Professional Documents
Culture Documents
Proceedings of Spie: Achieving A Trusted, Reliable, AI-ready Infrastructure For Military Medicine and Civilian Care
Proceedings of Spie: Achieving A Trusted, Reliable, AI-ready Infrastructure For Military Medicine and Civilian Care
Uploaded by
ultimatekp144Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Proceedings of Spie: Achieving A Trusted, Reliable, AI-ready Infrastructure For Military Medicine and Civilian Care
Proceedings of Spie: Achieving A Trusted, Reliable, AI-ready Infrastructure For Military Medicine and Civilian Care
Uploaded by
ultimatekp144Copyright:
Available Formats
PROCEEDINGS OF SPIE
SPIEDigitalLibrary.org/conference-proceedings-of-spie
Achieving a trusted, reliable, AI-ready
infrastructure for military medicine
and civilian care
Crump, Cindy, Schlachta-Fairchild, Loretta
Cindy Crump, Loretta M. Schlachta-Fairchild, "Achieving a trusted, reliable,
AI-ready infrastructure for military medicine and civilian care," Proc. SPIE
11413, Artificial Intelligence and Machine Learning for Multi-Domain
Operations Applications II, 114130C (21 April 2020); doi: 10.1117/12.2557514
Event: SPIE Defense + Commercial Sensing, 2020, Online Only
Downloaded From: https://www.spiedigitallibrary.org/conference-proceedings-of-spie on 01 May 2021 Terms of Use: https://www.spiedigitallibrary.org/terms-of-use
Achieving a Trusted, Reliable, AI-Ready Infrastructure for Military
Medicine and Civilian Care
Cindy A. Crump, PhD, PMP, CISSP; Loretta Schlachta-Fairchild, PhD, RN, FACHE, LTC (ret.)
U.S. Army Medical Research & Development Command 1054 Patchel Street, Ft. Detrick, MD, USA
21702-3012
ABSTRACT
It is envisioned that significant improvements in medical capabilities may be required to meet formidable
conditions expected in future military conflicts and global events such as the COVID-19 pandemic. Similar
challenges may exist for large-scale humanitarian assistance missions and civilian mass casualty events that do
not conform to prior assumptions for care delivery including evacuation within the golden hour and availability
of large medical footprints in non-traditional and field settings. The importance of standardization and
foundational infrastructure for medical devices, sensors, and data management is presented in order to achieve
safe, and effective medical systems that deliver dramatic advances in functionality made possible by Artificial
Intelligence and Machine Learning (AI/ML). The concept of autonomous, artificial intelligence based learning
systems for medical support in military Multi-Domain Operations (MDO) to meet evolving demands is
presented. Drivers towards greater use of Artificial Intelligence (AI) and Medical Autonomy to solve
anticipated gaps in forward resuscitative and stabilization care, as well as associated relevance and implications
for the management of civilian disasters are introduced. Finally, the central role of application architecture and
robust technology frameworks necessary to advance the state of the science are discussed.
The views, opinions, and/or findings contained in this abstract are those of the authors and do not
necessarily reflect the views of the Department of Defense and should not be construed as an official
DOD/Army position, policy, or decision unless so designated in other documentation. No official
endorsement of any product or vendor is made. Reference here-in to any specific commercial products,
process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily
constitute or imply its endorsement, recommendation, or favoring by the U.S. Government.
Keywords: Application architecture, AI Stack, Medical Artificial Intelligence (Medical AI), Medical Robotics
and Autonomous Systems (MedRAS), Multi-Domain Operations (MDO), Artificial Intelligence (AI) in
Medical Support, Medical Device Interoperability (MDI)
1. INTRODUCTION
Recent military conflicts have relied on air superiority and relatively few casualties to support treatment and
evacuation within 60 minutes, the so-called “Golden Hour.”1,2
Today, military and civilian medical planners cannot rely on these assumptions and need to prepare for
prolonged field care over many days in austere, pre-hospital conditions lacking facilities or infrastructure
required for the current state in medical planning, practices and evacuation support. In future conflicts, and
prolonged civilian disaster events such as pandemics or hurricanes, limited air access, extended geographic
supply lines, and high numbers of casualties may quickly overwhelm available medical and evacuation
resources. This gap suggests new solutions and greater efficiencies that can scale quickly while building, and
delivering local and regional medical expertise in real-time using ethical, evidence-based AI, medical robotics,
and autonomous systems (MedRAS). Artificial intelligence and machine learning (AI/ML) may enable medical
systems to automatically learn and improve from experience without being explicitly programmed to achieve
a target outcome. AI/ML may be applied to medical devices and patient monitoring data to identify hidden
patterns and features in the data supporting automated probabilistic inferences such as predicting the likelihood
Artificial Intelligence and Machine Learning for Multi-Domain Operations Applications II, edited by
Tien Pham, Latasha Solomon, Katie Rainey, Proc. of SPIE Vol. 11413, 114130C
© 2020 SPIE · CCC code: 0277-786X/20/$21 · doi: 10.1117/12.2557514
Proc. of SPIE Vol. 11413 114130C-1
Downloaded From: https://www.spiedigitallibrary.org/conference-proceedings-of-spie on 01 May 2021
Terms of Use: https://www.spiedigitallibrary.org/terms-of-use
an event will happen, or autonomously providing medical care in the same way that AI/ML can assist in
