Professional Documents
Culture Documents
Pleural Effusion
Pleural Effusion
Uploaded by
Elyas MehdarOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pleural Effusion
Pleural Effusion
Uploaded by
Elyas MehdarCopyright:
Available Formats
Pleural effusion
Davidson
Accumulation of serous fluid within the pleural space. Accumulation of frank pus is
termed empyema, that of blood is hemothorax, and that of chyle chylothorax. A
pleural fluid accumulates as a result of either increased HP or decreased
OP(transudative effusion, as seen in cardiac, liver or renal failure. Or from increased
microvascular pressure.
Clinical assessment: symptoms pain on inspiration and coughing.
Signs: 1. inspection tachypnea. 2. Palpation low expansion + trachea and apex
may be moved to other side. 3. Percussion stony dull. 4. Auscultation absent
breath sounds and absent vocal resonance + bronchial breathing or crackles heard
above effusion.
Investigation: chest film is of curved shadow at the lung base, blunting the costophrenic
angle. Fluid track up the lateral chest wall. Around 200mL of fluid is required in order for
it to be detectible of PA chest X-ray. US is more accurate for determining the presence of
fluid. Presence of sepetation suggests an evolving empyema or resolving hemothorax.
Pleural aspiration and biopsy: simple aspiration provides info on the color and texture of
fluid and these alone may immediately suggest an empyema or chylothorax. The
presence of blood is consistent with pulmonary infarction or malignancy but may result
from a traumatic tap. A low pH suggest infection but may also be seen in rheumatoid
arthritis, ruptured esophagus or advanced malignancy.
Empyema: this is a collection of pus in the pleural space. Microscopically, neutrophil
leukocytes are present in large numbers. It is usually Unilateral. It is always 2ry to
infection of nearby organ such as the lung, most commonly due to the bacterial
pneumonias and TB. Over 40% of patients with CAP develop as associate pleural effusion
(Para-pneumonic effusion). Other causes are infection of a hemothorax following
trauma or surgery, esophageal rupture and rupture of a sub-phrenic abscess through the
diaphragm. CLINICAL ASSESSMENT: should be suspected in patients with pulmonary
infection if there is severe pleuritic chest pain or persisting or recurrent pyrexia, despite
appropriate antibiotic treatment. Once empyema has developed, systemic features are
prominent. INVESTIGATION: chest X-ray appearance may be indistinguishable from
pleural effusion but can form a D- shaped shadow. US or CT is used to identify the
optimal site for aspiration using a wide bore needle. Other features suggesting
empyema 1. fluid glucose < 3.3mmol/L (60mg/dL). 2. LDH > 1000 U/L. 3. pH < 7.0. pus
measurements should be avoided if pus is thick.
You might also like
- Occupational Therapy Assessments Quick TableDocument5 pagesOccupational Therapy Assessments Quick Tableredsmartie100% (3)
- Pleural DiseasesDocument64 pagesPleural DiseasesDONALD UNASHENo ratings yet
- PleuritisDocument48 pagesPleuritisMuhammad FhaliqNo ratings yet
- Pleurisy Pleural Effusion EmpyemaDocument27 pagesPleurisy Pleural Effusion Empyemabima-senaNo ratings yet
- Pleural EffusionDocument3 pagesPleural EffusionRafahiah HaronNo ratings yet
- Pleural EffusionsDocument49 pagesPleural Effusionsdale 99No ratings yet
