Professional Documents
Culture Documents
Aaid Joi D 13 00158
Aaid Joi D 13 00158
Uploaded by
Meta Anjany FirmansyahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aaid Joi D 13 00158
Aaid Joi D 13 00158
Uploaded by
Meta Anjany FirmansyahCopyright:
Available Formats
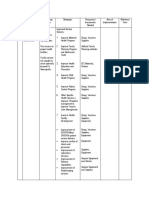
LITERATURE REVIEW
Tranexamic Acid Tamponade to Control Postoperative
Surgical Hemorrhage
Dennis Flanagan, DDS
When preparing for oral surgery, patients taking anticoagulants usually should not discontinue their medication because of the risk of a
thromboembolic event. The therapeutic effect of many anticoagulants is not readily measured, so preoperatively, the surgeon cannot
know the true risk for postoperative hemorrhage. The risk of a thromboembolic event usually outweighs the concerns of controlling
Downloaded from http://meridian.allenpress.com/joi/article-pdf/41/3/e82/2058461/aaid-joi-d-13-00158.pdf by Indonesia user on 07 June 2021
postoperative hemorrhage. Hemophilia patients are also at risk for postoperative bleeding. Single extractions probably do not pose a
serious risk for postoperative hemorrhage. However, when a mucogingival flap is raised in these patients, there may be prolonged
bleeding. Surgical sponges saturated with aqueous tranexamic acid solution and compressed onto the bleeding site with biting pressure
may stop bleeding. Bleeding was stopped in the case example presented here after three 10-minute compressions over 30 minutes in a
patient taking aspirin and clopidogrel for a previous thromboembolic event and a metal coronary stent. The clot formed is very fragile and
is prone to bleeding, so it should not be disturbed. This technique needs to be studied for efficacy.
Key Words: hemorrhage, coagulation, bleeding, bleeding control, local bleeding control, oral bleeding, oral surgery, dental implant,
anticoagulants.
INTRODUCTION cessation of anticoagulant therapy, thus minimizing the risk.6
The decision to stop or bridge anticoagulant therapy for an
T
he implant dentist can be confronted with patients
impending implant surgery is ultimately a clinical decision
who present with anticoagulant therapy for treatment
made by the implant dentist based on the magnitude of the
of various systemic conditions. Warfarin has been the
surgical wound, postoperative hemorrhage considerations, and
most frequently used anticoagulant, being the 21st
the thromboembolic risk. The cessation of anticoagulant,
most common prescription in the United States in 2011.1,2 It is
including aspirin and clopidogrel, may cause thrombosis.7
an anticoagulant for which the expected bleeding can be
These patients may be at the highest risk for a vascular event if
measured by the international normalized ratio (INR), which
anticoagulant therapy is ceased or bridged.7
measures the extrinsic coagulation cascade. This indicates to
Tranexamic acid, trans-4-(aminomethyl)cyclohexanecarbox-
the implant dentist whether patients may need to have the
ylic acid (TA; Cyclokapron, Pfizer, New York, NY; Figure 1) is
dosage of medication reduced to decrease the anticoagulation
derived from lecithin. It has been used systemically for many
so that the surgery will not induce prolonged bleeding. Drugs
years to minimize post- and intraoperative hemorrhage. Topical
with an antiplatelet effect, such as aspirin and clopidogrel
use has not been extensive. With the advent of anticoagulants
(Plavix), are commonly used.3 Tests to monitor their effect are
for which the therapeutic effect cannot be monitored
not widely available. Newer anticoagulants, such as rivaroxiban
conveniently, a topical hemostatic agent may be very beneficial
(Xaroleto) and dabigatran (Pradaxa), are being used more
if cessation or bridging is inappropriate.9
widely.4 Their therapeutic effect is not easily measured for
The aim of this article is to review the topical use of TA to
preoperative consideration.5 The implant dentist may not know
control postoperative bleeding for minor oral surgical proce-
preoperatively which patients will not stop bleeding quickly
dures in patients taking anticoagulant therapy and for whom the
after implant surgery. Cessation of an anticoagulant may have
decision has been made not to cease anticoagulant therapy.10
serious cardiovascular sequelae, such as myocardial infarction
or embolic cerebrovascular stroke.6–9 Cessation may have a 6%
risk for an adverse thromboembolic event.7 Stopping antico-
MATERIALS AND METHODS
agulant therapy should be done only after consultation with
the patient’s physician. Bridging therapy may be instituted Literature search
where low-molecular-weight heparin is administered to tem-
porarily perform the anticoagulant therapy.8 This may be done An electronic literature search was performed using the key
for some patients to allow for postsurgical clotting. Neverthe- word tranexamic acid AND hemorrhage. All addressed non-
less, many patients may undergo minor oral surgery without topical use of TA except one.
Patient usage
Private practice, Willimantic, Conn.
Corresponding author, e-mail: dffdds@comcast.net We included 10 patients who underwent an oral surgical
DOI: 10.1563/AAID-JOI-D-13-00158 procedure including extraction, apically positioned or partial
e82 Vol. XLI / No. Three / 2015
Flanagan
FIGURE 1. Molecular configuration of tranexamic acid—trans-4-
(aminomethyl)cyclohexanecarboxylic acid.
thickness mucogingival flap. All patients had a tamponade of
an aqueous saturated solution of TA. Most bleeding stopped in
Downloaded from http://meridian.allenpress.com/joi/article-pdf/41/3/e82/2058461/aaid-joi-d-13-00158.pdf by Indonesia user on 07 June 2021
10 minutes, and the patients on anticoagulant therapy
bleeding stopped with 1 or 2 additional applications.
CASE EXAMPLE
In 2009, a 51-year-old man with a history of high blood pressure
and cholesterol and cardiac stent surgery 7 years prior (2003),
presented for implant-supported restorative treatment. Clinical
and radiographic examination revealed maxillary right (teeth
Nos. 1–5) and mandibular left partial edentulism (tooth No. 19)
with moderate bone atrophy. Treatment options were dis-
cussed. The remaining teeth were to be restored as well. The
mandibular left premolars were deemed poor to guarded
periodontal, coronal, or endodontic prognosis.
Telephone consultation with his physician revealed that the
patient took the following medications daily: famotidine
besylate (Pepcid) 10 mg, rosuvastatin (Crestor) 10 mg,
ezetimibe (Zetia) 10 mg, lisinopril (Zestril) 20 mg, metoprolol
(Toprol) 100 mg, clopidogrel (Plavix) 75 mg, aspirin 81 mg, and FIGURE 2. One week postoperative healing of example patient.
L-thyroxine (Synthroid) 50 mg. The physician determined that
the patient would tolerate dental implant surgery well. The risk (Imprint, 3M ESPE) impression was made. A porcine collagen
for a thrombosis would be minimized by not discontinuing the matrix (MucoGraft) was placed under the flap to increase the
dual antiplatelet drugs, clopidogrel and aspirin. Implants were thickness of collagenous tissue. Healing caps were placed and
successfully placed at the maxillary right and restored without bleeding was controlled with a local anesthetic infiltration and a
cessation of anticoagulant therapy with no hemorrhagic tea bag compress. No sutures were placed, but a bis-acryl stent
sequellae. The maxillary right implants and restorations was placed. The patient was instructed on postoperative care and
(treatment by D.F.) were placed in 2010 and had been in left in good condition with no bleeding. However, that night, the
successful function for 2 years. patient awoke because of bleeding from the site. He went to a
In 2012, the mandibular left premolars were extracted with
local hospital emergency department for treatment. The
infiltration local anesthesia using articaine (Septocaine). The
physician on duty controlled the bleeding again with moistened
implants were placed flaplessly at the first molar site and
tea bag compression. The next morning, the patient was seen
immediately at the first premolar site, again without discon-
and the site was bleeding again. The stent was removed. A
tinuing the anticoagulant therapy. The premolar extraction
saturated aqueous solution (16%) of TA was made by dissolving
sites were filled with calcium sulfate and covered with collagen
plugs (Salvin) and secured with a 3-0 chromic suture. No TA powder in approximately 10 mL of water and soaking into 2 3
prolonged postoperative bleeding occurred. 2 surgical sponges. The sponges were placed on the surgical site
At second-stage uncover surgery for the left mandible, the and compressed with the patient’s biting pressure for 10 minutes.
anticoagulants were again not stopped. After facial and lingual This was repeated twice. After the third compression, the
infiltration of 1.6 mL articaine (Septcaine) at the No. 19 site, an bleeding stopped completely. The patient was monitored for
approximately 15-mm-long partial-thickness facial surgical flap another 30 minutes, and there was no reoccurrence of bleeding.
with releasing incisions was raised and apically positioned. The The patient was instructed as to home care and was dismissed.