navigating challenging terrain for the first time. “Machine learning focuses on the development of computer
programs that can access data and use it to learn for themselves.”3 Autonomy in an automated systems context
has been described as:
“…the level of independence that humans grant a system to execute a given task. It is the
condition or quality of being self-governing to achieve an assigned task based on the system’s
capabilities such as sensing, perceiving, analyzing, planning, and decision-making required
for taking action to achieve an objective.”4
Robotic and Autonomous Systems (RAS) is considered:
“…an accepted term in academia and the science and technology community and highlights
the physical (robotic) and cognitive (autonomous) aspects of these systems. For the purposes of this
concept, RAS is a framework to describe systems with a robotic elements, an autonomous element,
or more commonly, both.”5
2. FUTURE MILITARY MEDICAL CONDITIONS IN MDO
When support, medical infrastructure (medical devices, patient monitoring data and software systems), and
specialty care is either limited, or non-existent, military and civilian first responders in the future may need to
rely on semi-autonomous and fully autonomous medical capabilities to provide prolonged or remotely delivered
hospital-based or non-traditional/field care to patients. Preventable errors may result from the severe cognitive
and physical burdens placed on local healthcare providers when delivering care over extended periods of time.
Sustained stressors increase potential risks to patient and healthcare providers’ safety.
Just-in-time predictive placement and positioning of medical assets may be needed to assist caregivers in high-
demand situations with scarce, and/or rapidly diminishing supplies. In situations like the COVID-19 pandemic,
these capabilities could include human-machine collaboration for medical decision-making and advanced life-
support to sustain patients for several days until evacuation, and/or re-supply becomes possible. Based on local
conditions, smaller, more mobile medical units may require rapid expansion, greater self-sufficiency, and/or
semi- or fully autonomous medical diagnosis and treatment in advanced systems of care that serve to preserve
life and limb under dangerous, dirty, or denied conditions, and in dense, urban environments lacking the
infrastructure taken for granted today (including network communications, power and water). More
sophisticated cybersecurity measures may be needed to counter ongoing threats to military and civilian medical
missions.
3. ENVISIONING (AND RESEARCHING) THE FUTURE STATE OF MEDICAL CARE
FOR MULTI-DOMAIN OPERATIONS
The use of artificial intelligence (AI) to approximate human judgment at machine speed for a range of clinical
applications – from accurate diagnostic image analysis, to patient risk classification, triage, delivery of care
and beyond -- is a rapidly advancing field.6,7,8,9,10 Multiple strategic drivers point to the need for autonomous
systems that rely on machine learning for delivery of medical capabilities in contaminated or dispersed, far-
flung settings around the globe.11,12,13.14 Early applications to consider, as illustrative examples, include
autonomous closed loop control systems that regulate medical devices, patient monitoring data, medications
(pain meds/IV fluids, etc.) to automate trauma care for a Combat Medic managing multiple patients, and
blood resupply via unmanned aerial and ground vehicles.15
The Artificial Intelligence in Medical Sciences (AIMS) Task Force at the US Army Medical Research and
Development Command is charged with the development of cross-cutting research that will extend,
Proc. of SPIE Vol. 11413 114130C-2
Downloaded From: https://www.spiedigitallibrary.org/conference-proceedings-of-spie on 01 May 2021
Terms of Use: https://www.spiedigitallibrary.org/terms-of-use
synthesize, and integrate existing Science and Technology (S&T) lines of effort to close validated military
medicine capability gaps by:
1) Identifying and focusing medical research to take advantage of both current and emerging advances
in enabling AI technologies that directly address warfighter needs.
2) Establishing strategic, collaborative knowledge-generating research to solve challenging problems in
medical operations in a dispersed environment to support the future fight and Warfighter Readiness.
3) Forging Industry, and Academic partnerships as well as new cross-laboratory synergy by sharing
software, libraries, tools, methods, and data commons within common frameworks that build and
scale expertise and deliver useful, new medical capabilities.
4) Ensuring patient safety by providing ethical, evidence-based medical care that capitalizes on
emerging methods of “Assured” Autonomy and AI essential for delivering valid, and trusted clinical
inferences across a range of automated medical applications.
An application reference architecture can provide the organizing frame of reference laying the groundwork
for reliable, secure, ethical, and evidence-based semi- and fully autonomous medical systems. Sensors and
devices that a Warfighter, Combat Medic, or Corpsman carries into battle provide the basic building blocks
that enable Warfighter readiness, optimal performance and even delivery of needed care for casualties in
austere and dispersed operations. However, today’s versions of sensors, medical devices, and systems are
often non-standard and vendor proprietary. Such devices are not always interoperable to the level necessary,
as demonstrated and available in automated systems within other Industries. Nor are the devices necessarily
sufficiently robust to deliver an integrated, yet flexible, and modular set of services required for evolving
missions foreseen in MDO.
