Professional Documents
Culture Documents
Esophagus: Drzaiter
Esophagus: Drzaiter
Uploaded by
drynwhylCopyright:
Available Formats
You might also like
- Goljan Step 1 HY 36 Pages Notes PDFDocument36 pagesGoljan Step 1 HY 36 Pages Notes PDFTyler Lawrence CoyeNo ratings yet
- Louis S. Constine MD, Nancy J. Tarbell MD, Edward C. Halperin MD - Pediatric Radiation Oncology (2016, LWW) PDFDocument2,424 pagesLouis S. Constine MD, Nancy J. Tarbell MD, Edward C. Halperin MD - Pediatric Radiation Oncology (2016, LWW) PDFPan50% (2)
- Reading Test 01 - E2Lang PDFDocument25 pagesReading Test 01 - E2Lang PDFMuhammad Haneef100% (12)
- Toacs by ShireenDocument244 pagesToacs by ShireenMuhammad Zeeshan100% (1)
- Orthopaedic MCQDocument6 pagesOrthopaedic MCQGlucose DRglucoseNo ratings yet
- Surgery Lectures EsophagusDocument22 pagesSurgery Lectures Esophagusj,007No ratings yet
- Dyspepsia Lecture 6Document28 pagesDyspepsia Lecture 6Dhante MRDNo ratings yet
- Kuliah Upper Gi Tract DiseaseDocument78 pagesKuliah Upper Gi Tract DiseaseAnggun Pulihana WNo ratings yet
- Grand Rounds Index UTMB Otolaryngology Home PageDocument12 pagesGrand Rounds Index UTMB Otolaryngology Home Pagegdudex118811No ratings yet
- Bowel ObstructionDocument10 pagesBowel Obstructionenke.nwekeNo ratings yet
- 3-Pharynx. OesophagusDocument30 pages3-Pharynx. OesophagusislamNo ratings yet
- Dysphagia AhsDocument32 pagesDysphagia AhsIbrahim AchmadNo ratings yet
- Esophageal DisordersDocument37 pagesEsophageal DisordersDanielle FosterNo ratings yet
- Alimentary and Biliary Conditions 3-1Document249 pagesAlimentary and Biliary Conditions 3-1Mercy KeruboNo ratings yet
- Surgical Disease of The Esophagus: Mahteme Bekele, MD Assistant Professor of SurgeryDocument72 pagesSurgical Disease of The Esophagus: Mahteme Bekele, MD Assistant Professor of SurgeryBiniamNo ratings yet
- Class 7 (G1) - GI TractDocument112 pagesClass 7 (G1) - GI TractAdel mohammadNo ratings yet
- GIT - Prob 1Document143 pagesGIT - Prob 1anon_181166970No ratings yet
- The Blood Supply of EsophagusDocument4 pagesThe Blood Supply of EsophagusSaman SarKoNo ratings yet
- St. Anthony College of Roxas CityDocument14 pagesSt. Anthony College of Roxas CityMykristie Jho B. MendezNo ratings yet
- Gastric Outlet Obstruction (Stenosis) : Lior Shlomov 1852Document8 pagesGastric Outlet Obstruction (Stenosis) : Lior Shlomov 1852Lior ShlomovNo ratings yet
- Dysphagia: DR (Prof.) A B Singh Unit Department of General Surgery Patna Medical College & HospitalDocument48 pagesDysphagia: DR (Prof.) A B Singh Unit Department of General Surgery Patna Medical College & HospitalAswin Rajasekaran100% (1)
- Gastro NephroDocument93 pagesGastro Nephrohasanatiya41No ratings yet
- DYSPHAGIADocument46 pagesDYSPHAGIAnanohaniwiekoNo ratings yet
- Gastrointestinal and Abdominal Problems 3.LfDocument68 pagesGastrointestinal and Abdominal Problems 3.LfapocruNo ratings yet
- Powerpoint: Colorectal Surgical DiseasesDocument74 pagesPowerpoint: Colorectal Surgical Diseasesj.doe.hex_87100% (1)
- Examination of Intestinal Obstruction, Acute Abdomen and Acute Appendicitis - Eugh & BwembyaDocument29 pagesExamination of Intestinal Obstruction, Acute Abdomen and Acute Appendicitis - Eugh & BwembyaForeighn97No ratings yet
- Dysphagia: DR S Jaya SandeepDocument22 pagesDysphagia: DR S Jaya Sandeepsai kousikNo ratings yet
- Achalasia: Department of MedicineDocument21 pagesAchalasia: Department of Medicinekyliever100% (1)
- Nur Akbar A. Mini LectureDocument39 pagesNur Akbar A. Mini LectureanafauziahfitriNo ratings yet
- Esophageal DiseasesDocument9 pagesEsophageal DiseasesRashed ShatnawiNo ratings yet
- Dysphagia: DR Navin Shukla Associate Professor Department of E.N.T&H.N.SDocument64 pagesDysphagia: DR Navin Shukla Associate Professor Department of E.N.T&H.N.SNavin ShuklaNo ratings yet
- By: Isser Jorell L. Yao, RN, MAN, Ed.D.: Responses To Metabolic-Gastrointestinal and Liver AlterationsDocument65 pagesBy: Isser Jorell L. Yao, RN, MAN, Ed.D.: Responses To Metabolic-Gastrointestinal and Liver AlterationsNur SanaaniNo ratings yet
- Navan Ee Than 2015Document7 pagesNavan Ee Than 2015Yacine Tarik AizelNo ratings yet
- Pediatric Surgery PresentationDocument191 pagesPediatric Surgery PresentationdanoonotNo ratings yet
- Esophagus: Comments On Embryology of EsophagusDocument14 pagesEsophagus: Comments On Embryology of EsophagusDave AbrahamNo ratings yet
- IntussusceptionDocument24 pagesIntussusceptionOjambo Flavia100% (1)
- Intestinal Obstruction ChikaDocument45 pagesIntestinal Obstruction ChikarohitNo ratings yet
- Intestinal ObstructionDocument13 pagesIntestinal Obstructionsantosh kumarNo ratings yet
- Dysphagia: Departemen THT-KL Fakultas Kedokteran Universitas Padjadjaran 2016Document31 pagesDysphagia: Departemen THT-KL Fakultas Kedokteran Universitas Padjadjaran 2016Sherlyn YeeNo ratings yet
- Oral Revalida and Comprehensive ExamDocument13 pagesOral Revalida and Comprehensive Examlovelove DayoNo ratings yet
- Case Presentation: Intern: Iris Parcon Clerks: Karen Bianca Espinola Anna Sophia Lim Leo Salvador VedanaDocument50 pagesCase Presentation: Intern: Iris Parcon Clerks: Karen Bianca Espinola Anna Sophia Lim Leo Salvador VedanaKaren Bianca Matampale EspinolaNo ratings yet
- Surgical Diseases of The EsophagusDocument35 pagesSurgical Diseases of The Esophagusmogesie1995No ratings yet
- Peptic Ulcer DiseaseDocument63 pagesPeptic Ulcer DiseaseAli100% (1)
- CABITAC Histology (Digestive) FinalDocument9 pagesCABITAC Histology (Digestive) FinalZhon CabitacNo ratings yet
- PeritonitisDocument14 pagesPeritonitisAyad IdresNo ratings yet
- Bazo Errante 2016 REVISED Ijtra1601084Document4 pagesBazo Errante 2016 REVISED Ijtra1601084luisalfredo_montesNo ratings yet
- Power Git EndoDocument170 pagesPower Git Endoapi-3735995100% (1)