No. 21 implant had adequate attached tissue and did not require He was called 2 hours later, and he reported no bleeding from the
augmentation, and the gingival overgrowth here was removed site. The patient again reported no bleeding from the site 2 days
with a medium-coarse high-speed diamond stone. Abutment later. He subsequently returned 1 week later for follow-up and
analogues were placed, and an open tray polyvinyl siloxane was healing well with no bleeding reoccurrence (Figure 2). Three
Journal of Oral Implantology e83
Tranexamic Acid
weeks later, the fixed partial denture was fitted, adjusted, and reduce patient mortality and can improve symptoms.18,19 Drug-
definitively cemented with resin-modified glass ionomer cement eluting stents are now available, and discontinuing anticoag-
(FujiCem). ulant therapy may be possible with a low risk for serious
complications.19 For coronary stent patients on clopidogrel,
routine platelet function may be monitored, but this can be
DISCUSSION inconvenient and may not improve the clinical results.20 There
Example patient with TA tamponade is no consensus as to the most appropriate anticoagulant
therapy. Aspirin alone may be the best antiplatelet regimen.21
Oral anticoagulant therapy does not contraindicate dental After coronary stent surgery, dual anticoagulant therapy with
implant surgery.6,9 Discontinuing anticoagulant therapy is not clopidogrel and aspirin is well accepted.22 However, with
advisable for minor oral surgery, such as single tooth extraction clopidogrel, there is important patient variability in the
and implant placement. When there are more invasive antiplatelet response.22 These are genetically related and may
procedures such as large flap and autogenous bone grafting, have increased risks for bleeding sequelae.22 These issues may
anticoagulant cessation or bridging therapy may be instituted. affect the potential for dental implant surgery hemorrhage,
Downloaded from http://meridian.allenpress.com/joi/article-pdf/41/3/e82/2058461/aaid-joi-d-13-00158.pdf by Indonesia user on 07 June 2021
Topical agents and compression are generally effective in which may have been at least contributory to the incident
controlling postoperative bleeding in minor sites in these reported here.
patients.9–12 However, there is no definition of a ‘‘minor’’ site.
The extent of anticoagulation in individual patients may vary Clotting mechanism
due to dosage and timing, individual physiologic metabolism,
Thrombogenesis (clotting) is the result of a complex cascade of
or circadian variations. This creates an uncertain physiologic
biological chemical events.23 Generally, platelets become
parameter for the dentist. The above patient had 3 prior
activated by tissue factor released from injury to epithelium.
‘‘minor’’ oral surgeries and no bleeding complications. The
There then occurs a cascade of biochemical reactions by the
uncovery second-stage flap in the left mandible was a slightly
extrinsic and intrinsic pathways that contribute to the
larger surgical wound than the previous surgeries. The stent
conversion of prothrombin to thrombin, which in turn converts
protected the flap wound but did not apply pressure and
fibrinogen to fibrin. Fibrin is then cross-linked to stabilize the
prevented direct contact with the applied tea bags. After the
clot.
stent was removed, the wound was exposed for direct
compression and contact with the TA solution. The patient Pharmacology of TA
may have altered his dosing by inconsistent drug compliance
that resulted in less anticoagulation in the early surgeries and Tranexamic acid (TA) is a derivative of lysine that has been used
more during the last flap surgery. This may have contributed to as a first-line treatment to control bleeding of menorrhagia (at
the bleeding episode that required TA tamponade. least 80 mL blood loss per cycle) and cardiac surgery.24–26 Peak
The polypharmacy in the example patient herein may be of plasma concentration is reached within 1 hour with intravenous
concern. Among other drugs, he was taking famotidine injection with a dose of 10 mg/kg.27,28 After 24 hours, 90% of
(Pepcid), rosuvastatin (Crestor), ezetimibe (Zetia), metoprolol, TA is excreted in the urine, and the elimination half-life is 80
and lisinopril. Famotidine is an H2 receptor antagonist that may minutes.29 Oral administration of 10 to 15 mg/kg produces
rarely induce thrombocytopenia. This patient, however, was not peak plasma concentration within 3 hours.29 Taking TA with
thrombocytopenic. Rosuvastatin is a statin drug that does not food does not reduce or increase gastrointestinal absorption.30
have significant vascular side effects. Its clearance can be Tranexamic acid does accumulate in tissue and joint and
affected by some anticoagulants—clopidogrel not being one of synovial fluid.27,31 Tranexamic acid will pass the placental
those. Ezetimibe inhibits cholesterol intestinal absorption and barrier and be concentrated in breast milk.28,32 Studies have not
rarely induces thrombocytopenia. Metoprolol is a selective b-1 shown any teratogenic effects.33
blocker for hypertension with no hemorrhagic effects. Lisino- Tranexamic acid is antifibrinolytic by binding to plasmin-
pril, an angiotensin-converting enzyme (ACE) inhibitor, rarely ogen, preventing it from converting to plasmin in the clotting
may induce anemia, leukopenia, and thrombocytopenia, which cascade. Plasmin degrades fibrin.34 Tranexamic acid is much
may alter clotting. ACE inhibitors, such as lisinopril, may slightly more potent than alpha-aminocaproic acid and epsilon or para-
inhibit platelet function by various mechanisms.13,14 There is no aminomethyl benzoic acid in this action.33 In this competitive
evidence that the patient was not taking his L-thyroxine. inhibition activity, it bonds to the Kringle class disulfide linked
Hypothyroidism may induce a bleeding tendency.15 It is not proteins that interact with clotting factors.35 Tranexamic acid
certain whether the patient was using any complementary or inhibits plasmin action and with high dosage will reduce
alternative medication (CAM). CAMs may cause significant plasmin formation.35 The antifibrinolytic action of TA may also
perioperative bleeding.16,17 The patient had no clinical evi- act by reducing capillary leakage of the serum protein albumin,
dence of a blood dyscrasia. so as to maintain intravascular blood volume.36 Topical
This patient had a metal coronary artery stent placed 7 application may provide a high enough dose to accomplish
years prior and was chronically taking clopidogrel. Clopidogrel local coagulation, but in the past, most use has been parenteral
is a thienopyridine antithrombic drug used in coronary or via oral administration. Inhibition of plasminogen may
syndrome, peripheral vascular disease, cerebrovascular disease, additionally inhibit angiogenesis and bone repair, but this may
and coronary stents.18 Coronary stents have become routine not be clinically significant.37 In addition, cartilage matrix and
treatment for atherosclerotic coronary arteries. The stent can osteoblast formation may be inhibited by TA.37 The relatively
e84 Vol. XLI / No. Three / 2015
Flanagan
rapid clearance of TA precludes any significant inhibition of Systemic dosing techniques of TA have produced variations
osseous healing. in efficacy for optimal treatment, and it is difficult to maintain
stable therapeutic serum concentrations.48 Thus, individual
Intravenous use of TA patients may exhibit variable blood concentrations during oral
or intravenous administration, making dosage titration diffi-
In major surgical procedures, a preoperative intravenous TA
cult.48
dose of 20 mg/kg has been shown to reduce the postoperative
blood loss of bimaxillary osteotomy surgery as compared with Successful control of vaginal postpartum hemorrhage
placebo.38 exceeding 800 mL was effective with high-dose TA with a
Intravenously administered TA is cleared at approximately loading infusion dose of 4 g and 1 g/h for 6 hours.49 The high
the same rate as the patient’s glomerular filtration rate.39 The levels of plasminogen activator found in uterine and cervical
minimum safe nontoxic dosage of this drug has not been tissue may explain the beneficial effects of TA.50
determined. The serum concentration of intravenous TA shows
Oral administration of TA
high variation between patients, so the patient should be
Downloaded from http://meridian.allenpress.com/joi/article-pdf/41/3/e82/2058461/aaid-joi-d-13-00158.pdf by Indonesia user on 07 June 2021
monitored for this parameter.40 Intravenous administration Absorption after oral administration is about 40%, and
should not exceed 100 mg/min to avoid dizziness and bioavailability is not affected by taking with food. Tranexamic
hypotension. acid is eliminated by renal glomerular filtration, with only about
Transdermal enhanced administration may be possible with
5% being metabolized.
