Professional Documents
Culture Documents
Home Sleep Tests For Obstructive Sleep Apnea (OSA) : Mukesh Kapoor, MD, and Glen Greenough, MD
Home Sleep Tests For Obstructive Sleep Apnea (OSA) : Mukesh Kapoor, MD, and Glen Greenough, MD
Uploaded by
Phạm Văn HiệpCopyright:
Available Formats
You might also like
- ACS Surgery - Principles and Practice (PDFDrive) PDFDocument2,184 pagesACS Surgery - Principles and Practice (PDFDrive) PDFMandela Kibiriti100% (3)
- Mapeh Least Learned Competencies 6Document5 pagesMapeh Least Learned Competencies 6Anonymous QnNICuArTx75% (12)
- Cigna Medical Coverage Policy For Sleep Testing ServicesDocument29 pagesCigna Medical Coverage Policy For Sleep Testing ServicesPhạm Văn HiệpNo ratings yet
- Prov Prot 20118Document17 pagesProv Prot 20118IlhamNo ratings yet
- Estimation of The Apnea-Hypopnea Index in A Heterogeneous Sleep-Disordered Population Using Optimised Cardiovascular FeaturesDocument16 pagesEstimation of The Apnea-Hypopnea Index in A Heterogeneous Sleep-Disordered Population Using Optimised Cardiovascular FeaturesChuyên Mai TấtNo ratings yet
- (E) 2016 VERBRAECKEN Diagnostic Techniques TEXTDocument4 pages(E) 2016 VERBRAECKEN Diagnostic Techniques TEXTJPNo ratings yet
- Sleep Studies For Sleep-Related Breathing Disorders: ConsensusDocument9 pagesSleep Studies For Sleep-Related Breathing Disorders: Consensusoutro yoongiNo ratings yet
- Sleep Study InterpretationDocument4 pagesSleep Study InterpretationgreenNo ratings yet
- JCSM 14 9 1495Document7 pagesJCSM 14 9 1495Bagus Tri WahyudiNo ratings yet
- JcsmJC1900562 W22pod AnsweredDocument13 pagesJcsmJC1900562 W22pod Answeredlion5835No ratings yet
- Updates On Definition, Consequences, and Management of Obstructive Sleep ApneaDocument7 pagesUpdates On Definition, Consequences, and Management of Obstructive Sleep ApneapvillagranNo ratings yet
- Poly Som No GramDocument65 pagesPoly Som No Gramameer abdullahNo ratings yet
- Khan Doker Scoring Tit BDocument11 pagesKhan Doker Scoring Tit BbengheniaNo ratings yet
- PolysomnographyDocument65 pagesPolysomnographyRickamhaey FebreraNo ratings yet
- Clinical Assessment of SleepinessDocument8 pagesClinical Assessment of SleepinessYusmiatiNo ratings yet
- PolysomnographyDocument4 pagesPolysomnographySaba RiazNo ratings yet
- Polysomnography - Wikipedia, The Free EncyclopediaDocument7 pagesPolysomnography - Wikipedia, The Free EncyclopediaPrashant KumarNo ratings yet
- Automated Screening For Sleep Apnoea in The Home Environment v0Document15 pagesAutomated Screening For Sleep Apnoea in The Home Environment v0bengheniaNo ratings yet
- Obstructive Sleep Apnea Research PaperDocument7 pagesObstructive Sleep Apnea Research Paperefe8zf19100% (1)
- SleepMonitoring MPDI PDFDocument14 pagesSleepMonitoring MPDI PDFFanny MontesNo ratings yet
- Portable Devices Used For Home Testing in Obstructive Sleep ApneaDocument42 pagesPortable Devices Used For Home Testing in Obstructive Sleep ApneaCalifornia Technology Assessment Forum0% (1)
- Stopbang in AsianDocument6 pagesStopbang in AsianwandapandabebeNo ratings yet
- Interpretation of The PolysomnogramDocument15 pagesInterpretation of The Polysomnogramapi-19500641No ratings yet
- Society of Anesthesia and Sleep Medicine Educational Document: Recommendations For Management of Obstructive Sleep Apnea in The Perioperative PeriodDocument27 pagesSociety of Anesthesia and Sleep Medicine Educational Document: Recommendations For Management of Obstructive Sleep Apnea in The Perioperative PeriodMuhammad SyammNo ratings yet
- Lazazzera Et Al-2021-Detection and Classification of Sleep Apnea and Hypopnea Using PPG and $SpO - 2$Document13 pagesLazazzera Et Al-2021-Detection and Classification of Sleep Apnea and Hypopnea Using PPG and $SpO - 2$Peyman BakhshandeNo ratings yet
- 152 Obstructive Sleep Apnoea and Anaesthesia 1Document6 pages152 Obstructive Sleep Apnoea and Anaesthesia 1Echo WahyudiNo ratings yet
- Punjabi, 2008Document8 pagesPunjabi, 2008a3llamNo ratings yet
- Polisomnografí A Dinamica No Dise.: Club de Revistas Julián David Cáceres O. OtorrinolaringologíaDocument25 pagesPolisomnografí A Dinamica No Dise.: Club de Revistas Julián David Cáceres O. OtorrinolaringologíaDavid CáceresNo ratings yet
- Insomnia and Excessive Daytime Sleepiness in ObstrDocument3 pagesInsomnia and Excessive Daytime Sleepiness in ObstrChatterjee SomanNo ratings yet
- Sleep Disorders Research PaperDocument4 pagesSleep Disorders Research Papergvzexnzh100% (1)
- Sleep Apnea Term PaperDocument8 pagesSleep Apnea Term Paperf1gisofykyt3100% (1)
- Automatic Detection of Respiratory Arrests in OSA Patients Using PPG and Machine Learning TechniquesDocument15 pagesAutomatic Detection of Respiratory Arrests in OSA Patients Using PPG and Machine Learning TechniquesDayana VieiraNo ratings yet
- 2 - Sastow - Et - Al - 2024 - Controversies in Sleep ApneaDocument20 pages2 - Sastow - Et - Al - 2024 - Controversies in Sleep Apneaamalia2_3No ratings yet
- Literature Review Sleep ApnoeaDocument6 pagesLiterature Review Sleep Apnoeaelfgxwwgf100% (1)
- Development of An IoT Based Sleep Apnea MonitoringDocument16 pagesDevelopment of An IoT Based Sleep Apnea Monitoringngocoanh1828No ratings yet
- JCSM 13 3 479Document26 pagesJCSM 13 3 479Fitria ChandraNo ratings yet
- The Prevalence of Obstructive Sleep Apnea in Patients With Difficult-To-Treat AsthmaDocument7 pagesThe Prevalence of Obstructive Sleep Apnea in Patients With Difficult-To-Treat AsthmaBarbara WilhelminNo ratings yet
- Perioperative Management of OSADocument69 pagesPerioperative Management of OSAandynightmare97No ratings yet
- Neurological Assgfhgfhfgessment 1Document8 pagesNeurological Assgfhgfhfgessment 1Husaifah BaliwanNo ratings yet
- Clinical Context: Obesity RiskDocument3 pagesClinical Context: Obesity RiskkaznielsNo ratings yet
- Research Paper On Obstructive Sleep ApneaDocument6 pagesResearch Paper On Obstructive Sleep Apneaafeatoxmo100% (1)
- Obstructive Sleep ApnoeaDocument69 pagesObstructive Sleep ApnoeaPrasanna Datta100% (1)
- Journal of Sleep Research - 2016 - Lucey - Comparison of A Single Channel EEG Sleep Study To PolysomnographyDocument11 pagesJournal of Sleep Research - 2016 - Lucey - Comparison of A Single Channel EEG Sleep Study To PolysomnographyIoana GuțăNo ratings yet