- Pleural EffusionsDocument79 pagesPleural EffusionsDiana_anca6No ratings yet
- Approach To Pleura LeffusionDocument91 pagesApproach To Pleura Leffusionrodie1050% (1)
- Disease of PleuraDocument25 pagesDisease of PleuragodzahadesNo ratings yet
- Differential Diagnosis of TBC Pleurisy.Document13 pagesDifferential Diagnosis of TBC Pleurisy.Yvonne Nmeli MihesNo ratings yet
- Pleural EffusionDocument24 pagesPleural Effusionwheeyycoldandhot55No ratings yet
- Wardclass-Cardiac Tamponade and Pleural EffusionDocument13 pagesWardclass-Cardiac Tamponade and Pleural EffusionCyrusNo ratings yet
- Eff Pleura & Pneu Kuliah KBK SM VDocument59 pagesEff Pleura & Pneu Kuliah KBK SM VAnonymous h0DxuJTNo ratings yet
- Pleural Disease in The Emergency Department - The ClinicsDocument25 pagesPleural Disease in The Emergency Department - The ClinicsEdgardo Vargas AlvarezNo ratings yet
- 3 Restrictive DisordersDocument26 pages3 Restrictive DisordersLulu MushiNo ratings yet
- Pleural EffusionDocument22 pagesPleural EffusionNARUTONo ratings yet
- Srishti Gupta - 304 - Day 15Document3 pagesSrishti Gupta - 304 - Day 15Srishti Gupta - 304No ratings yet
- Pleural EffusionDocument4 pagesPleural Effusionrezairfan221No ratings yet
- Pleural Effusion - Clinical ManifestationDocument3 pagesPleural Effusion - Clinical ManifestationJonash MoralesNo ratings yet
- Pleural Effusion - Diagnosis, Treatment, and Management 1Document22 pagesPleural Effusion - Diagnosis, Treatment, and Management 1samice5No ratings yet
- Pleural EffusionDocument72 pagesPleural Effusionmaeliszxc kimNo ratings yet
- Definition:: Pleural EffusionDocument4 pagesDefinition:: Pleural EffusionGetom NgukirNo ratings yet
- Postmedj00740 0024Document6 pagesPostmedj00740 0024Danao, Aira A.No ratings yet
- Respiratory: Welcome!Document119 pagesRespiratory: Welcome!Majo ParagasNo ratings yet
- Respiratory Step 2 CK NoteDocument41 pagesRespiratory Step 2 CK NoteXboyx MahdiNo ratings yet
- Pleural EffusionDocument50 pagesPleural EffusionTushar GuptaNo ratings yet
- Pleural Effusion: Etiology: Pleural Fluid Formation AbsorptionDocument16 pagesPleural Effusion: Etiology: Pleural Fluid Formation AbsorptionitsireneNo ratings yet
- 01 IntroDocument57 pages01 IntroahmedNo ratings yet
- Pleural EffusionDocument13 pagesPleural EffusionAbdirahman Ali YabarNo ratings yet
- Pleural EffusionDocument10 pagesPleural EffusionShane PangilinanNo ratings yet
- Pleural Effusion: AetiologyDocument5 pagesPleural Effusion: AetiologyKingman844No ratings yet
- Pleural Effusion 23-24Document21 pagesPleural Effusion 23-24bazyan3aNo ratings yet
- Risk Factors, Med and NSG MGTDocument5 pagesRisk Factors, Med and NSG MGTHania PolangiNo ratings yet
- Esti2014 P-0058Document71 pagesEsti2014 P-0058Sitti_HazrinaNo ratings yet
- Trapped Lung - StatPearls - NCBI BookshelfDocument7 pagesTrapped Lung - StatPearls - NCBI BookshelfVinna KusumawatiNo ratings yet
- DR Ahmed - Surgery - Diseases of Pleura - 237Document18 pagesDR Ahmed - Surgery - Diseases of Pleura - 237Ahmed MohamadNo ratings yet
- Pleural EffusionDocument23 pagesPleural EffusionYousra ShaikhNo ratings yet
- Pleural Effusion: PathophysiologyDocument6 pagesPleural Effusion: PathophysiologyNyamburaNo ratings yet
- Pleural EffusionsDocument41 pagesPleural Effusionssanjivdas100% (1)
- Pleural DisorderDocument28 pagesPleural Disordernathan asfahaNo ratings yet
