Professional Documents
Culture Documents
Cit0110 Feature Williams
Cit0110 Feature Williams
Uploaded by
VidaOpinaldoCopyright:
Available Formats
You might also like
- Asepsis Antisepsis and Skin PreparationDocument6 pagesAsepsis Antisepsis and Skin PreparationDavid Tritono Di BallastrossNo ratings yet
- 2014 Changes in NSTE-ACSDocument4 pages2014 Changes in NSTE-ACSnbnbNo ratings yet
- Diabetes With Coronary Disease - A Moving Target Amid Evolving Therapies?Document3 pagesDiabetes With Coronary Disease - A Moving Target Amid Evolving Therapies?Aldy PratamaNo ratings yet
- What Are Optimal P2Y12 Inhibitor and Schedule of Administration in Patients With Acute Coronary Syndrome?Document10 pagesWhat Are Optimal P2Y12 Inhibitor and Schedule of Administration in Patients With Acute Coronary Syndrome?david1086No ratings yet
- Adding CABG To The Dual Antiplatelet Salad: Editorial CommentDocument3 pagesAdding CABG To The Dual Antiplatelet Salad: Editorial CommentVassili CrispiNo ratings yet
- Acuity TrialDocument10 pagesAcuity TrialAhsan KhanNo ratings yet
- Brodie 2000Document6 pagesBrodie 2000SuryaNo ratings yet
- Evidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Document11 pagesEvidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Edgar PazNo ratings yet
- 2009.-Prasugrel in Clinical PracticeDocument3 pages2009.-Prasugrel in Clinical Practicetristan9454No ratings yet
- White 2012 Champion PooledDocument13 pagesWhite 2012 Champion PooledRadu CiprianNo ratings yet
- PCI in Acute ST-elevation Myocardial Infarction (STEMI) : Reference - Ids - Tool - Tip Reference - IdsDocument5 pagesPCI in Acute ST-elevation Myocardial Infarction (STEMI) : Reference - Ids - Tool - Tip Reference - IdsfiraNo ratings yet
- 2015 ACC/AHA/SCAI Focused Update On Primary PCI For Patients With STEMIDocument8 pages2015 ACC/AHA/SCAI Focused Update On Primary PCI For Patients With STEMIrina1511No ratings yet
- CDT 08 05 647Document16 pagesCDT 08 05 647david1086No ratings yet
- Should B-Blockers Still Be Routine After Myocardial Infarction?Document6 pagesShould B-Blockers Still Be Routine After Myocardial Infarction?Raul GascueñaNo ratings yet
- Antithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextDocument12 pagesAntithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextenviNo ratings yet
- 1 s2.0 S000649712034115X MainDocument7 pages1 s2.0 S000649712034115X MainretnoNo ratings yet
- Isi BukuDocument183 pagesIsi BukuHayat Hamzah DawiNo ratings yet
- MainDocument1 pageMainDarimotu MankogulsNo ratings yet
- Beta Blockers Vs Calcium Channel Blockers White Paper 20190913Document3 pagesBeta Blockers Vs Calcium Channel Blockers White Paper 20190913mohammedyosif76No ratings yet
- Acs 37 001Document8 pagesAcs 37 001Luis Rafael Suárez U.No ratings yet
- Aspiration Thrombectomy For Acute ST-Elevation Myocardial Infarction: Literature ReviewDocument9 pagesAspiration Thrombectomy For Acute ST-Elevation Myocardial Infarction: Literature ReviewArdiana FirdausNo ratings yet
- 2510 FullDocument11 pages2510 FullTommy WidjayaNo ratings yet
- Fondaparinux in Acute Coronary Syndromes CA5068 Admin OnlyDocument9 pagesFondaparinux in Acute Coronary Syndromes CA5068 Admin OnlynaeamzNo ratings yet
- Pegasus TIMI 54 TrialDocument13 pagesPegasus TIMI 54 TrialIsaac Aaron Enriquez MonsalvoNo ratings yet
- Doacs in Patients With Mitral Stenosis and Atrial FibrillationDocument3 pagesDoacs in Patients With Mitral Stenosis and Atrial FibrillationNasriNo ratings yet
- Treatment Angina Where Are WeDocument16 pagesTreatment Angina Where Are WeFitra AlfaniNo ratings yet
- 1 s2.0 S0002870316000156 MainDocument9 pages1 s2.0 S0002870316000156 MainSaid Qadaru ANo ratings yet
- J Jcin 2023 01 366Document15 pagesJ Jcin 2023 01 366Kardiologi ManadoNo ratings yet
- Combining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHADocument7 pagesCombining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHADrHellenNo ratings yet
- Prasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesDocument15 pagesPrasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesDito LopezNo ratings yet