- Obstructive Sleep Apnea and Analgesia - SJH PowerpointDocument29 pagesObstructive Sleep Apnea and Analgesia - SJH PowerpointAbd ZouhierNo ratings yet
- From Pulses To Sleep Stages: Towards Optimized Sleep Classification Using Heart-Rate VariabilityDocument17 pagesFrom Pulses To Sleep Stages: Towards Optimized Sleep Classification Using Heart-Rate Variability葛子骏No ratings yet
- 1 s2.0 S0007091223001915 MainDocument3 pages1 s2.0 S0007091223001915 Mainema moralesNo ratings yet
- Obstructive Sleep Apnoea Syndrome A Systematic Literature ReviewDocument4 pagesObstructive Sleep Apnoea Syndrome A Systematic Literature Reviewc5nah867No ratings yet
- Treating Obstructive Sleep Apnea Improves Essential Hypertension and Quality of LifeDocument8 pagesTreating Obstructive Sleep Apnea Improves Essential Hypertension and Quality of Life'ArifahAhmadNo ratings yet
- Obstructive Sleep Apnea Syndrome: Diagnosis and Management: A B S T R A C TDocument13 pagesObstructive Sleep Apnea Syndrome: Diagnosis and Management: A B S T R A C Tsafwand90No ratings yet
- New Seep Apnea AIDocument15 pagesNew Seep Apnea AIgauravchauNo ratings yet
- A Respiratory Movement Monitoring System Using Fiber-Grating Vision Sensor For Diagnosing Sleep ApDocument8 pagesA Respiratory Movement Monitoring System Using Fiber-Grating Vision Sensor For Diagnosing Sleep ApRamzi AlmohtasibNo ratings yet
- 3389 PDFDocument6 pages3389 PDFvarun sahaniNo ratings yet
- Patient Characteristics Affecting Accurate Detection of Sleep Apnea Using A Bed Sheet-Type Portable MonitorDocument8 pagesPatient Characteristics Affecting Accurate Detection of Sleep Apnea Using A Bed Sheet-Type Portable MonitorNadhifa TrivandariNo ratings yet
- Pats 200709-155mgDocument8 pagesPats 200709-155mgDea MaulidiaNo ratings yet
- Home Set Up Polysomnography in The Assessment of Suspected Obstructive Sleep ApneaDocument7 pagesHome Set Up Polysomnography in The Assessment of Suspected Obstructive Sleep ApneaPhạm Văn HiệpNo ratings yet
- Questions About Sleep StudiesDocument2 pagesQuestions About Sleep Studiessuresh2250No ratings yet
- Botelho 09Document8 pagesBotelho 09moiNo ratings yet
- Evaluation of Pressure Bed Sensor For Automatic SAHS ScreeningDocument9 pagesEvaluation of Pressure Bed Sensor For Automatic SAHS ScreeningJuan José Santana HidalgoNo ratings yet
- Does Using Pressure-Controlled Ventilation To Rest Respiratory Muscles Improve Sleep in ICU PatientsDocument8 pagesDoes Using Pressure-Controlled Ventilation To Rest Respiratory Muscles Improve Sleep in ICU Patientscard breatheNo ratings yet
- Sleep Studies in ChildrenDocument12 pagesSleep Studies in ChildrenJHONATAN MATA ARANDANo ratings yet
- Ehac 349Document3 pagesEhac 349Akhmad HidayatNo ratings yet
- Fast Facts: Excessive Daytime Sleepiness Associated with Obstructive Sleep ApneaFrom EverandFast Facts: Excessive Daytime Sleepiness Associated with Obstructive Sleep ApneaNo ratings yet
- Sapa Where Heaven and Earth Meet - NHÓM 3Document22 pagesSapa Where Heaven and Earth Meet - NHÓM 3Phạm Văn HiệpNo ratings yet
- Unit Name: Unit Location: Program: Nova Scotia Health Authority Inpatient ProfileDocument4 pagesUnit Name: Unit Location: Program: Nova Scotia Health Authority Inpatient ProfilePhạm Văn HiệpNo ratings yet
- SapaDocument1 pageSapaPhạm Văn HiệpNo ratings yet
- Sapa Where Heaven and Earth Meet - NHÓM 3Document22 pagesSapa Where Heaven and Earth Meet - NHÓM 3Phạm Văn HiệpNo ratings yet
- k2 Attachments Danh Gia Thuc Trang Va Giai Phap Nang Cao Chat Luong Ghi Chep Ho So Benh An Cai Tien Cua DD Tai BvagDocument12 pagesk2 Attachments Danh Gia Thuc Trang Va Giai Phap Nang Cao Chat Luong Ghi Chep Ho So Benh An Cai Tien Cua DD Tai BvagPhạm Văn HiệpNo ratings yet
- Tracheostomy in Infants in The Neonatal Intensive Care Unit: Education/Practice GapsDocument14 pagesTracheostomy in Infants in The Neonatal Intensive Care Unit: Education/Practice GapsPhạm Văn HiệpNo ratings yet
- Quy Trinh Cham Soc Dieu Duong Noi KhoaDocument41 pagesQuy Trinh Cham Soc Dieu Duong Noi KhoaPhạm Văn HiệpNo ratings yet
- What Is OtolaryngologyDocument37 pagesWhat Is OtolaryngologyPhạm Văn HiệpNo ratings yet
- Lippert 2014Document5 pagesLippert 2014Phạm Văn HiệpNo ratings yet
- Home Set Up Polysomnography in The Assessment of Suspected Obstructive Sleep ApneaDocument7 pagesHome Set Up Polysomnography in The Assessment of Suspected Obstructive Sleep ApneaPhạm Văn HiệpNo ratings yet
- Polysomnograpy: Charmain Beatriz A. AtosDocument62 pagesPolysomnograpy: Charmain Beatriz A. AtosPhạm Văn HiệpNo ratings yet
- Caffeine Effects On Sleep Taken 0, 3, or 6 Hours Before Going To BedDocument6 pagesCaffeine Effects On Sleep Taken 0, 3, or 6 Hours Before Going To BedPhạm Văn HiệpNo ratings yet
- Polysomnography: Understanding This Technology's Past Might Guide Future DevelopmentsDocument3 pagesPolysomnography: Understanding This Technology's Past Might Guide Future DevelopmentsPhạm Văn HiệpNo ratings yet
- Kota Gal 2012Document16 pagesKota Gal 2012Phạm Văn HiệpNo ratings yet
- Digital Tools in Polysomnography: Rajeev Agarwal and Jean GotmanDocument8 pagesDigital Tools in Polysomnography: Rajeev Agarwal and Jean GotmanPhạm Văn HiệpNo ratings yet
- 498 Republic of Moldova Fact SheetsDocument2 pages498 Republic of Moldova Fact SheetsAlmubashir AlbaeidNo ratings yet
- Diabetic NeuropathyDocument4 pagesDiabetic NeuropathyAsish GeiorgeNo ratings yet
- Effects of Massage and Acupressure On Relieving.10Document9 pagesEffects of Massage and Acupressure On Relieving.10Riska amaliaNo ratings yet
- Jurnal Acute Decompensated Heart FailureDocument4 pagesJurnal Acute Decompensated Heart FailureMayang Sri WulandNo ratings yet
- Lesson 3 - Basic Principles of Physical FitnessDocument20 pagesLesson 3 - Basic Principles of Physical FitnessJohn Michael AgustinNo ratings yet
- Hospital and Clinical Pharmacy CH 1 Hospital Pharmacy NotesDocument12 pagesHospital and Clinical Pharmacy CH 1 Hospital Pharmacy Notesmaharachandana18No ratings yet
- Patient Admission Assessment FormDocument1 pagePatient Admission Assessment Formprasanna_326avanthiNo ratings yet