- GI Tract: Esophagus & StomachDocument126 pagesGI Tract: Esophagus & StomachPablo SisirucaNo ratings yet
- Swallowing Disorders 2022Document29 pagesSwallowing Disorders 2022Mohammed AhmedNo ratings yet
- Gastroenterology by Elagouri MohammedDocument31 pagesGastroenterology by Elagouri MohammedStylesh GuRlyNo ratings yet
- Problem 2 GI - VICKA AZWITADocument65 pagesProblem 2 GI - VICKA AZWITARana RickNo ratings yet
- Hrkansh NotesDocument424 pagesHrkansh NotesAhmed RagabNo ratings yet
- Plenary 3 Group 13Document122 pagesPlenary 3 Group 13Obet Agung 天No ratings yet
- Abdominal DistensionDocument10 pagesAbdominal DistensionMorad ImadNo ratings yet
- AchalasiaDocument5 pagesAchalasiaAli GhummiedNo ratings yet
- StomachDocument204 pagesStomachrajmv7No ratings yet
- Dysphagia and Oesophageal Carcinoma-Maj (DR) Francis KamunduDocument44 pagesDysphagia and Oesophageal Carcinoma-Maj (DR) Francis KamunduKutemwaNo ratings yet
- Pyloric StenosisDocument46 pagesPyloric Stenosishayssam rashwan81% (16)
- Obstruction EDocument10 pagesObstruction ECorina MunteanuNo ratings yet
- DYSPHAGIA Lecture NotesDocument84 pagesDYSPHAGIA Lecture Notesmcmak357No ratings yet
- DysphagiaDocument72 pagesDysphagiaMaisarah IsmailNo ratings yet
- AADocument20 pagesAAAiyaz AliNo ratings yet
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Meniscus Injury: Presented by Siti Nur Rifhan KamarudinDocument29 pagesMeniscus Injury: Presented by Siti Nur Rifhan KamarudindrynwhylNo ratings yet
- Ophthalmology SingiDocument20 pagesOphthalmology SingidrynwhylNo ratings yet
- PGI BiochemistryDocument171 pagesPGI BiochemistrydrynwhylNo ratings yet
- Deconstructing The ECG Curve - The Components of The Tracing: Key ConceptsDocument117 pagesDeconstructing The ECG Curve - The Components of The Tracing: Key ConceptsdrynwhylNo ratings yet
- Lymphatic SystemDocument22 pagesLymphatic SystemdrynwhylNo ratings yet
- Endocrine SystemDocument18 pagesEndocrine SystemdrynwhylNo ratings yet
- Digestive SystemDocument60 pagesDigestive SystemdrynwhylNo ratings yet
- Reproductive SystemDocument23 pagesReproductive SystemdrynwhylNo ratings yet
- Urinary SystemDocument30 pagesUrinary SystemdrynwhylNo ratings yet
- Thyroid ParathyroidDocument17 pagesThyroid ParathyroiddrynwhylNo ratings yet
- Energy BalanceDocument27 pagesEnergy BalancedrynwhylNo ratings yet
- Clinical Trials and BiostatisticsDocument16 pagesClinical Trials and BiostatisticsArumugam RamasamyNo ratings yet
- Stoma Care AlginateDocument6 pagesStoma Care AlginateWiwit ClimberNo ratings yet
- c-7 Case PresentatonDocument11 pagesc-7 Case PresentatonRaja0% (1)
- Exercise 1: Give The Correct Form of The Verb Given in Each Following BlankDocument9 pagesExercise 1: Give The Correct Form of The Verb Given in Each Following BlankSơn TrầnNo ratings yet
- Acute Kidney Injury in Patients With CancerDocument13 pagesAcute Kidney Injury in Patients With CancerzikryauliaNo ratings yet
- NIH Public Access: The Pathogenesis of Systemic Lupus Erythematosus - An UpdateDocument12 pagesNIH Public Access: The Pathogenesis of Systemic Lupus Erythematosus - An UpdateYessicaMariñosKirosNo ratings yet
- Exercise: Answer The Following Questions! Complete The Dialogue Below (For Questions Number 1 and 2)Document5 pagesExercise: Answer The Following Questions! Complete The Dialogue Below (For Questions Number 1 and 2)sindy vinaliaNo ratings yet
- Genetic DisordersDocument17 pagesGenetic DisordersNgz Krystle ChukwudifuNo ratings yet
- Paper Neupogen PDFDocument13 pagesPaper Neupogen PDFFranNo ratings yet
- Soal 1Document7 pagesSoal 1GABRIELAW ANGELIKANo ratings yet
- Salmonella 1Document3 pagesSalmonella 1Kristiara UnoNo ratings yet
- Aldinga Bay's Coastal Views March 2014Document44 pagesAldinga Bay's Coastal Views March 2014Aldinga BayNo ratings yet
- Jurnal Paliatif 1Document10 pagesJurnal Paliatif 1Anisa SilviaNo ratings yet
- DR Upul Pathirana: Endo-Bronchial Ultrasound & Trans-Bronchial Needle AspirationDocument26 pagesDR Upul Pathirana: Endo-Bronchial Ultrasound & Trans-Bronchial Needle AspirationUpul PathiranaNo ratings yet
- Adenoma Velloso y ApendicitisDocument4 pagesAdenoma Velloso y ApendicitisLuis MenesesNo ratings yet
- Uro Spots SummaryDocument25 pagesUro Spots Summarynthabiseng maboganaNo ratings yet
- Oral Manifestations of Systemic DiseasesDocument18 pagesOral Manifestations of Systemic DiseasesYashpreetsingh BhatiaNo ratings yet
- BSN - 4C: PresentorsDocument52 pagesBSN - 4C: PresentorsHanya Bint Potawan100% (1)
- 2nd Year UG SyllabusDocument24 pages2nd Year UG SyllabusMayur MulyeNo ratings yet
- NM Dosimetry Toolkit White Paper 2011 08 FV1Document16 pagesNM Dosimetry Toolkit White Paper 2011 08 FV1dengo100% (1)
- Meat Inspection GuidelineDocument43 pagesMeat Inspection GuidelineABOHEMEED ALY0% (1)
- OCDE - Health at A Glance 2019 - 4dd50c09-En PDFDocument243 pagesOCDE - Health at A Glance 2019 - 4dd50c09-En PDFJosé Anselmo de Carvalho JúniorNo ratings yet
- Classic Radiology SignsDocument9 pagesClassic Radiology SignsJui DirDapNo ratings yet
- Physical Assessment of CGDocument13 pagesPhysical Assessment of CGMichael John F. NatividadNo ratings yet
- Aplastic AnemiaDocument6 pagesAplastic AnemiaChukwu Henry ParadiseNo ratings yet
- Pain Management Guidelines HCANJ May 12 FinalDocument31 pagesPain Management Guidelines HCANJ May 12 FinalSudin SamNo ratings yet
Esophagus: Drzaiter
Esophagus: Drzaiter
Uploaded by
drynwhylOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Esophagus: Drzaiter
Esophagus: Drzaiter
Uploaded by
drynwhylCopyright:
Available Formats
esophagus
written by
DRzaiter
The Marketplace to Buy and Sell your Study Material
Buy and sell all your summaries, notes, theses, essays, papers, cases, manuals, researches, and
many more...