- Thesis On Acute Coronary SyndromeDocument5 pagesThesis On Acute Coronary Syndromejum1p0tonip3100% (2)
- Significant Early In-Hospital Benefit Was Seen. Clopidogrel Is Prefferd ToDocument8 pagesSignificant Early In-Hospital Benefit Was Seen. Clopidogrel Is Prefferd TogilnifNo ratings yet
- Disminucion de Lípidos en Sindrome Coronario Agudo. Nicholls S 2018Document2 pagesDisminucion de Lípidos en Sindrome Coronario Agudo. Nicholls S 2018Tony Miguel Saba SabaNo ratings yet
- Furtado 2016Document10 pagesFurtado 2016zzzzNo ratings yet
- Acs 07 04 506Document10 pagesAcs 07 04 506Mohammed ThabtNo ratings yet
- De Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IDocument43 pagesDe Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IAkhmad HidayatNo ratings yet
- 112294Document32 pages112294Ivan FirmansyahNo ratings yet
- Consesus Acute Coronary Taiwan-2018Document10 pagesConsesus Acute Coronary Taiwan-2018Gabriela Catana TurcuNo ratings yet
- Evidence-Based College of Chest Physicians: American New Antithrombotic DrugsDocument25 pagesEvidence-Based College of Chest Physicians: American New Antithrombotic DrugsDiego Fernando Escobar GarciaNo ratings yet
- European J of Heart Fail - 2021 - Greene - Another Reason To Embrace Quadruple Medical Therapy For Heart FailureDocument4 pagesEuropean J of Heart Fail - 2021 - Greene - Another Reason To Embrace Quadruple Medical Therapy For Heart FailureSrinivas PingaliNo ratings yet
- ESCAPE Study - JAMA 2005Document9 pagesESCAPE Study - JAMA 2005MICHAEL AMARILLO CORREANo ratings yet
- DabigatranDocument12 pagesDabigatranAdityaSaskaraNo ratings yet
- The Pulmonary Artery Catheter: Is It Still Alive?: ReviewDocument5 pagesThe Pulmonary Artery Catheter: Is It Still Alive?: ReviewAttilio Del RossoNo ratings yet
- Platelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionDocument9 pagesPlatelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionJanuar RezkyNo ratings yet
- Ticagrelor Vs Clopidogrel Clinical Outcomes in Stelevation Myocardial Infarction Patients March 2023 0716017862 7840249Document4 pagesTicagrelor Vs Clopidogrel Clinical Outcomes in Stelevation Myocardial Infarction Patients March 2023 0716017862 7840249Atul DwivediNo ratings yet
- 996 4398 3 PBDocument7 pages996 4398 3 PBM. PurnomoNo ratings yet
- 2013 ACCF/AHA Guideline For The Management of ST-Elevation Myocardial InfarctionDocument126 pages2013 ACCF/AHA Guideline For The Management of ST-Elevation Myocardial InfarctionDr Edi HidayatNo ratings yet
- 1 s2.0 S2405500X22006697 MainDocument12 pages1 s2.0 S2405500X22006697 MainOttofianus Alvedo Hewick KalangiNo ratings yet
- Year in NSTEMIDocument14 pagesYear in NSTEMILiviuNo ratings yet
- DudjDocument4 pagesDudjsyaiful rinantoNo ratings yet
- JCM 09 01963 v2Document18 pagesJCM 09 01963 v2Jesus MoscosoNo ratings yet
- Jaha 117 007288Document4 pagesJaha 117 007288Alberto PolimeniNo ratings yet
- Antiplatelet Therapy: New Antiplatelet Drugs in PerspectiveDocument4 pagesAntiplatelet Therapy: New Antiplatelet Drugs in Perspectivegeo_mmsNo ratings yet
- Tactics 2001 NejmDocument9 pagesTactics 2001 NejmGustavo Reyes QuezadaNo ratings yet
- 1 s2.0 S0735109716003995 MainDocument2 pages1 s2.0 S0735109716003995 MaintopanNo ratings yet
- Braunwalds PCI For AMIDocument44 pagesBraunwalds PCI For AMIusfcards100% (1)
- Managing Stable Ischemic Heart DiseaseDocument3 pagesManaging Stable Ischemic Heart Diseasealikarimiak1347No ratings yet
- Bleeding Is Out, Your Own Blood Is in 2014Document4 pagesBleeding Is Out, Your Own Blood Is in 2014viaereaNo ratings yet
- Antipl - After DischargeDocument8 pagesAntipl - After DischargeNagatzulNo ratings yet
- Cardiology Update 2018 The First QuarterDocument6 pagesCardiology Update 2018 The First QuarterAditya SutarNo ratings yet
- Manual of STEMI InterventionsFrom EverandManual of STEMI InterventionsSameer MehtaNo ratings yet
- Medwave 2018 07 E7354 PDFDocument7 pagesMedwave 2018 07 E7354 PDFMarceloNo ratings yet
- East FeedingDocument5 pagesEast FeedingJeya vanithaNo ratings yet
