Professional Documents
Culture Documents
OPHTHA 8.0 Neuro Ophthalmology Fundamentals Dr. Atienza
OPHTHA 8.0 Neuro Ophthalmology Fundamentals Dr. Atienza
Uploaded by
Maria Gracia YamsonCopyright:
Available Formats
You might also like
- Sensation and Perception Second Edition Ebook PDF VersionDocument61 pagesSensation and Perception Second Edition Ebook PDF Versioncalvin.glahn512100% (44)
- Wipro Brand Manual Lite VersionDocument54 pagesWipro Brand Manual Lite VersionFrank AntonyNo ratings yet
- Digital Matte Painting: Our Experts This IssueDocument5 pagesDigital Matte Painting: Our Experts This IssueacsamsonNo ratings yet
- The Special SensesDocument34 pagesThe Special SensespuchioNo ratings yet
- Part1 - Eye - DV (7 Files Merged)Document127 pagesPart1 - Eye - DV (7 Files Merged)Matthew MalekNo ratings yet
- Visual Pathway - Neurology - Medbullets Step 1Document5 pagesVisual Pathway - Neurology - Medbullets Step 1Andi.Roem_97No ratings yet
- Joukal (2017) Anatomy of The Human Visual PathwayDocument16 pagesJoukal (2017) Anatomy of The Human Visual PathwaysektemujibNo ratings yet
- NB (047) Vision - Central Visual Pathways 1 Lecture1 DR RadwaelzanatyDocument21 pagesNB (047) Vision - Central Visual Pathways 1 Lecture1 DR RadwaelzanatyZeyad AmrNo ratings yet
- Primary Visual Pathway: LIFE3082 Sensational NeuroscienceDocument27 pagesPrimary Visual Pathway: LIFE3082 Sensational NeuroscienceAngkelova ChristinaNo ratings yet
- Visual SystemDocument37 pagesVisual Systemmalinda100% (1)
- NST IllusionsDocument60 pagesNST IllusionsHoang Nhu NguyenNo ratings yet
- Visual PathwayDocument1 pageVisual PathwayJohn CoxNo ratings yet
- ANATO - Campos VisuaisDocument11 pagesANATO - Campos VisuaishelbertpalmieroNo ratings yet
- CN 1-6Document4 pagesCN 1-6prasvkk20No ratings yet
- Visual Neuroscience Revision QuestionsDocument6 pagesVisual Neuroscience Revision QuestionsAlex MNo ratings yet
- Special Senses Revision Notes (GMC - Sae - Hu)Document15 pagesSpecial Senses Revision Notes (GMC - Sae - Hu)Arrya DSNo ratings yet
- 10 - Accommodation & Pupillary Light ReflexDocument46 pages10 - Accommodation & Pupillary Light ReflexSugumar YathavanNo ratings yet
- Blurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocDocument15 pagesBlurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocRea Dominique CabanillaNo ratings yet
- Class01 - 08 Visual Optics IntroductionDocument13 pagesClass01 - 08 Visual Optics IntroductioncehborrotoNo ratings yet
- 27 Physiology of Visual AnalyzerDocument39 pages27 Physiology of Visual Analyzersiwap34656No ratings yet
- Brain&Behavior by DR - Los BanosDocument9 pagesBrain&Behavior by DR - Los BanosChiqui YumangNo ratings yet
- Embryology, Anatomy, and Physiology of The Afferent Visual PathwayDocument80 pagesEmbryology, Anatomy, and Physiology of The Afferent Visual PathwayTea Abramia AbramiaNo ratings yet
- Special SensesDocument18 pagesSpecial SensesStella ParkerNo ratings yet
- 0 OphthalmologyDocument12 pages0 OphthalmologyParsaant SinghNo ratings yet
- The Next Steps in Visual Processing: An Experiment On Colour AdaptationDocument1 pageThe Next Steps in Visual Processing: An Experiment On Colour AdaptationVipin ValsalanNo ratings yet
- (OPHTHA) - 10.1 CaseDiscussion-Dr. AtienzaDocument32 pages(OPHTHA) - 10.1 CaseDiscussion-Dr. AtienzaMaria Gracia YamsonNo ratings yet
- 1 - Newman1973Document16 pages1 - Newman1973Eduardo HernandezNo ratings yet
- Visual PathwayDocument63 pagesVisual Pathwaysenny chapagainNo ratings yet
- 13-2nd, 3rd, 4th & 6th Cranial NervesDocument27 pages13-2nd, 3rd, 4th & 6th Cranial NervesYana CatherineNo ratings yet
- Cerebrum Occipital Lobe Anatomy & Function AtfDocument2 pagesCerebrum Occipital Lobe Anatomy & Function Atfsiti.220010019No ratings yet
- Image Processing Image Processing: CSC CSC 447 447 Instructor: Dr. Shereen Aly Instructor: Dr. Shereen AlyDocument32 pagesImage Processing Image Processing: CSC CSC 447 447 Instructor: Dr. Shereen Aly Instructor: Dr. Shereen AlyyahiaNo ratings yet
- #The Pupillary PathwaysDocument2 pages#The Pupillary PathwaysameerabestNo ratings yet
- NeuroophthalmologyDocument4 pagesNeuroophthalmologysarguss14100% (2)
- The Eye Is Made Up of THREE LayersDocument2 pagesThe Eye Is Made Up of THREE LayersMarissa AsimNo ratings yet
- Visual Homework FabianDocument6 pagesVisual Homework FabianVignesh A KNo ratings yet
- Motor Control - Visual SystemDocument32 pagesMotor Control - Visual SystemJanani IyerNo ratings yet
- Geometric Optics: Kyla Mae M. Lagrimas (12-STEM 1)Document3 pagesGeometric Optics: Kyla Mae M. Lagrimas (12-STEM 1)allysa riveraNo ratings yet
- Duchowski chpt2Document10 pagesDuchowski chpt2eimaio karxasNo ratings yet
- Mchirs Real EstateDocument1 pageMchirs Real EstatechristabelbellzdankyesNo ratings yet
- ANAT204 Vision 2011Document18 pagesANAT204 Vision 2011freaky-mario3327No ratings yet
- B05 L8 VisionDocument21 pagesB05 L8 Visionspotifymailhamza12No ratings yet
- VISUAL PATHWAY Lecture AMENDEDDocument27 pagesVISUAL PATHWAY Lecture AMENDEDMarvel NnaemekaNo ratings yet
- Neurology I ReviewerDocument22 pagesNeurology I Reviewerlazyergophile100% (1)
- Visual PathwayDocument5 pagesVisual Pathwayskeleronnn14No ratings yet
- SquintDocument7 pagesSquintMohamed GhanemNo ratings yet
- L11-1434 Vision L1Document63 pagesL11-1434 Vision L1anu982954No ratings yet
- Psych 102 Lecture 5Document35 pagesPsych 102 Lecture 5YunNo ratings yet
- Laporan Kasus - Buta KortikalDocument31 pagesLaporan Kasus - Buta KortikalwadejackNo ratings yet
- Neuro Optha Mariano 6Document6 pagesNeuro Optha Mariano 6Dey SibalNo ratings yet
- NeuroDocument17 pagesNeuroJack Ortega PuruggananNo ratings yet
- VisualDocument3 pagesVisualMelisa HilaireNo ratings yet
- (OPTHA) Lec 5 - RetinaDocument5 pages(OPTHA) Lec 5 - RetinaPatricia ManaliliNo ratings yet
- 1 Online PDFDocument18 pages1 Online PDFFera SherlianaNo ratings yet
- Orbital Apex Syndrome. A ReviewDocument10 pagesOrbital Apex Syndrome. A ReviewAndrés Faúndez TeránNo ratings yet
- Journal Article OA PDFDocument6 pagesJournal Article OA PDFPutu 'yayuk' Widyani WiradiraniNo ratings yet
- 2011 - Binocular Sensory Status and Miscellaneous TestsDocument5 pages2011 - Binocular Sensory Status and Miscellaneous TestsLuis Miguel MartinsNo ratings yet
- Artificial VisionDocument8 pagesArtificial VisionARVINDNo ratings yet
- Review Article: Adaptive Optics For Visual SimulationDocument14 pagesReview Article: Adaptive Optics For Visual SimulationTit fuckerNo ratings yet
- OPHTHA - Review QuizDocument6 pagesOPHTHA - Review QuizADRIAN TIGLAONo ratings yet
- Chapter 4 - Perception and SensationDocument6 pagesChapter 4 - Perception and Sensationecaber.a12343991No ratings yet