www.stuvia.com
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Esophagus
Lecture 21-22
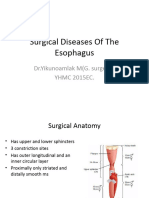
PATHOLOGY OF THE ESOPHAGUS ( Anatomy ) :
A) Function:
1) passage for ingested food
2) emesis
3) Conduit for endoscopic evaluation
4) Evaluation of aorta and heart (TEE)
B) Anatomy:
Muscular tube - Conduit from the pharynx to the stomach
Length is defined anatomically, from cricoid cartilage to the gastric orifice
Distance from the incisors 40-45 cm (actual length: M 22-28cm F 2cm shorter)
Arterial Supply
Upper → superior and inferior thyroid artery
Middle → Bronchial arteries and esophageal branches directly from aorta
Lower → L inferior phrenic and gastric
Venous Supply
Upper → esophageal venous plexus to azygos vein
Lower → esophageal branches of the coronary vein, a tributary of the portal vein
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Mucosa and 2 muscular layers
- mucosa is stratified squamous epithelium
- 2 muscular layers, inner layer is circular outer layer is longitudinal. There is not serosal
layer
- Musculature of upper 1/3 is skeletal and musculature of the lower 2/3 is smooth muscle.
2 sphincters: one is physiological one in the neck call upper esophageal sphincter, the
other is located at the diaphragm called lower esophageal sphincter
Physiology and Pathophysiology
Physiology:
food is propelled down the esophagus by a peristaltic wave.
-LES relaxes in anticipation of food, allows food enter stomach then returns to its high
resting pressure, to prevent reflux.
Pathophysiology:
- LES is to prevent reflux of gastric content.
1) Alteration of the mechanism of LES allows reflux of acid content, on an epithelial
surface that is rich in sensory innervation
2) Failure of LES to relax, causes proximal dilation with contractile disorders
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Clinical presentation
Dysphagia- difficulty in swallowing
•May be due to
- organic disease (benign strictures or esophageal carcinoma)
- esophagal motility disorders (achalasia or diffuse esophageal spasm)
•Dysphagia for solids implies severe disease, organic or functional
•Dysphagia for liquids- motility disorders
Odynophagia: painful swallowing
Esophageal pain - two sorts: heartburn and angina-like tightening pain
- Heartburn is due to reflux of gastric juice to the esophagus- esophagitis
- Angina-like tightening pain - esophageal anterior chest pain, simulates angina
pectoris - reflux esophagitis, motility disorders
Lump in the throat, evaluate carefully sensation b/c it may represent a mass lesion and
no a psychological symptom
Pyrosis or water brash associated with GERD , achalasia and esophageal strictures
Regurgitation:
- passive return of ingested food to oropharynx.
- effortless return of the gastric content into the mouth
• Postural regurgitation is a common symptom in reflux disease
• Precipitated by meals and increased in intraabd. pressure
• Overflow regurgitation into the pharynx-trachea – aspiration pneumonitis
Vomiting: active return of stomach content
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Recurrent episodes of bronchitis or pneumonia (very young, elderly, may be sign of
recurrent aspiration of esophageal or gastric content - esophageal obstruction,
congenital malformation, diverticula, or motility disorder).
Anemia (ulcerative esophagitis cause of esophageal bleeding, occult blood in stools)
Hiccups or singultus (sign of diaphragmatic irritation and early sign of stomach dilation,
MI or diaphragmatic hernia)
Esophageal diseases may mimic other process like angina pectoris. Must do cardiac
and esophageal evaluation simultaneously - both processess are common diseases.
Paraclinic investigation
Chest xray may reveal: (PA and lateral)
-aspiration pneumonitis,
-mediastinal widening,
-fluid/gas level,
-mediastinal emphysema,
-pleural effusion
Barium swallow: esophageal anatomy and function. It is safe and highly costeffective
Esophagoscopy:
-allows direct visualization of lumen of esophagus,
-essential in all patients with dysphagia asses severity of esophagitis
-can get directed Biopsy in cancer & can treat esophageal varices (injecting sclerosing
substances)
CT scan: relation to other anatomic structures and, mediastinum, esophgeal cancer.
-preop.assessment of esophageal malignancy
-extent of mural invasion,
-involvement of adjacent structures, mediastinal lymph nodes
MRI (no advantage over CT)
4
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Manometry - the pressure profile
-motility disorders
-24h.pH monitoring - pathological reflux is considered when the time in the acid zone
Ph<4 is more than 5 min.
Fluoroscopy (Radioisotope studies)
-assess g-e incompetence in pts. with reflux symptoms
esophageal transit of liquid and solid boluses in pts. with motility disorders
-stools (check for blood)
-Tests to exclude cardiac disease- ecg, coronary angiography
Disorders of Esophageal Motility
Are classified as functional disorders because they interfere with a normal act of
swallowing or produce dysphagia without any associated organic obstruction or extrinsic
compression
Upper esophageal sphincter dysfunction
-oropharyngeal dysphagia or cricopharyngeal dysfunction better described the
symptoms that occur
-when there’s difficulty propelling liquid or solid food from the oropharynx into the upper
esophagus
Causes of Oropharyngeal Dysphagia: neurogenic, myogenic, structural causes,
mechanical causes, iatrogenic causes
-The patient complains of cervical dysphagia which is localized between the thyroid
cartilage and the suprasternal notch (the classical “lump in the throat”)
-Expectoration of excessive saliva is common
-Intermittent hoarseness can occur
-Weight loss secondary to impaired caloric intake may occur
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Diagnostic Tests and Treatment
-Barium swallow may be normal especially in patients with intermittent symptoms
-Esophageal function studies (manometric and acid reflux testing) should be performed
whenever possible
-In patients with severe symptoms and no reflux, surgical intervention may be necessary
-Esophagomyotomy
Motor Disorders of the Body of the Esophagus
Esophageal motor disorders range from :
hypomotility (achalasia) to hypermotility (diffuse spasm)
Achalasia:
-primary esophageal motor disorder of unknow etiology
-uncommon (0.5-1 in 100,000)
-most common of esophageal motility disorder
-affects both sexes equally between the ages of 20 and 50
-it means “failure to relax” - the affected area is distal esophageal circular muscle.