- Rapid Response TeamDocument4 pagesRapid Response TeamMichael SilvaNo ratings yet
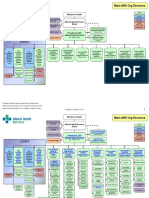
- Ahs Org OrgchartDocument2 pagesAhs Org OrgchartДрагослав БјелицаNo ratings yet
- Electrocardiographic Predictors of Incident Atrial Fibrillation - DavidDocument6 pagesElectrocardiographic Predictors of Incident Atrial Fibrillation - DavidDavid Jimmy Kurniawan RejosaputroNo ratings yet
- Biocide in WastewaterDocument19 pagesBiocide in WastewaterJohn SmithNo ratings yet
- Neonatal Mechanical Ventilation Predictors of Mortality and OutcomesDocument8 pagesNeonatal Mechanical Ventilation Predictors of Mortality and OutcomesAthenaeum Scientific PublishersNo ratings yet
- Natural Benefits - EnglishDocument124 pagesNatural Benefits - EnglishNaveen SinghNo ratings yet
- UrapidilDocument11 pagesUrapidilFrancesco LucianiNo ratings yet
- Icope Infographic FullDocument1 pageIcope Infographic Fulljon Torres100% (1)
- Updates and Management Algorithm For Neuroendocrine Tumors of The Uterine CervixDocument10 pagesUpdates and Management Algorithm For Neuroendocrine Tumors of The Uterine CervixdosiNo ratings yet
- AYUSHMAN BHARAT Seminar SlidesDocument42 pagesAYUSHMAN BHARAT Seminar Slidesgilbert2691No ratings yet
- Principles of Drug Addiction Treatment: A Research-Based GuideDocument44 pagesPrinciples of Drug Addiction Treatment: A Research-Based GuideKrishna RathodNo ratings yet
- Newly Diagnosed GlioblastomaDocument30 pagesNewly Diagnosed GlioblastomaJubairNo ratings yet
- Allysa Marie Silbol Beed I1Document3 pagesAllysa Marie Silbol Beed I1Allysa Marie SilbolNo ratings yet
- Control and RandomizationDocument18 pagesControl and RandomizationRARCHITA SHARMANo ratings yet
- Morton - Critical Care Nursing 10eDocument6 pagesMorton - Critical Care Nursing 10eblue_blood_boy100% (1)
- Xerophtalmia - KhuranaDocument4 pagesXerophtalmia - KhuranaAslesa Wangpathi Pagehgiri100% (1)
- Colegio Gonzalo Jimenez Navas: Individual WorkDocument3 pagesColegio Gonzalo Jimenez Navas: Individual WorkNicolas Cárdenas maldonadoNo ratings yet
- MIMS Doctor November 2016 RGDocument36 pagesMIMS Doctor November 2016 RGDarmawan HariyantoNo ratings yet
- Giardiasis and FecalysisDocument2 pagesGiardiasis and Fecalysiskmpg11No ratings yet
- Hashimoto's Triggers-Advanced Reader Copy-V2Document332 pagesHashimoto's Triggers-Advanced Reader Copy-V2Anonymous XiymFuQdF100% (2)
- OrganisationDocument46 pagesOrganisationShreyas Walvekar100% (1)
- AIIMS PG Jan 2015Document50 pagesAIIMS PG Jan 2015AnweshaBoseNo ratings yet
- Biophysical AssessmentDocument9 pagesBiophysical AssessmentSanjeev NambalateNo ratings yet
- OB Review QuestionsDocument15 pagesOB Review QuestionsDavid Hieu NgoNo ratings yet
- 19BMS134 - Divyajeet Singh'Document63 pages19BMS134 - Divyajeet Singh'Divyajeet SinghNo ratings yet
- Suicide in Children and Adolescents Cambridge Child and Adolescent PsychiatryDocument333 pagesSuicide in Children and Adolescents Cambridge Child and Adolescent PsychiatryFlorin Tudose100% (1)
- Naini 2020Document1 pageNaini 2020druzair007No ratings yet
Cit0110 Feature Williams
Cit0110 Feature Williams
Uploaded by
VidaOpinaldoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cit0110 Feature Williams
Cit0110 Feature Williams
Uploaded by
VidaOpinaldoCopyright:
Available Formats
COVER STORY
Guidelines
for STEMI
Key messages from the ACC/AHA/SCAI 2009 focused update
for the management of ST-elevation myocardial infarction.
BY JEFFREY M. SPARLING, MD; PINAK B. SHAH, MD; AND DAVID O. WILLIAMS, MD
he in-hospital management of ST-elevation the era before the widespread use of DAPT. Because of this
T myocardial infarction (STEMI) has evolved sig-
nificantly during the last decade, with particular
emphasis on primary percutaneous coronary
intervention (PCI) as the preferred treatment strategy
when feasible.
lack of effectiveness, the Task Force downgraded the rec-
ommendation for GP IIb/IIIa inhibitor use in STEMI, except
in selected patients with unique features (eg, persistent
thrombus burden) in whom these agents may have incre-
mental value.