- Visual Perception: Insights into Computational Visual ProcessingFrom EverandVisual Perception: Insights into Computational Visual ProcessingNo ratings yet
- Oculopathy: Disproves the orthodox and theoretical bases upon which glasses are so freely prescribed, and puts forward natural remedial methods of treatment for what are sometimes termed incurable visual defectsFrom EverandOculopathy: Disproves the orthodox and theoretical bases upon which glasses are so freely prescribed, and puts forward natural remedial methods of treatment for what are sometimes termed incurable visual defectsNo ratings yet
- Low Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsFrom EverandLow Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsNo ratings yet
- The Strife For Meaning: PhilsophyDocument22 pagesThe Strife For Meaning: PhilsophyMaria Gracia YamsonNo ratings yet
- Fields: Ucsp 1st Quarter - NotesDocument4 pagesFields: Ucsp 1st Quarter - NotesMaria Gracia YamsonNo ratings yet
- Earth and Life - 2ND SemDocument3 pagesEarth and Life - 2ND SemMaria Gracia YamsonNo ratings yet
- 2-Analyzing The Meaning of The Data and Drawing ConclusionsDocument37 pages2-Analyzing The Meaning of The Data and Drawing ConclusionsMaria Gracia YamsonNo ratings yet
- (IM2) 6.6 Sepsis & Septic Shock - DR - ChunguncoDocument13 pages(IM2) 6.6 Sepsis & Septic Shock - DR - ChunguncoMaria Gracia Yamson100% (2)
- (OPHTHA) 7.1-Pediatric Ophthalmology-Strabismus and Amblyopia - Dr. AtienzaDocument14 pages(OPHTHA) 7.1-Pediatric Ophthalmology-Strabismus and Amblyopia - Dr. AtienzaMaria Gracia YamsonNo ratings yet
- (OPHTHA) - 10.1 CaseDiscussion-Dr. AtienzaDocument32 pages(OPHTHA) - 10.1 CaseDiscussion-Dr. AtienzaMaria Gracia YamsonNo ratings yet
- Alzheimers Screening MSEDocument7 pagesAlzheimers Screening MSEMaria Gracia YamsonNo ratings yet
- RAI and Pregnancy OutcomesDocument8 pagesRAI and Pregnancy OutcomesMaria Gracia YamsonNo ratings yet
- Forgotten But Not Gone? A Probable Case of Wet BeriberiDocument6 pagesForgotten But Not Gone? A Probable Case of Wet BeriberiMaria Gracia YamsonNo ratings yet
- MedEthics LE2Document2 pagesMedEthics LE2Maria Gracia YamsonNo ratings yet
- PANTONE® PLASTICS Color System TMDocument3 pagesPANTONE® PLASTICS Color System TMmimjunNo ratings yet
- I4C Brand Guidelines v1.7 22-06-2021Document31 pagesI4C Brand Guidelines v1.7 22-06-2021José Luis Fernandez TorresNo ratings yet
- Question PhotographyDocument6 pagesQuestion PhotographyYumi TV100% (2)
- Principles of ArtsDocument19 pagesPrinciples of ArtsMiles SerranoNo ratings yet
- DR Laser ProtocolDocument26 pagesDR Laser ProtocolKatherinne Meza RamosNo ratings yet
- Introduction To Robot Vision: Ziv Yaniv Computer Aided Interventions and Medical Robotics, Georgetown UniversityDocument28 pagesIntroduction To Robot Vision: Ziv Yaniv Computer Aided Interventions and Medical Robotics, Georgetown UniversityVishnu PriyanNo ratings yet
- The Photoshop Cs5 Pocketguide: Ginormous Knowledge, Pocket-SizedDocument60 pagesThe Photoshop Cs5 Pocketguide: Ginormous Knowledge, Pocket-SizedPatricia BeckerNo ratings yet
- Photography Techniques (Elementary)Document90 pagesPhotography Techniques (Elementary)Truc Nguyen100% (2)
- Lens Quality: MTF, Resolution & ContrastDocument15 pagesLens Quality: MTF, Resolution & ContrastLaurentiu IacobNo ratings yet
- Congenital CATARACTDocument18 pagesCongenital CATARACTMohamad Hafyfy75% (4)
- Remote Sensing and GIS Module: Colour Composite Images and Visual Image InterpretationDocument21 pagesRemote Sensing and GIS Module: Colour Composite Images and Visual Image InterpretationVijaya Ratna MNo ratings yet
- A 1Document5 pagesA 1Budi BeniNo ratings yet
- Digital Image Processing: National University of Sciences and Technology (NUST)Document55 pagesDigital Image Processing: National University of Sciences and Technology (NUST)Muhammad Tehsin RashadNo ratings yet
- Sam GALAXYS21 UltraDocument2 pagesSam GALAXYS21 UltraTeereg VINo ratings yet
- Light: Physics - Grade 8 Hassan JavedDocument31 pagesLight: Physics - Grade 8 Hassan JavedAl Muhanad Al GhafriNo ratings yet
- R.jogi Basic Opthalmology PDFDocument512 pagesR.jogi Basic Opthalmology PDFLuhurulAmriNo ratings yet
- Depo Farmasi EksekutifDocument47 pagesDepo Farmasi EksekutifthitaqaisNo ratings yet
- Wang.2008.Central Serous ChorioretinopathyDocument20 pagesWang.2008.Central Serous ChorioretinopathyRohit GuptaNo ratings yet
- Vastu and Colors PDFDocument2 pagesVastu and Colors PDFSameera BommisettyNo ratings yet
- A3 Edge Digital Mapping CameraDocument3 pagesA3 Edge Digital Mapping CameraCarlos LuboNo ratings yet
- Pigments Dyes Product Range2015Document29 pagesPigments Dyes Product Range2015Badre AalamNo ratings yet
- Eye DiseasesDocument2 pagesEye DiseasesRaju ShresthaNo ratings yet
- Paleta CuloriDocument8 pagesPaleta CuloriAlexNeo AlexNo ratings yet
- Introduction To Understanding ColorDocument3 pagesIntroduction To Understanding ColorJorge Romero100% (1)
- Symmetrical BalanceDocument4 pagesSymmetrical Balanceapi-279436017No ratings yet
- Visual ImpairmentDocument26 pagesVisual ImpairmentMelody MejiaNo ratings yet
- Step-By-Step Guide To Painting LM-BS004Document58 pagesStep-By-Step Guide To Painting LM-BS004Silverio JuniorNo ratings yet
OPHTHA 8.0 Neuro Ophthalmology Fundamentals Dr. Atienza
OPHTHA 8.0 Neuro Ophthalmology Fundamentals Dr. Atienza
Uploaded by
Maria Gracia YamsonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
OPHTHA 8.0 Neuro Ophthalmology Fundamentals Dr. Atienza
OPHTHA 8.0 Neuro Ophthalmology Fundamentals Dr. Atienza
Uploaded by
Maria Gracia YamsonCopyright:
Available Formats
NEURO-OPHTHALMOLOGY FUNDAMENTALS OPTHALMOLOGY
Dr. Noel de Jesus Atienza
March 17, 2021 8.0
Outline VISUAL PATHWAY
I. Neuro-Ophthalmology Fundamentals
II. Confrontation Test
III. Optic Nerve
IV. Optic Chiasm
V. Retrochiasmatic Visual Pathway
VI. The pupils
VII. Cranial Nerve Palsies
LEGEND
Book Recording Previous Trans Must know
Important Concept
References:
1. PowerPoint Lecture
2. Upper Batch trans
I. NEURO-OPHTHALMOLOGY
Figure 2. The Visual Pathway. Light passes through the lens
and reaches the retina, where the formed image is reversed and
inverted. Axons leaving the retina forms the optic nerve. Fibers
will then pass through the optic chiasm where the nasal side of
the optic nerve would decussate to the contralateral optic tract
while the temporal side of the optic nerve would remain on the
ipsilateral optic tract. Axons in the optic tracts will synapse in
the lateral geniculate nucleus (LGN) of the thalamus. Fibers
from the LGN would then be optic radiations until it eventually
synapses with the primary visual cortex.
