D., and
BURTON L. WISE, M.D., San Francisco
In 1904, Cantonnet recommended les sub- osmotic diuretic.7,8 Recent experimental and
stances osmotiques (sodium chloride, lactose) clinical studies have demonstrated that hyper-
in the treatment of glaucoma.1 Since then a tonic mannitol solutions are effective in
number of osmotic agents have been used, lowering cerebrospinal fluid pressure and de-
with more or less success, to lower both cere- creasing brain mass.9,12,20 Mannitol is stable
brospinal fluid pressure and intraocular pres- in solution, inert, and nontoxic, and its distri-
sure.2-4 Recently, intravenous hypertonic bution is limited to the extracellular fluid
urea has been effectively used.5,6 compartment.8-10 These facts indicated that
Mannitol, a 6-carbon hexahydric alcohol, hypertonic mannitol might be an excellent
has been employed fairly extensively as an agent for the reduction of intraocular pres-
sure.
Submitted forpublication March 2, 1962.
USPHS Special Fellow in Ophthalmology (Dr. Methods and Materials
Weiss). Ten consecutive patients who received mannitol
From the Departments of Ophthalmology and infusions are included in this study. The group is
Neurological Surgery, University of California comprised of 2 patients from the neurosurgical
School of Medicine. service and 8 patients from the ophthalmological
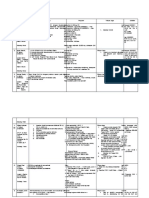
Table 1.—Effect of Hypertonic Mannitol Infusion upon Intraocular Pressure
t Serum
Intraocular Osmolality
Pressure (mOsm per
(mm. Hg) liter)
Patient
Dose of Before After
No. Age Sex Diagnosis Previous Med. Mannitol Mannitol Mannitol Before After
1 37 Malignant subcortical None 3.2gm/kg O.D. 17 Soft 287 329
glioma (papilledema) O.S. 17 Soft
2 43 F Olioblastoma multi¬ None 3gm/kg O.D. 21 5 286 319
forme (papilledema) O.S.19 Soft
3 57 Angle-closure glaucoma, Miotics 2.2gm/kg O.D. 57 <17 296 318
O.D. I. V. acetazolamide O.S.15 5
4 19 F Secondary glaucoma, Miotics, epineph- 2.1gm/kg O.D. 84 <17
O.U. rineand acetazol¬ O.S. 72 <17
amide
64 F Malignant glaucoma, Pilocarpine, aceta¬ ~2.1gm/kg O.D. 58 294 324
O.D. zolamide O.S.
6 57 F Chronic angle-closure Miotics, acetazolamide 1.3gm/kg O.D. 22 7 299 311
glaucoma, O.D. O.S.10 7
7 78 F Angle-closure glau¬ None 2.1gm/kg O.D. 88 Î51 296 308
coma, O.D. O.S. 23
55 F Retinal detachment, None <2gm/kg O.S.
O.D. O.D.
"normo- "Soft"
tensive"
9 33 M Hemorrliagic glaucoma, Miotics, epineph- 2.1gm/kg O.D. 12 Soft
O.S. rine, and aceta¬ O.S. 44 29
zolamide
10 42 M Central serous retin¬ None 1.1 gm/kg O.D. 19 12
opathy, O.D. O.S. 17 10
t Normal values were 289±4 mOsm per liter.
Î Pressure dropped to 15 mm. Hg after miotics and I.V. acetazolamide.
Downloaded From: http://archopht.jamanetwork.com/ by a Karolinska Institutet University Library User on 05/24/2015
Fig. 1.—The effect of
20% mannitol infusion
upon both the intraocular
pressure and the cerebro-
spinal fluid pressure.
service, representing a diversified and instructive cerebrospinal fluid pressure and the associated fall
group (Table 1). in intraocular pressure (Case 2). These were our
An infusion of 20% mannitol in water * was first patients, and 3 gm. per kilogram was adminis¬
given by intravenous drip. Infusion time varied tered. We then realized that this dosage rate was
from 25 minutes to 1 hour and 45 minutes ; the total probably unnecessarily high, and the dosage was
dosage varied from 1.1 to 3.2 gm. per kilogram. subsequently reduced.