Significantly, new information has emerged during the The role of thienopyridines continues to expand in
last 2 years regarding the practice of primary PCI that jus- STEMI care, a strategy certainly emphasized in the guide-
tifies a reassessment of procedural strategies and adjunc- line update. Thienopyridines, as adjuncts to aspirin, are
tive therapies. Ongoing review by the American College of now considered an essential component of the manage-
Cardiology/American Heart Association (ACC/AHA) Task ment of patients with STEMI, and the options available to
Force on Practice Guidelines of these data in 2009 the clinician have expanded in the time since the manage-
prompted a focused update, in conjunction with the ment guidelines were last updated. Prasugrel, a new
Society for Cardiovascular Angiography and Interventions thienopyridine with actions documented in the TRITON-
(SCAI), to the guidelines for management of patients with TIMI 38 trial, has been approved by the US Food and Drug
STEMI.1 The purpose of this article is to identify and com- Administration and is currently clinically available. In TRI-
ment on certain key points of this focused update that TON-TIMI 38, prasugrel afforded a 19% relative risk reduc-
should influence patient management in STEMI, both in tion in the primary composite endpoint of death, nonfatal
and out of the catheterization laboratory. MI, or nonfatal stroke when compared to clopidogrel, at
the expense of a significant increase in the risk of major
PHARM ACOLOGIC M ANAGE MENT bleeding.5 Three subgroups of patients appeared not to
The use of glycoprotein IIb/IIIa (GP IIb/IIIa) receptor benefit or even have net harm, including patients with pre-
inhibitors was reviewed by the Task Force based on a vious history of stroke or transient ischemic attack, those
number of recent important clinical trials, which resulted aged 75 years or older, and patients with body weights less
in a remarkable shift in treatment recommendations.1,2-4 than 60 kg, leading to a recommendation that prasugrel
The new guideline update advocates starting GP IIb/IIIa not be used in these patient populations. Prasugrel is
inhibitors only at the time of primary PCI, not before, and administered as a 60-mg preprocedural load followed by a
even then only in “selected” patients as a IIa recommen- maintenance dose of 10 mg/d. Although the exact role of
dation. Additionally, the initiation of GP IIb/IIIa inhibition prasugrel remains to be defined by clinicians, this year’s
before primary PCI is now classified as a IIb recommenda- focused guideline update now includes prasugrel as a class I
tion, and in fact, is termed “uncertain … usefulness.” recommendation.
The reasoning for this de-emphasis of the role for GP Recently, much attention has been given to the sup-
IIb/IIIa inhibitors results from trials demonstrating the lack posed interactions between thienopyridines and proton-
of efficacy of GP IIb/IIIa inhibitors in the era of dual- pump inhibitors, which are postulated to interfere with
antiplatelet therapy (DAPT). The body of evidence sup- the platelet inhibition of clopidogrel and, to a lesser extent,
porting the use of GP IIb/IIIa inhibitors was developed in prasugrel. Despite ex vivo platelet inhibition studies and
JANUARY/FEBRUARY 2010 I CARDIAC INTERVENTIONS TODAY I 31
COVER STORY
retrospective reports suggesting a negative interaction thrombosis in the pathogenesis of STEMI, thrombus
between the two classes, there exist no published, peer- removal has the potential of augmenting coronary blood
reviewed, randomized clinical trial data proving such a flow at both the epicardial and microvascular levels.
link. As such, the writing committee did not feel it pru- Furthermore, improved myocardial perfusion may trans-
dent to add a guideline addressing this potential interac- late into clinical benefit such as lower cardiovascular
tion despite the widespread concomitant use of these mortality rates. The data of two randomized trials,
two classes. Since that time, the COGENT trial, which TAPAS and EXPIRA, which evaluated manual thrombus
prospectively examined the interaction between clopido- aspiration as an initial reperfusion strategy, resulted in a
grel and omeprazole, was presented at the 2009 new IIa recommendation in the 2009 update. These trials
Transcatheter Cardiovascular Therapeutics Scientific demonstrated improved perfusion of the microcircula-
Sessions. Although the trial was discontinued early tion, reduction in infarct size in EXPIRA, and lower 1-year
because of funding, it did not demonstrate any adverse cardiac death or nonfatal reinfarction rates in TAPAS
effect of omeprazole on the effectiveness of clopidogrel.6 compared to patients who did not receive thrombus
Parenteral anticoagulants remain a cornerstone of aspiration.7,8 It is notable that in both trials, each patient
antithrombotic therapy for STEMI, and parenteral thera- who was assigned to the aspiration arm underwent
py is one area of greatest change in the 2009 focused thrombectomy, regardless of the extent of thrombus or
guideline update. Based on the HORIZONS-AMI trial, duration of MI; the writing committee thus included the
which compared the direct-thrombin inhibitor, caveat that it is unclear whether manual aspiration is
bivalirudin, to unfractionated heparin plus GP IIb/IIIa helpful in patients with small thrombus burdens or terri-
inhibitor, bivalirudin is now included as an additional tories of infarct, or for those patients in whom ischemic
class I recommendation for anticoagulant therapy in pri- time is long.