- Acne Blackheads Pimple Zits MedlinePlusgrzkjxirmtDocument2 pagesAcne Blackheads Pimple Zits MedlinePlusgrzkjxirmtdollarcanvas0No ratings yet
- Indian Nutraceutical IndustryDocument64 pagesIndian Nutraceutical Industryhariom100% (2)
- Architectural Planning 2Document24 pagesArchitectural Planning 2rogelio labiaoNo ratings yet
- TRIAGEDocument55 pagesTRIAGELaveena AswaleNo ratings yet
- Nishtha Annual Report 2014-15Document32 pagesNishtha Annual Report 2014-15Sunny DuggalNo ratings yet
- Contemporary Orthodontics, 5th Ed: Book ReviewDocument1 pageContemporary Orthodontics, 5th Ed: Book ReviewPaula Diaz100% (1)
- Safety Training ProgramDocument43 pagesSafety Training ProgramBhavesh PatelNo ratings yet
- Activity 1 - CPHDocument2 pagesActivity 1 - CPHMA. ANDREA NICOLE DURANNo ratings yet
- Midterm DraftDocument32 pagesMidterm DraftUn knownnnNo ratings yet
- AUS - Boardreviewer (Test Your Knowledge)Document177 pagesAUS - Boardreviewer (Test Your Knowledge)Yusra FaisalNo ratings yet
- Evolution of Bhramari Pranayam in The Management of Menopausal SyndromeDocument7 pagesEvolution of Bhramari Pranayam in The Management of Menopausal SyndromeDr Kirti BhatiNo ratings yet
- Health Infrastructure and Economic Development in IndiaDocument9 pagesHealth Infrastructure and Economic Development in IndiaAkanksha PalNo ratings yet
- Photo TherapyDocument7 pagesPhoto TherapyMaysa Ismail100% (1)
- SHE List DocumentDocument1 pageSHE List DocumentMunajamNo ratings yet
- COMMISSION ON HIGHER EDUCATION (CHED) Medtech Laws PHDocument2 pagesCOMMISSION ON HIGHER EDUCATION (CHED) Medtech Laws PHJohn Michael CastroNo ratings yet
- Capinpin Research PaperDocument16 pagesCapinpin Research Paperfrancine.malit24No ratings yet
- EDU501Document7 pagesEDU501PatriciaSugpatanNo ratings yet
- CASR Part 67 Ed. 1 Amdt 0 - Medical Standard and CertificationDocument43 pagesCASR Part 67 Ed. 1 Amdt 0 - Medical Standard and CertificationR SetiawanNo ratings yet
- 08 OHS Journal Aug 2012Document60 pages08 OHS Journal Aug 2012NazirAhmadBashiriNo ratings yet
- Acute ColitisDocument8 pagesAcute ColitisKhurram NadeemNo ratings yet
- Treatment of Endometriosis in Women Desiring FertilityDocument23 pagesTreatment of Endometriosis in Women Desiring FertilityVaisnavi Muthoovaloo67% (3)
Home Sleep Tests For Obstructive Sleep Apnea (OSA) : Mukesh Kapoor, MD, and Glen Greenough, MD
Home Sleep Tests For Obstructive Sleep Apnea (OSA) : Mukesh Kapoor, MD, and Glen Greenough, MD
Uploaded by
Phạm Văn HiệpOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Home Sleep Tests For Obstructive Sleep Apnea (OSA) : Mukesh Kapoor, MD, and Glen Greenough, MD
Home Sleep Tests For Obstructive Sleep Apnea (OSA) : Mukesh Kapoor, MD, and Glen Greenough, MD
Uploaded by
Phạm Văn HiệpCopyright:
Available Formats
CLINICAL REVIEW
Home Sleep Tests for Obstructive Sleep Apnea
(OSA)
Mukesh Kapoor, MD, and Glen Greenough, MD
Obstructive sleep apnea (OSA) is a fairly common condition that, if left untreated, can lead to complica-
tions such as high blood pressure and heart disease. Polysomnography (PSG) is the most accurate
method for diagnosing OSA, but it is a cumbersome and expensive test. A well-validated, easier to per-
form and less expensive alternative is the home sleep test (HST). The purpose of this review is to edu-
cate the primary care provider about the important differences between PSG and HSTs, the advantages
and limitations of both modalities, identifying patients who are appropriate candidates for the HST,
identifying patients in whom the HST should not be performed, and further evaluation of patients who
have a negative HST. (J Am Board Fam Med 2015;28:504 –509.)
Keywords: Home Sleep Testing, Monitoring, Obstructive Sleep Apnea, Out of Center Sleep Testing, Portable Moni-
toring
Obstructive sleep apnea (OSA) is thought to affect PSG, including electroencephalography (EEG)
between 3% and 7% of the population,1 although a leads, which record brain activity; electrooculog-
significantly higher prevalence is seen in certain raphy leads, which measure eye movement; elec-
subgroups of patients, such as those with atrial tromyography leads, which measure muscle tone;
fibrillation,2,3 congestive heart failure,4,5 resistant a nasal pressure transducer and oronasal therm-
hypertension,6 type 1 diabetes mellitus,7 type 2 istor, which measures respiratory airflow; respira-
diabetes mellitus,8 and morbid obesity.9 One study tory inductance plethysmography belts, which measure
showed that approximately 32% of patients in a respiratory effort; electrocardiography leads, which
primary care setting have a high pretest probability measure cardiac activity; a pulse oximeter probe,
for OSA.10 Some symptoms associated with OSA which measures oxygen saturation; and limb leads,
include snoring, observed pauses in breathing dur- which measure limb movements. EEG allows for
ing sleep, frequent awakenings, nocturia, nonre- the detection of different sleep stages, analysis of
freshing sleep, and feeling tired and sleepy during sleep architecture, differentiation between awake
the day. Untreated OSA can increase the risk for and sleep, and identification of abnormal brain ac-
developing other medical problems, including high tivity such as seizures. Electrooculography and
blood pressure and heart disease.11 electromyography help in the detection of rapid
The most accurate method for diagnosing eye movement (REM) sleep, as there are character-
OSA is by polysomnography (PSG), which re- istic eye movements and loss of muscle tone during
quires that the patient sleep overnight in a sleep this sleep stage. Trained sleep technologists set up
laboratory. Multiple sensors are used during the patient for PSG in the sleep laboratory and use
a video camera to monitor the patient during this
test. The position of the patient (supine vs. side vs.
This article was externally peer reviewed. prone) and abnormal body movements can be vi-
Submitted 8 September 2014; revised 8 February 2015;
accepted 23 February 2015. sually recorded. Some patients can have positional
From the Sleep Disorders Center, Dartmouth Hitchcock sleep apnea, which is more severe in the supine po-
Medical Center, Lebanon, NH.
