Professional Documents
Culture Documents
Sleep Wake Disorders
Sleep Wake Disorders
Uploaded by
Isabel CastilloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sleep Wake Disorders
Sleep Wake Disorders
Uploaded by
Isabel CastilloCopyright:
Available Formats
PSYCHIATRY III EXIMIUS
SLEEP-WAKE DISORDERS
2021
Ethel Maureen Pagaddu, MD December 2019
SLEEP DISORDERS awakenings. (In children, this may manifest as difficulty
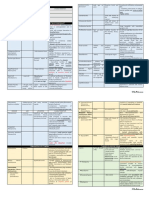
Sleep Disorder Classification returning to sleep without caregiver intervention.)
1. Insomnia Disorder 3. Early-morning awakening with inability to return to
2. Hypersomnolence Disorder sleep.
3. Narcolepsy B. The sleep disturbance causes clinically significant distress or
4. Breathing-Related Sleep Disorders: impairment in social, occupational, educational, academic,
a. Obstructive Sleep Apnea Hypopnea behavioral, or other important areas of functioning.
b. Central Sleep Apnea C. The sleep difficulty occurs at least 3 nights per week.
i. Idiopathic central sleep apnea D. The sleep difficulty is present for at least 3 months.
ii. Cheyne-Stokes breathing E. The sleep difficulty occurs despite adequate opportunity for sleep.
iii. Central sleep apnea comorbid with opioid use F. The insomnia is not better explained by and does not occur
c. Sleep-Related Hypoventilation exclusively during the course of another sleep-wake disorder (e.g.,
5. Circadian Rhythm Sleep-Wake Disorders: narcolepsy, a breathing-related sleep disorder, a circadian rhythm
a. Delayed sleep phase type sleep-wake disorder, a parasomnia).
b. Advanced sleep phase type G. The insomnia is not attributable to the physiological effects of a
c. Irregular sleep-wake type substance (e.g., a drug of abuse, a medication).
d. Non-24-hour sleep-wake type H. Coexisting mental disorders and medical conditions do not
e. Shift work type adequately explain the predominant complaint of insomnia.
f. Unspecified type
6. Parasomnias Specify if:
7. Non-Rapid Eye Movement Sleep Arousal Disorders: With non-sleep disorder mental comorbidity, including substance
a. Sleepwalking type use disorders
b. Sleep terror type With other medical comorbidity With other sleep disorder Coding
8. Nightmare Disorder note: The code 780.52 (G47.00) applies to all three specifiers. Code
9. Rapid Eye Movement Sleep Behavior Disorder also the relevant associated mental disorder, medical condition, or
10. Restless Legs Syndrome other sleep disorder immediately after the code for insomnia
11. Substance/Medication-Induced Sleep Disorder disorder in order to indicate the association.
COMMON POLYSOMNOGRAPHIC MEASURES Specify if:
§ Sleep latency: Period of time from turning out the lights until Episodic: Symptoms last at least 1 month but less than 3 months.
the appearance of stage II sleep Persistent: Symptoms last 3 months or longer.
§ Early morning awakening: Time of being continuously awake Recurrent: Two (or more) episodes within the space of 1 year.
from the last stage of the sleep until the end of the sleep record Note: Acute and short-term insomnia (i.e., symptoms lasting less
(usually at 7 AM) than 3 months but otherwise meeting all criteria with regard to
§ Sleep efficiency: Total sleep time or total time of the sleep frequency, intensity, distress, and/or impairment) should be coded
record x 100 as an other specified insomnia disorder.
§ Apnea index: Number of apneas longer than 10 seconds per
hour of sleep HYPERSOMNOLENCE DISORDER
§ Nocturnal myoclonus index: Number of periodic leg § Sleepiness can be a consequence of
movements per hour (1) insufficient sleep,
§ Rapid eye movement (REM) latency: Period of time from the (2) basic neurologic dysfunction in brain systems
onset of sleep until the first REM period of the night regulating sleep,
§ Sleep-onset REM period: REM sleep within the first 10 minutes (3) disrupted sleep, or
of sleep. (4) the phase of an individual's circadian rhythm.
INSOMIA DISORDER PARASOMNIA
§ difficulty initiating or maintaining sleep § an unusual or undesirable phenomenon that appears suddenly
§ the most common sleep complaint and may be transient or during sleep OR THAT occurs at the threshold between waking
persistent and sleeping
§ DSM-5 defines insomnia disorder as dissatisfaction with sleep § occurs in stages III and IV and, thus, is associated with poor
quantity or quality associated with one or more of the following recall of the disturbance
symptoms: difficulty in initiating sleep, difficulty in maintaining
sleep with frequent awakenings or problems returning to sleep, SLEEP-WAKE SCHEDULE DISTURBANCE
and early morning awakening with inability to return to sleep § involves the displacement of sleep from its desired circadian
period
DSM-5 Diagnostic Criteria for Insomnia Disorder § cannot sleep when they wish to sleep; they cannot be fully
A. A predominant complaint of dissatisfaction with sleep quantity or awake when they want to be fully awake
quality, associated with one (or more) of the following symptoms:
1. Difficulty initiating sleep. (In children, this may manifest Nonspecific Measures to Induce Sleep (Sleep Hygiene)
as difficulty initiating sleep without caregiver intervention. § Arise at the same time daily.