The patients were observed carefully and questioned Case 3.—This 57-year-old white female entered
concerning symptoms that might relate to the infu¬ the hospital with a painful, red right eye. The cor¬
sion. Patients who were immediately preoperative nea was hazy, the pupil semidilated, and intraocular
had indwelling catheters placed. Serum osmolality pressure was 58 mm. Hg. Gonioscopy revealed a
changes were determined by the freezing-point de¬ closed angle. Miotic drops were administered, and
pression technique. intravenous acetazolamide (Diamox) was given to
no avail. Four hours later intraocular pressure was
57 mm. Hg. Mannitol infusion was begun, and
Report of Cases the tension was reduced to 17 mm. Hg when the
Cases 1, 2.—These neurosurgical patients were patient was brought to surgery. At the time of
included in the study to demonstrate and correlate surgery the surgeon noted that the eye was even
the effect of increasing serum osmolality on both softer. Thermal sclerectomy was performed.
the cerebrospinal fluid pressure and the intraocular Comment.—Acute angle-closure glaucoma
pressure. Figure 1 illustrates the dramatic fall in that does not respond to miotics and acetazol¬
*
Supplied by Martin Roberts, Ph.D., Clinical Re- amide is probably the most frequent indica¬
search Division of Don Baxter, Inc., Glendale, Calif. tion for osmotic therapy. Mannitol infusion
Fig. 2.—The effect of
20% mannitol infusion
upon acute angle-closure
glaucoma which had not
responded to pilocarpine
and acetazolamide ther¬
apy.
Downloaded From: http://archopht.jamanetwork.com/ by a Karolinska Institutet University Library User on 05/24/2015
Fig. 3.—The effect of
20% mannitol infusion
upon a secondary glau¬
coma uncontrolled by
other medical therapy.
here lasted 1 hour and 45 minutes, accounting tion. Mannitol is the reduced form of man-
for the relatively slow drop in intraocular nose and therefore does not give a positive
pressure (Fig. 2). We now recommend a test for reducing substances. However, the
faster infusion rate. possibility does remain that a diuresis may
Case 4.—This 19-year-old diabetic girl had sec¬ carry sugar with it if the blood sugar level
ondary glaucoma in both eyes subsequent to several is approaching the renal threshold.
congenital cataract procedures in both eyes. On Case 5.—This 64-year-old white female had a
demecarium bromide (Humorsol), /-epinephrine
chronic narrow-angle glaucoma of the right eye for
(Eppy*), and acetazolamide her tensions were 84 which an iridectomy was performed. At the time of
mm. Hg in the right eye, 72 mm. Hg in the left
surgery her anterior chamber was shallow and ten¬
eye. Mannitol infusion resulted in a dramatic fall
sion was 30 mm. Hg ; gonioscopically the angle was
in intraocular pressure (Fig. 3).
closed except for a slit nasally. Two days post¬
Comment.—This girl's urine gave a 4 plus
operatively the eye became painful, and intraocular
Benedict's reaction immediately after the pressure rose to 58 mm. Hg. The anterior chamber
mannitol infusion. The resident surgeon was flat. Mannitol infusion was rapidly effective
alertly but erroneously reasoned that the (Fig. 4).
mannitol might be giving the positive reac- The nextmorning the intraocular pressure was
9 mm.Hg. The anterior chamber had re-formed.
*
Barnes\p=m-\HindOphthalmic Products, Inc., Sun- Gonioscopy revealed the nasal angle to be open to
nyvale, Calif. Grade 2, but the rest of the angle was occluded. A
Fig. 4.—The response
of a malignant glaucoma
to 20% mannitol infusion.
Downloaded From: http://archopht.jamanetwork.com/ by a Karolinska Institutet University Library User on 05/24/2015
Fig. 5.—The response
of chronic angle-closure
glaucoma to 20% mannitol
infusion.
cataract section was made above, a spatula was Comment.—Since intravenous mannitol
inserted across the anterior chamber, and an ante¬ re-formed the anterior chamber in a patient
rior synechialysis was performed below; the lens
was then removed intracapsularly. The
with malignant glaucoma, we decided to see
hyaloid face
was noted to be well back and concave. if it would deepen the anterior chamber in
Comment.—This represents a case of ma¬
this case. Apparently hypertonic mannitol
infusion does decrease the volume of the
lignant glaucoma, noteworthy in that hyper-
tonic mannitol administration re-formed the posterior segment either by dehydrating the
anterior chamber. The intraocular tension vitreous or by removing posterior chamber
was still low 6 hours after the infusion, even aqueous. In this case the anterior chamber
though the serum osmolality levels were re¬ deepened, and the iris dropped away from
the trabecular meshwork. Since no periph¬
turning to the baseline (see Figure). An eral anterior synechias were present, a pe¬
exciting possibility is raised: perhaps osmotic
therapy can interrupt the malignant cycle in ripheral iridectomy was performed.