Medical device interoperability (MDI) is needed but far from reality. Most medical devices have not been
designed to be standardized or secure, and some devices on the market today contain significant and
potentially dangerous cybersecurity vulnerabilities.16,17 The sensors and medical devices required for future
military operations, and in global or mass casualty incidents lack an overarching, interoperable, and secure
application and data framework. In addition, a cohesive set of standards is required to ensure the level of
seamless operation necessary to achieve semi- and fully autonomous care in environments lacking
skilled/specialty providers. Open source or standards-based software, and tools for collaboration could
provide greater accessibility, tailored to the evolving priorities of battlefield medicine and global medical
needs. These elements may support enhanced warfighter and medical readiness, and mission command
situational awareness, while minimizing technical support requirements and empowering medical personnel
operating under stressful conditions.
4. AN “AI-READY STACK” FOR ETHICAL, EVIDENCE-BASED HUMAN-MACHINE
TEAMING AND MEDICAL AUTONOMY
Systems engineering approaches specify an ordered method for integrating modular, and flexible sub-
components into highly complex, reliable, and scalable “system of systems” structures that achieve desired
automation goals. Industry and academic institutions are advancing the state of the art in AI and autonomous
systems through useful systems engineering models such as the concept of an “AI Stack.”18 The stack
provides a technical architecture framework composed of interoperable, layered components that abstract and
encapsulate complexity. This enables higher order functionality made possible the further one moves up the
stack. Interfaces between layers ensure consistency and interoperability - from the lowest elements in the
physical layer (computing, sensors) to fully autonomous applications in software that mimic elements of
human learning, and decision-making.
Proc. of SPIE Vol. 11413 114130C-3
Downloaded From: https://www.spiedigitallibrary.org/conference-proceedings-of-spie on 01 May 2021
Terms of Use: https://www.spiedigitallibrary.org/terms-of-use
To provide an analogy, the person shown in Figure 1 possesses an array of capacities inherent in human
cognition. Judgment is required for successful navigation of the environment. Experience supports and
improves decision-making through continuous learning from signals provided by the environment. Humans
use sensory perception to collect information, learn from experience, and store prior actions with responses
held in memory. This facilitates new decision-making and actions. These separable functions collectively
contribute to informed action in novel and evolving situations within a virtuous decision loop.
The AI Stack depicted in Figure 1 provides a conceptual model detailing an orderly and flexible set of
components that serve a higher automated system goal or mission. The combined elements support an
approximation of the functions of human cognition, i.e. perceive, learn, decide, and act.
Figure 1: The AI Stack (used with permission by Carnegie Mellon University)
Proc. of SPIE Vol. 11413 114130C-4
Downloaded From: https://www.spiedigitallibrary.org/conference-proceedings-of-spie on 01 May 2021
Terms of Use: https://www.spiedigitallibrary.org/terms-of-use
The AI stack is comprised of layered elements, each contributing to the automated system through the
specified function in each layer, enabled by services below. AI and autonomy is achieved through perception,
using basic computing and sensor devices to collect and store data from the environment (i.e. operating
system, sensors, actuators, and data management). Machine learning tools, modeling/simulation functions,
and decision support capabilities support the application which learns from the data available, and plans by
modeling probable outcomes for a constrained set of plausible actions. This layered approach culminates in
an autonomous system or human / AI interaction that achieves the highest order of functionality. The goal of
providing reliable, secure, and robust autonomous systems and human /AI teaming across diverse operational,
design and development contexts may be more likely to be achieved through use of a reference architecture.
The architecture and ethics, in combination, ensure the system adheres to specified policies that guide safety-
critical system design, and operation within appropriate bounds.
The AI Stack model presented in Figure 1 is similar in many respects to the internationally recognized Open
Systems Interconnection (OSI) “7-Layer Network Model” from the International Standards Organization
(ISO). 19 The network reference model has advanced the state of the science in network technologies
including the Internet. Significant innovation with economic benefits have been realized over the last forty
years because the model achieved its original objective of interoperability, and reliability using open
standards that have been proven across diverse systems and operating contexts.
Figure 2 depicts the concept of the Medical AI Stack adapted to medical missions supporting automated
clinical decision-making and autonomous systems envisioned in MDO. The architectural elements specify a
trusted, layered, and open framework for successful medical care using human-machine collaboration. The
medical providers ‘decision-loop’ in this context is approximated through technology components at the
lowest layers of computing and devices (sensors, robotic actuators, controls, network, etc.), combined with
shareable, high-quality data repositories, libraries, and toolsets that facilitate collaboration and learning.