2. Difficulty maintaining sleep, characterized by frequent § Limit daily in-bed time to the usual amount present before the
awakenings or problems returning to sleep after sleep disturbance.
§ Discontinue central nervous system (CNS)-acting drugs
(caffeine, nicotine, alcohol, stimulants).
TRANSCRIBERS Marky, Josh, Eina 1
PSYCHIATRY III EXIMIUS
SLEEP-WAKE DISORDERS
2021
Ethel Maureen Pagaddu, MD December 2019
§ Avoid daytime naps (except when sleep chart shows they IDIOPATHIC INSOMNIA
induce better night sleep). § starts early in life, sometimes at birth, and continues
§ Establish physical fitness by means of a graded program of throughout life
vigorous exercise early in the day. § suspected causes include neurochemical imbalance in
§ Avoid evening stimulation; substitute radio or relaxed reading brainstem reticular formation, impaired regulation of
for television. brainstem sleep generators (e.g., raphe nuclei, locus ceruleus),
§ Try very hot, 20-minute, body-temperature-raising bath soaks or basal forebrain dysfunction
near bedtime. § treatment is difficult
§ Eat at regular times daily; avoid large meals near bedtime. § improved sleep hygiene, relaxation therapy, and judicious use
§ Practice evening relaxation routines, such as progressive of hypnotic medicines are reportedly helpful
muscle relaxation or meditation. § shows some familial incidence
§ Maintain comfortable sleeping conditions. § most frequently begins in adolescence or young adulthood,
generally before the age of 30
Inadequate Sleep Hygiene § either progresses slowly or reaches a plateau that is
§ a patient's lifestyle leads to sleep disturbance maintained throughout life
§ referring to a problem in following generally accepted § The most common symptom is sleep attacks
practices to aid sleep § Another uncommon symptom is sleep paralysis, most often
§ include keeping regular hours of bedtime and arousal, occurring on awakening in the morning; during the episode,
avoiding excessive caffeine, not eating heavy meals before patients are apparently awake and conscious but unable to
bedtime, and getting adequate exercise. move a muscle
§ sometimes falls within the primary insomnia classification § HLA-DR2 is found in 90 to 100 percent of patients with
depending on the specific sleep hygiene factor involved narcolepsy
§ Treatment should focus on only two or three problem areas at § patients with narcolepsy are deficient in the neurotransmitter
a time hypocretin, which stimulates appetite and alertness
PSYCHOPHYSIOLOGICAL INSOMNIA NARCOLEPSY
§ presents as a primary complaint of difficulty in going to sleep DSM-5 Diagnostic Criteria for Narcolepsy
§ may describe this as having gone on for years and usually A. Recurrent periods of an irrepressible need to sleep, lapsing
denies that it is associated with stressful periods in his or her into sleep, or napping occurring within the same day.
life These must have been occurring at least three times per
§ also called conditioned insomnia week over the past 3 months.
§ Other features include (1) excessive worry about not being B. The presence of at least one of the following:
able to sleep; (2) trying too hard to sleep; (3) rumination, 1. Episodes of cataplexy, defined as either (a) or
inability to clear one's mind while trying to sleep; (4) increased (b), occurring at least a few times per month:
muscle tension when attempting to sleep; (5) other somatic a. In individuals with long-standing
manifestations of anxiety; (6) being able to sleep better away disease, brief (seconds to minutes)
from one's own bedroom; and (7) being able to fall asleep episodes of sudden bilateral loss of
when not trying (e.g., watching TV) muscle tone with maintained
§ Treatment can be difficult consciousness that are precipitated by
§ Sleeping pills be used sparingly and at the lowest effective laughter or joking.
dose b. In children or in individuals within 6
§ Stimulus control therapy is recommended to break the months of onset, spontaneous
conditioning grimaces or jaw-opening episodes with
§ relaxation therapy is a useful ancillary treatment tongue thrusting or a global hypotonia,
without any obvious emotional
SLEEP STATE MISPERCEPTION triggers.
§ also known as subjective insomnia 2. Hypocretin deficiency, as measured using
§ characterized by a dissociation between the patient's cerebrospinal fluid (CSF) hypocretin-1
experience of sleeping and the objective polygraphic immunoreactivity values (less than or equal to
measures of sleep one third of values obtained in healthy subjects
§ Cause is not yet understood tested using the same assay, or less than or
§ a patient complains of difficulty initiating or maintaining sleep equal to 110 pg/ml). Low CSF levels of
and no hypocretin-1 must not be observed in the
objective evidence of sleep disruption is found context of acute brain injury, inflammation, or
§ can occur in individuals who are apparently free from infection.
psychopathology or it can represent a somatic delusion or 3. Nocturnal sleep polysomnography showing rapid
hypochondriasis eye movement (REM) sleep latency less than or
§ Cognitive relabeling, diffusing the worry about being unable to equal to 15 minutes, or a multiple sleep latency
sleep, or both can help test showing a mean sleep latency less than or
§ anxiolytics can profoundly reduce the perception of equal to 8 minutes and two or more sleep-onset
sleeplessness REM periods.