- Cleveland Clinic Journal of Medicine 2005Document12 pagesCleveland Clinic Journal of Medicine 2005melianasulistioNo ratings yet
- Pledisuraealse - 30 Oktober 2012Document57 pagesPledisuraealse - 30 Oktober 2012Silvestri PurbaNo ratings yet
- DR M Abdur Rahim M.D.:, Asst. Professor of MedicineDocument43 pagesDR M Abdur Rahim M.D.:, Asst. Professor of Medicinedr_abdurNo ratings yet
- Body Fluids1Document93 pagesBody Fluids1Aliyah Tofani PawelloiNo ratings yet
- Tension PneumothoraxDocument5 pagesTension PneumothoraxKay BristolNo ratings yet
- Chest X-Ray ReviewDocument145 pagesChest X-Ray ReviewHamid ShaalanNo ratings yet
- Mediastinitis - IDDocument52 pagesMediastinitis - IDDidy Kurniawan100% (1)
- Pleural PathologiesDocument49 pagesPleural PathologiesIsaac ShirimaNo ratings yet
- Derrame Pleural Aafp 2014Document6 pagesDerrame Pleural Aafp 2014Mario Villarreal LascarroNo ratings yet
- Rest Torace Si PleuraDocument29 pagesRest Torace Si PleuraAndreea RalucaNo ratings yet
- Pleural Effusion: PathophysiologyDocument7 pagesPleural Effusion: PathophysiologyJackie MaggayNo ratings yet
- Yingyu 1Document31 pagesYingyu 1api-19916399No ratings yet
- Lung Abscess FinalDocument27 pagesLung Abscess FinalvivianNo ratings yet
- Empyema 5Document4 pagesEmpyema 5Samba SukanyaNo ratings yet
- LO Dan WO Cardio Week 2 (Rabu)Document45 pagesLO Dan WO Cardio Week 2 (Rabu)Alan Dwi SetiawanNo ratings yet
- Parapneumonic Pleural Effusions and Empyema Thoracis - Background, Pathophysiology, EpidemiologyDocument4 pagesParapneumonic Pleural Effusions and Empyema Thoracis - Background, Pathophysiology, EpidemiologyLorentina Den PanjaitanNo ratings yet
- Case Report 2Document7 pagesCase Report 2sofiosNo ratings yet
- SGL6 - CoughDocument63 pagesSGL6 - CoughDarawan MirzaNo ratings yet
- Bacterial Destruction of The LungsDocument46 pagesBacterial Destruction of The LungsAhmad Abu KushNo ratings yet
- Pleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandPleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Pleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandPleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Cardiology UQU 2022Document29 pagesCardiology UQU 2022Elyas MehdarNo ratings yet
- Hematology UQU 2022Document94 pagesHematology UQU 2022Elyas MehdarNo ratings yet
- Valvular Heart DiseaseDocument5 pagesValvular Heart DiseaseElyas MehdarNo ratings yet
- Acute Respiratory FailureDocument38 pagesAcute Respiratory FailureElyas MehdarNo ratings yet
- SCA + ThalassemiaDocument2 pagesSCA + ThalassemiaElyas MehdarNo ratings yet
- Diabetes MellitusDocument2 pagesDiabetes MellitusElyas MehdarNo ratings yet
- Memory Processes and Learning Theory DR Abeer Almarzouki MD, PHD 2017-2018Document32 pagesMemory Processes and Learning Theory DR Abeer Almarzouki MD, PHD 2017-2018Elyas MehdarNo ratings yet
- Asthma Davidson + Osmosis + Step Up MedicineDocument2 pagesAsthma Davidson + Osmosis + Step Up MedicineElyas MehdarNo ratings yet
- Copd Davidson + OsmosisDocument3 pagesCopd Davidson + OsmosisElyas MehdarNo ratings yet
- How To Take Medical History SheetDocument4 pagesHow To Take Medical History SheetElyas MehdarNo ratings yet
- Principles of Infectious Diseases - 2018-2019 - AlbugamiDocument33 pagesPrinciples of Infectious Diseases - 2018-2019 - AlbugamiElyas MehdarNo ratings yet
- Elective-Internship-Training-Program-2021 KSA Johns Hopkins AramcoDocument3 pagesElective-Internship-Training-Program-2021 KSA Johns Hopkins AramcoElyas MehdarNo ratings yet