-characterized by ineffective relaxation of the LES combined with loss of esophageal
peristalsis
-impaired emptying and gradual esophageal dilatation
-decrease or loss of myenteric ganglion cells
Symptoms
Dysfagia
- delayed and progressive; presentation (mean 2 years)
- exacerabated by emotional stress or cold fluid
Regurgitation of indigested food
6
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
- 60-90% report spontaneous or forced regurgitation of undigested food
Weight loss
Ps: Pain is not a hallmark
-Drinking large amounts of liquid necessary to push down food.
-Aspiration pneumonia is common (10% will have pulmonary complications)
-Very common complain of spitting up foul smelling secretions when lean forward.
Paraclinic Diagnosis:
CXR: air fluid levels
Barium swallow: dilated esophagus with Bird's beak deformity.
-pseudoachalasia from extrinsic mass may mimic the classic achalasia appearance
Manometry: gold standard
- elevated LES pressure (greater than 35mmHg)
- incomplete sphincter relaxation
- complete absence of peristalsis
Endoscopy: dilated esophagus with tightly closed LES→ gentle pressure will admit the
scope with a "pop“.
Treatment:
Palliation of dysphagia is the key → relieve functional obstruction of distal esophagus
- Pharmacotherapy
- botulinum toxin
- Esophageal dilation
- Operative myotomy (95% pts have complete relief)
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Pharmacotherapy: (poorly absorbed and short lived, best reserved as adjunct to other
therapies)
- Nitrites (sublingual isosorbide dinitrite)
- Ca++ channel blockers (Diltiazem, Nifedipine, Verapamil)
- Anticholinergics
- Opiods
Botox injection:
- Bind to cholinergic nerves and irreversibly inhibit Acetyl Choline release
- 60-85% of patient get relief but 50% get recurrent symptoms within 6 months.
- Endoscopically injected
- For pt who are not candidates for other therapies
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Advantages: safety, ease of administration, minimal side effects
Disadvantages: expensive, need for multiple injections, and efficacy decreased with
repeated injection
Cause obliteration of the dissection planes between submucosa and muscular layer
which will make subsequent surgery more difficult and increase risk of perforation.
Esophageal dilation
- Standard nonoperative therapy
- Break the muscle fibers (forceful dilatation of the gastroesophageal sphincter to a
diameter of 3 cm is necessary to tear the circular muscle)
- For pts with limited life expectancy
- Can have repeated dilatation
- 60-80% success rate, 5yr recurrence rate 50%
- Efficacy is decreased after second dilatation
- Perforation rate ~ 2%
Surgical treatment
- Excellent results in 90-95%
- Gold standard
- World’s largest experience in Brazil, Chagas’ disease-endemic(1 in 8 inhabitants, in
which 5% develops achalasia)
- Traditionally trans-thoracic or trans-abdominal
- Now minimally invasive Laparoscopic / Thoracoscopic
- Robotic Heller myotomy
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Indications:
- Younger than 40yrs old
- High risk of perforation
- Esophageal diverticula
- Previous surgery of GE junction
- Tortuous or dilated distal esophagus
- Recurrent symptoms despite Botox or PD therapy
- Personal choice of therapy
-Lower risk of perforation
-Better long term outcome
-Decrease chance of re-intervention
-Expose mucosal surface
-Length of myotomy
- Cephalad: 1-2 cm beyond the dilated esophagus
- Caudal: 1-2 cm into the gastric musculature or when transverse veins are encountered
Check for perforation : Meythlene blue / Air
10
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Complications
Intra-op: - Mucosa perforation
Post-op:
- Dysphagia- adhesion, inadequate myotomy
- GERD- long myotomy, nerve damage
- Delay perforation- inadequate myotomy
Diffuse Esophageal Spasm (DES)
Is poorly understood hypermotility disorder, Results from repetitive high amplitude
esophageal contractions, The etiology is unknown.
These patients typically are anxious and complain of chest pain inconsistent to eating,
exertion and position, The character of pain may mimic that of angina
-Symptoms are greatest during periods of emotional stress
Diagosis Classic criteria are: Simultaneous, multiphasic, epetitive, high amplitude
contractions that occur after a swallow
-Manometry-high amplitute repetitive contractions
11
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Treatment
-Due to the lack of understanding of this condition the treatment is less than satisfactory
-Surgery- long esophagomyotomy, from , from the arch of the aorta to just above the
LES,-antireflux op in case of GER
-Antispasmodics are occasionally helpful(calcium channel blockers and smooth muscle
relaxants)
-Response to sublingual nitroglycerin is variable
Esophageal motor disturbances
Esophageal motor disturbances occur in several of the collagen vascular diseases:
- Scleroderma (extremely common)
- Dermatomyositis
- Polymyositis
- Lupus erythematosus
Etiology is unknown, Characterized by induration of skin, fibrous replacement of smooth
muscle of internal organs and progressive loss of visceral and cutaneous function
-70% of pts have esophageal abnormalities with progressive decline in muscular
contractility towards LES.
MC GI symptom is dysphagia, Dx is made by Barium swallow xrays.
-Testing Esophageal manometry and intraesophageal pH readings are sensitive means of
detection
-Progressive reflux, ulceration of distal esophagus, strictures.
Treatment
Standard antireflux medicine includes H-2 blockers
In patients with intractable symptoms gastroesophageal reflux surgery should be
considered
12
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Esophageal Diverticula
2 nd most common motility disorder, It is an out-pouching of all or part of the wall of the
esophagus, May ocurr at any level in esophagus.
-Almost all are acquired and occur predominantly in adulthood
-Most diverticula are caused by an underlying motility disorder of the esophagus.
Classification :
Site of occurrence
- Pharyngoesophageal
- Parabronchial
- Epiphrenic
Wall thickness – True - False
Mechanism of formation
- Pulsion (as cervical Zenker’s diverticula)
- Traction
Pharyngoesophageal Diverticula (Zenker)
The most common esophageal diverticulum, Occurs between the ages of 30-50 (believed
to be acquired)
-Arises within the inferior pharyngeal constrictor, between the oblique fibers of the
thyropharyngeus muscle and the cricopharyngeus muscle
-Is a pulsion diverticulum
13
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Complaints are :
- cervical dysplasia,
- effortless regurgitation of food or pills sometimes consumed hours earlier
-Sometimes a gurgling sensation in the neck after swallowing is felt
-Putrid breath odor.