mary PCI, providing clinicians with a new therapy option Stent selection continues to be an important decision
with proven efficacy. Although patients assigned to for clinicians performing primary PCI in the setting of
bivalirudin demonstrated a similar 1-year rate of com- STEMI, particularly because frequently, little historical
bined death, MI, ischemic target vessel revascularization clinical information about the STEMI patient is available
(TVR), and stroke to those assigned to heparin and GP before the primary PCI procedure. Questions then arise
IIb/IIIa inhibitors, bleeding was less common among regarding a patient’s clinical appropriateness for 12
bivalirudin patients, as was all-cause mortality. Because months of DAPT, his or her medical compliance, or
of significant crossover in the trial (ie, many patients in access to DAPT, all of which directly affect the decision to
the bivalirudin arm initially received unfractionated select drug-eluting (DES) or bare-metal (BMS) stents.
heparin, yet still a significant outcomes difference was This issue was readily acknowledged by the writing com-
realized), it is likewise considered acceptable to adminis- mittee, which advocates avoiding DES placement in any
ter bivalirudin for primary PCI in patients who have patient for whom there exists concerns regarding the
already received heparin.4 ability to tolerate prolonged DAPT, as with elective PCI.1
Despite the improved clinical outcomes in HORIZIONS- The writing committee reviewed a number of trials,
AMI for patients receiving bivalirudin, there was concern the largest of which was a prespecified substudy of the
for a statistically significant increase in the number of HORIZIONS-AMI trial in regard to the safety and efficacy
patients experiencing acute stent thrombosis (< 24 of DES compared to BMS in STEMI.9-11 Because safety
hours) when compared to those in the unfractionated appears equivalent and rates of TVR appear slightly lower
heparin arm.4 This difference disappeared after 24 hours with DES as compared to BMS, a new class IIa recom-
and did not affect overall clinical outcomes, but it did mendation was created acknowledging DES as an accept-
draw the attention of the writing committee, who rec- able alternative to BMS. It is also noteworthy that the
ommend a 600-mg load with clopidogrel before primary slight benefit from TVR reduction may not offset the
PCI for patients receiving bivalirudin as a parenteral anti- cost of DES and its concomitant longer DAPT require-
coagulant. ment, particularly when patient variables are often
unknown.
MECHANIC AL THER APIE S
Among the new in-lab procedural recommendations SUMM ARY
made in the 2009 focused update, much attention was The 2009 Focused Update for the Management of
paid to the technique of thrombus aspiration, as well as Patients with ST-Elevation Myocardial Infarction is an
stent selection. important, timely addition to the body of information
Given the fundamental role of acute intracoronary used to provide competent and appropriate patient care.
32 I CARDIAC INTERVENTIONS TODAY I JANUARY/FEBRUARY 2010
COVER STORY
guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coro-
The document incorporates information that is relevant, nary intervention (updating the 2005 guideline and 2007 focused update): a report of the
up-to-date, and of sufficient importance to alter practice American College of Cardiology Foundation/American Heart Association Task Force on
Practice Guidelines. J Am Coll Cardiol. 2009;54:2205-2241.
patterns for many cardiologists. ■ 2. Mehilli J, Kastrati A, Schulz S, et al. Abciximab in patients with acute ST-segment-eleva-
tion myocardial infarction undergoing primary percutaneous coronary intervention after
Jeffrey M. Sparling, MD, is an interventional cardiology fel- clopidogrel loading: a randomized double-blind trial. Circulation. 2009;119:1933-1940.
3. Van’t Hof AW, Ten Berg J, Heestermans T, et al. Prehospital initiation of tirofiban in
low at Brigham and Women’s Hospital, Harvard Medical patients with ST-elevation myocardial infarction undergoing primary angioplasty (On-TIME
School in Boston, Massachusetts. He has disclosed that he 2): a multicenter, double-blind randomized controlled trial. Lancet. 2008;372:537-546.
holds no financial interest in any product or manufacturer 4. Stone GW, Witzenbichler B, Guagliumi G, et al. Bivalirudin during primary PCI in acute
myocardial infarction. N Engl J Med. 2008;358:2218-2230.
mentioned herein. Dr. Sparling may be reached at (617) 732- 5. Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with
7144; jsparling@partners.org. acute coronary syndromes. N Engl J Med. 2007;357:2001-2015.
6. Bhatt D. The COGENT Trial. Presented at: 2009 Transcatheter Cardiovascular Therapeutics
Pinak B. Shah, MD, is from the Division of Cardiovascular annual meeting; September 23, 2009; San Francisco, CA.
Medicine at Brigham and Women’s Hospital in Boston, 7. Svilaas T, Vlaar PJ, van der Horst I, et al. Thrombus aspiration during primary percuta-
Massachusetts. He has disclosed that he holds no financial neous intervention. N Engl J Med. 2008;358:557-567.