- Heart Failure DavidsonDocument3 pagesHeart Failure DavidsonElyas MehdarNo ratings yet
- Heimlich Heroes To The Rescue!Document4 pagesHeimlich Heroes To The Rescue!Peter M. HeimlichNo ratings yet
- Jacobson 1986-Types and Timing of Social SupportDocument16 pagesJacobson 1986-Types and Timing of Social SupportmavNo ratings yet
- ASNT Basic Level III Module 1 (Study Test)Document3 pagesASNT Basic Level III Module 1 (Study Test)DESTINY SIMON100% (1)
- TemplateDocument2 pagesTemplateDiego PavezNo ratings yet
- GCF and LCMDocument34 pagesGCF and LCMНикому Не Известный ЧеловекNo ratings yet
- CRP SCHOOL REQ RPT Academic Records Transcripts Form A Rev-JDocument4 pagesCRP SCHOOL REQ RPT Academic Records Transcripts Form A Rev-Jla.venus14No ratings yet
- Post-Mco Y6 RPT English MDM VJMDocument7 pagesPost-Mco Y6 RPT English MDM VJMVisha D'Of ChandranNo ratings yet
- Lecture 1-2 (Week 01)Document30 pagesLecture 1-2 (Week 01)saqib khan afridiNo ratings yet
- 05 Activity 13Document5 pages05 Activity 13Miguel MenesesNo ratings yet
- Architecture Decision RecordsDocument54 pagesArchitecture Decision RecordsFernandoFernandesNo ratings yet
- Module6 TMPG1Document24 pagesModule6 TMPG1Prince Mhar SurioNo ratings yet
- PartbplansforlearningsegmentDocument8 pagesPartbplansforlearningsegmentapi-402331516No ratings yet
- Lesson Plan 25Document17 pagesLesson Plan 25Jay BolanoNo ratings yet
- Oral Presentation RubricDocument1 pageOral Presentation Rubrickjoerg1084100% (1)
- Leyte Normal UniversityDocument4 pagesLeyte Normal UniversityJudy ConstanciandraNo ratings yet
- Personal Essay Thesis Statement ExamplesDocument7 pagesPersonal Essay Thesis Statement Examplesafkollnsw100% (2)
- Assignment Abah PART ADocument5 pagesAssignment Abah PART AFnatashaaNo ratings yet
- Logistics Thesis ProposalDocument5 pagesLogistics Thesis Proposalkcaevuief100% (2)
- Michelin Case Potential AnswersDocument2 pagesMichelin Case Potential AnswersfidanNo ratings yet
- Common Error Types For English Language LearnersDocument2 pagesCommon Error Types For English Language LearnersjhonatantHarolNo ratings yet
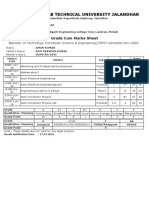
- I.K.Gujral Punjab Technical University Jalandhar: Grade Cum Marks SheetDocument1 pageI.K.Gujral Punjab Technical University Jalandhar: Grade Cum Marks SheetAman KumarNo ratings yet
- Plot 2: Rejecting MR Perfect: Rej Ect Ing MR Per Fec TDocument5 pagesPlot 2: Rejecting MR Perfect: Rej Ect Ing MR Per Fec TMonica PatraNo ratings yet
- Speakout Intermediate Video Podcast Unit 1 Identity WorksheetDocument3 pagesSpeakout Intermediate Video Podcast Unit 1 Identity WorksheetAldric NikoNo ratings yet
- Empathy Challenge Write-UpDocument11 pagesEmpathy Challenge Write-UpSatrih SMAN 8 KDINo ratings yet
- AcknowledgementDocument2 pagesAcknowledgementalienajNo ratings yet
- Briefing em ArquiteturaDocument4 pagesBriefing em ArquiteturafreitasmachadocarolNo ratings yet
- Mind SetDocument21 pagesMind SetL Mahender Reddy100% (3)
- Cavite State University Don Severino de Las Alas CampusDocument1 pageCavite State University Don Severino de Las Alas Campuslouie roderosNo ratings yet
- Grammatical and Syntactical Functions of Auxiliaries in English and UrduDocument18 pagesGrammatical and Syntactical Functions of Auxiliaries in English and UrduBahmano BahmanoNo ratings yet