-Barium swallow establishes the diagnosis
Treatment: Surgery is indicated in symptomatic patients regardless of the size
Midesophageal (Traction) Diverticula:
Are typically associated with mediastinal granulomatous disease (TB, histoplasmosis)
-They are usually small with a blunt taperedtip that points upward
-These are usually an incidental finding on barium swallow
-They rarely cause symptoms or require treatment
-Need to be differentiated from pulsion diverticula which can also occur in this location
(associated with neuromotor esophageal dysfunction).
14
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Epiphrenic (Supradiaphragmatic) Diverticula
Generally occur within the distal 10cm of the thoracic esophagus, These are pulsion
diverticula that arise due to esophageal motor dysfunction or mechanical distal
obstruction
-Many patients are asymptomatic when diagnosed
-When symptomatic their symptoms are difficult to differentiate from: hiatal hernia, DES,
achalasia, reflux esophagitis and carcinoma
-Dysphagia and regurgitation are common symptoms
Diagnosis and Treatment:
-Diagnosis is easily made with barium swallow
-Esophageal function studies should also be performed to rule out any motor
disturbances
-Lesions < 3 cm often require no treatment
-Extreme symptomatic patients sometimes require surgical repair
Esophageal perforation
is rupture of the oesophageal wall. 56% of oesophageal perforations are iatrogenic,
usually due to medical instrumentation such as an endoscopy or paraoesophageal
surgery.[1] In contrast, the term Boerhaave's syndrome is reserved for the 10% of
oesophageal perforations which occur due to vomiting.[2]
Spontaneous perforation of the oesophagus most commonly results from a sudden
increase in intraoesophageal pressure combined with relatively negative intrathoracic
pressure caused by straining or vomiting (effort rupture of the oesophagus or
Boerhaave's syndrome). Other causes of spontaneous perforation include caustic
ingestion, pill oesophagitis, Barrett's oesophagus, infectious ulcers in patients with AIDS,
and following dilation of oesophageal strictures.
Symptoms:
Pain: acute, severe, diffuse. Over chest, neck, abdomen, with back , shoulder,inter-
scapular radiation. Back pain may predominant
15
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
-Dysphagia, dyspnea, hematemesis, cyanosis
-Sepsis, shock
-Abd. Rigidity, hypotension, fever
-Sub-cutaneous emphysema, mediastinal emphysema
-Systemic infection occur in 12 hr, polymicrobial (strepto, staphylo, psudomonas,
bacteroid)
TOPOGRAPHY:
-Spontaneous perforation: posterolateral wall of distal esophagus
-trauma : proximal ( neck or thorax, middle third )
-Iatrogenic : pharyngoesophageal junction (cricopharyngeus muscle), 0.03% risk
-Dilation: proximal or at stricture site , 1-10% risk
Paraclinic investigations
=CXR : pleural effusion : > 50% of p’t with intrathoracic perforation ( direct
contamination or reactive) , pneumomediastimum , subcutaneous emphysema,
mediastinal widening, pulmonary infiltration ;
-radiographic abnormalities in 90% p’t, but may not present in first few hours
-CT , endoscope : confirm dx
Pleural-centesis : amylase, exudate, gastric content, food
Blood test : non-specific,
Esophagram: gastrografin (FN:10%) vs barium (contraindicated if thoracoesophageal
fistula or perforation to lung suspected)
Esophageal perforation – Boerhaaven Syndrome
Spontaneous esophageal rupture followed by retching, severe N/V, without
instrumentation and external trauma
-RF: GERD, alcoholism, neurological diseases, hypertension, esophageal stricture,
esophagitis, neoplasm
16
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Management:
-Early diagnosis
-Early aggressive surgical treatment
-Broad spectrum antibiotics
-Conservative : stable, without evidence of sepsis, contained esophageal perforation
(esophagram)
Surgery : Boerhaave syndrome, unstable patients with sepsis ,contamination of
mediastinum/pleural space, retained foreign bodies, failed medical treatment
Conservative : Drainage, tube thoracostomy, stent
Surgical:
Exploration & drainage, primary closure, primary closure with cover (pleural flap/muscle
wrape, fundoplication/diaphragmatic flap), resection only ,2 stage closure, resection &
reconstruction
Hospital mortality associated with stent : 40%
Hospital mortality associated with conservative surgery : 43%
GERD (Gastroesophageal reflux disease)
GERD = symptoms of mucosal damage produced by abnormal reflux of gastric contents
into the esophagus Persistent reflux that occurs more than twice a week is considered
GERD
Pathophysiology:
Lower Esophageal Sphincter– changes in resting pressure (incompetent LES), abnormal
location (hiatal hernia)
-Excess acid production
-Delayed gastric emptying
-Decreased mucosal resistance to acid injur
17
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Other factors that may contribute to GERD include
obesity
pregnancy
smoking
Common foods that can worsen reflux symptoms include :
-citrus fruits -chocolate -spicy foods
-drinks with caffeine or alcohol
-fatty and fried foods
-garlic and onions
-mint flavorings
Symptoms Highly specific for GERD:
1-Heartburn (pyrosis)– retrosternal burning discomfort radiating toward neck
2-Regurgitation
3-Occurs mainly after large/fatty meals, worse with recumbency, and relieved by
antacids
Alarm symptoms– suggest complicated disease
Dysphagia– difficulty swallowing
Odynophagia– painful swallowing
Bleeding
Weight loss
Anemia
Long duration
No response to treatment
Complications:
Esophageal Complications :
-Esophagitis - damage of the lining(cause bleeding or ulcers)
18
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
-Peptic Strictures - scars from tissue damage →
-Barrett’s Esophagus– increased risk for adenocarcinoma
Extraesophageal Complications Secondary to pharyngeal reflux & silent aspiration
-Laryngitis
-Reactive airway disease
-Recurrent pneumonia
-Pulmonary fibrosis
Diagnosis
Empirical Treatment: Symptomatic response to antisecretory therapy with proton
pump inhibitor (PPI) or H2 antagonists assume diagnosis of GERD
Endoscopy: Part of initial evaluation, Typical esophagitis is essentially diagnostic,
Biopsy- to confirm Barrett’s
