Professional Documents
Culture Documents
Varicella, Meningitis and DHF
Varicella, Meningitis and DHF
Uploaded by
debayn0 ratings0% found this document useful (0 votes)
16 views7 pagesVaricella zoster virus causes chickenpox in children and shingles in adults. It can cause serious complications like encephalitis or pneumonia with chickenpox, and post herpetic neuralgia with shingles. A live attenuated vaccine is available to protect against chickenpox and reduce the risk of shingles. The virus spreads through respiratory droplets or direct contact with skin lesions, causing a characteristic rash that progresses from papules to vesicles to crusts over the course of a week.
Original Description:
Original Title
Varicella, Meningitis and Dhf
Copyright
© © All Rights Reserved
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentVaricella zoster virus causes chickenpox in children and shingles in adults. It can cause serious complications like encephalitis or pneumonia with chickenpox, and post herpetic neuralgia with shingles. A live attenuated vaccine is available to protect against chickenpox and reduce the risk of shingles. The virus spreads through respiratory droplets or direct contact with skin lesions, causing a characteristic rash that progresses from papules to vesicles to crusts over the course of a week.
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
Download as doc, pdf, or txt
0 ratings0% found this document useful (0 votes)
16 views7 pagesVaricella, Meningitis and DHF
Varicella, Meningitis and DHF
Uploaded by
debaynVaricella zoster virus causes chickenpox in children and shingles in adults. It can cause serious complications like encephalitis or pneumonia with chickenpox, and post herpetic neuralgia with shingles. A live attenuated vaccine is available to protect against chickenpox and reduce the risk of shingles. The virus spreads through respiratory droplets or direct contact with skin lesions, causing a characteristic rash that progresses from papules to vesicles to crusts over the course of a week.
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
Download as doc, pdf, or txt
You are on page 1of 7
VARICELLA ZOSTER VIRUS is one of eight herpes viruses known to shingles in adults, until the vaccination was given
he vaccination was given to the entire population—
infect humans (and other vertebrates). It commonly causes chicken-pox in because adults who have had chickenpox as a child are less likely to have
children and both shingles and post herpetic neuralgia in adults. shingles in later life if they have been exposed occasionally to the
chickenpox virus (for example by their children). This is because the
• Nomenclature exposure acts as a booster vaccine.
Varicella zoster virus is known by many names, including: chickenpox virus,
Varicella virus, zoster virus, and human herpes virus type 3 (HHV-3). • Chickenpox
Chickenpox is a highly contagious illness caused by primary infection with
• Human disease Varicella zoster virus (VZV). It generally begins with conjunctival and
Primary VZV infection results in chickenpox (Varicella), which may rarely catarrhal symptoms and then characteristic spots appearing in two or three
result in complications including encephalitis or pneumonia. Even when waves, mainly on the body and head rather than the hands and becoming
clinical symptoms of chickenpox have resolved, VZV remains dormant in the itchy raw pockmarks, small open sores which heal mostly without scarring.
nervous system of the infected person (REDIRECT virus latency), in the Chickenpox has a 10-21 day incubation period and is spread easily through
trigeminal and dorsal root ganglia. In about 10-20% of cases, VZV aerosolized droplets from the nasopharynx of ill individuals or through direct
reactivates later in life producing a disease known as herpes zoster or contact with secretions from the rash. Following primary infection there is
shingles. Serious complications of shingles include post herpetic neuralgia, usually lifelong protective immunity from further episodes of chickenpox.
zoster multiplex, myelitis, herpes ophthalmicus, or zoster sine herpete. Chickenpox is rarely fatal, although it is generally more severe in adults than
in children. Pregnant women and those with a suppressed immune system
• Morphology are at highest risk of serious complications. The most common late
VZV is closely related to the herpes simplex viruses (HSV), sharing much
complication of chicken pox is shingles, caused by reactivation of the
genome homology. The known envelope glycoprotein (gB, gC, gE, gH, gI,
Varicella zoster virus decades after the initial episode of chickenpox.
gK, gL) correspond with those in HSV, however there is no equivalent of
HSV gD. VZV also fails to produce the LAT (latency-associated transcripts) • Signs and symptoms
that play an important role in establishing HSV latency (REDIRECT herpes Chickenpox is a highly contagious disease that spreads from person to
simplex virus). VZV virions are spherical and 150-200 nm in diameter. Their person by direct contact or through the air from an infected person's
lipid envelope encloses the nucleocapsid of 162 capsomeres arranged in an coughing or sneezing. Touching the fluid from a chickenpox blister can also
icosahedral form. Its DNA is a single, linear, double-stranded molecule; spread the disease. A person with chickenpox is contagious from one to five
125,000 nt long. The capsid is surrounded by a number of loosely associated days before the rash appears until all blisters have formed scabs. This may
proteins known collectively as the tegument; many of these proteins play take 5-10 days. It takes from 10-20 days after contact with an infected
critical roles in initiating the process of virus reproduction in the infected cell. person for someone to develop chickenpox.
The tegument is in turn covered by a lipid envelope studded with The chicken pox lesions (blisters) start as a two to four millimeter red papule
glycoproteins that are displayed on the exterior of the virion. which develops an irregular outline (a rose petal). A thin-walled, clear vesicle
The virus is very susceptible to disinfectants, notably sodium hypochlorite. (dew drop) develops on top of the area of redness. This "dew drop on a rose
Within the human body it can be treated by a number of drugs and petal" lesion is very characteristic for chickenpox. After about 8 to 12 hours
therapeutic agents including acyclovir, zoster-immune globulin (ZIG), and the fluid in the vesicle gets cloudy and the vesicle breaks leaving a crust.
vidarabine. The fluid is highly contagious, but once the lesion crusts over, it is not
considered contagious. The crust usually falls off after seven days
• Vaccine sometimes leaving a crater-like scar. Although one lesion goes through this
A live attenuated VZV Oka/Merck strain vaccine is available and is marketed
complete cycle in about seven days, another hallmark of chickenpox is the
in the United States under the trade name Varivax. It was developed by
fact that new lesions crop up every day for several days. Therefore it may be
Merck, Sharp & Dohme in the 1980s from the Oka strain virus isolated and
a week before new lesions stop appearing and existing lesions crust over.
attenuated by Michiaki Takahashi and colleagues in the 1970s. It was
Children are not to be sent back to school until all lesions have crusted over.
submitted to the U.S. Food and Drug Administration for approval in 1990 and
Zoster, also known as shingles, is a reactivation of chickenpox and may also
was approved in 1995. Since then, it has been added to the recommended
be a source of the virus for susceptible children and adults. It is not
vaccination schedules for children in Australia, the United States, and many
necessary to have physical contact with the infected person for the disease
other countries. Varicella vaccination has raised concerns in some that the
to spread. Those infected can spread chickenpox before they know they
immunity induced by the vaccine may not be lifelong, possibly leaving adults
have the disease - even before any rash develops. People with chickenpox,
vulnerable to more severe disease as the immunity from their childhood
in fact, can infect others from about two days before the rash develops until
immunization wanes. Vaccine coverage in the United States in the
all the sores have crusted over, usually four or five days after the rash starts.