• Summary of conscious vision perception
o Retina → Optic Nerve → Optic Chiasm →
Optic Tract → Lateral Geniculate Body →
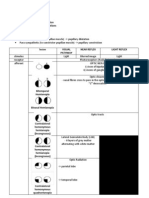
Figure 1. Visual Field Defects. (a) Hemianopsia, (b) Optic Radiation → Primary Visual Cortex
Quadrantanopia, and (c) Scotoma.
• Additional pathways
• Specialty dealing with the problems of the Optic nerve. o Retina → Optic Nerve → Optic Chiasm →
• Could be the first to diagnose tumors, strokes, and Optic Tract → Pretectal Area and Superior
small lesions in the brain (multiple sclerosis, Colliculus
degenerative brain disease). ▪ Pupillary Light Reflex
• Deals with CN II, III, IV, V, VI, VII, and IX. ▪ Eye movements towards visual
• Use of CT scans and MRI to corroborate and identify stimuli
suspicious brain lesions.
How to identify if a lesion is Glaucomatous vs.
Neurological?
• Neurologic problems have a vertical line (in
cases like hemianopia wherein whole left or right
visual field is lost).
• Glaucomatous lesion usually horizontal line
(defects are seen either in up or down visual field).
[INOCENCIO] EDITOR: [JARIEL] Page 1 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
VISUAL FIELD DEFECTS • More congruous (more similar in size, shape and
location) – more posterior lesion.
Figure 4. Difference in the visual field affected by lesions in the
optic tract and lateral geniculate nucleus. (NFT: This was
supposed to be an example showing “the more congruous, the
more posterior the lesion” analogy, but as you can see the lesion
in the LGN is more incongruent even though its more posterior.
So idk with doc. It is what it is I guess.)
• Optic Tract Lesions vs. Occipital Lobe Lesions
o Optic Tract – incongruous homonymous
defects
o Occipital lobe – identical defects in each field
(congruous)
Figure 5. Incongruent Homonymous Hemianopsia of a lesion
in the Optic Tract vs. Congruent Homonymous Hemianopsia in
lesions in the Right Occipital Lobe. (NFT: This one is properly
Figure 3. Visual Field Defects. Transection in the different
showing the “more posterior, the more congruent” rule.)
areas of the optic nerve would have different manifestations
depending on the area of the lesion. Correlate with Figure 2.
II. CONFRONTATION TEST
Table 1. Visual Field Defects
• To screen for visual field defects
DEFECT LESION • Finger counting
A Scotoma Retina • Simultaneous finger counting
B Monocular vision loss Optic Nerve • Penlight (for patients who only have light perception)
C Bitemporal Hemianopsia Optic Chiasm • Test set-up
o Test each eye separately.
o Seat the patient 1 meter (3 feet) facing the
D Contralateral Optic Tract
examiner.
Homonymous
o By convention, test the patient’s right eye or
Hemianopsia
whichever is the better eye first.
E
Figure Contralateral
SEQ Figure \*Superior Inferiorinsert
ARABIC 1. Always optic radiation
caption!
o Completely occlude the patient’s other eye
How? Right click the image and look (Temporal
Quadrantanopia for “Insert Caption”.
lobe)
Italicized caption liftedInferior
from [insert reference]. that is not being tested.
F Contralateral Superior optic radiation
o The examiner must close the eye that is
Quadrantanopia (Parietal lobe)
directly opposite the patient’s occluded eye.
K Contralateral Occipital Lobe
▪ For example: to test the patient’s
Homonymous
right eye, the patient’s left eye and
Hemianopsia with
the examiner’s right eye must be
Macular sparing
covered.
o Ask the patient to focus on a target in a
• Hemianopsia should have intact visual acuity in the
straight gaze position (example, the
spared visual field. examiner’s nose)
• Lesions that are:
o Anterior to the optic chiasm – Unilateral
o At the chiasm – Bitemporal Hemianopsia
o Posterior to the chiasm – Contralateral
Hemianopia or Quadrantanopia
[INOCENCIO] EDITOR: [JARIEL] Page 2 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
Figure 7. Optic disc edema. Left image: Elevated disc with
indistinct disc and cup borders. Right image: severe papilledema
Figure 6. The Confrontation Test. It may be caused by hypertensive retinopathy grade 4.
III. THE OPTIC NERVE OPTIC ATROPHY
• Features of optic neuropathy • Non-specific response to optic nerve damage from
o Reduced visual acuity any cause including retinal diseases such as:
o Afferent pupillary defect o retinitis pigmentosa and CRAO
o Poor color vision • May be a sign of prior disc edema.
o Optic disc changes • May be a late sign of compressive optic
o Visual field defect neuropathy.
• Very bad lesions presenting immediately.
• Optic nerve in the canal is most susceptible to
damage.
• Axons can be dysfunctional long before the optic nerve
becomes atrophic.
OPTIC DISC EDEMA
• Predominantly in diseases directly affecting the Figure 8. Optic Atrophy. Pale disc but with distinct disc border.
anterior part of the optic nerve. Loss of the normal pinkish color of a normal nerve and the cup
o increased intracranial pressure is hardly seen. Patients with optic atrophy usually has
o compression of the intraorbital optic nerve permanent visual loss.