Ambulatory Reflux Monitoring:
Gold Standard for diagnosis– study actual amount of reflux occurring Usually when the
PH < 4 its pathological
Indications:
-trial of acid suppression has failed, no evidence for mucosal damage on endoscopy
-monitor control of reflux in patients w/continued symptoms on therapy Method: trans-
nasally placed catheter or wireless device attached to distal esophageal mucosa
-pH sensor connected to portable data logger
-Collection time: traditionally 24 hrs, 2-4 days with wireless device
-Consume unrestricted diet
Esophageal Manometry
19
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Measure LES pressure
Minimal use in diagnosis
Exception: evaluation of peristaltic function before antireflux surgery to exclude
major motility disorders
Barium swallow
-Limited use in diagnosis, Low sensitivity with milder forms of GERD
-Most useful for detecting peptic strictures
Treatment
Goals :
•Eliminate symptoms
•Heal esophagitis
•Prevent relapse and complications
Modalities :
Lifestyle Modification
- Most effective for infrequent heartburn
- Modify factors that may precipitate reflux:
Elevate head of bed
Decrease fat intake
Stop smoking (tobacco inhibits saliva, stimulates gastric acid, relaxes LES)
Avoid recumbency 3 hrs after eating
Lose weight if obese
- Avoid foods that decrease LES pressure: Chocolate, alcohol, peppermint, coffee, maybe
onions and garlic
- Avoid foods that can irritate damaged esophageal lining: Citrus juice, tomato juice,
pepper
Acid Suppression and Promotility Therapy
20
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Antacids
H2 Receptor Blockers
Proton Pump Inhibitors (PPIs)
-Prokinetics (help strengthen the LES and make the stomach empty faster): bethanechol
(Urecholine) and metoclopramide (Reglan)
Surgery
Indications: recurrent symptoms despite medical therapy, severe esophagitis, recurrent
pulmonary symptoms, benign stricture, Barrett’s esophagus
Most common procedures:
Nissen fundoplication (complete 360 degree)- open (abdominal or transthoracic) or
laparoscopic
Comparable safety, short-term efficacy, and pt satisfaction
Belsey Mark IV- transthoracic partial fundoplication 270 degrees (for poor esophageal
motility)
Hill Gastropexy- reconstruction of the angle of His, gastroesophageal valve for prevention
of reflux
Endoscopic Therapy
Newly approved by FDA– long-term efficacy still being defined
Methods:
1-Radiofrequency application to LES areaelectrodes to create tiny burns on the LES
(Stretta system)
2-Endoscopic sewing stitches in the LES that help strengthen the muscle (EndoCinch and
NDO Plicator )
3-Injection of nonresorbable polymer into LES region
Caustic strictures
21
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Most frequent complication of caustic burns, Caused by ingestion of caustic agents: lye,
soda, acids
Commonly taken: caustic soda, sulphuric acid from car batteries in attempted suicide
Diagnosis: history of caustic ingestion: retrosternal pain, dysphagia, shock
-Usually develops between three and eight weeks after initial injury, Pharynx is relatively
spared- short contact time
-Edema of the laryngopharynx- respiratory sy.
-Esophagus - inflammation, ulceration, necrosis, perforation
-Stomach is protected- its contents dilute whatever and neutralizes alkali.
-Perforation can occur between 3h.-3 weeks
endoscopy- the severity and extent of lesions
Early endoscopy
- asses the severity and extent of lesions
- performed within a few hours of injury
Ps: Complete endoscopy should not be attempted if there is a severe necrotizing lesion
Treatment
fluid ressuscitation,
total parenteral nutrition,
antibiotics,
Steroids
Barium swallow after 10-14 days
Strictures- dilatation treatment 3/4w.after injestion or esophageal replacement
(reconstruction: colon interposition)
22
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Benign Tumors
Benign tumors are rare (< 1 %) Classified in two groups:
- Mucosal
- Extramucosal (intramural)
60% are leiomyomas & 20% are cysts & 5% are polyps
Leiomyomas
Most common benign tumor of the esophagus its Intramural, Occur between 20-50 years
of age with no gender preponderance
-80% occur in the middle and lower third of the esophagus, they are rare in the cervical
region
-Obstruction and regurgitation may occur in large lesions(>5cm)
-Bleeding is a more common symptom of the malignant form of the tumor:
leiomyosarcoma
Esophageal Cysts
Over 60% are located along the right side of the esophagus, Are often associated with
vertebral anomalies (ex:spina bifida)
-60% present in the first year of life with either respiratory or esophageal symptoms
-Cyst found in the upper third of the esophagus present in infancy while lower third
lesions present later in childhood
23
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Pedunculated Intraluminal Tumors (Polyps)
Benign polyps are rare, Usually occur in older men and may cause intermittent
dysphagia
-Are sometimes easily missed with barium swallow and esophagoscopy
Treatment is required in symptomatic cases
- tumor enucleation
- rarely limited resection
Esophageal Carcinoma
Usually are in advanced stages at the time of diagnosis (involving the muscular wall and
extending into adjacent tissues)
Alcohol consumption and cigarette smoking seem to be the most consistent risk factors
Localization - upper 20% - middle 30% - lower 50%
CLASSIFICATION
Squamous carcinoma
- is a disease of men (5: 1)
-occurs least frequently in the cervical esophagus and most often in the upper and
midthoracic segments
Adenocarcinoma
– Type 1: Intestinal metaplasia of tubular oesophagus
– Type 2: True junctional tumours of the gastric cardia
– Type 3: Subcardial tumours which infiltrate superiorly
-Most often occur in the distal third of the esophagus(specialised columnar epithelium)in
the 6th decade of life.
-Male to female ratio is 3:1
24
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
-Patients with Barretts metaplasia are 40 times more likely to develop adenocarcinoma
Clinical Presentation:
Dysphagia is the presenting complaint in 80-90% of patients with esophageal carcinoma,
Early symptoms are sometimes nonspecific retrosternal discomfort or indigestion, As the
tumor enlarges, dysphagia becomes more progressive.