8. Sardella G, Mancone M, Bucciarelli-Ducci C, et al. Thrombus aspiration during primary
interest in any product or manufacturer mentioned herein. percutaneous coronary intervention improves myocardial reperfusion and reduces infarct
David O. Williams, MD, is from the Division of size: the EXPIRA (thrombectomy with export catheter in infarct-related artery during primary
Cardiovascular Medicine, Department of Medicine at Brigham percutaneous coronary intervention) prospective, randomized trial. J Am Coll Cardiol.
2009;53:309-315.
and Woman’s Hospital, Harvard Medical School in Boston, 9. Pasceri V, Patti G, Speciale G, et al. Meta-analysis of randomized trials on drug-eluting
Massachusetts. He has disclosed that he holds no financial stents for treatment of acute myocardial infarction. Am Heart J. 2007;153:749-754.
interest in any product or manufacturer mentioned herein. Dr. 10. Kastrati A, Dibra A, Spaulding C, et al. Meta-analysis of randomized trials on drug-elut-
ing stents vs. bare-metal stents in patients with acute myocardial infarction. Eur Heart J.
Williams may be reached at dowilliams@partners.org. 2007;28:2706-2713.
11. De Luca G, Stone GW, Suryapranta H, et al. Efficacy and safety of drug-eluting stents in
1. Kushner FG, Hand M, Smith SC Jr, et al. 2009 Focused Updates: ACC/AHA guidelines for ST-segment elevation myocardial infarction: a meta-analysis of randomized trials. Int J
the management of patients with ST-elevation myocardial infarction (updating the 2005 Cardiol. 2009;133:213-222.
You might also like
- Asepsis Antisepsis and Skin PreparationDocument6 pagesAsepsis Antisepsis and Skin PreparationDavid Tritono Di BallastrossNo ratings yet
- 2014 Changes in NSTE-ACSDocument4 pages2014 Changes in NSTE-ACSnbnbNo ratings yet
- Diabetes With Coronary Disease - A Moving Target Amid Evolving Therapies?Document3 pagesDiabetes With Coronary Disease - A Moving Target Amid Evolving Therapies?Aldy PratamaNo ratings yet
- What Are Optimal P2Y12 Inhibitor and Schedule of Administration in Patients With Acute Coronary Syndrome?Document10 pagesWhat Are Optimal P2Y12 Inhibitor and Schedule of Administration in Patients With Acute Coronary Syndrome?david1086No ratings yet
- Adding CABG To The Dual Antiplatelet Salad: Editorial CommentDocument3 pagesAdding CABG To The Dual Antiplatelet Salad: Editorial CommentVassili CrispiNo ratings yet
- Acuity TrialDocument10 pagesAcuity TrialAhsan KhanNo ratings yet
- Brodie 2000Document6 pagesBrodie 2000SuryaNo ratings yet
- Evidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Document11 pagesEvidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Edgar PazNo ratings yet
- 2009.-Prasugrel in Clinical PracticeDocument3 pages2009.-Prasugrel in Clinical Practicetristan9454No ratings yet
- White 2012 Champion PooledDocument13 pagesWhite 2012 Champion PooledRadu CiprianNo ratings yet
- PCI in Acute ST-elevation Myocardial Infarction (STEMI) : Reference - Ids - Tool - Tip Reference - IdsDocument5 pagesPCI in Acute ST-elevation Myocardial Infarction (STEMI) : Reference - Ids - Tool - Tip Reference - IdsfiraNo ratings yet
- 2015 ACC/AHA/SCAI Focused Update On Primary PCI For Patients With STEMIDocument8 pages2015 ACC/AHA/SCAI Focused Update On Primary PCI For Patients With STEMIrina1511No ratings yet
- CDT 08 05 647Document16 pagesCDT 08 05 647david1086No ratings yet
- Should B-Blockers Still Be Routine After Myocardial Infarction?Document6 pagesShould B-Blockers Still Be Routine After Myocardial Infarction?Raul GascueñaNo ratings yet
- Antithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextDocument12 pagesAntithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextenviNo ratings yet
- 1 s2.0 S000649712034115X MainDocument7 pages1 s2.0 S000649712034115X MainretnoNo ratings yet
- Isi BukuDocument183 pagesIsi BukuHayat Hamzah DawiNo ratings yet
- MainDocument1 pageMainDarimotu MankogulsNo ratings yet
- Beta Blockers Vs Calcium Channel Blockers White Paper 20190913Document3 pagesBeta Blockers Vs Calcium Channel Blockers White Paper 20190913mohammedyosif76No ratings yet
- Acs 37 001Document8 pagesAcs 37 001Luis Rafael Suárez U.No ratings yet