a carbamic acid salt ester of TA, which may facilitate
Tranexamic acid has been used to successfully treat
treatment.41 This approach was done in an effort to trans-
menorrhagia in von Willebrand’s disease with a single daily
dermally administer as a TA ester. The intradermally placed
4000-mg oral dose for 3–5 days.51
ester would then dissociate into an active metabolite to
Most patients can tolerate 3–6 g/d orally of TA, and it may
successfully cause skin barrier homeostasis.
be considered a first-line treatment for bleeding control of
Because of its inhibition of fibrinolysis, TA may be an
some conditions.24
important drug for bleeding in factor XI patients in whom high
fibrinolytic activity occurs.42 However, the oral administration of 1 g 4 times a day for 4
Topical TA therapy may decrease the risk of secondary days of TA can produce nausea, vomiting, diarrhea, and
hemorrhage in ambulatory ophthalmic patients with hyphe- abdominal pain in 12% of patients.52
ma.43 Dental surgical patients with hemophilia who were treated
Tranexamic acid enhances ultrafiltration volume in dialysis with TA 1 g 3 times a day for 5 days beginning 2 hours prior to
patients, of which the mechanism of action is unknown.44 Thus, surgery had significantly less postoperative bleeding as
there may be a decreased therapeutic action of drugs that compared with a placebo group.53 Hospital stay time can also
depend on ultrafiltration for clearance. be reduced with treatment.54
A Cochrane review found that when TA was administered
intravenously at the time of surgery, it reduced bleeding, with Anticoagulants and TA local hemorrhage control
no significant side effects.45
No anticoagulant acts to 100% prevent coagulation. Tranexa-
In mice, the lethal dose for 50% of subjects (LD50) is more
mic acid may act locally to act on any clotting that may occur to
than 10 mg/kg. Symptoms of overdose may include nausea,
stabilize that clot and any further clotting activity that can
vomiting, diarrhea, and/or hypotension. Thus, TA should be
occur. With time, the clotting can be significant to stop local
injected intravenously slowly, less than 1 mL/min. There is no
bleeding at the oral surgical site. Hence, TA may be effective
evidence of teratogenicity, mutagenicity, or fertility effects, so
with a multiplicity of anticoagulants.
TA is classed as a category B drug by the US Food and Drug
Warfarin (Coumadin) is an anticoagulant that is widely used.
Administration Pharmaceutical Pregnancy Categories. Throm-
bosis may occur when TA is intravenously administered with It acts by inhibiting the vitamin K recycling metabolism in the
factor IX or anti-inhibitor coagulant.46 formation of prothrombin and affects factors II, VII, IX, and X in
Tranexamic acid is used in oral surgical patients with the clotting cascade.1,55 Warfarin takes about 2–5 days to
hemophilia for short-term use (2–8 days) to reduce or prevent become clinically significant and the same to reverse its activity
hemorrhage following tooth extraction. Patients with most with vitamin K therapy.55 Warfarin interacts with many
clotting disorders get an abnormal fibrin network because of medications and foods that may increase or decrease its
lower or delayed thrombin production. The clotting process in effects. The INR measures the blood level of warfarin, which
patients with hemophilia is compromised, making the clot optimally ranges from 2.5–4.5 depending on the condition
more soluble, and cross-linking in the fibrin polymer does not being treated.56 The INR is calculated by dividing the patient’s
effectively occur.47 Patients with the rare factor XI bleeding prothrombin time (PT) by a standard control PT as determined
disorder have varying tendencies of hemorrhage. Surgical by the World Health Organization. This ratio standardizes
bleeding has been successfully treated in these patients with results for laboratory testing differences. Excessive alcohol use
TA and recombinant activated factor VII.42 In addition, TA may can increase the INR. Leafy green vegetables and some oils are
be used to prevent episodes of angioedema by preventing high in vitamin K and may decrease the action of warfarin.
activation of the initial complement protein. Thus, TA may have Warfarin increases the risk for osteoporosis fracture in men.57
multiple modes of pharmacologic action that need to be Broad-spectrum antibiotics may reduce gastroenteral bacteria
investigated. that generate vitamin K, thus increasing the effects of
Journal of Oral Implantology e85
Tranexamic Acid
warfarin.58 The TA tamponade may be able to control local oral not be able to predict preoperatively the patient’s ability to
bleeding with these patients. postoperatively coagulate. Since there may be different
Enoxaparin (Lovenox) is a low-molecular-weight heparin mechanisms of action of TA, a tamponade may be able to
that is used to treat patients with a history of deep vein control local oral bleeding by fibrin stabilization.
thrombosis or pulmonary embolism.5,59 It is administered by
subcutaneous injection by a health care provider or the patient. Topical use of TA
It acts by activating thrombin III and inhibits clotting factor Xa,
Topical TA has been used in ophthalmic, coronary, dental, and
which converts prothrombin to thrombin, preventing the fibrin
hemophiliac surgery.
clot. Heparin-induced thrombocytopenia, a decrease of plate-
Topical ophthalmic TA may cause enhanced therapeutic
lets by 50%, is a very rare side effect of enoxaparin caused by an
intraocular drug concentrations in hyphema (blood in the iris or
interaction with immunospecific antibodies and carries a
cornea) patients with minimal toxicity.69 This treatment intends
significant risk for thrombosis.60 Tranexamic acid may be a
to prevent additional bleeding in the eye.
local antidote to enoxaparin because of its stabilization of the
Microhemorrhage after coronary artery bypass surgery can
fibrin clot. Any clotting that forms may be induced to prolong
Downloaded from http://meridian.allenpress.com/joi/article-pdf/41/3/e82/2058461/aaid-joi-d-13-00158.pdf by Indonesia user on 07 June 2021
be controlled with topical compression with TA reducing total
and resist breakdown.
blood loss.70
Clopidogrel (Plavix) is a thienopyridine antiplatelet antico- Tranexamic acid has been used systemically and locally to
agulant.18,61 It acts as a P2Y(12)-ADP receptor antagonist to reduce postextraction and periodontal surgical bleeding by its
prevent thrombosis.18 It is metabolically inactivated by antifibrinolytic activity during operative procedures in hemo-
carboxylesterase-1 into carbolic acid metabolites.62 Genetic philiac and cirrhosis patients.71–74 Topical TA for oral-dental
variations can be responsible for a spectrum of drug activity has been primarily used as a mouth rinse for
responses.63 About 25% of patients may not fully respond to postoperative bleeding in hemophilia patients.11,72,74 In addi-
therapy.61 Since clopidogrel is a prodrug that is transformed tion, a 4.8% tranexamic mouthwash for 2 days has been used to
into an active metabolite by hepatic CYP2C19 patients, genetic control postextraction bleeding in patients taking warfarin.12 In
variations of this enzyme may have a subtherapeutic response a study by Waly, dual TA mouthwash and systemic TA was
or no response.61,64 Because of this, each oral surgical patient compared with systemic TA alone, and dual therapy was found
taking clopidogrel should be treated with caution and to be dramatically superior in postextraction bleeding in
hemorrhagic control measures should be ready to be instituted children with hemophilia.72
if anticoagulant therapy is not to be stopped or bridged. In patients with von Willebrand’s disease, oral or topical TA
Anticoagulant bridging therapy can be done with low- has been used to control oral bleeding such as frenum tears
molecular-weight heparin to anticoagulate the patient with a and lacerations of the lips and buccal mucosa.75,76
measurable method. Since clopidogrel is an antiplatelet and TA When 10 mL of 5% aqueous TA is administered orally as an
is an antifibrinolytic and some clotting would occur from an oral rinse for 2 minutes, it can be detected at a therapeutic level
alternative pathway, topical TA tamponade may be helpful in in saliva for 2 hours but is undetectable in blood plasma.71,72
oral bleeding control in these patients because of the different Systemic TA can be administered with an oral rinse to
mechanisms of action. significantly reduce postoperative bleeding.77
Rivaroxaban inhibits factor Xa in the clotting cascade and is When oral surgery is performed on patients with hemo-
administered orally daily.65 The factor Xa does not recover for philia who are anticoagulated, the surgery should be per-
about 24 hours, and the drug has no antagonist. A tamponade formed as atraumatically as possible by an experienced
of TA is an antifibrinolytic and may contribute to local surgeon.78 Extraction sockets can be filled with collagen plugs
hemorrhage control in patients taking rivaroxaban. soaked in 5% TA and secured with a resorbable suture. A 5% TA
Aspirin (acetylsalicylic acid [ASA]) is a nonsteroidal anti- 3-times-daily postoperative 7-day oral rinse may be additionally
inflammatory drug with antiplatelet anticoagulant activity. prescribed. Alternatively, surgical sponges soaked in a 5% TA
Acetylsalicylic acid inhibits platelet aggregation by blocking solution may be used by the patient to bite on to promote
formation of platelet thromboxane A2. The thromboxane fibrin clot stability.