• Papilledema – optic disc edema caused by an
OPTIC HEMORRHAGE
increase in intracranial pressure.
• If located in the nerve fiber layer (NFL) of the retina
o A common cause of neurologic emergency. If
– splinter or flame-shaped hemorrhages.
presenting with headache, we immediately
• If located deeper – disc hemorrhages (appear round
consider doing a CT-scan
and blotchy)
o Generally will not cause BOV, only increase
• Two theories:
in the size of physiologic blind spot.
o Mechanical (shearing forces)
• Other causes include retinal disease (in CRVO),
o Vascular (ischemia)
uveitis, and ocular hypotony.
Important Concept
• It is important to differentiate optic neuritis from
papilledema – both will present with blurred disc
borders, elevated disc margins, tortuous vessels,
possible hemorrhage
• Papilledema – usually normal vision Figure 9. Optic Nerve Hemorrhage. Left image, hemorrhage
involving eyes with well-developed papilledema. Middle and
o In very severe papilledema – florid
Right image showing a localized flame hemorrhage.
hemorrhage and disorganized posterior pole
• Optic neuritis – often associated with blurred OTHER OPTIC NERVE PATHOLOGIES
vision • Optic Neuritis
• Anterior Ischemic Optic Neuropathy
• Papilledema
• Neoplastic Optic Nerve Infiltration
• Neoplastic Optic Nerve Compression
• Nutritional and Optic Neuropathies
• Optic Nerve Trauma
[INOCENCIO] EDITOR: [JARIEL] Page 3 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
• Hereditary Optic Neuropathies
o Leber’s Hereditary Optic Neuropathy
IV. THE OPTIC CHIASM
Figure 13. Bitemporal Hemianopsia. Visual field of a patient
with a lesion affecting the optic chiasm.
OPTIC CHIASM PATHOLOGIES
• Pituitary Adenoma – common in Adults
• Craniopharyngioma – common in Children
• Suprasellar Meningioma
Figure 10. Relationship of the Optic Chiasm to neighboring • Chiasmatic and Optic Nerve Glioma
structures (median sagittal section). Closely related to the base V. RETROCHIASMATIC VISUAL PATHWAY
of the brain THE LATERAL GENICULATE BODY
V. RETROCHIASMATIC VISUAL PATHWAY
• Starts from the Optic tract to Primary visual cortex
• Cerebrovascular disease and tumors are the most
common lesions of the retrochiasmatic visual
pathways.
• Due to their multiple vascular supply, the optic tracts
and LGN are rarely affected by vascular lesions.
• Retrochiasmatic field defects are homonymous.
• In patients above 50 years old, vascular lesions are
Figure 11. Relationship of the Optic Chiasm and the Pituitary the most common (80%) cause of occipital lobe
Gland. conditions.
• The pattern of field defect depends on the affected area
• Chiasmal lesions cause Bitemporal Hemianopsia. of the occipital lobe.
• Early stage – field defects are incomplete and • Macular sparing occurs due to the dual blood supply
asymmetric. of the occipital lobe:
• Later stage – temporal field defects become complete. o Posterior cerebral artery – Main blood
supply
o Branches of the middle cerebral artery –
Supplies the occipital lobe tip.
▪ responsible for the central macular
vision.
NFT: Basically pag tinamaan yung PCA cause
of vascular lesions hindi masasama yung
macula sa magkakaroon ng loss of vision kasi
iba blood supply nya which is MCA = middle
cerebral artery = MaCulA.
Figure 12. Gross and MRI image of a Pituitary Adenoma.
This lesion may cause impingement of the optic chiasm resulting
to Bitemporal Hemianopsia.
Figure 14. Left Homonymous Hemianopsia with Macular
sparing. Lesion is in the PCA, due to the dual blood supply
macula is spared.
[INOCENCIO] EDITOR: [JARIEL] Page 4 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
Figure 15. Homonymous Macular Scotoma. If the lesion is in
the MCA instead of PCA, there will be scotoma.
VI. THE PUPILS
• 20-40% of normal patients have physiologic Anisocoria
(~0.5mm).
• Anisocoria – pupils are asymmetric, one pupil is larger
than the other
o Possible cause is herniation Figure 17. Swinging Flashlight Test. Relative Afferent
Pupillary Defect (RAPD) or Marcus Gunn Pupil, caused by optic
• Pupil size varies according to the sympathetic
nerve lesion or extensive retinal disease.
innervation of the iris dilator muscle.
PUPILLARY LIGHT REFLEX
Figure 18. The difference between CN II (afferent) lesion vs.
CN III (efferent) lesion. Optic nerve lesion there will be loss of
direct pupillary reflex but consensual pupillary reflex is
preserved. Oculomotor nerve lesion there will be loss of
consensual pupillary light reflex.
PUPILLARY NEAR REFLEX
• Triad of
o Convergence
o Accommodation
o Miosis
Figure 16. Pathway of the Pupillary Light Reflex. CNII → • Pupillary constriction accompanying the triad. Not easy
Optic Nerve → Optic Chiasm → Optic Tract → Pretectal Area to elicit especially in children.
and Superior Colliculus → Edinger-Westphal Nucleus → CNIII o Relatively easier to see in blue-eyed
→ Ciliary Ganglion → Pupillary sphincter. Caucasian people.
• When you ask the patient to fixate from distant to near,
• Afferent arm Cranial Nerve II (Optic Nerve)
you also expect the pupils to constrict. So, pupils
• Efferent arm Cranial Nerve III (Oculomotor Nerve)
constrict not just to light stimulus, it also constricts to
near vision.
RELATIVE AFFERENT PUPILLARY DEFECT
• Also known as Marcus Gunn Pupil
ANISOCORIA
• Sensitive and specific sign to detect optic nerve
pathology or large retinal pathology.
Table 2. Anisocoria and their associated conditions
• “Relative” – in relation to the contralateral eye.
DEFECT CONDITION
• “Afferent” – refers to the afferent arm of the pupillary Anisocoria in Dark > Anisocoria in Horner’s
light pathway (optic nerve).
Bright Syndrome
Anisocoria in Bright > Anisocoria in Adie’s Tonic
Dark Pupil
Anisocoria in Dark = Anisocoria in Physiologic
Bright = Anisocoria in Near Response Anisocoria
Anisocoria in Dark = Anisocoria in Light Near
Bright < Anisocoria in Near Response Accommodation
Anisocoria ± CN 3 Palsy Aneurysm
[INOCENCIO] EDITOR: [JARIEL] Page 5 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
PUPILLARY LIGHT NEAR DISSOCIATION
• Miosis at near > miosis to light
• Occurs in lesions that affect the ciliary ganglion or
the midbrain, in which the light reflex pathway is
relatively dorsal compared to the near response
pathway.
• Etiology:
o Adie’s tonic pupil
o Argyll Robertson pupils
o Midbrain tumor or infarct
o CNS degenerative disease
o CNS infection
o DM
o chronic alcoholism
ARGYLL-ROBERTSON PUPIL
• Prostitute’s Pupil
• Accommodates, but does NOT react
• Small (<3mm) pupils, irregular, eccentric
• Difficult to dilate due to iris atrophy Figure 19. Pilocarpine 0.125% test for Adie's Pupil. Even with
diluted pilocarpine the right pupils constricted due to denervation
• Highly suggest tertiary (CNS) syphilis
hypersensitivity.