- Aspiration Thrombectomy For Acute ST-Elevation Myocardial Infarction: Literature ReviewDocument9 pagesAspiration Thrombectomy For Acute ST-Elevation Myocardial Infarction: Literature ReviewArdiana FirdausNo ratings yet
- 2510 FullDocument11 pages2510 FullTommy WidjayaNo ratings yet
- Fondaparinux in Acute Coronary Syndromes CA5068 Admin OnlyDocument9 pagesFondaparinux in Acute Coronary Syndromes CA5068 Admin OnlynaeamzNo ratings yet
- Pegasus TIMI 54 TrialDocument13 pagesPegasus TIMI 54 TrialIsaac Aaron Enriquez MonsalvoNo ratings yet
- Doacs in Patients With Mitral Stenosis and Atrial FibrillationDocument3 pagesDoacs in Patients With Mitral Stenosis and Atrial FibrillationNasriNo ratings yet
- Treatment Angina Where Are WeDocument16 pagesTreatment Angina Where Are WeFitra AlfaniNo ratings yet
- 1 s2.0 S0002870316000156 MainDocument9 pages1 s2.0 S0002870316000156 MainSaid Qadaru ANo ratings yet
- J Jcin 2023 01 366Document15 pagesJ Jcin 2023 01 366Kardiologi ManadoNo ratings yet
- Combining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHADocument7 pagesCombining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHADrHellenNo ratings yet
- Prasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesDocument15 pagesPrasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesDito LopezNo ratings yet
- Thesis On Acute Coronary SyndromeDocument5 pagesThesis On Acute Coronary Syndromejum1p0tonip3100% (2)
- Significant Early In-Hospital Benefit Was Seen. Clopidogrel Is Prefferd ToDocument8 pagesSignificant Early In-Hospital Benefit Was Seen. Clopidogrel Is Prefferd TogilnifNo ratings yet
- Disminucion de Lípidos en Sindrome Coronario Agudo. Nicholls S 2018Document2 pagesDisminucion de Lípidos en Sindrome Coronario Agudo. Nicholls S 2018Tony Miguel Saba SabaNo ratings yet
- Furtado 2016Document10 pagesFurtado 2016zzzzNo ratings yet
- Acs 07 04 506Document10 pagesAcs 07 04 506Mohammed ThabtNo ratings yet
- De Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IDocument43 pagesDe Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IAkhmad HidayatNo ratings yet
- 112294Document32 pages112294Ivan FirmansyahNo ratings yet
- Consesus Acute Coronary Taiwan-2018Document10 pagesConsesus Acute Coronary Taiwan-2018Gabriela Catana TurcuNo ratings yet
- Evidence-Based College of Chest Physicians: American New Antithrombotic DrugsDocument25 pagesEvidence-Based College of Chest Physicians: American New Antithrombotic DrugsDiego Fernando Escobar GarciaNo ratings yet
- European J of Heart Fail - 2021 - Greene - Another Reason To Embrace Quadruple Medical Therapy For Heart FailureDocument4 pagesEuropean J of Heart Fail - 2021 - Greene - Another Reason To Embrace Quadruple Medical Therapy For Heart FailureSrinivas PingaliNo ratings yet
- ESCAPE Study - JAMA 2005Document9 pagesESCAPE Study - JAMA 2005MICHAEL AMARILLO CORREANo ratings yet
- DabigatranDocument12 pagesDabigatranAdityaSaskaraNo ratings yet
- The Pulmonary Artery Catheter: Is It Still Alive?: ReviewDocument5 pagesThe Pulmonary Artery Catheter: Is It Still Alive?: ReviewAttilio Del RossoNo ratings yet
- Platelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionDocument9 pagesPlatelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionJanuar RezkyNo ratings yet
- Ticagrelor Vs Clopidogrel Clinical Outcomes in Stelevation Myocardial Infarction Patients March 2023 0716017862 7840249Document4 pagesTicagrelor Vs Clopidogrel Clinical Outcomes in Stelevation Myocardial Infarction Patients March 2023 0716017862 7840249Atul DwivediNo ratings yet
- 996 4398 3 PBDocument7 pages996 4398 3 PBM. PurnomoNo ratings yet
- 2013 ACCF/AHA Guideline For The Management of ST-Elevation Myocardial InfarctionDocument126 pages2013 ACCF/AHA Guideline For The Management of ST-Elevation Myocardial InfarctionDr Edi HidayatNo ratings yet
- 1 s2.0 S2405500X22006697 MainDocument12 pages1 s2.0 S2405500X22006697 MainOttofianus Alvedo Hewick KalangiNo ratings yet
- Year in NSTEMIDocument14 pagesYear in NSTEMILiviuNo ratings yet
- DudjDocument4 pagesDudjsyaiful rinantoNo ratings yet
- JCM 09 01963 v2Document18 pagesJCM 09 01963 v2Jesus MoscosoNo ratings yet
- Jaha 117 007288Document4 pagesJaha 117 007288Alberto PolimeniNo ratings yet