metabolites are responsible for the aggregating ability of Hewson et al78 evaluated the postoperative course of 50
platelets.66 hemophilia patients for 113 extractions. They were prescribed a
The example patient presented above was taking 81 mg postoperative regimen of 5% TA oral rinse 3 times a day for 7
oral ASA daily working in tandem with the oral clopidogrel. The days and 5% TA surgical sponge tamponade as necessary for
combination of clopidogrel and aspirin is used for anticoagu- any moderate bleeding. Patients were treated with clotting
lant therapy but is not recommended by current guidelines.67 factor replacement therapy coverage if it was their normal
However, some patients will be prescribed this dual therapy protocol depending on the severity of their disease. On the
because of their specific cardiovascular issues, such as having eighth day, 41 patients had no bleeding incidents, 6 had mild
an implanted metal coronary stent surgery. The TA was bleeding, 3 had moderate postoperative bleeding that was
effective in stopping the local oral bleeding after 30 minutes treated with the tamponade, and no patient had severe
of tamponade in this dual-therapy patient. postoperative bleeding. What minimum clotting factor replace-
Dabigatran (Pradaxa) is a synthetic anticoagulant that ment level to provide a hemostatic effect in various surgical
directly inhibits thrombin and is not influenced by dietary procedures is not known, but TA may be able to reduce the
vitamin K.68 The usual dose is 150 mg twice a day. Blood level concentration of the therapy in these patients.79
monitoring is not required, but, again, the implant dentist may Tranexamic acid may be better used in a surgical sponge as
e86 Vol. XLI / No. Three / 2015
Flanagan
Downloaded from http://meridian.allenpress.com/joi/article-pdf/41/3/e82/2058461/aaid-joi-d-13-00158.pdf by Indonesia user on 07 June 2021
FIGURE 3. Immediate postoperative bleeding. FIGURE 4. Bleeding controlled with tranexamic acid tamponade.
a direct pressure tamponade when there is active bleeding important modality for bleeding control in these patients. A TA
(Figures 3 and 4). The most appropriate concentration of the TA oral rinse was not used in the case example to preclude a
solution is not known. The patient treated here was given TA potential dislodging or lifting of the surgical flap by the
topically as a saturated solution. circulating solution in the mouth.
Some patients take 2 anticoagulants for dual therapy. Here, A moistened tea bag has been used with compression to
TA may be used with other topical modalities, such as a tea stop postoperative bleeding from third molar extraction. Tea
bag, to induce local hemorrhage control. These conditions leaves contain tannic acid and tannins that may induce
need to be studied for appropriate treatment to be ascertained. vasoconstriction.82–84 There is a recent report of successful
In another placebo-controlled study, TA oral rinse alone use of combined tannic acid and aluminum potassium sulfate
was able to control gingival bleeding after dental scaling in as a sclerosing agent for hemorrhoids in patients taking
hemophilia patients.80 No preoperative clotting factor replace- anticoagulants and those not taking anticoagulants.85
ment therapy was used with the TA rinse in these hemophilia Ice applications may not adequately slow bleeding and
patients. may impair coagulation and hemostasis. Ice may be more
useful in controlling pain.86
Contraindications In patients in whom stents are to be placed, a tamponade
should be used to control hemorrhage before the stent is
Tranexamic acid is contraindicated for sensitivity, subarachnoid
applied.87 The stent may preclude direct contact of the TA with
hemorrhage, macroscopic hematuria, and ongoing acute
the bleeding surgical site. The clot formed is very fragile and
venous or arterial thrombosis.1 There may be a risk for
cannot be disturbed lest bleeding restarts.
thromboembolism if TA is administered after high doses of
prothrombin complex concentrates. Intravenous TA should not
be used to stop bleeding in the upper urinary tract, where clot
CONCLUSIONS
formation may cause an obstruction. Because of its renal
clearance, the intravenous TA dosage should be reduced in There is a risk of an adverse thromboembolic event for
patients with renal insufficiency. anticoagulant cessation when planning oral surgical proce-
dures. While the risk is low, about 6%, the risk for such an event
Epinephrine, compression, tannins, and ice for bleeding
may be life threatening or seriously debilitating. The patient
control
should, however, stop using CAMs for a week or two before the
Local circumferential injection of the surgical site with an surgery, as some of these may contribute to perioperative
epinephrine containing local anesthetic may be a consider- bleeding.8 Thus, local bleeding control is a preoperative
ation. However, in cardiac patients, this may be contraindicat- consideration for the dental implant surgical patient if cessation
ed, especially after the administration of the local anesthetic for is inappropriate.
intraoperative pain control. The very small number of patients reported herein does not
Compression by itself may stop bleeding but may not qualify as a high level of evidence. Topical TA treatment for
significantly contribute to the cessation in anticoagulated hemorrhage control needs to be investigated for efficacy.
patients.81 Tranexamic acid pressure tamponade may be an A saturated aqueous solution of TA may be used topically
Journal of Oral Implantology e87
Tranexamic Acid
in a surgical sponge with biting compression to control postoperative bleeding in anticoagulated patients requiring dental extrac-
postoperative bleeding in dental implant patients and poten- tions. Int J Oral Maxillofac Surg. 2003;32:504–507.
13. Bauriedel G, Skowasch D, Schneider M, Andrie R, Jabs A, Luderitz B.
tially in those who are taking anticoagulants. The clot formed is Antiplatelet effects of angiotensin-converting enzyme inhibitors compared
fragile and prone to rebleeding. Many anticoagulants cannot be with aspirin and clopidogrel: a pilot study with whole-blood aggregometry.
readily measured by clinical testing and thus place the patient Am Heart J. 2003;145:343–348.
at risk for postoperative hemorrhage. Local bleeding control 14. Malinin AI, Ong S, Makarov LM, Petukhova EY, Serebruany VL.
Platelet inhibition beyond conventional antiplatelet agents: expanding role
measures in these patients may be a preoperative consider- of angiotensin receptor blockers, statins and selective serotonin reuptake
ation. While TA may not directly interact with anticoagulants, its inhibitors. Int J Clin Pract. 2006;60:993–1002.
antifibrinolytic action stabilizes any clotting that does occur. 15. Marongiu F, Barcellona D, Mameli A, Mariotti S. Thyroid disorders
and hypocoagulability. Semin Thromb Hemost. 2011;37:11–16.
Tranexamic acid may have additional metabolic activity related
16. Roehm CE, Tessema B, Brown SM. The role of alternative medicine
or unrelated to coagulation. This report has a low level of in rhinology. Facial Plast Surg Clin North Am. 2012;20:73–81.
credibility. Research is needed to determine if TA is truly 17. McGillicuddy EA, Maxfield MW, Salameh B, Stein LH, Ahmad U,
effective. A congener of TA or a local submucosal injection of Longo WE. Bleeding diatheses and preoperative screening. J Surg Educ.
2013;70:423–431.