Funding: none. sition and less so when positioned on the side.12
Conflict of interest: none declared. If a patient is spending the majority of the night on
Corresponding author: Mukesh Kapoor, MD, 18 Old Etna
Road, Lebanon, NH 03766 (E-mail: mukeshkapoor2011@ their side, the technologist can intervene and have
u.northwestern.edu). them spend some time on their back to look for such
504 JABFM July–August 2015 Vol. 28 No. 4 http://www.jabfm.org
a positional change.13 If there is evidence of signifi- arousal from sleep. Patients may also have other
cant OSA during the early part of this test, the tech- respiratory abnormalities during which there is in-
nologist can initiate continuous positive airway pres- creased effort to breathe, leading to an arousal.
sure titration and continue this for the remainder of These episodes are called respiratory effort–related
the study time. arousals. The above respiratory abnormalities have
Some patients undergoing PSG may experience very specific technical definitions, and the reader is
anxiety and discomfort associated with sleeping referred to the American Academy of Sleep Medi-
outside of the home environment. Depending on cine (AASM) guidelines on scoring respiratory
the geographic location, PSG might be unavailable events for further details.23
or there might be a long wait time before a patient The principal way to detect arousals from sleep
can undergo this test.14,15 PSG is cumbersome be- is through the use of EEG. It is important for
cause multiple sensors (detailed above) are used, health care providers to recognize that the most
and it can be uncomfortable for some patients. PSG commonly used HSTs do not typically include
is also expensive; reimbursement from the Centers EEG and thus cannot detect respiratory events that
for Medicare & Medicaid Services (CMS) is ap- lead only to an arousal. Thus a patient with OSA
proximately $700. consisting of predominantly arousal-based respira-
A well-validated alternative to PSG is the home tory events can have a negative HST. This is espe-
sleep test (HST).16 –22 This is also referred to as a cially important in pediatric patients and patients
portable monitor or an out-of-center sleep test. As who have a low body mass index (BMI) because
the name of this test suggests, the patient stays in both are more likely to have respiratory events that
their home when it is performed.13 This is espe- lead to an arousal rather than desaturation.24,25
cially beneficial for patients who might feel anxious The parameters which are commonly measured
staying overnight in a sleep laboratory for PSG. by a HST are also recorded during PSG in addition
The HST has fewer sensors, is more compact, and to several other variables including brain activity
is less cumbersome to perform. A technologist is through EEG. Thus, having EEG during PSG
not needed to monitor the patient during the HST. allows for the detection of respiratory events that
Given the prevalence of OSA, as discussed earlier, are associated with arousals. The EEG component
the HST can be a useful tool for primary care of PSG also allows one to know when a patient is
providers to evaluate their patients suspected to awake and when they are asleep, providing a more
have this disorder. The HST can aid in the early accurate assessment for the presence of OSA and its
diagnosis and initiation of treatment in these pa- severity. For example, a patient undergoing PSG
tients. The HST is also less expensive; reimburse- may spend 10 hours in bed on the night of the test,
ment from the CMS is approximately $250. but the EEG may show that the patient actually
The HSTs most commonly used in routine clin- slept for only 5 hours. If a total of 100 respiratory
ical practice have sensors that measure only respi- events were recorded during the test, one would
ratory airflow, respiratory effort, and oxygen satu- calculate the severity of this patient’s sleep apnea at
ration. Some HSTs have a built-in sensor to detect 100 events in 5 hours, or 20 events/h. By contrast,
body position and an actigraph, which can be used a HST cannot differentiate between wake and
as a surrogate marker for identifying when the sleep. If the above patient were to undergo a HST,
patient is awake and sleep.13 The majority of com- the severity of their sleep apnea would be calculated
monly used HSTs do not include EEG monitoring. at 100 events (in all likelihood the HST would
The few HSTs that do have the capability of EEG detect fewer of the respiratory events as well, but
monitoring are not widely available and are more for argument’s sake we will leave the number at
cumbersome and expensive. 100) in the total recording time of 10 hours, or 10
Patients with OSA can have several different events/h. Thus a HST tends to underestimate the
kinds of respiratory abnormalities. They can have severity of sleep apnea. This is especially of conse-
apneas, which are defined as the cessation of quence in patients with mild sleep apnea in whom
breathing for ⱖ10 seconds. Another type of respi- the HST can be negative because of the above.
ratory abnormality is the hypopnea, which repre- While some HSTs use actigraphy to differentiate
sents attenuation in the depth of respiration for at between wake and sleep, one must remember that
least 10 seconds that leads to desaturation or this is only a surrogate marker and can give flawed
doi: 10.3122/jabfm.2015.04.140266 Home Sleep Tests for OSA 505
results, particularly in the presence of periodic limb BMI.29 –31 It is therefore advisable to perform PSG
movements, body movements following an arousal, in patients with morbid obesity (BMI ⱖ40 kg/m2).
and in patients with REM sleep behavior disorder.13 Primary care physicians frequently have patients
The AASM recommends that the HST should with hypertension and diabetes mellitus. Neither of
be used only in patients with a high pretest prob- these conditions is a contraindication to perform-
ability for moderate to severe OSA.26 Unfortu- ing the HST.
nately, in our current health care environment, the As mentioned earlier, the most commonly used
majority of patients suspected of having OSA are HSTs lack EEG monitoring and thus should not be
channeled toward getting the HST, irrespective of used in patient suspected of having nocturnal sei-
their pretest probability.27 This increases the risk zures. Other patients who are poor candidates for
of having false-negative results with the HST. the HST include those in whom hypoventilation
Many patients and clinicians are falsely reassured (such as patients using narcotics, those who have
by a nondiagnostic HST. Not acting on these neg- neuromuscular disease, or those who have a high
ative results by pursuing PSG can leave a patient BMI and could have OHS) or nocturnal arrhyth-
with OSA undiagnosed. mias are suspected.32 Patients who have low oxygen
A study published by a referral sleep disorders saturation at baseline or are receiving supplemental
center looked at 187 patients who were suspected oxygen are also poor candidates for the HST.32 In
of having OSA (history of snoring along with an addition, the HST should not be used in pediatric
Epworth score ⬎7 and/or a history of tiredness) patients because it can miss arousal-based hypopneas,
but had a negative HST.28 All these patients un- which tend to be more frequent in this population.24
derwent PSG, which showed that 90% of them had If the patient spends the majority of the night on
OSA (26% had mild OSA, 43% had moderate their side or outside of REM sleep, one might
OSA, and 21% had severe OSA). The fact that such never know the true severity of their OSA because
a significant number of patients with a negative the latter tends to be worse in the supine position
HST were found to be positive for OSA on PSG and during REM sleep.12 Some HSTs have a body
was likely secondary to several factors, including position monitor whereas others do not. The most
the inability of the HST device to detect respira- commonly available HSTs do not have EEG mon-
tory events which were only associated with arous- itoring and therefore cannot record sleep stages.