Higher levels of functionality including machine learning, and modeling support the ability of the system to
mimic some of the cognitive processes of a healthcare provider. These functions include ability to assess,
decide, and ultimately intervene in and conduct autonomous patient care. The architecture bounds the range
of possible actions to ensure policy-based, ethical, evidence-based systems that safely deliver valid clinical
inferences and outcomes.
Proc. of SPIE Vol. 11413 114130C-5
Downloaded From: https://www.spiedigitallibrary.org/conference-proceedings-of-spie on 01 May 2021
Terms of Use: https://www.spiedigitallibrary.org/terms-of-use
Figure 2: The Medical AI / Autonomy Stack (Adapted with permission of Carnegie Mellon University)
Proc. of SPIE Vol. 11413 114130C-6
Downloaded From: https://www.spiedigitallibrary.org/conference-proceedings-of-spie on 01 May 2021
Terms of Use: https://www.spiedigitallibrary.org/terms-of-use
5. TACKLING THE STACK ONE LAYER AT A TIME: A MEDICAL DEVICE
INTEROPERABILITY REFERENCE ARCHITECTURE (MDIRA) RESEARCH
COLLABORATION
The Defense Health Agency in collaboration with the US Army Medical Research and Development
Command is sponsoring research to design and develop a secure, interoperable medical device
interoperability reference architecture.1 The architecture research collaboration includes an array of Industry
and Academic partners as well as Federal Agency participation from the Food and Drug Administration
(FDA), and the National Institutes of Standards and Technology (NIST). The research is expected to include
design guidance and specifications for secure, and interoperable medical AI/autonomy applications. The
applications could include: 1) closed loop control systems of medical care that securely and safely support
patient assessment and direct clinical interventions in semi or fully autonomous modes, and 2) AI-assisted
clinical decision support.
The central aim of the MDIRA research is to engage the medical device community in broad-based research
that fosters not only a standards-based reference architecture, but also reference implementations. The
reference implementations are expected to demonstrate future state possibilities and prototypes for Medical
AI and autonomous medical capabilities. Open-source reference models, demonstrations, and running code in
collaboration with the community is an expected outcome to encourage adoption of standards-based solutions
necessary to advance the state of the science.20 For those interested in participating in this open research
collaboration, more information, as well as the draft architecture specifications are available for review on the
website.21
REFERENCES
[1] Johns Hopkins Applied Physics Laboratory “Medical Device Interoperability Reference Architecture Research
Collaboration Video,” Youtube, October 23, 2019.” https://www.youtube.com/watch?v=aMMbCpNqIiI
[2] Rasmussen, T. E., & Kellermann, A. L.,“Wartime Lessons — Shaping a National Trauma Action Plan,” The New
England Journal of Medicine. 375(17), 1612–1615 (2016).
[3] Varone M, Mayer D., & Melegari, A. “What is Machine Learning? A Definition,” Expert System
https://www.expertsystem.com/machine-learningdefinition/ (2019).
[4] Congressional Research Service, “U.S. Ground Forces Robotics and Autonomous Systems (RAS) and Artificial
Intelligence (AI): Considerations for Congress.” https://crsreports.congress.gov/product/pdf/R/R45392 p. 2 (1
November 2018).
[5] Ibid.
[6] Hinton, G. “ Deep Learning - A Technology With the Potential to Transform Health Care.” JAMA, 320(11) (2018).
[7] Maddox, T. M., Rumsfeld, J. S., & Payne, P. R. O, “Questions for Artificial Intelligence in Health Care,” Journal of
the American Medical Association, 321(1), 31–32, https://doi.org/10.1001/jama.2018.18932 (2019).
[8] Shah, N. H., Milstein, A., & Bagley PhD, S. C., “Making Machine Learning Models Clinically Useful,” JAMA
Français. Chicago, IL : https://doi.org/10.1001/jama.2019.10306 (2019).
[9] Sim, I., “Mobile Devices and Health,” New England Journal of Medicine, 381(10), 956–968.
https://doi.org/10.1056/nejmra1806949 (2019).
[10] Stead, W., “Clinical Implications and Challenges of Artificial Intelligence and Deep Learning,” JAMA, 320(11).
Retrieved from http://search.proquest.com/docview/2116408195/ (2018).
[11] Fisher, N., & Gilbert, G., “Medical Robotic and Autonomous System Technology Enablers for the Multi-Domain
Battle 2030-2050,” Small War Journal. (2017).
[12] Joint Chiefs of Staff. (2015). “Joint Concept for Health Services,”
https://www.jcs.mil/Portals/36/Documents/Doctrine/concepts/joint_concept_health_services.pdf?ver=2017-12-28-
162027-633 (2015).
Proc. of SPIE Vol. 11413 114130C-7
Downloaded From: https://www.spiedigitallibrary.org/conference-proceedings-of-spie on 01 May 2021
Terms of Use: https://www.spiedigitallibrary.org/terms-of-use
[13] Congressional Research Service, “U.S. Ground Forces Robotics and Autonomous Systems (RAS) and Artificial
Intelligence (AI): Considerations for Congress.” https://crsreports.congress.gov/product/pdf/R/R45392 (1 November
2018).