Specify whether:
347.00 (G47.419) Narcolepsy without cataplexy but with hypocretin
deficiency: Criterion B requirements of low CSF hypocretin-1 levels
TRANSCRIBERS Marky, Josh, Eina 2
PSYCHIATRY III EXIMIUS
SLEEP-WAKE DISORDERS
2021
Ethel Maureen Pagaddu, MD December 2019
and positive polysomnography/multiple sleep latency test are met, OBSTRUCTIVE SLEEP APNEA SYNDROME
but no cataplexy is present (Criterion B1 not met). § characterized by periods of functional obstruction of the
347.01 (G47.411) Narcolepsy with cataplexy but without hypocretin upper airway during sleep, resulting in decreases in arterial
deficiency: In this rare subtype (less than 5 percent of narcolepsy oxygen saturation and a transient arousal, after which
cases), Criterion B requirements of cataplexy and positive respiration (at least briefly) resumes normally.
polysomnography/multiple sleep latency test are met, but CSF § occur in patients who snore
hypocretin-1 levels are normal (Criterion B2 not met). § patients are overweight, and it appears more frequently in
347.00 (G47.419) Autosomal dominant cerebellar ataxia, deafness, patients with smaller jaws or true micrognathia, acromegaly,
and narcolepsy: This subtype is caused by exon 21 DNA (cytosine-5)- and hypothyroidism
methyltransferase-1 mutations and is characterized by late-onset § Medical consequences include cardiac arrhythmias, systemic
(age 30 to 40 years) narcolepsy (with low or intermediate CSF and pulmonary hypertension, and decreased sexual drive or
hypocretin-1 levels), deafness, cerebellar ataxia, and eventually function
dementia. § an illness of middle age, primarily in men, but can occur at any
347.00 (G47.419) Autosomal dominant narcolepsy, obesity, and type age, including children
2 diabetes: Narcolepsy, obesity, and type 2 diabetes with low CSF § OSA in adults are characterized by multiple periods of at least
hypocretin-1 levels have been described in rare cases and are 10 seconds in duration in which nasal and oral airflow ceases
associated with a mutation in the myelin oligodendrocyte completely (an apnea) or partially (a hypopnea
glycoprotein gene. § Central sleep apnea (CSA), which tends to occur in the elderly,
347.10 (G47.429) Narcolepsy secondary to another medical results from periodic failure of central nervous system (CNS)
condition: This subtype is for narcolepsy that develops secondary to mechanisms that stimulate breathing
medical conditions that cause infectious (e.g., Whipple's disease, § features of CSA are similar to those of OSA, except that, during
sarcoidosis), traumatic, or tumoral destruction of hypocretin the periods of apnea, a cessation of respiratory effort is seen
neurons. in the abdominal and chest expansion leads
Coding note (for ICD-9-CM code 347.10 only): Code first the § Several features of OSA and CSA:
underlying medical condition (e.g., 040.2 Whipple's disease; 347.10 § decreased ability to concentrate, decreased libido, memory
narcolepsy secondary to Whipple's disease). complaints, and deficits in neuropsychological testing.
§ Nasal continuous positive airway pressure (nCPAP) is the
Specify current severity: treatment of choice for OSA
Mild: Infrequent cataplexy (less than once per week), need for naps § Others: include weight loss, nasal surgery, tracheostomy, and
only once or twice per day, and less disturbed nocturnal sleep. uvulopalatoplasty
Moderate: Cataplexy once daily or every few days, disturbed § SSRIs and heterocyclic antidepressant drugs sometimes help
nocturnal sleep, and need for multiple naps daily. treat sleep apnea
Severe: Drug-resistant cataplexy with multiple attacks daily, nearly § theophylline has been shown to decrease the number of
constant sleepiness, and disturbed nocturnal sleep (i.e., movements, episodes of apnea
insomnia, and vivid dreaming). § avoid the use of sedative medication, including alcohol
Treatment CENTRAL ALVEOLAR HYPOVENTILATION
§ No cure exists for narcolepsy § refers to several conditions marked by impaired ventilation in
§ a regimen of forced naps at a regular time of day occasionally which the respiratory abnormality appears or greatly worsens
helps patients with narcolepsy and, in some cases, the only during sleep and in which no significant apneic episodes
regimen alone, without medication, can almost cure the are present
condition § inadequate tidal volume or respiratory rate during sleep
§ When medication is required, stimulants are most commonly § Death may occur during sleep (Ondine's curse).
used. § treated with some form of mechanical ventilation (e.g., nasal
§ Modafinil (Provigil), an alpha1-adrenergic receptor agonist, ventilation).