als, the use of total recording time in lieu of total sleep Body position and sleep stages are routinely re-
time, and the use of the HST device in a population corded during PSG. This can quantify the exact
of patients who might not have had a high pretest duration of time spent by the patient in the supine
probability for moderate to severe OSA. position and in REM sleep. Other problems with
The AASM recommends that the HST should the HST include a data loss rate of between 3% and
not be used in patients with significant comorbid 18%.13 As opposed to PSG, loss of a sensor signal
medical conditions (such as those with moderate to cannot be corrected during a HST because of the
severe pulmonary disease, neuromuscular disease, lack of live monitoring and the absence of a tech-
and congestive heart failure) that may degrade the nologist during this test. For similar reasons, con-
accuracy of this test and in patients suspected of tinuous positive airway pressure titration cannot be
having other sleep disorders (such as central sleep performed during a HST.13
apnea, periodic limb movement disorder, insomnia, There is a unique HST that collects peripheral
parasomnias, circadian rhythm disorders, narco- arterial tone (PAT), oxygen saturation, heart rate, and
lepsy, and REM sleep behavior disorder).26 The actigraphy data.32 This device is validated for the
AASM also recommends against using the HST for diagnosis of OSA.22,33–36 The PAT signal is a mea-
screening asymptomatic populations.26 sure of sympathetic activity and is augmented, along
There are no clear-cut guidelines for sleep test- with an increase in the heart rate and a decrease in
ing in obese (BMI ⱖ30 kg/m2) patients suspected oxygen saturation, at the termination of a respiratory
of having OSA. Obesity by itself is not an indica- event.32,34 Using the above measurements, this device
tion for obtaining a PSG. Obese patients who are can indirectly detect respiratory events. It also has an
suspected of having obesity hypoventilation syn- built-in algorithm that uses the PAT and actigraphy
drome (OHS), however, should undergo PSG. The data to estimate sleep stages.32 This device does not,
incidence of OHS increases with an increase in however, measure direct respiratory flow and respira-
506 JABFM July–August 2015 Vol. 28 No. 4 http://www.jabfm.org
tory effort and thus cannot distinguish between cen- occur in patients who have periodic limb move-
tral apneas, obstructive apneas, and hypopneas.34 In ments.34 Lastly, the detection of sleep stages by this
addition, this device has no way of quantifying the device has only moderate agreement with the more
cause of increased sympathetic activity which can also standard technique of PSG.37
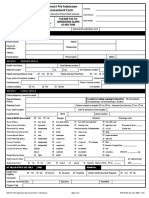
Figure 1. A suggested algorithm for using home sleep testing (HST) in adult patients suspected of having
obstructive sleep apnea (OSA). Note that HST should not be used in pediatric patients. *Significant comorbid
medical disorders include conditions such as moderate to severe pulmonary disease, neuromuscular disease, and
congestive heart failure which may degrade the accuracy of the home sleep test. Patients who have low baseline
oxygen saturation or are on supplemental oxygen are also poor candidates for a home sleep test. Note that
hypertension and diabetes mellitus are not contraindications for obtaining a home sleep test. See manuscript text
for discussion on decision making in obese patients. †Comorbid sleep disorders include conditions such as
central sleep apnea, periodic limb movement disorder, insomnia, parasomnias, circadian rhythm disorders,
narcolepsy, and REM sleep behavior disorder. Central sleep apnea is often seen in patients with heart failure and
those on narcotic medications. ‡Causes of hypoventilation include neuromuscular disease, restrictive lung
disease, and use of narcotic medications. Patients with an elevated body mass index are also at risk for
hypoventilation. PSG, polysomnography. (Adapted with permission from Collop et al.26)
Patient suspected to have OSA
Yes
Pediatric patient Yes
No
Patient has high pretest probability for
No
moderate to severe OSA
Yes
Patient has significant comorbid
Yes
medical disorder*
No
Patient has comorbid sleep disorder† Yes
Perform in-laboratory PSG
Patient is suspected to have nocturnal
seizures, hypoventilation‡ , nocturnal Yes
arrhythmias
No
Patient is on opiates Yes
No
Perform HST
HST positive for OSA No
Yes
HST shows prolonged sustained
hypoxemia, central apneas, or mixed Yes
apneas
No
Treat
doi: 10.3122/jabfm.2015.04.140266 Home Sleep Tests for OSA 507
When faced with a patient suspected of having 8. Storgaard H, Mortensen B, Almdal T, Laub M,
OSA, a primary care provider may choose either to Tarnow L. At least one in three people with Type 2
diabetes mellitus referred to a diabetes centre has
refer their patient to a board-certified sleep special-
symptomatic obstructive sleep apnoea. Diabet Med
ist for further evaluation or to directly order a 2014;31:1460 –7.
HST. When electing to do the latter, the primary 9. Lopez PP, Stefan B, Schulman CI, Byers PM. Prev-
care provider should be aware of the type of device alence of sleep apnea in morbidly obese patients who
being used, along with its sensitivity and specificity presented for weight loss surgery evaluation: more
in different populations. The presence of pro- evidence for routine screening for obstructive sleep
longed sustained hypoxemia, central apneas, mixed apnea before weight loss surgery. Am Surg 2008;74:
834 – 8.
apneas, or a negative HST are indications for re-
10. Netzer NC, Hoegel JJ, Loube D, et al. Prevalence of
ferring a patient for PSG. Other things to keep in symptoms and risk of sleep apnea in primary care.
mind are that at least 300 minutes of recording time Chest 2003;124:1406 –14.
are needed during a HST for accurate diagnosis of 11. Monahan K, Redline S. Role of obstructive sleep
OSA and its severity,38 and that manual scoring is apnea in cardiovascular disease. Curr Opin Cardiol
superior to automatic scoring.39 – 42 A suggested algo- 2011;26:541–7.
rithm for using the HST is shown in Figure 1. 12. Eiseman NA, Westover MB, Ellenbogen JM, Bian-
The HST is an important tool if used and in- chi MT. The impact of body posture and sleep stages
on sleep apnea severity in adults. J Clin Sleep Med
terpreted in the right manner in the right popula-
2012;8:655– 66A.
tion. A patient’s symptoms and examination must
13. Shah P, Gurubhagavatula I. Portable monitoring:
be kept in mind when determining the appropri- practical aspects and case examples. Sleep Med Clin
ateness for ordering a HST, which has the potential 2011;6:355– 66.
to save money, is easy to perform, improves access 14. Flemons WW, Douglas NJ, Kuna ST, Rodenstein
to sleep testing, and can be done in the patient’s DO, Wheatley J. Access to diagnosis and treatment
home. It must be remembered, however, that a of patients with suspected sleep apnea. Am J Respir
Crit Care Med 2004;169:668 –72.
patient suspected of having OSA and a negative
15. Masa Jimenez JF, Barbe Illa F, Capote Gil F, et al.
HST should undergo PSG for further diagnostic
[Resources and delays in the diagnosis of sleep ap-
evaluation.26,28 nea-hypopnea syndrome]. Arch Bronconeumol
2007;43:188 –98.
References 16. El Shayeb M, Topfer LA, Stafinski T, Pawluk L,
1. Punjabi NM. The epidemiology of adult obstructive Menon D. Diagnostic accuracy of level 3 portable
sleep apnea. Proc Am Thorac Soc 2008;5:136 – 43. sleep tests versus level 1 polysomnography for sleep-
2. Gami AS, Pressman G, Caples SM, et al. Association disordered breathing: a systematic review and meta-
of atrial fibrillation and obstructive sleep apnea. Cir- analysis. CMAJ 2014;186:E25–51.
culation 2004;110:364 –7. 17. Rosen CL, Auckley D, Benca R, et al. A multisite
3. Patel D, Mohanty P, Di Biase L, et al. Safety and randomized trial of portable sleep studies and posi-
efficacy of pulmonary vein antral isolation in patients tive airway pressure autotitration versus laboratory-
with obstructive sleep apnea: the impact of continu- based polysomnography for the diagnosis and treat-
ous positive airway pressure. Circ Arrhythm Electro- ment of obstructive sleep apnea: the HomePAP
physiol 2010;3:445–51. study. Sleep 2012;35:757– 67.
4. Javaheri S. Sleep disorders in systolic heart failure: a 18. Mulgrew AT, Fox N, Ayas NT, Ryan CF. Diagnosis
prospective study of 100 male patients. The final and initial management of obstructive sleep apnea
report. Int J Cardiol 2006;106:21– 8. without polysomnography: a randomized validation
5. Yumino D, Wang H, Floras JS, et al. Prevalence and study. Ann Intern Med 2007;146:157– 66.
physiological predictors of sleep apnea in patients 19. Ghegan MD, Angelos PC, Stonebraker AC, Gil-
with heart failure and systolic dysfunction. J Card lespie MB. Laboratory versus portable sleep studies:
Fail 2009;15:279 – 85. a meta-analysis. Laryngoscope 2006;116:859 – 64.
6. Florczak E, Prejbisz A, Szwench-Pietrasz E, et al. 20. Kuna ST, Gurubhagavatula I, Maislin G, et al. Non-
Clinical characteristics of patients with resistant hy- inferiority of functional outcome in ambulatory
pertension: the RESIST-POL study. J Hum Hyper- management of obstructive sleep apnea. Am J Respir
tens 2013;27:678 – 85. Crit Care Med 2011;183:1238 – 44.
7. Manin G, Pons A, Baltzinger P, et al. Obstructive 21. Berry RB, Hill G, Thompson L, McLaurin V. Por-
sleep apnoea in people with Type 1 diabetes: preva- table monitoring and autotitration versus polysom-
lence and association with micro- and macrovascular nography for the diagnosis and treatment of sleep
complications. Diabet Med 2014;32:90 – 6. apnea. Sleep 2008;31:1423–31.