ADIE’S TONIC PUPILS
• Due to damage of the ciliary ganglion (in the orbit) HORNER’S SYNDROME
or short ciliary nerves
o Short ciliary nerves subserve the near
response more than they subserve the light
reaction (30:1)
• Etiology
o autonomic neuropathy
o after retinal laser photocoagulation
• Young females
• Usually isolated and benign
• In 50% of cases, the contralateral eye may be
involved in the next 10 years.
• Denervation hypersensitivity to 0.125% pilocarpine
(pupils constrict to weak pilocarpine)
• Early stage – pupil is dilated, accommodation is
impaired. Figure 20. The Oculosympathetic Pathway. 1st order
• Later stage – accommodation recovers, incomplete (central): Posterior hypothalamus to C8-T2 → 2nd order (pre-
ganglionic): C8-T2 to superior cervical ganglion → 3rd order
reinnervation of the iris (post-ganglionic): Superior cervical ganglion to the carotid
o Segmental iris constriction (more constricted plexus and CNV1 (trigeminal), which enters the orbit.
than the normal contralateral eye)
o Pupil LND • Due to damage to the oculosympathetic pathway
• ADIE-HOLMES: Adie’s tonic pupil + loss of DTRs. • Triad:
o Ptosis
o Miosis
o Anhydrosis
[INOCENCIO] EDITOR: [JARIEL] Page 6 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
• 40% Trauma – most common cause
• 30% Idiopathic
• 20% Ischemic (diabetic)
• 10% Tumor
CN VI PALSY
Figure 21. Test for Horner's syndrome. 10% cocaine
instillation to confirm it presence. Next, we do 1% Figure 24. Right CN VI palsy. Loss of function of the Lateral
hydroxyamphetamine test to localize the lesion. If the pupil rectus resulting to esotropia (unopposed action of the medial
dilates – pre-ganglionic lesion but if pupils did not change – rectus).
post-ganglionic lesion.
VII. CRANIAL NERVE PALSIES RECALLS/NUGGETS
CN III PALSY
Right homonymous Left optic tract
hemianopsia
Optic disc edema
RAPD Dilate affected eye
when light is shine
through the unaffected eye
Figure 22. Right pupil with complete CN III palsy. "Down and
Out" presentation. Incomplete CN3 palsy Absence of ptosis
PLS STUDY FIGURES 1&2
• Complete or Incomplete AND TABLES 1&2
o Complete – SR, MR, IR, IO, levator
palpebrae superioris and (+) ptosis
o Incomplete – SR, MR, IR, IO with (-) ptosis
• Pupil-involving or Pupil-sparing
o (+) dilated pupil – request for a cranial MRI
to rule out cerebral aneurysm
o Normal pupil – most likely ischemic only
CN IV PALSY
Figure 23. Right CN IV palsy. “Tilted and turned AWAY” from
the lesion.
• Loss of function of the Superior Oblique – eye
torsion
[INOCENCIO] EDITOR: [JARIEL] Page 7 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
APPENDIX
[INOCENCIO] EDITOR: [JARIEL] Page 8 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
NFTH: Study these figures/tables from upper batch trans
[INOCENCIO] EDITOR: [JARIEL] Page 9 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
SUMMARY
I. Neuro-ophthalmology • Specialty dealing with the problems of the Optic nerve.
• Could be the first to diagnose tumors, strokes, and small lesions in the brain (multiple sclerosis,
degenerative brain disease).
• Deals with CN II, III, IV, V, VI, VII, and IX.
• Use of CT scans and MRI to corroborate and identify suspicious brain lesions.
VISUAL PATHWAY
Visual Field Defects. (a)
Hemianopsia, (b) Quadrantanopia, and
(c) Scotoma.
. The Visual Pathway. Light passes through the lens and reaches the retina, where the formed image is
reversed and inverted. Axons leaving the retina forms the optic nerve. Fibers will then pass through the
optic chiasm where the nasal side of the optic nerve would decussate to the contralateral optic tract while
the temporal side of the optic nerve would remain on the ipsilateral optic tract. Axons in the optic tracts will
synapse in the lateral geniculate nucleus (LGN) of the thalamus. Fibers from the LGN would then be
optic radiations until it eventually synapses with the primary visual cortex.
• Summary of conscious vision perception
o Retina → Optic Nerve → Optic Chiasm → Optic Tract → Lateral Geniculate Body →
Optic Radiation → Primary Visual Cortex
• Additional pathways
o Retina → Optic Nerve → Optic Chiasm → Optic Tract → Pretectal Area and
Superior Colliculus
▪ Pupillary Light Reflex
▪ Eye movements towards visual stimuli
Visual Field Defects
DEFECT LESION
A Scotoma Retina
B Monocular vision loss Optic Nerve
C Bitemporal Hemianopsia Optic Chiasm
D Contralateral Optic Tract
Homonymous
Hemianopsia
E Contralateral Superior Inferior optic radiation
Quadrantanopia (Temporal lobe)
F Contralateral Inferior Superior optic radiation
Quadrantanopia (Parietal lobe)
K Contralateral Occipital Lobe
Homonymous
Hemianopsia with Macular
sparing
II. Confrontation test III. To screen for visual field defects
[INOCENCIO] EDITOR: [JARIEL] Page 10 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
IV. Finger counting
V. Simultaneous finger counting
VI. Penlight (for patients who only have light perception)
VII. Test set-up
a. Test each eye separately.
b. Seat the patient 1 meter (3 feet) facing the examiner.
c. By convention, test the patient’s right eye or whichever is the better eye first.
d. Completely occlude the patient’s other eye that is not being tested.
e. The examiner must close the eye that is directly opposite the patient’s occluded eye.
i. For example: to test the patient’s right eye, the patient’s left eye and the
examiner’s right eye must be covered.
f. Ask the patient to focus on a target in a straight gaze position (example, the examiner’s
nose)
III. Optic nerve • Features of optic neuropathy
o Reduced visual acuity
o Afferent pupillary defect
o Poor color vision
o Optic disc changes
o Visual field defect
• Very bad lesions presenting immediately.
• Optic nerve in the canal is most susceptible to damage.
• Axons can be dysfunctional long before the optic nerve becomes atrophic.
Optic Disc Edema • Predominantly in diseases directly affecting the anterior part of the optic nerve.
o increased intracranial pressure
o compression of the intraorbital optic nerve
• Papilledema – optic disc edema caused by an increase in intracranial pressure.
o A common cause of neurologic emergency. If presenting with headache, we
immediately consider doing a CT-scan
o Generally will not cause BOV, only increase in the size of physiologic blind spot.
• Other causes include retinal disease (in CRVO), uveitis, and ocular hypotony.
Optic Atrophy • Non-specific response to optic nerve damage from any cause including retinal diseases such
as:
o retinitis pigmentosa and CRAO
• May be a sign of prior disc edema.
• May be a late sign of compressive optic neuropathy.
Optic Hemorrhage • If located in the nerve fiber layer (NFL) of the retina – splinter or flame-shaped
hemorrhages.