population recommended for vaccination is approaching 90%, with
concomitant reductions in the incidence of Varicella cases, and • Infection in Pregnancy and Neonates
hospitalizations and deaths due to VZV. So far, clinical data has proved that Varicella infection in pregnant women can lead to viral transmission
the vaccine is effective for over 10 years in preventing Varicella infection in via the placenta and infection of the fetus. If infection occurs during the first
healthy individuals and when breakthrough infections do occur, illness is 28 weeks of gestation, this can lead to fetal Varicella syndrome (also known
typically mild. In 2007, the ACIP recommended a second dose of vaccine as congenital Varicella syndrome). Effects on the fetus can range in severity
before school entry to ensure the maintenance of high levels of Varicella from underdeveloped toes and fingers to severe anal and bladder
immunity. malformation. Possible problems include:
In 2006, the FDA approved Zostavax for the prevention of shingles. Zostavax a. Damage to BRAIN: encephalitis, microcephaly, hydrocephaly, aplasia
is a more concentrated formulation of the Varivax vaccine, designed to elicit of brain
an immune response in older adults whose immunity to VZV wanes with b. Damage to the EYE (optic stalk, optic cap, and lens vesicles):
advancing age. microphthalmia, cataracts, chorioretinitis, optic atrophy
Some countries require the Varicella vaccination or an exemption before c. Other NEUROLOGICAL disorder: damage to cervical and lumbosacral
entering elementary school. Protection is not permanent and further spinal cord, motor/sensory deficits, absent deep tendon reflexes,
vaccination is necessary five years after the initial immunization. anisocoria/Horner's syndrome
In the United Kingdom, Varicella antibodies are measured in women with no d. Damage to BODY: hypoplasia of upper/lower extremities, anal and
history of the disease as part of routine of prenatal care. By 2005 all National bladder sphincter dysfunction
Health Service personnel had determined their immunity and been e. SKIN disorders: (cicatricial) skin lesions, hypopigmentation
immunized if they were non-immune and have direct patient contact. Infection late in gestation or immediately post-partum is referred to as
Population-based immunization against Varicella is not otherwise practiced neonatal Varicella. Maternal infection is associated with premature delivery.
in the UK. It is feared that there would be a greater number of cases of The risk of the baby developing the disease is greatest following exposure to
1
Beckydecena2008
infection in the period 7 days prior to delivery and up to 7 days post-partum.
The neonate may also be exposed to the virus via infectious siblings or other • Prognosis
contacts, but this is of less concern if the mother is immune. Newborns that Chickenpox infection is milder in young children, and symptomatic treatment,
develop symptoms are at a high risk of pneumonia and other serious with a sodium bicarbonate baths or antihistamine medication may ease
complications of the disease. itching. Paracetamol (acetaminophen) is widely used to reduce fever.
Aspirin, or products containing aspirin, must not be given to children with
• Pathophysiology chickenpox (or any fever-causing illness suspected of being of viral origin),
Chickenpox is usually acquired by the inhalation of airborne respiratory as this risks causing the serious and potentially fatal Reye's Syndrome.
droplets from an infected host. The highly contagious nature of VZV explains In adults, the disease can be more severe, though the incidence is much
the epidemics of chickenpox that spread through schools as one child who is less common. Infection in adults is associated with greater morbidity and
infected quickly spreads the virus to many classmates. High viral titers are mortality due to pneumonia, hepatitis and encephalitis. In particular, up to
found in the characteristic vesicles of chickenpox; thus, viral transmission 10% of pregnant women with chickenpox develop pneumonia, the severity of
may also occur through direct contact with these vesicles, although the risk which increases with onset later in gestation. In England and Wales, 75% of
is lower. deaths due to chickenpox are in adults. [4] Inflammation of the brain, or
After initial inhalation of contaminated respiratory droplets, the virus infects encephalitis, can occur in immunocompromised individuals, although the risk
the conjunctivae or the mucosa of the upper respiratory tract. Viral is higher with herpes zoster. Necrotizing fasciitis is also a rare complication.
proliferation occurs in regional lymph nodes of the upper respiratory tract 2-4 Secondary bacterial infection of skin lesions, manifesting as impetigo,
days after initial infection and is followed by primary viremia on postinfection cellulitis, and erysipelas, is the most common complication in healthy
days 4-6. A second round of viral replication occurs in the body's internal children. Disseminated primary Varicella infection, usually seen in the
organs, most notably the liver and the spleen, followed by a secondary immunocompromised or adult populations, may have high morbidity. Ninety
viremia 14-16 days postinfection. This secondary viremia is characterized by percent of cases of Varicella pneumonia occur in the adult population. Rarer
diffuse viral invasion of capillary endothelial cells and the epidermis. VZV complications of disseminated chickenpox also include myocarditis, hepatitis,
infection of cells of the Malpighian layer produces both intercellular and and glomerulonephritis.
intracellular edema, resulting in the characteristic vesicle. Hemorrhagic complications are more common in the immunocompromised
Exposure to VZV in a healthy child initiates the production of host or immunosuppressed populations, although healthy children and adults
immunoglobulin G (IgG), immunoglobulin M (IgM), and immunoglobulin A have been affected. Five major clinical syndromes have been described:
(IgA) antibodies; IgG antibodies persist for life and confer immunity. Cell- febrile purpura, malignant chickenpox with purpura, postinfectious purpura,
mediated immune responses are also important in limiting the scope and the purpura fulminans, and anaphylactoid purpura. These syndromes have
duration of primary Varicella infection. After primary infection, VZV is variable courses, with febrile purpura being the most benign of the
hypothesized to spread from mucosal and epidermal lesions to local sensory syndromes and having an uncomplicated outcome. In contrast, malignant
nerves. VZV then remains latent in the dorsal ganglion cells of the sensory chickenpox with purpura is a grave clinical condition that has a mortality rate
nerves. Reactivation of VZV results in the clinically distinct syndrome of of greater than 70%. The etiology of these hemorrhagic chickenpox
herpes zoster (shingles). syndromes is not known.
• Diagnosis • Epidemiology
The diagnosis of Varicella is primarily clinical. In a non-immunized individual Primary Varicella is an endemic disease. Cases of Varicella are seen
with typical prodromal symptoms associated with the appropriate appearing throughout the year but more commonly in winter and early spring. This is
rash occurring in "crops", no further investigation would normally be unlike enteroviruses and lends some support to the view that, like measles
undertaken. and rubella, Varicella is spread mainly by the respiratory route. In contrast,
If further investigation is undertaken, confirmation of the diagnosis can be herpes zoster occurs sporadically and evenly throughout the year. Varicella
sought through either examination of the fluid within the vesicles, or by is one of the classic diseases of childhood, with the highest prevalence in the
testing blood for evidence of an acute immunologic response. Vesicle fluid 4 - 10 years age group. Like rubella, it is uncommon in preschool children.
can be examined with a Tsanck smear, or better with examination for direct Varicella is highly communicable, with an infection rate of 90% in close
fluorescent antibody. The fluid can also be "cultured", whereby attempts are contacts. Most people become infected before adulthood but 10% of young
made to grow the virus from a fluid sample. Blood tests can be used to adults remain susceptible. However, this pattern of infection is not universal,
identify a response to acute infection (IgM) or previous infection and e.g. in rural India, Varicella is predominantly a disease of adults, with the
subsequent immunity (IgE). mean age of infection 23.4 years. It has been suggested that this could be
Prenatal diagnosis of fetal Varicella infection can be performed using due to interference by other respiratory viruses that children are exposed to.
ultrasound, though a delay of 5 weeks following primary maternal infection is Historically, Varicella has been a disease predominantly affecting preschool
advised. A PCR (DNA) test of the mother's amniotic fluid can also be and school-aged children. In adults the pock marks are darker and the scars
performed, though the risk of spontaneous abortion due to the amniocentesis more prominent than in children.
procedure is higher than the risk of the baby developing fetal Varicella
syndrome. • History
One history of medicine book credits Giovanni Filippo (1510–1580) of
• Treatment Palermo with the first description of Varicella (chickenpox). Subsequently in
There is no evidence to support the effectiveness of topical application of the 1600s, an English physician named Richard Morton described what he
calamine lotion, a topical barrier preparation containing zinc oxide in spite of thought a mild form of smallpox as "chicken pox." Later, in 1767, a physician
its wide usage and excellent safety profile. [9] It is important to maintain good named William Heberden, also from England, was the first physician to
hygiene and daily cleaning of skin with warm water to avoid secondary clearly demonstrate that chickenpox was different from smallpox. However, it
bacterial infection. is believed the name chickenpox was commonly used in earlier centuries
If exposure to Varicella in certain 'at risk' populations is confirmed before doctors identified the disease.