[14] U.S. Training and Doctrine Command. “Multi-Domain Battle: Evolution of Combined Arms for the 21st Century
2025-2040,” https://www.tradoc.army.mil/Portals/14/Documents/MDB_Evolutionfor21st (1).pdf (2017).
[15] Schlachta-Fairchild, L., Crump, C., Gilbert, G., Little, J., Salinas, J., Benante, J. P., … Bills, M. (2019). Medical
Autonomous Systems for Improving Healthcare Delivery. Proc. AUVSI XPONENTIAL 2019,
https://www.xponential.org/xponential2019/public/SessionDetails.aspx?FromPage=Speakers.aspx&SessionID=3138&na
v=true&Role=U%27 (2019).
[16] Health Care Industry Cybersecurity Task Force. “Report on Improving Cybersecurity in the Health Care Industry,”
https://www.phe.gov/Preparedness/planning/CyberTF/Documents/report2017.pdf (2017).
[17] Klonoff, D., & Han, J. (2019). The First Recall of a Diabetes Device Because of Cybersecurity Risks. Journal of
Diabetes Science and Technology, 13(5), 817–820. https://doi.org/10.1177/1932296819865655
[18] Carnegie Mellon University School of Computer Science, “AI Stack,” (2019).
[19] Weik, M. H., “OSI Reference Model-The ISO Model of Architecture for Open Systems Interconnection,” Computer
Science and Communications Dictionary, C(4), 1146–1146. https://doi.org/10.1007/1-4020-0613-6_12825 (2006).
[20] Goldman, J. “Medical Device “Plug-and-Play” Interoperability Program,” https://www.mdpnp.org (2020).
[21] Johns Hopkins University Applied Physics Laboratory “Medical Device Interoperability Reference Architecture
Specifications,” https://secwww.jhuapl.edu/mdira (2020).
Proc. of SPIE Vol. 11413 114130C-8
Downloaded From: https://www.spiedigitallibrary.org/conference-proceedings-of-spie on 01 May 2021
Terms of Use: https://www.spiedigitallibrary.org/terms-of-use
You might also like
- SAP Security GRC COURSE CONTENT PDFDocument2 pagesSAP Security GRC COURSE CONTENT PDFSan DeeptiNo ratings yet
- Hgrid: An Economical Model For Mass-Health Care System Using Latest Technology (Grid Computing)Document5 pagesHgrid: An Economical Model For Mass-Health Care System Using Latest Technology (Grid Computing)IJMERNo ratings yet
- Artificial Intelligence and Healthcare Regulatory and Legal ConcernsDocument5 pagesArtificial Intelligence and Healthcare Regulatory and Legal ConcernsLingha Dharshan AnparasuNo ratings yet
- 1 s2.0 S2772918423000048 MainDocument13 pages1 s2.0 S2772918423000048 Maindaenieltan2No ratings yet
- (IJCST-V8I6P6) :akshat AgrawalDocument7 pages(IJCST-V8I6P6) :akshat AgrawalEighthSenseGroupNo ratings yet
- Public Health Reporting and Outbreak Response Synergies With Evolving Clinical StandardsDocument3 pagesPublic Health Reporting and Outbreak Response Synergies With Evolving Clinical StandardsMelisa BravoNo ratings yet
- 1 s2.0 S2214212623002053 MainDocument15 pages1 s2.0 S2214212623002053 MainDr. V. Padmavathi Associate ProfessorNo ratings yet
- Report Task2 MohammadDocument7 pagesReport Task2 MohammadNaveed Akhtar BalochNo ratings yet
- Name:: Mohammad Khamis BalochiDocument7 pagesName:: Mohammad Khamis BalochiNaveed Akhtar BalochNo ratings yet
- Week 1 ArticleDocument20 pagesWeek 1 Articleapi-213038536No ratings yet
- Trans - Mls 101 - Chapter 4Document3 pagesTrans - Mls 101 - Chapter 4Camille De CastroNo ratings yet
- Handling Privacy-Sensitive Medical Data With Federated Learning: Challenges and Future DirectionsDocument14 pagesHandling Privacy-Sensitive Medical Data With Federated Learning: Challenges and Future DirectionsAfrin IbrahimNo ratings yet
- Continuidad D Negocios y Operaciones CHEST 2014Document15 pagesContinuidad D Negocios y Operaciones CHEST 2014Victoria SalazarNo ratings yet
- Ho, Calvin W. L. - Implementing The Human Right To Science in The Regulatory Governance of Artificial Intelligence in Healthcare (Oktobar, 2023)Document30 pagesHo, Calvin W. L. - Implementing The Human Right To Science in The Regulatory Governance of Artificial Intelligence in Healthcare (Oktobar, 2023)file.dropping19No ratings yet
- Ethical Considerations For Artificial Intelligence - An Overview of The Current Radiology Landscape - PMCDocument16 pagesEthical Considerations For Artificial Intelligence - An Overview of The Current Radiology Landscape - PMCparas.sharmaNo ratings yet