Case 7.—This 78-year-old white female requested
some cases of malignant glaucoma, thereby
treatment because she noticed that the vision in
abrogating the need for surgical intervention. her right eye had worsened ; previously noted vis¬
Case 6.—This 57-year-old white female intermit¬ ual acuity was only 20/100 in the right eye as a
tently saw halos around lights for several months. result of cataractous lens changes. The right eye
The left eye had been blind for many years from was markedly congested, the cornea steamy, and
chronic angle-closure glaucoma. When the patient the angle was closed. Tension of the right eye
was first seen the tension in the right eye was was 88 mm. Hg. No miotics or acetazolamide were
poorly controlled on miotics and acetazolamide. administered, but 209?· mannitol infusion was begun.
Gonioscopy revealed most of the angle to be closed The tension dropped from 88 mm. Hg to 51 mm.
except for a small area where the angle appeared Hg. A small additional infusion of mannitol was
slit-like. When she was hospitalized for surgery, given without effect, a significant subcutaneous in¬
tension in her right eye was reduced from 35 to 22 filtration occurring at this time. Pilocarpine (4%)
mm. I lg. With the recollection of our recent malig¬ drops were then instilled, and 500 mg. of intra¬
nant glaucoma case fresh in mind we administered venous acetazolamide was given. The tension
intravenous mannitol, both as a prophylactic and di¬ dropped to 15 mm. H g (Fig. 6), and a cataract
agnostic procedure. After the mannitol infusion extraction with complete iridectomy was subse¬
(Fig. 5) the anterior chamber was markedly deep¬ quently performed.
ened. Gonioscopy revealed the angle to be open Comment.—Because of this patient's age
(2 plus) in its entire circumference, and on this and debilitated condition, the intravenous in¬
basis the referring surgeon elected to do a periph¬ fusion was given slowly. As a result, the
eral iridectomy instead of a filtering procedure. Al¬
serum osmolality was not elevated as much
though her tension is now controlled on medication,
as we would have liked (see Figure), a fact
aqueous outflow is poor. Further surgery may be
necessary. we should have been able to predict because
Downloaded From: http://archopht.jamanetwork.com/ by a Karolinska Institutet University Library User on 05/24/2015
Fig. 6.—The moderate
response of prolonged
angle-closure glaucoma-
without previous therapy
to 20% mannitol infusion.
Further reduction of the
intraocular pressure to
normotensive levels fol¬
lowed the administration
of pilocarpine drops and
intravenous acetazolam¬
ide.
of the poor diuretic response. Nonetheless, Comment
a drop of over 35 mm. Hg occurred,
Although this is a relatively small series,
"priming" the eye for a further response to there canbe little doubt that intravenous hy¬
normotensive levels upon the subsequent ad¬
pertonic mannitol is an effective osmotic
ministration of miotics and acetazolamide.
agent for the reduction of intraocular pres¬
We do not recommend that osmotic therapy sure. Experience with over fifty neurosurgi-
should precede standard administration of cal patients has established its safety and
miotics and acetazolamide. effectiveness in lowering cerebrospinal fluid
Although 15-20 cc. of hypertonic mannitol pressure (CSF) and decreasing brain mass.12
infiltrated subcutaneously, there was no ap¬
Ligation of the renal arteries has demon¬
parent pain, and, next morning, no swelling, strated the CSF hypotensive effect to be in¬
redness, or induration was present at the
dependent of the diuretic effect* The
infiltrated site. A similar infiltration with resultant diuresis probably prolongs the hy¬
urea could be expected to produce a severe
local reaction.11
potensive response. In this regard, water in¬
Case 8.—This patient had recurrent retinal de¬
gestion should probably be somewhat limited,
so that increased serum osmolality levels are
tachment. A high scierai buckle was deemed nec¬
essary, but relatively little subretinal fluid was
maintained.