(immunosuppressed individuals, pregnant seronegative women, neonates), There are many explanations offered for the origin of the name chickenpox:
anti-Varicella zoster immunoglobulin may be given prior to onset of disease Samuel Johnson suggested that the disease was "less dangerous", thus a
symptoms. "chicken" version of the pox; the specks that appear looked as though the
Infection in otherwise healthy adults tends to be more severe and active; skin was pecked by chickens; the disease was named after chick peas, from
treatment with antiviral drugs (e.g. acyclovir) is generally advised. Patients of a supposed similarity in size of the seed to the lesions; the term reflects a
any age with depressed immune systems or extensive eczema are at risk of corruption of the Old English word giccin, which meant itching.
more severe disease and should also be treated with antiviral medication. In As "pox" also means curse, in medieval times some believed it was a plague
the U.S., 55 percent of chickenpox deaths are in the over-20 age group, brought on to curse children by the use of black magic.
even though they are a tiny fraction of the cases.
2
Beckydecena2008
From ancient times, neem has been used by Indians to alleviate the external During the lumbar puncture procedure, the opening pressure is measured. A
symptoms of itching and to minimize scarring. Neem baths (neem leaves and pressure of over 180 mm H2O is indicative of bacterial meningitis.
a dash of turmeric powder in water) are commonly given for the duration. The cerebrospinal fluid (CSF) sample is examined for white blood cells (and
Neem branches are hung at the entrance of households to announce that which subtypes), red blood cells, protein content and glucose level. Gram
illness to visitors. Neem branches are kept handy by the affected person to staining of the sample may demonstrate bacteria in bacterial meningitis, but
gently brush the skin, to soothe the itching sensation. absence of bacteria does not exclude bacterial meningitis; microbiological
During the medieval era, oatmeal was discovered to soothe the sores, and culture of the sample may still yield a causative organism. The type of white
oatmeal baths are today still commonly given to relieve itching. blood cell predominantly present predicts whether meningitis is due to
bacterial or viral infection. Other tests performed on the CSF sample include
MENINGITIS is the inflammation of the protective membranes covering latex agglutination test, limulus lysates, or polymerase chain reaction (PCR)
the brain and spinal cord, known collectively as the meninges. Meningitis for bacterial or viral DNA. If the patient is immunocompromised, testing the
may develop in response to a number of causes, usually bacteria, viruses CSF for toxoplasmosis, Epstein-Barr virus, cytomegalovirus, JC virus and
and other pathogens, but also physical injury, cancer or certain drugs. While fungal infection may be performed.
some forms of meningitis are mild and resolve on their own, meningitis is a Cultures are often negative if CSF is taken after the administration of
potentially life-threatening condition due to the proximity of the inflammation antibiotics. In these patients, PCR can be helpful in arriving at a diagnosis. It
to the brain and spinal cord. The potential for serious neurological damage or has been suggested that CSF cortisol measurement may be helpful.
even death necessitates prompt medical attention and evaluation. Infectious Aseptic meningitis refers to non-bacterial causes of meningitis and includes
meningitis, the most common form, is typically treated with antibiotics and infective etiologies such as viruses and fungi, neoplastic etiologies such as
requires close observation. Some forms of meningitis (such as those carcinomatous and lymphomatous meningitis, inflammatory causes such as
associated with meningococcus, mumps virus or pneumococcus infections) sarcoidosis (neurosarcoidosis)) and chemical causes such as meningitis
may be prevented with immunization. secondary to the intrathecal introduction of contrast media.
Although the term "viral meningitis" is often used in any patient with a mild
• Signs and symptoms meningeal illness with appropriate CSF findings, certain patients will present
Severe headache is the most common symptom of meningitis (87 percent) with clinical and CSF features of viral meningitis, yet ultimately is diagnosed
followed by nuchal rigidity ("neck stiffness", found in 83%). The classic triad with one of the other conditions categorized as "aseptic meningitis". This
of diagnostic signs consists of nuchal rigidity (being unable to flex the neck may be prevented by performing polymerase chain reaction or serology on
forward), sudden high fever and altered mental status. All three features are CSF or blood for common viral causes of meningitis (enterovirus, herpes
present in only 44% of all cases of infectious meningitis. Other signs simplex virus 2 and mumps in those not vaccinated for this).
commonly associated with meningitis are photophobia (inability to tolerate A related diagnostic and therapeutic conundrum is the "partially treated
bright light), phonophobia (inability to tolerate loud noises), irritability and meningitis", i.e. meningitis symptoms in patients who have already been
delirium (in small children) and seizures (in 20-40% of cases). In infants (0-6 receiving antibiotics (such as for presumptive sinusitis). In these patients,
months), swelling of the fontanel (soft spot) may be present. CSF findings may resemble those of viral meningitis, but antibiotic treatment
Nuchal rigidity is typically assessed with the patient lying supine, and both may need to be continued until there is definitive positive evidence of a viral
hips and knees flexed. If pain is elicited when the knees are passively cause (e.g. a positive enterovirus PCR).
extended (Kernig's sign), this indicates nuchal rigidity and meningitis. In
infants, forward flexion of the neck may cause involuntary knee and hip • Prediction rules
flexion (Brudzinski's sign). Although commonly tested, the sensitivity and The Bacterial Meningitis Score predicts reliably whether a child (older than
specificity of Kernig's and Brudzinski's tests are uncertain. two months) may have infectious meningitis. In children with at least 1 risk
In "meningococcal" meningitis (i.e. meningitis caused by the bacteria factor (positive CSF Gram stain, CSF absolute Neutrophil count ≥ 1000
Neisseria meningitidis), a rapidly-spreading petechial rash is typical, and cell/µL, CSF protein ≥ 80 mg/dL, peripheral blood absolute Neutrophil count
may precede other symptoms. The rash consists of numerous small, ≥ 10,000 cell/µL, history of seizure before or at presentation time) it had a
irregular purple or red spots on the trunk, lower extremities, mucous sensitivity of 100%, specificity of 63.5%, and negative predictive value of
membranes, conjunctiva, and occasionally on the palms of hands and soles 100%.
of feet. Other clues to the nature of the cause may be the skin signs of hand, • Causes
foot and mouth disease and genital herpes, both of which may be associated
Most cases of meningitis are caused by microorganisms, such as viruses,
with viral meningitis.
bacteria, fungi, or parasites, that spread into the blood and into the
Meningitis can be diagnosed after death has occurred. The findings from a
cerebrospinal fluid (CSF).[9] Non-infectious causes include cancers, systemic
post mortem are usually a diffuse (widespread) inflammation of the pia-
lupus erythematosus and certain drugs. The most common cause of
arachnoid area. Neutrophil leucocytes tend to have migrated to the
meningitis is viral, and often runs its course within a few days. Bacterial
cerebrospinal fluid and the base of the brain, along with cranial nerves and
meningitis is the second most frequent type and can be serious and life-
the spinal cord, may be surrounded with pus—as may the meningeal
threatening. Numerous microorganisms may cause bacterial meningitis, but
vessels.