508 JABFM July–August 2015 Vol. 28 No. 4 http://www.jabfm.org
22. Garg N, Rolle AJ, Lee TA, Prasad B. Home-based 32. Berry RB. Uses and limitations of portable monitor-
diagnosis of obstructive sleep apnea in an urban ing for diagnosis and management of obstructive
population. J Clin Sleep Med 2014;10:879 – 85. sleep apnea. Sleep Med Clin 2011;6:309 –33.
23. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for 33. Hesselbacher S, Mattewal A, Hirshkowitz M,
scoring respiratory events in sleep: update of the Sharafkhaneh A. Classification, technical specifica-
2007 AASM Manual for the Scoring of Sleep and tions, and types of home sleep testing devices for
sleep-disordered breathing. Sleep Med Clin 2011;6:
Associated Events. Deliberations of the Sleep Apnea
261– 82.
Definitions Task Force of the American Academy of
Sleep Medicine. J Clin Sleep Med 2012;8:597– 619. 34. Yuceege M, Firat H, Demir A, Ardic S. Reliability of
the Watch-PAT 200 in detecting sleep apnea in
24. Tan HL, Gozal D, Ramirez HM, Bandla HP, Khei- highway bus drivers. J Clin Sleep Med 2013;9:339 –
randish-Gozal L. Overnight polysomnography ver- 44.
sus respiratory polygraphy in the diagnosis of pedi-
35. Pittman SD, Pillar G, Berry RB, Malhotra A, Mac-
atric obstructive sleep apnea. Sleep 2014;37:255– 60. Donald MM, White DP. Follow-up assessment of
25. Guilleminault C, Hagen CC, Huynh NT. Compar- CPAP efficacy in patients with obstructive sleep ap-
ison of hypopnea definitions in lean patients with nea using an ambulatory device based on peripheral
known obstructive sleep apnea hypopnea syndrome arterial tonometry. Sleep Breath 2006;10:123–31.
(OSAHS). Sleep Breath 2009;13:341–7. 36. Yalamanchali S, Farajian V, Hamilton C, Pott TR,
26. Collop NA, Anderson WM, Boehlecke B, et al. Clin- Samuelson CG, Friedman M. Diagnosis of obstruc-
tive sleep apnea by peripheral arterial tonometry:
ical guidelines for the use of unattended portable
meta-analysis. JAMA Otolaryngol Head Neck Surg
monitors in the diagnosis of obstructive sleep apnea
2013;139:1343–50.
in adult patients. Portable Monitoring Task Force of
the American Academy of Sleep Medicine. J Clin 37. Hedner J, White DP, Malhotra A, et al. Sleep stag-
Sleep Med 2007;3:737– 47. ing based on autonomic signals: a multi-center vali-
dation study. J Clin Sleep Med 2011;7:301– 6.
27. Collop N. Home sleep testing: appropriate screen-
38. Wittine LM, Olson EJ, Morgenthaler TI. Effect of
ing is the key. Sleep 2012;35:1445– 6. recording duration on the diagnostic accuracy of
28. Nerfeldt P, Aoki F, Friberg D. Polygraphy vs. poly- out-of-center sleep testing for obstructive sleep ap-
somnography: missing osas in symptomatic snor- nea. Sleep 2014;37:969 –75.
ers–a reminder for clinicians. Sleep Breath 2014;18: 39. Masa JF, Corral J, Pereira R, et al. Effectiveness of
297–303. sequential automatic-manual home respiratory
29. Mokhlesi B, Tulaimat A, Faibussowitsch I, Wang Y, polygraphy scoring. Eur Respir J 2013;41:879 – 87.
Evans AT. Obesity hypoventilation syndrome: prev- 40. Aurora RN, Swartz R, Punjabi NM. Misclassifica-
alence and predictors in patients with obstructive tion of obstructive sleep apnea severity with auto-
sleep apnea. Sleep Breath 2007;11:117–24. mated scoring of home sleep recordings. Chest 2014;
147:719 –27.
30. Laaban JP, Chailleux E. Daytime hypercapnia in
41. Park DY, Kim HJ, Kim CH, et al. Reliability and
adult patients with obstructive sleep apnea syndrome
validity testing of automated scoring in obstructive
in France, before initiating nocturnal nasal continu-
sleep apnea diagnosis with the Embletta X100. La-
ous positive airway pressure therapy. Chest 2005; ryngoscope 2015;125:493–7.
127:710 –5.
42. Nigro CA, Dibur E, Aimaretti S, Gonzalez S, Rho-
31. Resta O, Foschino-Barbaro MP, Bonfitto P, et al. dius E. Comparison of the automatic analysis versus
Prevalence and mechanisms of diurnal hypercapnia the manual scoring from ApneaLink device for the
in a sample of morbidly obese subjects with obstruc- diagnosis of obstructive sleep apnoea syndrome.
tive sleep apnoea. Respir Med 2000;94:240 – 6. Sleep Breath 2011;15:679 – 86.
doi: 10.3122/jabfm.2015.04.140266 Home Sleep Tests for OSA 509
You might also like
- ACS Surgery - Principles and Practice (PDFDrive) PDFDocument2,184 pagesACS Surgery - Principles and Practice (PDFDrive) PDFMandela Kibiriti100% (3)
- Mapeh Least Learned Competencies 6Document5 pagesMapeh Least Learned Competencies 6Anonymous QnNICuArTx75% (12)
- Cigna Medical Coverage Policy For Sleep Testing ServicesDocument29 pagesCigna Medical Coverage Policy For Sleep Testing ServicesPhạm Văn HiệpNo ratings yet
- Prov Prot 20118Document17 pagesProv Prot 20118IlhamNo ratings yet
- Estimation of The Apnea-Hypopnea Index in A Heterogeneous Sleep-Disordered Population Using Optimised Cardiovascular FeaturesDocument16 pagesEstimation of The Apnea-Hypopnea Index in A Heterogeneous Sleep-Disordered Population Using Optimised Cardiovascular FeaturesChuyên Mai TấtNo ratings yet
- (E) 2016 VERBRAECKEN Diagnostic Techniques TEXTDocument4 pages(E) 2016 VERBRAECKEN Diagnostic Techniques TEXTJPNo ratings yet
- Sleep Studies For Sleep-Related Breathing Disorders: ConsensusDocument9 pagesSleep Studies For Sleep-Related Breathing Disorders: Consensusoutro yoongiNo ratings yet
- Sleep Study InterpretationDocument4 pagesSleep Study InterpretationgreenNo ratings yet
- JCSM 14 9 1495Document7 pagesJCSM 14 9 1495Bagus Tri WahyudiNo ratings yet
- JcsmJC1900562 W22pod AnsweredDocument13 pagesJcsmJC1900562 W22pod Answeredlion5835No ratings yet
- Updates On Definition, Consequences, and Management of Obstructive Sleep ApneaDocument7 pagesUpdates On Definition, Consequences, and Management of Obstructive Sleep ApneapvillagranNo ratings yet
- Poly Som No GramDocument65 pagesPoly Som No Gramameer abdullahNo ratings yet
- Khan Doker Scoring Tit BDocument11 pagesKhan Doker Scoring Tit BbengheniaNo ratings yet
- PolysomnographyDocument65 pagesPolysomnographyRickamhaey FebreraNo ratings yet
- Clinical Assessment of SleepinessDocument8 pagesClinical Assessment of SleepinessYusmiatiNo ratings yet
- PolysomnographyDocument4 pagesPolysomnographySaba RiazNo ratings yet