present. Hypertonic mannitol infusion softened the A brief comparison of mannitol with urea
eye, and a high buckle was easily effected. is given in Table 2. We have previously used
Case 9.—This case is that of a 33-year-old sea¬ urea with good results. Its advantages lie in
man who had severe eye pain for 1 week while at
its low molecular weight and its poor ocular
sea, subsequent to a central retinal vein occlusion
3 months earlier. Because this was a hemorrhagic penetrance. Despite its usefulness it does
glaucoma of 1 week's duration (with 2 plus ante¬ have certain disadvantages. Urea is unstable
rior chamber flare and cells), the drop in intra¬ in solution and must be freshly prepared be¬
ocular pressure from 44 mm. Hg to 29 mm. Hg fore using, a tedious and time-consuming
was no less than was anticipated. A breakdown
in the blood-aqueous barrier is one reason for the chore. It cannot be sterilized by heat. In a
frequently poor response of hemorrhagic glaucomas relatively large series of patients 13 84% com¬
to osmotic therapy. Poor posterior segment circu¬ plained of severe pain in the arm receiving
lation is probably a frequent contributing factor. the infusion; this has been attributed to the
Case 10.—A solution of 20% mannitol, 1.1 gm. hypertonicity of the solution but is probably
per kilogram, was administered to this patient with also related to the proteolytic effect of urea
central serous retinopathy in an attempt to reduce
in 30% solution. Because of this proteolytic
posterior pole transudate. The intraocular pressure
was lowered, but the effect on posterior pole fluid effect, extravasated urea can cause severe
was minimal. local reaction, and sloughs have occurred.11
Downloaded From: http://archopht.jamanetwork.com/ by a Karolinska Institutet University Library User on 05/24/2015
Table 2.—Mannitol and Urea: A Comparison
Local
Formula Mol. Wt. Distribution Dose Solution Activity Reaction Cost
Mannitol CH, OH (CHOH), CH. OH 182 Extracellular fluid 2.0 gm/kg Stable Inert Little Less
UreaNH, CONH. 60 Total body water 1.0 to 1.5 Unstable Proteolytic Marked More
gm/kg
Urea apparently has slight fibrinolytic ac¬ cidental extravasation of hypertonic mannitol
tivity,14 and increased bleeding tendency has seems to provoke considerably less local re¬
been noted in the early stages of neurosurgi- action than does urea (Case 7).
cal operations.15 However, we are not aware There was no evidence of cardiocirculatory
of any reports of severe bleeding related to overload in any of our patients. Larger
urea administration. Experimental evidence dosages given even more rapidly have not
of toxic effect on the heart with marked produced cardiocirculatory overload in over
changes in the electrocardiogram has been 50 neurosurgical patients.12 This is not to say
reported.19 that such overloading cannot occur ; it has
The molecular weight of mannitol is 3 been reported 8—as indeed it has also been
times that of urea. However, mannitol is reported with urea therapy.18
concentrated in the extracellular fluid com¬
partment 16·17 which comprises only one-third Summary
of the total body water (see Table 2) ; the Mannitol, the reduced form of mannose, is
relative disadvantage of greater molecular stable in solution, easily administered, inert,
weight is thereby largely overcome. Although and nontoxic. The intravenous administra¬
we have not measured the ocular penetrance tion of 20% mannitol solution (2 gm. per
of mannitol, we may deduce from our clin¬ kilogram) has been shown to effectively re¬
ical results that it crosses the blood-aqueous duce the intraocular pressure. The concen¬
barrier slowly, if at all. tration of mannitol in the extracellular fluid
Mannitol is available in 20% solution for compartment enhances its osmotic efficacy.
Tt is worth remembering that any intra¬
parenteral infusion. It may require slight
venous infusion, no matter how "inert,"
heating for complete solution. We recom¬ carries with it some inherent risk. Caution
mend a dose of 2 gm. per kilogram, infused
over a 30- to 45-minute span. This dose should be exercised where there is evidence
should be flexible: a smaller dose should be of cardiocirculatory insufficiency, debility, or
given if the intraocular pressure is not too oliguria.
We would like to thank Drs. Frederick C. Cordes,
high or if there is cardiocirculatory insuffici¬ Michael J. Hogan, George N. Hosford, William
ency; a larger dose may be given if the case Richardson, and Ariah Schwartz for the privilege of
is likely to be a refractory one, as in the seeing their patients.
presence of marked anterior chamber flare We would also like to thank Drs. Eggert, Fine,
and cells. Up to 4.25 gm. per kilogram has Hales, Morgan, and Reynolds for their assistance.
been used in neurosurgical patients. A sig¬ Robert N. Shaffer, M.D., 490 Post St., San
nificant diuresis occurred in all of our pa¬ Francisco, Calif.
tients except one. Three of our patients were
Addendum
nauseated, 2 experienced headache, and 2
complained of dizziness ; any osmotic agent Since submitting this paper we have used
which lowers the intracranial pressure to mannitol in ten additional instances of acute
negative levels will produce this effect.11 Only glaucoma. The results have been uniformly
1 of our patients complained of transient arm excellent. Arm pain and phlebitis have not
pain, suggesting that this symptom will occur occurred and other side-effects have been
less frequently than with urea infusion. Ac- minimal.