• If located deeper – disc hemorrhages (appear round and blotchy)
• Two theories:
o Mechanical (shearing forces)
o Vascular (ischemia)
Optic nerve pathologies • Optic Neuritis
• Anterior Ischemic Optic Neuropathy
• Papilledema
• Neoplastic Optic Nerve Infiltration
• Neoplastic Optic Nerve Compression
• Nutritional and Optic Neuropathies
• Optic Nerve Trauma
• Hereditary Optic Neuropathies
o Leber’s Hereditary Optic Neuropathy
IV. Optic Chiasm • Chiasmal lesions cause Bitemporal Hemianopsia.
• Early stage – field defects are incomplete and asymmetric.
• Later stage – temporal field defects become complete.
• Pituitary adenoma – common in adults
• Craniopharyngioma – common in children
[INOCENCIO] EDITOR: [JARIEL] Page 11 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
• Suprasellar Meningioma
• Chiasmatic and Optic Nerve Glioma
V. Retrochiasmatic Visual Pathway • Starts from the Optic tract to Primary visual cortex
• Cerebrovascular disease and tumors are the most common lesions of the retrochiasmatic
visual pathways.
• Due to their multiple vascular supply, the optic tracts and LGN are rarely affected by vascular
lesions.
• Retrochiasmatic field defects are homonymous.
• In patients above 50 years old, vascular lesions are the most common (80%) cause of
occipital lobe conditions.
• The pattern of field defect depends on the affected area of the occipital lobe.
• Macular sparing occurs due to the dual blood supply of the occipital lobe:
o Posterior cerebral artery – Main blood supply
o Branches of the middle cerebral artery – Supplies the occipital lobe tip.
▪ responsible for the central macular vision.
VI. The pupils • 20-40% of normal patients have physiologic Anisocoria (~0.5mm).
• Anisocoria – pupils are asymmetric, one pupil is larger than the other
o Possible cause is herniation
• Pupil size varies according to the sympathetic innervation of the iris dilator muscle.
Pupillary Light Reflex Pathway of the Pupillary Light Reflex. CNII → Optic
Nerve → Optic Chiasm → Optic Tract → Pretectal
Area and Superior Colliculus → Edinger-Westphal
Nucleus → CNIII → Ciliary Ganglion → Pupillary
sphincter.
• Afferent arm Cranial Nerve II (Optic
Nerve)
• Efferent arm Cranial Nerve III
(Oculomotor Nerve)
Relative Afferent Pupillary Defect • Also known as Marcus Gunn Pupil
• Sensitive and specific sign to detect optic
nerve pathology or large retinal
pathology.
• “Relative” – in relation to the contralateral
eye.
• “Afferent” – refers to the afferent arm of the
pupillary light pathway (optic nerve).
Swinging Flashlight Test. Relative Afferent
Pupillary Defect (RAPD) or Marcus Gunn Pupil,
caused by optic nerve lesion or extensive retinal The difference between CN II (afferent) lesion vs.
disease. CN III (efferent) lesion. Optic nerve lesion there will
be loss of direct pupillary reflex but consensual
pupillary reflex is preserved. Oculomotor nerve lesion
there will be loss of consensual pupillary light reflex.
Pupillary Near reflex • Triad of Convergence, Accommodation, and Miosis.
• Pupillary constriction accompanying the triad. Not easy to elicit especially in children.
o Relatively easier to see in blue-eyed Caucasian people.
[INOCENCIO] EDITOR: [JARIEL] Page 12 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
• When you ask the patient to fixate from distant to near, you also expect the pupils to constrict.
So, pupils constrict not just to light stimulus, it also constricts•to near vision.
Anisocoria DEFECT CONDITION
Anisocoria in Dark > Anisocoria in Bright Horner’s
Syndrome
Anisocoria in Bright > Anisocoria in Dark Adie’s Tonic Pupil
Anisocoria in Dark = Anisocoria in Bright = Physiologic
Anisocoria in Near Response Anisocoria
Anisocoria in Dark = Anisocoria in Bright < Light Near
Anisocoria in Near Response Accommodation
Anisocoria ± CN 3 Palsy Aneurysm
Pupillary light near dissociation • Miosis at near > miosis to light
• Occurs in lesions that affect the ciliary ganglion or the midbrain, in which the light reflex
pathway is relatively dorsal compared to the near response pathway.
• Etiology:
o Adie’s tonic pupil
o Argyll Robertson pupils
o Midbrain tumor or infarct
o CNS degenerative disease
o CNS infection
o DM
o chronic alcoholism
ARGYLL-ROBERTSON PUPIL • Prostitute’s Pupil
• Accommodates, but does NOT react
• Small (<3mm) pupils, irregular, eccentric
• Difficult to dilate due to iris atrophy
• Highly suggest tertiary (CNS) syphilis
ADIE’S TONIC PUPILS • Due to damage of the ciliary ganglion (in the orbit) or short ciliary nerves
o Short ciliary nerves subserve the near response more than they subserve the light
reaction (30:1)
• Etiology
o autonomic neuropathy
o after retinal laser photocoagulation
• Young females
• Usually isolated and benign
• In 50% of cases, the contralateral eye may be involved in the next 10 years.
• Denervation hypersensitivity to 0.125% pilocarpine (pupils constrict to weak pilocarpine)
• Early stage – pupil is dilated, accommodation is impaired.
• Later stage – accommodation recovers, incomplete reinnervation of the iris
o Segmental iris constriction (more constricted than the normal contralateral eye)
o Pupil LND
• ADIE-HOLMES: Adie’s tonic pupil + loss of DTRs
Horner’s Syndrome • Due to damage to the oculosympathetic pathway
• Triad:
o Ptosis
o Miosis
o Anhydrosis
The Oculosympathetic Pathway. 1st
order (central): Posterior hypothalamus to
C8-T2 → 2nd order (pre-ganglionic): C8-T2
to superior cervical ganglion → 3rd order
(post-ganglionic): Superior cervical ganglion Figure 25. Test for Horner's syndrome. 10% cocaine
to the carotid plexus and CNV1 (trigeminal), instillation to confirm it presence. Next, we do 1%
which enters the orbit. hydroxyamphetamine test to localize the lesion. If the pupil
[INOCENCIO] EDITOR: [JARIEL] Page 13 of 14
OTORHINOLARYNGOLOGY BASIC EYE EXAM LECTURE 8.0
dilates – pre-ganglionic lesion but if pupils did not
change – post-ganglionic lesion.
VIII. Cranial Nerve Palsies • Complete or Incomplete
o Complete – SR, MR, IR, IO, levator
CN III Palsy
palpebrae superioris and (+) ptosis
o Incomplete – SR, MR, IR, IO with (-)
ptosis
• Pupil-involving or Pupil-sparing
o (+) dilated pupil – request for a cranial
MRI to rule out cerebral aneurysm
o Normal pupil – most likely ischemic
only
Right pupil with complete CN III palsy.
"Down and Out" presentation.
CN IV Palsy • Loss of function of the Superior Oblique – eye
torsion
• 40% Trauma – most common cause
• 30% Idiopathic
• 20% Ischemic (diabetic)
• 10% Tumor
. Right CN IV palsy. “Tilted and turned
AWAY” from the lesion.
CN VI Palsy Right CN VI palsy. Loss of function of the Lateral rectus
resulting to esotropia (unopposed action of the medial
rectus).