Neisseria meningitidis ("meningococcus") and Streptococcus pneumoniae
• Diagnosis/Investigations ("pneumococcus") are the most common pathogens in patients without
Investigations include blood tests (electrolytes, liver and kidney function, immune deficiency, with meningococcal disease being more common in
inflammatory markers and a complete blood count) and usually X-ray children. Staphylococcus aureus may complicate neurosurgical operations,
examination of the chest. The most important test in identifying or ruling out and Listeria monocytogenes is associated with poor nutritional state and
meningitis is analysis of the cerebrospinal fluid (fluid that envelops the brain alcoholism. Haemophilus influenzae (type B) incidence has been much
and the spinal cord) through lumbar puncture (LP). However, if the patient is reduced by immunization in many countries. Mycobacterium tuberculosis
at risk for a cerebral mass lesion or elevated intracranial pressure (recent (the causative agent of tuberculosis) rarely causes meningitis in Western
head injury, a known immune system problem, localizing neurological signs, countries but is common and feared in countries where tuberculosis is
or evidence on examination of a raised ICP), a lumbar puncture may be endemic.
contraindicated because of the possibility of fatal brain herniation. In such • Treatment
cases a CT or MRI scan is generally performed prior to the lumbar puncture
to exclude this possibility. Otherwise, the CT or MRI should be performed
a. Initial treatment
Meningitis is a life-threatening condition and treatment should not be delayed
after the LP, with MRI preferred over CT due to its superiority in
for confirmation if suspected. If a physician is present on scene then
demonstrating areas of cerebral edema, ischemia, and meningeal
treatment should begin immediately with benzylpenicillin. High-flow oxygen
inflammation.
should be administered as soon as possible, along with an intravenous fluids
if hypotensive or in shock.
3
Beckydecena2008
b. Bacterial meningitis Unlike bacteria, viruses cannot be killed by antibiotics. Drugs such as
Bacterial meningitis is a medical emergency and has a high mortality rate if acyclovir may be employed if herpes virus infection is either suspected or
untreated. All suspected cases, however mild, need emergency medical demonstrated.
attention. Empiric antibiotics must be started immediately, even before the d. Fungal meningitis
results of the lumbar puncture and CSF analysis are known. Antibiotics This form of meningitis is rare in otherwise healthy people but is a higher risk
started within 4 hours of lumbar puncture will not significantly affect lab in those who have AIDS, other forms of immunodeficiency (an immune
results. Adjuvant treatment with corticosteroids reduces rates of mortality, system that does not respond adequately to infections) and
severe hearing loss and neurological sequelae in adults, specifically when immunosuppression (immune system malfunction as a result of medical
the causative agent is Pneumococcus. treatment). In AIDS, Cryptococcus neoformans is the most common cause of
Age group Causes fungal meningitis; it requires Indian ink staining of the CSF sample for
Group B Streptococci, Escherichia coli, Listeria identification of this capsulated yeast. Fungal meningitis is treated with long
Neonates courses of highly dosed antifungal.
monocytogenes
Neisseria meningitidis, Haemophilus influenzae, Streptococcus • Complications
Infants
pneumoniae In children there are several potential disabilities which result from damage
Children N. meningitidis, S. pneumoniae to the nervous system. These include sensorineural hearing loss, epilepsy,
Adults S. pneumoniae, N. meningitidis, Mycobacteria, Cryptococci diffuse brain swelling, hydrocephalus, cerebral vein thrombosis, intra
The choice of antibiotic depends on local advice. In most of the developed cerebral bleeding and cerebral palsy. Acute neurological complications may
world, the most common organisms involved are Streptococcus pneumoniae lead to adverse consequences. In childhood acute bacterial meningitis
and Neisseria meningitidis: first line treatment in the UK is a third-generation deafness is the most common serious complication. Sensorineural hearing
cephalosporin (such as ceftriaxone or cefotaxime). In those under 3 years of loss often develops during first few days of the illness as a result of inner ear
age, over 50 years of age, or immunocompromised, ampicillin should be dysfunction, but permanent deafness is rare and can be prevented by
added to cover Listeria monocytogenes. In the U.S. and other countries with prompt treatment of meningitis.
high levels of penicillin resistance, the first line choice of antibiotics is Those that contract the disease during the neonatal period and those
vancomycin and a carbapenem (such as meropenem). In sub-Saharan infected by S. pneumoniae and gram negative bacilli are at greater risk of
Africa, oily chloramphenicol or ceftriaxone are often used because only a developing neurological, auditory, or intellectual impairments or functionally
single dose is needed in most cases. important behavior or learning disorders which can manifest as poor school
Staphylococci and gram-negative bacilli are common infective agents in performance.
patients who have just had a neurosurgical procedure. Again, the choice of In adults central nervous system complications include brain infarction, brain
antibiotic depends on local patterns of infection: cefotaxime and ceftriaxone swelling, hydrocephalus, intracerebral bleeding; systemic complications are
remain good choices in many situations, but ceftazidime is used when dominated by septic shock, adult respiratory distress syndrome and
Pseudomonas aeruginosa is a problem, and intraventricular vancomycin is disseminated intravascular coagulation. Those who have underlying
used for those patients with intraventricular shunts because of high rates of predisposing conditions e.g. head injury may develop recurrent meningitis. [18]
staphylococcal infection. In patients with intracerebral prosthetic material Case-fatality ratio is highest for gram-negative etiology and lowest for
(metal plates, electrodes or implants, etc.) then sometimes chloramphenicol meningitis caused by H. influenzae (also a gram negative bacillus). Fatal
is the only antibiotic that will adequately cover infection by Staphylococcus outcome in patients over 60 years of age is more likely to be from systemic
aureus (cephalosporins and carbapenems are inadequate under these complications e.g. pneumonia, sepsis, cardio-respiratory failure; however in
circumstances). younger individuals it is usually associated with neurological complications.
Once the results of the CSF analysis are known along with the Gram-stain Age more than 60, low Glasgow coma scale at presentation and seizure
and culture, empiric therapy may be switched to therapy targeted to the within 24 hours increase the risk of death among community acquired
specific causative organism and its sensitivities. meningitis.
Neisseria meningitidis (Meningococcus) can usually be treated with a 7-day
course of IV antibiotics: • Prevention
- Penicillin-sensitive -- PENICILLIN G or AMPICILLIN a. Immunization
- Penicillin-resistant -- CEFTRIAXONE or CEFOTAXIME Vaccinations against Haemophilus influenzae (Hib) have decreased early
- Prophylaxis for close contacts (contact with oral secretions) -- RIFAMPIN childhood meningitis significantly.
600 mg bid for 2 days (adults) or 10 mg/kg bid (children). Rifampin is not Vaccines against type A and C Neisseria meningitidis, the kind that causes
recommended in pregnancy and as such, these patients should be most disease in preschool children and teenagers in the United States, have
treated with single doses of CIPROFLOXACIN, AZITHROMYCIN or also been around for a while. Type A is also prevalent in sub-Sahara Africa
CEFTRIAXONE and W135 outbreaks have affected those on the Hajj pilgrimage to Mecca.
Streptococcus pneumoniae (Pneumococcus) can usually be treated with a 2- Immunization with the ACW135Y vaccine against four strains is now a visa
week course of IV antibiotics: requirement for taking part in the Hajj.
- Penicillin-sensitive -- PENICILLIN G Vaccines against type B Neisseria meningitidis are much harder to produce,
- Penicillin-intermediate -- CEFTRIAXONE OR CEFOTAXIME as its capsule is very weakly immunogenic masking its antigenic proteins.
- Penicillin-resistant -- CEFTRIAXONE or CEFOTAXIME + VANCOMYCIN There is also a risk of autoimmune response, and the porA and porB
Listeria monocytogenes is treated with a 3-week course of IV AMPICILLIN + proteins on Type B resemble neuronal molecules. A vaccine called MeNZB
GENTAMICIN. for a specific strain of type B Neisseria meningitidis prevalent in New
Gram negative bacilli -- CEFTRIAXONE or CEFOTAXIME Zealand has completed trials and is being given to many people in the
Pseudomonas aeruginosa -- CEFTAZIDIME country under the age of 20 free of charge. There is also a vaccine,
Staphylococcus aureus MenBVac, for the specific strain of type B meningococcal disease prevalent
- Methicillin-sensitive -- NAFCILLIN in Norway, and another specific vaccine for the strain prevalent in Cuba.[citation
needed]
- Methicillin-resistant -- VANCOMYCIN According to reports released in May 2008, Novartis is in the advanced
Streptococcus agalactiae -- PENICILLIN G or AMPICILLIN stages of testing a general meningococcus type B vaccine.