Downloaded From: http://archopht.jamanetwork.com/ by a Karolinska Institutet University Library User on 05/24/2015
REFERENCES 10. Ellis, F. W., and Drentz, J. C., Jr.: Sugar
Alcohols: Metabolism and Toxicity Studies with
1. Cantonnet, A.: Essai de traitement du glau- Mannitol and Sorbitol in Men and Animals, J. Biol.
come par les substances osmotiques, Arch. Ophtal. Chem. 141:47, 1941.
(Par.) 24:1, 1904. 11. Davis, M. D.; Duehr, P. A., and Javid, M.:
2. Bullock, L. T.; Gregersen, M. I., and Kinney, The Clinical Use of Urea for Reduction of Intra-
R.: The Use of Hypertonic Sucrose Solution ocular Pressure, Arch. Ophthal. 65:526, 1961.
Intravenously to Reduce Cerebrospinal Fluid Pres- 12. Wise, B. L., and Chater, N.: Hypertonic
sure Without a Secondary Rise, Amer. J. Physiol.
Mannitol to Lower CSF Pressure, Surg. Forum
112:82, 1935. 12:398, 1961.
3. Bellows, J. ; Puntenney, J., and Cowen, J. : 13. Tarter, R. C., and Linn, J. G., Jr.: A Clinical
Use of Sorbitol in Glaucoma, Arch. Ophthal. 20: Study of the Use of Intravenous Urea in Glaucoma,
1036, 1938. Amer. J. Ophthal. 52:323, 1961.
4. Davson, H., and Thomassen, T. L. : The Effect 14. von Kaulla, K., and Smith, R.: Plasma Clot
of Intravenous Infusion of Hypertonic Saline on Dissolution by Urea Derivatives, Nature (Lond.)
the Intraocular Pressure, Brit. J. Ophthal. 34:355,
190:449, 1961.
1950. 15. Stubbs, J., and Pennybacker, J.: Reduction
5. Javid, M.: Urea : New Use of an Old Agent, of Intracranial Pressure with Hypertonic Urea,
Surg. Clin. N. Amer. 38:907, 1958. Lancet 1:1094, 1960.
6. Galin, M. A.; Aizawa, F., and McLean, J. M. : 16. Elkington, J. R.: The Volume of Distribution
Urea as an Osmotic Ocular Hypotensive Agent in of Mannitol as a Measure of the Volume of Extra-
Glaucoma, A.M.A. Arch. Ophthal. 62:347, 1959. cellular Fluid, J. Clin. Invest. 26:1088, 1947.
7. Barry, K. G., and Berman, A. R.: Mannitol 17. Dominguez, R.; Corcoran, A. C., and Page,
Infusion : 3. The Acute Effect of the Intravenous I. H.: Mannitol : Kinetics of Distribution, Excre-
Infusion of Mannitol on Blood and Plasma Volumes, tion, and Utilization in Human Beings, J. Lab.
New Engl. J. Med. 1085, 1961. Clin. Med. 32:1192, 1947.
8. Bernstein, L. M.; Blumberg, B., and Arkin, 18. Ackerman, A. L.: The Action of Urea in
M. C. : Osmotic Diuretic Treatment of Refractory Acute Glaucoma, Amer. J. Ophthal. 52 :875, 1961.
Edema, Circulation 17:1013, 1958. 19. Bering, E. A., Jr., and Avman, N.: The Use
9. Wise, B. L., and Chater, N. : Effect of Man- of Hypertonic Urea Solutions in Hypothermia, J.
nitol on Cerebrospinal Fluid Pressure, Arch. Neurol. Neurosurg. 17:1073, 1960.
4:200, 1961. 20. Wise, B. L. : Unpublished data.