-Later symptoms include weight loss, odynophagia, chest pain and hematemesis
Diagnostic:
Esophageal biopsy
Brushings for cytologic evaluation
Barium swallow
Lugol’s solution Staging of Tumors
Endoscopic ultrasound-to define the depth of invasion and presence of
paraesophageal lymph nodes
Chest x-ray ± abnormal findings
CT scan (most widely used and now standard radiographic means of staging)
Bronchoscopy for tumors which are proximal to the trachea
Esophageal Carcinoma - TNM
Primary Tumour (T) invades
T1 l.propria/submucosa
T2 m.propria
T3 adventitia
T4 adjacent structures
Regional LNs (N)
25
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
N1 regional LN mets
Metastases (M)
Lower oesophagus:
M1a coeliac axis node
M1b distant mets
Mid/upper oesophagus
M1a not applicable
M1b distant metastases
26
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
27
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
28
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
29
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
30
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
31
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
32
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
33
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
34
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
Esophageal Carcinoma – Palliative Treatment
Extensive disease requires palliation of dysphagia:
35
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Stuvia.com - The Marketplace to Buy and Sell your Study Material
-endoscopic laser surgery for lesions less than 8 cm long
-oesophageal stentinge.g. with a Celestin tube - if longer than 8 cm
36
Downloaded by:: egoodmanmd1 | egoodman@chpnet.org
Distribution of this document is illegal
Powered by TCPDF (www.tcpdf.org)
You might also like
- Goljan Step 1 HY 36 Pages Notes PDFDocument36 pagesGoljan Step 1 HY 36 Pages Notes PDFTyler Lawrence CoyeNo ratings yet
- Louis S. Constine MD, Nancy J. Tarbell MD, Edward C. Halperin MD - Pediatric Radiation Oncology (2016, LWW) PDFDocument2,424 pagesLouis S. Constine MD, Nancy J. Tarbell MD, Edward C. Halperin MD - Pediatric Radiation Oncology (2016, LWW) PDFPan50% (2)
- Reading Test 01 - E2Lang PDFDocument25 pagesReading Test 01 - E2Lang PDFMuhammad Haneef100% (12)
- Toacs by ShireenDocument244 pagesToacs by ShireenMuhammad Zeeshan100% (1)
- Orthopaedic MCQDocument6 pagesOrthopaedic MCQGlucose DRglucoseNo ratings yet
- Surgery Lectures EsophagusDocument22 pagesSurgery Lectures Esophagusj,007No ratings yet
- Dyspepsia Lecture 6Document28 pagesDyspepsia Lecture 6Dhante MRDNo ratings yet
- Kuliah Upper Gi Tract DiseaseDocument78 pagesKuliah Upper Gi Tract DiseaseAnggun Pulihana WNo ratings yet
- Grand Rounds Index UTMB Otolaryngology Home PageDocument12 pagesGrand Rounds Index UTMB Otolaryngology Home Pagegdudex118811No ratings yet
- Bowel ObstructionDocument10 pagesBowel Obstructionenke.nwekeNo ratings yet
- 3-Pharynx. OesophagusDocument30 pages3-Pharynx. OesophagusislamNo ratings yet
- Dysphagia AhsDocument32 pagesDysphagia AhsIbrahim AchmadNo ratings yet
- Esophageal DisordersDocument37 pagesEsophageal DisordersDanielle FosterNo ratings yet
- Alimentary and Biliary Conditions 3-1Document249 pagesAlimentary and Biliary Conditions 3-1Mercy KeruboNo ratings yet
- Surgical Disease of The Esophagus: Mahteme Bekele, MD Assistant Professor of SurgeryDocument72 pagesSurgical Disease of The Esophagus: Mahteme Bekele, MD Assistant Professor of SurgeryBiniamNo ratings yet
- Class 7 (G1) - GI TractDocument112 pagesClass 7 (G1) - GI TractAdel mohammadNo ratings yet
- GIT - Prob 1Document143 pagesGIT - Prob 1anon_181166970No ratings yet
- The Blood Supply of EsophagusDocument4 pagesThe Blood Supply of EsophagusSaman SarKoNo ratings yet
- St. Anthony College of Roxas CityDocument14 pagesSt. Anthony College of Roxas CityMykristie Jho B. MendezNo ratings yet
- Gastric Outlet Obstruction (Stenosis) : Lior Shlomov 1852Document8 pagesGastric Outlet Obstruction (Stenosis) : Lior Shlomov 1852Lior ShlomovNo ratings yet
- Dysphagia: DR (Prof.) A B Singh Unit Department of General Surgery Patna Medical College & HospitalDocument48 pagesDysphagia: DR (Prof.) A B Singh Unit Department of General Surgery Patna Medical College & HospitalAswin Rajasekaran100% (1)
- Gastro NephroDocument93 pagesGastro Nephrohasanatiya41No ratings yet
- DYSPHAGIADocument46 pagesDYSPHAGIAnanohaniwiekoNo ratings yet
- Gastrointestinal and Abdominal Problems 3.LfDocument68 pagesGastrointestinal and Abdominal Problems 3.LfapocruNo ratings yet
- Powerpoint: Colorectal Surgical DiseasesDocument74 pagesPowerpoint: Colorectal Surgical Diseasesj.doe.hex_87100% (1)
- Examination of Intestinal Obstruction, Acute Abdomen and Acute Appendicitis - Eugh & BwembyaDocument29 pagesExamination of Intestinal Obstruction, Acute Abdomen and Acute Appendicitis - Eugh & BwembyaForeighn97No ratings yet
- Dysphagia: DR S Jaya SandeepDocument22 pagesDysphagia: DR S Jaya Sandeepsai kousikNo ratings yet
- Achalasia: Department of MedicineDocument21 pagesAchalasia: Department of Medicinekyliever100% (1)
- Nur Akbar A. Mini LectureDocument39 pagesNur Akbar A. Mini LectureanafauziahfitriNo ratings yet
- Esophageal DiseasesDocument9 pagesEsophageal DiseasesRashed ShatnawiNo ratings yet
- Dysphagia: DR Navin Shukla Associate Professor Department of E.N.T&H.N.SDocument64 pagesDysphagia: DR Navin Shukla Associate Professor Department of E.N.T&H.N.SNavin ShuklaNo ratings yet
- By: Isser Jorell L. Yao, RN, MAN, Ed.D.: Responses To Metabolic-Gastrointestinal and Liver AlterationsDocument65 pagesBy: Isser Jorell L. Yao, RN, MAN, Ed.D.: Responses To Metabolic-Gastrointestinal and Liver AlterationsNur SanaaniNo ratings yet
- Navan Ee Than 2015Document7 pagesNavan Ee Than 2015Yacine Tarik AizelNo ratings yet
- Pediatric Surgery PresentationDocument191 pagesPediatric Surgery PresentationdanoonotNo ratings yet
- Esophagus: Comments On Embryology of EsophagusDocument14 pagesEsophagus: Comments On Embryology of EsophagusDave AbrahamNo ratings yet
- IntussusceptionDocument24 pagesIntussusceptionOjambo Flavia100% (1)
- Intestinal Obstruction ChikaDocument45 pagesIntestinal Obstruction ChikarohitNo ratings yet
- Intestinal ObstructionDocument13 pagesIntestinal Obstructionsantosh kumarNo ratings yet