Haemophilus influenzae -- CEFTRIAXONE or CEFOTAXIME Pneumococcal polysaccharide vaccine against Streptococcus pneumoniae is
c. Viral meningitis recommended for all people 65 years of age or older. Pneumococcal
Patients diagnosed with mild viral meningitis may improve quickly enough to conjugate vaccine is recommended for all newborns starting at 6 weeks - 2
not require admission to a hospital, while others may be hospitalized for months, American Academy of Pediatrics (AAP) recommendations.
many more days for observation and supportive care. Overall, the illness is Mumps vaccination has led to a sharp decline in mumps virus associated
usually much less severe than bacterial meningitis. meningitis, which prior to vaccination occurred in 15% of all cases of mumps.
4
Beckydecena2008
b. Prophylaxis and therefore the majority of patients with TB meningitis are started on
In cases of meningococcal meningitis, prophylactic treatment of close treatment before the diagnosis is confirmed.
relatives with antibiotics (e.g. rifampicin, ciprofloxacin or ceftriaxone) may a. Nucleic acid amplification tests (NAAT)
reduce the risk of further cases. This is a heterogeneous group of tests that use polymerase chain reaction
• Epidemiology (PCR) to detect mycobacterial nucleic acid. These tests vary in which nucleic
Meningitis can affect anyone in any age group, from the newborn to the acid sequence they detect and vary in their accuracy. The two most common
elderly. commercially available tests are the amplified mycobacterium tuberculosis
The "Meningitis Belt" is an area in sub-Saharan Africa which stretches from direct test (MTD, Gen-Probe) and Amplicor. In 2007, a systematic review of
Senegal in the west to Ethiopia in the east in which large epidemics of NAAT by the NHS Health Technology Assessment Program concluded that
meningococcal meningitis occur (this largely coincides with the Sahel for diagnosing tuberculous meningitis "Individually, the AMTD test appears to
region). It contains an estimated total population of 300 million people. The perform the best (sensitivity 74% and specificity 98%)”. In the NHS meta-
largest epidemic outbreak was in 1996, when over 250,000 cases occurred analysis, they found the pooled prevalence of TB meningitis to be 29%;
and 25,000 people died as a consequence of the disease. however there was much heterogeneity in the reported sensitivities. Using a
clinical calculator, these numbers yield a positive predictive value of 94%
• History and a negative predictive value of 90%; however the 30% prevalence may
Meningitis was first described in the 1020s in Avicenna's The Canon of
be high due to referral bias. Alternate estimates of disease prevalence can
Medicine, and again more accurately by Avenzoar of al-Andalus in the 12th be entered into the clinical calculator to refine the predictive values.
century. Symptoms of the disease were also noted in 1805 by the Swiss
Gabinetto Vieusseux (a scientific-literary association) during an outbreak in
b. Imaging
Imaging studies such as CT or MRI may show features strongly suggestive
Geneva, Switzerland. In 1887, Dr. Anton Weichselbaum (1845-1920) of
of TB meningitis, but cannot diagnose it.
Vienna became the first to isolate the specific germ, meningococcus.
In the 19th century, meningitis was a scourge of the Japanese imperial • Treatment
family, playing the largest role in the horrendous pre-maturity mortality rate The treatment of TB meningitis is isoniazid, rifampicin, pyrazinamide and
the family endured. In the mid-1800s, only the Emperor Kōmei and two of his ethambutol for two months, followed by isoniazid and rifampicin alone for a
siblings reached maturity out of fifteen total children surviving birth. Kōmei's further ten months. Steroids are always used in the first six weeks of
son, the Emperor Meiji, was one of two survivors out of Kōmei's six children, treatment (and sometimes for longer). A few patients may require
including an elder brother of Meiji who would have taken the throne had he immunomodulatory agents such as thalidomide.
lived to maturity. Five of Meiji's 15 children survived, including only his third Treatment must be started as soon as there is a reasonable suspicion of the
son, Emperor Taishō, who was feeble-minded, perhaps as a result of having diagnosis. Treatment must not be delayed while waiting for confirmation of
contracted meningitis himself. By Emperor Hirohito's generation the family the diagnosis.
was receiving modern medical attention. As the focal point of tradition in Hydrocephalus occurs as a complication in about a third of patients with TB
Japan, during the Tokugawa Shogunate the family was denied modern meningitis and will require a ventricular shunt.
"Dutch" medical treatment then in use among the upper caste; despite
extensive modernization during the Meiji Restoration the Emperor insisted on DENGUE FEVER and DENGUE HEMORRHAGIC FEVER
traditional medical care for his children.
(DHF) are acute febrile diseases, found in the tropics and Africa, and
caused by four closely related virus serotypes of the genus Flavivirus, family
TUBERCULOUS MENINGITIS is also known as TB meningitis or Flaviviridae. The geographical spread is similar to malaria, but unlike
tubercular meningitis. Tuberculous meningitis is a Mycobacterium
malaria, dengue is often found in urban areas of tropical nations, including
tuberculosis infection of the meninges. It is the most common form of CNS Puerto Rico, Singapore, Malaysia, Taiwan, Indonesia, Philippines, India and
tuberculosis.
Brazil. Each serotype is sufficiently different that there is no cross-protection
• Clinical features and epidemics caused by multiple serotypes (hyperendemicity) can occur.
Dengue is transmitted to humans by the Aedes aegypti (rarely Aedes
Fever and headache are the cardinal features. Confusion is a late feature
and coma bears a poor prognosis. Meningism is absent in a fifth of patients
albopictus) mosquito, which feeds during the day.
with TB meningitis. Patients may also have focal neurological deficits. • Signs and symptoms
• Pathology This infectious disease is manifested by a sudden onset of fever, with severe
headache, muscle and joint pains (myalgias and arthralgias—severe pain
Mycobacterium tuberculosis of the meninges is the cardinal feature and the
gives it the name break-bone fever or bonecrusher disease) and rashes. The
inflammation is concentrated towards the base of the brain. Infection begins
dengue rash is characteristically bright red petechiae and usually appears
in the lungs and may spread to the meninges by a variety of routes.
first on the lower limbs and the chest; in some patients, it spreads to cover
Blood-borne spread certainly occurs and 25% of patients with miliary TB
most of the body. There may also be gastritis with some combination of
have TB meningitis, presumably by crossing the blood-brain barrier; but a
associated abdominal pain, nausea, vomiting or diarrhea. Other symptoms
proportion of patients may get TB meningitis from rupture of a cortical focus
include:
in the brain (a so-called Rich focus); an even smaller proportion get it from
- fever
rupture of a bony focus in the spine. It is rare and unusual for TB of the spine
- bladder problems
to cause TB of the central nervous system, but isolated cases have been
- constant headaches
described.
- severe dizziness
• Diagnosis - loss of appetite
Diagnosis of TB meningitis is made by analyzing CSF collected by lumbar - uncontrollable laughing
puncture. When collecting CSF for suspected TB meningitis, a minimum of - extreme constipation
1ml of fluid should be taken (preferably 5 to 10ml). Some cases develop much milder symptoms which can, when no rash is
The CSF usually has a high protein, low glucose and a raised number of present, be misdiagnosed as influenza or other viral infection. Thus travelers
lymphocytes. Acid-fast bacilli are sometimes seen on a CSF smear, but more from tropical areas may inadvertently pass on dengue in their home
commonly, M. tuberculosis is grown in culture. A spiderweb clot in the countries, having not been properly diagnosed at the height of their illness.
collected CSF is characteristic of TB meningitis, but is a rare finding. Patients with dengue can pass on the infection only through mosquitoes or
More than half of cases of TB meningitis cannot be confirmed blood products and only while they are still febrile.
microbiologically, and these patients are treated on the basis of clinical The classic dengue fever lasts about six to seven days, with a smaller peak
suspicion only. The culture of TB from CSF takes a minimum of two weeks, of fever at the trailing end of the disease (the so-called "biphasic pattern").