Downloaded From: http://archopht.jamanetwork.com/ by a Karolinska Institutet University Library User on 05/24/2015
You might also like
- ProjectDocument43 pagesProjectPradnya Shinde100% (2)
- The Use of Certain Cannabis Derivatives (Canasol) in GlaucomaDocument4 pagesThe Use of Certain Cannabis Derivatives (Canasol) in Glaucomapedrofar-1No ratings yet
- Er MathDocument17 pagesEr MathMichael RamosoNo ratings yet
- Keam 2002Document13 pagesKeam 2002Minas AliNo ratings yet
- Mapping Aqshai (Iso) DPJP:DR - Evamusdalita, SP - PD Cow:Dr. Intandandr. Reza Senin, 20 November 2017Document10 pagesMapping Aqshai (Iso) DPJP:DR - Evamusdalita, SP - PD Cow:Dr. Intandandr. Reza Senin, 20 November 2017Luthfi LazuardiNo ratings yet
- Wa0048.Document19 pagesWa0048.Ruchitha SriNo ratings yet
- Netarsudil A Novel Intra Ocular Pressure Lowering AgentDocument3 pagesNetarsudil A Novel Intra Ocular Pressure Lowering Agentalifah syarafinaNo ratings yet
- Hypertonic Saline and Mannitol Therapy in Critical Care NeurologyDocument9 pagesHypertonic Saline and Mannitol Therapy in Critical Care NeurologyRonAlNo ratings yet
- Patient Profile Form 1&2-1Document4 pagesPatient Profile Form 1&2-1varishNo ratings yet
- Creatina FosfoquinasaDocument1 pageCreatina Fosfoquinasasusey tepaNo ratings yet
- AU Instructions For Use Creatine Kinase (CK NAC)Document8 pagesAU Instructions For Use Creatine Kinase (CK NAC)Anas TjNo ratings yet
- GLAUCOMA (Compatibility Mode)Document17 pagesGLAUCOMA (Compatibility Mode)Ritesh SoodNo ratings yet
- Các Hợp Chất Ức Chế Enzyme Α-glucosidase Ðược Cô Lập Từ Lá Azadirachta Indica a.juss Trồng ở Tỉnh Ninh ThuậnDocument7 pagesCác Hợp Chất Ức Chế Enzyme Α-glucosidase Ðược Cô Lập Từ Lá Azadirachta Indica a.juss Trồng ở Tỉnh Ninh Thuậnquỳnh anh nguyễn ngọcNo ratings yet
- Post Matur It AsDocument5 pagesPost Matur It AsSitti FatimahNo ratings yet
- Lontara 3 Bawah Depan (Bedah Saraf) : Selasa, 14 Agustus 2018Document5 pagesLontara 3 Bawah Depan (Bedah Saraf) : Selasa, 14 Agustus 2018Sitti FatimahNo ratings yet
- Jurnal NetarsudilDocument7 pagesJurnal Netarsudilppds standartigaNo ratings yet
- PR STEPLADDER CTS AmmaliaDocument27 pagesPR STEPLADDER CTS AmmaliaAmmalia RachmiNo ratings yet
- Polo Poster ISCA - 2022Document1 pagePolo Poster ISCA - 2022LUTHIEN orquideaNo ratings yet
- Embolization of High Flow Arteriovenous Malformations: Experience With Use of Superabsorbent Polymer MicrospheresDocument9 pagesEmbolization of High Flow Arteriovenous Malformations: Experience With Use of Superabsorbent Polymer MicrospheresYAŞAR TÜRKNo ratings yet
- 1312 Glu PiiiDocument1 page1312 Glu PiiiAhmad MajeedNo ratings yet
- Toxicologic-Emergencies-2020 08 09-22 55 59-UtcDocument16 pagesToxicologic-Emergencies-2020 08 09-22 55 59-UtcMichael RamosoNo ratings yet
- Case Presentation On Ischemic Stroke: G.Hari Prakash Pharm.D InternDocument22 pagesCase Presentation On Ischemic Stroke: G.Hari Prakash Pharm.D InterngeethaNo ratings yet
- MDICU 5th Floor HandoverDocument5 pagesMDICU 5th Floor HandoverKailash KhatriNo ratings yet
- PR Stepladder Cts AmmaliaDocument27 pagesPR Stepladder Cts AmmaliaAmmalia RachmiNo ratings yet
- Date 05-8-20 2 Floor Ext.: 6431: Mri Done Showed Periventricular Lesions Eeg Done Showed Epileptical WavesDocument3 pagesDate 05-8-20 2 Floor Ext.: 6431: Mri Done Showed Periventricular Lesions Eeg Done Showed Epileptical WavesAli El SafadiNo ratings yet
- 3/2 CBC - Na - K - Crea - TPAG - CXR Post Intubation - ABG - Eta GscsDocument2 pages3/2 CBC - Na - K - Crea - TPAG - CXR Post Intubation - ABG - Eta GscserikaNo ratings yet