- Networked Medical Devices Ass2Document9 pagesNetworked Medical Devices Ass2Sarah AlsaidanNo ratings yet
- PaperonHEalth4.0205 ArticleText 473 1 10 20190126 PDFDocument15 pagesPaperonHEalth4.0205 ArticleText 473 1 10 20190126 PDFDaniel Stiven TamayoNo ratings yet
- Autonomic Security in Health SystemsDocument6 pagesAutonomic Security in Health SystemsFarrelNo ratings yet
- Forecasting 03 00012 v2Document26 pagesForecasting 03 00012 v2sidd karkeeNo ratings yet
- Overview of Health InformaticsDocument2 pagesOverview of Health Informaticsjoy kristine morallosNo ratings yet
- Big Data Security in Healthcare 1Document8 pagesBig Data Security in Healthcare 1International Journal of Innovative Science and Research TechnologyNo ratings yet
- Final Synopsis DibasDocument12 pagesFinal Synopsis DibasDibash HembramNo ratings yet
- MINIMAR (MINimum Information For Medical AI)Document5 pagesMINIMAR (MINimum Information For Medical AI)sbutelli.almawaveNo ratings yet
- Chapter 2Document15 pagesChapter 2Swathi. N.No ratings yet
- Health 4.0: Applications, Management, Technologies and ReviewDocument15 pagesHealth 4.0: Applications, Management, Technologies and ReviewAnand BhagwaniNo ratings yet
- Blockchain: A Panacea For Healthcare Cloud-Based Data Security and Privacy?Document7 pagesBlockchain: A Panacea For Healthcare Cloud-Based Data Security and Privacy?omarNo ratings yet
- Deep Learning in Healthcare System For Quality ofDocument11 pagesDeep Learning in Healthcare System For Quality ofMadhu BalaNo ratings yet
- HIS Lesson 3. Health Informatics-FinalDocument27 pagesHIS Lesson 3. Health Informatics-FinalArmand HisonaNo ratings yet
- Modul Cloud Computing Dan Hl7 Dalam Pelayanan Kesehatan (HIM750)Document27 pagesModul Cloud Computing Dan Hl7 Dalam Pelayanan Kesehatan (HIM750)stellaNo ratings yet
- A Systematic Review For Enabling of Develop A Blockchain Technology in Healthcare Application TaxonomyDocument35 pagesA Systematic Review For Enabling of Develop A Blockchain Technology in Healthcare Application TaxonomyAshraf AbdouNo ratings yet
- L3 Overview of Health InformaticsDocument3 pagesL3 Overview of Health InformaticsVera June RañesesNo ratings yet
- April 2019 IJIRMF201903023Document8 pagesApril 2019 IJIRMF201903023Ishika KharbandaNo ratings yet
- Governance of Automated Image Analysis and Arti Ficial Intelligence Analytics in HealthcareDocument9 pagesGovernance of Automated Image Analysis and Arti Ficial Intelligence Analytics in Healthcareyulita basirNo ratings yet
- Applications of Wireless Sensor Networks in HealthcareDocument34 pagesApplications of Wireless Sensor Networks in HealthcaresaisreeknsNo ratings yet
- CAM: Cloud-Assisted Privacy Preserving Mobile Health MonitoringDocument13 pagesCAM: Cloud-Assisted Privacy Preserving Mobile Health MonitoringakttripathiNo ratings yet
- Jama Minssen 2023 VP 230073 1689353551.26861Document2 pagesJama Minssen 2023 VP 230073 1689353551.26861Neethu KinaraNo ratings yet
- A Secure Cloud-Based Patient Electronic Medical Records System Using Two-Factor AuthenticationDocument6 pagesA Secure Cloud-Based Patient Electronic Medical Records System Using Two-Factor AuthenticationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Individual AssignmentDocument13 pagesIndividual AssignmentLife of LokiniNo ratings yet
- A Review of Ambient Intelligence Assisted Healthcare MonitoringDocument10 pagesA Review of Ambient Intelligence Assisted Healthcare MonitoringOnur OzdemirNo ratings yet
- Medical Applications of Industrial Safety Science: EditorialDocument3 pagesMedical Applications of Industrial Safety Science: Editorialujangketul62No ratings yet
- IJERT Paper TemplateDocument6 pagesIJERT Paper TemplatePawankumar KhetreNo ratings yet
- PSMPA: Patient Self-Controllable and Multi-Level Privacy-Preserving Cooperative Authentication in Distributed M-Healthcare Cloud Computing SystemDocument8 pagesPSMPA: Patient Self-Controllable and Multi-Level Privacy-Preserving Cooperative Authentication in Distributed M-Healthcare Cloud Computing SystemISAR-PublicationsNo ratings yet