Clinically, the platelet count will drop until the patient's temperature is normal.
5
Beckydecena2008
Cases of DHF also show higher fever, hemorrhagic phenomena, The first epidemics occurred almost simultaneously in Asia, Africa, and North
thrombocytopenia, and hemoconcentration. A small proportion of cases lead America in the 1780s. The disease was identified and named in 1779. A
to dengue shock syndrome (DSS) which has a high mortality rate. global pandemic began in Southeast Asia in the 1950s and by 1975 DHF
Dengue should be suspected when you have sudden onset of high fever, 39- had become a leading cause of death among children in many countries in
40°C, accompanied with severe headache, pain behind the eyes, body that region. Epidemic dengue has become more common since the 1980s.
aches, rashes on the skin and nausea or vomiting. The fever lasts for 5-7 By the late 1990s, dengue was the most important mosquito-borne disease
days. In some patients, fever comes down on the third or fourth day but it affecting humans after malaria, there being around 40 million cases of
recurs. dengue fever and several hundred thousand cases of dengue hemorrhagic
fever each year. There was a serious outbreak in Rio de Janeiro in February
• Diagnosis 2002 affecting around one million people and killing sixteen.
The diagnosis of dengue is usually made clinically. The classic picture is On March 20, 2008, the secretary of health of the state of Rio de Janeiro,
high fever with no localizing source of infection, a petechial rash with Sérgio Côrtes, announced that 23,555 cases of dengue, including 30 deaths,
thrombocytopenia and relative leukopenia. had been recorded in the state in less than three months. Côrtes said, "I am
The WHO definition of dengue hemorrhagic fever has been in use since treating this as an epidemic because the number of cases is extremely high."
1975; all four criteria must be fulfilled: Federal Minister of Health José Gomes Temporão also announced that he
- Fever was forming a panel to respond to the situation. Cesar Maia, mayor of the
- bladder problem city of Rio de Janeiro, denied that there was serious cause for concern,
- constant headaches saying that the incidence of cases was in fact declining from a peak at the
- severe dizziness and loss of appetite beginning of February. By April 3, 2008, the number of cases reported rose
a. HEMORRHAGIC TENDENCY (positive TOURNIQUET TEST, to 55,000
spontaneous bruising, bleeding from mucosa, gingival, injection sites, Significant outbreaks of dengue fever tend to occur every five or six months.
etc.; vomiting blood, or bloody diarrhea) The cyclicity in numbers of dengue cases is thought to be the result of
b. THROMBOCYTOPENIA (<100,000 platelets per mm³ or estimated seasonal cycles interacting with a short-lived cross-immunity for all four
as less than 3 platelets per high power field) strains, in people who have had dengue (Wearing and Rohani 2006). When
c. EVIDENCE OF PLASMA LEAKAGE (hematocrit more than 20% the cross-immunity wears off, the population is then more susceptible to
higher than expected, or drop in hematocrit of 20% or more from transmission whenever the next seasonal peak occurs. Thus in the longer
baseline following IV fluid, pleural effusion, ascites, hypoproteinemia) term of several years, there tend to remain large numbers of susceptible
people in the population despite previous outbreaks because there are four
DENGUE SHOCK SYNDROME is defined as Dengue Hemorrhagic different strains of the dengue virus and because of new susceptible
Fever plus:
individuals entering the target population, either through childbirth or
- Weak rapid pulse,
immigration.
- Narrow pulse pressure (less than 20 mm Hg) or,
There is significant evidence, originally suggested by S.B. Halstead in the
- Cold, clammy skin and restlessness
1970s that dengue hemorrhagic fever is more likely to occur in patients who
- Serology and polymerase chain reaction (PCR) studies are available
have secondary infections by serotypes different from the primary infection.
to confirm the diagnosis of dengue if clinically indicated
One model to explain this process is known as antibody-dependent
• Treatment enhancement (ADE), which allows for increased uptake and virion replication
The mainstay of treatment is supportive therapy. Increased oral fluid intake is during a secondary infection with a different strain. Through an
recommended to prevent dehydration. Supplementation with intravenous immunological phenomenon, known as original antigenic sin, the immune
fluids may be necessary to prevent dehydration and significant concentration system is not able to adequately respond to the stronger infection, and the
of the blood if the patient is unable to maintain oral intake. A platelet secondary infection becomes far more serious. This process is also known
transfusion is indicated in rare cases if the platelet level drops significantly as superinfection (Nowak and May 1994; Levin and Pimentel 1981).
(below 20,000) or if there are significant bleeding. In Singapore, there are about 4,000–5,000 reported cases of dengue fever
The presence of melena may indicate internal gastrointestinal bleeding or dengue hemorrhagic fever every year. In the year 2003, there were six
requiring platelet and/or red blood cell transfusion. deaths from dengue shock syndrome. It is believed that the reported cases
Like most viral diseases there is no specific cure for dengue fever. Antibiotics of dengue are an underrepresentation of all the cases of dengue as it would
do not help. ASPIRIN and NON-STEROIDAL ANTI-INFLAMMATORY ignore subclinical cases and cases where the patient did not present for
DRUGS should be avoided as these drugs may worsen the bleeding medical treatment. With proper medical treatment, the mortality rate for
tendency associated with some of these infections. Patients may receive dengue can therefore be brought down to less than 1 in 1000.
paracetamol preparations to deal with these symptoms if dengue is • Prevention
suspected.
Most patients with dengue fever can be treated at home. They should take
a. Vaccine development
There is no commercially available vaccine for the dengue Flavivirus.
rest, drink plenty of fluids and eat nutritious food. Whenever available, Oral
However, one of the many ongoing vaccine development programs is the
Rehydration Salt (commonly used in treating diarrhea) should be used.
Pediatric Dengue Vaccine Initiative which was set up in 2003 with the aim of
Sufficient fluid intake is very important. Generally the progression towards
accelerating the development and introduction of dengue vaccine(s) that are
dengue hemorrhagic fever or dengue shock syndrome occurs after 3-5 days
affordable and accessible to poor children in endemic countries. Thai
of fever. At this time, fever has often come down. This may mislead many of
researchers are testing a dengue fever vaccine on 3,000–5,000 human
us to believe that the patient is heading towards recovery. This is the most
volunteers after having successfully conducted tests on animals and a small
dangerous period that requires high vigilance. It is best to consult a
group of human volunteers. A number of other vaccine candidates are
physician. Indications for hospitalization are persistent vomiting, inability to
entering phase I or II testing.
take oral fluids, persistent abdominal pain, restlessness, or bleeding from
any site (nose, gums, passage of black stools). b. Mosquito control
a. Emerging treatments Primary prevention of dengue mainly resides in mosquito control. There are
two primary methods: LARVAL CONTROL and ADULT MOSQUITO
Emerging evidence suggests that mycophenolic acid and ribavirin inhibit
CONTROL. In urban areas, Aedes mosquitoes breed on water collections in
dengue replication. Initial experiments showed a fivefold increase in
artificial containers such as plastic cups, used tires, broken bottles, flower
defective viral RNA production by cells treated with each drug. In vivo
pots, etc. Continued and sustained artificial container reduction or periodic
studies, however, have not yet been done.