has been approved to reduce the number of sleep attacks and
to improve psychomotor performance in narcolepsy CIRCADIAN RHYTHM SLEEP DISORDER
§ tricyclic drugs or SSRIs to reduce cataplexy § includes a wide range of conditions involving a misalignment
§ scheduled naps, lifestyle adjustment, psychological between desired and actual sleep periods
counseling, drug holidays to reduce tolerance, and careful § four types of circadian rhythm sleep disorders: delayed sleep
monitoring of drug refills, general health, and cardiac status phase type, jet lag type, shift work type, and unspecified
BREATHING-RELATED SLEEP DISORDER JET LAG TYPE
§ characterized by sleep disruption leading to excessive § depending on the length of the east-to-west trip and
sleepiness or insomnia caused by a sleep-related breathing individual sensitivity
disturbance § disappears spontaneously in 2 to 7 days
§ include apneas, hypopneas, and oxygen desaturations § no specific treatment is required
§ invariably cause hypersomnia. § can prevent the symptoms by altering their mealtimes and
§ Two disorders of the respiratory system that can produce sleep times in an appropriate direction before traveling
hypersomnia : sleep apnea and central alveolar § Melatonin taken orally at prescribed times is useful
hypoventilation § Maximizing light exposure during the new daytime and
minimizing light during the new nighttime are also helpful
TRANSCRIBERS Marky, Josh, Eina 3
PSYCHIATRY III EXIMIUS
SLEEP-WAKE DISORDERS
2021
Ethel Maureen Pagaddu, MD December 2019
SHIFT WORK TYPE PARASOMNIAS
§ among night shift workers is to come home in the early NIGHTMARE DISORDER
morning, to go to bed feeling exhausted, to sleep only 2 to 3 § Nightmares are vivid dreams that become progressively more
hours, and to awaken feeling unrefreshed but unable to anxiety producing, ultimately resulting in an awakening
continue sleeping § nightmares almost always occur during REM sleep and usually
§ strategies, including napping before going into work in the after a long REM period late in the night
evening or taking a scheduled nap during nighttime work § No specific treatment is usually required for nightmare
hours, may be helpful disorder.
§ Using bright light at night and avoiding light during the day § Agents that suppress REM sleep, such as tricyclic drugs, may
have been proposed reduce the frequency of nightmares,
§ benzodiazepines have also been used
PERIODIC LIMB MOVEMENT SYNDROME
§ also known as nocturnal myoclonus SLEEP TERROR DISORDER
§ consists of highly stereotyped abrupt contractions of certain § an arousal in the first third of the night during deep NREM
leg muscles during sleep (stages III and IV) sleep
§ include extension of the toes, as well as flexion of the ankle § inaugurated by a piercing scream or cry and accompanied by
and knee behavioral manifestations of intense anxiety bordering on
§ patient is usually unaware that these movements occur, panic
although the bed partner may be only too aware § Patients may remain awake in a disoriented state, but more
§ associated with renal disease, as well as iron and vitamin B12 often fall asleep, and as with sleepwalking, they forget the
anemia; exacerbated by tricyclic antidepressants episodes
§ of middle age in both sexes, with increasing frequency with § A night terror episode after the original scream frequently
advancing age develops into a sleepwalking episode
§ PLM index of at least five per hour § About 1-6% of children have the disorder; more common in
§ No treatment for nocturnal myoclonus is universally effective boys than in girls; tends to run in families
§ may be useful include benzodiazepines, levodopa (Larodopa), § Specific treatment is seldom required
quinine, and, in rare cases, opioids § individual or family therapy is sometimes useful
§ diazepam (Valium) in small doses at bedtime improves the
RESTLESS LEGS SYNDROME condition
§ also known as Ekbom syndrome
§ an uncomfortable, subjective sensation of the limbs, usually SLEEPWALKING DISORDER
the legs, described as a “creepy crawly” feeling or as the § known as somnambulism
sensation of ants walking on the skin § consists of a sequence of complex behaviors that are initiated
§ worse at night, relieved by walking or moving about in the first third of the night during deep NREM (stage III and
§ a cause of sleep initiation insomnia,: ultimate cause is IV) sleep and frequently, although not always, “progress
unknown but it appears often in pregnancy, iron or vitamin without full consciousness or later memory of the episode” to
B12 deficiency anemia, and renal disease leaving bed and walking about
§ first step in treatment is looking for anemia and treating it § The behavior occasionally terminates in awakening, with
§ Benzodiazepines are relatively ineffective several minutes of confusion; more frequently, the person
§ off-label use of L-dopa and carbidopa , bromocriptine, and returns to sleep without any recollection of the sleepwalking
pergolide is often helpful event
§ off-label use of narcotic analgesics can help when other § begins between ages 4 and 8 and tends to dissipate in
treatments have been tried and have failed adolescence; peak prevalence is at about 12 years old
§ Ropinirole (Requip), a dopamine agonist available for § more common in boys
treatment of Parkinson's disease, now the first drug approved § tends to run in families
by the FDA for treatment of moderate to severe RLS § a minor neurological abnormality probably underlies the
condition; should not be considered purely psychogenic
KLEINE-LEVIN SYNDROME § Treatment: primarily of educating and reassuring the parents
§ a relatively rare condition consisting of recurrent periods of § Medical intervention is rarely needed for typical night terrors
prolonged sleep (from which patients may be aroused) with or sleepwalking
intervening periods of normal sleep and alert waking § in difficult cases, off-label use of benzodiazepines, which
§ During the hypersomniac episodes, wakeful periods are decrease slow-wave sleep
usually marked by withdrawal from social contacts and return
to bed at the first opportunity; patients may also display REM SLEEP BEHAVIOR DISORDER
apathy, irritability, confusion, voracious eating, loss of sexual § episodes of complex, often violent, behavior and is thought to
inhibitions, delusions, hallucinations, frank disorientation, represent a patient acting out his or her dreams
memory impairment, incoherent speech, excitation or § more common in older men
depression, and truculence. § often a history exists of a small stroke or other CNS insult in
§ Uncommon the last months or year.