TA may be most efficacious. In the end, TA may be considered
Downloaded from http://meridian.allenpress.com/joi/article-pdf/41/3/e82/2058461/aaid-joi-d-13-00158.pdf by Indonesia user on 07 June 2021
18. Fareed J, Jeske W, Thethi I. Metabolic differences of current
to be part of an armamentarium for postoperative hemorrhage thienopyridine antiplatelet agents. Expert Opin Drug Metab Toxicol. 2013;9:
control of localized oral sites. 307–317.
19. Ghosh BD, Swaminathan RV, Kim LK, Feldman DN. Reperfusion
therapy in ST-elevation myocardial infarction: guidelines, strategies,
pharmacology, and stent selection. Minerva Med. 2012;103:431–439.
ABBREVIATIONS 20. Collet JP, Montalescot G. Antithrombotic and antiplatelet therapy
in TAVI patients: a fallow field? EuroIntervention. 2013;9(suppl):S43–S47.
ACE: angiotensin-converting enzyme 21. Vanstreels L, Molenberghs G, Voigt JU. Secondary stroke preven-
ASA: acetylsalicylic acid tion: misguided by guidelines? Acta Cardiol. 2012;67:431–438.
CAM: complementary or alternative medication 22. Trenk D, Zolk O, Fromm MF, Neumann FJ, Hochholzer W.
Personalizing antiplatelet therapy with clopidogrel. Clin Pharmacol Ther.
INR: international normalized ratio 2012;92:476–485.
PT: prothrombin time 23. Furie B, Furie BC. Thrombus formation in vivo. J Clin Invest. 2005;
TA: tranexamic acid 115:3355–3362.
24. Wellington K, Wagstaff AJ. Tranexamic acid: a review of its use in
the management of menorrhagia. Drugs. 2003;63:1417–1433.
25. Hoylaerts M, Lijen HR, Collen D. Studies on the mechanism of the
REFERENCES fibrinolytic action of tranexamic acid. Biochim Biophys Acta. 1981;673:75–85.
26. Cap AP, Baer DG, Orman JA, Aden J, Ryan K, Blackbourne LH.
1. Majerus PW, Broze GJ, Militich JP, Tollefsen DM. Anticoagulant, Tranexamic acid for trauma patients: a critical review of the literature. J
thrombolytic and antiplatelet drugs. In: Hardman JG, ed. Goodman and Trauma. 2011;71(1 suppl):S9–S14.
Gilman’s The Pharmacological Basis of Therapeutics. 9th ed. New York, NY: 27. Andersson L, Nilsson IM, Nihlen JE, Hedner U, Granstrand B,
McGraw Hill; 1996:1346–1359. Melander B. Experimental and clinical studies on AMCA, the antifibrinolyti-
2. Kleinrock M. The Use of Medicines in the United States: Review of cally active isomer of p-aminomethyl cvclohexane carboxylic acid. Scand J
2011. Parsippany, NJ: IMS Institute for Healthcare Informatics; 2012. Haematol. 1965;2:230–247.
3. Vandvik PO, Lincoff AM, Gore JM, et al. Primary and secondary 28. Andersson L, Nilsson IM, Colleen S, Granstrand B, Melander B. Role
prevention of cardiovascular disease: antithrombotic therapy and preven- of urokinase and tissue activator in sustaining bleeding and the
tion of thrombosis, 9th ed: American College of Chest Physicians evidence- management thereof with EACA and AMCA. Ann N Y Acad Sci. 1968;146:
based clinical practice guidelines. Chest. 2012;141(2 suppl):e637S–e668S. 642–658.
4. Kirley K, Qato DM, Kornfield R, Stafford RS, Alexander GC. National 29. Verstraete M. Clinical application of inhibitors of fibrinolysis. Drugs.
trends in oral anticoagulant use in the United States, 2007 to 2011. Circ 1985;29:236–261.
Cardiovasc Qual Outcomes. 2012;5:615–621. 30. Pilbrant A, Schannong M, Vessman J. Pharmacokinetics and
5. Yoshida Rde A, Yoshida WB, Maffei FH, El Dib R, Nunes R, Rollo HA. bioavailability of tranexamic acid. Eur J Clin Pharmacol. 1981;20:65–72.
Systematic review of randomized controlled trials of new anticoagulants for 31. Ahlberg A, Eriksson O, Kjellman H. Diffusion of tranexamic acid to
venous thromboembolism prophylaxis in major orthopedic surgeries, the joint. Acta Orthop Scand. 1976;47:486–488.
compared with enoxaparin. Ann Vasc Surg. 2013;27:355–369. 32. Kullander S, Nilsson IM. Human placental transfer of an antifibri-
6. Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for nolytic agent (AMCA). Acta Obstet Gynecol Scand. 1970;49:241–242.
VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: 33. Nilsson IM. Haemorrhagic and Thrombotic Disease. London, UK:
American College of Chest Physicians evidence-based clinical practice John Wiley and Sons; 1974.
guidelines. Chest. 2012;141(2 suppl):e419S–e494S. 34. The CRASH-2 Collaborators. The importance of early treatment with
7. Fassa AA, Urban P. Stents and antiplatelet therapy. Adv Cardiol. tranexamic acid in bleeding trauma patients: an exploratory analysis of the
2012;47:114–124. CRASH-2 randomized controlled trial. Lancet. 2011;377:1096–1101, e1–e2.
8. Eijgenraam P, Ten Cate H, Ten Cate-Hoek AJ. Safety and efficacy of 35. Atkinson RA, Williams RJ. Solution structure of the kringle 4 domain
bridging with low molecular weight heparins: a systematic review and from human plasminogen by 1H nuclear magnetic resonance spectroscopy
partial meta-analysis. Curr Pharm Des. 2013;19:4014–4023. and distance geometry. J Mol Biol. 1990;212:541–552.
9. Madrid C, Sanz M. What influence do anticoagulants have on oral 36. O’Brien JG, Battistini B, Zaharia F, Plante GE, Sirois P. Effects of
implant therapy? A systematic review. Clin Oral Implants Res. 2009;20(suppl tranexamic acid and aprotinin, two antifibrinolytic drugs, on PAF-induced
4):96–106. plasma extravasation in unanesthetized rats. Inflammation. 2000;24:411–429.
10. Madrid C. Dental extractions in patients taking anticoagulants: is 37. Kawao N, Tamura Y, Okumoto K, et al. Plasminogen plays a crucial
alteration of the anticoagulant regime necessary? Rev Med Suisse. 2005;1(21): role in bone repair. J Bone Miner Res. 2013;28:1561–1574.
1418, 1421–1412, 1424. 38. Choi WS, Irwin MG, Samman N. The effect of tranexamic acid on
11. Coetzee MJ. The use of topical crushed tranexamic acid tablets to blood loss during orthognathic surgery: a randomized controlled trial. J Oral
control bleeding after dental surgery and from skin ulcers in haemophilia. Maxillofac Surg. 2009;67:125–133.
Haemophilia. 2007;13:443–444. 39. Sharma V, Fan J, Jerath A, et al. Pharmacokinetics of tranexamic
12. Carter G, Goss A. Tranexamic acid mouthwash—a prospective acid in patients undergoing cardiac surgery with use of cardiopulmonary
randomized study of a 2-day regimen vs 5-day regimen to prevent bypass. Anaesthesia. 2012;67:1242–1250.
e88 Vol. XLI / No. Three / 2015
Flanagan
40. Bojko B, Vuckovic D, Mirnaghi F, et al. Therapeutic monitoring of 64. US Food and Drug Administration. http://edocket.access.gpo.gov/
tranexamic acid concentration: high-throughput analysis with solid-phase 2008/pdf/E8-11806.pdf.
microextraction. Ther Drug Monit. 2012;34:31–37. 65. Thomas TF, Ganetsky V, Spinler SA. Rivaroxaban: an oral factor Xa
41. Novotný M, Hrabálek A, Janůsová B, Novotný J, Vávrová K. inhibitor. Clin Ther. 2013;35:4–27.
Transkarbams as transdermal permeation enhancers: effects of ester 66. Tohgi H, Konno S, Tamura K, Kimura B, Kawano K. Effects of low-to-
position and ammonium carbamate formation. Bioorg Med Chem Lett. high doses of aspirin on platelet aggregability and metabolites of
2010;20:2726–2728. thromboxane A2 and prostacyclin. Stroke. 1992;23:1400–1403.