draining of artificial containers is the most effective way of reducing the larva
• Epidemiology and thereby the Aedes mosquito load in the community. Larvicide treatment
is another effective way of control the vector larvae but the Larvicide chosen
6
Beckydecena2008
should be long lasting and preferably have World Health Organization
clearance for use in drinking water. There are some very effective insect
growth regulators (IGR`s) available which are both safe and long lasting e.g.
pyriproxyfen. For reducing the adult mosquito load, fogging with insecticide is
somewhat effective.
c. Prevention of mosquito bites
Prevention of mosquito bites is another way of preventing disease. This can
be achieved either by personal protection or by using mosquito nets. In
1998, scientists from the Queensland Institute of Research in Australia and
Vietnam's Ministry of Health introduced a scheme that encouraged children
to place a water bug, the crustacean Mesocyclops, in water tanks and
discarded containers where the Aedes aegypti mosquito was known to
thrive. This method is viewed as being more cost-effective and more
environmentally friendly than pesticides, though not as effective, and
requires the ongoing participation of the community.
d. Personal protection
Personal prevention consists of the use of mosquito nets, repellents
containing NNDB or DEET, covering exposed skin, use of DEET-
impregnated bednets, and avoiding endemic areas.
e. Potential antiviral approaches
In cell culture experiments and mice Morpholino antisense oligos have
shown specific activity against Dengue virus.
The yellow fever vaccine (YF-17D) is a related Flavivirus, thus the chimeric
replacement of yellow fever vaccine with dengue has been often suggested
but no full scale studies have been conducted to date.
In 2006, a group of Argentine scientists discovered the molecular replication
mechanism of the virus, which could be attacked by disruption of the
polymerase's work.
• History
The origins of the word dengue are not clear, but one theory is that it is
derived from the Swahili phrase "Ka-dinga pepo", which describes the
disease as being caused by an evil spirit. The Swahili word "dinga" may
possibly have its origin in the Spanish word "dengue" (fastidious or careful);
describing the gait of a person suffering dengue fever or, alternatively, the
Spanish word may derive from the Swahili. It may also be attributed to the
phrase meaning "Break bone fever", referencing the fact that pain in the
bones is a common symptom.
Outbreaks resembling dengue fever have been reported throughout history.
The first definitive case report dates from 1789 and is attributed to Benjamin
Rush, who coined the term "breakbone fever" (because of the symptoms of
myalgia and arthralgia). The viral etiology and the transmission by
mosquitoes were deciphered only in the 20th century. Population
movements during World War II spread the disease globally.
In 2007 replication mechanism of the virus was interrupted by interception of
the viral protease, and currently a project to identify new protease
interception mechanisms of the whole family of the virus has been launched
(Dengue virus belong to the family Flaviviridae, which includes among others
HCV, West Nile and Yellow fever viruses).
7
Beckydecena2008
You might also like
- NLN Medication Exam Study Guide QuizletDocument36 pagesNLN Medication Exam Study Guide Quizletmaniz442No ratings yet
- NeuroinfecciónDocument19 pagesNeuroinfecciónfabio100% (1)
- Philippine Handbook On Adult Immunization 2012 PDFDocument140 pagesPhilippine Handbook On Adult Immunization 2012 PDFLinius CruzNo ratings yet
- CH 5.1 - Vaccine Saftey ForwardDocument24 pagesCH 5.1 - Vaccine Saftey Forwardtolerancelost607100% (4)
- AMCQ Pictures Review PART IIDocument61 pagesAMCQ Pictures Review PART IIKyi Lai Lai Aung100% (3)
- 7 Reasons Not To VaccinateDocument4 pages7 Reasons Not To VaccinateMiri Ch67% (3)
- Varicella/Herpes Zoster: Communicable Disease Management ProtocolDocument5 pagesVaricella/Herpes Zoster: Communicable Disease Management Protocolyuliyanto.efendiNo ratings yet
- Fwd. Epi 8Document40 pagesFwd. Epi 8Sumayya ChughtaiNo ratings yet
- VaricellaDocument4 pagesVaricellasingcojericho11No ratings yet
- Vaccinated Persons: Other Typical Symptoms That May Begin To Appear 1-2 Days Before Rash IncludeDocument5 pagesVaccinated Persons: Other Typical Symptoms That May Begin To Appear 1-2 Days Before Rash IncludePrimita Ayu DamayantiNo ratings yet
- ChickenpoxDocument16 pagesChickenpoxJeet ThuraiNo ratings yet
- Varicella Zoster Virus Infection: July 2015Document19 pagesVaricella Zoster Virus Infection: July 2015nickNo ratings yet
- Chicken PoxDocument15 pagesChicken PoxQareeb KhanNo ratings yet
- Home Visual Library Resources News Resources Mobile Subscribe Contact Skip To Main Page ContentDocument50 pagesHome Visual Library Resources News Resources Mobile Subscribe Contact Skip To Main Page ContentAnastasia Lilian SuryajayaNo ratings yet
- Pinkbook: Herpes Zoster - CDCDocument8 pagesPinkbook: Herpes Zoster - CDCRezza PratamaNo ratings yet
- Chickenpox and SmallpoxDocument28 pagesChickenpox and SmallpoxFourth YearNo ratings yet
- Herpes Zoster Overview: Natural History and Incidence: Bethany A. Weaver, DO, MPHDocument5 pagesHerpes Zoster Overview: Natural History and Incidence: Bethany A. Weaver, DO, MPHRobbyNo ratings yet
- Varicella ZosterDocument41 pagesVaricella Zostertummalapalli venkateswara raoNo ratings yet
- Herpes 3, VSVDocument21 pagesHerpes 3, VSVCharles SainzNo ratings yet
- Varicella: Immunization, Vaccines and BiologicalsDocument1 pageVaricella: Immunization, Vaccines and BiologicalsRozakNo ratings yet
- VariselaDocument5 pagesVariselaalrisimanungkalit27No ratings yet
- 22 Varicella Pink BookDocument24 pages22 Varicella Pink BookMohamad Syaikhul IslamNo ratings yet
- Varicella Zoster VirusDocument3 pagesVaricella Zoster VirusjojecoyocaNo ratings yet
- Indonesian VaricellaDocument18 pagesIndonesian VaricellaWahyu FathurrachmanNo ratings yet
- VaricellachickenpoxDocument6 pagesVaricellachickenpoxDedi SofyanNo ratings yet
- CASE STUDY - Docx Maam AlapDocument7 pagesCASE STUDY - Docx Maam AlapSam Aquino IINo ratings yet
- ChickenpoxDocument21 pagesChickenpoxanishadange7273No ratings yet
- CHICKENPOXDocument32 pagesCHICKENPOXCharlz ZipaganNo ratings yet
- Varicella Zoster (Chickenpox) : Frequently Asked QuestionsDocument2 pagesVaricella Zoster (Chickenpox) : Frequently Asked QuestionsMuhammad mukramNo ratings yet
- 2018 Varicella-Zoster Virus InfectionDocument11 pages2018 Varicella-Zoster Virus Infectioneva yustianaNo ratings yet
- Varicella/Herpes Zoster: Communicable Disease Management ProtocolDocument0 pagesVaricella/Herpes Zoster: Communicable Disease Management ProtocolJohn StenlyNo ratings yet