[INOCENCIO] EDITOR: [JARIEL] Page 14 of 14
You might also like
- Sensation and Perception Second Edition Ebook PDF VersionDocument61 pagesSensation and Perception Second Edition Ebook PDF Versioncalvin.glahn512100% (44)
- Wipro Brand Manual Lite VersionDocument54 pagesWipro Brand Manual Lite VersionFrank AntonyNo ratings yet
- Digital Matte Painting: Our Experts This IssueDocument5 pagesDigital Matte Painting: Our Experts This IssueacsamsonNo ratings yet
- The Special SensesDocument34 pagesThe Special SensespuchioNo ratings yet
- Part1 - Eye - DV (7 Files Merged)Document127 pagesPart1 - Eye - DV (7 Files Merged)Matthew MalekNo ratings yet
- Visual Pathway - Neurology - Medbullets Step 1Document5 pagesVisual Pathway - Neurology - Medbullets Step 1Andi.Roem_97No ratings yet
- Joukal (2017) Anatomy of The Human Visual PathwayDocument16 pagesJoukal (2017) Anatomy of The Human Visual PathwaysektemujibNo ratings yet
- NB (047) Vision - Central Visual Pathways 1 Lecture1 DR RadwaelzanatyDocument21 pagesNB (047) Vision - Central Visual Pathways 1 Lecture1 DR RadwaelzanatyZeyad AmrNo ratings yet
- Primary Visual Pathway: LIFE3082 Sensational NeuroscienceDocument27 pagesPrimary Visual Pathway: LIFE3082 Sensational NeuroscienceAngkelova ChristinaNo ratings yet
- Visual SystemDocument37 pagesVisual Systemmalinda100% (1)
- NST IllusionsDocument60 pagesNST IllusionsHoang Nhu NguyenNo ratings yet
- Visual PathwayDocument1 pageVisual PathwayJohn CoxNo ratings yet
- ANATO - Campos VisuaisDocument11 pagesANATO - Campos VisuaishelbertpalmieroNo ratings yet
- CN 1-6Document4 pagesCN 1-6prasvkk20No ratings yet
- Visual Neuroscience Revision QuestionsDocument6 pagesVisual Neuroscience Revision QuestionsAlex MNo ratings yet
- Special Senses Revision Notes (GMC - Sae - Hu)Document15 pagesSpecial Senses Revision Notes (GMC - Sae - Hu)Arrya DSNo ratings yet
- 10 - Accommodation & Pupillary Light ReflexDocument46 pages10 - Accommodation & Pupillary Light ReflexSugumar YathavanNo ratings yet
- Blurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocDocument15 pagesBlurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocRea Dominique CabanillaNo ratings yet
- Class01 - 08 Visual Optics IntroductionDocument13 pagesClass01 - 08 Visual Optics IntroductioncehborrotoNo ratings yet
- 27 Physiology of Visual AnalyzerDocument39 pages27 Physiology of Visual Analyzersiwap34656No ratings yet
- Brain&Behavior by DR - Los BanosDocument9 pagesBrain&Behavior by DR - Los BanosChiqui YumangNo ratings yet
- Embryology, Anatomy, and Physiology of The Afferent Visual PathwayDocument80 pagesEmbryology, Anatomy, and Physiology of The Afferent Visual PathwayTea Abramia AbramiaNo ratings yet
- Special SensesDocument18 pagesSpecial SensesStella ParkerNo ratings yet
- 0 OphthalmologyDocument12 pages0 OphthalmologyParsaant SinghNo ratings yet
- The Next Steps in Visual Processing: An Experiment On Colour AdaptationDocument1 pageThe Next Steps in Visual Processing: An Experiment On Colour AdaptationVipin ValsalanNo ratings yet
- (OPHTHA) - 10.1 CaseDiscussion-Dr. AtienzaDocument32 pages(OPHTHA) - 10.1 CaseDiscussion-Dr. AtienzaMaria Gracia YamsonNo ratings yet
- 1 - Newman1973Document16 pages1 - Newman1973Eduardo HernandezNo ratings yet
- Visual PathwayDocument63 pagesVisual Pathwaysenny chapagainNo ratings yet
- 13-2nd, 3rd, 4th & 6th Cranial NervesDocument27 pages13-2nd, 3rd, 4th & 6th Cranial NervesYana CatherineNo ratings yet
- Cerebrum Occipital Lobe Anatomy & Function AtfDocument2 pagesCerebrum Occipital Lobe Anatomy & Function Atfsiti.220010019No ratings yet
- Image Processing Image Processing: CSC CSC 447 447 Instructor: Dr. Shereen Aly Instructor: Dr. Shereen AlyDocument32 pagesImage Processing Image Processing: CSC CSC 447 447 Instructor: Dr. Shereen Aly Instructor: Dr. Shereen AlyyahiaNo ratings yet
- #The Pupillary PathwaysDocument2 pages#The Pupillary PathwaysameerabestNo ratings yet
- NeuroophthalmologyDocument4 pagesNeuroophthalmologysarguss14100% (2)
- The Eye Is Made Up of THREE LayersDocument2 pagesThe Eye Is Made Up of THREE LayersMarissa AsimNo ratings yet
- Visual Homework FabianDocument6 pagesVisual Homework FabianVignesh A KNo ratings yet
- Motor Control - Visual SystemDocument32 pagesMotor Control - Visual SystemJanani IyerNo ratings yet
- Geometric Optics: Kyla Mae M. Lagrimas (12-STEM 1)Document3 pagesGeometric Optics: Kyla Mae M. Lagrimas (12-STEM 1)allysa riveraNo ratings yet
- Duchowski chpt2Document10 pagesDuchowski chpt2eimaio karxasNo ratings yet
- Mchirs Real EstateDocument1 pageMchirs Real EstatechristabelbellzdankyesNo ratings yet
- ANAT204 Vision 2011Document18 pagesANAT204 Vision 2011freaky-mario3327No ratings yet
- B05 L8 VisionDocument21 pagesB05 L8 Visionspotifymailhamza12No ratings yet
- VISUAL PATHWAY Lecture AMENDEDDocument27 pagesVISUAL PATHWAY Lecture AMENDEDMarvel NnaemekaNo ratings yet
- Neurology I ReviewerDocument22 pagesNeurology I Reviewerlazyergophile100% (1)
- Visual PathwayDocument5 pagesVisual Pathwayskeleronnn14No ratings yet
- SquintDocument7 pagesSquintMohamed GhanemNo ratings yet
- L11-1434 Vision L1Document63 pagesL11-1434 Vision L1anu982954No ratings yet
- Psych 102 Lecture 5Document35 pagesPsych 102 Lecture 5YunNo ratings yet
- Laporan Kasus - Buta KortikalDocument31 pagesLaporan Kasus - Buta KortikalwadejackNo ratings yet
- Neuro Optha Mariano 6Document6 pagesNeuro Optha Mariano 6Dey SibalNo ratings yet
- NeuroDocument17 pagesNeuroJack Ortega PuruggananNo ratings yet
- VisualDocument3 pagesVisualMelisa HilaireNo ratings yet
- (OPTHA) Lec 5 - RetinaDocument5 pages(OPTHA) Lec 5 - RetinaPatricia ManaliliNo ratings yet
- 1 Online PDFDocument18 pages1 Online PDFFera SherlianaNo ratings yet
- Orbital Apex Syndrome. A ReviewDocument10 pagesOrbital Apex Syndrome. A ReviewAndrés Faúndez TeránNo ratings yet
- Journal Article OA PDFDocument6 pagesJournal Article OA PDFPutu 'yayuk' Widyani WiradiraniNo ratings yet