§ first attack occurs between the ages of 10 and 21 years § can also appear as an early event in the evolution of
§ invariably self-limited, and enduring remission occurs Parkinson's disease
spontaneously before age 40 in early-onset cases § most widely used treatment is the off-label administration of
clonazepam , 0.5 to 2.0 mg a day
§ Carbamazepine, 100 mg three times a day, is also effective
TRANSCRIBERS Marky, Josh, Eina 4
PSYCHIATRY III EXIMIUS
SLEEP-WAKE DISORDERS
2021
Ethel Maureen Pagaddu, MD December 2019
SLEEPTALKING (SOMNILOQUY)
§ in children and adults
§ found in all stages of sleep
§ involves a few words that are difficult to distinguish
§ involve the sleeper's life and concerns, but sleeptalkers do not
relate their dreams during sleep, nor do they often reveal
deep secrets
§ sometimes accompany night terrors and sleepwalking
§ requires no treatment
SLEEP-RELATED HEAD BANGING (JACTATIO CAPITIS NOCTURNA)
§ a sleep behavior consisting chiefly of rhythmic to-and-fro head
rocking (less commonly, total body rocking) occurring just
before or during sleep
§ observed in the immediate presleep period and is sustained
into light sleep
§ uncommonly persists into, or occurs in, deep NREM sleep
§ Treatment consists of measures to prevent injury
SLEEP PARALYSIS
§ Familial sleep paralysis is characterized by a sudden inability
to execute voluntary movements, either just at the onset of
sleep or on awakening during the night or in the morning
TRANSCRIBERS Marky, Josh, Eina 5
You might also like
- AHA-PALS 2010: Pediatric Chain of SurvivalDocument10 pagesAHA-PALS 2010: Pediatric Chain of SurvivalIsabel CastilloNo ratings yet
- Pediatric Advanced Life Support: I. PALS System Approach AlgorithmDocument19 pagesPediatric Advanced Life Support: I. PALS System Approach AlgorithmIsabel Castillo100% (1)
- Abnormal Psych Case Study Assignment 1Document2 pagesAbnormal Psych Case Study Assignment 1dor8661No ratings yet
- Schizophrenia: According To StuartDocument24 pagesSchizophrenia: According To Stuartchik_1215No ratings yet
- Droogleever 2011 Narcolepsy and Psychiatry: An Evolving Association of Increasing InterestDocument6 pagesDroogleever 2011 Narcolepsy and Psychiatry: An Evolving Association of Increasing InterestlalipredebonNo ratings yet
- Psychosocial Theories in NursingDocument9 pagesPsychosocial Theories in NursingNursidar Pascual Mukattil0% (1)
- History of Psychopathology 30092020 070926pmDocument46 pagesHistory of Psychopathology 30092020 070926pmRitika ManglaniNo ratings yet
- Psychopharmacology HandoutsDocument13 pagesPsychopharmacology HandoutsAyuy Welliss MedusaNo ratings yet
- Schizophrenia in Adults - Clinical Manifestations, Course, Assessment, and Diagnosis - UpToDateDocument18 pagesSchizophrenia in Adults - Clinical Manifestations, Course, Assessment, and Diagnosis - UpToDateJose YupanquiNo ratings yet
- Introductory Textbook of Psychiatry Chapter 5Document30 pagesIntroductory Textbook of Psychiatry Chapter 5Luthfia PrasetiaNo ratings yet
- Anxiety Dis. OCD and OtherDocument6 pagesAnxiety Dis. OCD and OtherIsabel CastilloNo ratings yet
- History Psychiatry ANAMNESISDocument21 pagesHistory Psychiatry ANAMNESISDr. BrainNo ratings yet
- Function-Memory, Smell And: Persecutory / Paranoid Delusions - Involve TheDocument4 pagesFunction-Memory, Smell And: Persecutory / Paranoid Delusions - Involve TheMark Christian CaasiNo ratings yet
- PSYCH 2.1 Anxiety DisordersDocument17 pagesPSYCH 2.1 Anxiety DisordersZazaNo ratings yet
- HISTORY of Abnormal PsychologyDocument12 pagesHISTORY of Abnormal PsychologyDaisy AllenNo ratings yet
- Objectives: Schizophrenia. Cause, Pathophysiology: WomenDocument11 pagesObjectives: Schizophrenia. Cause, Pathophysiology: WomenDuha B. SalimNo ratings yet
- History of PsychiatryDocument8 pagesHistory of PsychiatryAngie MandeoyaNo ratings yet
- Psych GENDER IDENTITY DISORDERS TRANSDocument8 pagesPsych GENDER IDENTITY DISORDERS TRANSIsabel CastilloNo ratings yet