42. O’Connell NM. Factor XI deficiency. Semin Hematol. 2004;41(1 suppl 67. Thomson RM, Anderson DC. Aspirin and clopidogrel for prevention
1):76–81. of ischemic stroke. Curr Neurol Neurosci Rep. 2013;13:327.
43. Clarke WN, Noël LP. Outpatient treatment of microscopic and rim 68. Cheng JW, Vu H. Dabigatran etexilate: an oral direct thrombin
hyphemas in children with tranexamic acid. Can J Ophthalmol. 1993;28:325– inhibitor for the management of thromboembolic disorders. Clin Ther. 2012;
327. 34:766–787.
44. Kuriyama S, Nakayama M, Tomonari H, Kawaguchi Y, Hosoya T. 69. Damji KF, Noël LP, Peterson RG, et al. Topical versus intravenous
Tranexamic acid increases peritoneal ultrafiltration volume in patients on administration of tranexamic acid: a comparison of intraocular and serum
CAPD. Perit Dial Int. 1999;19:38–44.
concentrations in the rabbit. Can J Ophthalmol. 1998;33:308–313.
45. Henry DA, Carless PA, Moxey AJ, O’Connell D, Stokes BJ, Fergusson
70. Fawzy H, Elmistekawy E, Bonneau D, Latter D, Errett L. Can local
DA. Anti-fibrinolytic use for minimizing perioperative allogeneic blood
application of tranexamic acid reduce post-coronary bypass surgery blood
Downloaded from http://meridian.allenpress.com/joi/article-pdf/41/3/e82/2058461/aaid-joi-d-13-00158.pdf by Indonesia user on 07 June 2021
transfusion (review). Cochrane Database Syst Rev. 2011;(3):CD001886.
loss? A randomized controlled trial. J Cardiothorac Surg. 2009;4:25.
46. Pfizer. http://www.pfizer.com/tranexamicacid. Accessed January 28,
71. Sindet-Pedersen S, Stenbjerg S. Effect of local antifibrinolytic
2013.
47. Brummel-Ziedins KE, Branda RF, Butenas S, Mann K. Discordant treatment with tranexamic acid in hemophiliacs undergoing oral surgery.
fibrin formation in hemophilia. J Thromb Haemost. 2009;7:825–832. J Oral Maxillofac Surg. 1986;44:703–707.
48. Dowd NP, Karski JM, Cheng DC, et al. Pharmacokinetics of 72. Sindet-Pedersen S. Distribution of tranexamic acid to plasma and
tranexamic acid during cardiopulmonary bypass. Anesthesiology. 2002;97: saliva after oral administration and mouth rinsing: a pharmacokinetic study.
390–399. J Clin Pharmacol. 1987;27:1005–1008.
49. Ducloy-Bouthors AS, Jude B, Duhamel A, et al. High-dose 73. Waly NG. Local antifibrinolytic treatment with tranexamic acid in
tranexamic acid reduces blood loss in postpartum haemorrhage. Crit Care. hemophilic children undergoing dental extractions. Egypt Dent J. 1995;41:
2011;15:R117. 961–968.
50. Landin LE, Weiner E. Late-bleeding after conization: the effect of 74. Perdigão JP, de Almeida PC, Rocha TD, et al. Postoperative bleeding
tranexamic acid (Cyklokapron). Opusc Med. 1975;20:280–284. after dental extraction in liver pretransplant patients. J Oral Maxillofac Surg.
51. Ong YL, Hull DR, Mayne EE. Menorrhagia in von Willebrand disease 2012;70:e177–e184.
successfully treated with single daily dose tranexamic acid. Haemophilia. 75. Nickles K, Wohlfeil M, Alesci S, Miesbach W, Eickholz P. Compre-
1998;4:63–65. hensive treatment of periodontitis in patients with von Willebrand disease. J
52. Preston JT, Cameron IT, Adams EJ, Smith SK. Comparative study of Periodontol. 2010;81:1432–1440.
tranexamic acid and norethisterone in the treatment of ovulatory 76. Jiménez-Yuste V, Prim MP, De Diego JI, et al. Otorhinologic surgery
menorrhagia. Br J Obstet Gynaecol. 1995;102:401–406. in children with von Willebrand disease. Arch Otolaryngol Head Neck Surg.
53. Forbes CD, Barr RD, Reid G, et al. Tranexamic acid in control of 2002;128:1365–1368.
haemorrhage after dental extraction in haemophilia and Christmans disease. 77. Piot B, Sigaud-Fiks M, Huet P, Fressinaud E, Trossaërt M, Mercier J.
Br Med J. 1972;2:311–313. Management of dental extraction in patients with bleeding disorders. Oral
54. Ramstrom G, Blomback M. Tooth extractions in hemophilia. Int J Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:247–250.
Oral Surg. 1975;4:1–17. 78. Hewson J, Makhmalbaf P, Street A, McCarthy P, Walsh M. Dental
55. Ansell J, Hirsh J, Hyleke. Pharmacology and management of the surgery with minimal factor support in the inherited bleeding disorder
vitamin K antagonists: American College of Chest Physicians evidence-based population at the Alfred Hospital. Haemophilia. 2011;17:e185–e188.
clinical practice guidelines (8th edition). Chest. 2008;133(6 suppl):160S–198S. 79. Schulman S. Continuous infusion. Haemophilia. 2003:9:36875.
56. Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of 80. Lee AP, Boyle CA, Savidge GF, Fiske J. Effectiveness in controlling
warfarin and its drug and food interactions. Arch Intern Med. 2005;165:1095– haemorrhage after dental scaling in people with haemophilia by using
1106.
tranexamic acid mouthwash. Br Dent J. 2005;198:33–38.
57. Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF. Risk
81. Siritongtaworn P. Management of life threatening hemorrhage
of osteoporotic fracture in elderly patients taking warfarin: results from the
from facial fracture. J Med Assoc Thai. 2005;88:382–385.
National Registry of Atrial Fibrillation 2. Arch Intern Med. 2006;166:241–246.
82. Chung KT, Wong TY, Wei CI, Huang YW, Lin H. Tannins and human
58. Juurlink DN. Drug interactions with warfarin: what clinicians need
health: a review. Crit Rev Food Sci Nutr. 1998;38:421–464.
to know. CMAJ. 2007;177:369–371.
59. Levy JH, Tanaka KA, Hursting MJ. Reducing thrombotic complica- 83. Pryor JC, Hirsch JA, Hurst RW. Endovascular management of tumors
tions in the perioperative setting: an update on heparin-induced and vascular malformations of the head and neck. In: Hurst RW, Rosenwasser
thrombocytopenia. Anesth Analg. 2007;105:570–582. RH, eds. Interventional Radiology. New York, NY: Informa Healthcare; 2008:
60. Warkentin TE, Greinacher A. Heparin-induced thrombocytopenia: 209.
recognition, treatment, and prevention. Chest. 2004;126:S311–S337. 84. Halkens S. The use of tannic acid in the local treatment of burn
61. Ellis KJ, Stouffer GA, McLeod HL, Lee CR. Clopidogrel pharmaco- wounds: intriguing old and new perspectives. Wounds. 2001;13:144–158.
genomics and risk of inadequate platelet inhibition: US FDA recommenda- 85. Yano T, Nogaki T, Asano M, Tanaka S, Kawakami K, Matsuda Y.
tions. Pharmacogenomics. 2009;10:1799–1817. Outcomes of case-matched injection sclerotherapy with a new agent for
62. Lewis JP, Horenstein RB, Ryan K, et al. The functional G143E variant hemorrhoids in patients treated with or without blood thinners. Surg Today.
of carboxylesterase 1 is associated with increased clopidogrel active 2013;43:854–858.
metabolite levels and greater clopidogrel response. Pharmacogenet Genom. 86. Forsyth AL, Zourikian N, Valentino LA, Rivard GE. The effect of
2013;23:1–8. cooling on coagulation and haemostasis: should ‘‘Ice’’ be part of treatment
63. Roden DM. Cardiovascular pharmacogenomics: the future of of acute haemarthrosis in haemophilia? Haemophilia. 2012;18:843–850.
cardiovascular therapeutics? Can J Cardiol. 2013;29:58–66. 87. Flanagan D. The bis-acryl stent. J Oral Implantol. 2013;39:69–72.