- Health Healthsec10Document2 pagesHealth Healthsec10angelonioNo ratings yet
- Lesson 4. Overview of Health InformaticsDocument2 pagesLesson 4. Overview of Health InformaticsClark AraraoNo ratings yet
- Authenticated Medical Documents Releasing With Privacy Protection and Release ControlDocument4 pagesAuthenticated Medical Documents Releasing With Privacy Protection and Release ControlInternational Journal of Trendy Research in Engineering and TechnologyNo ratings yet
- LATIS Pervasive PatientDocument6 pagesLATIS Pervasive PatientdaghfahsNo ratings yet
- Grid Infrastructure For Healthcare Web ServicesDocument5 pagesGrid Infrastructure For Healthcare Web Servicessurendiran123No ratings yet
- Crisis Management and The Cloud: Lessons From COVID-19: Hyland Healthcare - WhitepaperDocument6 pagesCrisis Management and The Cloud: Lessons From COVID-19: Hyland Healthcare - WhitepaperGustavoJPereiraSNo ratings yet
- Handling Privacy-Sensitive Medical Data With Federated Learning: Challenges and Future DirectionsDocument15 pagesHandling Privacy-Sensitive Medical Data With Federated Learning: Challenges and Future DirectionsRamona AnaNo ratings yet
- Peerj Cs 09 1279Document34 pagesPeerj Cs 09 1279Pedro SeguraNo ratings yet
- Security Vulnerabilities Detected MDDocument6 pagesSecurity Vulnerabilities Detected MDKamalanathan KandasamyNo ratings yet
- Masters in Health Policy's PresentationDocument17 pagesMasters in Health Policy's PresentationAdriel GeorgeNo ratings yet
- Big Data Analytics in Cloud Computing For Scientific AnalyticsDocument7 pagesBig Data Analytics in Cloud Computing For Scientific AnalyticsIJRASETPublicationsNo ratings yet
- Study of Cloud Computing in HealthCare IDocument5 pagesStudy of Cloud Computing in HealthCare IDina TrisnawatiNo ratings yet
- Smart Phone Based Intelligent Health Care SystemDocument4 pagesSmart Phone Based Intelligent Health Care SystemIJSTENo ratings yet
- Big Data SecurityDocument6 pagesBig Data SecurityAaPka ApNa MaNaSNo ratings yet
- Networking Architecture and Key Supporting Technologies For Human Digital Twin in Personalized Healthcare: A Comprehensive SurveyDocument41 pagesNetworking Architecture and Key Supporting Technologies For Human Digital Twin in Personalized Healthcare: A Comprehensive SurveySourour AbdellaouiNo ratings yet
- Individual AssignmentDocument12 pagesIndividual AssignmentLife of LokiniNo ratings yet
- Informatics Chap 10 Trustworthy System For Safe and Private Healthcare - MJSabadoDocument6 pagesInformatics Chap 10 Trustworthy System For Safe and Private Healthcare - MJSabadoRhodge SarmientoNo ratings yet
- Cybersecurity Vulnerability Analysis of Medical deDocument13 pagesCybersecurity Vulnerability Analysis of Medical demarcelo.lacknerNo ratings yet
- Data-Driven Healthcare: Revolutionizing Patient Care with Data ScienceFrom EverandData-Driven Healthcare: Revolutionizing Patient Care with Data ScienceNo ratings yet
- Sumathi Sangeetha2020 - Article - AGroup Key basedSensitiveAttriDocument15 pagesSumathi Sangeetha2020 - Article - AGroup Key basedSensitiveAttriultimatekp144No ratings yet
- Multi-User of Oading For Edge Computing Networks: A Dependency-Aware and Latency-Optimal ApproachDocument12 pagesMulti-User of Oading For Edge Computing Networks: A Dependency-Aware and Latency-Optimal Approachultimatekp144No ratings yet
- Mathematical Modeling and Models For Optimal Decision-Making in Health CareDocument178 pagesMathematical Modeling and Models For Optimal Decision-Making in Health Careultimatekp144No ratings yet
- IoT Aware Architecture For Smart LivingDocument12 pagesIoT Aware Architecture For Smart Livingultimatekp144No ratings yet
- SYLLABUSDocument1 pageSYLLABUSultimatekp144No ratings yet
- Applied Sciences: An Optimized Brain-Based Algorithm For Classifying Parkinson's DiseaseDocument16 pagesApplied Sciences: An Optimized Brain-Based Algorithm For Classifying Parkinson's Diseaseultimatekp144No ratings yet
- Digilent Embedded Linux Guide PDFDocument23 pagesDigilent Embedded Linux Guide PDFultimatekp144100% (1)