- Conrad - Delusional Mood, Psychosis, and Beginning of SDocument5 pagesConrad - Delusional Mood, Psychosis, and Beginning of SLajos HorváthNo ratings yet
- The Extended Bio-Psycho-Social Model: A Few Evidences of Its EffectivenessDocument3 pagesThe Extended Bio-Psycho-Social Model: A Few Evidences of Its EffectivenessHemant KumarNo ratings yet
- Module 4: Mood Disorders: Disorders and Individuals With Bipolar Disorders. The Key Difference BetweenDocument7 pagesModule 4: Mood Disorders: Disorders and Individuals With Bipolar Disorders. The Key Difference BetweenLiz Evermore0% (1)
- Bipolar Disorder in Children and Adolescents An Update On DiagnosisDocument12 pagesBipolar Disorder in Children and Adolescents An Update On DiagnosisLAURA FRITSCHE GARCIANo ratings yet
- Chapter 7 Study GuideDocument4 pagesChapter 7 Study GuidejbradeeNo ratings yet
- Somatoform and Sleep DisordersDocument18 pagesSomatoform and Sleep DisordersedhobiondiNo ratings yet
- Behaviour ModificationDocument26 pagesBehaviour ModificationtulsiNo ratings yet
- Mental Health Case StudyDocument13 pagesMental Health Case Studyapi-590353096No ratings yet
- PsyDocument12 pagesPsyImaneNo ratings yet
- Hallucination PDFDocument10 pagesHallucination PDFfebriantinurulwNo ratings yet
- Delirium: EpidemiologyDocument8 pagesDelirium: EpidemiologyNunuNo ratings yet
- Stress-Related Disorders: Dissociative DisordersDocument36 pagesStress-Related Disorders: Dissociative Disorderspranay javeriNo ratings yet
- Depression in Older PeopleDocument4 pagesDepression in Older PeopleAlina AlinaNo ratings yet
- Schizophrenia: Psychiatric DisordersDocument33 pagesSchizophrenia: Psychiatric DisordersNdoo Ndoo100% (1)
- Mental Disorder Schizophrenia Schizophrenia (Document9 pagesMental Disorder Schizophrenia Schizophrenia (Adriano SonnyNo ratings yet
- Dissociation DisorderDocument33 pagesDissociation DisorderVaibhav KrishnaNo ratings yet
- Format of Study: 1 Dr. G. Jayarama, Reader & Hod-Clinical PsychologyDocument16 pagesFormat of Study: 1 Dr. G. Jayarama, Reader & Hod-Clinical PsychologyAppas SahaNo ratings yet
- Schizophrenia: Signs and SymptomsDocument6 pagesSchizophrenia: Signs and SymptomsTherese ArambuloNo ratings yet
- Schizophrenia: Onset of Symptoms Typically Occurs in Young Adulthood, With Around 0.4-0.6% of TheDocument3 pagesSchizophrenia: Onset of Symptoms Typically Occurs in Young Adulthood, With Around 0.4-0.6% of ThepapatukNo ratings yet
- Epilepsy 1Document66 pagesEpilepsy 1bbc_dkkNo ratings yet
- Major Depression Disorder: Mars Hervie S. Cuchapin, RPH NeurologyDocument8 pagesMajor Depression Disorder: Mars Hervie S. Cuchapin, RPH NeurologyLoren SangalangNo ratings yet
- Neurocognitive DisorderDocument50 pagesNeurocognitive DisorderMechaela SiasatNo ratings yet
- Chapter 14 Psychological Disorders.Document9 pagesChapter 14 Psychological Disorders.BorisVanIndigoNo ratings yet
- Joshua Dodot Case StudyDocument2 pagesJoshua Dodot Case StudyJoshua Ringor100% (1)
- Antidepressants For The Treatment of NarcolepsyDocument5 pagesAntidepressants For The Treatment of NarcolepsyMOHAMAD FAKIHNo ratings yet
- Behavioral Management of HipersomniaDocument7 pagesBehavioral Management of HipersomniaHernán MarínNo ratings yet
- Recreational Therapy: Ms. Priyanka Kumari F.Y. M.Sc. NursingDocument22 pagesRecreational Therapy: Ms. Priyanka Kumari F.Y. M.Sc. NursingHardeep KaurNo ratings yet
- Disorders of Thought and SpeechDocument50 pagesDisorders of Thought and SpeechTilarupa BhattaraiNo ratings yet
- Dissociative DisordersDocument24 pagesDissociative DisordersSimón Ortiz LondoñoNo ratings yet
- Notes For ExamDocument37 pagesNotes For ExamKristine Violon SecorinNo ratings yet
- Phenomenology Yr4Document52 pagesPhenomenology Yr4Mohd ImranNo ratings yet
- Case Analysis Assignment: Interpersonal and Social Rhythm TherapyDocument2 pagesCase Analysis Assignment: Interpersonal and Social Rhythm TherapyJoshua RingorNo ratings yet