- Primary Angle Closure GlaucomaDocument39 pagesPrimary Angle Closure GlaucomaMaria ShafiqNo ratings yet
- Hypon at R em Ia: ST Epw Ise Appr Oach T o Diagn Osis: Ser U M Sodiu M 135 M M Ol/ LDocument1 pageHypon at R em Ia: ST Epw Ise Appr Oach T o Diagn Osis: Ser U M Sodiu M 135 M M Ol/ LMaría José GalvisNo ratings yet
- Adobe Scan Apr 01, 2024Document1 pageAdobe Scan Apr 01, 2024najrinkNo ratings yet
- Insulin Signaling Pathways That Regulate Glucose Metabolism in Muscle Cells and AdipocytesDocument32 pagesInsulin Signaling Pathways That Regulate Glucose Metabolism in Muscle Cells and AdipocytesnurfadilaNo ratings yet
- Ophthalmology - Ocular TherapeuticsDocument6 pagesOphthalmology - Ocular TherapeuticsjbtcmdtjjvNo ratings yet
- Efficacy of Thalidomide in Systemic OnseDocument4 pagesEfficacy of Thalidomide in Systemic OnseParvez AlamNo ratings yet
- AkiDocument13 pagesAkiharshe v100% (1)
- Diabetic CataracDocument4 pagesDiabetic CataracHanda YaniNo ratings yet
- Matsui 1999Document6 pagesMatsui 1999manikNo ratings yet
- Small Animal/ExoticsDocument3 pagesSmall Animal/Exoticstaner_soysurenNo ratings yet
- Macular Edema 2Document1 pageMacular Edema 2Chris ChrisNo ratings yet
- Case Report: Treatment of Recurrent Painful Ophthalmoplegic Neuropathy: A Case Where Pregabalin Was Successfully EmployedDocument6 pagesCase Report: Treatment of Recurrent Painful Ophthalmoplegic Neuropathy: A Case Where Pregabalin Was Successfully EmployedKoas Neuro UnpattiNo ratings yet
- GlaucomaDocument2 pagesGlaucomaSagar KrNo ratings yet
- DSS - Protocolo - Suberato de DisuccinimidilaDocument3 pagesDSS - Protocolo - Suberato de DisuccinimidilaDnane AlmeidaNo ratings yet
- Cormack2005 PDFDocument4 pagesCormack2005 PDFBENITO SEVILLANo ratings yet
- Felinos, Dexmedetomina em Infusão e Reversão Com Atipamezole 2017Document7 pagesFelinos, Dexmedetomina em Infusão e Reversão Com Atipamezole 2017Joyce De PaulaNo ratings yet
- Glukoma 1Document11 pagesGlukoma 1nugrahaNo ratings yet
- Rapid Publication: Accelerated Death of Retinal Microvascular Cells in Human and Experimental Diabetic RetinopathyDocument8 pagesRapid Publication: Accelerated Death of Retinal Microvascular Cells in Human and Experimental Diabetic RetinopathyacNo ratings yet
- Martin JosephDocument7 pagesMartin JosephmartinNo ratings yet
- Lapjag 20 Okrober 2020Document11 pagesLapjag 20 Okrober 2020Ardina MaristaNo ratings yet
- Dahlia 1Document7 pagesDahlia 1Alfani FajarNo ratings yet
- Local AnaestheticsDocument16 pagesLocal Anaestheticsapi-98304344No ratings yet
- About The Authors: Lai Ling TanDocument12 pagesAbout The Authors: Lai Ling TanStrawberry ShortcakeNo ratings yet
- COVID MX BsmmuDocument2 pagesCOVID MX BsmmuNuhiat NahreenNo ratings yet
- Cardiac Emergency Drugs and Nurses Role Review ArticleDocument7 pagesCardiac Emergency Drugs and Nurses Role Review Articlehakky gamyNo ratings yet
- Glukoma 2Document13 pagesGlukoma 2nugrahaNo ratings yet
- Hyper Osmolar Non Ketotic ComaDocument18 pagesHyper Osmolar Non Ketotic ComasnigdhaNo ratings yet
- Pharmacology of The EyeDocument8 pagesPharmacology of The EyeRahul IyerNo ratings yet
- Study On Pharmacology .Document93 pagesStudy On Pharmacology .upbandaraNo ratings yet
- Pathological Changes in The Vagus Nerve in Diabetics and AlcoholicsDocument5 pagesPathological Changes in The Vagus Nerve in Diabetics and AlcoholicsWill MurphyNo ratings yet
- Aldose Reductase InhibitorsDocument44 pagesAldose Reductase InhibitorsmplennaNo ratings yet