- Polysomnography - Wikipedia, The Free EncyclopediaDocument7 pagesPolysomnography - Wikipedia, The Free EncyclopediaPrashant KumarNo ratings yet
- Automated Screening For Sleep Apnoea in The Home Environment v0Document15 pagesAutomated Screening For Sleep Apnoea in The Home Environment v0bengheniaNo ratings yet
- Obstructive Sleep Apnea Research PaperDocument7 pagesObstructive Sleep Apnea Research Paperefe8zf19100% (1)
- SleepMonitoring MPDI PDFDocument14 pagesSleepMonitoring MPDI PDFFanny MontesNo ratings yet
- Portable Devices Used For Home Testing in Obstructive Sleep ApneaDocument42 pagesPortable Devices Used For Home Testing in Obstructive Sleep ApneaCalifornia Technology Assessment Forum0% (1)
- Stopbang in AsianDocument6 pagesStopbang in AsianwandapandabebeNo ratings yet
- Interpretation of The PolysomnogramDocument15 pagesInterpretation of The Polysomnogramapi-19500641No ratings yet
- Society of Anesthesia and Sleep Medicine Educational Document: Recommendations For Management of Obstructive Sleep Apnea in The Perioperative PeriodDocument27 pagesSociety of Anesthesia and Sleep Medicine Educational Document: Recommendations For Management of Obstructive Sleep Apnea in The Perioperative PeriodMuhammad SyammNo ratings yet
- Lazazzera Et Al-2021-Detection and Classification of Sleep Apnea and Hypopnea Using PPG and $SpO - 2$Document13 pagesLazazzera Et Al-2021-Detection and Classification of Sleep Apnea and Hypopnea Using PPG and $SpO - 2$Peyman BakhshandeNo ratings yet
- 152 Obstructive Sleep Apnoea and Anaesthesia 1Document6 pages152 Obstructive Sleep Apnoea and Anaesthesia 1Echo WahyudiNo ratings yet
- Punjabi, 2008Document8 pagesPunjabi, 2008a3llamNo ratings yet
- Polisomnografí A Dinamica No Dise.: Club de Revistas Julián David Cáceres O. OtorrinolaringologíaDocument25 pagesPolisomnografí A Dinamica No Dise.: Club de Revistas Julián David Cáceres O. OtorrinolaringologíaDavid CáceresNo ratings yet
- Insomnia and Excessive Daytime Sleepiness in ObstrDocument3 pagesInsomnia and Excessive Daytime Sleepiness in ObstrChatterjee SomanNo ratings yet
- Sleep Disorders Research PaperDocument4 pagesSleep Disorders Research Papergvzexnzh100% (1)
- Sleep Apnea Term PaperDocument8 pagesSleep Apnea Term Paperf1gisofykyt3100% (1)
- Automatic Detection of Respiratory Arrests in OSA Patients Using PPG and Machine Learning TechniquesDocument15 pagesAutomatic Detection of Respiratory Arrests in OSA Patients Using PPG and Machine Learning TechniquesDayana VieiraNo ratings yet
- 2 - Sastow - Et - Al - 2024 - Controversies in Sleep ApneaDocument20 pages2 - Sastow - Et - Al - 2024 - Controversies in Sleep Apneaamalia2_3No ratings yet
- Literature Review Sleep ApnoeaDocument6 pagesLiterature Review Sleep Apnoeaelfgxwwgf100% (1)
- Development of An IoT Based Sleep Apnea MonitoringDocument16 pagesDevelopment of An IoT Based Sleep Apnea Monitoringngocoanh1828No ratings yet
- JCSM 13 3 479Document26 pagesJCSM 13 3 479Fitria ChandraNo ratings yet
- The Prevalence of Obstructive Sleep Apnea in Patients With Difficult-To-Treat AsthmaDocument7 pagesThe Prevalence of Obstructive Sleep Apnea in Patients With Difficult-To-Treat AsthmaBarbara WilhelminNo ratings yet
- Perioperative Management of OSADocument69 pagesPerioperative Management of OSAandynightmare97No ratings yet
- Neurological Assgfhgfhfgessment 1Document8 pagesNeurological Assgfhgfhfgessment 1Husaifah BaliwanNo ratings yet
- Clinical Context: Obesity RiskDocument3 pagesClinical Context: Obesity RiskkaznielsNo ratings yet
- Research Paper On Obstructive Sleep ApneaDocument6 pagesResearch Paper On Obstructive Sleep Apneaafeatoxmo100% (1)
- Obstructive Sleep ApnoeaDocument69 pagesObstructive Sleep ApnoeaPrasanna Datta100% (1)
- Journal of Sleep Research - 2016 - Lucey - Comparison of A Single Channel EEG Sleep Study To PolysomnographyDocument11 pagesJournal of Sleep Research - 2016 - Lucey - Comparison of A Single Channel EEG Sleep Study To PolysomnographyIoana GuțăNo ratings yet
- Obstructive Sleep Apnea and Analgesia - SJH PowerpointDocument29 pagesObstructive Sleep Apnea and Analgesia - SJH PowerpointAbd ZouhierNo ratings yet
- From Pulses To Sleep Stages: Towards Optimized Sleep Classification Using Heart-Rate VariabilityDocument17 pagesFrom Pulses To Sleep Stages: Towards Optimized Sleep Classification Using Heart-Rate Variability葛子骏No ratings yet
- 1 s2.0 S0007091223001915 MainDocument3 pages1 s2.0 S0007091223001915 Mainema moralesNo ratings yet
- Obstructive Sleep Apnoea Syndrome A Systematic Literature ReviewDocument4 pagesObstructive Sleep Apnoea Syndrome A Systematic Literature Reviewc5nah867No ratings yet
- Treating Obstructive Sleep Apnea Improves Essential Hypertension and Quality of LifeDocument8 pagesTreating Obstructive Sleep Apnea Improves Essential Hypertension and Quality of Life'ArifahAhmadNo ratings yet
- Obstructive Sleep Apnea Syndrome: Diagnosis and Management: A B S T R A C TDocument13 pagesObstructive Sleep Apnea Syndrome: Diagnosis and Management: A B S T R A C Tsafwand90No ratings yet
- New Seep Apnea AIDocument15 pagesNew Seep Apnea AIgauravchauNo ratings yet
- A Respiratory Movement Monitoring System Using Fiber-Grating Vision Sensor For Diagnosing Sleep ApDocument8 pagesA Respiratory Movement Monitoring System Using Fiber-Grating Vision Sensor For Diagnosing Sleep ApRamzi AlmohtasibNo ratings yet
- 3389 PDFDocument6 pages3389 PDFvarun sahaniNo ratings yet
- Patient Characteristics Affecting Accurate Detection of Sleep Apnea Using A Bed Sheet-Type Portable MonitorDocument8 pagesPatient Characteristics Affecting Accurate Detection of Sleep Apnea Using A Bed Sheet-Type Portable MonitorNadhifa TrivandariNo ratings yet
- Pats 200709-155mgDocument8 pagesPats 200709-155mgDea MaulidiaNo ratings yet
- Home Set Up Polysomnography in The Assessment of Suspected Obstructive Sleep ApneaDocument7 pagesHome Set Up Polysomnography in The Assessment of Suspected Obstructive Sleep ApneaPhạm Văn HiệpNo ratings yet
- Questions About Sleep StudiesDocument2 pagesQuestions About Sleep Studiessuresh2250No ratings yet
- Botelho 09Document8 pagesBotelho 09moiNo ratings yet