- Half Life of FactsDocument8 pagesHalf Life of FactsDino Mozardien100% (1)
- Notes On Dissociative DisordersDocument7 pagesNotes On Dissociative DisordersPrince Rener Velasco PeraNo ratings yet
- Bipolar and Related DisordersDocument31 pagesBipolar and Related DisordersNoelle Grace Ulep BaromanNo ratings yet
- DelusionsDocument8 pagesDelusionsvenkyreddy97No ratings yet
- Chapter 7 - Somatoform and Dissociative Disorders: B32: AbnormalDocument14 pagesChapter 7 - Somatoform and Dissociative Disorders: B32: AbnormalNiky GiaccioNo ratings yet
- 1 - What Is CounsellingDocument27 pages1 - What Is CounsellingveronicaNo ratings yet
- SchezophreniaDocument22 pagesSchezophreniaxion_mew2No ratings yet
- Cognitive Case Formulation Science or Science Fiction PDFDocument18 pagesCognitive Case Formulation Science or Science Fiction PDFNicole Flores MuñozNo ratings yet
- SOCPDocument3 pagesSOCPALEXZANDRA CLEMENTENo ratings yet
- Columbia Suicide Severity Rating Scale Screen VersionDocument2 pagesColumbia Suicide Severity Rating Scale Screen VersionPaul SmithNo ratings yet
- Opioid Chapter 2Document7 pagesOpioid Chapter 2Likoh TimothyNo ratings yet
- Surgical Pathology - Major and Minor Salivary GlandsDocument2 pagesSurgical Pathology - Major and Minor Salivary GlandsIsabel CastilloNo ratings yet
- Ok Ok Notes PediaDocument10 pagesOk Ok Notes PediaIsabel CastilloNo ratings yet
- Dermatology - Skin NeoplasmsDocument12 pagesDermatology - Skin NeoplasmsIsabel CastilloNo ratings yet
- Pediatric Therapeutics: Eximius 2021Document13 pagesPediatric Therapeutics: Eximius 2021Isabel CastilloNo ratings yet
- Dermatology - Exanthematous Viral DiseasesDocument6 pagesDermatology - Exanthematous Viral DiseasesIsabel CastilloNo ratings yet
- DERMATOLOGY - Cuteneous Candidiasis, PityrosporumDocument4 pagesDERMATOLOGY - Cuteneous Candidiasis, PityrosporumIsabel CastilloNo ratings yet
- SURGICAL PATHOLOGY SOFT TISSUES TableDocument4 pagesSURGICAL PATHOLOGY SOFT TISSUES TableIsabel CastilloNo ratings yet
- EMBRYOGENESIS and Fetal DevtDocument50 pagesEMBRYOGENESIS and Fetal DevtIsabel CastilloNo ratings yet
- Surgical Pathology - CNSDocument2 pagesSurgical Pathology - CNSIsabel CastilloNo ratings yet
- Diseases of The Newborn: ObjectivesDocument17 pagesDiseases of The Newborn: ObjectivesIsabel CastilloNo ratings yet
- Growth and DevelopmentDocument60 pagesGrowth and DevelopmentIsabel CastilloNo ratings yet
- Implantataion Placental Development and AbnormalitiesDocument62 pagesImplantataion Placental Development and AbnormalitiesIsabel CastilloNo ratings yet
- Acute Appendicitis and Peritonitis: RLQ, To The Pelvis, Right FlankDocument4 pagesAcute Appendicitis and Peritonitis: RLQ, To The Pelvis, Right FlankIsabel CastilloNo ratings yet
- Pneumonia: TranscribersDocument6 pagesPneumonia: TranscribersIsabel CastilloNo ratings yet
- Adolescent Medicine: Early AdolescenceDocument2 pagesAdolescent Medicine: Early AdolescenceIsabel CastilloNo ratings yet
- Interatitial Lung DiseaseDocument2 pagesInteratitial Lung DiseaseIsabel CastilloNo ratings yet
- Irritable Bowel SyndromeDocument3 pagesIrritable Bowel SyndromeIsabel CastilloNo ratings yet
- Pedia Pre School NewsDocument3 pagesPedia Pre School NewsIsabel CastilloNo ratings yet
- Acute and Chronic PancreatitisDocument8 pagesAcute and Chronic PancreatitisIsabel CastilloNo ratings yet
- Approach To The Patient With Disease of The Respiratory SystemDocument3 pagesApproach To The Patient With Disease of The Respiratory SystemIsabel CastilloNo ratings yet
- Inflammatory Bowel Disease: Microorganisms That Drive DiseaseDocument4 pagesInflammatory Bowel Disease: Microorganisms That Drive DiseaseIsabel CastilloNo ratings yet
- AsthmaDocument4 pagesAsthmaIsabel CastilloNo ratings yet
- Causes of HypothyroidismDocument6 pagesCauses of HypothyroidismIsabel Castillo100% (1)
- Pack-Years of Cigarette Smoking Is The Most HighlyDocument5 pagesPack-Years of Cigarette Smoking Is The Most HighlyIsabel CastilloNo ratings yet