- Glaucoma: Doc Ernesto Pangalanan JRDocument3 pagesGlaucoma: Doc Ernesto Pangalanan JRErnani BatimanaNo ratings yet
- LASER Manual In Ophthalmology-116-120Document5 pagesLASER Manual In Ophthalmology-116-120Viankis GarcíaNo ratings yet
- Effect of A Tight Necktie On Intraocular Pressure: Scientific ReportDocument3 pagesEffect of A Tight Necktie On Intraocular Pressure: Scientific Reportlosviajesdeyora76No ratings yet
- Acid Base Case StudyDocument6 pagesAcid Base Case Studyquina mjNo ratings yet
- MUHS Question BankDocument23 pagesMUHS Question BanksuhasNo ratings yet
- (Essentials in Ophthalmology) Gyan Prakash, Takeshi Iwata - Advances in Vision Research, Volume II - Genetic Eye Research in Asia and The Pacific (2019, Springer Singapore) PDFDocument464 pages(Essentials in Ophthalmology) Gyan Prakash, Takeshi Iwata - Advances in Vision Research, Volume II - Genetic Eye Research in Asia and The Pacific (2019, Springer Singapore) PDFtegarbondanNo ratings yet
- Paul Healey Trab ChapterDocument13 pagesPaul Healey Trab ChapterPushpa RamanNo ratings yet
- كتاب علاج الامراض الجلدية والمعدية topical preparations OTC PDF-1Document150 pagesكتاب علاج الامراض الجلدية والمعدية topical preparations OTC PDF-1ريدان عياشNo ratings yet
- Seminar On GlaucomaDocument26 pagesSeminar On GlaucomaPriya A100% (1)
- BCQs POOLDocument39 pagesBCQs POOLabusaudinternationalNo ratings yet
- Drug-Study (Open Glaucoma)Document4 pagesDrug-Study (Open Glaucoma)aliannaNo ratings yet
- Referensi 9 PDFDocument4 pagesReferensi 9 PDFDzulkifli SukriNo ratings yet
- PMBLST of All ConditionsDocument18 pagesPMBLST of All ConditionsMitchell GowNo ratings yet
- GP Factsheet - Steroids and The EyeDocument6 pagesGP Factsheet - Steroids and The EyeBima RizkiNo ratings yet
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocument37 pagesPractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses CentralNo ratings yet
- 316 08Document9 pages316 08sivaNo ratings yet
- Feline Diffuse Iridal Melanoma: PresentationDocument23 pagesFeline Diffuse Iridal Melanoma: PresentationJosh LittleNo ratings yet
- Clinical Ophthalmology Dadapeer 23 28Document6 pagesClinical Ophthalmology Dadapeer 23 28AntaraaNo ratings yet
- Eye DiagnosisDocument10 pagesEye DiagnosisAfrah NajeebNo ratings yet
- Glaucoma: Seminar OnDocument43 pagesGlaucoma: Seminar OnSanjay GarasiyaNo ratings yet
- Prevalence and Associated Factor of Glaucoma in Aligarh, India A Population Based StudyDocument6 pagesPrevalence and Associated Factor of Glaucoma in Aligarh, India A Population Based StudyBeci TomNo ratings yet
- Tobradex Eye Drops: Consumer Medicine InformationDocument5 pagesTobradex Eye Drops: Consumer Medicine InformationFranc VenturaNo ratings yet
- Ophthalmology NotesDocument4 pagesOphthalmology NotesEmily Williams100% (1)
- Sin Brown2Document353 pagesSin Brown2Vlady Borda100% (6)
- Aravind Eye Care System-Case StudyDocument21 pagesAravind Eye Care System-Case StudyAbhinav MalikNo ratings yet
- 10.5.2019 Quality of Life in GlaucomaDocument30 pages10.5.2019 Quality of Life in Glaucomaneha midhaNo ratings yet
- Ilmu Kesehatan Mata PDFDocument164 pagesIlmu Kesehatan Mata PDFTania Silvia Alexandra100% (1)
- Davinci Medical AcademyDocument13 pagesDavinci Medical AcademyskNo ratings yet
- English - XI - Sample PaperDocument9 pagesEnglish - XI - Sample PaperPranav katariaNo ratings yet
- GlaucomaDocument23 pagesGlaucomaToshiba Satellite0% (1)
- Update On Congenital Glaucoma PrintDocument15 pagesUpdate On Congenital Glaucoma Printalfath rezaNo ratings yet
- CataractDocument6 pagesCataractSairileenDoradoNo ratings yet