- Varicella 1. Symptoms and SignsDocument3 pagesVaricella 1. Symptoms and SignsBahar KeyNo ratings yet
- Background: Pediatric Chickenpox Next Section: PathophysiologyDocument12 pagesBackground: Pediatric Chickenpox Next Section: PathophysiologyRachel Johann Aquinto100% (1)
- Martinon TorresDocument4 pagesMartinon TorresFiqha RosaNo ratings yet
- Calixtro, LJ Viral Infections Narrative PathophysiologyDocument29 pagesCalixtro, LJ Viral Infections Narrative PathophysiologyKim SunooNo ratings yet
- Green Book Chapter 34 v3 0Document22 pagesGreen Book Chapter 34 v3 0حسام الدين إسماعيلNo ratings yet
- Chickenpox Chickenpox Is A Highly Contagious Disease Caused by Primary Infection With Varicella ZosterDocument12 pagesChickenpox Chickenpox Is A Highly Contagious Disease Caused by Primary Infection With Varicella Zostersubbu2raj3372100% (2)
- German MeaslesDocument25 pagesGerman MeaslesVysakhi PVNo ratings yet
- DR OWOWODocument34 pagesDR OWOWOhezekiahjoshua02No ratings yet
- ChickenpoxDocument23 pagesChickenpoxLukman HikimNo ratings yet
- Kutis PorcelanaDocument34 pagesKutis Porcelanaapi-3743483No ratings yet
- Varicella Vaccine: Clinical DescriptionDocument1 pageVaricella Vaccine: Clinical DescriptionArturo XadoNo ratings yet
- Viral DiseasesDocument54 pagesViral Diseasesapi-19916399No ratings yet
- Clinical Features of Varicella-Zoster Virus Infection - Chickenpox - UpToDateDocument16 pagesClinical Features of Varicella-Zoster Virus Infection - Chickenpox - UpToDatevotuyetdongtrinhNo ratings yet
- Varicella ZoosterDocument6 pagesVaricella ZoosterDayana PrasanthNo ratings yet
- PAEDS 4 - 18.10.19 Viral InfectionDocument15 pagesPAEDS 4 - 18.10.19 Viral Infectionlotp12No ratings yet
- Signs and Symptoms: Chickenpox Is A HighlyDocument4 pagesSigns and Symptoms: Chickenpox Is A HighlysaaaraelleNo ratings yet
- Small PoxDocument12 pagesSmall Poxnn1216100% (1)
- Varicella by Siva MurugadossDocument34 pagesVaricella by Siva MurugadossPrakask BalanNo ratings yet
- Varicella ZosterDocument1 pageVaricella Zosterapi-276987332No ratings yet
- Chickenpox (Varicella) For Healthcare Professionals CDCDocument1 pageChickenpox (Varicella) For Healthcare Professionals CDClaucavalcanteNo ratings yet
- Presentation and Management of Herpes Zoster (Shingles) in The Geriatric PopulationDocument9 pagesPresentation and Management of Herpes Zoster (Shingles) in The Geriatric PopulationGrace Febryanti TodingNo ratings yet
- AnalysisDocument4 pagesAnalysisfortuneayaNo ratings yet
- Communicable Disease: - East Africa University Bosaso, Puntland Somalia Mr. Buruj AliDocument38 pagesCommunicable Disease: - East Africa University Bosaso, Puntland Somalia Mr. Buruj AliShaimaa AbdulkadirNo ratings yet
- Varicella Zoster VirusDocument13 pagesVaricella Zoster VirusyatikriyaNo ratings yet
- Chicken Pox and Herpes ZosterfinalDocument31 pagesChicken Pox and Herpes ZosterfinalBinayaNo ratings yet
- Chickenpo X: Presented By:-Priya Yadav Roll No 02 2 Yeat BSC Nursing (H) College of Nursing Dr. RML HospitalDocument41 pagesChickenpo X: Presented By:-Priya Yadav Roll No 02 2 Yeat BSC Nursing (H) College of Nursing Dr. RML HospitalNikita JangraNo ratings yet
- Case Presentation - Chicken PoxDocument5 pagesCase Presentation - Chicken PoxNadzmiera SalaNo ratings yet
- Varicella Zooster VirusDocument9 pagesVaricella Zooster VirusChikita Artia SariNo ratings yet
- Viruses: Clinical Features of Varicella-Zoster Virus InfectionDocument11 pagesViruses: Clinical Features of Varicella-Zoster Virus InfectionBobby S PromondoNo ratings yet
- Humen Herpesvirus and Chicken PoxDocument62 pagesHumen Herpesvirus and Chicken Poxprabad dunusingheNo ratings yet
- Advances and Perspectives in The Management of Varicella-Zoster VirusDocument69 pagesAdvances and Perspectives in The Management of Varicella-Zoster VirusCitra Annisa FitriNo ratings yet
- Quiz 1Document5 pagesQuiz 1Francis Rafael PadillaNo ratings yet
- Drugs in PediatricsDocument18 pagesDrugs in PediatricsKarla Sanchez100% (5)
- 膚科Document191 pages膚科Sai TaiNo ratings yet
- Antenatal CareDocument82 pagesAntenatal Caremdasad18No ratings yet
- Soal MCQDocument39 pagesSoal MCQRonald Allan Valle SantosNo ratings yet
- Management of Varicella in Neonates and Infants: Sophie Blumental, Philippe LepageDocument6 pagesManagement of Varicella in Neonates and Infants: Sophie Blumental, Philippe LepageMaria Noviyanti FransiskaNo ratings yet
- CD DRILLS (Communicable DiseasesDocument8 pagesCD DRILLS (Communicable DiseasesJune DumdumayaNo ratings yet
- BRY's Microbiology, 1st SemesterDocument95 pagesBRY's Microbiology, 1st SemesterSaima ZuberiNo ratings yet
- Virology Micro D&R AgamDocument142 pagesVirology Micro D&R AgamNirosha Arul100% (1)
- Session 1 Part 2Document216 pagesSession 1 Part 2AmalNo ratings yet
- Drugs GRP!!Document89 pagesDrugs GRP!!Joanne SandovalNo ratings yet
- Systematic Review of Anti-Inflammatory Properties of Phyllanthus NiruriDocument4 pagesSystematic Review of Anti-Inflammatory Properties of Phyllanthus NiruriInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Viral Skin Infections: Verrucae ValgarusDocument14 pagesViral Skin Infections: Verrucae Valgarusمسلم هاشم منافNo ratings yet
- Pathophysiology - Chicken Pox Paper PDFDocument6 pagesPathophysiology - Chicken Pox Paper PDFRhiannon MartinNo ratings yet
- Oxfordshire ADULT Antimicrobial Prescribing Guidelines For Primary CareDocument21 pagesOxfordshire ADULT Antimicrobial Prescribing Guidelines For Primary CareDan IonescuNo ratings yet
- Chemotherapy Leukemia: B. Administer Varicella-Zoster Immune Globulin To The ClientDocument12 pagesChemotherapy Leukemia: B. Administer Varicella-Zoster Immune Globulin To The ClientAsterlyn ConiendoNo ratings yet
- Hippo EM Foundations - Pediatric Emergencies Written SummaryDocument31 pagesHippo EM Foundations - Pediatric Emergencies Written Summarykaylawilliam01No ratings yet
- Viral InfectionsDocument103 pagesViral InfectionsAkash Anilkumar MaliniNo ratings yet
- Case Report Herpes Zoster Regio Th11 - L5Document37 pagesCase Report Herpes Zoster Regio Th11 - L5fatqur28No ratings yet
- Chicken Pox N C P BY BHERU LALDocument2 pagesChicken Pox N C P BY BHERU LALBheru Lal100% (1)
- NDT LecDocument19 pagesNDT LecGummy BearsNo ratings yet
- This Is A Document About Chicken PoxDocument24 pagesThis Is A Document About Chicken Poxarul100% (1)
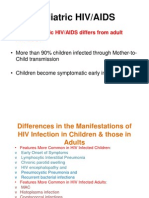
- Paediatric HIV Infection by DR A.K.Gupta, Additional Project Director, Delhi State AIDS Control SocietyDocument88 pagesPaediatric HIV Infection by DR A.K.Gupta, Additional Project Director, Delhi State AIDS Control Societydr.a.k.gupta6924No ratings yet
- Preventive and Social MedicineDocument14 pagesPreventive and Social MedicineSuresh GuduruNo ratings yet