- Mesenteric Vascular Insufficiency: ClassificationDocument2 pagesMesenteric Vascular Insufficiency: ClassificationIsabel CastilloNo ratings yet
- Anorectal Disease and Common Anorectal DisordersDocument2 pagesAnorectal Disease and Common Anorectal DisordersIsabel CastilloNo ratings yet
- Hyperthyroidism: EpidemiologyDocument8 pagesHyperthyroidism: EpidemiologyIsabel CastilloNo ratings yet
- Diseases of Esophagus.Document3 pagesDiseases of Esophagus.Isabel Castillo100% (2)
- Lou Gehrigs Disease PresentationDocument15 pagesLou Gehrigs Disease PresentationAdi ParamarthaNo ratings yet
- MigraineDocument51 pagesMigraineIndraYudhiNo ratings yet
- Laporan Geriatri Bulan Jan, Feb, MaretDocument54 pagesLaporan Geriatri Bulan Jan, Feb, MaretnisaNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakaFrans JobethNo ratings yet
- Ei Diag Conditions ListDocument2 pagesEi Diag Conditions ListThuran NathanNo ratings yet
- Progressive Supranuclear Palsy. Kam Newman, Saeed KahkeshaniDocument1 pageProgressive Supranuclear Palsy. Kam Newman, Saeed KahkeshanijingerbrunoNo ratings yet
- This Is Sample ArticleDocument3 pagesThis Is Sample ArticleilalcNo ratings yet
- Brain Imaging Abnormalities in Autism DisordersDocument3 pagesBrain Imaging Abnormalities in Autism DisordersasclepiuspdfsNo ratings yet
- GC EncephilitisDocument1 pageGC EncephilitisCik MunirahNo ratings yet
- SeizureDocument10 pagesSeizureRomeo ReyesNo ratings yet
- Sleep Disordered Breathing and Anesthesia: DefinitionsDocument1 pageSleep Disordered Breathing and Anesthesia: DefinitionsMuhammad SyammNo ratings yet
- Oscillopsia Is The Illusion of Oscillation of The Visual Surroundings While Vertigo Refers To A Sense of Spinning or Other Motion That May Be PhysiologicalDocument2 pagesOscillopsia Is The Illusion of Oscillation of The Visual Surroundings While Vertigo Refers To A Sense of Spinning or Other Motion That May Be PhysiologicalRubie Ann TillorNo ratings yet
- Pemicu 3 Kelompok 14: Kamis, 8 Oktober 2020Document54 pagesPemicu 3 Kelompok 14: Kamis, 8 Oktober 2020Ceryle EriadyNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaAngga Wahyu PerdanaNo ratings yet
- Exercise For CoordinationDocument19 pagesExercise For Coordinationbpt250% (2)
- Autism Spectrum OET-Reading-14Document25 pagesAutism Spectrum OET-Reading-14Aravind JosephNo ratings yet
- Behaviour And/or Feelings.: Published March 2022Document1 pageBehaviour And/or Feelings.: Published March 2022Var InderNo ratings yet
- Kristin Neff - Self-CompassionDocument4 pagesKristin Neff - Self-CompassionKrishnaNo ratings yet
- Parkinsonism 0Document3 pagesParkinsonism 0keroNo ratings yet
- Speech OutlineDocument4 pagesSpeech Outlineapi-335645447No ratings yet
- About Frontotemporal DementiaDocument2 pagesAbout Frontotemporal DementiaRuwanthi FonsekaNo ratings yet
- Cerebral PalsyDocument55 pagesCerebral PalsyFuküi AliNo ratings yet
- Parkinsons DiseaseDocument37 pagesParkinsons DiseaseAi-ni BautistaNo ratings yet
- PT Neuro & Bio-Engi. MCQDocument19 pagesPT Neuro & Bio-Engi. MCQmanish singhNo ratings yet
- Chronic Paroxysmal Hemicrania Neurological-Conditions/chronic-Paroxysmal-Hemicrania)Document2 pagesChronic Paroxysmal Hemicrania Neurological-Conditions/chronic-Paroxysmal-Hemicrania)fitriaNo ratings yet
- Cerebral InfractionDocument2 pagesCerebral InfractionEdsel MagnoNo ratings yet
- Table 57-3 - Early Cognitive Symptoms Associated With DifferenDocument3 pagesTable 57-3 - Early Cognitive Symptoms Associated With DifferenDragutin PetrićNo ratings yet
- PACES 10 - CNS - Speech & Higher Cortical FunctionsDocument6 pagesPACES 10 - CNS - Speech & Higher Cortical FunctionsDrShamshad KhanNo ratings yet
- Copy-A CASE OF ALTERED SENSORIUM - ALOKDocument37 pagesCopy-A CASE OF ALTERED SENSORIUM - ALOKAlok MohanNo ratings yet
- Alzheimer's Disease: PathophysiologyDocument3 pagesAlzheimer's Disease: PathophysiologyMello D. ConsulNo ratings yet