- Dysphagia: Departemen THT-KL Fakultas Kedokteran Universitas Padjadjaran 2016Document31 pagesDysphagia: Departemen THT-KL Fakultas Kedokteran Universitas Padjadjaran 2016Sherlyn YeeNo ratings yet
- Oral Revalida and Comprehensive ExamDocument13 pagesOral Revalida and Comprehensive Examlovelove DayoNo ratings yet
- Case Presentation: Intern: Iris Parcon Clerks: Karen Bianca Espinola Anna Sophia Lim Leo Salvador VedanaDocument50 pagesCase Presentation: Intern: Iris Parcon Clerks: Karen Bianca Espinola Anna Sophia Lim Leo Salvador VedanaKaren Bianca Matampale EspinolaNo ratings yet
- Surgical Diseases of The EsophagusDocument35 pagesSurgical Diseases of The Esophagusmogesie1995No ratings yet
- Peptic Ulcer DiseaseDocument63 pagesPeptic Ulcer DiseaseAli100% (1)
- CABITAC Histology (Digestive) FinalDocument9 pagesCABITAC Histology (Digestive) FinalZhon CabitacNo ratings yet
- PeritonitisDocument14 pagesPeritonitisAyad IdresNo ratings yet
- Bazo Errante 2016 REVISED Ijtra1601084Document4 pagesBazo Errante 2016 REVISED Ijtra1601084luisalfredo_montesNo ratings yet
- Power Git EndoDocument170 pagesPower Git Endoapi-3735995100% (1)
- GI Tract: Esophagus & StomachDocument126 pagesGI Tract: Esophagus & StomachPablo SisirucaNo ratings yet
- Swallowing Disorders 2022Document29 pagesSwallowing Disorders 2022Mohammed AhmedNo ratings yet
- Gastroenterology by Elagouri MohammedDocument31 pagesGastroenterology by Elagouri MohammedStylesh GuRlyNo ratings yet
- Problem 2 GI - VICKA AZWITADocument65 pagesProblem 2 GI - VICKA AZWITARana RickNo ratings yet
- Hrkansh NotesDocument424 pagesHrkansh NotesAhmed RagabNo ratings yet
- Plenary 3 Group 13Document122 pagesPlenary 3 Group 13Obet Agung 天No ratings yet
- Abdominal DistensionDocument10 pagesAbdominal DistensionMorad ImadNo ratings yet
- AchalasiaDocument5 pagesAchalasiaAli GhummiedNo ratings yet
- StomachDocument204 pagesStomachrajmv7No ratings yet
- Dysphagia and Oesophageal Carcinoma-Maj (DR) Francis KamunduDocument44 pagesDysphagia and Oesophageal Carcinoma-Maj (DR) Francis KamunduKutemwaNo ratings yet
- Pyloric StenosisDocument46 pagesPyloric Stenosishayssam rashwan81% (16)
- Obstruction EDocument10 pagesObstruction ECorina MunteanuNo ratings yet
- DYSPHAGIA Lecture NotesDocument84 pagesDYSPHAGIA Lecture Notesmcmak357No ratings yet
- DysphagiaDocument72 pagesDysphagiaMaisarah IsmailNo ratings yet
- AADocument20 pagesAAAiyaz AliNo ratings yet
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Meniscus Injury: Presented by Siti Nur Rifhan KamarudinDocument29 pagesMeniscus Injury: Presented by Siti Nur Rifhan KamarudindrynwhylNo ratings yet
- Ophthalmology SingiDocument20 pagesOphthalmology SingidrynwhylNo ratings yet
- PGI BiochemistryDocument171 pagesPGI BiochemistrydrynwhylNo ratings yet
- Deconstructing The ECG Curve - The Components of The Tracing: Key ConceptsDocument117 pagesDeconstructing The ECG Curve - The Components of The Tracing: Key ConceptsdrynwhylNo ratings yet
- Lymphatic SystemDocument22 pagesLymphatic SystemdrynwhylNo ratings yet
- Endocrine SystemDocument18 pagesEndocrine SystemdrynwhylNo ratings yet
- Digestive SystemDocument60 pagesDigestive SystemdrynwhylNo ratings yet
- Reproductive SystemDocument23 pagesReproductive SystemdrynwhylNo ratings yet
- Urinary SystemDocument30 pagesUrinary SystemdrynwhylNo ratings yet
- Thyroid ParathyroidDocument17 pagesThyroid ParathyroiddrynwhylNo ratings yet
- Energy BalanceDocument27 pagesEnergy BalancedrynwhylNo ratings yet
- Clinical Trials and BiostatisticsDocument16 pagesClinical Trials and BiostatisticsArumugam RamasamyNo ratings yet
- Stoma Care AlginateDocument6 pagesStoma Care AlginateWiwit ClimberNo ratings yet
- c-7 Case PresentatonDocument11 pagesc-7 Case PresentatonRaja0% (1)
- Exercise 1: Give The Correct Form of The Verb Given in Each Following BlankDocument9 pagesExercise 1: Give The Correct Form of The Verb Given in Each Following BlankSơn TrầnNo ratings yet
- Acute Kidney Injury in Patients With CancerDocument13 pagesAcute Kidney Injury in Patients With CancerzikryauliaNo ratings yet
- NIH Public Access: The Pathogenesis of Systemic Lupus Erythematosus - An UpdateDocument12 pagesNIH Public Access: The Pathogenesis of Systemic Lupus Erythematosus - An UpdateYessicaMariñosKirosNo ratings yet
- Exercise: Answer The Following Questions! Complete The Dialogue Below (For Questions Number 1 and 2)Document5 pagesExercise: Answer The Following Questions! Complete The Dialogue Below (For Questions Number 1 and 2)sindy vinaliaNo ratings yet
- Genetic DisordersDocument17 pagesGenetic DisordersNgz Krystle ChukwudifuNo ratings yet
- Paper Neupogen PDFDocument13 pagesPaper Neupogen PDFFranNo ratings yet
- Soal 1Document7 pagesSoal 1GABRIELAW ANGELIKANo ratings yet
- Salmonella 1Document3 pagesSalmonella 1Kristiara UnoNo ratings yet
- Aldinga Bay's Coastal Views March 2014Document44 pagesAldinga Bay's Coastal Views March 2014Aldinga BayNo ratings yet
- Jurnal Paliatif 1Document10 pagesJurnal Paliatif 1Anisa SilviaNo ratings yet
- DR Upul Pathirana: Endo-Bronchial Ultrasound & Trans-Bronchial Needle AspirationDocument26 pagesDR Upul Pathirana: Endo-Bronchial Ultrasound & Trans-Bronchial Needle AspirationUpul PathiranaNo ratings yet
- Adenoma Velloso y ApendicitisDocument4 pagesAdenoma Velloso y ApendicitisLuis MenesesNo ratings yet
- Uro Spots SummaryDocument25 pagesUro Spots Summarynthabiseng maboganaNo ratings yet
- Oral Manifestations of Systemic DiseasesDocument18 pagesOral Manifestations of Systemic DiseasesYashpreetsingh BhatiaNo ratings yet
- BSN - 4C: PresentorsDocument52 pagesBSN - 4C: PresentorsHanya Bint Potawan100% (1)
- 2nd Year UG SyllabusDocument24 pages2nd Year UG SyllabusMayur MulyeNo ratings yet
- NM Dosimetry Toolkit White Paper 2011 08 FV1Document16 pagesNM Dosimetry Toolkit White Paper 2011 08 FV1dengo100% (1)
- Meat Inspection GuidelineDocument43 pagesMeat Inspection GuidelineABOHEMEED ALY0% (1)
- OCDE - Health at A Glance 2019 - 4dd50c09-En PDFDocument243 pagesOCDE - Health at A Glance 2019 - 4dd50c09-En PDFJosé Anselmo de Carvalho JúniorNo ratings yet
- Classic Radiology SignsDocument9 pagesClassic Radiology SignsJui DirDapNo ratings yet
- Physical Assessment of CGDocument13 pagesPhysical Assessment of CGMichael John F. NatividadNo ratings yet
- Aplastic AnemiaDocument6 pagesAplastic AnemiaChukwu Henry ParadiseNo ratings yet
- Pain Management Guidelines HCANJ May 12 FinalDocument31 pagesPain Management Guidelines HCANJ May 12 FinalSudin SamNo ratings yet