- 2011 - Binocular Sensory Status and Miscellaneous TestsDocument5 pages2011 - Binocular Sensory Status and Miscellaneous TestsLuis Miguel MartinsNo ratings yet
- Artificial VisionDocument8 pagesArtificial VisionARVINDNo ratings yet
- Review Article: Adaptive Optics For Visual SimulationDocument14 pagesReview Article: Adaptive Optics For Visual SimulationTit fuckerNo ratings yet
- OPHTHA - Review QuizDocument6 pagesOPHTHA - Review QuizADRIAN TIGLAONo ratings yet
- Chapter 4 - Perception and SensationDocument6 pagesChapter 4 - Perception and Sensationecaber.a12343991No ratings yet
- Visual Perception: Insights into Computational Visual ProcessingFrom EverandVisual Perception: Insights into Computational Visual ProcessingNo ratings yet
- Oculopathy: Disproves the orthodox and theoretical bases upon which glasses are so freely prescribed, and puts forward natural remedial methods of treatment for what are sometimes termed incurable visual defectsFrom EverandOculopathy: Disproves the orthodox and theoretical bases upon which glasses are so freely prescribed, and puts forward natural remedial methods of treatment for what are sometimes termed incurable visual defectsNo ratings yet
- Low Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsFrom EverandLow Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsNo ratings yet
- The Strife For Meaning: PhilsophyDocument22 pagesThe Strife For Meaning: PhilsophyMaria Gracia YamsonNo ratings yet
- Fields: Ucsp 1st Quarter - NotesDocument4 pagesFields: Ucsp 1st Quarter - NotesMaria Gracia YamsonNo ratings yet
- Earth and Life - 2ND SemDocument3 pagesEarth and Life - 2ND SemMaria Gracia YamsonNo ratings yet
- 2-Analyzing The Meaning of The Data and Drawing ConclusionsDocument37 pages2-Analyzing The Meaning of The Data and Drawing ConclusionsMaria Gracia YamsonNo ratings yet
- (IM2) 6.6 Sepsis & Septic Shock - DR - ChunguncoDocument13 pages(IM2) 6.6 Sepsis & Septic Shock - DR - ChunguncoMaria Gracia Yamson100% (2)
- (OPHTHA) 7.1-Pediatric Ophthalmology-Strabismus and Amblyopia - Dr. AtienzaDocument14 pages(OPHTHA) 7.1-Pediatric Ophthalmology-Strabismus and Amblyopia - Dr. AtienzaMaria Gracia YamsonNo ratings yet
- (OPHTHA) - 10.1 CaseDiscussion-Dr. AtienzaDocument32 pages(OPHTHA) - 10.1 CaseDiscussion-Dr. AtienzaMaria Gracia YamsonNo ratings yet
- Alzheimers Screening MSEDocument7 pagesAlzheimers Screening MSEMaria Gracia YamsonNo ratings yet
- RAI and Pregnancy OutcomesDocument8 pagesRAI and Pregnancy OutcomesMaria Gracia YamsonNo ratings yet
- Forgotten But Not Gone? A Probable Case of Wet BeriberiDocument6 pagesForgotten But Not Gone? A Probable Case of Wet BeriberiMaria Gracia YamsonNo ratings yet
- MedEthics LE2Document2 pagesMedEthics LE2Maria Gracia YamsonNo ratings yet
- PANTONE® PLASTICS Color System TMDocument3 pagesPANTONE® PLASTICS Color System TMmimjunNo ratings yet
- I4C Brand Guidelines v1.7 22-06-2021Document31 pagesI4C Brand Guidelines v1.7 22-06-2021José Luis Fernandez TorresNo ratings yet
- Question PhotographyDocument6 pagesQuestion PhotographyYumi TV100% (2)
- Principles of ArtsDocument19 pagesPrinciples of ArtsMiles SerranoNo ratings yet
- DR Laser ProtocolDocument26 pagesDR Laser ProtocolKatherinne Meza RamosNo ratings yet
- Introduction To Robot Vision: Ziv Yaniv Computer Aided Interventions and Medical Robotics, Georgetown UniversityDocument28 pagesIntroduction To Robot Vision: Ziv Yaniv Computer Aided Interventions and Medical Robotics, Georgetown UniversityVishnu PriyanNo ratings yet
- The Photoshop Cs5 Pocketguide: Ginormous Knowledge, Pocket-SizedDocument60 pagesThe Photoshop Cs5 Pocketguide: Ginormous Knowledge, Pocket-SizedPatricia BeckerNo ratings yet
- Photography Techniques (Elementary)Document90 pagesPhotography Techniques (Elementary)Truc Nguyen100% (2)
- Lens Quality: MTF, Resolution & ContrastDocument15 pagesLens Quality: MTF, Resolution & ContrastLaurentiu IacobNo ratings yet
- Congenital CATARACTDocument18 pagesCongenital CATARACTMohamad Hafyfy75% (4)
- Remote Sensing and GIS Module: Colour Composite Images and Visual Image InterpretationDocument21 pagesRemote Sensing and GIS Module: Colour Composite Images and Visual Image InterpretationVijaya Ratna MNo ratings yet
- A 1Document5 pagesA 1Budi BeniNo ratings yet
- Digital Image Processing: National University of Sciences and Technology (NUST)Document55 pagesDigital Image Processing: National University of Sciences and Technology (NUST)Muhammad Tehsin RashadNo ratings yet
- Sam GALAXYS21 UltraDocument2 pagesSam GALAXYS21 UltraTeereg VINo ratings yet
- Light: Physics - Grade 8 Hassan JavedDocument31 pagesLight: Physics - Grade 8 Hassan JavedAl Muhanad Al GhafriNo ratings yet
- R.jogi Basic Opthalmology PDFDocument512 pagesR.jogi Basic Opthalmology PDFLuhurulAmriNo ratings yet
- Depo Farmasi EksekutifDocument47 pagesDepo Farmasi EksekutifthitaqaisNo ratings yet
- Wang.2008.Central Serous ChorioretinopathyDocument20 pagesWang.2008.Central Serous ChorioretinopathyRohit GuptaNo ratings yet
- Vastu and Colors PDFDocument2 pagesVastu and Colors PDFSameera BommisettyNo ratings yet
- A3 Edge Digital Mapping CameraDocument3 pagesA3 Edge Digital Mapping CameraCarlos LuboNo ratings yet
- Pigments Dyes Product Range2015Document29 pagesPigments Dyes Product Range2015Badre AalamNo ratings yet
- Eye DiseasesDocument2 pagesEye DiseasesRaju ShresthaNo ratings yet
- Paleta CuloriDocument8 pagesPaleta CuloriAlexNeo AlexNo ratings yet
- Introduction To Understanding ColorDocument3 pagesIntroduction To Understanding ColorJorge Romero100% (1)
- Symmetrical BalanceDocument4 pagesSymmetrical Balanceapi-279436017No ratings yet
- Visual ImpairmentDocument26 pagesVisual ImpairmentMelody MejiaNo ratings yet
- Step-By-Step Guide To Painting LM-BS004Document58 pagesStep-By-Step Guide To Painting LM-BS004Silverio JuniorNo ratings yet