Journal of Oral Implantology e89
You might also like
- Geriatric Anxiety Scale v2.0 FINALDocument2 pagesGeriatric Anxiety Scale v2.0 FINALpujipurwaningsih67% (3)
- CPD 1-CPG For The Management of Childhood AsthmaDocument43 pagesCPD 1-CPG For The Management of Childhood AsthmaizatisarefNo ratings yet
- Terapia Antiplaquetaria y ExodontiaDocument6 pagesTerapia Antiplaquetaria y ExodontiaDentalib OdontologíaNo ratings yet
- Oral Surgery in Patients Under Antithrombotic Therapy. Narrative ReviewDocument7 pagesOral Surgery in Patients Under Antithrombotic Therapy. Narrative ReviewAsmy ChubbiezztNo ratings yet
- Treatment in Dental Practice of The Patient Receiving Anticoagulation Therapy PDFDocument7 pagesTreatment in Dental Practice of The Patient Receiving Anticoagulation Therapy PDFJorge AlvaradoNo ratings yet
- Antiplatelet DrugsDocument5 pagesAntiplatelet DrugsAhmad DzakyNo ratings yet
- BMM 5Document5 pagesBMM 5Meta Anjany FirmansyahNo ratings yet
- A Review On The Management of Patients On Anticoagulant Therapy Programmed For Dental Extraction and Minor Oral SurgeryDocument3 pagesA Review On The Management of Patients On Anticoagulant Therapy Programmed For Dental Extraction and Minor Oral SurgeryInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- PT On Anti CoagulantsDocument4 pagesPT On Anti CoagulantsShivendra Nath TripathiNo ratings yet
- Ijd2018 6595406Document6 pagesIjd2018 6595406José Cunha CoutinhoNo ratings yet
- Managing Anticoagulant and Antiplatelet Drugs Before Dental ProceduresDocument3 pagesManaging Anticoagulant and Antiplatelet Drugs Before Dental Proceduresmamfm5No ratings yet
- AnnMaxillofacSurg11175-8428373 232443Document5 pagesAnnMaxillofacSurg11175-8428373 232443Wilson WijayaNo ratings yet
- Otley1996 Warfarina, Aas, Ains-ComplicatiiDocument6 pagesOtley1996 Warfarina, Aas, Ains-ComplicatiiGabriela Catana TurcuNo ratings yet
- New Antithrombotic Agents in The Ambulatory SettingDocument8 pagesNew Antithrombotic Agents in The Ambulatory SettingyuyoideNo ratings yet
- Gelatamp Study 06 15Document6 pagesGelatamp Study 06 15andrada67No ratings yet
- Circoutcomes 115 002430Document4 pagesCircoutcomes 115 002430Valentina MerolaNo ratings yet
- Managment of Dental Extraction in Patients Undergoing Anticoagulant Oral Direct Treatment Apilot StudyDocument10 pagesManagment of Dental Extraction in Patients Undergoing Anticoagulant Oral Direct Treatment Apilot Studyzahra.khalid-aliNo ratings yet
- Anesthesia AtricleDocument4 pagesAnesthesia Atriclemrxmdxsc7nNo ratings yet
- Perioperatorio AnticuagulaciónDocument8 pagesPerioperatorio AnticuagulaciónHans GonzalesNo ratings yet
- Aep 373Document7 pagesAep 373Salsabila FitriaNo ratings yet
- Anaesthesia For Vitreo-Retinal SurgeryDocument6 pagesAnaesthesia For Vitreo-Retinal SurgeryRuwan KuruppuNo ratings yet
- Hemostasia 2Document4 pagesHemostasia 2Laura OrtizNo ratings yet
- Efficacy and Safety o A Dedicated LAAO Protocol 2022Document3 pagesEfficacy and Safety o A Dedicated LAAO Protocol 2022吳醫師No ratings yet
- 3238-Article Text-12302-1-10-20200515Document5 pages3238-Article Text-12302-1-10-20200515Afif NadirrafiNo ratings yet
- Management of Bleeding in CancerDocument12 pagesManagement of Bleeding in CancerRoyan M. VarendraNo ratings yet
- Immediate Laser-Induced Hemostasis in Anticoagulated Rats Subjected To Oral Soft Tissue Surgery - A Double-Blind StudyDocument8 pagesImmediate Laser-Induced Hemostasis in Anticoagulated Rats Subjected To Oral Soft Tissue Surgery - A Double-Blind Studypolianass1109No ratings yet
- Articulo - FarmacologíaDocument13 pagesArticulo - FarmacologíaJhon RVNo ratings yet
- 508 - 7 CardiologyDocument9 pages508 - 7 CardiologymlinaballerinaNo ratings yet
- Dental Update 2014. Haemostasis Part 1. The Management of Post-Extraction HaemorrhageDocument6 pagesDental Update 2014. Haemostasis Part 1. The Management of Post-Extraction Haemorrhageindimazaya100% (1)
- Ifferences Between Warfarin and New Oral Anticoagulants in Dental Clinical PracticeDocument6 pagesIfferences Between Warfarin and New Oral Anticoagulants in Dental Clinical PracticeCezara PanainteNo ratings yet
- Anticoagulant and Antiplatelet Medications and Dental Procedures ADADocument8 pagesAnticoagulant and Antiplatelet Medications and Dental Procedures ADADeeNo ratings yet
- Direct Oral Anticoagulants Evidence and Unresolved Issues 2020Document10 pagesDirect Oral Anticoagulants Evidence and Unresolved Issues 2020Sebastián Camilo DuqueNo ratings yet
- Hemostasis in Oral Surgery PDFDocument7 pagesHemostasis in Oral Surgery PDFBabalNo ratings yet
- 832-Article Text-1421-1-10-20200824Document11 pages832-Article Text-1421-1-10-20200824Juan Carlos Vera SuárezNo ratings yet
- ProspectDocument8 pagesProspectValentina MerolaNo ratings yet
- Out RealDocument6 pagesOut RealJeferson SoriaNo ratings yet
- Complications Andmanagement Ofseptoplasty: Amy S. Ketcham,, Joseph K. HanDocument8 pagesComplications Andmanagement Ofseptoplasty: Amy S. Ketcham,, Joseph K. HanEduardo Cantu GarzaNo ratings yet
- AFP 2014 12 Clinical RahmanDocument6 pagesAFP 2014 12 Clinical RahmanmyscribeNo ratings yet
- Adult Patients On Antiplatelet Therapy Who Require Elective Surgery or An Invasive Procedure Management of CA5127 V6Document5 pagesAdult Patients On Antiplatelet Therapy Who Require Elective Surgery or An Invasive Procedure Management of CA5127 V6adybutucNo ratings yet
- CG A002 Medication That May Influence HaemostasisDocument5 pagesCG A002 Medication That May Influence HaemostasismahmoudNo ratings yet
- Surgical Decompression: Chronic Subdural HematomaDocument3 pagesSurgical Decompression: Chronic Subdural Hematomaeirene simbolonNo ratings yet
- N 793 Manuscript Final ZeregaDocument4 pagesN 793 Manuscript Final Zeregaapi-266543811No ratings yet
- Neuraxial Blockade and AnticoagulantsDocument69 pagesNeuraxial Blockade and Anticoagulantskamel6No ratings yet
- Periprocedural Anticoagulation v2Document27 pagesPeriprocedural Anticoagulation v2Joanne HoNo ratings yet
- Tranexamic Acid As A Mouthwash in Anticoagulant Treared Patients Undergoing Oral SurgeryDocument3 pagesTranexamic Acid As A Mouthwash in Anticoagulant Treared Patients Undergoing Oral SurgeryNoviantiNo ratings yet
- Resuming Anticoagulation After Hemorrhage: A Practical ApproachDocument12 pagesResuming Anticoagulation After Hemorrhage: A Practical ApproachNurul FajriNo ratings yet
- Special Care Dentistry Dental Management of Patients With Drug Related Acquired Bleeding DisordersDocument6 pagesSpecial Care Dentistry Dental Management of Patients With Drug Related Acquired Bleeding DisordersRatri ReswitadewiNo ratings yet