- Evaluation of Pressure Bed Sensor For Automatic SAHS ScreeningDocument9 pagesEvaluation of Pressure Bed Sensor For Automatic SAHS ScreeningJuan José Santana HidalgoNo ratings yet
- Does Using Pressure-Controlled Ventilation To Rest Respiratory Muscles Improve Sleep in ICU PatientsDocument8 pagesDoes Using Pressure-Controlled Ventilation To Rest Respiratory Muscles Improve Sleep in ICU Patientscard breatheNo ratings yet
- Sleep Studies in ChildrenDocument12 pagesSleep Studies in ChildrenJHONATAN MATA ARANDANo ratings yet
- Ehac 349Document3 pagesEhac 349Akhmad HidayatNo ratings yet
- Fast Facts: Excessive Daytime Sleepiness Associated with Obstructive Sleep ApneaFrom EverandFast Facts: Excessive Daytime Sleepiness Associated with Obstructive Sleep ApneaNo ratings yet
- Sapa Where Heaven and Earth Meet - NHÓM 3Document22 pagesSapa Where Heaven and Earth Meet - NHÓM 3Phạm Văn HiệpNo ratings yet
- Unit Name: Unit Location: Program: Nova Scotia Health Authority Inpatient ProfileDocument4 pagesUnit Name: Unit Location: Program: Nova Scotia Health Authority Inpatient ProfilePhạm Văn HiệpNo ratings yet
- SapaDocument1 pageSapaPhạm Văn HiệpNo ratings yet
- Sapa Where Heaven and Earth Meet - NHÓM 3Document22 pagesSapa Where Heaven and Earth Meet - NHÓM 3Phạm Văn HiệpNo ratings yet
- k2 Attachments Danh Gia Thuc Trang Va Giai Phap Nang Cao Chat Luong Ghi Chep Ho So Benh An Cai Tien Cua DD Tai BvagDocument12 pagesk2 Attachments Danh Gia Thuc Trang Va Giai Phap Nang Cao Chat Luong Ghi Chep Ho So Benh An Cai Tien Cua DD Tai BvagPhạm Văn HiệpNo ratings yet
- Tracheostomy in Infants in The Neonatal Intensive Care Unit: Education/Practice GapsDocument14 pagesTracheostomy in Infants in The Neonatal Intensive Care Unit: Education/Practice GapsPhạm Văn HiệpNo ratings yet
- Quy Trinh Cham Soc Dieu Duong Noi KhoaDocument41 pagesQuy Trinh Cham Soc Dieu Duong Noi KhoaPhạm Văn HiệpNo ratings yet
- What Is OtolaryngologyDocument37 pagesWhat Is OtolaryngologyPhạm Văn HiệpNo ratings yet
- Lippert 2014Document5 pagesLippert 2014Phạm Văn HiệpNo ratings yet
- Home Set Up Polysomnography in The Assessment of Suspected Obstructive Sleep ApneaDocument7 pagesHome Set Up Polysomnography in The Assessment of Suspected Obstructive Sleep ApneaPhạm Văn HiệpNo ratings yet
- Polysomnograpy: Charmain Beatriz A. AtosDocument62 pagesPolysomnograpy: Charmain Beatriz A. AtosPhạm Văn HiệpNo ratings yet
- Caffeine Effects On Sleep Taken 0, 3, or 6 Hours Before Going To BedDocument6 pagesCaffeine Effects On Sleep Taken 0, 3, or 6 Hours Before Going To BedPhạm Văn HiệpNo ratings yet
- Polysomnography: Understanding This Technology's Past Might Guide Future DevelopmentsDocument3 pagesPolysomnography: Understanding This Technology's Past Might Guide Future DevelopmentsPhạm Văn HiệpNo ratings yet
- Kota Gal 2012Document16 pagesKota Gal 2012Phạm Văn HiệpNo ratings yet
- Digital Tools in Polysomnography: Rajeev Agarwal and Jean GotmanDocument8 pagesDigital Tools in Polysomnography: Rajeev Agarwal and Jean GotmanPhạm Văn HiệpNo ratings yet
- 498 Republic of Moldova Fact SheetsDocument2 pages498 Republic of Moldova Fact SheetsAlmubashir AlbaeidNo ratings yet
- Diabetic NeuropathyDocument4 pagesDiabetic NeuropathyAsish GeiorgeNo ratings yet
- Effects of Massage and Acupressure On Relieving.10Document9 pagesEffects of Massage and Acupressure On Relieving.10Riska amaliaNo ratings yet
- Jurnal Acute Decompensated Heart FailureDocument4 pagesJurnal Acute Decompensated Heart FailureMayang Sri WulandNo ratings yet
- Lesson 3 - Basic Principles of Physical FitnessDocument20 pagesLesson 3 - Basic Principles of Physical FitnessJohn Michael AgustinNo ratings yet
- Hospital and Clinical Pharmacy CH 1 Hospital Pharmacy NotesDocument12 pagesHospital and Clinical Pharmacy CH 1 Hospital Pharmacy Notesmaharachandana18No ratings yet
- Patient Admission Assessment FormDocument1 pagePatient Admission Assessment Formprasanna_326avanthiNo ratings yet
- Acne Blackheads Pimple Zits MedlinePlusgrzkjxirmtDocument2 pagesAcne Blackheads Pimple Zits MedlinePlusgrzkjxirmtdollarcanvas0No ratings yet
- Indian Nutraceutical IndustryDocument64 pagesIndian Nutraceutical Industryhariom100% (2)
- Architectural Planning 2Document24 pagesArchitectural Planning 2rogelio labiaoNo ratings yet
- TRIAGEDocument55 pagesTRIAGELaveena AswaleNo ratings yet
- Nishtha Annual Report 2014-15Document32 pagesNishtha Annual Report 2014-15Sunny DuggalNo ratings yet
- Contemporary Orthodontics, 5th Ed: Book ReviewDocument1 pageContemporary Orthodontics, 5th Ed: Book ReviewPaula Diaz100% (1)
- Safety Training ProgramDocument43 pagesSafety Training ProgramBhavesh PatelNo ratings yet
- Activity 1 - CPHDocument2 pagesActivity 1 - CPHMA. ANDREA NICOLE DURANNo ratings yet
- Midterm DraftDocument32 pagesMidterm DraftUn knownnnNo ratings yet
- AUS - Boardreviewer (Test Your Knowledge)Document177 pagesAUS - Boardreviewer (Test Your Knowledge)Yusra FaisalNo ratings yet
- Evolution of Bhramari Pranayam in The Management of Menopausal SyndromeDocument7 pagesEvolution of Bhramari Pranayam in The Management of Menopausal SyndromeDr Kirti BhatiNo ratings yet
- Health Infrastructure and Economic Development in IndiaDocument9 pagesHealth Infrastructure and Economic Development in IndiaAkanksha PalNo ratings yet
- Photo TherapyDocument7 pagesPhoto TherapyMaysa Ismail100% (1)
- SHE List DocumentDocument1 pageSHE List DocumentMunajamNo ratings yet
- COMMISSION ON HIGHER EDUCATION (CHED) Medtech Laws PHDocument2 pagesCOMMISSION ON HIGHER EDUCATION (CHED) Medtech Laws PHJohn Michael CastroNo ratings yet
- Capinpin Research PaperDocument16 pagesCapinpin Research Paperfrancine.malit24No ratings yet
- EDU501Document7 pagesEDU501PatriciaSugpatanNo ratings yet
- CASR Part 67 Ed. 1 Amdt 0 - Medical Standard and CertificationDocument43 pagesCASR Part 67 Ed. 1 Amdt 0 - Medical Standard and CertificationR SetiawanNo ratings yet
- 08 OHS Journal Aug 2012Document60 pages08 OHS Journal Aug 2012NazirAhmadBashiriNo ratings yet
- Acute ColitisDocument8 pagesAcute ColitisKhurram NadeemNo ratings yet
- Treatment of Endometriosis in Women Desiring FertilityDocument23 pagesTreatment of Endometriosis in Women Desiring FertilityVaisnavi Muthoovaloo67% (3)