- Antiplatelet Therapy: New Antiplatelet Drugs in PerspectiveDocument4 pagesAntiplatelet Therapy: New Antiplatelet Drugs in Perspectivegeo_mmsNo ratings yet
- Tactics 2001 NejmDocument9 pagesTactics 2001 NejmGustavo Reyes QuezadaNo ratings yet
- 1 s2.0 S0735109716003995 MainDocument2 pages1 s2.0 S0735109716003995 MaintopanNo ratings yet
- Braunwalds PCI For AMIDocument44 pagesBraunwalds PCI For AMIusfcards100% (1)
- Managing Stable Ischemic Heart DiseaseDocument3 pagesManaging Stable Ischemic Heart Diseasealikarimiak1347No ratings yet
- Bleeding Is Out, Your Own Blood Is in 2014Document4 pagesBleeding Is Out, Your Own Blood Is in 2014viaereaNo ratings yet
- Antipl - After DischargeDocument8 pagesAntipl - After DischargeNagatzulNo ratings yet
- Cardiology Update 2018 The First QuarterDocument6 pagesCardiology Update 2018 The First QuarterAditya SutarNo ratings yet
- Manual of STEMI InterventionsFrom EverandManual of STEMI InterventionsSameer MehtaNo ratings yet
- Medwave 2018 07 E7354 PDFDocument7 pagesMedwave 2018 07 E7354 PDFMarceloNo ratings yet
- East FeedingDocument5 pagesEast FeedingJeya vanithaNo ratings yet
- Rapid Response TeamDocument4 pagesRapid Response TeamMichael SilvaNo ratings yet
- Ahs Org OrgchartDocument2 pagesAhs Org OrgchartДрагослав БјелицаNo ratings yet
- Electrocardiographic Predictors of Incident Atrial Fibrillation - DavidDocument6 pagesElectrocardiographic Predictors of Incident Atrial Fibrillation - DavidDavid Jimmy Kurniawan RejosaputroNo ratings yet
- Biocide in WastewaterDocument19 pagesBiocide in WastewaterJohn SmithNo ratings yet
- Neonatal Mechanical Ventilation Predictors of Mortality and OutcomesDocument8 pagesNeonatal Mechanical Ventilation Predictors of Mortality and OutcomesAthenaeum Scientific PublishersNo ratings yet
- Natural Benefits - EnglishDocument124 pagesNatural Benefits - EnglishNaveen SinghNo ratings yet
- UrapidilDocument11 pagesUrapidilFrancesco LucianiNo ratings yet
- Icope Infographic FullDocument1 pageIcope Infographic Fulljon Torres100% (1)
- Updates and Management Algorithm For Neuroendocrine Tumors of The Uterine CervixDocument10 pagesUpdates and Management Algorithm For Neuroendocrine Tumors of The Uterine CervixdosiNo ratings yet
- AYUSHMAN BHARAT Seminar SlidesDocument42 pagesAYUSHMAN BHARAT Seminar Slidesgilbert2691No ratings yet
- Principles of Drug Addiction Treatment: A Research-Based GuideDocument44 pagesPrinciples of Drug Addiction Treatment: A Research-Based GuideKrishna RathodNo ratings yet
- Newly Diagnosed GlioblastomaDocument30 pagesNewly Diagnosed GlioblastomaJubairNo ratings yet
- Allysa Marie Silbol Beed I1Document3 pagesAllysa Marie Silbol Beed I1Allysa Marie SilbolNo ratings yet
- Control and RandomizationDocument18 pagesControl and RandomizationRARCHITA SHARMANo ratings yet
- Morton - Critical Care Nursing 10eDocument6 pagesMorton - Critical Care Nursing 10eblue_blood_boy100% (1)
- Xerophtalmia - KhuranaDocument4 pagesXerophtalmia - KhuranaAslesa Wangpathi Pagehgiri100% (1)
- Colegio Gonzalo Jimenez Navas: Individual WorkDocument3 pagesColegio Gonzalo Jimenez Navas: Individual WorkNicolas Cárdenas maldonadoNo ratings yet
- MIMS Doctor November 2016 RGDocument36 pagesMIMS Doctor November 2016 RGDarmawan HariyantoNo ratings yet
- Giardiasis and FecalysisDocument2 pagesGiardiasis and Fecalysiskmpg11No ratings yet
- Hashimoto's Triggers-Advanced Reader Copy-V2Document332 pagesHashimoto's Triggers-Advanced Reader Copy-V2Anonymous XiymFuQdF100% (2)
- OrganisationDocument46 pagesOrganisationShreyas Walvekar100% (1)
- AIIMS PG Jan 2015Document50 pagesAIIMS PG Jan 2015AnweshaBoseNo ratings yet
- Biophysical AssessmentDocument9 pagesBiophysical AssessmentSanjeev NambalateNo ratings yet
- OB Review QuestionsDocument15 pagesOB Review QuestionsDavid Hieu NgoNo ratings yet
- 19BMS134 - Divyajeet Singh'Document63 pages19BMS134 - Divyajeet Singh'Divyajeet SinghNo ratings yet
- Suicide in Children and Adolescents Cambridge Child and Adolescent PsychiatryDocument333 pagesSuicide in Children and Adolescents Cambridge Child and Adolescent PsychiatryFlorin Tudose100% (1)
- Naini 2020Document1 pageNaini 2020druzair007No ratings yet