- Manejo Pacientes Anticoagulados en Cirugía OralDocument9 pagesManejo Pacientes Anticoagulados en Cirugía OralCindy Bernal MNo ratings yet
- CCJM Warfarin PDFDocument12 pagesCCJM Warfarin PDFmyscribeNo ratings yet
- KJR 11 257Document12 pagesKJR 11 257Priyo ArdaniNo ratings yet
- DabigatranDocument6 pagesDabigatranNayelis SalasNo ratings yet
- Perioperative Management of Patients Receiving Anticoagulants - UpToDateDocument69 pagesPerioperative Management of Patients Receiving Anticoagulants - UpToDatePhúc NguyễnNo ratings yet
- MÓDULO 2 - MATERIAL COMPLEMENTAR Artigo HematológicoDocument14 pagesMÓDULO 2 - MATERIAL COMPLEMENTAR Artigo HematológicoIvan CarlosNo ratings yet
- CRP2019 9308631Document13 pagesCRP2019 9308631Diego DíazNo ratings yet
- Perioperative Anesthesia Anagement OnDocument30 pagesPerioperative Anesthesia Anagement OnryandikaNo ratings yet
- Non Vitamin K Antagonist Oral Anticoagulation The Future of Anticoagulation Following Mitral Reparative SurgeryDocument3 pagesNon Vitamin K Antagonist Oral Anticoagulation The Future of Anticoagulation Following Mitral Reparative SurgeryPaul HartingNo ratings yet
- BRUISE CONTROL-2 Trial. EHJ 2018Document8 pagesBRUISE CONTROL-2 Trial. EHJ 2018Ernesto J. Rocha ReyesNo ratings yet
- Ketorolac Usage in Tonsillectomy and Uvulopalatopharyngoplasty Patients 2019Document4 pagesKetorolac Usage in Tonsillectomy and Uvulopalatopharyngoplasty Patients 2019Azzam SaqrNo ratings yet
- Antipatelet Drug TherapyDocument6 pagesAntipatelet Drug TherapySayali KhandaleNo ratings yet
- SOGC DVT ProphylaxisDocument16 pagesSOGC DVT Prophylaxisibrahimnazeh96No ratings yet
- ASRA Guidelines Regional Anaesthesia in Anticoagulated PatientDocument10 pagesASRA Guidelines Regional Anaesthesia in Anticoagulated PatientRizg AlamriNo ratings yet
- Skala Prilaku FranklDocument6 pagesSkala Prilaku FranklMeta Anjany FirmansyahNo ratings yet
- BMM 5Document5 pagesBMM 5Meta Anjany FirmansyahNo ratings yet
- Immediate Removable Partial Denture For Aesthetic Anterior Maxillary Tooth RehabilitationDocument9 pagesImmediate Removable Partial Denture For Aesthetic Anterior Maxillary Tooth RehabilitationMeta Anjany FirmansyahNo ratings yet
- Rehabilitation of Patient With Immediate Cast Partial Denture Using Patient's Natural Maxillary Anterior TeethDocument6 pagesRehabilitation of Patient With Immediate Cast Partial Denture Using Patient's Natural Maxillary Anterior TeethMeta Anjany FirmansyahNo ratings yet
- Ijrr001 PDFDocument3 pagesIjrr001 PDFMeta Anjany FirmansyahNo ratings yet
- Pulp CappingDocument3 pagesPulp CappingMeta Anjany FirmansyahNo ratings yet
- Xvaginal Breech DeliveryDocument21 pagesXvaginal Breech DeliveryiqiqiqiqiqNo ratings yet
- Assisted Suicide and Euthanasia Beyond Terminal IllnessDocument4 pagesAssisted Suicide and Euthanasia Beyond Terminal Illnesscreyente_madrileñoNo ratings yet
- Human HealthDocument9 pagesHuman HealthCreativity HouseNo ratings yet
- Board Exam Oct 2Document12 pagesBoard Exam Oct 2Aljee Sumampong BationNo ratings yet
- WHO CINDI Programme-Implemented Projects and Activities in Macedonia, 2001-2005Document5 pagesWHO CINDI Programme-Implemented Projects and Activities in Macedonia, 2001-2005Ass. Prof. Vera Simovska, MD., PhD.100% (1)
- v10 Liposculpture As A Complementary Treatment in RhytidoplastyDocument5 pagesv10 Liposculpture As A Complementary Treatment in RhytidoplastyAlisNo ratings yet
- Heat StressDocument39 pagesHeat StressDelando CoriahNo ratings yet
- Presented by MR S. Jugroo (PMSM) : National Dialysis Coordinator Ministry of Health and WellnessDocument56 pagesPresented by MR S. Jugroo (PMSM) : National Dialysis Coordinator Ministry of Health and WellnessKhedu VeemlaNo ratings yet
- Tinjauan Alur Prosedur Pelayanan Pasien Rawat Jalan Peserta BPJS Di RSU Imelda Pekerja Indonesia MedanDocument7 pagesTinjauan Alur Prosedur Pelayanan Pasien Rawat Jalan Peserta BPJS Di RSU Imelda Pekerja Indonesia Medannurintan kurniaNo ratings yet
- SITUATION 131 PagesDocument8 pagesSITUATION 131 PagesCharmaine Rose Inandan TriviñoNo ratings yet
- Assessment of The Gastrointestinal SystemDocument4 pagesAssessment of The Gastrointestinal SystemAvery SandsNo ratings yet
- EBM and EconomicsDocument14 pagesEBM and EconomicsSofyan HarahapNo ratings yet
- VY-EnFlow Brochure CF805170019 (2) Jul10-FinalDocument8 pagesVY-EnFlow Brochure CF805170019 (2) Jul10-FinalShaikh Emran HossainNo ratings yet
- Severe Injured Patient Multiple Fracture Patient Principle of Treatment & Maintenance of PatientDocument14 pagesSevere Injured Patient Multiple Fracture Patient Principle of Treatment & Maintenance of PatientAilar NasirzadehNo ratings yet
- AOP Form 3Document4 pagesAOP Form 3Ferzada SajiranNo ratings yet
- Classification System For Complete EdentulismDocument33 pagesClassification System For Complete EdentulismSahana RangarajanNo ratings yet
- Breathe Light To Breathe Right - PDF RoomDocument58 pagesBreathe Light To Breathe Right - PDF Roomfabricio100% (3)
- The Volume-Viscosity Swallow Test For Clinical Screening of Dysphagia and AspirationDocument10 pagesThe Volume-Viscosity Swallow Test For Clinical Screening of Dysphagia and AspirationMarcia SantanaNo ratings yet
- BONEJDocument3 pagesBONEJZohair AlamNo ratings yet
- Technical Description of A Stethoscope Final DraftDocument4 pagesTechnical Description of A Stethoscope Final Draftapi-317066744No ratings yet
- What Makes Continuing Education Effective PerspectDocument6 pagesWhat Makes Continuing Education Effective PerspecttestNo ratings yet
- Reaction PaperDocument2 pagesReaction PaperLinzie CariquetanNo ratings yet
- Date and Time Objectives Learning Contents Strategies Target Population Resources Evaluation OutcomeDocument8 pagesDate and Time Objectives Learning Contents Strategies Target Population Resources Evaluation OutcometrizzlecNo ratings yet
- Acupuncture - MeniereDocument4 pagesAcupuncture - MeniereTinnitus Man IndonesiaNo ratings yet
- Morgan Haines Interplast Diary 2016Document1 pageMorgan Haines Interplast Diary 2016leh.mo9315No ratings yet
- Dr. Mowlavi Selected To RealSelf Medical Advisory BoardDocument2 pagesDr. Mowlavi Selected To RealSelf Medical Advisory BoardPR.comNo ratings yet
- Diabetes Educators' Success Stories PDFDocument210 pagesDiabetes Educators' Success Stories PDFRavi V Potluri0% (1)
- لقطة شاشة ٢٠٢١-٠٧-١٠ في ١٢.٠٢.٥٥ مDocument41 pagesلقطة شاشة ٢٠٢١-٠٧-١٠ في ١٢.٠٢.٥٥ مmonNo ratings yet