- 64 - Electronics and CommunicationDocument1 page64 - Electronics and Communicationultimatekp144No ratings yet
- What Is An Embedded System ?Document9 pagesWhat Is An Embedded System ?ultimatekp144No ratings yet
- Asv Platform Based2Document13 pagesAsv Platform Based2ultimatekp144No ratings yet
- Directions From Hyderabad To KollurDocument3 pagesDirections From Hyderabad To Kollurultimatekp144No ratings yet
- Unit - 1 DSDDocument56 pagesUnit - 1 DSDultimatekp144No ratings yet
- Smart Home Automation Using AndroidDocument8 pagesSmart Home Automation Using Androidultimatekp144100% (1)
- Understanding The SelfDocument112 pagesUnderstanding The SelfFatimah MangondatoNo ratings yet
- Unit-4 Case Study-Windows 2000Document21 pagesUnit-4 Case Study-Windows 2000mirdanishmajeed1735No ratings yet
- 2024 Autauga Prattville Library PolicyDocument53 pages2024 Autauga Prattville Library PolicyWilli MorrisNo ratings yet
- Smith KJ Student Mathematics Handbook and Integral Table ForDocument328 pagesSmith KJ Student Mathematics Handbook and Integral Table ForStrahinja DonicNo ratings yet
- Multi-Criteria Code Refactoring Using Search-Based Software EngineeringDocument53 pagesMulti-Criteria Code Refactoring Using Search-Based Software EngineeringElizaNo ratings yet
- Lab - 1-Routers Configurations Subnetting + Assignment 5 Marks - PDFDocument20 pagesLab - 1-Routers Configurations Subnetting + Assignment 5 Marks - PDFSalar AhmedNo ratings yet
- Interface StrategyDocument3 pagesInterface StrategyShenbagarajan RajanNo ratings yet
- Practical Cases in Obstetrics and Gynecology by Kanan Yelikar 2015 05 31 B01K04YXO4 PDFDocument2 pagesPractical Cases in Obstetrics and Gynecology by Kanan Yelikar 2015 05 31 B01K04YXO4 PDFSaeed HasanNo ratings yet
- Skaka DocsDocument9 pagesSkaka DocsJose Luis DorronsoroNo ratings yet
- Creation of New Property IDDocument12 pagesCreation of New Property IDTChandraRuhelaNo ratings yet
- Spectronic Genesys 10 Vis2Document180 pagesSpectronic Genesys 10 Vis2aczirokNo ratings yet
- Encapsulation: Exercise #1Document3 pagesEncapsulation: Exercise #1Marvin TorreNo ratings yet
- Certificate of Learning: Shoaib ShekasanDocument2 pagesCertificate of Learning: Shoaib ShekasanShoaib Asif ShekasanNo ratings yet
- SDA General English Question Paper 19 09 2021Document20 pagesSDA General English Question Paper 19 09 2021gayathri nathNo ratings yet
- MC780 - Maintenance Manual (1 of 2) Printer UnitDocument221 pagesMC780 - Maintenance Manual (1 of 2) Printer UnitSidnei OliveiraNo ratings yet
- Lista Track ToeflDocument7 pagesLista Track ToefllizardbulbNo ratings yet
- A Primer On Process Mining Practical Skills With Python and GraphvizDocument101 pagesA Primer On Process Mining Practical Skills With Python and GraphvizPeter JacksonNo ratings yet
- Chapter6 - Test BankDocument4 pagesChapter6 - Test BankbusatiNo ratings yet
- Overvoltage Repair Manual SEPT 2015Document143 pagesOvervoltage Repair Manual SEPT 2015Luis Humberto AguilarNo ratings yet
- Enjoy 2 20210202Document1 pageEnjoy 2 20210202manuelc2005No ratings yet
- Unit-4 Cookies and Browser DataDocument55 pagesUnit-4 Cookies and Browser Data103-abhijit aroteNo ratings yet
- CA2C - Notes - 31012023Document129 pagesCA2C - Notes - 31012023mdazriismail14No ratings yet
- Cost Center and GL - Budget UploadDocument61 pagesCost Center and GL - Budget UploadLovish RawatNo ratings yet
- LT1033Document16 pagesLT1033Sharafat KabirNo ratings yet
- Shimi Profile 09-08-2023Document59 pagesShimi Profile 09-08-2023Velur Ranganathan GanapathyNo ratings yet
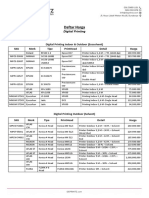
- Daftar Harga: Digital PrintingDocument4 pagesDaftar Harga: Digital PrintingHikmatus Shoimah Firdausi NuzulaNo ratings yet
- M-Commerce Seminar ReportDocument34 pagesM-Commerce Seminar Reportvivekin2k100% (2)
- Madam / Sir,: Please Affix Your Recent Passport Size Colour Photograph & Sign AcrossDocument3 pagesMadam / Sir,: Please Affix Your Recent Passport Size Colour Photograph & Sign Acrossvipin singhNo ratings yet
- Christopher Styles Pro Resume v7.2.0Document8 pagesChristopher Styles Pro Resume v7.2.0ashish ojhaNo ratings yet